Abstract
OBJECTIVES:
Prior studies have reported mixed findings about the existence of racial disparities in readmission rates among Medicare Advantage beneficiaries, but these studies have used data from one state, focused on black-white disparities and have not focused on patients discharged to skilled nursing facilities (SNFs). The objective of the study was to characterize racial and ethnic disparities in rates of 30-day rehospitalization directly from SNF among fee-for-service and Medicare Advantage patients.
DESIGN:
A cross-sectional study of admissions to SNFs in 2015 was conducted.
SETTING:
Skilled Nursing Facilities across the US.
PARTICIPANTS:
The sample included 1,500,334 white, 213,848 African-American and 99,781 Hispanic Medicare patients who were admitted to 13,375 SNFs.
MEASUREMENTS:
The main outcome of interest was readmission, which was identified as patients sent back to any hospital directly from the SNF within 30 days of admission, as indicated on the Minimum Data Set discharge assessment.
RESULTS:
Overall readmission rates for fee-for-service patients were 16.7% (95% CI, 16.7% to 16.8%) for whites, 18.8% (95% CI, 18.7% to19.0%) for African-Americans, 17.4% (95% CI, 17.1% to 17.7%) for Hispanics. Readmission rates in Medicare Advantage were 14.7% (95% CI, 14.5% to 14.8%) for whites, 16.8% (95% CI, 16.6% to 17.1%) for African-Americans, and 15.3% (95% CI, 14.9% to 15.6%) for Hispanics. In addition, we also found that African-Americans had about 1% higher readmission rates than whites, even when they received care within the same SNF. There were no statistically significant differences in the magnitude of within-SNF racial disparities in Medicare Advantage compared to Medicare fee-for-service.
CONCLUSION:
We found racial disparities in readmission rates even within the same facility for both Medicare Advantage and fee-for-service beneficiaries. Intervention to reduce disparities in readmission rates, as well as more comprehensive quality measures that incorporate outcomes for Medicare Advantage enrollees are needed.
Keywords: Disparities in 30-Day Readmission Rates, Readmissions in skilled nursing facilities, Medicare Advantage, Disadvantaged populations in skilled nursing facilities, Disparities in readmissions among Medicare Advantage and fee-for-service patients
INTRODUCTION
About 20 percent of Medicare patients are discharged to skilled nursing facilities (SNFs) following a hospital stay.1 Readmissions from SNFs are common and costly; in 2010, one-quarter of SNF patients were readmitted to the hospital within 30 days of discharge, which cost Medicare over $4 billion. 2 In addition to the cost, readmissions to hospitals are also viewed as a measure of SNF quality.3 The Centers for Medicare and Medicaid (CMS) have focused efforts to reduce readmissions, including profiling SNF’s readmission rates, and including instituting financial penalties for SNFs with higher-than-expected readmission rates.4
Evidence has shown that overall rates of readmission have decreased over time; 5,6 however, racial disparities remain evident.7–10 One study by Li and colleagues11 found that, in 2008, rehospitalization rates were 14.3 percent for White patients, compared to 18.6 percent among African-American Medicare patients admitted to SNFs for post-acute care. The CMS measures readmission rates from fee-for-service patients exclusively and does not collect or report data on racial/ethnic variations. Yet, Medicare Advantage (MA) provides coverage to 17.6 million people (31% of Medicare beneficiaries), and it is the preferred choice of coverage for minority groups.12 Approximately 40% of MA beneficiaries have incomes of less than $20,000, and 45% of Hispanics and 29% of African-Americans enrolled in a MA plan in 2016.12
Prior studies have reported mixed findings about the existence of racial disparities in readmission rates among MA beneficiaries, but these studies have used data from one state, only focused on black-white disparities, and did not consider SNF specific effects. 13,14 Therefore, there is limited national evidence on racial/ethnic disparities among post-acute SNFs residents enrolled in fee-for-service and MA. Using a national dataset, we characterized racial and ethnic disparities in 30-day rehospitalization rates and the quality of admitted SNF among fee-for-service and MA patients admitted to SNFs. Based on literature on disparities in quality of SNF care and rehospitalization rates,11 we hypothesized that African-Americans and Hispanics admitted to SNFs would experience higher rates of rehospitalization, and racial/ethnic differences in readmission rates will be partially explained by within-facility disparities. We also hypothesized that disparities will be lower among MA patients.
STUDY DATA AND METHODS
Data and Population
We used the 2015 national Minimum Data Set 3.0 (MDS)15 merged to the Medicare Master Beneficiary Summary File (MBSF).16 In addition, we merged these files to the Long-Term Care: Facts on Care in the US (LTCFocus)17 and Nursing Home Compare (NHC) Five-Star Ratings database to obtain facility-level characteristics using the provider number.18 Finally, we obtained information regarding rurality from Census and merged it using SNF county number.19 The MDS provides patient level information on all nursing home admissions, including patients in MA. The MBSF contains: race/ethnicity, dual-eligibility and enrollment status. We used the Research Triangle Institute’s race/ethnicity variable with mutually exclusive categories: non-Hispanic white (hereafter, “white”), non-Hispanic African-American (hereafter, “African-American”), and Hispanic. 20 LTCFocus contains information regarding SNF characteristics, and NHC contained information about nursing home quality star ratings. The Census provided the percentage of the county population living in rural areas.
We applied previously published eligibility criteria used by the American Health Care Association (AHCA).21 We identified all fee-for-service and MA patients with first non-entry tracking MDS assessments who were admitted from an acute hospital to a SNF. We identified 1,851,078 patients from 15,412 SNFs. There were 15% of data with missing values regarding most AHCA domains and facility characteristics and we used multiple imputation to account for missing data. The variable with the highest fraction of missing was whether the patient was receiving cancer chemotherapy with 12%. We generated 5 replicates of complete datasets imputed for analysis. The imputation model included age, sex, race and ethnicity, cognitive impairment and the outcome variable. We completed the imputation step and the pooling step by using mi impute and mi estimate procedures in STATA 15.22
Our final analyses included patients in facilities with at least 30 admissions in the denominator. Hence, our final sample included 1,813,963 (1,500,334 White, 213, 848 African-American and 99,781 Hispanic) patients from 13,375 SNFs. Sensitivity analysis were performed with all facilities irrespective of sample size and with complete cases and the results remained stable (See Supplementary Material). The study protocol was approved by the Brown University’s Human Research Protections Office and the Centers for Medicare & Medicaid Services Privacy Board.
Measures
The outcome of interest was readmission directly from the SNF, which was identified as patients sent back to any hospital (excluding ER only visits) from the SNF within 30 days of admission, as indicated on the MDS discharge assessment.23
Independent variables
The primary independent variables were race/ethnicity and enrollment in Medicare fee-for-service or MA at admission.
Individual-level variables
Demographic covariates, based on the AHCA risk-adjusted model included:21 age <65, male sex, dual Medicaid eligibility status. Other covariates, grouped by domain, included: functional status: Total bowel incontinence, eating dependent, needs two-person assistance in activities of daily living (ADLs), cognitive impairment; prognosis: End stage prognosis poor, history of respiratory failure, receiving hospice care; clinical condition: Daily pain, pressure ulcer stage (4 variables), venous arterial ulcer, diabetic foot ulcer; diagnosis: Anemia, asthma, diabetes, history of heart failure, history of sepsis, history of viral hepatitis, history of internal bleeding; and services and treatments: Dialysis, insulin prescribed, ostomy care, cancer chemotherapy, receiving radiation therapy, continue to receive IV medication, continue to receive oxygen, continued tracheostomy care.
Facility-level variables
Variables at the facility level included percentage of residents whose primary support is Medicaid, for-profit tax status, whether the facility is part of a chain, the number of certified nursing assistant hours per resident day, licensed practical nurse per resident day, registered nurse per resident day, and percent rurality (the percentage of the county population living in rural areas of the county where the SNF was located).
In addition, we reported two other variables of interest including, quality and racial composition of the SNF. We measured quality using NHC five-star quality rating with values ranging from 1 star for lowest quality to 5 stars for the highest quality facilities.18 Racial composition of SNF was measured by calculating the percentage of white patients that were admitted to each SNF.
Analytical Approach
First, we compared the frequency of readmissions among racial and ethnic groups using chi-square tests. Then, we examined the readmission rates in order to determine how much of the racial and ethnic inequality in readmission rates is attributable to differences across SNFs versus within SNFs. Prior research examining overall and within-disparities have used this approach.24–26 Model 1 assessed readmission differences relative to whites using Ordinary Least Square (OLS) regression models. This model examined the overall difference in the risk of readmissions between African-Americans and Hispanics compared to Whites, controlling for individual-level risk factors. Model 2 included facility-level characteristics (for-profit status, staffing variables, %Medicaid, rurality). Model 3 was specified using SNF fixed-effects to account for the clustering of patients within facilities and estimate the mean within-SNF disparity for white and minority patients admitted to the same SNF. We included an interaction term in the models to test whether racial and ethnic disparities varied by MA status.
In addition, we ran OLS regression models to compare 30-day adjusted readmission rates by the decile of the proportion of white patients admitted to the SNF; and 30-day adjusted readmission rates and SNF star ratings stratified by enrollment status. We plotted the results of these two models. SAS 9.4 was used to construct analytic datasets and Stata 15 was used to conduct the analyses.
RESULTS
Table 1 summarizes descriptive and clinical characteristics of the sample by race and ethnic group and by MA enrollment. African-Americans and Hispanics were slightly younger and have higher proportions of males and dual eligibility for Medicaid compared to whites regardless of type of plan. However, MA patients have one to eleven percent fewer people that were dual eligible for Medicare/Medicaid. In addition, African-Americans and Hispanics had worse functional status and cognitive impairment, along with higher rates among fee-for-service patients. Finally, African-Americans and Hispanics were more likely to have anemia and diabetes. Similarly, fee-for-service patients had higher rates of these conditions (See Supplementary Table S1 for complete Table). In addition, African-Americans and Hispanics in both Medicare programs were admitted to a higher proportion of SNFs with for-profit status, with residents whose primary support is Medicaid, and lower registered nurse hours per resident day (See Supplementary Table S2).
Table 1.
Characteristics of patients admitted to skilled nursing facilities, by race and ethnic group and by Medicare fee-for-service and Medicare Advantage Enrollment Status (N=1,813,963).
| Fee-for-Service | Medicare Advantage | |||||
|---|---|---|---|---|---|---|
| Whites (1,085,349) |
African- Americans (144,253) |
Hispanics (61,531) |
Whites (414,985) |
African- Americans (69,595) |
Hispanics (38,250) |
|
| Numbers presented in percentages | ||||||
| Age < 65 | 8.01 | 20.0 | 15.2 | 7.01 | 15.1 | 10.4 |
| Male | 36.3 | 41.0 | 42.2 | 35.9 | 36.6 | 41.3 |
| Dual status | 30.4 | 60.5 | 68.6 | 29.0 | 56.4 | 57.6 |
| Total bowel incontinence | 48.4 | 62.6 | 58.0 | 46.5 | 58.4 | 53.7 |
| Eating dependent | 4.8 | 11.9 | 11.4 | 3.8 | 8.7 | 7.7 |
| Two-person assistance | 54.7 | 56.9 | 54.6 | 55.8 | 54.5 | 51.3 |
| Cognitive impairment | ||||||
| Intact | 49.8 | 42.0 | 38.6 | 50.6 | 44.4 | 43.3 |
| Mildly impaired | 18.3 | 17.9 | 18.4 | 17.1 | 17.2 | 17.7 |
| Moderately impaired | 29.4 | 36.6 | 39.1 | 30.5 | 35.7 | 36.6 |
| Severely impaired | 2.4 | 3.5 | 3.9 | 1.8 | 2.6 | 2.4 |
| Anemia | 28.6 | 37.2 | 33.3 | 28.1 | 34.4 | 30.1 |
| Diabetes | 31.2 | 47.8 | 50.1 | 32.7 | 48.0 | 49.9 |
| Dialysis | 2.0 | 9.7 | 7.5 | 1.6 | 5.9 | 4.4 |
| Insulin prescribed | 20.6 | 34.9 | 38.9 | 19.6 | 31.7 | 33.6 |
Notes: Differences across fee-for-service and Medicare Advantage groups significant at P< .001.
The frequency of readmissions was lower for whites as compared with African-Americans and Hispanics in both MA and fee-for-service patients (16.1% vs. 21.3% vs. 19.3% for fee-for-service; 14.9% vs. 18.8% vs. 16.6% for MA; P<.0001). However, MA patients had readmissions that were about one to three percentage points (p.p.) lower than their counterparts.
Readmission rates for fee-for-service patients were 16.7% (95% Confidence Interval [CI], 16.7% to 16.8%) for whites, 18.8% (95% CI, 18.7% to19.0%) for African-Americans, 17.4% (95% CI, 17.1% to 17.7%) for Hispanics vs. rates for MA were 14.7% (95% CI, 14.5% to 14.8%) for whites, 16.8% (95% CI, 16.6% to 17.1%) for African-Americans, and 15.3% (95% CI, 14.9% to 15.6%) for Hispanics. Accordingly, adjusted readmission rates were lower for whites by 2.1 percentage points than African-Americans (95% CI, 1.9 to 2.3) and 0.7 p.p. than Hispanics (95% CI, 0.4 to 1.0) among fee-for-service patients (See Figure 1). Similarly, among patients in MA the rates were lower for whites by 2.1 p.p. (95% CI, 1.8 to 2.4) than African-Americans and by 0.5 p.p. (95% CI, 0.2 to 0.9) than Hispanics. We found African-Americans had higher readmission rates overall (the difference persisted, although the magnitude was reduced, after including facility attributes [or state fixed effects; See Supplementary Table S3]), as well as within the same facility. For example, as shown in Table 2, among fee-for-service patients, the overall differences in readmission rates were 0.7 p.p. higher [95% CI, 0.4 to 0.9] for African-Americans than whites within the same facility. Similarly, there were 0.6 p.p. higher [95% CI, 0.3 to 0.9] for African-American beneficiaries when compared to White beneficiaries in the MA program. Among Hispanics, ethnicity was no longer a significant predictor of readmissions after including facility-level characteristics.
FIGURE 1. Patient level 30-day risk-adjusted readmission rates by racial and ethnic groups and by Medicare Advantage and fee-for-service.
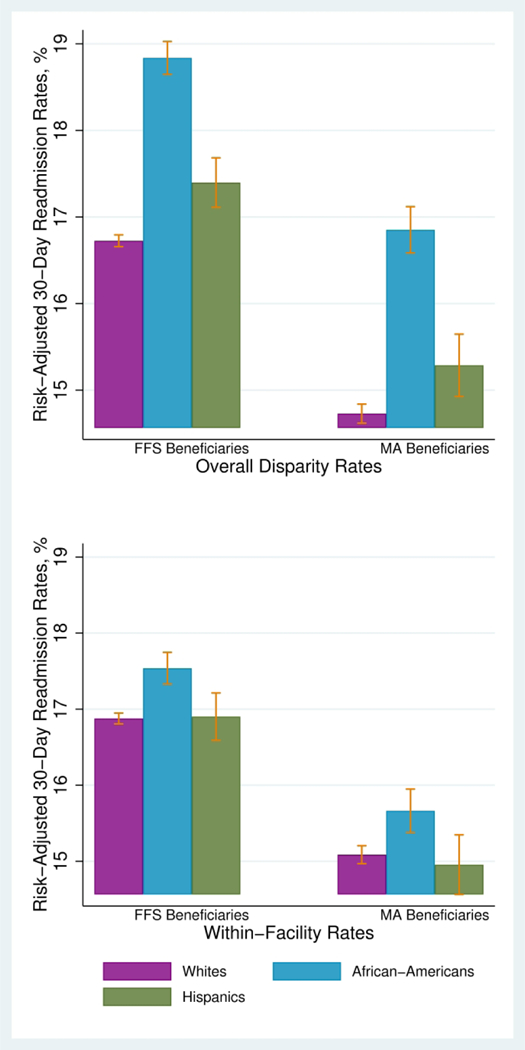
The top panel shows overall racial and ethnic disparities in readmission rates and the bottom panel shows within-facility readmission rates. Readmissions were measured directly from the Skilled Nursing Facility (SNF), which was identified as patients sent back to any hospital (excluding ER only visits) from the SNF within 30 days of admission, as indicated on the discharge assessment. The models adjusted for demographic covariates, based on the American Health Care Association risk-adjusted model included:18 age <65, male sex, dual Medicaid eligibility status; functional status: Total bowel incontinence, eating dependent, needs two-person assistance in activities of daily living (ADLs), cognitive impairment; prognosis: End stage prognosis poor, history of respiratory failure, receiving hospice care; clinical condition: Daily pain, pressure ulcer stage (4 variables), venous arterial ulcer, diabetic foot ulcer; diagnosis: Anemia, asthma, diabetes, history of heart failure, history of sepsis, history of viral hepatitis, history of internal bleeding; and services and treatments: Dialysis, insulin prescribed, ostomy care, cancer chemotherapy, receiving radiation therapy, continue to receive IV medication, continue to receive oxygen, continued tracheostomy care.
Table 2:
Overall, within-facility effects on 30-day readmission rates among post-acute care patients by Medicare Advantage status (N=1,813,963).
| Groups | Overall effects | +Facility characteristics |
+Within-facility effects |
|---|---|---|---|
| Medicare Fee-for-service | |||
| African-Americans vs. Whites | 2.1 [1.9 to 2.3] | 1.8 [1.6 to 2.0] | 0.7 [0.4 to 0.9] |
| Hispanics vs. Whites | 0.7 [0.4 to 1.0] | 0.3 [−0.02 to 0.6] | 0.02 [−0.3 to 0.3] |
| Medicare Advantage | |||
| African-Americans vs. Whites | 2.1[1.8 to 2.4] | 1.9 [1.6 to 2.2] | 0.6 [0.3 to 0.9] |
| Hispanics vs. Whites | 0.6 [0.2 to 0.9] | 0.2 [−0.02 to 0.5] | −0.1 [−0.5 to 0.3] |
Notes: Readmissions were measured directly from the skilled nursing facility (SNF), which was identified as patients sent back to any hospital (excluding ER only visits) from the SNF within 30 days of admission, as indicated on the discharge assessment. The models adjusted for demographic covariates, based on the American Health Care Association risk-adjusted model included:18 age <65, male sex, dual Medicaid eligibility status; functional status: Total bowel incontinence, eating dependent, needs two-person assistance in activities of daily living (ADLs), cognitive impairment; prognosis: End stage prognosis poor, history of respiratory failure, receiving hospice care; clinical condition: Daily pain, pressure ulcer stage (4 variables), venous arterial ulcer, diabetic foot ulcer; diagnosis: Anemia, asthma, diabetes, history of heart failure, history of sepsis, history of viral hepatitis, history of internal bleeding; and services and treatments: Dialysis, insulin prescribed, ostomy care, cancer chemotherapy, receiving radiation therapy, continue to receive IV medication, continue to receive oxygen, continued tracheostomy care. Disparities were not different between MA and FFs tested via interaction terms.
Figures 2 and 3 describe the relationship between the proportion of White patients and the quality measures in the SNF. We found that readmission rates for the three groups decreased as the quality of SNF increased (Figure 2). However, Whites had lower rates compared to Hispanics and African-Americans regardless of the SNF star rating. In addition, rates were about two p.p. lower for beneficiaries in the MA program across SNFs (P<.0001). For instance, for beneficiaries enrolled in fee-for-service that were admitted to SNFs with one-star rating, readmission rates for Whites were 17.2% (95% CI, 17.1% to 17.3) compared to 17.9% (95% CI, 17.6% to 18.2%) for Hispanics and 19.3% (95% CI, 19.1% to 19.5%) for African-Americans. Readmission rates for White MA beneficiaries who were admitted to SNFs with one-star rating were 15.8% (95% CI, 15.7% to 16.0%), and approximately 2.1 (95% CI, 1.8 to 2.4) p.p. higher for African-Americans and 0.6 (95% CI, 0.2 to 0.9) p.p. higher for Hispanics.
FIGURE 2. Patient level 30-day risk-adjusted readmission rates by racial and ethnic groups and by quality of chosen skilled nursing facility stratified by Medicare Advantage and fee-for-service beneficiaries.
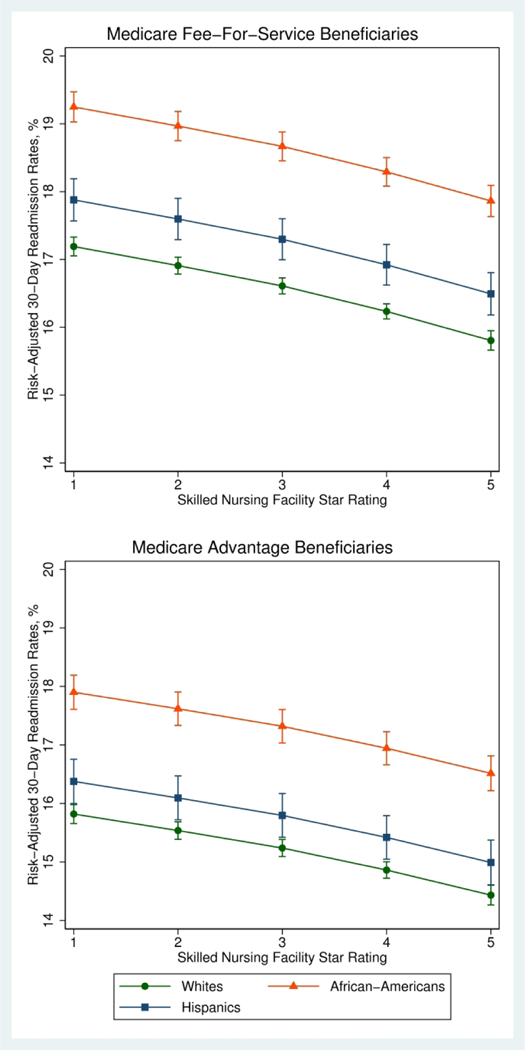
Readmissions were measured directly from the Skilled nursing facility (SNF), which was identified as patients sent back to any hospital (excluding ER only visits) from the SNF within 30 days of admission, as indicated on the discharge assessment. The models adjusted for demographic covariates, based on the American Health Care Association risk-adjusted model included:18 age <65, male sex, dual Medicaid eligibility status; functional status: Total bowel incontinence, eating dependent, needs two-person assistance in activities of daily living (ADLs), cognitive impairment; prognosis: End stage prognosis poor, history of respiratory failure, receiving hospice care; clinical condition: Daily pain, pressure ulcer stage (4 variables), venous arterial ulcer, diabetic foot ulcer; diagnosis: Anemia, asthma, diabetes, history of heart failure, history of sepsis, history of viral hepatitis, history of internal bleeding; and services and treatments: Dialysis, insulin prescribed, ostomy care, cancer chemotherapy, receiving radiation therapy, continue to receive IV medication, continue to receive oxygen, continued tracheostomy care. The SNF’s Medicare five-star quality rating is a composite measure summarizing skilled nursing facilities’ staffing, quality measures, and health inspections related information with values ranging from 1 star for lowest quality to 5 stars for the highest quality facilities.
FIGURE 3. Patient level 30-day risk-adjusted readmission rates by racial and ethnic group and by the decile of the percent of White patients in the chosen skilled nursing facility stratified by Medicare Advantage and fee-for-service beneficiaries.
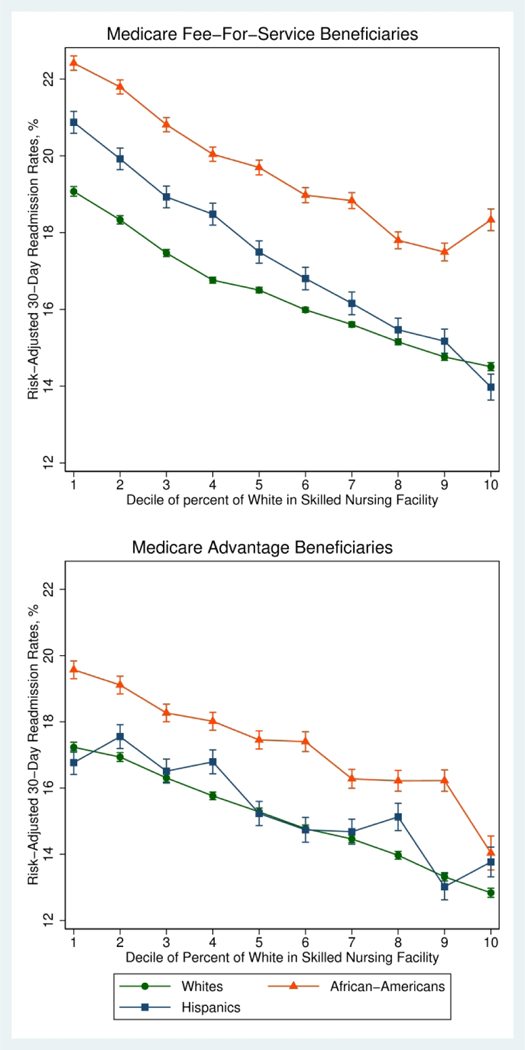
Readmissions were measured directly from the skilled nursing facility (SNF), which was identified as patients sent back to any hospital (excluding ER only visits) from the SNF within 30 days of admission, as indicated on the discharge assessment. The models adjusted for demographic covariates, based on the American Health Care Association risk-adjusted model included:18 age <65, male sex, dual Medicaid eligibility status; functional status: Total bowel incontinence, eating dependent, needs two-person assistance in activities of daily living (ADLs), cognitive impairment; prognosis: End stage prognosis poor, history of respiratory failure, receiving hospice care; clinical condition: Daily pain, pressure ulcer stage (4 variables), venous arterial ulcer, diabetic foot ulcer; diagnosis: Anemia, asthma, diabetes, history of heart failure, history of sepsis, history of viral hepatitis, history of internal bleeding; and services and treatments: Dialysis, insulin prescribed, ostomy care, cancer chemotherapy, receiving radiation therapy, continue to receive IV medication, continue to receive oxygen, continued tracheostomy care.
Rates were slightly lower for MA beneficiaries when compared to fee-for-service beneficiaries regardless of the racial compassion of the SNF (See Figure 3; P<.0001), but readmission rates for Whites and Hispanics in the MA program was somewhat similar as compared to those beneficiaries in the fee-for-service program. For fee-for-service beneficiaries admitted to SNFs in the first decile of percent of white patients, readmission rates were 19.1% (95% CI, 19.0 to 19.2) for whites, 20.9% (95% CI, 20.6 to 21.2) for Hispanics and 22.4% (95% CI, 22.2 to 22.6) for African-Americans. Whereas for MA beneficiaries admitted to the same facilities, readmission rates were 17.2% (95% CI, 17.1% to 17.4%) for Whites, 16.8% (95% CI, 16.4% to 17.1%) for Hispanics 19.6% (95% CI, 19.3% to 19.8%) for African-Americans.
DISCUSSION
In this national study of racial and ethnic differences in 30-day readmission rates among MA and fee-for-service patients following admission to SNFs, we found statistically significant racial and ethnic differences of about 2 percentage points higher rates for African-Americans, and less than one percentage point for Hispanics. MA patients had about 2 percentage points lower readmission rates compared to fee-for-service patients. However, the magnitude of racial/ethnic disparity in readmission rates was not different in MA compared to fee-for-service. In addition, we found that readmission rates for the three groups decreased as the fraction of White patients in the facility increased.
Our findings extend previous studies by showing that racial and ethnics disparities in readmission rates among Medicare SNF patients are partially due to within-facility disparity, meaning that African-Americans in the same SNF are more likely than whites to be readmitted to the hospital than whites. Prior studies have found differences in 30-day readmission rates among Medicare beneficiaries.8,10 Li et al.27 found that among Medicare post-acute SNF patients, African-Americans had higher rates of rehospitalizations than whites, as well as 40% higher risk of being hospitalized within 30 days of admission.11 Observed racial differences in these studies have been partially attributable to SNFs with higher concentrations of African-American residents. Similarly, Rivera-Hernandez and colleagues found that SNFs that served higher proportion of African-Americans had higher readmission rates.28 We extended this work to explore racial and ethnic differences in 30-day readmission rates among Medicare fee-for-service and MA post-acute SNF patients and the role of race and ethnicity driving these disparities. The findings of our study reinforce the results of others, demonstrating that racial disparities persisted within subgroups of patients in the same SNFs.11,29 Contrary to the results of other studies that have found that MA has been successful at reducing racial disparities13 or the studies that have found greater disparities in readmission rates among MA patients compared to those in fee-for-service,14 we found similar racial differences in adjusted readmission rates for MA and fee-for-service enrollees. In addition, our study contrasts with the findings of Rodriguez and colleagues30 who found that Hispanic Medicare patients had substantially higher readmission rates within 30 days after being discharged for heart failure and acute myocardial infarction as compared to white patients.
Our findings may have differed from those of previous studies for three reasons. First, prior studies30 have compared condition-specific readmission rates whereas we used all-cause readmission rates. Second, studies have limited their data to inpatient claims, which often excludes MA patients.8,10,27 Our study is focused on patients who receive post-acute care at SNFs and uses the MDS to capture patients that were discharged to the hospital. Third, our analysis included demographic and clinical variables from a well-validated model applied by AHCA.21 Finally, other studies have limited their analysis to specific region(s),13,14 whereas we included national data and focus on fee-for-service and MA patients.
Our findings have important policy implications. Our study highlights that racial and ethnic differences in readmission rates are partially due to within-SNF disparity. For African-Americans, within-facility effects appeared to be ~30% of the overall effects. In terms of readmissions among Hispanics, we found no within-facility disparities. Our study suggests that racial and ethnic disparities in readmission rates is partially due to a cross-facility differences. Patients from facilities with higher concentration of Whites have lower readmission rates. Our findings suggest that these facilities may provide overall better quality, as reflected by higher star ratings and better staffing. As it has been suggested by prior literature,28,31 it is important to address issues influencing the quality of care of SNFs that serve predominantly minority populations.
Decreasing the rate of hospitalizations from nursing home facilities continues to be an important area of emphasis for CMS and other policy makers. The recently implemented Skilled Nursing Facility Value-Based Purchasing Program (SNF VBP) includes financial penalties for SNFs with high readmission rates, as measured by the risk-standardized 30-day rate of unplanned readmissions within 30 days among fee-for-service enrollees. 4 Our findings suggest that SNFs that provide care to minority patients may be subjected to higher penalties. Our results also suggest the need to track outcomes for MA patients and importance of measuring and reporting hospital readmissions from post-acute patients for both MA and fee-for-service rather than just those patients covered by fee-for-service. This is particularly important in monitoring quality and disparities for minority patients, since African-Americans and Hispanics are more likely to be enrolled in MA.
Successful efforts to reduce rehospitalizations in SNF settings often require improving care coordination and care planning.32 Racial and ethnic differences have been noted in provider and patient communication, as well as higher utilization of aggressive end-of-life treatment among minority patients.33 For instance, African-Americans and Hispanics in particular are less likely to document advanced care plans.34–36 Racial disparities regarding advance health care planning has also been found in the Medicare population.37 Studies have shown lower 30-day readmission rates among post-acute care patients who received a palliative care consultation.38,39 The potential mediators of within-facility racial and ethnic disparities in rehospitalization, including patient preferences or provider attitudes,40,41 deserve further investigation.
Our study has some limitations. Although we used MDS resident assessment records and adjusted for clinical and demographic characteristics, we did not include risk factors or other variables related to caregiver, family support or patient preferences regarding end-of-life care40 that may be associated with rehospitalization. In addition, our study did not include information regarding discharged hospitals or other geographic factors such as provider norms,2 practice patterns that may influence hospital readmissions among post-acute care patients. However, we used a well-recognized risk-adjusted model from AHCA. We further adjusted for SNFs characteristics and compared quality and racial composition of SNF with readmission rates. Future studies should explore the potential impact of these or other factors in racial differences in skilled nursing facility readmissions. Second, our study has missing data. However, sensitivity analyses irrespective of size and data completeness show similar patterns regarding racial disparities (See Supplementary Tables S4 and S5). Third, our findings may not generalize to specific clinical conditions, and our data do not allow stratification according to medical vs. surgical patients. 13,14 Studies have found poor agreement between condition-specific and all-cause readmission measures.42 Yet, the SNF Readmission Measure from CMS is also an all-cause risk-standardized readmission measure.43 To this extent, our study aligns with CMS goals to target a larger proportion of readmissions and provide comprehensive information about quality of care.43 Of note, a strength of this study is that we included MA patients, which the CMS SNF readmission measure excludes.
CONCLUSION
Overall, among a national cohort of African-Americans, Hispanics and White patients admitted to skilled nursing facilities post-acute care, we found disparities in readmission rates even within the same facility. Intervention to reduce disparities in readmission rates, as well as more comprehensive quality measures that incorporate outcomes for MA enrollees are needed.
Supplementary Material
Acknowledgments
Funding/Support: Research reported in this publication was supported by the National Institute on Aging of the National Institutes of Health under award numbers P01AG027296–07S1 and by Institutional Development Award Number U54GM115677 from the National Institute of General Medical Sciences of the National Institutes of Health, which funds Advance Clinical and Translational Research (Advance-CTR).
Footnotes
Conflict of Interest:
Dr. Amal Trivedi receives consulting fees to edit the Merck Manual. No other disclosures are reported. Dr. Vincent Mor has three Significant Financial Interests (SFIs) that are broadly related to his area of research. His research area addresses policy issues related to the quality of nursing home care. It is conceivable that results from my research could affect the entire nursing home/post-acute care industry, including companies with which I work and/or in which I have financial interests.
He is the Chair of the Independent Quality Committee at HCR ManorCare and is compensated for this service. HCR is a provider of short-term, post-hospital services, and long-term care. The company has a network of more than 500 nursing and rehabilitation centers, assisted living facilities, outpatient rehabilitation clinics, and hospice and home health care agencies.
He is a paid consultant to NaviHealth, Inc. and chair their Scientific Advisory Board. NaviHealth is wholly owned by Cardinal Health. The company offers post-acute care (PAC) management and services to more than 1.5 million beneficiaries in all regions of the country through its partnerships with health plans and health systems
He is former Director at PointRight, Inc. While he no longer provides any services or holds any positions at PointRight, He holds less than 1%equity. PointRight is a private company based in Cambridge, MA. It provides predictive analytics solutions to thousands of post-acute providers, long-term care providers, hospitals, payers and insurance organizations.
Contributor Information
Maricruz Rivera-Hernandez, Department of Health Services, Policy & Practice, Brown University School of Public Health, Providence, Rhode Island; Center for Gerontology & Healthcare Research, Brown University School of Public Health, Providence, Rhode Island.
Momotazur Rahman, Department of Health Services, Policy & Practice, Brown University School of Public Health, Providence, Rhode Island; Center for Gerontology & Healthcare Research, Brown University School of Public Health, Providence, Rhode Island.
Vincent Mor, Department of Health Services, Policy & Practice, Brown University School of Public Health, Providence, Rhode Island; Center for Gerontology & Healthcare Research, Brown University School of Public Health, Providence, Rhode Island; Providence VA Medical Center, Providence, Rhode Island.
Amal N. Trivedi, Department of Health Services, Policy & Practice, Brown University School of Public Health, Providence, Rhode Island; Center for Gerontology & Healthcare Research, Brown University School of Public Health, Providence, Rhode Island; Providence VA Medical Center, Providence, Rhode Island.
REFERENCES
- 1.The Medicare Payment Advisory Commission. Encouraging Medicare beneficiaries to use higher quality post-acute care providers [Internet]. MEDPAC; 2018. Available from: http://www.medpac.gov/docs/default-source/reports/jun18_ch5_medpacreport_sec.pdf?sfvrsn=0 [Google Scholar]
- 2.Mor V, Intrator O, Feng Z, Grabowski DC. The revolving door of rehospitalization from skilled nursing facilities. Health Aff Proj Hope. 2010. February;29(1):57–64. PMCID: PMC2826971 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.The Medicare Payment Advisory Commission. Skilled nursing facility services: Assessing payment adequacy and updating payments [Internet]. 2018. Available from: http://www.medpac.gov/docs/default-source/reports/mar18_medpac_ch8_sec.pdf?sfvrsn=0
- 4.Centers for Medicare & Medicaid Services. The Skilled Nursing Facility Value-Based Purchasing Program (SNF VBP) [Internet]. 2018. [cited 2018 Aug 8]. Available from: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Value-Based-Programs/Other-VBPs/SNF-VBP.html
- 5.Wasfy JH, Zigler CM, Choirat C, Wang Y, Dominici F, Yeh RW. Readmission Rates After Passage of the Hospital Readmissions Reduction Program. Ann Intern Med. 2017. March 7;166(5):324–331. PMCID: PMC5507076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Medicare Payment Advisory Commission. The Hospital Readmissions Reduction Program has succeeded for beneficiaries and the Medicare program [Internet]. 2018. [cited 2018 Aug 8]. Available from: http://www.medpac.gov/-blog-/the-hospital-readmissions-reduction-program-(hrrp)-has-succeeded-for-beneficiaries-and-the-medicare-program/2018/06/15/the-hospital-readmissions-reduction-program-has-succeeded-for-beneficiaries-and-the-medicare-program
- 7.Kroch E, Duan M, Martin J, Bankowitz RA. Patient Factors Predictive of Hospital Readmissions Within 30 Days. J Healthc Qual Off Publ Natl Assoc Healthc Qual. 2016. April;38(2):106–115. PMID: [DOI] [PubMed] [Google Scholar]
- 8.Joynt KE, Orav EJ, Jha AK. Patient race, site of care, and 30-day readmission rates among elderly Americans. Jama. 2011. February 16;305(7):675–681. PMCID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Basu J, Hanchate A, Bierman A. Racial/Ethnic Disparities in Readmissions in US Hospitals: The Role of Insurance Coverage. Inq J Med Care Organ Provis Financ [Internet]. 2018. May 7 [cited 2018 Aug 8];55 Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5946640/PMCID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tsai TC, Orav EJ, Joynt KE. Disparities in Surgical 30-Day Readmission Rates for Medicare Beneficiaries by Race and Site of Care. Ann Surg. 2014. June;259(6):1086–1090. PMCID: PMC4107654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Li Y, Glance LG, Yin J, Mukamel DB. Racial disparities in rehospitalization among Medicare patients in skilled nursing facilities. Am J Public Health. 2011. May;101(5):875–882. PMCID: PMC3076407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jacobson G, Gold M, Damico A, Casillas G. Medicare Advantage 2016 Data Spotlight: Overview of Plan Changes-Plan Offerings in 2016 [Internet]. 2015. [cited 2016 Oct 27]. Available from: http://kff.org/report-section/medicare-advantage-2016-data-spotlight-overview-of-plan-changes-plan-offerings-in-2016/
- 13.Li Y, Cen X, Cai X, Wang D, Thirukumaran CP, Glance LG. Does Medicare Advantage Reduce Racial Disparity in 30-Day Rehospitalization for Medicare Beneficiaries? Med Care Res Rev MCRR. 2016. December 6; PMID: [DOI] [PubMed] [Google Scholar]
- 14.Li Y, Cen X, Cai X, Thirukumaran CP, Zhou J, Glance LG. Medicare Advantage Associated With More Racial Disparity Than Traditional Medicare For Hospital Readmissions. Health Aff (Millwood). 2017. July 1;36(7):1328–1335. [DOI] [PubMed] [Google Scholar]
- 15.Centers for Medicare and Medicaid Services. MDS 3.0 Quality Measures: USER’S MANUAL [Internet]. 2017. p. 100 Available from: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/NursingHomeQualityInits/Downloads/MDS-30-QM-Users-Manual-V11-Final.pdf
- 16.Research Data Assistance Center. Master Beneficiary Summary File [Internet]. 2017. [cited 2017 Sep 19]. Available from: https://www.resdac.org/cms-data/files/mbsf
- 17.LTC focus. Long-Term Care: Facts on Care in the US [Internet]. 2017. [cited 2017 Jun 28]. Available from: http://ltcfocus.org/
- 18.Centers for Medicare & Medicaid Services. Design for Nursing Home Compare Five-Star Quality Rating System: Technical Users’ Guide [Internet]. 2017. Available from: https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/CertificationandComplianc/Downloads/usersguide.pdf
- 19.US Census Bureau Geography. Urban and Rural [Internet]. 2018. [cited 2019 Mar 15]. Available from: https://www.census.gov/geo/reference/urban-rural.html
- 20.Eicheldinger C, Bonito A. More accurate racial and ethnic codes for Medicare administrative data. Health Care Financ Rev. 2008;29(3):27–42. PMCID: PMC4195038 [PMC free article] [PubMed] [Google Scholar]
- 21.American Health Care Association. 30-Day Risk-Adjusted SNF Rehospitalization Measure [Internet]. 2017. Available from: https://www.ahcancal.org/research_data/trendtracker/Documents/Rehospitalization%20Help%20Doc.pdf
- 22.StataCorp. STATA 15. College Station, TX: StataCorp LLC; 2017. [Google Scholar]
- 23.Rahman M, Tyler D, Acquah JK, Lima J, Mor V. Sensitivity and Specificity of the Minimum Data Set 3.0 Discharge Data Relative to Medicare Claims. J Am Med Dir Assoc. 2014. November;15(11):819–824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cai S, Feng Z, Fennell ML, Mor V. Despite Small Improvement, Black Nursing Home Residents Remain Less Likely Than Whites To Receive Flu Vaccine. Health Aff (Millwood). 2011. October 1;30(10):1939–1946. PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rodriguez HP, von Glahn T, Grembowski DE, Rogers WH, Safran DG. Physician effects on racial and ethnic disparities in patients’ experiences of primary care. J Gen Intern Med. 2008. October;23(10):1666–1672. PMCID: PMC2533359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Weech-Maldonado R, Elliott MN, Morales LS, Spritzer K, Marshall GN, Hays RD. Health Plan Effects on Patient Assessments of Medicaid Managed Care Among Racial/Ethnic Minorities. J Gen Intern Med. 2004. February;19(2):136–145. PMCID: PMC1492141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Li Y, Cai X, Glance LG. Disparities in 30-day rehospitalization rates among Medicare skilled nursing facility residents by race and site of care. Med Care. 2015. December;53(12):1058–1065. PMCID: PMC4648673 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rivera-Hernandez M, Rahman M, Mukamel DB, Mor V, Trivedi AN. Quality of Post-Acute Care in Skilled Nursing Facilities That Disproportionately Serve Black and Hispanic Patients. J Gerontol A Biol Sci Med Sci. 2018. April 25; PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hefele JG, Ritter GA, Bishop CE, Acevedo A, Ramos C, Nsiah-Jefferson LA, Katz G. Examining Racial and Ethnic Differences in Nursing Home Quality. Jt Comm J Qual Patient Saf. 2017. November;43(11):554–564. PMID: [DOI] [PubMed] [Google Scholar]
- 30.Rodriguez F, Joynt KE, López L, Saldaña F, Jha AK. Readmission rates for Hispanic Medicare beneficiaries with heart failure and acute myocardial infarction. Am Heart J. 2011. August 1;162(2):254–261.e3. [DOI] [PubMed] [Google Scholar]
- 31.Zheng NT, Mukamel DB, Caprio T, Cai S, Temkin-Greener H. Racial Disparities in In-Hospital Death and Hospice Use Among Nursing Home Residents at the End-of-life. Med Care. 2011. November;49(11):992–998. PMCID: PMC3215761 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Agency for Healthcare Research and Quality. THE ISSUE: EFFECTIVE COMMUNICATION AND CARE COORDINATIO [Internet]. 2016. Available from: https://www.ahrq.gov/sites/default/files/wysiwyg/workingforquality/nqs-priority-focus-carecoordination.pdf
- 33.Hanchate A, Kronman AC, Young-Xu Y, Ash AS, Emanuel E. Racial and Ethnic Differences in End-of-Life Costs: Why Do Minorities Cost More Than Whites? Arch Intern Med. 2009. March 9;169(5):493–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.LoPresti MA, Dement F, Gold HT. End-of-Life Care for People With Cancer From Ethnic Minority Groups: A Systematic Review. Am J Hosp Palliat Med. 2016. April 1;33(3):291–305. [DOI] [PubMed] [Google Scholar]
- 35.Degenholtz HB, Arnold RA, Meisel A, Lave JR. Persistence of racial disparities in advance care plan documents among nursing home residents. J Am Geriatr Soc. 2002. February;50(2):378–381. PMID: [DOI] [PubMed] [Google Scholar]
- 36.Smith AK, McCarthy EP, Paulk E, Balboni TA, Maciejewski PK, Block SD, Prigerson HG. Racial and Ethnic Differences in Advance Care Planning Among Patients With Cancer: Impact of Terminal Illness Acknowledgment, Religiousness, and Treatment Preferences. J Clin Oncol. 2008. September 1;26(25):4131–4137. PMCID: PMC2654372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Musich S, Wang SS, Hawkins K, Yeh CS. Disparities Among Those With Advance Directives in a Medicare Supplement Population. Am J Hosp Palliat Care. 2016. June;33(5):463–470. PMID: [DOI] [PubMed] [Google Scholar]
- 38.Enguidanos S, Vesper E, Lorenz K. 30-day readmissions among seriously ill older adults. J Palliat Med. 2012. December;15(12):1356–1361. PMID: [DOI] [PubMed] [Google Scholar]
- 39.O’Connor NR, Moyer ME, Behta M, Casarett DJ. The Impact of Inpatient Palliative Care Consultations on 30-Day Hospital Readmissions. J Palliat Med. 2015. November;18(11):956–961. PMID: [DOI] [PubMed] [Google Scholar]
- 40.Grabowski DC, Stewart KA, Broderick SM, Coots LA. Predictors of Nursing Home Hospitalization: A Review of the Literature. Med Care Res Rev. 2008. February 1;65(1):3–39. [DOI] [PubMed] [Google Scholar]
- 41.Ashton CM, Haidet P, Paterniti DA, Collins TC, Gordon HS, O’Malley K, Petersen LA, Sharf BF, Suarez-Almazor ME, Wray NP, Street RL. Racial and Ethnic Disparities in the Use of Health Services. J Gen Intern Med. 2003. February;18(2):146–152. PMCID: PMC1494820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rosen AK, Chen Q, Shwartz M, Pilver C, Mull HJ, Itani KFM, Borzecki A. Does Use of a Hospital-wide Readmission Measure Versus Condition-specific Readmission Measures Make a Difference for Hospital Profiling and Payment Penalties? Med Care. 2016. February;54(2):155–161. PMID: [DOI] [PubMed] [Google Scholar]
- 43.Smith L, West S, Coots L, Ingber M, Reilly K, Feng Z, Tan S, Bender R, Chiri G, Barch D, Manning J, Etlinger A. Skilled Nursing Facility Readmission Measure (SNFRM) NQF #2510: All-Cause Risk-Standardized Readmission Measure [Internet]. RTI International; 2015. Available from: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/NursingHomeQualityInits/Downloads/SNFRM-Technical-Report-3252015.pdf [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


