Short abstract
Objective
To compare the effectiveness, accuracy, and surgical safety of a navigation technique with those of a traditional technique for intraoperative mandibular angle osteotomy.
Methods
Forty-three postsurgical patients with mandibular angle hypertrophy who were admitted to our Department from June 2014 to June 2017 were retrospectively reviewed. Of these patients, 23 underwent mandibular angle osteotomy using computer-assisted navigation (navigation group), and 20 underwent osteotomy using a traditional technique (traditional group). Postoperative computed tomography images were analyzed by three-dimensional software. Each patient’s facial proportion indices were measured using Mimics 19.0 software, and statistical comparisons and analyses were performed preoperatively and postoperatively.
Results
The postoperative facial contour morphology and facial proportion were improved in both groups; the navigation group showed greater improvement. The difference between the predicted and postoperative values was smaller in the navigation group than traditional group. The postoperative shape of the mandibular angle sample was similar to the preoperative predicted shape in the navigation group. No complications occurred in the navigation group, but paresthesia occurred in 17% of patients in the traditional group.
Conclusions
Mandibular angle osteotomy aided with computer-assisted navigation is more effective, accurate, and safe than the traditional technique and represents a promising clinical approach.
Keywords: Mandibular angle osteotomy, surgical navigation, accuracy, effectiveness, safety, mandibular angle hypertrophy
Introduction
A prominent mandibular angle is characteristic of a square or trapezoidal facial appearance. This facial characteristic has been viewed as rough or masculine in some cultures, which has led to a negative body image particularly in young Asian women who exhibit this contour symmetry. Because Oriental culture views an elliptical and slim facial profile as more feminine and beautiful, mandibular angle osteotomy (MAO) continues to be the most important and frequently requested procedure in craniofacial contouring surgery.1–3 However, the anatomical location of the mandible is where critical blood vessels and nerves converge, thus increasing the surgical risks.4
During the actual operation, the visual field is narrowed to a gap between the mouth and the mandible, and retractors can easily cause damage to the mandibular branch of the facial nerve. Surgical success relies largely on the surgeon’s clinical experience and interpretation of the preoperative computed tomography (CT) images, but the tissue structure and the adjoining relationship of the intraoperative mandible cannot be visualized in real time. This can lead to multiple complications such as massive bleeding, accidental mandibular fractures, facial nerve injury, and a second mandibular fracture line. Perfection and optimization of the mandibular surgical technique to achieve the expected efficacy and reduce the probability of complications is the goal of all plastic surgeons.5–9
The availability of sophisticated techniques such as image-guided surgery has broadened, and the application of this technology in craniomaxillofacial surgery has grown in recent years. Image-guided surgery integrates the preoperative imaging data into a three-dimensional (3D), multiplanar, computerized reconstruction of the asymmetric oral cavity. By visualizing the physical landmarks of the tissue using the radiographic map, a preoperative simulation of the surgical plan can be prepared. In addition, image-guided surgery can be used for image-guided navigation during the surgical procedure and evaluation of the postoperative efficacy of the procedure. Although not a substitute for operative experience, image-guided surgery can improve the accuracy of surgery, reduce risks, and ensure postoperative efficacy.10,11 The goal of this study was to compare the effectiveness, accuracy, and surgical safety of computer-navigated MAO with those of MAO performed by the traditional surgical approach.
Materials and methods
Patients
We retrospectively reviewed postsurgical patients with mandibular angle hypertrophy who were admitted to the Plastic and Reconstructive Surgery Department from June 2014 to June 2017. The study population comprised patients who underwent MAO assisted by computer navigation (navigation group) and patients who underwent MAO using the traditional technique (traditional group). All surgeries were performed by the same team of senior surgeons who had at least 10 years of operative experience in craniofacial surgery. The team was also specialized in operating the computer-assisted navigation system used in this study.
Preoperative analysis and study design
CT data from each patient were obtained using a spiral CT scanner (Lightspeed 16, model no. 5232083-8; GE Healthcare, Milwaukee, WI, USA).These digital imaging and communications in medicine (DICOM) files were imported into Mimics 19.0 software (Materialise, Leuven, Belgium) to render a 3D image of the mandible and soft tissues. Surgical procedures were performed virtually on cutting planes that were generated to ensure the desire outcome (Figure 1).
Figure 1.
The preoperative design was created using computer-aided design software. (a) Left oblique view. (b) Cutting planes planned by the software and prepared as the assisted information for MAO and (c) Left virtual postoperative view.
Mimics 19.0 software was used to perform 3D cephalometric measurements of each patient’s facial proportion indices. The facial proportion indices were the widest part of the midface (WM) (widest distance between the bilateral zygomatic arches), the widest part of the lower face (WL) (distance between the mandibular angles on both sides), and the facial height (FH) (distance from the nasal roots to the infraorbital point). The mandibular angle was also measured for each patient during preoperative preparation and at the postoperative follow-up visits. This angle is the intersection of two tangents: the ascending branch of the mandible tangent to the posterior edge of the condyle, and the tangent that reaches the lowest part of the lower mandible. Preoperative and postoperative data were statistically analyzed.
Surgical technique
Computer-assisted navigation
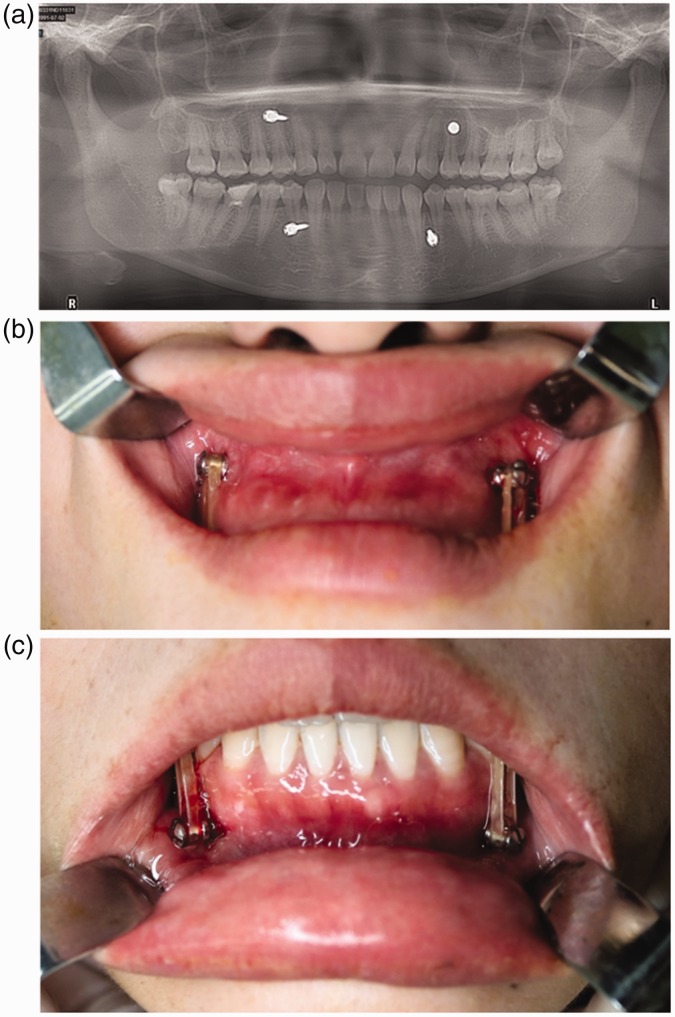
Before CT scanning, four traction screws were implanted into the alveolar bone on the cheek side of the bilateral upper and lower cuspids and the first premolar under local anesthesia (Figure 2). A fixation screw with an elastic snare was used to ensure that the occlusal relationship was stable and the mandible had no movement. The data of the preoperative osteotomy plan could then be imported into the surgical navigation system for 3D real-time visualization during surgery after CT scanning and establishment of the cutting plan design.
Figure 2.
Traction screw implantation.
A navigation reference support was installed on the right side of the patient’s head (Figure 3(a)). The surgeon then stabilized the occlusal relationship with a wire-jaw ligation to ensure that the mandible was inactive under general anesthesia (Figure 3(b)). Subperiosteal separation was performed to expose the lateral mandibular angle, mandibular edge, and part of the medial surface. The navigation probe was used to locate the osteotomy points (Figure 3(c) and (d)), and a pencil was used to mark the mandibular angle of the outer plate (Figure 3(e)). To determine the osteotomy plane and thickness, a navigation blade was used to accurately guide the MAO with real-time navigation aids (Figure 3(f)). The mandibular angle was removed completely, and the mandible was smoothed.
Figure 3.
Surgical procedures. (a) Probe marker position. (b) Intermaxillary ligation. (c, d) Navigation support mounting and (e, f) Guided osteotomy using pencil markers.
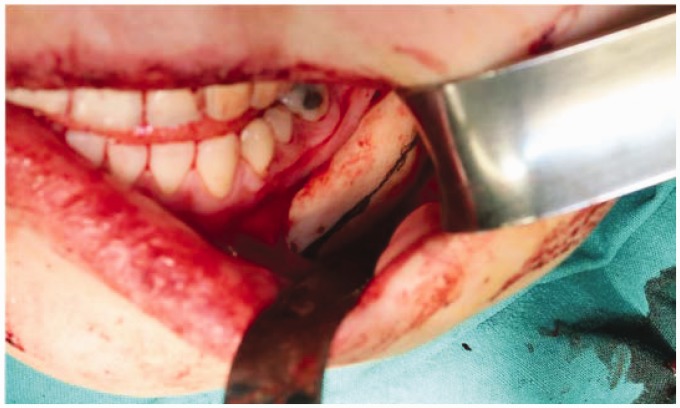
Traditional technique
The osteotomy line was determined by the surgeon based on the relationship between the osteotomy and the mandibular angle. The cutting plane was performed at the appropriate location and angulation by gross visualization (Figure 4). The two bone segments were then compared to ensure symmetry. If the incision was not appropriate or accurate, the osteotomy was modified.
Figure 4.
An incision line was made using a pencil under gross visualization in the traditional group.
Postoperative measurement and assessment
At the follow-up visits (6 months to 2 years), the patients underwent cranial CT examination and 3D skull reconstruction. The measurement indices were the same as those used before the operation (WL, FH, and WM). The WM/WL, WM/FH, and WL/FH ratios were calculated from hard tissue and soft tissue.12 The preoperative and postoperative facial measurement data were statistically analyzed.
The preoperatively predicted MAO and the postoperative mandibular angle specimens were subjected to CT scans and 3D reconstruction. The mandibular angle model was reconstructed using Mimics 19.0 software. The STL format data were imported into Rapidform 2006 software (INUS Technology, Seoul, South Korea), and the preoperatively predicted osteotomy was performed. Morphological comparisons with the postoperative mandibular angle alignment showed overlapping images on the same coordinate point. The software used different colors to highlight differences between predicted outcomes and postoperative results, and the accuracy of the osteotomy was visually displayed.
During the postoperative examinations, the patients were questioned and examined for the presence of postoperative complications such as numbness, hematoma, mandibular fracture, facial asymmetry, angulation deformity in the mandibular body after MAO, and infection. Any reports or observations of postoperative complications were recorded in the patient’s chart.
Statistical analysis
The mandibular angle model was reconstructed using Mimics 19.0 software, and the STL format data were imported into Rapidform 2006 software. SPSS 19.0 software (IBM Corp., Armonk, NY, USA) was used for the statistical analysis, and the matched t-test was used to determine statistical significance (P < 0.05 indicated significant differences). Normalized measurement data are presented as mean ± standard deviation.
Ethics
This study was approved by the internal review board of the Ninth People’s Hospital of the Shanghai Jiao Tong University School of Medicine, and all procedures complied with the ethical standards of the 1964 Helsinki declaration and its later amendments. All methods were performed in accordance with the relevant guidelines and regulations. Written informed consent was obtained from all patients prior to performance of the advanced digital imaging and MAO.
Results
Patients
In total, 43 patients were included in this study. The navigation group comprised 23 patients, and the traditional group comprised 20 patients. All patients were female; other demographic and radiographic data are presented in Table 1. The mean patient age in the navigation group was 28.17 ± 5.56 years (range, 19–43 years), and that in the traditional group was 27.65 ± 3.90 years (range, 23–44 years).
Table 1.
Demographic data of the patients in the two groups.
| Navigation group | Traditional group | |
|---|---|---|
| Patients, n | 23 | 20 |
| Sex | Female | Female |
| Age at operation, y | 28.17 ± 5.56 | 27.65 ± 3.90 |
Effectiveness
The preoperative low-angle mandibular angle hypertrophy showed significant postoperative improvements in both groups. In the navigation group, the right mandibular angle significantly increased from 108.71° ± 3.80° to 125.32° ± 3.68°, while the left mandibular angle increased from 108.54° ± 4.0° to 125.03° ± 4.36° (P < 0.001). The WL significantly decreased from 101.54 ± 2.92 to 97.46 ± 3.07 mm (P < 0.001). The WM/WL ratio increased from 1.27 ± 0.04 to 1.32 ± 0.05, and the WL/FH ratio significantly decreased from 0.87 ± 0.03 to 0.84 ± 0.04 (P < 0.001). In the traditional group, the right mandibular angle increased from 108.67° ± 4.02° to 124.82° ± 3.51°, while the left mandibular angle significantly increased from 108.56° ± 4.20° to 124.48° ± 4.08° (P < 0.001). The WL decreased from 101.69 ± 2.90 to 98.49 ± 3.14 mm (P < 0.001). The WM/WL ratio significantly increased from 1.26 ± 0.043 to 1.30 ± 0.053, and the WL/FH ratio decreased from 0.87 ± 0.037 to 0.85 ± 0.040 (P < 0.001). These results indicate that the patients who underwent navigation-assisted surgery exhibited greater improvements in their postoperative facial contour morphologies and facial proportions than did patients who underwent surgery via the traditional approach (Table 2).
Table 2.
Three-dimensional measurements of facial bones before and after mandibular osteotomy in the two groups.
|
Navigation group |
Traditional group |
|||||
|---|---|---|---|---|---|---|
| Facial morphometry | Preop | Postop | P | Preop | Postop | P |
| Right mandibular angle | 108.71° ± 3.80° | 125.32° ± 3.68° | <0.001 | 108.67° ± 4.02° | 124.82° ± 3.51° | <0.001 |
| Left mandibular angle | 108.54° ± 4.00° | 125.03° ± 4.36° | <0.001 | 108.56° ± 4.20° | 124.48° ± 4.08° | <0.001 |
| WL, mm | 101.54 ± 2.92 | 97.46 ± 3.07 | <0.001 | 101.69 ± 2.90 | 98.49 ± 3.14 | <0.001 |
| WM/WL | 1.27 ± 0.04 | 1.32 ± 0.05 | <0.001 | 1.26 ± 0.043 | 1.30 ± 0.053 | <0.001 |
| WL/FH | 0.87 ± 0.03 | 0.84 ± 0.04 | <0.001 | 0.87 ± 0.037 | 0.85 ± 0.040 | <0.001 |
FH = facial height; WM = widest part of the midface; WL = widest part of the lower face; Preop = preoperative; Postop = postoperative.
Accuracy
The facial indicators and mandibular angle volumetrics of the two groups were measured, and the differences between the preoperative predicted values and postoperative values were calculated. In the navigation group, the left mandibular angle volumetric discrepancy was 0.15 ± 0.06 mm³, while the right mandibular angle volumetric discrepancy was 0.06 ± 0.03 mm³. In the traditional group, the left mandibular angle volumetric discrepancy was 0.35 ± 0.16 mm³, and the right mandibular angle volumetric discrepancy was 0.31 ± 0.12 mm³ (P < 0.001). A statistical analysis was conducted to evaluate the accuracy of the procedure by comparing the discrepancy between the two groups, and no other variables were statistically different (Table 3).
Table 3.
Comparison of differences between preoperative predicted values and postoperative values between the two groups.
|
Volume of mandibular angle, mm³ |
Mandibular angle |
WL, cm | WM/WL | WL/FH | |||
|---|---|---|---|---|---|---|---|
| Left side | Right side | Right side | Left side | ||||
| Navigation | 0.15 ± 0.06 | 0.06 ± 0.03 | 3.33° ± 3.67° | 2.52° ± 2.16° | 1.83 ± 1.41 | 0.02 ± 0.02 | 0.01 ± 0.01 |
| Traditional | 0.35 ± 0.16 | 0.31 ± 0.12 | 2.65° ± 1.69° | 2.16° ± 1.42° | 1.92 ± 1.16 | 0.03 ± 0.02 | 0.02 ± 0.01 |
| P-value | <0.001 | <0.001 | >0.05 | >0.05 | >0.05 | >0.05 | >0.05 |
FH = facial height; WM = widest part of the midface; WL = widest part of the lower face.
In the navigation group, Mimics 19.0 software was used to perform preoperative–postoperative mandibular angle 3D reconstructions and human–computer interaction registrations. Blue colors indicated the preoperatively predicted mandibular angle morphology, and gray colors indicated the reconstruction of the mandibular angle specimens after surgery. Regions that overlapped between the preoperative and postoperative conditions were colored gray (Figure 5(a)). Rapidform 2006 software was used for preoperative design and analysis of surface differences in the mandibular angle samples (Figure 5(b)). In the traditional group, however, multiple osteotomies were performed and the 3D reconstruction of the mandibular angle morphology was therefore prone to errors compared with the preoperative design; thus, no reference value was obtained in the traditional group. These results suggest that greater similarity between the postoperative mandibular angle sample morphology and the preoperative prediction results was obtained in the navigation than traditional group.
Figure 5.
Three-dimensional (3D) reconstruction and analysis of mandibular angles. (a) Mimics 19.0 software was used to create 3D reconstructions of preoperative (blue) and postoperative (gray) mandibular angles. (b) Rapidform 2006 software was used to analyze the difference between the preoperative design and the mandibular angle samples.
Safety
All 23 patients in the navigation group recovered well after surgery. They were discharged from the hospital 1 week after the operation, and soft tissue swelling resolved or was significantly reduced after 2 to 3 weeks. The patients received follow-up care for postoperative facial measurements and to report any complications. No complications were reported, and no patients required secondary repairs. Of the 20 patients in the traditional group, 3 patients reported numbness (paresthesia), and 1 of these 3 still showed no recovery 6 months postoperatively. No other complications were identified or reported (Table 4).
Table 4.
Complications in the two surgical groups.
|
Navigation group |
Traditional group |
|||
|---|---|---|---|---|
| Complications | Case | Treatment | Case | Treatment |
| Paresthesia | 0 | – | 3 (17.4%) | Neurotrophic signs, close follow-up |
| Transitory (<6 months) | 0 | – | 2 | – |
| Duration (>6 months) | 0 | – | 1 | – |
| Hematoma | 0 | – | 0 | – |
| Mandible fracture | 0 | – | 0 | – |
| Facial asymmetry | 0 | – | 0 | – |
| Secondary mandibular angle | 0 | – | 0 | – |
| Infection | 0 | – | 0 | – |
| Altogether | 0 | – | 3 | – |
Discussion
With the growing influence of fashion and media, increasingly more young Asian women are expressing a preference for the softer or more feminine appearance of an egg-shaped face. Therefore, the number of plastic surgeries to correct the mandibular angle has increased in East Asian countries. The structural bone interactions in this region are complex, limiting the oral field and making precise location of the osteotomy lines through an intraoral incision the most important and challenging aspect of the operation.13–15 Although various modifications have been made to MAO, improvements in the efficiency and accuracy of surgery are required.
With the development of high-tech digital imaging technology, many computer software programs have been applied to formulate preoperative planning on 3D skeletal models extracted from CT images. This advancement reduces the difficulty of preoperative planning, and the real-time navigation system can transfer the preoperative plan to the actual surgery to optimize the accuracy and efficiency of the operation.16
Many studies have applied real-time navigation systems to actual operations.17–20 In 1908, the first intraoperative navigation technique was used in neurosurgery by Horsley and Clarke.21 Since then, intraoperative navigation has developed rapidly, especially in the areas of complex anatomy such as the head and neck. In maxillofacial surgery, navigation techniques are mainly used in temporomandibular joint arthroplasty, reduction of maxillofacial fractures, tumor resection, and foreign body removal. This represents a major improvement in the management of complex cases with no loss of anatomy, allowing surgeons to understand the operating area in real time.22
However, limited research has been performed to compare intraoperative navigation with traditional techniques in the field of plastic surgery.23 Ma et al.24 compared the accuracy and precision of image-based navigation against individualized guides for distal radius osteotomy. Cheng et al.25 conducted a meta-analysis to determine whether computer-assisted surgery provides a superior mechanical leg axis, and we conducted the present study to compare the accuracy, efficacy, and safety of navigation-assisted versus traditional MAO.
Many factors were analyzed in the present study, including facial morphometry before and after MAO, the difference between preoperative predicted values and postoperative values, and documented complications. Navigation-assisted MAO has significant advantages over traditional MAO. In terms of effectiveness, postoperative facial contour morphologies and facial proportions improved significantly compared with those in patients who underwent traditional surgery. Under the guidance of the navigation system, additional mandibular angle tissue can be removed without damaging the blood vessels and nerves. In terms of accuracy, the difference between the preoperative predicted values and postoperative values of the mandibular angle volumetric data were smaller in the navigation than traditional group, and the range and angle of the osteotomy could be modified similar to the predicted value under navigation assistance. However, the surgeon performed the intraoperative osteotomy without the aid of a surgical microscope or other visual technology in the traditional surgery group. In terms of safety, the navigation-assisted MAO approach is safer for patients. The range of lesions and the surrounding anatomical structures were accurately located and the structure of important vascular nerve tissues was protected using intraoperative navigation. Moreover, the real-time 3D navigation allowed visualization of the operation without any visual obstructions. The combination of virtual and actual results effectively reduced the occurrence of complications. This is illustrated by the fact that no complications occurred in the navigation-assisted group compared with 17.4% in the traditional surgery group.
Nevertheless, navigational operations must still overcome technology-related difficulties such as systematic errors, image errors, registration errors, and operational errors. Because of the special anatomy of the mandible, intraoperative instability causes displacements that lead to deviations from the preoperative CT image position.26,27 In this study, all patients treated by navigation-assisted surgery underwent intermaxillary ligature before CT imaging to prevent errors in image registration.28,29 Despite these disadvantages, we believe that navigation assistance is effective, accurate, and safe and that it is a promising approach for plastic surgery procedures such as MAO.
Conclusion
The navigation-assisted technique proved to be more effective, accurate, and safe than the traditional surgical approach. This study has demonstrated that computer navigation-aided MAO is a valuable surgical approach with direct clinical applicability.
Acknowledgments
The authors would like to thank the research staff and clinical personnel of the Shanghai 9th People’s Hospital for their outstanding performance and patient care. The authors would also like to thank Dr. Bai Shan-shan for proofreading the manuscript.
Declaration of conflicting interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
This work was supported by the National Natural Science Foundation of China (Grant No. 81471886) and the Medical-Engineering Cross Foundation of Shanghai Jiaotong University (Grant No. YG2015QN06).
References
- 1.Satoh K, Mitsukawa N. Mandibular marginal contouring in oriental aesthetic surgery: refined surgical concept and operative procedure. Ann Plast Surg 2014; 72: 498–502. 2013/05/03. DOI: 10.1097/SAP.0b013e31826a18d3. [DOI] [PubMed] [Google Scholar]
- 2.Khadka A, Hsu Y, Hu J, et al. Clinical observations of correction of square jaw in East Asian individuals. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2011; 111: 428–434. 2010/09/30. DOI: 10.1016/j.tripleo.2010.05.061. [DOI] [PubMed] [Google Scholar]
- 3.Kim SK, Han JJ, Kim JT. Classification and treatment of prominent mandibular angle. Aesthetic Plast Surg 2001; 25: 382–387. 2001/11/03. DOI: 10.1007/s002660010150. [DOI] [PubMed] [Google Scholar]
- 4.Ye N, Long H, Zhu S, et al. The accuracy of computer image-guided template for mandibular angle ostectomy. Aesthetic Plast Surg 2015; 39: 117–123. 2014/12/30. DOI: 10.1007/s00266-014-0424-1. [DOI] [PubMed] [Google Scholar]
- 5.Chen H, Sun J, Wang J. Reducing prominent mandibular angle osteotomy complications: 10-year retrospective review. Ann Plast Surg 2018; 81: S5–S9. 2018/02/27. DOI: 10.1097/sap.0000000000001372. [DOI] [PubMed] [Google Scholar]
- 6.Kang M. Incidence of complications associated with mandibuloplasty: a review of 588 cases over 5 years. Plast Reconstr Surg Glob Open 2014; 2: e139. 2014/10/08. DOI: 10.1097/gox.0000000000000090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yuan Q, Liu DL, Wang XJ. Analysis of the complications resulted from intraoral mandibular angle reduction. Zhonghua Zheng Xing Wai Ke Za Zhi 2009; 25: 197–199. 2009/10/07. DOI: 10.1360/972009-1549. [PubMed] [Google Scholar]
- 8.Huang LP, Gui L, Zhang ZY, et al. Analysis of the complications following correction of mandibular angle prominence. Zhonghua Zheng Xing Wai Ke Za Zhi 2003; 19: 364–366. 2004/06/08. DOI: 10.1139/y80-200. [PubMed] [Google Scholar]
- 9.Yang DB, Song HS, Park CG. Unfavorable results and their resolution in mandibular contouring surgery. Aesthetic Plast Surg 1995; 19: 93–102. 1995/01/01. DOI: 10.1007/BF00209317. [DOI] [PubMed] [Google Scholar]
- 10.Andrews BT, Thurston TE, Tanna N, et al. A multicenter experience with image-guided surgical navigation: broadening clinical indications in complex craniomaxillofacial surgery. J Craniofac Surg 2015; 26: 1136–1139. 2015/06/17. DOI: 10.1097/scs.0000000000001672. [DOI] [PubMed] [Google Scholar]
- 11.Zhang W, Wang C, Yu H, et al. Effect of fiducial configuration on target registration error in image-guided cranio-maxillofacial surgery. J Craniomaxillofac Surg 2011; 39: 407–411. 2010/11/12. DOI: 10.1016/j.jcms.2010.10.008. [DOI] [PubMed] [Google Scholar]
- 12.Li D, Xu H, Xu L, et al. The aesthetic proportion index of facial contour surgery. J Craniofac Surg 2015; 26: 586–589. 2015/02/24. 10.1097/scs.0000000000001475. [DOI] [PubMed] [Google Scholar]
- 13.Kim Y, Park B. Resection of the prominent mandible angle with intraoral and external approach. Aesthetic Plast Surg 2003; 27: 38–42. 2003/03/13. DOI: 10.1007/s00266-002-2078-7. [DOI] [PubMed] [Google Scholar]
- 14.Nagase T, Yoshimura K, Aiba E, et al. Angle-splitting ostectomy followed by face lift for elderly patients with prominent mandibular angles. Plast Reconstr Surg 2005; 115: 633–640. 2005/02/05. DOI: 10.1097/01.prs.0000150155.56974.79. [DOI] [PubMed] [Google Scholar]
- 15.Liu D, Huang J, Shan L, et al. Intraoral curved ostectomy for prominent mandibular angle by grinding, contiguous drilling, and chiseling. J Craniofac Surg 2011; 22: 2109–2113. 2011/11/10. DOI: 10.1097/SCS.0b013e318232a58a. [DOI] [PubMed] [Google Scholar]
- 16.Desban M, Gauchy C, Kemel ML, et al. Three-dimensional organization of the striosomal compartment and patchy distribution of striatonigral projections in the matrix of the cat caudate nucleus. Neuroscience 1989; 29: 551–566. 1989/01/01. DOI: 10.1097/00006534-199706000-00005. [DOI] [PubMed] [Google Scholar]
- 17.Shenaq DS, Matros E. Virtual planning and navigational technology in reconstructive surgery. J Surg Oncol 2018; 118: 845–852. 2018/10/08. DOI: 10.1002/jso.25255. [DOI] [PubMed] [Google Scholar]
- 18.Li L, Yang J, Chu Y, et al. A novel augmented reality navigation system for endoscopic sinus and skull base surgery: a feasibility study. PLoS One 2016; 11: e0146996. 2016/01/13. DOI: 10.1371/journal.pone.0146996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Okamoto T, Onda S, Yanaga K, et al. Clinical application of navigation surgery using augmented reality in the abdominal field. Surg Today 2015; 45: 397–406. 2014/06/06. DOI: 10.1007/s00595-014-0946-9. [DOI] [PubMed] [Google Scholar]
- 20.Bobek SL. Applications of navigation for orthognathic surgery. Oral Maxillofac Surg Clin North Am 2014; 26: 587–598. 2014/09/23. DOI: 10.1016/j.coms.2014.08.003. [DOI] [PubMed] [Google Scholar]
- 21.Horsley V, Clarke RH. The structure and functions of the cerebellum examined by a new method. Brain 1908; 31: 45–124. DOI: 10.1093/brain/awm115. [Google Scholar]
- 22.Feichtinger M, Pau M, Zemann W, et al. Intraoperative control of resection margins in advanced head and neck cancer using a 3D-navigation system based on PET/CT image fusion. J Craniomaxillofac Surg 2010; 38: 589–594. 2010/04/13. DOI: 10.1016/j.jcms.2010.02.004. [DOI] [PubMed] [Google Scholar]
- 23.Zinser MJ, Mischkowski RA, Dreiseidler T, et al. Computer-assisted orthognathic surgery: waferless maxillary positioning, versatility, and accuracy of an image-guided visualisation display. Br J Oral Maxillofac Surg 2013; 51: 827–833. 2013/09/21. DOI: 10.1016/j.bjoms.2013.06.014. [DOI] [PubMed] [Google Scholar]
- 24.Ma B, Kunz M, Gammon B, et al. A laboratory comparison of computer navigation and individualized guides for distal radius osteotomy. Int J Comput Assist Radiol Surg 2014; 9: 713–724. 2013/12/11. DOI: 10.1007/s11548-013-0966-8. [DOI] [PubMed] [Google Scholar]
- 25.Cheng T, Zhao S, Peng X, et al. Does computer-assisted surgery improve postoperative leg alignment and implant positioning following total knee arthroplasty? A meta-analysis of randomized controlled trials. Knee Surg Sports Traumatol Arthrosc 2012; 26: 1307–1322. 2011/07/07. DOI: 10.1007/s00167-011-1588-8. [DOI] [PubMed] [Google Scholar]
- 26.Chen X, Lin Y, Wang C, et al. A surgical navigation system for oral and maxillofacial surgery and its application in the treatment of old zygomatic fractures. Int J Med Robot 2011; 7: 42–50. 2011/02/23. DOI: 10.1002/rcs.367. [DOI] [PubMed] [Google Scholar]
- 27.Nijmeh AD, Goodger NM, Hawkes D, et al. Image-guided navigation in oral and maxillofacial surgery. Br J Oral Maxillofac Surg 2005; 43: 294–302. 2005/07/05. DOI: 10.1016/j.bjoms.2004.11.018. [DOI] [PubMed] [Google Scholar]
- 28.Yu H, Shen SG, Wang X, et al. The indication and application of computer-assisted navigation in oral and maxillofacial surgery-Shanghai's experience based on 104 cases. J Craniomaxillofac Surg 2013; 41: 770–774. DOI: 10.1016/j.jcms.2013.01.016. [DOI] [PubMed] [Google Scholar]
- 29.Casap N, Wexler A, Eliashar R. Computerized navigation for surgery of the lower jaw: comparison of 2 navigation systems. J Oral Maxillofac Surg 2008; 66: 1467–1475. 2008/06/24. DOI: 10.1016/j.joms.2006.06.272. [DOI] [PubMed] [Google Scholar]