Abstract
Aim of the study
Augmented reality (AR) has the potential to offer a novel approach to CPR training that supplements conventional training methods with gamification and a more interactive learning experience. This is done through computer-generated imagery superimposed on users’ view of the real environment to simulate interactive training scenarios. We sought to test the feasibility of an AR CPR training system (CPReality) for health care providers (HCPs).
Methods
In this feasibility trial, a CPR training manikin was integrated with a commercial AR device (Microsoft HoloLens) to provide participants with real-time audio-visual feedback via a holographic overlay of blood flow to vital organs dependent on CC quality. In this system, higher quality CC visually improved virtual blood circulation. HCPs performed a 2-minute cycle of hands-only CPR using only the AR system, and CC parameters were recorded. Descriptive data on participants’ demographics, CC quality, and satisfaction with the training environment were reported using quantitative and qualitative analysis.
Results
Between 10/2018–11/2018, we enrolled a convenience sample of 51 HCPs. The median age of participants was 31 years (IQR 27–41), 71% (36/51) were female, and 67% (34/51) were registered nurses. CC rates (mean 126 ± 12.9 cpm), depths (median 53 mm, IQR 46–58), and percent with complete recoil (median 80%, IQR 12–100) were consistent with guideline recommendations for good quality CPR. Participants were predominantly satisfied with the system, with 82% perceiving the experience as realistic, 98% recognizing the visualizations as helpful for training, and 94% willing to use the application in future CPR training.
Conclusions
As AR is increasingly applied in the healthcare setting, integration in CPR training offers a novel and promising educational approach. In this convenience sample of trained HCPs, high quality CC delivery was feasible using the AR CPR training system which was received favorably by most participants.
Keywords: Computer science, Cardiology, Emergency medicine, Health profession, Augmented reality, Cardiac arrest, Cardiopulmonary resuscitation, Simulation
1. Introduction
Efforts directed towards improving in-hospital resuscitation performance, such as early cardiopulmonary resuscitation (CPR) and standardized post-resuscitation care, have been modestly successful, raising in-hospital cardiac arrest (IHCA) survival rates to an estimated 25% in 2017 [1]. Despite clear guidelines for high quality CPR [2, 3], one explanation for the marginal improvement may be health care provider's (HCP) poor adherence to evidence-based CPR performance in clinical practice, in addition to skill decay after initial training [4, 5, 6, 7, 8]. This calls into question the effectiveness of the current CPR certification paradigm, and underpins the importance of innovations in CPR teaching. Numerous investigators have attempted to address this missed opportunity by exploring different educational approaches such as the use of CPR-sensing and feedback devices [9, 10], team debriefing programs [11, 12], high fidelity simulation trainings [13], and refresher training programs [14, 15, 16]; solutions that have had mixed institutional responses and buy-in.
A recent 2018 statement by the American Heart Association (AHA) highlighted the role of immersive technologies and gamified learning in advancing educational strategies in resuscitation by enhancing users' learning experience [17]. Wearable devices, that utilize augmented and virtual reality technology, have already shown promise as a useful training tool in many healthcare training studies with various applications in nasogastric tube placement [18], echocardiography [19], central line placement [20, 21], surgery [22, 23], and pathology [24]. This novel technology allows for high-fidelity simulation and experiential learning by means of holographic visualizations superimposed on what a user sees in the real world. The user's heightened perception of a more realistic scenario potentiates the learning experience, while allowing the user to practice in interactive high-risk situations. The objective of our study was to test the feasibility of an augmented reality (AR) platform for CPR training as a proof-of-concept that overlays an interactive holographic circulatory system next to the physical training manikin during CPR (Fig. 1). We tested the validity of this training system against CPR guidelines and evaluated participants' perception of this educational tool.
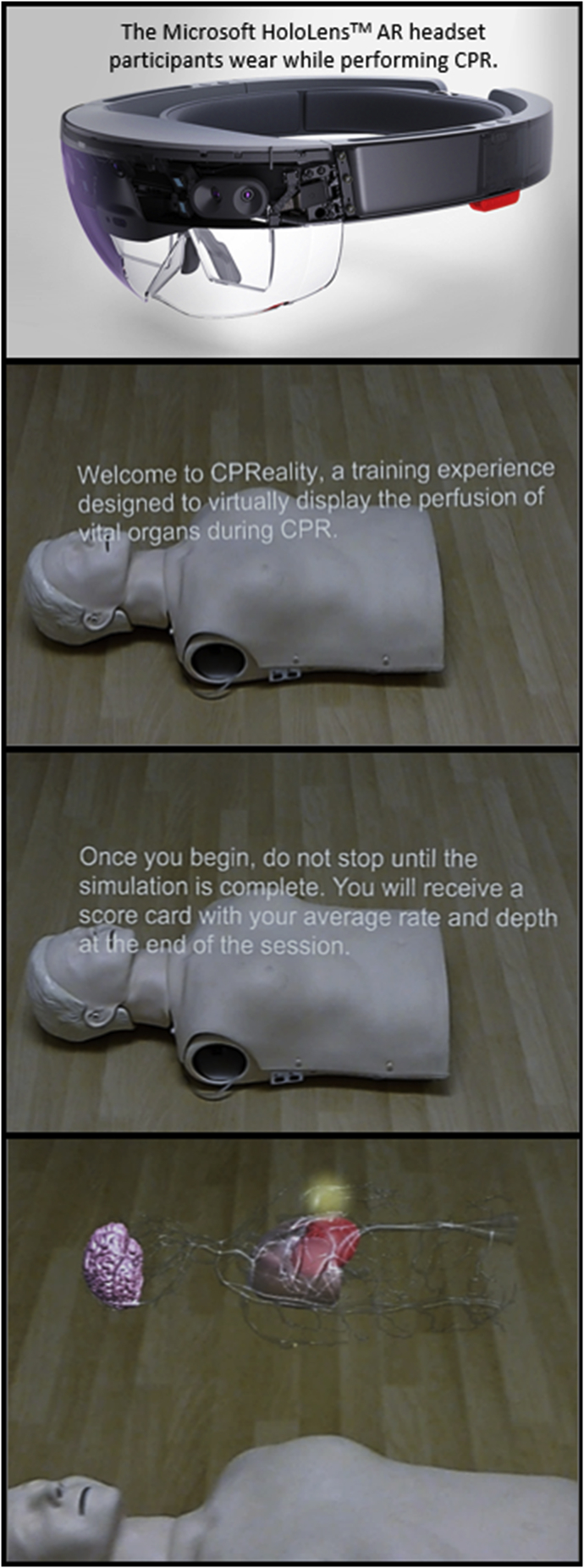
Fig. 1.
The CPReality AR CPR training application: Microsoft HoloLens device integrated with a Laerdal CPR feedback manikin displaying the holographic circulatory system.
2. Methods
2.1. Study design and participants
This was a feasibility study of a novel CPR training tool. Between October and November 2018, we enrolled a convenience sample of HCPs from different specialties and hospitals within one health system, presenting for mandatory Basic Life Support (BLS) and/or Advanced Cardiovascular Life Support (ACLS) recertification training to the health system simulation center. Research staff approached potential participants and asked if they would participate in a short 15-minute AR CPR study prior to the start of their scheduled training session. Enrollment into the study did not impact subsequent BLS or ACLS training and recertification processes.
2.2. Augmented reality system
The AR CPR training application (CPReality) was developed as part of a University of Pennsylvania technology competition in 2017 to create an immersive multi-sensory (audio, visual, tactile) CPR teaching tool. As seen in Fig. 1, it consists of a CPR recording manikin (Laerdal Medical, Wappinger Falls, NY) integrated with a head-mounted commercial AR device (Microsoft Hololens, Microsoft, Redmond WA). As hands-only CPR is performed on the manikin, the system renders recorded quantitative chest compression (CC) data (CC rate, depth, recoil) into an AR holographic image of the circulatory system in front of the study participant. As a form of visual feedback, blood flow to vital organs either increases or decreases based on the actual quality of CC being performed by the subject. If the subject performed CC at a rate outside of the guideline range (100–120 cpm), auditory feedback from the Hololens device, in the form of a heartbeat at 110 bpm, was audible to the subject as a guide. At the end of the CPR cycle, the application also provides participants with a CPR quality score calculated using sensor data and an industry-standard algorithm.
2.3. Study protocol
This protocol was reviewed by the Institutional Review Board at the University of Pennsylvania and granted exemption. Data collection and analysis were compliant with the Health Insurance Portability and Accountability Act of 1996 (HIPAA) regulations. Verbal consent was obtained from HCPs prior to the training session by clinical research coordinators.
Upon verbal consent, data collection was performed in three stages: (1) pre-CPR demographics survey, (2) AR CPR training, (3) post-CPR satisfaction survey. The first survey collected demographic and baseline HCP training information including age, gender, race, healthcare position, number of attended resuscitations per month, and years in training. This was followed by a brief orientation to the Hololens device. As the purpose of the study was feasibility testing of the system for CCs without ventilations, participants then performed a single 2-minute hands-only CPR cycle using the CPReality AR system. Finally, a post-survey was administered to assess participants’ satisfaction with the overall experience and perception of AR technology use in future CPR training applications. The satisfaction survey questions were answered on a four-point Likert scale including the following selections: “strongly agree”, “agree”, “disagree”, and “strongly disagree”. Participants were concurrently asked to provide qualitative feedback about the CPReality system in addition to improvement suggestions.
2.4. Data collection
Over a 2-minute cycle, three CC measurements were recorded: mean CC rate in compressions per minute (cpm), mean CC depth in millimeters (mm), and percent of CCs with complete chest recoil (%). CPR quality was analyzed based on the standard AHA guidelines of a CC rate of 100–120 cpm, a depth between 50 and 60 mm, and maximizing full chest recoil [2, 3]. Unidentified data from pre- and post-CPR surveys, initially collected on paper forms, were entered into a REDCap database, an institutionally approved and password protected web application.
2.5. Data analysis
Descriptive statistics were used to summarize participant characteristics, CC parameters, and participant satisfaction survey results. As this was a pilot study on a small HCP population, data was not anticipated to be normally distributed. The Shapiro-Wilk test was however used when applicable, and when the normality assumption was violated, continuous variables were reported as medians with IQR (Q1-Q3) instead of means ±SD. Categorical variables were presented as frequencies and percentages.
Comparative analysis of continuous CPR quality data between HCPs with BLS versus ACLS certification was conducted using the independent samples t-test and Mann-Whitney U tests for parametric and non-parametric data respectively. All statistical tests were 2-sided, and a P-value of <0.05 was statistically significant.
To assess participants’ positive and negative observations of the system, qualitative inductive content analysis was performed on free-text responses to open-ended questions [25]. After identification of prevalent topics in responses, related topics were clustered around central ideas using open coding. Higher order categories and headings were generated according to the thematic relationship between codes. Finally, the number of instances of codes falling under different categories were counted to assess the prevalence of raised comments, with certain individual comments addressing more than a single category. Data were managed and analyzed using standard statistical software (IBM SPSS Statistics for Windows, Version 23, Armonk, NY).
3. Results
3.1. Participant demographics
During our enrollment time period, 51 HCPs were enrolled at a centralized simulation and training center, which is part of a multihospital academic health system. Baseline characteristics of participants are presented in Table 1. The median age of participants was 31 years (IQR 27–41), 70.6% (36/51) were female, and 70.6% (36/51) were white. The median years of experience in healthcare was 5 years (IQR 3–15), 66.7% (34/51) were registered nurses, and 60.9% (31/51) of participants participated in at least one resuscitation per month. All participants were at least previously BLS certified (100%), and 66.7% (34/51) had prior ACLS training. Only two participants (4%) had previous experience with the use of AR applications.
Table 1.
Baseline participant characteristics.
| Age (years), median (IQR) | 31 (27–41) |
| Gender (female) | 36 (70.6%) |
| Race (white) | 36 (70.6%) |
| Healthcare experience (years), median (IQR) | 5 (3–15) |
| Healthcare position | |
| Registered nurse | 34 (66.7%) |
| Physician | 8 (15.7%) |
| Advanced practice registered nurse | 2 (3.9%) |
| Technician | 2 (3.9%) |
| Pharmacy | 2 (3.9%) |
| Other | 3 (5.9%) |
| Resuscitations per month | |
| 0 | 20 (39.2%) |
| 1 | 18 (35.3%) |
| 2-3 | 10 (19.6%) |
| >4 | 3 (5.9%) |
| BLS last certified | |
| ≤1 month | 4 (7.8%) |
| 2–6 months | 14 (27.5%) |
| 7–12 months | 8 (15.7%) |
| 13–24 months | 20 (39.2%) |
| >24 months | 5 (9.8%) |
| ACLS last certified | |
| 2–6 months | 6 (11.8%) |
| 7–12 months | 3 (5.9%) |
| 13–24 months | 21 (41.2%) |
| >24 months | 4 (7.8%) |
| No Response | 5 (9.8%) |
| Not certified | 12 (23.5%) |
| Used AR device in the past (yes) | 2 (3.9%) |
IQR, interquartile range; BLS, basic life support; ACLS, advanced cardiac life support; AR, augmented reality.
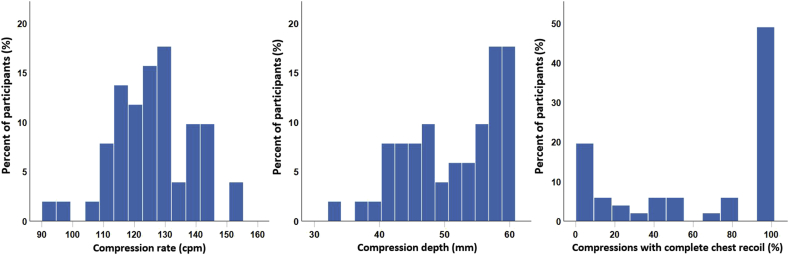
3.2. CPR quality
The distributions for mean CC rate, mean CC depth, and percentage of compressions with complete chest recoil per participant after 2 min of hands-only CPR appear in Fig. 2. The mean CC rate was normally distributed; mean CC depth and percent complete recoil were skewed right towards higher depths and percentages, respectively. CC rates and depths were often between the recommended CPR standards by the AHA, with a mean rate of 126 ± 12.9 cpm, and a median depth of 53 mm (IQR 46–58) (Table 2). Among participants, the percentage of compressions with complete recoil was dispersed but with a high median of 80% (IQR 12–100). No comparative data were reported on CPR quality between HCPs with only BLS versus ACLS certification since no significant differences were found.
Fig. 2.
Frequency histograms of participants' mean CC rate (cpm), mean CC depth (mm), and percent of CC with complete chest recoil (%) after 2 min of CPR.
Table 2.
Hands-only CPR performance parameters during AR resuscitation.
| CC rate (cpm), mean ± SD | 126 ± 12.9 |
| CC depth (mm), median (IQR) | 53 (46–58) |
| CC with complete recoil (%), median (IQR) | 80 (12–100) |
CC, chest compression; cpm, compressions per minute; SD, standard deviation; mm, millimeters, IQR, interquartile range. When the normality assumption was violated, variables were reported as medians (interquartile range) instead of means ±standard deviation.
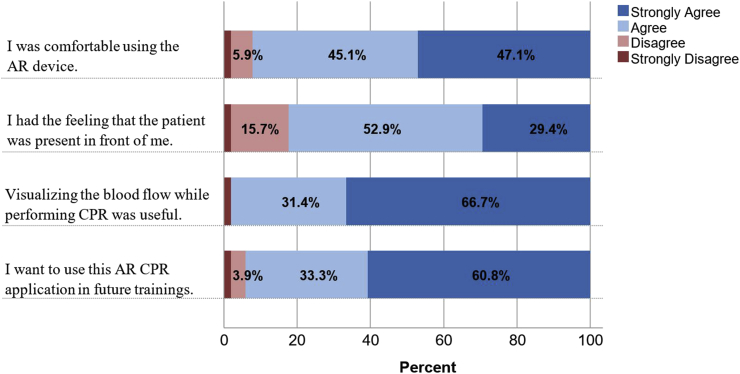
3.3. Participant satisfaction
The results of the participant satisfaction survey were largely positive (Fig. 3). From the cohort, 92.2% (47/51) of participants agreed or strongly agreed that the device was comfortable to use, with 82.3% (42/51) reporting that the application made the experience more realistic since subjects felt that the patient was in front of them during CPR. A total of 98.1% (50/51) perceived the visualization of blood flow as useful for training, and 94.1% (48/51) expressed a willingness to use the CPReality application in future CPR training.
Fig. 3.
Likert scale participant evaluation of the CPReality system.
Participants’ open-ended responses were sorted thematically in Table 3, with some comments falling under more than one category when they made reference to more than one feature. Positive responses were largely related to the immersive visualizations and the feedback they provided. The visualizations were described as more realistic, helpful in visualizing the goal of vital organ perfusion, and generally allowing for a better understanding of the effects of high-quality CPR on patients. As for the feedback component, subjects felt that the auditory (heartbeat metronome) and visual cues (increase or decrease in blow flow to vital organs) allowed for appropriate real-time adjustment of compressions, reinforcing the delivery of effective CPR. Improvement suggestions focused mostly on repositioning the blood circulation hologram closer to or directly on the manikin, and the addition of real-time numerical CC statistics (rate and depth) to the HoloLens view as compressions are being delivered (Table 3).
Table 3.
Open-ended participant feedback about the CPReality application categorized thematically, N = 51.
| Number of responses | ||
|---|---|---|
| Please tell us what you liked about the augmented reality CPR training application?a | Real-time audiovisual feedback:
|
35 |
Blood flow visualization:
|
24 | |
| Use of technology | 3 | |
| Performance scorecard at the end | 1 | |
| Nothing | 1 | |
| No response | 7 | |
| What would you change about the augmented reality CPR training application?a | Position the blood circulation hologram on top of instead of next to the manikin | 12 |
| Provide users with real-time stats during CC | 9 | |
| Sound effect quality or volume | 4 | |
| Headset weight and stability | 2 | |
| Subject reported dizziness | 1 | |
| Nothing | 8 | |
| No response | 15 |
CPR, cardiopulmonary resuscitation; CC, chest compression.
Some comments fall under more than one category.
4. Discussion
This is the first US pilot study to develop an AR CPR system and assess its efficacy in a HCP adult resuscitation training setting. In our cohort, we report a mean CC rate of 126 ± 12.9 cpm, a median CC depth of 53 mm (IQR 46–58), and reduced leaning on the chest, as half of the participants delivered more than 80% of compressions with complete chest recoil [2, 3]. In addition, the AR experience was received favorably by most participants, who found the audio-visual feedback from the interactive circulatory system as educational and helpful in guiding effective compression delivery. Accordingly, our guideline-compliant findings in the AR training environment, and positive participant evaluations demonstrate the feasibility of using this multisensory teaching tool in future CPR trainings for HCPs.
The results of this study are consistent with past research that has shown the value of audio-visual feedback [9, 10] and high fidelity simulation trainings [13] in providing timely information for CPR technique correction, while exposing trainees to simulated clinical situations.
However, our work also contextualizes goal-directed hemodynamic resuscitation by incorporating notions of tailored therapy in CPR; this may serve as a more effective educational approach in line with contemporary patient-centered medical care. As participants are able to visualize the effect of CCs on vital organ perfusion, CPR can be titrated to a virtual measure of blood flow, similar to other investigated physiologic markers such as end-tidal CO2 [26], arterial blood pressure [27], and oxygen content [28]. Similarities may be drawn between the CPReality system and the Brayden illuminating CPR manikin, however AR may offer additional capacity for more vivid and interactive training sessions, besides the greater adaptability of the system to various CPR manikins already in use by various training centers. As may be expected, integrating the proposed technology with standard training manikins will increase costs despite no proven added benefit at this early stage, a question that we aim to address in upcoming randomized controlled trials and prospective cost-benefit analyses of this integration.
Ultimately, CPReality combines both feedback and simulation training into a single immersive experience, coupled with gaming features that can enhance users' attitudes towards CPR training. Gamified learning, recognized by the AHA as an important area of focus for innovation in future resuscitation education [17], has already been evidenced by several studies to be more engaging, enjoyable, and to increase subjects' knowledge retention and self-efficacy while facilitating practice in team-based scenarios [29, 30, 31]. Interestingly, the AHA recently launched an interactive AR hands-only CPR training application using Google's ARCore platform, which allows users to practice and track their own performance on a virtual person, in any location, and without the need for an instructor [32]. One randomized controlled trial found that the use of AR glasses in Pediatric Advanced Life Support (PALS) showed improved adherence to resuscitation guidelines, with a significant reduction of errors in defibrillation doses by 52.5%, compared to pocket reference cards [33]. Another controlled trial on CPR coaching using Google Glass showed a significant increase in the number of successful defibrillations by 32% [34]. While systematic reviews cannot validate the effects of such learning modules at this early stage [35], these promising results suggest an evolution in healthcare education with a potentially impactful influence on patient outcomes.
Several pilot studies have shown creative implementations of technology-enhanced simulation that highlight valuable new opportunities for HCPs to practice technical skills in a safe environment while maintaining the feeling of a high-risk setting. The stated benefits of fidelity and engagement were recognized as ideal for real-life training by CPR instructors in a recent VR CPR trial in Singapore [29]. Investigators have also shown practical implementations in crisis management training, such as in Advanced Trauma Life Support (ATLS), which requires team-based simulation sessions that are otherwise costly and difficult to coordinate with larger teams [36]. Concurrently, recent work from our team with VR technology was able to examine lay bystander response to a realistic sudden cardiac arrest scenario, capturing data previously beyond the reach of investigators [37]. Other implementations in simulated nasogastric tube or central line placement [18, 20, 21], ultrasound image acquisition [19], and endovascular surgery [38] have also shown promise, and as applications evolve, simulated realities will foreseeably approximate to real clinical practice.
There are several limitations to this study, primarily related to the inherent selection bias in enrolling a convenience sample of experienced HCPs already trained in CPR, a learning effect, and a lack of control for confounders since there was neither a pre-test phase to establish baseline CPR performance, nor a control group against which to compare CC quality outcomes. HCPs who volunteered to participate in our study may conceivably have a higher self-efficacy, an important factor that may positively skew CC parameters in our results. As this was a feasibility study however, limitations on the generalizability of our results and inferences about the effectiveness of AR CPR are expected; we aim to address these limitations in a Phase 2 study comparing the AR system to a CPR feedback device. In addition, as enrollments occurred prior to participants’ scheduled BLS and/or ACLS recertification trainings, the duration of the AR simulation was reduced to a single 2-minute cycle to minimize interference with classes; longer durations would have allowed participants for more time to adjust to the environment prior to performance assessment and valuation of the system in the post-CPR survey. Lastly, our reported results on the quality of CPR performed were possibly underestimated since, for most participants, this was their first experience using an AR interface, and only after a short tutorial given by the research coordinators.
5. Conclusions
Overall, the results of this pilot study suggest that AR integration into CPR training may be an effective educational strategy that extends beyond the translation of knowledge and skills, to an inclusive physiology-grounded resuscitation experience in a simulated high-stress environment. As participants generally delivered compressions with adequate rates, depths, and complete chest recoil, the proposed study addresses one of many research questions on technology-enhanced resuscitation education [17], and its possible role in improving HCP's compliance with CPR guidelines. However, given the limitations of this study, further investigations are needed to compare CPReality to traditional CPR training systems.
Declarations
Author contribution statement
Steve Balian: Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data; Wrote the paper.
Shaun K. McGovern: Performed the experiments; Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data; Wrote the paper.
Benjamin S. Abella: Contributed reagents, materials, analysis tools or data; Wrote the paper.
Audrey L. Blewer: Analyzed and interpreted the data; Wrote the paper.
Marion Leary: Conceived and designed the experiments; Performed the experiments; Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data; Wrote the paper.
Funding statement
Marion Leary was supported by the Zoll Foundation for this work.
Competing interest statement
The authors declare the following conflict of interests:
Benjamin Abella received research funding from the American Heart Association, National Institutes of Health, Patient Centered Outcomes Research Institute and CR Bard; speaking honoraria from CR Bard and Stryker.
Audrey Blewer was supported through an American Heart Association Mentored Clinical and Population Award and a Doris Duke grant.
Marion Leary has received research support from the Zoll Foundation for this work. Ms. Leary has received research support from the American Heart Association, Laerdal Foundation and the Medtronic Foundation. Ms. Leary has received in-kind support from Laerdal Medical. Ms. Leary is licensing IP related to her virtual reality technology.
Steve Balian and Shaun McGovern report no conflicts of interest.
Additional information
No additional information is available for this paper.
Acknowledgements
The authors thank the team at the Penn Medicine Clinical Simulation Center and the participating healthcare providers without whom this study would not have been possible. Steve Balian would also like to acknowledge the training received under the Scholars in HeAlth Research Program (SHARP) in clinical and translational research.
References
- 1.Benjamin E.J., Muntner P., Alonso A., Bittencourt M.S., Callaway C.W., Carson A.P. Heart disease and stroke statistics-2019 update: a report from the American Heart Association. Circulation. 2019;139:e56–e528. doi: 10.1161/CIR.0000000000000659. [DOI] [PubMed] [Google Scholar]
- 2.Hazinski M.F., Nolan J.P., Aickin R., Bhanji F., Billi J.E., Callaway C.W. Part 1: executive summary: 2015 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Circulation. 2015;132:S2–39. doi: 10.1161/CIR.0000000000000270. [DOI] [PubMed] [Google Scholar]
- 3.Neumar R.W., Shuster M., Callaway C.W., Gent L.M., Atkins D.L., Bhanji F. Part 1: executive summary: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015;132:S315–S367. doi: 10.1161/CIR.0000000000000252. [DOI] [PubMed] [Google Scholar]
- 4.Kilgannon J.H., Kirchhoff M., Pierce L., Aunchman N., Trzeciak S., Roberts B.W. Association between chest compression rates and clinical outcomes following in-hospital cardiac arrest at an academic tertiary hospital. Resuscitation. 2017;110:154–161. doi: 10.1016/j.resuscitation.2016.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cheng A., Brown L.L., Duff J.P., Davidson J., Overly F., Tofil N.M. Improving cardiopulmonary resuscitation with a CPR feedback device and refresher simulations (CPR CARES Study): a randomized clinical trial. JAMA Pediatr. 2015;169:137–144. doi: 10.1001/jamapediatrics.2014.2616. [DOI] [PubMed] [Google Scholar]
- 6.Cheng A., Overly F., Kessler D., Nadkarni V.M., Lin Y., Doan Q. Perception of CPR quality: influence of CPR feedback, Just-in-Time CPR training and provider role. Resuscitation. 2015;87:44–50. doi: 10.1016/j.resuscitation.2014.11.015. [DOI] [PubMed] [Google Scholar]
- 7.Sugerman N.T., Edelson D.P., Leary M., Weidman E.K., Herzberg D.L., Vanden Hoek T.L. Rescuer fatigue during actual in-hospital cardiopulmonary resuscitation with audiovisual feedback: a prospective multicenter study. Resuscitation. 2009;80:981–984. doi: 10.1016/j.resuscitation.2009.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Smith K.K., Gilcreast D., Pierce K. Evaluation of staff's retention of ACLS and BLS skills. Resuscitation. 2008;78:59–65. doi: 10.1016/j.resuscitation.2008.02.007. [DOI] [PubMed] [Google Scholar]
- 9.Kirkbright S., Finn J., Tohira H., Bremner A., Jacobs I., Celenza A. Audiovisual feedback device use by health care professionals during CPR: a systematic review and meta-analysis of randomised and non-randomised trials. Resuscitation. 2014;85:460–471. doi: 10.1016/j.resuscitation.2013.12.012. [DOI] [PubMed] [Google Scholar]
- 10.Gruber J., Stumpf D., Zapletal B., Neuhold S., Fischer H. Real-time feedback systems in CPR. Trends Anaesth. Crit. Care. 2012;2:287–294. [Google Scholar]
- 11.Seethala R.R., Esposito E.C., Abella B.S. Approaches to improving cardiac arrest resuscitation performance. Curr. Opin. Crit. Care. 2010;16:196–202. doi: 10.1097/MCC.0b013e328338c121. [DOI] [PubMed] [Google Scholar]
- 12.Couper K., Perkins G.D. Debriefing after resuscitation. Curr. Opin. Crit. Care. 2013;19:188–194. doi: 10.1097/MCC.0b013e32835f58aa. [DOI] [PubMed] [Google Scholar]
- 13.Mundell W.C., Kennedy C.C., Szostek J.H., Cook D.A. Simulation technology for resuscitation training: a systematic review and meta-analysis. Resuscitation. 2013;84:1174–1183. doi: 10.1016/j.resuscitation.2013.04.016. [DOI] [PubMed] [Google Scholar]
- 14.Au K., Lam D., Garg N., Chau A., Dzwonek A., Walker B. Improving skills retention after advanced structured resuscitation training: a systematic review of randomized controlled trials. Resuscitation. 2019;138:284–296. doi: 10.1016/j.resuscitation.2019.03.031. [DOI] [PubMed] [Google Scholar]
- 15.Niles D.E., Nishisaki A., Sutton R.M., Elci O.U., Meaney P.A., O'Connor K.A. Improved retention of chest compression psychomotor skills with brief “rolling refresher” training. Simul. Healthc. 2017;12:213–219. doi: 10.1097/SIH.0000000000000228. [DOI] [PubMed] [Google Scholar]
- 16.Sullivan N.J., Duval-Arnould J., Twilley M., Smith S.P., Aksamit D., Boone-Guercio P. Simulation exercise to improve retention of cardiopulmonary resuscitation priorities for in-hospital cardiac arrests: a randomized controlled trial. Resuscitation. 2015;86:6–13. doi: 10.1016/j.resuscitation.2014.10.021. [DOI] [PubMed] [Google Scholar]
- 17.Cheng A., Nadkarni V.M., Mancini M.B., Hunt E.A., Sinz E.H., Merchant R.M. Resuscitation education science: educational strategies to improve outcomes from cardiac arrest: a scientific statement from the American Heart Association. Circulation. 2018;138:e82–e122. doi: 10.1161/CIR.0000000000000583. [DOI] [PubMed] [Google Scholar]
- 18.Aebersold M., Voepel-Lewis T., Cherara L., Weber M., Khouri C., Levine R. Interactive anatomy-augmented virtual simulation training. Clin. Simul. Nurs. 2018;15:34–41. doi: 10.1016/j.ecns.2017.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mahmood F., Mahmood E., Dorfman R.G., Mitchell J., Mahmood F.U., Jones S.B. Augmented reality and ultrasound education: initial experience. J. Cardiothorac. Vasc. Anesth. 2018;32:1363–1367. doi: 10.1053/j.jvca.2017.12.006. [DOI] [PubMed] [Google Scholar]
- 20.Huang C.Y., Thomas J.B., Alismail A., Cohen A., Almutairi W., Daher N.S. The use of augmented reality glasses in central line simulation: “see one, simulate many, do one competently, and teach everyone”. Adv. Med. Educ. Pract. 2018;9:357–363. doi: 10.2147/AMEP.S160704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rochlen L.R., Levine R., Tait A.R. First-person point-of-view-augmented reality for central line insertion training: a usability and feasibility study. Simul. Healthc. 2017;12:57–62. doi: 10.1097/SIH.0000000000000185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Alaker M., Wynn G.R., Arulampalam T. Virtual reality training in laparoscopic surgery: a systematic review & meta-analysis. Int. J. Surg. 2016;29:85–94. doi: 10.1016/j.ijsu.2016.03.034. [DOI] [PubMed] [Google Scholar]
- 23.Bernardo A. Virtual reality and simulation in neurosurgical training. World Neurosurg. 2017;106:1015–1029. doi: 10.1016/j.wneu.2017.06.140. [DOI] [PubMed] [Google Scholar]
- 24.Hanna M.G., Ahmed I., Nine J., Prajapati S., Pantanowitz L. Augmented reality technology using Microsoft HoloLens in anatomic pathology. Arch. Pathol. Lab Med. 2018;142:638–644. doi: 10.5858/arpa.2017-0189-OA. [DOI] [PubMed] [Google Scholar]
- 25.Elo S., Kyngas H. The qualitative content analysis process. J. Adv. Nurs. 2008;62:107–115. doi: 10.1111/j.1365-2648.2007.04569.x. [DOI] [PubMed] [Google Scholar]
- 26.Sutton R.M., French B., Meaney P.A., Topjian A.A., Parshuram C.S., Edelson D.P. Physiologic monitoring of CPR quality during adult cardiac arrest: a propensity-matched cohort study. Resuscitation. 2016;106:76–82. doi: 10.1016/j.resuscitation.2016.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mally S., Jelatancev A., Grmec S. Effects of epinephrine and vasopressin on end-tidal carbon dioxide tension and mean arterial blood pressure in out-of-hospital cardiopulmonary resuscitation: an observational study. Crit. Care. 2007;11:R39. doi: 10.1186/cc5726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Spindelboeck W., Schindler O., Moser A., Hausler F., Wallner S., Strasser C. Increasing arterial oxygen partial pressure during cardiopulmonary resuscitation is associated with improved rates of hospital admission. Resuscitation. 2013;84:770–775. doi: 10.1016/j.resuscitation.2013.01.012. [DOI] [PubMed] [Google Scholar]
- 29.Wong M.A.M.E., Chue S., Jong M., Benny H.W.K., Zary N. Clinical instructors' perceptions of virtual reality in health professionals' cardiopulmonary resuscitation education. SAGE Open Med. 2018;6 doi: 10.1177/2050312118799602. 2050312118799602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kron F.W., Gjerde C.L., Sen A., Fetters M.D. Medical student attitudes toward video games and related new media technologies in medical education. BMC Med. Educ. 2010;10:50. doi: 10.1186/1472-6920-10-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Creutzfeldt J., Hedman L., Fellander-Tsai L. Cardiopulmonary resuscitation training by avatars: a qualitative study of medical students' experiences using a multiplayer virtual world. JMIR Serious Games. 2016;4:e22. doi: 10.2196/games.6448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.New Augmented Reality Hands-Only CPR Makes Training Life-like and mobile, Retrieved from: newsroom.heart.org/news/new-augmented-reality-hands-only-cpr-makes-training-life-like-and-mobile (March 20, 2018, accessed March 3 2019).
- 33.Siebert J.N., Ehrler F., Gervaix A., Haddad K., Lacroix L., Schrurs P. Adherence to AHA guidelines when adapted for augmented reality glasses for assisted pediatric cardiopulmonary resuscitation: a randomized controlled trial. J. Med. Internet Res. 2017;19:e183. doi: 10.2196/jmir.7379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Perez Alonso N., Pardo Rios M., Juguera Rodriguez L., Vera Catalan T., Segura Melgarejo F., Lopez Ayuso B. Randomised clinical simulation designed to evaluate the effect of telemedicine using Google Glass on cardiopulmonary resuscitation (CPR) Emerg. Med. J. 2017;34:734–738. doi: 10.1136/emermed-2016-205998. [DOI] [PubMed] [Google Scholar]
- 35.Akl E.A., Kairouz V.F., Sackett K.M., Erdley W.S., Mustafa R.A., Fiander M. Educational games for health professionals. Cochrane Database Syst. Rev. 2013;3:CD006411. doi: 10.1002/14651858.CD006411.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Youngblood P., Harter P.M., Srivastava S., Moffett S., Heinrichs W.L., Dev P. Design, development, and evaluation of an online virtual emergency department for training trauma teams. Simul. Healthc. 2008;3:146–153. doi: 10.1097/SIH.0b013e31817bedf7. [DOI] [PubMed] [Google Scholar]
- 37.Leary M., Almodovar A., Jr., Buckler D.G., Bhardwaj A., Blewer A.L., Abella B.S. Using an immersive virtual reality system to assess lay provider response to an unannounced simulated sudden cardiac arrest in the out-of-hospital setting. Simul. Healthc. 2018 doi: 10.1097/SIH.0000000000000338. [DOI] [PubMed] [Google Scholar]
- 38.Kuhlemann I., Kleemann M., Jauer P., Schweikard A., Ernst F. Towards X-ray free endovascular interventions - using HoloLens for on-line holographic visualisation. Healthc. Technol. Lett. 2017;4:184–187. doi: 10.1049/htl.2017.0061. [DOI] [PMC free article] [PubMed] [Google Scholar]