Abstract
Healthcare in the United States is undergoing a transition from volume to value. Current alternative payment models (APMs) use value-based payments to incentivize providers to provide high-quality care and generate short-term savings. In 2017, an estimated thirty-four percent of all health care payments in the United States were issued as part of an APM, with further growth projected in coming years.1 To date, APMs have demonstrated mixed success in reducing total costs—potentially because of the lead time needed to engage providers and payers—but also potentially because of an issue with the design of the APMs.2,3 Current APMs may not provide strong enough incentives for meaningful practice transformation necessary to address determinants of health care costs outside of current clinical workflows.4 For example, even though unaddressed mental health and substance use are significant cost drivers,5,6 early evidence found that many Accountable Care Organizations (ACOs) did not taken meaningful steps to improve their behavioral health care.7 To reduce total costs, APMs will likely need to share both short- and long-term savings achieved with providers, offering sufficient financial incentives for implementing new interventions or building out new population health management capabilities necessary to curb costs.
This paper explores the incentive misalignment that arises from current APM design; outlines an approach to building on APMs using a construct of “Net Present Value of Care” (NPVoC) to share both past-year savings and the future-years savings predicted by past-year health outcomes; and explores potential initial applications for NPVoC-based APMs as well as limitations to the approach.
Total Cost of Care and Current APMs
Most APMs today share a common mechanism for determining the amount of value-based payments. In most APMs, the payer determines the benchmark expected costs for a population attributed to a provider over a time period, the provider offers care to the population, and the payer shares some proportion of the savings in the actual costs incurred (the Total Cost of Care or TCOC) relative to the benchmark – adjusted by whether the provider met quality goals. While APMs differ, this TCOC-based methodology generally spans models, from population-based payment models like ACOs to episode-based payment models like Bundled Payments for Care Improvement (BPCI) Advanced. Because the APMs focus on past-year or past-episode savings to determine incentives, TCOC-based models focus efforts on annual cost-containment rather than long-term health promotion and overall cost drivers.
For example, depression after an acute myocardial infarction (AMI) significantly predicts high-cost health events in the next two years.8 Current APMs could cover the initial AMI and related costs in the near term under their TCOC calculations, but costs predicted by post-AMI depression that occurs over a year later, however, would fall under a different TCOC calculation cycle (or may even fall outside of an APM entirely). The mental health care to address post-AMI depression and reduce the likelihood of later costs would fall under the first TCOC calculation, potentially counting against the shared-savings. Unless the providers have relative certainty that they will be able to share in the later savings, or the quality measures correctly reinforce the activity, the TCOC-based APM design may financially disincentivize efforts to address depression and reduce associated costs.
Depression post-AMI is just a single example. Many cost-saving interventions take more than a single year to produce those savings—especially in behavioral health and primary prevention.9 Some enterprising provider groups do make longer-term investments to capture greater shared-savings in later payment cycles,10 but the design of the current APMs does not effectively reinforce these decisions. APM design should ideally incentivize providers to promote both short-term and longer-term cost-savings to realize health reform goals.
Net Present Value of Care and Its Potential
Slight changes in the APM methodology could more effectively capture longer-term payoffs. Payers can build on TCOC to share both past-year savings and some of the future years savings that the providers’ past-year outcomes predict (see Figure 1). For example, if depression remission post-AMI predicts $1000 in savings over the next two years, then a payer could offer $500 incentive for each past-year depression remission post-AMI achieved over the expected benchmark for the attributed population. By incorporating future savings into the shared-savings methodology, the APMs use NPVoC rather than TCOC for calculating shared-savings. In 2018, Maryland used this logic in its updated all-payer model by introducing “outcomes-based credits,” in which the Centers for Medicare and Medicaid Services (CMS) give a credit toward the annual shared-savings incentives based on the expected future savings to CMS associated with improvements in certain population health outcomes.11 The approach has yet to be applied to provider group APMs, but would be just as applicable.
Figure. 1.
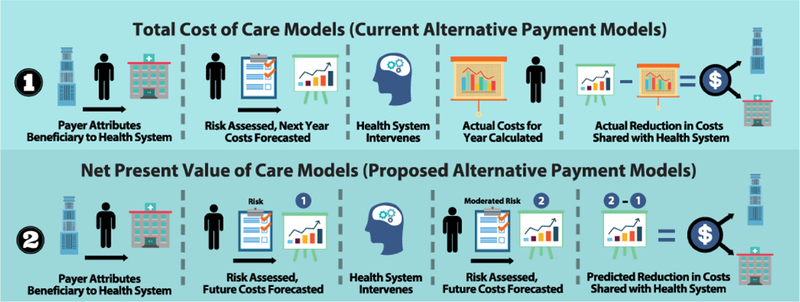
Comparison of TCOC-based APMs and NPVoC-Based APMs.
With NPVoC, payers can build the financial logic for the long-term cost-neutrality of health promotion and prevention into their APM designs. As long as the total amount paid in shared-savings does not exceed the future savings predicted by past-year outcomes, the payer can be relatively confident that the investment will be at least cost-neutral over the long-term. NPVoC-based APMs can incentivize the providers to invest in effective depression care post-AMI, or take on other opportunities to achieve savings over more than a single year. This approach also may intrinsically risk adjusts and promotes health equity, as there may be greater opportunities for savings where there are more expected health care needs.12 By making the longer-term savings more salient, NPVoC-based APMs incentivize investment in interventions that are more likely to decrease overall health care costs, resulting in lower total spending for the payer, greater revenue for the provider, and better population health for those served.
Applications and Considerations for NPVoC
NPVoC-based APMs would require additional research, infrastructure, and policy change to implement at scale, but important applications are viable today. At present, payers may have limited ability to determine the amount of longer-term cost savings predicted by past-year outcomes. Further, the duration over which an individual is likely to remain with a payer likely varies widely and may only be a year or two in many cases, limiting the time over which future savings can be considered. Some payers though do expect to cover some populations for at least several years, and payers can calculate the NPVoC conservatively at first, minimizing any potential losses while still creating potentially salient incentives. Initial NPVoC-based APMs can be tested in settings where they are most likely to be successful and then iteratively improved upon—as has been the process with many APMs to date, with two examples presented in Figure 2.
Figure 2.
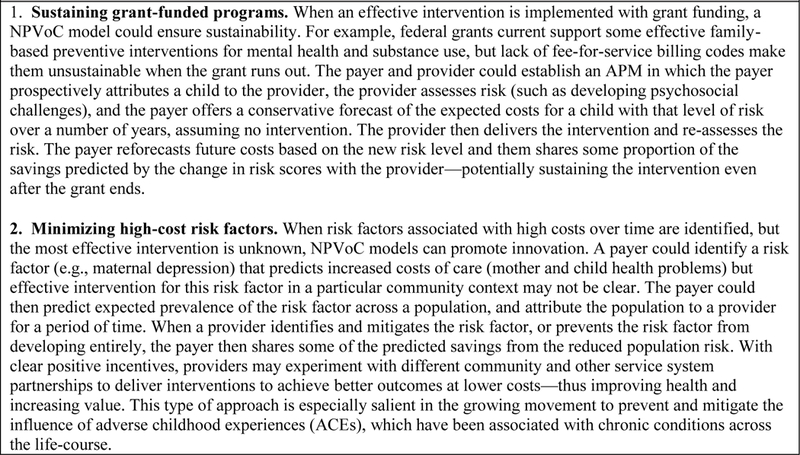
Two Current Applications of Net Present Value of Care.
For NPVoC-based APMs to be successful at scale, payers would need changes in both their infrastructure and incentives. To capture short-term clinical outcomes of interest and build meaningful predictive models, payers and providers will need enhanced data collection systems. As health and non-health care data systems are increasingly integrated13 and the richness of information in health care grows with the focus on health-related social needs,14 more precise models can be built for NPVoC. To increase the relevance of these calculations, payers will also need additional incentives to promote long-term cost-savings. Approaches such as multi-payer or all-payer arrangements, in which multiple health payers agree to similar and mutually beneficial policies, can increase the relevant time horizon as payers will be able to reap collective benefits even when individuals switch coverage between payers.15
NPVoC-based payment also require additional protections at scale. As with all value-based payment models, payers will need to be careful which past-year performance measures they value, as sharing predicted future savings could further magnify misaligned incentives created by inappropriate measures. The increasing incentives also raise issues in gamesmanship, if, for example, apparent improvements in outcomes reflect changes in coding practices rather than more effective interventions. As with other payment models, an auditing methodology can be established to identify and investigate possible exploitation of incentives. Standard incentives will also need to be set for avoiding serious adverse events that may not technically cost a payer very much, such as when an intervention would not be cost-saving long-term because the individual would otherwise die. Regulations could set standard penalties for use in NPVoC APMs, in the way that all-cause mortality following hospitalization is included as a performance measure in some current APMs as a check against inappropriate shared savings.
NPVoC also only promotes the implementation of cost-saving interventions, not cost-effective interventions that do not otherwise save money overall. Additional work on aligning cost-effectiveness with the “value” in value-based payment more generally would be necessary to address this issue.
Conclusion
As the steady progress of healthcare reform continues, payers and providers have the opportunity to pioneer a next generation of value-based payment focused on the Net Present Value of Care. To the extent that the amount of predicted savings to be shared is more than the cost to intervene, the NPVoC model can sustain effective interventions, drive down health care costs, and improve population health.
Acknowledgments
The authors received no funding for the completion of this work.
References
- 1.Measuring Progress: Adoption of Alternative Payment Models in Commercial, Medicaid, Medicare Advantage, and Fee-for-Service Medicare Programs. Health Care Payment and Learning Action Network; 2018. October 22 http://hcp-lan.org/workproducts/apm-methodology-2018.pdf [Google Scholar]
- 2.Smith KW, Bir A, Freeman NL, Koethe BC, Cohen J, Day TJ. Impact of health care delivery system innovations on total cost of care. Health Affairs. 2017. March 1;36(3):509–15. [DOI] [PubMed] [Google Scholar]
- 3.McWilliams JM, Hatfield LA, Landon BE, Hamed P, Chernew ME. Medicare Spending after 3 Years of the Medicare Shared Savings Program. New England Journal of Medicine. 2018. September 20;379(12):1139–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Briggs AD, Alderwick H, Fisher ES. Overcoming challenges to US payment reform: could a place-based approach help?. Jama. 2018. April 17;319(15):1545–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Roehrig C Mental disorders top the list of the most costly conditions in the United States: $201 billion. Health Affairs. 2016. May 18;35(6):1130–5. [DOI] [PubMed] [Google Scholar]
- 6.de Oliveira C, Cheng J, Vigod S, Rehm J, Kurdyak P. Patients with high mental health costs incur over 30 percent more costs than other high-cost patients. Health Affairs. 2016. January 1;35(1):36–43. [DOI] [PubMed] [Google Scholar]
- 7.Busch AB, Huskamp HA, McWilliams JM. Early efforts by Medicare accountable care organizations have limited effect on mental illness care and management. Health Affairs. 2016. July 1;35(7):1247–56. [DOI] [PubMed] [Google Scholar]
- 8.Meijer A, Conradi HJ, Bos EH, Thombs BD, van Melle JP, de Jonge P. Prognostic association of depression following myocardial infarction with mortality and cardiovascular events: a meta-analysis of 25 years of research. General hospital psychiatry. 2011. May 1;33(3):203. [DOI] [PubMed] [Google Scholar]
- 9.Counts NZ, Halfon N, Kelleher KJ, Hawkins JD, Leslie LK, Boat TF, McCabe MA, Beardslee WR, Szapocznik J, Brown CH. Redesigning Provider Payments to Reduce Long-Term Costs by Promoting Healthy Development. NAM Perspectives. 2018. April 20 https://nam.edu/wp-content/uploads/2018/05/Redesigning-Provider-Payments-to-Reduce-Long-Term-Cost-paper.pdf [Google Scholar]
- 10.Kelleher K, Reece J, Sandel M. The Healthy Neighborhood, Healthy Families Initiative. Pediatrics. 2018. September 1;142(3):e20180261. [DOI] [PubMed] [Google Scholar]
- 11.Maryland Total Cost of Care Model. U.S. Centers for Medicare & Medicaid Services. Accessed on 12 Dec 2018 https://innovation.cms.gov/initiatives/md-tccm/
- 12.Joynt Maddox KE. Financial Incentives and Vulnerable Populations—Will Alternative Payment Models Help or Hurt?. New England Journal of Medicine. 2018. March 15;378(11):977–9. [DOI] [PubMed] [Google Scholar]
- 13.Washington V, DeSalvo K, Mostashari F, Blumenthal D. The HITECH era and the path forward. New England Journal of Medicine. 2017. September 7;377(10):904–6. [DOI] [PubMed] [Google Scholar]
- 14.The Accountable Health Communities Health-Related Social Needs Screening Tool. Centers for Medicare & Medicaid Services. 2018. January 8 https://innovation.cms.gov/Files/worksheets/ahcm-screeningtool.pdf [Google Scholar]
- 15.Nichols DE, Haber SG, Romaire MA, Wensky SG. Changes in Utilization and Expenditures for Medicare Beneficiaries in Patient-centered Medical Homes: Findings From the Multi-Payer Advanced Primary Care Practice Demonstration. Medical care. 2018. September 1;56(9):775–83. [DOI] [PubMed] [Google Scholar]


