Abstract
Background
Despite the knowledge that the vast majority of skin aging is caused by the sun, and the widespread prevalence of sunscreen usage, solar skin damage continues to occur due to the combined biological impact of ultraviolet, visible light and near-infrared radiation. Sunscreens have only proven effective at filtering ultraviolet light. They do not attenuate visible light or near-infrared.
Objective
To evaluate the effectiveness of a novel, solar-specific skincare approach embracing both comprehensive daily solar protection from ultraviolet through to near-infrared radiation and nightly solar repair.
Participants
Eighteen Japanese patients were enrolled in this study. Topical skincare products (The Essential Six, RATIONALE, Victoria, Australia), comprising solar protection preparations to be used in the morning and topical solar repair at night, were applied to the patients’ skin for 12 months. Patients refrained from using any other skincare formulations and did not undergo any form of medical esthetic treatment during the study.
Measurements
Digital facial skin and three-dimensional volumetric assessment were performed pre- and post-treatment, and patient assessments were recorded after 6 and 12 months post-treatment.
Results
Improvements in skin texture and luminosity as recorded via digital photography, significant amelioration of skin redness and pigmentation in facial surface analysis, and volumetric reduction in three-dimensional volumetric assessment were observed compared to the pre-treatment for all patients. Eighty-nine percent, and 94% of patients self-reported their approval of treatment outcomes after 6 and 12 months post-treatment, respectively. Minor complications, characterized by slight pain and itching were observed in 3 patients. These minor complications resolved spontaneously.
Conclusion
The results of this study indicate that the solar-specific skincare formulations focused on the daily comprehensive prevention of negative solar effects and nightly repair of photodamage provide a safe and highly effective pathway to skin preservation and rejuvenation.
Keywords: long-term objective assessment, rejuvenation, solar protection, solar repair, sunscreen, volumetric measurement
Introduction
Incident solar energy comprises less than 10% ultraviolet (UV), approximately 40% visible light (VL), and over 50% near-infrared (NIR) radiation. Despite widespread sunscreen use globally, motivated by the desire to prevent skin damage, skin cancer and photoaging continue to pose a health threat worldwide.1 Over 90% of solar radiation affecting the Earth consists of VL and NIR, and intensive or ongoing exposure to VL and NIR, when combined with UV, also contributes to skin cancer and photoaging.1
Regardless of age and skin type, clinical signs of skin aging such as loss of skin luminosity, redness, pigmentation and skin laxity are major common complaints among patients seeking rejuvenation and cosmetic procedures.
The introduction and ongoing development of medical esthetic procedures including facelifting, laser resurfacing and ablative procedures designed to repair actinic and intrinsic aging through skin tightening and wrinkle smoothing have not met with widespread acceptance, due to their potential risks and downtime.2–12
Regarding NIR, the author has previously reported that solar NIR has measurable aging effects on human skin. Biomarkers and clinical evidence of solar damage similar to that caused by UV can be observed where biological NIR protection is impaired.13,14 The sequelae of NIR exposure include muscle thinning, skin sagging and ptosis, chronic vasodilation and potentially photocarcinogenesis.13,14 It must be noted that the global sunscreen industry has not embraced effective formulation technologies designed to filter VL and NIR.
A significant limitation in studies designed to measure skin rejuvenation is the absence of an agreed standard for precisely capturing the levels of observed effects. Two-dimensional (2-D) imaging has been widely deployed, but may not represent an unquestionably accurate objective representation. In the author’s prior studies, this limitation was overcome by the addition of a superimposed three-dimensional (3-D) color schematic scan to increase data precision, as well as demonstrate results not visible in 2-D imagery.
Although rejuvenating effects attributed to various skincare products and medical devices have been reported extensively by previous researchers, long-term skin evaluation using digital facial surface analysis, and 3-D volumetric assessment following skincare products without any other products and treatments has not been reported.
The author examined the concept proposed by Australian skincare company RATIONALE that a comprehensive approach to daily skincare embracing daily solar protection and nightly repair of photodamage incorporating topical immune boosters, antioxidants, UV+VL+NIR solar filters, barrier repair lipids, hydroxy acids, and retinoids would enhance skin health through the prevention and rejuvenation of solar skin damage. The author evaluated the efficacy of The RATIONALE “Essential Six” formulations on achieving these objectives using objective digital facial surface analysis and 3-D volumetric assessment.
Materials and methods
Japanese patients
Eighteen Japanese patients (15 females and 3 males) aged 22–70 years (mean age, 41.5±14.2 years) with Fitzpatrick skin type III to V were enrolled in this study. All of the patients had visited the Clinica Tanaka Anti-Aging Center to seek restoration of skin health and luminosity. In this group, no patients were known to be suffering from any form of skin disease or undergone cosmetic treatments affecting the treatment zone within two years of this study. Patients were directed not to use any other skincare products or undergo any form of esthetic procedure during the study. Additionally, they were instructed to continue with their normal diet throughout the study. As this study involved a retrospective review of patients previously treated, the approval of an ethics committee was not required.
Patients who lost weight during the study period were excluded from the 3-D volumetric reporting as changes in this variable may affect volumetric measurements. All patients signed an informed consent document of participation following an explanation of the study design and execution, and agreed to publication of results and images.
Topical skincare approach
The Essential Six (RATIONALE, Victoria, Australia) was used in this study. The Essential Six represents a comprehensive topical dermatologic approach to skin environmental protection and repair, encompassing the entire solar spectrum (approximately 290 nm–3200 nm) and the effects of pollution and desiccation. The Essential Six consists of three solar protective formulations (Immunologist Serum, Antioxidant Serum, and Photodynamic Day Cream) to be used in the morning and three solar repair formulations (Proceramide Cleanser, Catalyst Serum, and DNA Night Cream) to be used at night.
Patients applied these products as directed to the facial skin for 12 months without any other specific skin care product or medical treatment.
Morning
Immunologist serum
B group vitamins and immune-enhancing Australian botanical extracts provide protection from solar-induced photoimmunosuppression.
Antioxidant serum
A comprehensive complex of skin-identical vitamin, mineral, enzymatic antioxidants help to prevent the formation of solar and pollution-related free radicals.
Photodynamic day cream SPF15
A combination of zinc oxide, provitamin D, melanin, and heat shock proteins provide complete protection through the entire solar spectrum, including UV, VL, and NIR radiation (Figure 1).
Figure 1.

Optical evaluation of sunscreens using transmission spectra. To evaluate sunscreens produced by internationally well-known companies, a double-beam spectrophotometer was used to optically measure the transmission spectra. Sunscreens were embedded in sapphire cuvette with a thickness of 0.1 mm. The spectrophotometer utilizes a unique, single monochromatic design covering a wavelength range of 240–2600 nm. The emitted light was detected by a photomultiplier tube. The red line indicates the sunscreen (RATIONALE Photodynamic Day Cream SPF15) used in the study while the black lines indicate sunscreens produced by internationally well-known companies. Although standard sunscreens (SPF50+, PA+++ or ++++) block UV, they cannot block VL and NIR sufficiently. The Photodynamic Day Cream used in the study alone demonstrates the capacity to minimize penetration of UV, VL, and NIR.
Night
Proceramide cleanser
Skin identical concentrations of barrier lipids including ceramides, triglycerides, and cholesterol clean the skin of carbon-based particulate matter and toxic chemicals while restoring stratum corneum barrier function.
Catalyst serum
This complex of endogenous and exogenous alpha and beta hydroxyl acids restores skin pH to desirable acidic levels to enhance nightly DNA repair functions.
DNA night cream
A novel complex of retinoids and DNA Repair Enzymes promotes initiates skin cellular DNA repair caused by solar and environmental damage.
Objective assessments
Digital facial topography analyses were conducted as objective computer measurements using VISIA Complexion Analysis (Canfield Scientific Inc., Fairfield, NJ). Eight objective parameter analytics were executed immediately following image capture with photography modes including UV, color, and cross-polarized light. Improvements in redness and pigmentation were evaluated by percentile which was calculated to include data variables of sex, age, and ethnicity.
3-D imaging was used as an objective assessment, acquired with a VECTRA Handy Camera and associated software (Canfield Scientific Inc., Fairfield, NJ). This system realistically captures changes in skin topographic data as well as 2-D color representations. The camera sequence of image capture was calibrated to less than 3 ms to accurately record facial topography even if the subject was not able to maintain perfect stillness. Differences in facial tissue volume pre- and post-treatment were demonstrated via 3-D schematics, with relative degrees of skin tightening being represented by yellow to red zones (red, −5 mm change). Areas of no change to the face illuminate as green zones. These volumetric changes were performed up to 12 months following treatment, with patients directed to maintain the same neutral facial expression for accuracy during all image capture sessions.
Subjective patient assessments
Subjective data were obtained from patients via questionnaires collected as 6- and 12-month intervals post-treatment. Patients also rated their satisfaction with the degree of improvement to the treatment areas. A 0–4 rating system was deployed, with 0 representing a worse outcome, 1= minimal satisfaction/lack of acceptable outcome, 2= a moderate improvement detected, 3= quite satisfied, and 4= very satisfied with the outcomes.
Statistical analysis
The Wilcoxon Signed Rank Test was engaged to determine the statistical significance of the median change in facial volume. The statistical significance cutoff point was set as P<0.01. A box plot graph was used to illustrate the median change and its variability.
Results
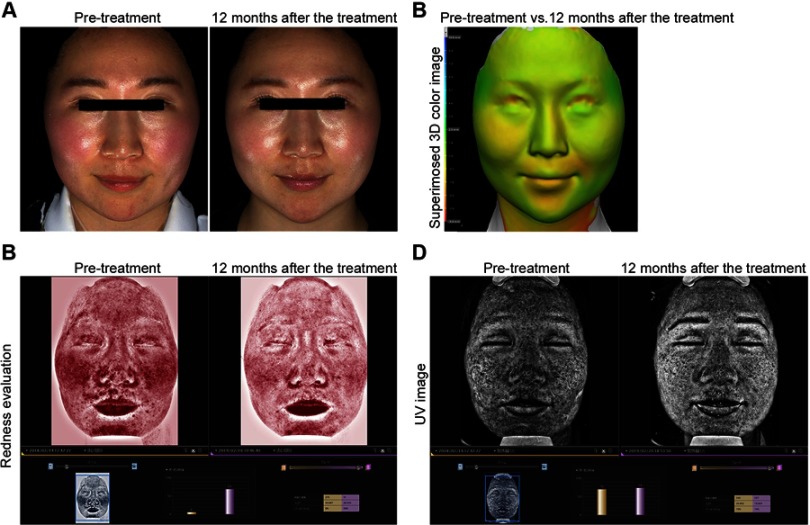
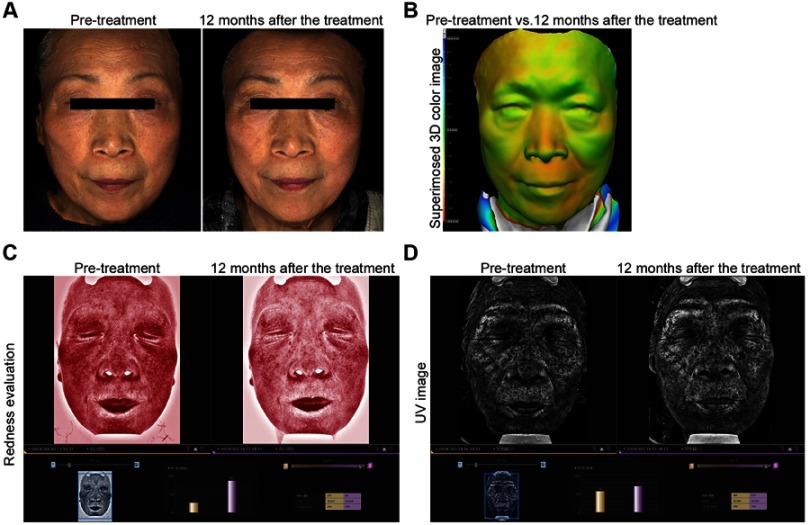
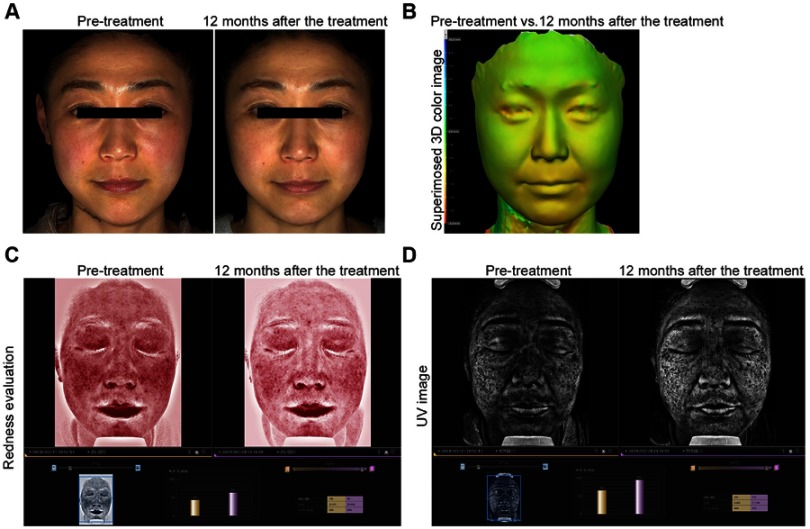
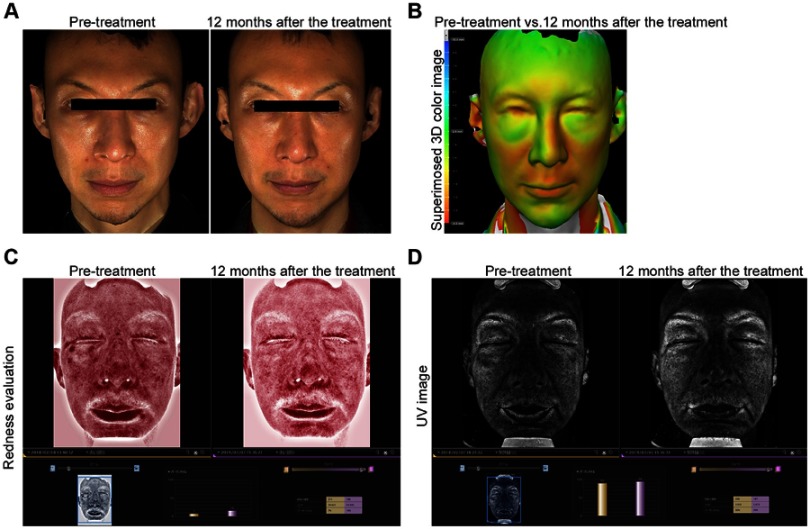
Marked improvement in skin texture and luminosity was observed in 2-D color digital photographs compared to the pre-treatment for all patients (Figures 2A–5A).
Figure 2.
A 28-year-old Japanese female. Marked improvement of skin texture and luminosity was observed in 2-D color digital photographs compared to the pre-treatment (A). Volumetric reduction in 3-D volumetric assessment was observed compared to the pre-treatment (B). The varying degrees of tightening achieved are shown in colors yellow to red. Green areas indicate areas that remained unchanged. Tightening effects on the lower two-thirds of the face, as well as the lower cheeks and peri-oral areas that were induced by the treatment lasted for 12 months. Significant improvement of skin redness (C) and pigmentation (D) were observed in facial surface analysis compared to the pre-treatment.
Figure 5.
A 71-year-old Japanese female. Improvement of skin texture and luminosity was observed in 2-D color digital photographs compared to the pre-treatment (A). Marked volumetric reduction in 3-D volumetric assessment was observed compared to the pre-treatment (B). Significant improvement of skin redness (C) and pigmentation (D) were observed in facial surface analysis compared to the pre-treatment.
Volumetric reduction in 3-D volumetric assessment was observed compared to the pre-treatment for all patients (Figures 2B–5B). Skin-firming effects were induced at perioral, lower cheek, and lower two-thirds of the face. These results were sustained over 12 months without the edematous reactions observed in laser and RF therapies.
Significant improvement of skin redness (Figures 2C–5C) and pigmentation (Figures 2D–5D) was observed in facial surface analysis compared to the pre-treatment for all patients.
Figure 3.
A 43-year-old Japanese female. Improvement of skin texture and luminosity was observed in 2-D color digital photographs compared to the pre-treatment (A). Volumetric reduction in 3-D volumetric assessment was observed compared to the pre-treatment (B). Significant improvement of skin redness (C) and pigmentation (D) were observed in facial surface analysis compared to the pre-treatment.
Figure 4.
A 44-year-old Japanese male. Improvement of skin texture and luminosity was observed in 2-D color digital photographs compared to the pre-treatment (A). Marked volumetric reduction in 3-D volumetric assessment was observed compared to the pre-treatment (B). Significant improvement of skin redness (C) and pigmentation (D) were observed in facial surface analysis compared to the pre-treatment.
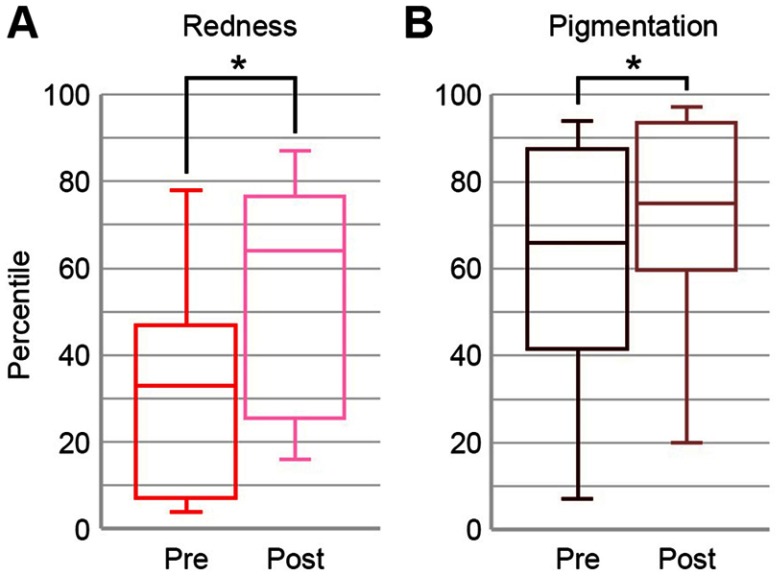
The mean pre-treatment percentiles of redness and pigmentation were 31.67±25.98 and 64.50±25.95, respectively. The mean post-treatment percentiles of redness and pigmentation were 54.67±27.08 and 76.50±22.77, respectively (Figure 6). Objective computer assessments in redness and pigmentation showed significant improvement after treatment (P<0.01) (Figure 6).
Figure 6.
Objective computer assessments in redness (A) and pigmentation (B) showed significant improvement compared with pre-treatment (P=0.0021 and 0.0022, respectively). The box illustrates the interquartile range extending from the 25th percentile to the 75th percentile with a line at the median (50th percentile). The bottom and top end of whiskers show the minimum and maximum data points, respectively. Significant differences compared with pre-treatment are indicated (*P<0.05).
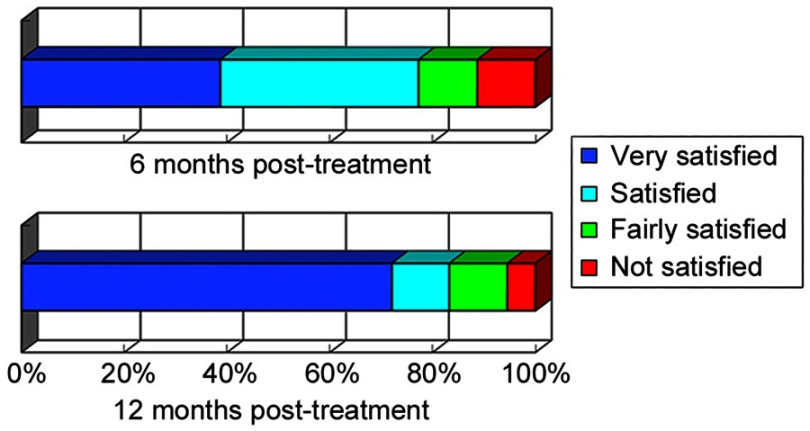
Eighty-nine percent and 94% of patients were satisfied with the treatment outcomes after 6 and 12 months post-treatment, respectively (Figure 7). The mean degrees of satisfaction after 6 and 12 months post-treatment based on a 5-point scale from 0 to 4 were 3.06±0.99 and 3.50±0.92, respectively.
Figure 7.
Subjective assessments were performed using questionnaire data collected 6 and 12 months post-treatment. Patients rated their degree of satisfaction with improvement of the treated area. Subjective assessments are shown as follows: very satisfied (blue), satisfied (light blue), fairly satisfied (green), and not satisfied (red).
Minor complications, characterized by slight pain and itching, were observed in 3 (17%) patients. These minor complications resolved within 2 weeks. Side effects including post-inflammatory hyperpigmentation and epidermal trauma were not observed.
Discussion
Improvement in skin texture and luminosity are most frequently requested by the patients seeking laser or light therapies. These treatments may provide the requested improvement if patients are treated continuously at clinics. Interestingly, this skincare approach used in the study provided all of these improvements as shown through 2D photos and satisfied most of the patients even though the treatments were performed by the patients themselves at home daily.
Skin redness and pigmentation is usually treated by lasers or other light therapies. However, these treatments are usually accompanied by inflammation and downtime. Post-treatment care including comprehensive solar protection is critical to minimize post-inflammatory hyperpigmentation and other complications following all forms of phototherapy.
As the biological effects of solar energy (UV, VL, and NIR) are significant, this skincare approach consisting of solar protection from UV, VL, and NIR and of nightly solar repair appeared to be effective in preventing and repairing photoaging. The results shown through objective digital facial surface analysis were impressive and most of the patients were extremely satisfied with the results.
Chronic NIR exposure can induce rosacea, a condition found most commonly in fair-skinned, Caucasian populations.15 NIR is now accepted as a key factor in the etiology and progression of this disorder.13
Another relevant condition is erythema ab igne, which can also be induced by exposure to fire and heat, all sources of NIR.16 Of great importance is the fact that histopathological alternations seen in erythema ab igne are very similar to those detected in sun-damaged skin.17 Age-related, deteriorative skin changes, such as pigmentary incontinence and telangiectasia, are directly related to ongoing sun exposure and tanning,15 while thermal keratotic lesions including keratinocyte dysplasia, hyperkeratosis, and elastosis of the dermis follow a similar pathway to that seen in actinically damaged skin.18
Vascular smooth muscle cell apoptosis and degeneration of myoglobin are non-thermally induced by NIR, resulting in long-lasting vasodilation.13,14 As abundant sources of hemoglobin and myoglobin, muscles are targets for NIR damage.19 Ongoing NIR exposure leads to superficial tissue damage and deeper ptosis by thinning facial muscles and their extensions into the dermis.14 This damage is more profound in fair skin with its lower concentrations of photoprotective melanin and a thinner dermis, compared to darker-skinned populations.14 The vulnerability of fair skin to solar damage and photoaging is universally acknowledged,20,21 with age-related changes accelerated in Caucasians populations.22 It must also be noted the heat-induced erythema ab igne can give rise to carcinomas.23,24,25 Clearly, NIR exposure, when layered with UV irradiation, is capable of inducing photoaging and possibly photocarcinogenesis.26
Nonsurgical volumetric reduction and skin tightening are usually achieved by NIR, RF, or other thermal approaches. The author has previously reported that these treatments could provide impressive results shown through 3-D volumetric assessment in prior studies. However, these treatments are always accompanied by thermal damage to the dermis, and edematous reactions that can last up to 2 months after treatment.
Interestingly, the long-term use of the skincare regime examined in this study consisting of daily solar protection from UV to NIR and nightly solar repair provided the volumetric reduction and skin tightening effects seen in the medical procedures outlined above without thermal stimulation of collagen production, edematous reactions, or thermal damage to the dermis. Significant improvement of various skin conditions without thermal damage and post-procedural complications enhanced patient satisfaction rates.
Minor complications, characterized by slight pain, and itching were observed in 3 patients. These resolved spontaneously. They might occur due to hydroxy acids and retinoids as part of the formulation, and further investigations might be needed to minimize the complications.
Furthermore, the skincare regime is pain-free, convenient, and cost-effective, with results that parallel invasive medical treatments. Although significant improvements in skin conditions were observed following the skincare approach, further studies are needed to determine if additional treatment or topical actives may be even more effective in skin rejuvenation and prevention of photoaging.
It is acknowledged that this a preliminary study based on a relatively small number of patients. Further studies are needed in larger numbers of patients to evaluate variations in treatment parameters. Moreover, lifestyle choices, including diet, alcohol and salt intake, exercise and sleep patterns, may influence the outcomes reported in this study.
Limitations
The absence of a control group and a comparison study may limit the significance of these findings.
Conclusion
Solar damage and skin aging have various physical and mental health implications, increasing the imperative for home-based, non-invasive treatments. The advantages of this skincare approach revolve around comprehensive solar protection and repair with its safety and high efficacy as demonstrated through objective digital facial surface analysis and 3-D volumetric assessments. Objectively, outcomes were demonstrable and impressive, with patients reporting a high level of satisfaction with almost no downtime, discomfort, and negligible side effects.
Unlike conventional procedures including medical treatments and conventional sunscreen use, this skincare approach represents a safe and highly efficacious treatment for solar damage and skin aging without tissue damage, and is recommended as a regime for skin rejuvenation and prevention of photoaging. These advantages and clinical benefits of this approach would suggest it would be easily adopted by socially active people and develop widespread acceptance by patients regardless of age, sex, or skin type.
Acknowledgment
I thank Richard Parker and Joshua Gosling from RATIONALE for formulation information relating to the skincare regime used in the study and helpful comments. This study was conducted without financial support from a third party.
Disclosure
The author discloses that no financial support was received for this study and therefore declares no conflicts of interest.
References
- 1.Tanaka Y. Photoprotection update. Non-Surgical Symposium; June 15; 2018; Gold Coast, Australia. [Google Scholar]
- 2.Tanaka Y, Matsuo K, Yuzuriha S, Shinohara H. Differential long-term stimulation of type I versus type III collagen after infrared irradiation. Dermatol Surg. 2009;35:1099–1104. doi: 10.1111/j.1524-4725.2009.01194.x [DOI] [PubMed] [Google Scholar]
- 3.Tanaka Y, Matsuo K, Yuzuriha S. Long-term evaluation of collagen and elastin following infrared (1000 to 1800 nm) irradiation. J Drugs Dermatol. 2009;8:708–712. [PubMed] [Google Scholar]
- 4.Tanaka Y, Matsuo K, Yuzuriha S. Long-term histological comparison between near-infrared irradiated skin and scar tissues. Clin Cosmet Investig Dermatol. 2010;3:143–149. doi: 10.2147/CCID.S15729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tanaka Y, Matsuo K, Yuzuriha S. Objective assessment of skin rejuvenation using near-infrared 1064-nm neodymium: YAG laser in Asians. Clin Cosmet Investig Dermatol. 2011;4:123–130. doi: 10.2147/CCID.S22841 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tanaka Y, Matsuo K, Yuzuriha S. Long-lasting relaxation of corrugator supercilii muscle contraction induced by near infrared irradiation. ePlasty. 2011;11:e6. [PMC free article] [PubMed] [Google Scholar]
- 7.Tanaka Y, Tsunemi Y, Kawashima M, Nishida H, Tatewaki N. Objective assessment of skin tightening using water-filtered near-infrared (1000-1800 nm) device with a contact cooling and freezer stored gel in Asians. Clin Cosmet Investig Dermatol. 2013;6:167–176. doi: 10.2147/CCID.S47299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tanaka Y. Long-term three-dimensional volumetric assessment of skin tightening using a sharply tapered non-insulated microneedle radiofrequency applicator with novel fractionated pulse mode in Asians. Lasers Surg Med. 2015;47(8):626–633. doi: 10.1002/lsm.22401 [DOI] [PubMed] [Google Scholar]
- 9.Tanaka Y, Nakayama J. Up-regulated epidermal growth factor receptor expression following near-infrared irradiation simulating solar radiation in a 3-dimensional reconstructed human corneal epithelial tissue culture model. Clin Interv Aging. 2016;11:1027–1033. doi: 10.2147/CIA.S111530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Calderhead G, Tanaka Y. Photobiological basics and clinical indications of phototherapy for skin rejuvenation. Photomedicine. 2017; 215–252. Available from: https://www.intechopen.com/books/photomedicine-advances-in-clinical-practice/photobiological-basics-and-clinical-indications-of-phototherapy-for-skin-rejuvenation. Accessed July 25, 2019. [Google Scholar]
- 11.Tanaka Y. Treatment of skin laxity using multisource, phase-controlled radiofrequency. Dermatol Surg Proc. 2018;175–192. ISBN 978-953-51-3852-5, Print ISBN 978-953-51-3851-8 Available from: https://www.intechopen.com/books/dermatologic-surgery-and-procedures/treatment-of-skin-laxity-using-multisource-phase-controlled-radiofrequency. Accessed July 25, 2019. [DOI] [PubMed] [Google Scholar]
- 12.Tanaka Y, Nakayama J. Up-regulated expression of La ribonucleoprotein domain family member 6 and collagen type I gene following water-filtered broad-spectrum near-infrared irradiation in a 3-dimensional human epidermal tissue culture model as revealed by microarray analysis. Australas J Dermatol. 2018;59(2):e87–e92. doi: 10.1111/ajd.2018.59.issue-2 [DOI] [PubMed] [Google Scholar]
- 13.Tanaka Y. The impact of near-infrared radiation in dermatology. Review. World J Dermatol. 2012;1:30–37. doi: 10.5314/wjd.v1.i3.30 [DOI] [Google Scholar]
- 14.Tanaka Y, Gale L. Beneficial applications and deleterious effects of near-infrared from biological and medical perspectives. Opt Photon J. 2013;3:31–39. doi: 10.4236/opj.2013.34A006 [DOI] [Google Scholar]
- 15.Berg M. Epidemiological studies of influence of sunlight on the skin. Photodermatol. 1989;6:80–84. [PubMed] [Google Scholar]
- 16.Findlayson GR, Sams WM Jr, Smith JG. Erythema ab igne. A histopathological study. J Invest Dermatol. 1966;46:104–107. doi: 10.1038/jid.1966.15 [DOI] [PubMed] [Google Scholar]
- 17.Page EH, Shear NH. Temperature-dependent skin disorders. J Am Acad Dermatol. 1988;18:1003–1019. doi: 10.1016/s0190-9622(88)70098-5 [DOI] [PubMed] [Google Scholar]
- 18.Arrington JH III, Lockman DS. Thermal keratoses and squamous cell carcinoma in situ associated with erythema ab igne. Arch Dermatol. 1979;115:1226–1228. [PubMed] [Google Scholar]
- 19.Srinivasan S, Pogue BW, Jiang S, et al. Interpreting hemoglobin and water concentration, oxygen saturation, and scattering measured in vivo by near-infrared breast tomography. Proc Natl Acad Sci USA. 2003;100:12349–12354. doi: 10.1073/pnas.2032822100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Anderson RR, Parrish JA. The optics of human skin. J Invest Dermatol. 1981;77:13–19. doi: 10.1111/1523-1747.ep12479191 [DOI] [PubMed] [Google Scholar]
- 21.Rawlings AV. Ethnic skin types: are there differences in skin structure and function? Review article. Int J Cosmet Sci. 2006;28:79–93. doi: 10.1111/j.1467-2494.2006.00302.x [DOI] [PubMed] [Google Scholar]
- 22.Odunze M, Rosenberg DS, Few JW. Periorbital aging and ethnic considerations: a focus on leteral canthal complex. Plast Reconstr Surg. 2008;121:1002–1008. doi: 10.1097/01.prs.0000299381.40232.79 [DOI] [PubMed] [Google Scholar]
- 23.Kligman LH. Intensification of ultraviolet-induced dermal damage by infrared radiation. Arch Dermatol Res. 1982;272:229–238. [DOI] [PubMed] [Google Scholar]
- 24.Jones CS, Tyring SK, Lee PC, Fine JD. Development of neuroendocrine (Merkel cell) carcinoma mixed with squamous-cell carcinoma in erythema ab igne. Arch Dermatol. 1988;124:110–113. [PubMed] [Google Scholar]
- 25.Hewitt JB, Sherif A, Kerr KM, Stankler L. Merkel cell and squamous-cell carcinomas arising in erythema ab igne. Br J Dermatol. 1993;128:591–592. doi: 10.1111/j.1365-2133.1993.tb00247.x [DOI] [PubMed] [Google Scholar]
- 26.Schieke SM, Schroeder P, Krutmann J. Review article. Cutaneous effects of infrared radiation: from clinical observations to molecular response mechanisms. Photodermatol Photoimmunol Photomed. 2003;19:228–234. [DOI] [PubMed] [Google Scholar]