Abstract
Objective
To compare exophthalmometry measured by Hertel exophthalmometer versus computed tomography (CT) scan.
Methods
For this study, 133 patients with thyroid-associated orbitopathy (TAO) were analyzed retrospectively. Two experienced clinical observers independently measured proptosis using a Hertel exophthalmometer. The CT approaches used to measure proptosis included two previous methods and one new method. Method 1 used both lateral orbital rims–corneal surface in the axial plane, method 2 used lateral to medial orbital rims–corneal surface in the axial plane, and method 3 used superior to inferior orbital rims–corneal surface in the sagittal plane (new method). Patients were separated into two groups based on 2-mm differences in proptosis between eyes. Correlation analysis was performed to find the association between Hertel and CT values.
Results
The Pearson’s coefficient (r) was 0.727 for Hertel exophthalmometry and CT method 1, 0.712 for Hertel and CT method 2, and 0.623 for Hertel and CT method 3. For patients with eye proptosis differences larger than 2 mm between eyes, Pearson’s coefficient (r) was 0.495 for Hertel exophthalmometry and CT method 1, 0.634 for Hertel and CT method 2, and 0.635 for Hertel and CT method 3.
Conclusion
The three CT methods mentioned above had statistically significant relationships with Hertel exophthalmometry. Methods 2 and 3, which measured both eyes through different cut sections, had a significant relationship with Hertel values with eye proptosis differences larger than 2 mm. Thus, the new additive method may be effective for measuring proptosis in patients with differences greater than 2 mm between eyes.
Keywords: orbital disease, exophthalmos, thyroid-associated orbitopathy
Introduction
Thyroid-associated orbitopathy (TAO) is an inflammatory condition of the orbital tissues.1,2 After the acute edematous stage, fibrosis and fatty infiltration eventually occur, accompanied by restriction of extra-ocular muscles and proptosis.3,4
Proptosis is a measurement of the antero-posterior position of the globe in the orbit relative to the orbital rim.5,6 Proptosis is an important sign in TAO.2,7,8 Exophthalmometry is valuable in diagnosing and treating TAO.5,9 A Hertel exophthalmometer is often used clinically to measure proptosis.5,9,10 However, previous studies have found poor reproducibility (interobserver variation) and repeatability (intraobserver variation) with Hertel exophthalmometers.9–12 Interobserver and intraobserver variations reduced the reliability of the Hertel instrument.12–15 Moreover, it is difficult to measure proptosis in patients with severe upper eyelid swelling, ptosis, hyper-deviated eyes and poor cooperation.
The radiologic measurement of proptosis in patients with TAO has been conducted with computed tomography (CT).16 This method provides an objective assessment of proptosis measurements. CT scans are widely available and have high repeatability and reproducibility. This allows accurate measurement of proptosis and early detection of TAO.16–19 Some investigators have used CT to replace Hertel exophthalmometer. Nkenke et al reported similar readings for Hertel exophthalmometer and CT scans.18
Previous reports have studied proptosis measurements made with axial CT views.18,19 One method used the distance from both lateral rims to the corneal surface while the other used the distance from the lateral to medial rims to the corneal surface in the axial plane. These two methods correlated approximately with Hertel exophthalmometry values.18,19 However, these two methods use only one plane, the axial view. If both eyes are not located on the axial plane due to a patient’s head tilt or vertical eye deviation, significant errors may occur. Proptosis analysis measured by a sagittal view may reduce the error caused by a patient’s head position.
This study devised a new method using sagittal CT views. Three different CT techniques and Hertel exophthalmometry were compared for proptosis estimation.
Materials and methods
This study was performed according to the Declaration of Helsinki on Biomedical Research Involving Human Subjects. The Institutional Review Board of Chung-Ang University approved the clinical study, and the requirement for informed consent was waived.
Baseline characteristics and mean value of exophthalmometry
Data from 133 patients examined between January 2014 and December 2017 were obtained from the Chung-Ang university hospital database and were reviewed retrospectively. Patients with any history of orbital trauma or surgery were excluded.
Two experienced clinical observers (ophthalmologists) independently measured proptosis using a Hertel exophthalmometer in their first hospital visit. We used the same exact Hertel exophthalmometer in all measurements. The measurements were taken each 3 times of two observers and calculated the mean value with the patient’s head in the primary position and the examiner’s eyes at the same level as the patient’s eyes in a well-lit room. The reading was taken as the distance between the point on the temporal orbital rim, the deepest palpable point of the angle, and the apex of the cornea. Right eye and left eye readings were taken sequentially without removing the instrument from the orbital rims. Exophthalmometry was conducted using a one-mirror Hertel exophthalmometer (Hertel Exophthalmometer, Oculus, Germany), and measurements were recorded to the nearest 0.5 mm.
CT scan analysis
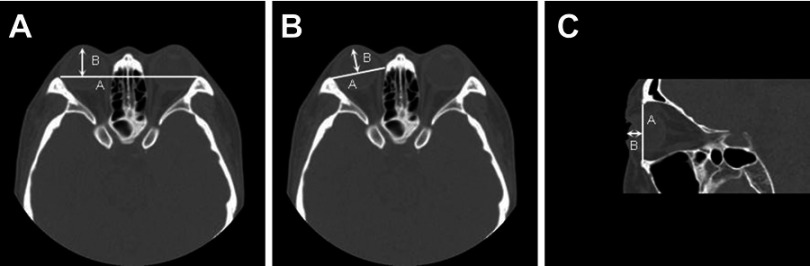
We scanned orbital CT for the clinical purpose for TAO patients. Orbital CT scans were obtained using contiguous axial slices, with the patient’s head positioned parallel to the Frankfurt plane. Patients were asked to look at a fixed point while CT was taken. First of all, we used 2.5 mm cuts orbital CT for low radiation exposure. CT scans were performed using 2.5 mm sections through the orbit on a CT machine (Light speed pro 16, GE Healthcare, Milwaukee, WI, USA). The three CT measurement methods were as follows (Figure 1):
Method 1: Proptosis measurements were made on the CT scan by drawing a horizontal line between the lateral orbital rims on the axial plane that bisects the lens and then drawing a perpendicular line forward to the posterior surface of the cornea. The posterior surface of the cornea was chosen because it can be difficult to define the anterior surface of the cornea on CT images (Figure 1A).
Method 2: Proptosis measurements were made on the CT scan by drawing a line between the lateral orbital rims and the medial orbital rim on the axial plane that bisects the lens and then by drawing a perpendicular line forward to the posterior surface of the cornea (Figure 1B).
Method 3: A new CT method for measuring proptosis involved drawing a line between the superior orbital rims and the inferior orbital rim on the sagittal plane that bisects the lens and then drawing a perpendicular line forward to the posterior surface of the cornea (Figure 1C).
Figure 1.
Three CT techniques for proptosis estimation. (A) Method 1: A line is drawn between the lateral orbital rims on the section that bisects the lens. B line is drawn between A line and the posterior surface of the cornea. (B) Method 2: A line is drawn between the lateral and medial orbital rims on the same axial plane. B line is drawn between A line and the posterior surface of the cornea. (C) Method 3: A line is drawn between the superior and inferior orbital rims on the sagittal plane. B line is drawn between A line and the posterior surface of the cornea.
Patients were separated into two groups to compare associations between Hertel and different CT methods for measuring proptosis differences between eyes. A proptosis difference larger than 2 mm was the classification criteria.
Statistical analysis
Mean values were given with standard deviation. Correlation analysis was performed to find associations between Hertel exophthalmometry and CT values. Patients were separated into two groups. One group included patients with proptosis differences larger than 2 mm by Hertel exophthalmometry, while the other group had differences smaller than 2 mm. Correlation analysis was used to investigate associations between Hertel and CT estimates in the 2 groups. P-values equal to or less than 0.05 were considered significant. All calculations were made using SPSS Version 21 for Windows (SPSS Inc., Chicago, USA).
Results
Among 133 patients, 93 were women and 40 were men. The mean age was 36.98±13.46 years (13 to 79 years). Hertel exophthalmometry and CT findings of the three techniques are summarized in Table 1.
Table 1.
Baseline characteristics and mean hertel exophthalmometry
| Characteristics | Value |
|---|---|
| Number of patients (N) | 133 |
| Sex, N (%) | |
| Male | 40 (30.08) |
| Female | 93 (69.92) |
| Age (years) | |
| <30 years (%) | 42 (31.58) |
| 30≤×<40 years (%) | 40 (30.08) |
| 40≤×<50 years (%) | 28 (21.05) |
| 50≤×<60 years (%) | 13 (9.77) |
| 60≤ years (%) | 10 (7.52) |
| Mean difference in eye proptosis (mm) | 1.32±1.25 |
| Mean difference in eye proptosis ≤2 mm (%) | 110 (82.7) |
| Mean difference in eye proptosis >2 mm (%) | 23 (17.3) |
Mean exophthalmometry was 17.17±3.02 mm by Hertel, 20.14±2.94 mm by CT method 1, 15.66±2.69 mm by CT method 2, and 11.13±2.57 mm by CT method 3 in the right eye. Mean exophthalmometry was 17.33±2.90 mm by Hertel instrument, 20.31±3.01 mm by CT method 1, 15.40±2.78 mm by CT method 2, and 11.29±2.55 mm by CT method 3 in the left eye. The mean difference in eye proptosis was 1.32±1.25 mm. The difference was smaller than 2 mm in 110 patients (82.71%) and larger than 2 mm in 23 patients (17.29%) (Table 2).
Table 2.
Exophthalmometric values of hertel exophthalmometry and CT techniques
| Right eye (mm) | Left eye (mm) | Mean difference in eye proptosis (mm) | |
|---|---|---|---|
| Hertel | 17.17±3.02 | 17.33±2.90 | 1.32±1.25 |
| CT method 1 | 20.14±2.94 | 20.31±3.01 | 1.15±1.00 |
| CT method 2 | 15.66±2.69 | 15.40±2.78 | 1.15±1.03 |
| CT method 3 | 11.13±2.57 | 11.29±2.55 | 1.22±1.01 |
Notes: CT method 1, both lateral rims to corneal surface; CT method 2, lateral to medial rims to corneal surface; CT method 3, superior to inferior rims to corneal surface.
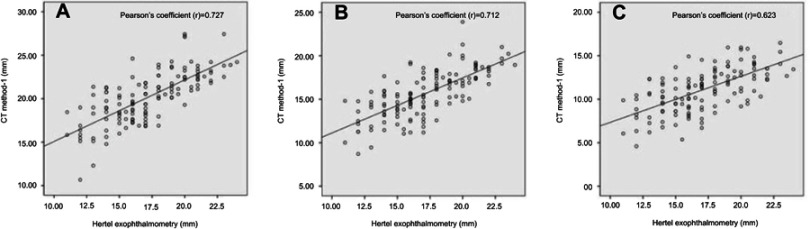
Pearson’s coefficient (r) was 0.727 for Hertel exophthalmometry and CT method 1 (Figure 2A), 0.712 for Hertel and CT method 2 (Figure 2B), and 0.623 for Hertel and CT method 3 (Figure 2C). The correlation analysis results are summarized in Figure 2.
Figure 2.
Association between Hertel and CT techniques by Pearson’s correlation analysis. The correlation between Hertel and CT method 1 is shown in (A), CT method 2 in (B), and CT method 3 in (C). Pearson’s (r) was 0.727 (A), 0.712 (B), and 0.623 (C).
The mean difference in eye proptosis measured by Hertel was 0.91±0.85 mm in the first group (proptosis difference ≤2 mm). The mean difference in eye proptosis of the first group was 1.01±0.81 mm with CT method 1 and 0.92±0.75 mm with CT method 2. The mean difference in eye proptosis in the first group measured by CT method 3 was 1.01±0.80 mm (Table 3).
Table 3.
Mean eye proptosis differences of Hertel and CT techniques (mm)
| Methods | Group 1 | Group 2 |
|---|---|---|
| Hertel exophthalmometry | 0.91±0.85 | 3.28±0.96 |
| CT method 1 | 1.01±0.81 | 1.79±1.49 |
| CT method 2 | 0.92±0.75 | 2.25±1.46 |
| CT method 3 | 1.01±0.80 | 2.24±1.30 |
Notes: CT method 1, both lateral rims to corneal surface; CT method 2, lateral to medial rims to corneal surface; CT method 3, superior to inferior rims to corneal surface.
For analysis of the first group (proptosis difference ≤2 mm), Pearson’s coefficient (r) was 0.624 for Hertel exophthalmometry and CT method 1, 0.588 for Hertel and CT method 2, and 0.598 for Hertel and CT method 3. Correlation analysis results are summarized in Table 4.
Table 4.
Correlation analysis between Hertel and CT techniques (proptosis difference ≤2.0 mm, N=110)
| Pearson’s Coefficient (r) | r2 | P-value | |
|---|---|---|---|
| Hertel - CT method 1 | 0.624 | 0.389 | <0.001* |
| Hertel - CT method 2 | 0.588 | 0.346 | <0.001* |
| Hertel - CT method 3 | 0.598 | 0.357 | <0.001* |
Notes: CT method 1, both lateral rims to corneal surface; CT method 2, lateral to medial rims to corneal surface; CT method 3, superior to inferior rims to corneal surface. *P<0.05 by correlation analysis.
The mean difference in eye proptosis of the second group measured by Hertel was 3.28±0.96 mm (proptosis difference ≥2 mm). The mean difference in eye proptosis of the second group was 1.79±1.49 mm with CT method 1, 2.25±1.46 mm with CT method 2, and 2.24±1.30 mm with CT method 3 (Table 3).
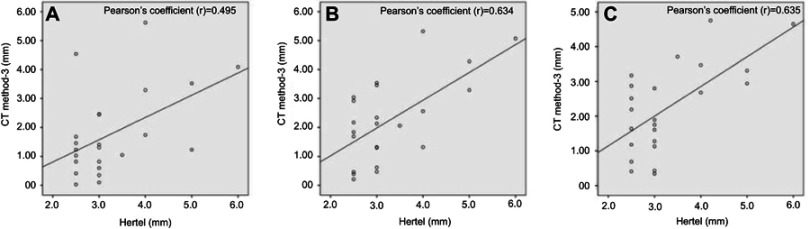
Regarding the second group (proptosis difference >2 mm), Pearson’s coefficient (r) was 0.495 for Hertel exophthalmometry and CT method 1 (Figure 3A), 0.634 for Hertel and CT method 2 (Figure 3B), and 0.635 for Hertel and CT method 3 (Figure 3C).
Figure 3.
Association between Hertel and CT techniques (proptosis difference >2 mm) by Pearson’s correlation analysis. The correlation between Hertel and CT method 1 was (A), CT method 2 was (B), and CT method 3 was (C) (proptosis difference >2 mm). Pearson’s (r) was 0.495 (A), 0.634 (B), and 0.635 (C).
Discussion
The absolute values for Hertel and CT were not the same. Proptosis readings with CT scans tended to be lower than those with Hertel exophthalmometry readings. Corneal thickness was approximately 0.5 mm, and CT scans used 2.5 mm sections through the orbit. The lower values found with CT scans are attributed to this difference between Hertel and CT. Proptosis readings were the shortest with CT method 3. A line between the superior and inferior orbital rims on the sagittal plane was anteriorly positioned compared to the line between the lateral orbital rims in the axial plane used by CT method 1 and the line between the lateral and medial orbital rims in the same axial plane used by CT method 2.
The results show a strong correlation between proptosis measurements determined by Hertel exophthalmometry and CT techniques. Pearson’s coefficient was the largest for Hertel and CT method 1 (r =0.727), with statistically significant correlation (P<0.001). The concepts of CT method 1 and Hertel exophthalmometry were the same, and both used the distance of a line from both lateral orbital rims to the corneal apex. There were statistically significant correlations between Hertel and CT methods 2 and 3 (r =0.712, 0.623, respectively; P<0.001) (Figure 2). A Hertel exophthalmometer was difficult to use for patients with orbital bone disorders, severe lid swelling, retraction, or strabismus. The CT techniques can serve as substitutes for proptosis measurements in patients with orbital pathology, lid swelling, retraction, hyper or hypotropia, and poor cooperation.
Correlation analysis indicated that CT method 1 had the most significant relationship with Hertel exophthalmometry. This is consistent with what was identified as the greatest Pearson’s coefficient (r =0.727). CT method 1 used the distance from the corneal apex to a line from both lateral orbital rims, similar to the basic concept of Hertel exophthalmometry. This is similar to the results reported by Segni et al from their work measuring proptosis with Hertel exophthalmometry and CT scans, where they obtained correlation coefficients of 0.93.20
CT method 2 also correlated with Hertel values (r =0.712). In CT method 2, measurement errors may frequently occur by drawing a line between the lateral and medial orbital rims in only one axial plane. The standard location of both medial orbital rims was not distinct, which may have lowered accuracy and repeatability. Additionally, a patient’s globe was located 23.5 degrees medially at the midline level, and the vertical line in CT method 2 did not accord with gaze direction. CT method 3 was statistically correlated with Hertel value, but with a weaker relationship than between Hertel and CT methods 1 or 2 (r =0.623).
CT methods 2 and 3 showed a higher correlation with the Hertel measurements compared to CT method 1 in the patients with a proptosis difference of more than 2 mm between the two eyes. CT method 3 used a standard line between the superior and inferior orbital rims on two sagittal planes whereas CT methods 1, which had a lower correlation (r =0.495), used only one axial plane (Figure 3). Results of CT methods 1 were influenced by patient head tilt because these methods only used one axial plane. This may have resulted in lower Pearson’s coefficients. Two different sagittal cut sections were used in CT method 3. Exophthalmometry was measured through two different cut sections of the right and left eyes. The two sagittal sections used by CT method 3 likely reduced the gap between Hertel exophthalmometry and CT in the second group of patients (proptosis difference >2 mm).
CT method 2 had a similar correlation with method 3, but method 2 had less consistency with Hertel exophthalmometry due to gaze directions that differed by 23.5 degrees and ambiguous principle points of medial orbital rims in the second group patients (proptosis difference >2 mm).
CT method 3 had a higher correlation with Hertel for proptosis measurement because each sagittal plane accurately represented eye exophthalmometry. We recommend method 2 and the new CT method 3 as a useful method in measuring the proptosis in patients with proptosis differences greater than 2 mm. Method 3 is similar to the proptosis measurement using a Naugle exophthalmometer in the clinic. The previous study reported that Naugle instrument is comparable in accuracy to the Hertel instrument for measuring ocular position.21 We also suggest CT method 3 for patients with horizontal and vertical strabismus.
This study is limited as follows. A 1 mm sectioned CT scan was not used. We used CT plane that bisects the lens, so proptosis value in 2.5 mm cuts CT scan showed no statistically significant difference in 1 mm cuts CT scan. Observer measurement errors are also possible. In patients with large differences in exophthalmos, Hertel exophthalmometry was incorrect.
Hertel exophthalmometry was the most reliable method for proptosis measurements, but previous studies indicated high risks of inter- and intra-observer differences.9 These errors influenced adverse effects in surgical outcomes of bony and fat orbital decompressions with TAO. For accurate proptosis measurements, objective CT methods are alternative options. The three CT methods mentioned above had statistically significant relationships with Hertel exophthalmometry. The method that used both lateral orbital rims on the axial plane had a higher correlation with Hertel values in patients with proptosis differences less than 2 mm. The method that used the lateral and medial rims on the axial plane and the method that used superior and inferior orbital rims on the sagittal plane had a significant relationship with Hertel values in patients with proptosis differences greater than 2 mm. In patients with TAO, depending on the degree of proptosis differences of the patient, the proper use of the Hertel exophthalmometry and the three CT methods can be effective methods for proptosis measurements.
Acknowledgments
The authors received non-governmental financial support for this study, and they have no proprietary or commercial interest in any of the methods or materials described in this article.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Bartalena L, Baldeschi L, Dickinson A, et al. Consensus statement of the European Group on Graves’ Orbitopathy (EUGOGO) on management of GO. Eur J Endocrinol. 2008;158(3):273–285. doi: 10.1530/EJE-07-0666 [DOI] [PubMed] [Google Scholar]
- 2.Bartalena L, Pinchera A, Marcocci C. Management of Graves’ ophthalmopathy: reality and perspectives. Endocr Rev. 2000;21(2):168–199. doi: 10.1210/edrv.21.2.0393 [DOI] [PubMed] [Google Scholar]
- 3.Alsuhaibani AH, Carter KD, Policeni B, Nerad JA. Effect of orbital bony decompression for Graves’ orbitopathy on the volume of extraocular muscles. Br J Ophthalmol. 2011;95(9):1255–1258. doi: 10.1136/bjo.2010.188946 [DOI] [PubMed] [Google Scholar]
- 4.Wu CH, Chang TC, Liao SL. Results and predictability of fat-removal orbital decompression for disfiguring graves exophthalmos in an Asian patient population. Am J Ophthalmol. 2008;145(4):755–759. doi: 10.1016/j.ajo.2007.11.020 [DOI] [PubMed] [Google Scholar]
- 5.Segni M, Bartley GB, Garrity JA, Bergstralh EJ, Gorman CA. Comparability of proptosis measurements by different techniques. Am J Ophthalmol. 2002;133(6):813–818. doi: 10.1016/s0002-9394(02)01429-0 [DOI] [PubMed] [Google Scholar]
- 6.Ameri H, Fenton S. Comparison of unilateral and simultaneous bilateral measurement of the globe position, using the Hertel exophthalmometer. Ophthal Plast Reconstr Surg. 2004;20(6):448–451. [DOI] [PubMed] [Google Scholar]
- 7.Burch HB, Wartofsky L. Graves’ ophthalmopathy: current concepts regarding pathogenesis and management. Endocr Rev. 1993;14(6):747–793. doi: 10.1210/edrv-14-6-747 [DOI] [PubMed] [Google Scholar]
- 8.Alsuhaibani AH, Carter KD, Policeni B, Nerad JA. Orbital volume and eye position changes after balanced orbital decompression. Ophthal Plast Reconstr Surg. 2011;27(3):158–163. doi: 10.1097/IOP.0b013e3181ef72b3 [DOI] [PubMed] [Google Scholar]
- 9.Lam AK, Lam CF, Leung WK, Hung PK. Intra-observer and inter-observer variation of Hertel exophthalmometry. Ophthalmic Physiol Opt. 2009;29(4):472–476. doi: 10.1111/j.1475-1313.2008.00617.x [DOI] [PubMed] [Google Scholar]
- 10.Kashkouli MB, Nojomi M, Parvaresh MM, Sanjari MS, Modarres M, Noorani MM. Normal values of hertel exophthalmometry in children, teenagers, and adults from Tehran, Iran. Optom Vis Sci. 2008;85(10):1012–1017. doi: 10.1097/OPX.0b013e3181890dc7 [DOI] [PubMed] [Google Scholar]
- 11.Kashkouli MB, Beigi B, Noorani MM, Nojoomi M. Hertel exophthalmometry: reliability and interobserver variation. Orbit. 2003;22(4):239–245. [DOI] [PubMed] [Google Scholar]
- 12.Mourits MP, Lombardo SH, van der Sluijs FA, Fenton S. Reliability of exophthalmos measurement and the exophthalmometry value distribution in a healthy Dutch population and in Graves patients. An Exploratory Study. Orbit. 2004;23(3):161–168. [DOI] [PubMed] [Google Scholar]
- 13.Sleep TJ, Manners RM. Interinstrument variability in Hertel-type exophthalmometers. Ophthal Plast Reconstr Surg. 2002;18(4):254–257. doi: 10.1097/01.IOP.0000021971.72318.95 [DOI] [PubMed] [Google Scholar]
- 14.Vardizer Y, Berendschot TT, Mourits MP. Effect of exophthalmometer design on its accuracy. Ophthal Plast Reconstr Surg. 2005;21(6):427–430. [DOI] [PubMed] [Google Scholar]
- 15.Beden U, Ozarslan Y, Oztürk HE, et al. Exophthalmometry values of Turkish adult population and the effect of age, sex, refractive status, and the Hertel base values on Hertel readings. Eur J Ophthalmol. 2008;18(2):165–171. [DOI] [PubMed] [Google Scholar]
- 16.Fang ZJ, Zhang JY, He WM. CT features of exophthalmos in Chinese subjects with thyroid-associated ophthalmopathy. Int J Ophthalmol. 2013;6(2):146–149. doi: 10.3980/j.issn.2222-3959.2013.02.07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kim IT, Choi JB. Normal range of exophthalmos values on orbit computerized tomography in Koreans. Ophthalmologica. 2001;215(3):156–162. doi: 10.1159/000050850 [DOI] [PubMed] [Google Scholar]
- 18.Nkenke E, Benz M, Maier T, et al. Relative en- and exophthalmometry in zygomatic fractures comparing optical non-contact, non-ionizing 3D imaging to the Hertel instrument and computed tomography. J Craniomaxillofac Surg. 2003;31(6):362–368. [DOI] [PubMed] [Google Scholar]
- 19.Nkenke E, Maier T, Benz M, et al. Hertel exophthalmometry versus computed tomography and optical 3D imaging for the determination of the globe position in zygomatic fractures. Int J Oral Maxillofac Surg. 2004;33(2):125–133. doi: 10.1054/ijom.2002.0481 [DOI] [PubMed] [Google Scholar]
- 20.Ramli N, Kala S, Samsudin A, et al. Proptosis–correlation and agreement between hertel exophthalmometry and computed tomography. Orbit. 2015;34(5):257–262. doi: 10.3109/01676830.2015.1057291 [DOI] [PubMed] [Google Scholar]
- 21.Cole HP 3rd, Couvillion JT, Fink AJ, Haik BG, Kastl PR. Exophthalmometry: a comparative study of the Naugle and Hertel instruments. Ophthalmic Plast Reconstr Surg. 1997;13(3):189–194. [PubMed] [Google Scholar]