Abstract
Background:
Emergency Departments (EDs) are beginning to notify their physicians of patients reporting chronic noncancer pain (CNCP) who frequent EDs, and are suggesting that the physicians not prescribe opioids to these patients.
Objectives:
We hypothesized that this intervention would reduce both the number of opioids prescribed to these patients by their ED physicians and the number of these patients’ return visits to the ED.
Methods:
We conducted a randomized controlled trial of this intervention in 13 electronically linked EDs. Patients eligible for the study were characterized by CNCP, lacked evidence of sickle cell anemia and suicide ideation, and made frequent (>10) visits to the EDs over a 12-month period. We randomly assigned 411 of these patients to either an intervention group or a control group. Our intervention comprised both an alert placed in eligible patients’ medical files and letters sent to the patients and their community-based providers. The alert suggested that physicians decline requests for opioid analgesic prescriptions and instead refer these patients to community-based providers to manage their ongoing pain.
Results:
During the 12 months after randomization, patients in the intervention and control groups averaged 11.9 and 16.6 return visits, and received prescriptions for opioids on 16% and 26% of those visits, respectively. Altogether, patients in the intervention group made 1033 fewer return visits to the EDs in the follow-up year than those in the control group.
Conclusion:
This intervention constitutes a promising practice that EDs should consider to reduce the number of visits made by frequent visitors with CNCP.
Keywords: chronic noncancer pain, frequent visitors, emergency departments
INTRODUCTION
Deaths due to the misuse of opioids nearly doubled in the 10-year period ending in 2007 (1). The age-adjusted death rate from unintentional poisoning in the United States increased by 125% from 1999 to 2007, and prescription drugs have accounted for at least 90% of the deaths over that period (2). Between 1999 and 2008, the rate of admissions to drug treatment facilities reporting pain medication abuse increased by 400% (3). Further, between 1999 and 2006, the use of prescription opioids quadrupled in the United States (4). There is a linear relationship between sales of prescribed opioids and mortality attributable to drug poisoning (5). In 2012, about 2.6% of Americans aged 12 years and over reported that they had used prescription psychotherapeutic drugs in the past year that had not been prescribed to them, and about 8000 people develop opioid addiction daily (6,7). In 2006, the nonmedical use of oxycodone and hydrocodone accounted for 120,000 emergency department (ED) visits, and rates of ED visits related to narcotic analgesics rose by 155% between 2004 and 2009 (8,9). The total costs of prescription opioid abuse to society as of 2009 were estimated at $55.7 billion, of which $25.0 billion were borne by the health care system, $25.6 billion related to workplace costs, and $5.1 billion were associated with costs related to criminal justice (10).
Deaths attributable to opioid analgesics are increasingly recognized as preventable (9). Hospital EDs, which are a source of prescription drugs that patients may then either misuse or provide to others, constitute one appropriate target for prevention efforts (11). In response, some EDs have begun to develop a strategy to notify their providers of patients who frequently visit EDs seeking treatment for chronic noncancer pain (CNCP). The strategy typically suggests that the ED provider decline the patients’ requests for controlled substances and instead advise them to seek help managing their chronic pain from a community-based primary care provider (12). Given that repeat visitors often appear at EDs due to pain-related symptoms, they are at elevated risk of being prescribed medications associated with increased risk of injury (13,14). One study found that repeat visitors with 25 or more visits in the prior year had five times the odds of having a past prescription for an opioid compared to individuals with no history of an ED visit in the prior year (15).
Two previous evaluations of ED-based interventions of this nature have noted substantial reductions in ED visits, one by 40.9% and the other by 71.6% (16,17). However, both used single-group designs with very small samples (36 and 24 patients, respectively). In addition, unpublished data available from studies of interventions that have been conducted in Olympia and Spokane, Washington have reported reductions in ED visits of 55% and 48%, respectively (18,19). However, this approach to the care of patients with CNCP in EDs has yet to be subjected to a formal evaluation.
In this article we present the results of a randomized controlled trial of an intervention designed to reduce both the number of opioids prescribed by ED physicians to repeat ED visitors reporting CNCP, and the number of hospital visits made by these patients. The intervention in the study consisted of an alert placed in patients’ medical files and a letter sent to the patients and their community-based providers. The alert suggested that physicians decline requests for repeat opioid prescriptions and instead refer these patients to community-based providers to manage their ongoing pain. The letter informed patients and their community-based providers of this protocol. We hypothesized that patients in the intervention group would manifest both fewer return visits to the EDs and fewer prescriptions for opioid medications from study ED providers, compared to patients in the control group.
MATERIALS AND METHODS
Setting
The Injury Prevention Research Center of the University of North Carolina at Chapel Hill conducted this study in collaboration with Carolinas HealthCare System (CHS), located in Charlotte, North Carolina. CHS constitutes one of the largest public hospital systems in the United States, and contributed 13 of their electronically net-worked EDs to the study. The EDs participating in the study were located in five contiguous counties that included both metropolitan and rural areas.
Intervention
The intervention for this study comprised two components, of which the first consisted of an alert placed in patients’ electronic medical records. The alert informed pertinent ED staff that the patients were enrolled in the study’s intervention group, that a multidisciplinary review team at CHS had determined that the patients had made multiple visits to various CHS EDs for treatment of CNCP, and that it was in the patients’ best interests to receive treatment for their pain from a community-based provider. The alert continued by recommending that the ED provider should suggest to these patients that they visit a community-based primary care provider, pain clinic, or other facility such as a drug treatment or mental health facility. In addition, we instructed ED staff to give each of these patients a list of appropriate community resources, which the study provided to ED staff. The intervention also invited the ED provider not to prescribe opioid medications to the patient, and not to write prescriptions for any medications that the patient reported as lost or stolen. However, the alert also stated that the provider should follow a customary standard of care for patients presenting with acute pain, and that the provider’s clinical judgment should ultimately determine the nature of the care offered for both acute and chronic pain.
The second component of the intervention was a letter sent to both patients and their community-based providers. The letter informed patients that a group of medical providers affiliated with CHS had determined that they should no longer receive opioid pain medication for their CNCP from a CHS ED, and their pain would best be treated by a community-based provider. However, to avoid discouraging use of the ED for medical emergencies, the letter encouraged the patient to return to the ED for assistance with other medical needs. The letter also included a phone number that patients could use to call with any concerns related to the letter and informed them that we had mailed a similar letter to their primary care provider if one was listed in their electronic medical record. Copies of the text of the electronic alert and the letters we sent to both the patients and their primary care providers are available from the first author upon request.
Patients enrolled in the control group did not receive either of the intervention components.
Participant Selection
Study subjects for this randomized controlled trial were identified in a step-wise fashion. We initially identified patients by reviewing electronic medical charts over a 12-month period from October of 2010 to September of 2011. Patients eligible for the study were between 18 and 89 years of age and had visited CHS’ EDs more than 10 times over this period. As we found no established definition of “frequent” ED use, we selected 11 visits as an arbitrary threshold to include patients who had visited the ED almost monthly (20). This initial process yielded a potential sample pool of 1539 patients. To secure the sample for our study, we reviewed each of these patients’ medical records in a downward hierarchical fashion beginning with those who had made the largest number of visits.
During an 8-month period beginning in October of 2011, a clinical staff team reviewed and summarized every visit made by each patient. This summary included the presenting complaint, discharge codes, all physicians’ notes related to acute and chronic pain, and all pain medicines either administered in the ED or written as a prescription. Key terms that we utilized in our review of physicians’ notes included chronic or acute pain; injury; drug abuse, misuse, or addiction; cancer; and suicide or self-harm.
Inclusionary criteria for the study comprised patients who, in at least two of these visits, had a discharge code related to nonspecific, subjective pain, which we defined as back or neck pain, headache or migraine, arthritis or joint pain, chronic pain syndrome, or generalized pain. We also applied a set of exclusionary criteria, namely, patients who had preexisting sickle cell anemia or a diagnosis of cancer (other than nonmelanoma skin cancer), to ensure that we would do nothing to harm these vulnerable populations by suggesting that their providers deny them the opioid analgesics they might need to manage their pain. We also excluded patients who had not visited the ED within the 120 days preceding the end of the eligibility period, reasoning that they may have moved out of the area or found an alternate source for pain management. A committee of eight medical staff who represented a variety of medical professions experienced with responding to opioid-abusing patients, and who comprised ED providers, a dentist, a pharmacist, and an orthopedist, reviewed each chart summary. They then voted as to whether to exclude any patients who were potentially eligible for the study. This committee discussed the records of any patients whose vote was not unanimous, and a majority vote determined whether the patient was ultimately eligible for enrollment.
As specified in Figure 1, we excluded 382 (48%) of 793 patients identified with the highest number of ED visits, who in aggregate had made an average of 14 visits (SD = 18) to at least one of CHS’ EDs in the previous 12 months. Of these, 107 had not visited any of CHS’ constituent EDs in the 120 days prior to the conclusion of the eligibility period. Subsequent to our initial enrollment procedures, but prior to random assignment, we learned that one of CHS’ EDs had previously instituted a set of protocols similar to ours, and we dropped the 22 patients identified as having been enrolled in that plan. Additionally, because two CHS ED facilities chose not to participate in the study, we also excluded 188 patients who made the majority of their visits during the eligibility period to these EDs. We excluded an additional 49 patients because they lacked a diagnosis of chronic pain or because their records provided evidence of any of the other reasons specified in this figure, including suicide attempts or ideation. We excluded these latter patients because we were concerned that our intervention might precipitate suicidal behavior among patients who were already so disposed.
Figure 1.
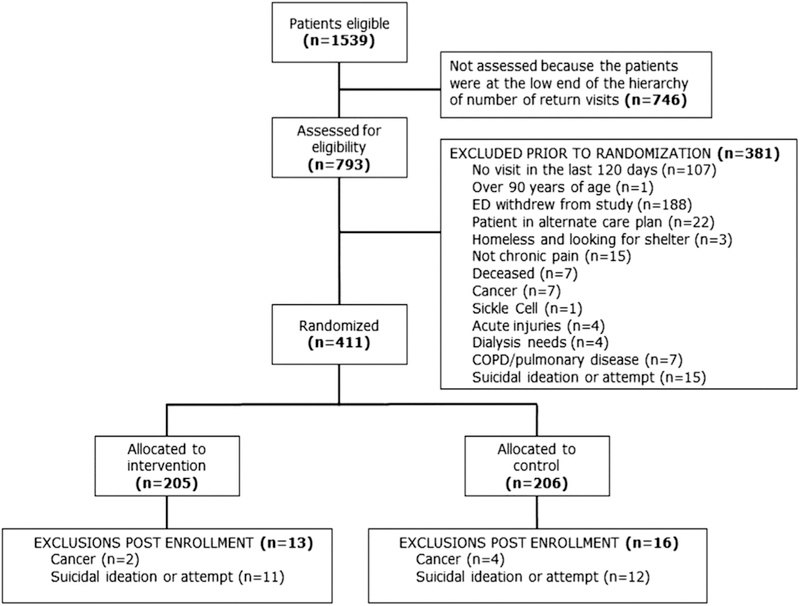
Flow chart of patients initially eligible to participate in the study. COPD = chronic obstructive pulmonary disease; ED = emergency department.
Using a Web-based random number generator, the first author randomly assigned 204 and 206 patients to the intervention and control groups, respectively, within four consecutive cohorts over 51 days beginning in May 2012 and continuing through August of that year. During the course of the 12-month intervention for each cohort, we identified 13 and 16 patients in the intervention and control groups, respectively, whom we learned, from an ongoing review of their medical records, had received a new cancer diagnosis or had attempted or considered suicide. We then removed these patients from the study because they no longer met its eligibility criteria, and did not follow them further. However, these patients continued to provide data for our intent-to-treat study until the date they received either of these diagnoses. Five participants from the intervention group were excluded after randomization but prior to the activation of the intervention because they manifested evidence of exclusionary criteria within this period. We completed data collection for all subjects in July of 2013. See Figure 2 for a schematic of the study timeline.
Figure 2.
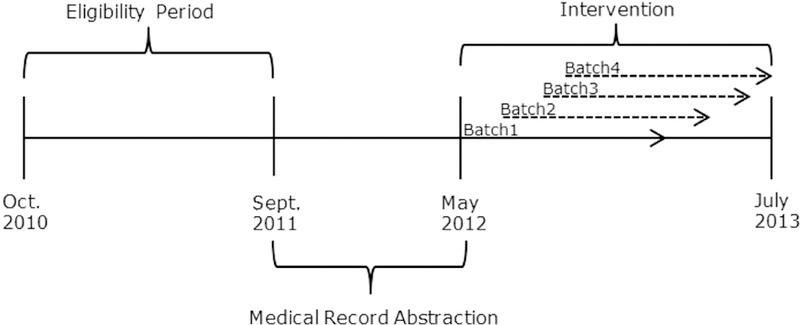
Study timeline.
Our calculations indicated that a sample size of 204 and 206 patients in the intervention and control groups, respectively, would have 66% effect to detect a difference in means between the two groups of 2.5 visits, assuming a common SD of 10.60 using a two-group t-test (p < 0.05) (21,22). The estimation was based on the assumption that the intervention would result in a 37% reduction in ED visits in the intervention group. We calculated the SD using the SD of total hospital visits for the entire study population during the baseline period.
Because we were primarily interested in changing ED providers’ prescribing practices, we secured consents (response rate = 96%) only from CHS’ ED providers. All study protocols were approved by the Institutional Review Boards (IRBs) of both Injury Prevention Research Center of the University of North Carolina at Chapel Hill and Carolinas HealthCare System, which granted us waivers of active patient consent because they determined the risk of harm to patients was no more than minimal, that patients would never be denied care they needed, and that their data would be fully de-identified before CHS shared the data with investigators at Injury Prevention Research Center of the University of North Carolina at Chapel Hill. The IRBs further determined that we could not reasonably have conducted our study had patient-level consent been required.
Methods and Measurements
The primary goals of the intervention were to reduce provider prescribing of opioids to frequent ED visitors and to improve CNPC. Due to data constraints, we were unable to directly measure the effect of the intervention on providers’ prescribing behaviors. However, we did measure the number of visits study subjects made to CHS EDs for any reason and the number of written prescriptions for opioid analgesics they received from ED providers that will serve as proxy outcome measures in the analyses. We identified opioid prescriptions from patients’ electronic medical records employing charge codes and National Drug Classification codes. We also collected descriptive data concerning patients enrolled in the study, and characteristics of their ED visits during the year prior to the study’s onset, that we used to determine initial eligibility. Descriptive data included gender, age, payer type, primary complaint at admission by patient, and discharge diagnosis by physician. We categorized primary complaints and discharge diagnoses related to CNCP as neck pain, headache or migraine, chronic pain, generalized pain, or other, the International Classification of Diseases, Ninth Revision (ICD-9) codes for which may be found in Table 1. We also used ICD-9 codes to identify patients’ primary complaint at admission and physician discharge diagnosis.
Table 1.
Hospital Visit Information During Twelve-month Baseline Period Prior to Intervention Activation*
| Intervention (n = 4544) | Control (n = 4515) | Total (n = 9059) | p-Value | |
|---|---|---|---|---|
| Primary complaint, n (%)† | 0.17 | |||
| Neck pain | 511 (11.3) | 485 (10.7) | 996 (11.0) | |
| Headache or migraine | 325 (7.2) | 543 (12.0) | 868 (9.6) | |
| Chronic pain | 24 (0.5) | 29 (0.6) | 53 (0.6) | |
| Generalized pain | 492 (10.8) | 388 (8.6) | 880 (9.7) | |
| Other | 3192 (70.3) | 3070 (68.0) | 6262 (69.1) | |
| Admission diagnosis, n (%)† | 0.21 | |||
| Neck pain | 353 (7.8) | 322 (7.1) | 675 (7.5) | |
| Headache or migraine | 293 (6.5) | 515(11.4) | 808 (8.9) | |
| Chronic pain | 50 (1.1) | 52 (1.2) | 102 (1.1) | |
| Generalized pain | 409 (9.0) | 304 (6.7) | 713(7.9) | |
| Other | 3439 (75.7) | 3322 (73.6) | 6761 (74.6) | |
| Payer type, n (%) | 0.10 | |||
| Commercial/managed care | 408 (9.0) | 469 (10.4) | 877 (9.7) | |
| Medicaid | 3122 (68.7) | 3047 (67.5) | 6169(68.1) | |
| Medicare | 976 (21.5) | 977 (21.6) | 1953(21.6) | |
| Other‡ | 38 (0.8) | 22 (0.5) | 60 (0.7) | |
| ED visits | 0.64 | |||
| Mean (SD) | 22.72 (12.4) | 21.92 (8.7) | 22.31 (10.6) | |
| Prescribed opioids | 0.04 | |||
| Mean (SD) | 0.26 (0.5) | 0.28 (0.5) | 0.27 (0.5) | |
ED = emergency department.
Percentages are column based.
International Classification of Diseases, Ninth Revision codes. Neck Pain: 723, 723.1 722.7, 722.71, 722, 722.1, 724, 724.2, 724.5; Headache/Migraine: 307.81, 339, 339.01, 339.02, 339.05, 339.1, 339.11, 339.12, 339.2, 339.21, 339.22, 339.3, 339.4, 339.42, 339.43, 339.44, 339.8, 339.81, 339.82, 339.83, 339.84, 339.85, 339.89, 784, 346, 346.01, 346.02, 346.03. 346.1, 346.11. 346.12, 346.13, 346.2, 346.21, 346.22, 346.23, 346.3, 346.31, 346.32, 346.33, 346.4, 346.41, 346.42, 346.43, 346.5, 346.51, 346.52, 346.53, 346.6,346.61, 346.62, 346.63, 346.7, 346.71, 346.72, 346.73, 346.8, 346.81, 346.82, 346.83, 346.9,346.91, 346.92, 346.93; Chronic Pain: 338.2, 338.21, 338.22, 338.28, 338.29, 339.3, 338.4; Generalized Pain: 338, 338.1, 338.11, 338.12, 338.18, 338.19, 780.96, 789, 789.07.
Other includes: Workers Compensation, North Carolina agencies/correctional facilities, bankruptcy, clinical denial, Civilian Health and Medical Program of the Uniformed Services (CHAMPUS), estates, facility billing, liabilities, Medicaid pending, management review, small claims, technical denial, VIP.
Analysis
We began by examining the patient-level variables specified above at baseline, both to describe our sample and to determine the success of randomization in achieving equivalency across the study’s two groups. To that end we used bivariate analyses to detect any differences in baseline characteristics between study groups. We also employed Wilcoxon-Mann Whitney tests to detect differences in continuous variables between groups, and Mantel-Haenszel chi-squared statistics to detect differences in categorical variables between groups.
To address the study’s two hypotheses, we compared differences between the intervention and control groups in the number of 1) ED visits patients made and 2) prescriptions for opioids they received from emergency physicians. In our initial analysis of these hypotheses, we used t-tests to determine any difference between groups. We then ran two Poisson regressions, one crude and one adjusted, for both hospital visits and prescribed opioids. We adjusted the multivariate models for participant race and baseline opioid prescriptions because they were found to differ significantly between groups at baseline. We assessed each model for over-dispersion and, if it was present, used a negative binomial model instead (23). Because we could not assume independence between patient-level observations, insofar as patients could be clustered both within EDs and providers, we employed robust standard errors for repeated subjects, with an equi-correlated covariance structure in all models. We established a threshold of significance as p < 0.05, and conducted all analyses using SAS Version 9.3 (Cary, NC).
RESULTS
A total of 406 patients were included in the final analysis, 200 and 206 randomized to the intervention and control groups, respectively. As displayed in Table 2, the average patient in both study groups was 39 years old, female, and white. However, we did find a significantly higher (p = 0.004) proportion of white patients in the control than the intervention group.
Table 2.
Baseline Patient Characteristics
| Intervention (n = 200) |
Control (n = 206) |
Total (n = 406) |
p-Value | |
|---|---|---|---|---|
| Age | ||||
| Mean (SD) | 38.98 (11.2) | 39.70 (12.2) | 39.34 (11.7) | 0.78 |
| Gender | ||||
| Male (%) | 81 (40.5) | 68 (33.0) | 149 (36.7) | 0.12 |
| Female (%) | 119 (59.5) | 138 (67.0) | 257 (63.3) | |
| Race | ||||
| White (%) | 126 (63.0) | 158 (76.7) | 284 (70.0) | 0.004 |
| Black (%) | 73 (36.5) | 47 (22.8) | 120 (29.6) | |
| Other (%) | 1 (0.5) | 1 (0.5) | 2 (0.5) | |
Overall, the study’s subjects made a total of 9059 ED visits during the preactivation period, of which patients in the intervention and control groups made 4544 and 4515 visits, respectively. The most common chronic pain-related complaint was neck pain for patients in the intervention group, and headache or migraine for those in the control group. Medicaid paid for nearly all of the hospital visits for both groups. During the 12-month baseline period, patients averaged 22 ED visits and were prescribed an average 0.27 opioid prescriptions (0.26 vs. 0.28 for the intervention and control groups, respectively) per hospital visit: that is, they received an opioid prescription at discharge in slightly over one visit out of four. However, during this period, patients in both the intervention and control groups were administered opioids while being treated in the ED for an average of 91% of their visits (confidence intervals [CIs] ± 1.9 and ± 1.7, respectively, ns). During the follow-up period, our intent-to-treat analysis found that patients in the intervention (n = 200) and control (n = 206) groups were administered opioids in 29% (95% CI 0.27–0.31) and 45% (95% CI 0.43–0.47) of their visits, respectively, and received prescriptions for opioids in 16% (CI 0.15–0.18) and 26% (CI 0.25–0.28) of their visits, respectively.
Table 3 displays the unadjusted comparisons of the study’s two key outcomes, disaggregated by group. As expected, during the study period, patients in the intervention group made significantly fewer hospital visits and received fewer prescribed opioids from emergency physicians than control patients. On average, an intervention patient made nearly five fewer hospital ED visits than did controls (p < 0.001). In Figure 3 we graphically display the disparity between visits made by intervention and control patients over the follow-up period, disaggregated into 13 28-day temporal increments. Altogether, 18 patients (11 in the intervention and 7 in the control group, ns) made no return visits to EDs during the study period. The median number of return visits in the intervention and control groups was 9.0 (range = 0 to 111) and 13.5 (range = 0 to 106), respectively.
Table 3.
Hospital Visit Information by Group During 1-Year Study Period
| Intervention (n = 2387) | Control (n = 3420) | Total (n = 5807) | p-Value | |
|---|---|---|---|---|
| ED visits, mean (SD) | 11.88 (13.8) | 16.57 (14.8) | 14.26 (14.50) | <0.0001 |
| Prescribed opioids, mean (SD) | 0.16 (0.38) | 0.26 (0.45) | 0.22 (0.43) | <0.0001 |
ED = emergency department.
Figure 3.
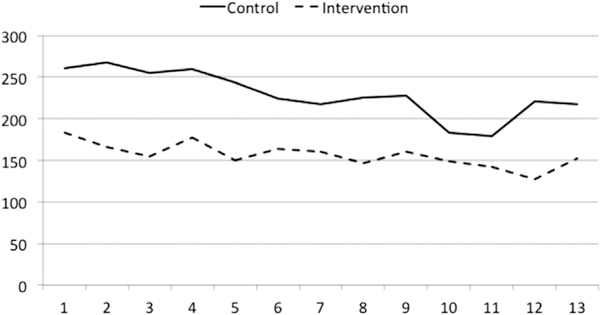
Number of emergency department visits per 28-day period.
Despite randomization, participant race was significantly different between groups. Because this difference may have confounded the crude estimate, we adjusted our regression models for this variable. Table 4 shows the unadjusted and adjusted rate ratios for the main effect regression models. After adjusting for differences in race and baseline prescription opioids, and as compared to those in the control group, patients in the intervention group had 0.69 times the rate of hospital visits (95% CI 0.57–0.84; p < 0.0002,) and 0.57 times the rate of prescribed opioids (95% CI 0.46–0.70; p < 0.0001) during the 1-year follow-up period.
Table 4.
Main Effect Models for Main Outcomes
| Rate Ratio | 95% CI | p-Value | |
|---|---|---|---|
| Number of ED visits* | |||
| Unadjusted | 0.717 | 0.59–0.88 | 0.0012 |
| Adjusted† | 0.690 | 0.57–0.84 | <0.0002 |
| Number of opioid prescriptions‡ | |||
| Unadjusted | 0.570 | 0.46–0.71 | <0.0001 |
| Adjusted† | 0.569 | 0.46–0.70 | <0.0001 |
CI = confidence interval; ED = emergency department.
Negative binomial model used to account for over-dispersion.
Adjusted for participant race and baseline opioid prescriptions.
Poisson model.
DISCUSSION
The results of our study supported our hypotheses that our ED-based care coordination plan targeting frequent visitors with CNCP would decrease in the EDs that participated in the study, the number of both the patients’ repeat visits, and the prescriptions they received for opioid analgesics. We note that these reductions were clinically as well as statistically significant, insofar as they represented reductions of 28% and 38% in the number of return visits by and opioids prescribed to patients in the intervention and control group, respectively.
We were surprised to discover that during the 12-month eligibility period prior to random assignment, the frequent ED visitors in our sample received prescriptions for opioid analgesics in only one visit out of four, which seemed to us an insufficiently consistent incentive to warrant their return visits. However, we also noted that patients in both the intervention and control groups were administered opioids in the ED, prior to their discharge, in almost all (i.e., 91%) of their visits. We thus surmise that patients’ primary incentive for continuing ED visits was to receive parenteral or oral opioids in the ED itself. If so, this finding suggests that the patients in our sample were unlikely to have visited EDs to secure prescriptions for opioids that they subsequently intended to divert.
As expected, the average number of prescriptions for opioids that patients in the control group received per visit during the baseline and follow-up year, 0.27 and 0.26, respectively, remained largely static. However, a visual inspection of Figure 2 reveals a slight downward trend in the monthly increments assessed in prescriptions for both the intervention and control groups. This decline could be attributed to several factors, including a secular trend toward more constrained opioid prescribing practices. It is also possible that as the intervention progressed, providers became more likely to decline opportunities to prescribe opioid analgesics to their CNCP patients. To explore the potential of a provider learning effect over time on these prescribing behaviors, we conducted a post hoc analysis of the association between enrollment cohort and number of prescriptions written and found no association. The decline we noted may also be attributable to contamination effects, as providers sensitized by the flags placed in the files of intervention group patients began to consider these warnings when they treated other frequent visitors reporting chronic pain, including those in the control group. However, we think the most likely factor to which the declines we noted can be attributed is regression to the mean from extreme values; other studies have reported that even in the absence of any intervention, the number of ED visits made by frequent visitors in any given year tend to decrease in the following one, and thus this status may be temporary (24–26).
From the study’s outset we were aware that the EDs in the medical system that served as our study site would be unable to provide continuity of care to uninsured patients enrolled in the intervention group who lacked community-based health providers and thus, potentially, the means to pay for their services. Although we gave consideration to compensating the providers to whom the EDs’ providers might refer these patients, study resources were inadequate to do so. We were also aware that other hospital systems that might adopt an intervention similar to ours would also be unlikely to have discretionary funds that they could offer these patients’ community-based providers, and thus believe that our approach is reflective of the constraints that EDs generally face. However, the overwhelming majority (>99%) of visits made by study patients were supported either by Medicare, Medicaid, or commercial or managed care plans, a finding that is consistent with that reported by other studies of frequent ED visitors (26). We thus expect that almost all the patients in our intervention group should have had access to a community-based provider, although some of those covered by Medicaid may have experienced challenges in scheduling outpatient appointments or in finding a provider who would accept their insurance. That said, we cannot exclude the possibility that we may have harmed some of the patients in our intervention group because they were not administered or prescribed appropriate medications to assist them in managing their pain.
We also note that the process we used to screen out patients as ineligible for the study was both labor intensive and expensive, insofar as it required a close, ongoing scrutiny of patients’ discharge codes and a content analysis of their providers’ chart notes to identify those who either developed a diagnosis of cancer or sickle cell anemia, or who gave evidence of suicide ideation or attempts. As approved by our institutions’ IRBs, our study protocols also required that summaries of each patient’s records be prepared and reviewed by a team of health professionals to ensure that we did not enroll patients who met any exclusionary criteria. We suspect, however, that our procedures, which involved a formal data abstraction process from both coded and textual medical records followed by a review by eight medical staff, may have been unnecessarily cautious. Perhaps an ongoing chart review by one or two medical experts would suffice, as long as it included an inspection of text available in eligible patients’ medical records to verify that no disqualifying criteria are present. We are concerned that staff in EDs that seek to replicate our protocols may not go to sufficient lengths to ensure that patients with diagnoses of cancer-related pain, or those who manifest either suicide ideations or attempts, are exempted from the intervention. In addition, we hope that other EDs that may consider our protocols will have the means that CHS lacked to refer CNCP patients who lacked primary care providers—and particularly those demonstrating evidence of suicide ideation or attempts—to specific community-based health professionals who are trained to manage their chronic pain needs. We believe that the resource guide we provided these patients was adequate but clearly suboptimal.
We also note several issues related to our study’s methodology. The average number of visits our study’s subjects made to the ED, 22.3, was very high - almost twice a month over the course of the initial 12-month period of eligibility determination. Although there is no standard definition for “frequent ED use,” the threshold of four visits per year has appeared frequently in the literature, and one empirical study has defined “highly frequent use’” as at least 18 visits per year (20,26–28). As mentioned earlier, we deliberately selected those patients who had visited CHS’ EDs most frequently to maximize our power to detect differences in return visits between our intervention and control groups. Other EDs serving smaller numbers of frequent visitors with CNCP, who average fewer numbers of visits, may not fully replicate our results.
Limitations
We do not know how the providers who treated the subjects in our intervention group used the flags on their patients’ charts. Some may have discussed the alert with their patients, whereas other may not. Nor do we know if these patients understood the letters we sent to inform them of the intervention, or whether they talked about their plan with their community-based providers. Thus, we are unsure whether their behavior changed as a result of their providers’ behaviors, their own awareness of the content and implications of the intervention, or some combination of both. Insofar as only 5.5% of patients in the intervention group returned to the ED at least once after we sent our initial letters informing them of the intervention, it seems likely that changes in providers’ prescribing behaviors made a significant contribution to the outcomes noted.
Subjects in the intervention group had many alternatives to the services they received in CHS’ EDs. Charlotte, the large metropolitan area in North Carolina that served as the site for our study, has other hospital systems whose records are not linked to those of CHS; patients could also have sought medical care in any of those other facilities, some of which are located in South Carolina, across the nearby state line. Patients may also have secured opioid analgesics from their primary care providers. Thus, patients in our intervention group may have compensated for what they may have perceived as denial of care by seeking medical attention elsewhere.
Other limitations to our study should be considered. First, the heterogeneity of the counties that CHS’ systems served - one urban, several quite rural - increases uncertainty about the external validity of our study’s findings; that is, whether they would likely be replicated in entirely urban or rural environments. Also potentially limiting our study’s external validity is the insurance status of our patient population; as indicated in Table 1, almost all were covered by some form of insurance (about two-thirds by Medicaid and one-fifth by Medicare). Hospital EDs serving populations characterized by very different payer mechanisms may have different experiences with the intervention we tested.
As a final study limitation, we recognize that our patients were clustered both within and across both CHS’ constituent ED providers, who themselves may have served multiple EDs. It is also possible that patients could have been clustered within providers within the same visit, if more than one attended to a particular patient. Rather than attempting to control for this multiple and complex clustering, we chose simply to compare the patients in our intervention and control groups as if they were statistically independent of one another. Thus, our providers may have become sensitized over time to the opioid-seeking behaviors of all the frequent visitors with CNCP whom they treated. If that is indeed the case, our findings may be considered conservative— that is, the true difference between providers’ prescribing behaviors related to patients in the intervention and control groups would have been attenuated. This may also serve to explain two unexpected findings related to our control group: first, that the proportion of control patients who were administered opioid analgesics in the ED decreased from 91% of their visits at baseline to 45% over follow-up, and second (as depicted in Figure 3), that the number making return visits to the ED decreased in each 28-day period. On the other hand, this reduction could also have represented providers’ increasing wariness over time in regards to responding to the articulated pain management needs of this cohort of frequent visitors.
CONCLUSION
Our study has demonstrated the positive effects of our intervention on repeat visits and opioid analgesics prescribed to a population of very frequent visitors to a set of electronically linked EDs who are characterized by CNCP. Hospital systems considering adopting a similar program should do so with the key proviso that frequent visitors be informed that the ED continues to be available to them to manage health concerns unrelated to chronic pain. Frequent ED visitors constitute a highly heterogeneous group who suffer from a variety of physical and psychiatric comorbid conditions, and their access to prompt medical attention to treat these conditions must not be curtailed, particularly as their conditions may not be adequately met by their primary providers (20,24,25,27).
ARTICLE SUMMARY.
-
Why is this topic important?
Some patients with complaints of chronic noncancer pain (CNCP) visit emergency departments (EDs) frequently, seeking controlled substances either to manage their condition or to use or divert for nonmedical reasons.
-
What does this study attempt to show?
In this randomized controlled trial, we investigated the effects of an alert placed in the electronic files of patients enrolled in the intervention group, notifying their providers that they were frequent ED visitors with CNCP whose needs for pain management would best be managed by a community-based provider. We examined whether the alerts would reduce the number of these patients’ return visits to the ED, as well as the number of visits on which they were prescribed controlled substances.
-
What are the key findings?
During the 12 months after randomization, patients in the intervention and control groups averaged 11.9 and 16.6 return visits, and received prescriptions for opioids on 16% and 26% of those visits, respectively.
-
How is patient care impacted?
The alert specified substantially reduced participating EDs’ burden of patients who frequently visited the ED seeking care for CNCP that was more appropriately provided in community-based medical settings.
Acknowledgment
This project was funded by the Centers for Disease Control and Prevention under contract #BAA 2011- N-13277 (grant number: CDC 200–2011-39651). The content is solely the responsibility of the authors and does not necessarily represent the official views of the CDC.
REFERENCES
- 1.Johnston B Harm reduction for unintentional poisoning. Inj Prev 2011;16:217–8. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention (CDC). Prescription painkiller overdoses in the U.S. 2011. Available at: http://www.cdc.gov/VitalSigns/PainkillerOverdoses/index.html. Accessed July 1, 2014. [Google Scholar]
- 3.Office of Applied Studies (OAS), Substance Abuse and Mental Health Services Administration (SAMHSA). Substance abuse treatment admissions involving abuse of pain relievers: 1998 and 2008. The TEDS Report. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2010. Available at: http://oas.samhsa.gov/2k10/230/230PainRelvr2k10.htm. Accessed July 1, 2014. [Google Scholar]
- 4.Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. Web-based Injury Statistics Query and Reporting System (WISQARS). (1999–2007) [2011 Nov 1]. Available at: www.cdc.gov/ncipc/wisqars. Accessed July 1, 2014.
- 5.Paulozzi LJ, Ryan GW. Opioid analgesics and rates of fatal drug poisoning in the United States. Am J Prev Med 2006;31:506–11. [DOI] [PubMed] [Google Scholar]
- 6.Substance Abuse and Mental Health Services Administration (SAMHSA). Results from the 2012 National Survey on Drug Use and Health: summary of national findings, NSDUH Series H-46, HHS Publication No. (SMA) 13–4795. Rockville, MD: SAMHSA; 2013. [Google Scholar]
- 7.Substance Abuse and Mental Health Services Administration (SAMHSA). Results from the 2008 National Survey on Drug Use and Health: national findings (Office of Applied Studies, NSDUH Series H-36, HHS Publication no SMA 09–4434). Rockville, MD: SAMHSA; 2009. [Google Scholar]
- 8.Substance Abuse and Mental Health Services Administration (SAMHSA). Drug Abuse Warning Network, 2006: national estimates of drug-related emergency department visits, DAWN Series D-30, DHHS Publication No (SMA) 08–4339. Rockville, MD: SAMHSA; 2006. [Google Scholar]
- 9.Maxwell J The prescription drug epidemic in the United States: a perfect storm. Drug Alcohol Rev 2011;30:264–70. [DOI] [PubMed] [Google Scholar]
- 10.Birnbaum H, White A, Schiller M, et al. Societal costs of prescription opioid abuse, dependence, and misuse in the United States. Pain Med 2011;12:657–67. [DOI] [PubMed] [Google Scholar]
- 11.Logan J, Liu Y, Paulozzi L, Zhang L, Jones C. Opioid prescribing in emergency departments: the prevalence of potentially inappropriate prescribing and misuse. Med Care 2013;51:646–53. [DOI] [PubMed] [Google Scholar]
- 12.Washington Chapter of American College of Emergency Physicians, Washington State Emergency Nurses Association, Washington State Medical Association, Washington State Hospital Association. Washington emergency department opioid prescribing guidelines. Available at: http://washingtonacep.org/Postings/edopioidabuseguidelinesfinal.pdf. Accessed July 2014.
- 13.Miller JB, Brauer E, Rao H, et al. The most frequent ED patients carry insurance and a significant burden of disease. Am J Emerg Med 2013;31:16–9. [DOI] [PubMed] [Google Scholar]
- 14.Blank FS, Li H, Henneman PL, et al. A descriptive study of heavy emergency department users at an academic emergency department reveals heavy ED users have better access to care than average users. J Emerg Nurs 2005;31:139–44. [DOI] [PubMed] [Google Scholar]
- 15.Doran KM, Raven MC, Rosenheck RA. What drives frequent emergency department use in an integrated health system? National data from the Veterans Health Administration. Am J Emerg Med 2013; 62:151–9. [DOI] [PubMed] [Google Scholar]
- 16.Woodhouse J, Peterson M, Gathercoal K, Campbell C. The efficacy of a brief behavioral health intervention for managing high-utilization of Emergency Department services by patients with chronic pain. J Emerg Nurs 2010;36:399–403. [DOI] [PubMed] [Google Scholar]
- 17.Pope D, Fernades C, Bouthillette F, Etherington J. Frequent uses of the emergency department: a program to improve care and reduce visits. Can Med Assoc J 2000;162:1017–20. [PMC free article] [PubMed] [Google Scholar]
- 18.Busch D, Rubin D. Emergency department consistent care program at Providence St. Peter Hospital: an evaluative report. 2010. Available at: www.crhn.org/www/files/EDCCPEvaluation2010.pdf. Accessed July 1, 2014.
- 19.Neven D Spokane pain initiatives presentation. 2011. Spokane County Medical Society. Available at: http://spcms.org/attachments/SpokanePainInitiatives.pdf. Accessed July 1, 2014.
- 20.LaCalle E, Rabin E. Frequent users of emergency departments: the myths, the data, and the policy implications. Ann Emerg Med 2010; 56:42–8. [DOI] [PubMed] [Google Scholar]
- 21.Dixon WJ, Massey FJ. Introduction to statistical analysis 4th edn New York: McGraw-Hill; 1983. [Google Scholar]
- 22.O’Brien RG, Muller KE. Applied analysis of variance in behavior science New York: Marcel Dekker; 1983. [Google Scholar]
- 23.Gardner W, Mulvey EP, Shaw EC. Regression analyses of counts and rates: Poisson, overdispersed Poisson, and negative binomial models. Pyschol Bull 1995;118:392–404. [DOI] [PubMed] [Google Scholar]
- 24.Shumway M, Boccellari A, O’Brien K, Orkin RL. Cost-effectiveness of clinical case management for ED frequent users: results of a randomized trial. Am J Emerg Med 2008;26:155–64. [DOI] [PubMed] [Google Scholar]
- 25.Kne T, Young R, Spillane L. Frequent ED users: patterns of use over time. Am J Emerg Med 1998;16:648–52. [DOI] [PubMed] [Google Scholar]
- 26.Fuda KK, Immekus R. Frequent users of Massachusetts emergency departments: a statewide analysis. Ann Emerg Med 2006; 48:9–16. [DOI] [PubMed] [Google Scholar]
- 27.Lucas RH, Sanford SM. An analysis of frequent users of emergency care at an urban university hospital. Ann Emerg Med 1998;32: 563–8. [DOI] [PubMed] [Google Scholar]
- 28.Doupe MB, Palatnick W, Day S, et al. Frequent users of emergency departments: developing standard definitions and defining prominent risk factors. Ann Emerg Med 2012;60:24–32. [DOI] [PubMed] [Google Scholar]


