Abstract
Purpose of Review
To assess complications after minimally invasive spinal surgeries including transforaminal lumbar interbody fusion (MI-TLIF) by reviewing the most recent literature.
Recent Findings
Current literature demonstrates that minimally invasive surgery (MIS) in spine has improved clinical outcomes and reduced complications when compared with open spinal procedures. Recent studies describing MI-TLIF primarily for degenerative disk disease, spondylolisthesis, and vertebral canal stenosis cite over 89 discrete complications, with the most common being radiculitis (ranging from 2.8 to 57.1%), screw malposition (0.3–12.7%), and incidental durotomy (0.3–8.6%).
Summary
Minimally invasive spine surgery has a distinct set of complications in comparison with other spinal procedures. These complications vary based on the exact MIS procedure and indication. The most frequently documented MI-TLIF complications in current published literature were radiculitis, screw malposition, and incidental durotomy.
Keywords: Minimally invasive, Spine, Transforaminal lumbar interbody fusion (TLIF), Complications, Systematic review
Introduction
In the USA, around 80% of the population will experience back pain during their lifetime [1], many of whom will require surgical intervention. Over the past 30 years, minimally invasive surgery (MIS) has emerged as a leading treatment choice for spinal ailments. These techniques caused a major paradigm shift in spine surgery by proving that decreased operating exposure can translate to clinical benefits, such as decreased rates of CSF leaks, infection, and length of stay [2, 3, 4••].
Minimally invasive lumbar spine procedures are used for discectomy, spinal decompression, posterior lumbar interbody fusion (MI-PLIF), and transforaminal lumbar interbody fusion (MI-TLIF). Each of these operations is associated with distinct complication profiles. The complication rate for discectomy procedures is around 1.5% and includes dural tears, nerve root injury, and discitis [5]. Following decompression, common complications include dural tears and delayed pseudomeningocele formation [6, 7]. A review found complication rates ranged from 0 to 33.3% for MI-TLIF and 1.6–16.7% for MI-PLIF with radiculopathy and cerebrospinal fluid leakage being the most common etiologies [8].
Not only is there variation in complication rates among different minimally invasive spine procedures, but there also is a wide range in complication profiles based on the specific surgical approach and indication. Despite leading to decreased complication rates, there are unique complications after minimally invasive spinal procedures, especially MI-TLIF. By understanding the complications associated with once novel, and now commonplace, minimally invasive spinal techniques, surgeons can better prepare for these complications and address them when they occur.
Methods
A systematic review in PubMed was performed to identify all articles published from January 2002 to January 2019 for patients undergoing MI-TLIF. The search terms included MeSH terms for minimally invasive surgical procedures and transforaminal lumbar interbody fusion. Abstracts were screened for the following inclusion criteria: English language, patients who underwent MI-TLIF procedure(s), with sample size of at least 100 subjects. Exclusion criteria included: studies involving non-surgical patients, abstracts, case reports, meta-analyses, literature reviews, technical notes, and studies that did not document complications. Among articles meeting inclusion criteria, article information and data on complication types, rates, and outcomes were summarized. The search was independently replicated by internal author (B.H.) to ensure accuracy.
Results
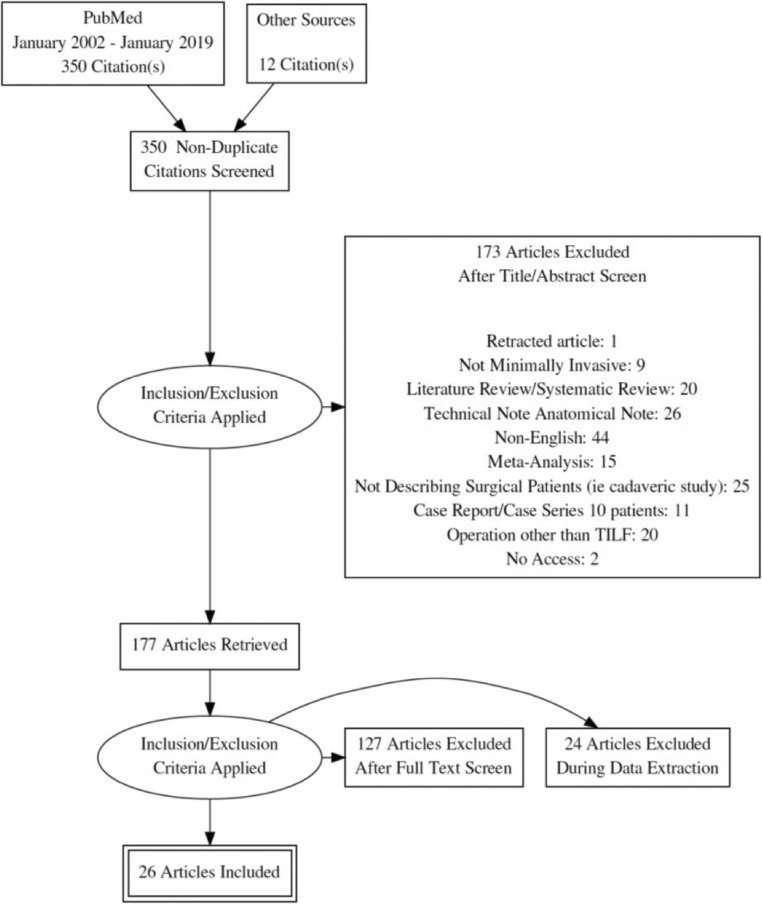
Review of the literature for MI-TLIF studies resulted in 31 articles published from 2008 to 2019 meeting eligibility criteria (Fig. 1). Indications for MI-TLIF included degenerative disk disease, spondylolisthesis, and vertebral canal stenosis as the indicators for surgery. These studies included 12 retrospective single-arm studies, 8 retrospective comparative studies, 3 prospective comparative studies, and 3 prospective single-arm studies. In total, 6699 patients undergoing MI-TLIF were included in the final 31 studies.
Fig. 1.
PRISMA systematic review flow chart. PRISMA flow chart displaying the systematic review of minimally invasive transforaminal lumbar interbody fusion (MI-TLIF)
Of the 31 articles, 26 articles specified the complications following MI-TLIF (Table 1). There were five articles that met inclusion criteria but did not report complications [35–39]. The most common complication cited after MI-TLIF surgery was radiculitis, with a range between rates of 2.8 and 57.1%. The second most common complication documented in the literature was screw malposition, ranging between rates of 0.3 and 12.7%. The third most common complication was incidental durotomy, with a range between 0.3 and 8.6%. Six articles specifically focused on one type of complication, including graft extrusion, incidental durotomy, pedicle breach, cage subsidence, superior facet violation, and screw malposition. These articles did not document data on other complications. In total, the studies referenced 89 (range 1 to 21) discrete complications for MI-TLIF.
Table 1.
Included study characteristics and corresponding complication data for MI-TLIF
| Author | Year | Design | F/U | MI-TLIF patient sample |
Complication | N | % | Recommended treatment | Resolution of complication on follow-up |
|---|---|---|---|---|---|---|---|---|---|
| Senker et al. [9] | 2018 | Retrospective, single arm | 1 mo to 1 y | 229 patients |
Postoperative neurologic deficit Incorrect fixation (rod) Screw loosening (osteoporotic) Dermal excoriation due to surgical draping Activated omarthrosis by surgery storage Adjacent segment disease Urinary tract infection Hematoma (spinal epidural, POD 4) Screw pullout (osteoporotic) Screw malposition Vertebral canal narrowing (POD 1, bony fragment) Vertebral canal narrowing (POD 16, pedicle fracture) Mechanical dislocation of proximal fusion system Cerebrospinal fluid leak |
1 2 2 1 1 1 2 1 1 1 1 1 1 3 |
0.4 0.9 0.9 0.4 0.4 0.4 0.9 0.4 0.4 0.4 0.4 0.4 0.4 1.3 |
NR NR NR NR NR NR NR Revision surgery Cement screws (after 2 months) Revision surgery (day 3) Revision surgery (day 1) Revision surgery day 16 Revision surgery, 1 month NR |
NR NR NR NR NR NR NR NR NR NR NR NR NR NR |
| Fan et al. [10] | 2017 | Prospective, comparative | NR | 126 patients, comparing localization systems in overweight/obese (BMI ≥ 24) patients |
Cerebrospinal fluid leak (intraoperatively) Surgical site infection Guide wire breakage |
2 2 1 |
1.6 1.6 0.8 |
Conservative treatment Antibiotics Broken wire removed intra-operatively |
NR NR Resolved |
| Singh et al. [11] | 2017 | Retrospective, comparative | 6–12 wks. | 139 patients comparing post-op analgesia | Unspecified: either incidental durotomy, epidural hematoma, ligament tear, perioperative fracture, vascular injury, hemorrhage | 1 | 0.7 | NR | NR |
| Li et al. [12] | 2017 | Prospective, comparative | 30.3 mo mean | 103 patients using tunnel technique, compared to open TLIF |
Pneumonia Screw malposition |
1 3 |
1.0 2.9 |
Not reported Asymptomatic, no replacement needed |
NR NR |
| Liu and Zhou [13] | 2017 | Prospective, comparative | 46.5 mean | 192 patients compared to PELD |
Incidental durotomy; cerebrospinal fluid leak (lasted 3–5 days post-op) Adjacent segment disease Surgical site infection (deep) |
6 5 1 |
3.1 2.6 0.5 |
overlying fascia closed tightly, supine bed rest few days post-operatively NR Surgery |
Resolved within 1 week; CSF leakage lasted 3–5 days NR Resolved |
| Tay et al. [14] | 2016 | Retrospective, comparative | 2.71–2.88 y mean | 230 patients comparing outcomes in patients with and without mild lumbar scoliosis |
Graft site infection (iliac crest); Non-union; cage retropulsion Screw malposition; pneumonia; cage migration Broken cage (intraoperatively) Graft site infection (iliac crest); Incidental durotomy Screw malposition (medial R L5 pedicle); cage migration Urinary tract infection Skin urticaria Cage subsidence; progression of spondylolisthesis Cage subsidence Progression of spondylolisthesis Broken screw (left L5 pedicle) Screw loosening (right L5 pedicle) Screw malposition Radiculopathy (persistent, left L5) Non-union Cage subsidence; broken screw (right S1 pedicle) Cage migration Cage migration; progression of spondylolisthesis Cage subsidence; screw loosening (B/L L4 pedicle) |
1 1 1 1 1 1 1 2 7 1 1 1 1 1 1 1 3 1 1 |
0.4 0.4 0.4 0.4 0.4 0.4 0.4 0.9 3.0 0.4 0.4 0.4 0.4 0.4 0.4 0.4 1.3 0.4 0.4 |
Exploration, debridement, oral antibiotics, revision 4 y later Revision surgery (2 wks), pneumonia resolved with IV antibiotics Cage could not be removed debridement, oral antibiotics; dural tear repaired with collagen matrix, fibrin glue intraoperatively Revision MIS surgery (2 wks.) Conservative treatment Conservative treatment No intervention No intervention No intervention No intervention No intervention No intervention Left L4–L5 pedicle screws, rod removed Revision MIS instrumentation with bone grafting 2 y later No intervention No intervention No intervention No intervention |
Resolved Poor outcome Resolved Resolved Resolved Resolved Resolved Asymptomatic Asymptomatic Asymptomatic Asymptomatic Asymptomatic Asymptomatic No improvement; poor outcome Resolved Asymptomatic Asymptomatic Asymptomatic Asymptomatic |
| Bakhsheshian et al. [15] | 2016 | Retrospective, single arm | 13.6 mo (8.8) mean (SD) | 513 patients focused on graft extrusions |
Graft extrusion Graft extrusion; hematoma (spinal epidural) |
4 1 |
0.8 0.2 |
2 patients required revision surgery for cage migration, 2 patients had no clinical consequences Revision surgery POD 3 |
NR NR |
| Wong et al. [16••] | 2015 | Prospective, single arm | 13.6 mo (8.8) mean (SD) | 513 patients |
Incidental durotomy Instrumentation failure Urinary retention Pulmonary embolism Neurological deficit Ileus Hematoma Deep vein thrombosis Surgical site infection |
26 11 7 5 4 4 4 2 1 |
5.1 2.1 1.4 1.0 0.8 0.8 0.8 0.4 0.2 |
Flat bed rest overnight Revision surgery (2), k wire retrieved (5), intraoperative repositioning and removal of k wire fragment (1) No intervention Anticoagulation therapy Physical therapy No intervention Reoperation for evacuation (for the 3 patients who had continued radicular sx) Anticoagulation therapy NR |
Resolved Resolved Resolved Resolved (1 death) 2 residual weakness, 2 resolved Resolved Resolved Resolved NR |
| Giorgi et al. [17] | 2015 | Prospective, single arm | 1y | 182 patients |
Non-union Screw malposition (symptomatic) Non-union Surgical site infection Bleeding (unspecified) Other complications without revision |
2 5 2 1 1 5 |
1.1 2.7 1.1 0.5 0.5 2.7 |
Revision surgery Revision surgery Revision surgery Revision surgery Revision surgery No intervention |
NR NR NR NR NR NR |
| Klingler et al. [18] | 2015 | Retrospective, single arm | NR | 372 patients focus on incidental durotomies |
Incidental durotomy There were 3 additional complications noted, but only within the accidental durotomy group, so excluded |
32 | 8.6 | Conservative treatment | Resolved |
| Scheer et al. [19] | 2015 | Retrospective, comparative | 1 y | 282 patients comparing in situ arthrodesis vs reduction |
C. difficile diarrhea Pneumonia Cholecystitis Atrial flutter Acute mental status change Stroke Urinary retention Deep vein thrombosis Ileus Urinary tract infection Pulmonary embolism Incarcerated hernia Cage retropulsion Cage expulsion Extruded interbody cage Cerebrospinal fluid leak Kwire fracture Hematoma (wound) Surgical site infection Neurologic deficit (somatosensory evoked potentials) Neurologic deficit (loss motor evoked potentials) |
1 2 1 1 2 2 3 1 1 1 2 1 1 1 1 22 2 2 1 4 2 |
0.4 0.7 0.4 0.4 0.7 0.7 1.1 0.4 0.4 0.4 0.7 0.4 0.4 0.4 0.4 7.8 0.7 0.7 0.4 1.4 0.7 |
NR NR NR NR NR NR NR NR NR NR NR NR NR NR NR NR NR NR NR NR NR |
NR NR NR NR NR NR NR NR NR NR NR NR NR NR NR NR NR NR NR NR NR |
| Park et al. [20] | 2015 | Retrospective, single arm | NR | 124 patients |
Temporary postoperative neuralgia Deep wound infection Screw malposition Cage migration Incidental durotomy Graft extrusion |
3 2 2 2 1 1 |
2.4 1.6 1.6 1.6 0.8 0.8 |
NR Reoperation Reoperation Reoperation Repaired Reoperation |
Resolved Resolved Resolved (one pseudoarthrosis) Resolved Resolved Resolved |
| Eckman et al. [21] | 2014 | Retrospective, comparative | 3 mo | 1005 patients 1114 procedures |
Transfusions Infection (unspecified) Revision surgery (unspecified) |
7 1 33 |
0.7 0.1 3.3 |
NR NR NR |
NR NR NR |
| Park et al. [22] | 2014 | Retrospective, single arm | 5 y | 124 patients |
Incidental durotomy Screw malposition Cage migration Graft extrusion Temporary postoperative neuralgia Deep wound infection Pseudoarthrosis Adjacent segment disease (symptomatic) Spinal stenosis (including foraminal stenosis) Vertebral compression fracture Herniated lumbar disc Spondylolisthesis |
1 2 2 1 3 2 41 35 25 5 3 2 |
0.8 1.6 1.6 0.8 2.4 1.6 33.1 28.2 20.2 4 2.4 1.6 |
NR Secondary surgery (2) Secondary surgery (2) Secondary surgery (1) NR Secondary surgery (2) secondary surgery, for pseudoarthrosis and ASD (1) Secondary surgery (7) Secondary surgery (7) NR NR NR |
NR NR NR NR NR NR NR NR NR NR NR NR |
| Perez-Cruet et al. [23] | 2014 | Prospective, single arm | 47 mo mean | 304 patients |
Screw malposition Incidental durotomy Interbody cage retropulsion Bleeding (intraoperative hemorrhage > 500 mL) Broken screw (7mo. post-operative) Urinary retention Surgical site infection (superficial) Atelectasis Pneumonia Urinary tract infection Deep vein thrombosis |
1 1 3 1 1 17 11 8 3 2 1 |
0.3 0.3 1 0.3 0.3 5.6 3.6 2.6 1 0.7 0.3 |
Return to operating room Conversion to open TLIF Reoperation NR NR NR NR NR NR NR NR |
NR NR NR NR NR NR NR NR NR NR NR |
| Smith et al. [24] | 2014 | Prospective, single arm | 9 mo mean | 151 patients focus on pedicle breach after percutaneous screw fixation | Transient nerve root complication | 2 | 1.3 | No intervention | Resolved |
| Wang et al. [25] | 2014 | Retrospective, single arm | 1 mo | 204 patients |
Myocardial infarction Stroke Gastric bleeding Pneumonia Urinary retention Urinary tract infection Hardware malposition Hematoma (local epidural) Graft dislodgement Manipulative error Nerve impingement Surgical site infection (superficial) Incidental durotomy Neurologic deficit (leg sensory disturbance) |
1 1 3 2 15 6 3 2 1 1 1 5 10 24 |
0.5 0.5 1.5 1 7.4 2.9 1.5 1 0.5 0.5 0.5 2.5 4.9 11.8 |
NR NR NR NR NR NR NR Reoperation within 1 week Reoperation within 1 week No intervention Reoperation within 1 week NR Fascia closed tightly over No intervention |
NR NR NR NR NR NR Permanent neurologic damage (1), resolved (2) Resolved Resolved Permanent neurologic damage Resolved NR Resolved NR |
| Wong et al. [26] | 2014 | Retrospective, comparative | 46 mo | 144 patients compared with open TLIF |
Neurologic radiculitis; neurologic deficit (immediate postoperative) Neurologic radiculitis; neurologic deficit (> 48 h) Cerebrospinal fluid leaks Vascular or abdominal injury Persistent stenosis (symptomatic) Screw malposition Cage migration Transfusion (postoperative) Respiratory infection Urinary tract infection Surgical site infection (superficial) Hematoma (diagnosed postoperatively) Deep vein thrombosis (symptomatic) Revision surgery (4 y, overall) Repeat decompression Revision surgery (hardware issues) Vascular or abdominal repair Pseudarthrosis Adjacent-level degeneration (new) |
8 4 5 1 7 2 1 3 3 3 6 3 2 12 2 3 1 3 3 |
5.6 2.8 3.5 0.7 4.9 1.4 0.7 2.1 2.1 2.1 4.2 2.1 1.4 8.3 1.4 2.1 0.7 2.1 2.1 |
NR NR NR NR NR Revision surgery Revision surgery NR NR NR NR NR NR Revision surgery Revision surgery Revision surgery Reoperation NR NR |
NR NR NR NR NR NR NR NR NR NR NR NR NR NR NR NR NR NR NR |
| Kim et al. [27] | 2013 | Retrospective, single arm | 2 y | 104 patients focus on cage subsidence |
Cage subsidence < 2 mm 2–4 mm < 4 mm |
22 10 8 |
21.2 9.6 7.7 |
NR NR NR |
NR NR NR |
| Lau et al. [28] | 2013 | Retrospective, comparative | NR | 142 patients focus on superior facet violation; comparing open vs MI-TLIF, imaging technique | Superior facet violation | 9 | 6.3 | NA | NA |
| Silva et al. [29] | 2013 | Retrospective, comparative | 33 mo mean | 138 patients |
Incidental durotomy Urinary retention; perineal hypesthesia Radiculopathy (severe, transient, postoperative) Surgical site infection (superficial) Radiculopathy (motor, persistent) Screw malposition Hematoma (extradural) Myocardial infarction |
8 1 3 2 1 1 1 1 |
5.8 0.7 2.2 1.5 0.7 0.7 0.7 0.7 |
Corrected intraoperatively convert to open procedure (1) NR NR NR NR Revision Reintervention NR |
Resolved; persistent neurogenic bladder, perineal hypesthesia (1) NR NR NR NR NR NR NR |
| Singh et al. [30] | 2013 | Retrospective, single arm | 1 y | 610 patients 573 followed up |
Radiculitis Incidental durotomy Surgical site infection Neuroforaminal bone growth; osteolysis; cage migration Revision surgery (other) Bone overgrowth; nerve impingement; radiculopathy Cage migration; osteolysis (in 2 of the above bone overgrowth patients) Calcified fluid collection Pseudoarthrosis |
327 23 3 10 39 10 2 1 39 |
57.1 4.0 0.5 1.7 6.8 1.7 0.3 0.2 6.8 |
Medrol dose pack 1 month NR Irrigation and debridement (1) Revision surgery (3 underwent two revisions) NR NR Revision surgery NR Revision arthrodesis |
Resolved (except cases that underwent revision surgery before) NR NR NR NR NR NR NR NR |
| Kim et al. [31] | 2011 | Retrospective, single arm | NR | 110 patients focus on pedicle malposition screws (% reflects screw malposition per 488 total screws placed) |
Screw malposition (cortical encroachment) Screw malposition (Frank penetration) Minor (< 2 mm) Moderate (≥ 2, < 4 mm) Severe (≥ 4 mm) |
61* 46* 7* 1* |
12.5* 9.4* 1.4* 0.2* |
NR NR 2 needed revision |
NR NR Of revision patients: 1 residual neurological deficit, 1 resolved |
| Rouben et al. [32] | 2011 | Prospective, single arm | 49 mo | 169 patients |
Screw malposition (painful pedicle screws) Pseudarthrosis Infection (staph) Broken pedicles (L4, postoperative fall) |
6 1 1 1 |
3.6 0.6 0.6 0.6 |
Revision needed, 3 needed fusion with adjacent level due to pain NR Revision surgery Revision surgery |
Resolved Resolved Resolved Resolved |
| Matsumoto et al. [33] | 2010 | Retrospective, comparative | NR | 379 patients combined TLIF and PLIF, not specified | Dural injury | 1 | 0.3 | Specific treatment not documented | NR |
| Rosen et al. [34] | 2008 | Prospective, single arm | 14.8 mo mean | 110 patients |
Urinary retention Lower extremity weakness Delirium Radiculopathy (postoperative) Positioning injury Incidental durotomy Surgical site infection (superficial) Congestive heart failure exacerbation Hypertension Hypotension Ileus |
4 1 5 5 1 2 1 1 2 2 1 |
3.6 0.9 4.5 4.5 0.9 1.8 0.9 0.9 1.8 1.8 0.9 |
NR NR NR NR NR NR NR NR NR NR NR |
NR NR NR NR NR NR NR NR NR NR NR |
F/U, follow-up time period; NR, not reported; y, year; mo, months; wks, weeks; b/l, bilateral; post-op, postoperative; sx, symptoms; PLIF, posterior lumbar interbody fusion; TLIF, transforaminal lumbar interbody fusion; POD, postoperative day; BMI, body mass index; PELD, percutaneous endoscopic lumbar discectomy; ASD, adjacent segment disease; kwire, kirschner wire
*Values are represented as the number and the percentage of misplaced screws (n = 488)
Discussion
Minimally invasive spine surgery has shown favorable clinical outcomes when compared with open procedure [2, 3, 4••, 40, 41]. Minimally invasive spine surgery has been shown to have decreased blood loss, hospital stay, medical and surgical complications, and equivalent patient satisfaction rates as traditional methods [42]. Although minimally invasive spine surgery has a favorable complication profile when compared with open methods, extensive studies continue to reveal that these newer techniques have distinct complications. In the review of the literature, 31 articles describing MI-TLIF were identified but only 26 articles reported complications. The top three complication categories among large sample size MI-TLIF studies were radiculitis, screw malposition, and incidental durotomy.
Open TLIF is progressively being replaced with minimally invasive techniques. First described in 2002 by Foley and Gupta, MI-TLIF was reported to have decreased paraspinous tissue damage, without weakening the effectiveness of the spinal fusion [43]. Meta-analyses comparing minimally invasive and open TLIF have documented decreased blood loss and quicker rehabilitation in the minimally invasive cohorts. The improved timing to postoperative ambulation in turn results in decreased complication rates, decreased length of stay, and ultimately decreased healthcare costs [4••, 40, 41]. For these reasons, trends favor minimally invasive approaches for lumbar fusion. Due to smaller surgical window and introduction of novel techniques, common complications include neurological deficits, cerebrospinal fluid leaks, and misplaced hardware [44]. This systematic review corroborates previous published common MI-TLIF complications. Cerebrospinal fluid leaks have been shown to occur less often in minimally invasive spine surgery when compared with open surgery, and when they do occur, CSF leaks in open surgical procedures result in higher rates of lumbar drain placement and surgical intervention [26]. There are some unique but uncommon complications that are becoming more prevalent with the use of minimally invasive spine surgical approaches. One such complication is a Kirschner wire (K-wire) fracture during MI-TLIF. Although rare, with one study revealing an incidence as low as 1.2%, K-wire fractures pose a potential risk for migration and further complications [45]. There are limited data on K-wire fractures, often because this might go undocumented and is thus underreported in the literature on complications following minimally invasive spine procedures.
Additionally, specific patient characteristics might influence the rates and variability of complications following spine surgery including body mass and age. Obesity has been associated with greater rates of perioperative complications during thoracic and lumbar fusion [46]. However, studies investigating outcomes in obese populations compared with normal weight populations undergoing MI-TLIF have found no significant difference in complications [28], with some studies suggesting decreased complications in obese patients undergoing minimally invasive surgery compared with open TLIF [47•]. A retrospective analysis of elderly patients revealed a complication rate of 11.1% and all complications resolving by the 1-year follow-up, suggesting minimally invasive spinal surgery may be safe in elderly populations [48].
Minimally invasive spine surgery for adult spinal deformity also is an important subgroup with a different complication profile. Open surgery for adult scoliosis has been described as having very high complication rates, up to 66% [49]. Minimally invasive lateral transpsoas surgery for adult degenerative scoliosis (DS), however, has been shown to have significantly decreased complications when compared with open surgery [50, 51]. In one study investigating concave versus convex approaches for minimally invasive lateral lumbar interbody fusions for thoracolumbar DS, complications occurred approximately 25% of the time and reoperations were required in 18.8% of patients, with higher complication risk in the concave approach [19]. Although minimally invasive surgery using a lateral approach has been shown to be effective for both coronal and sagittal spine realignment, cage subsidence remains a serious complication [52].
Minimally invasive spinal decompression (MISD) has been shown to have equivalent efficacy to traditional, open decompression methods, with decreased pain, recovery time, and opioid use [53, 54]. Rahman et al. compared open decompressive laminectomy with minimally invasive lumbar laminectomy for lumbar stenosis, finding complication rates of 16.1% in the open group compared with 7.9% in the minimally invasive cohort [53]. A systematic review describing MISD for degenerative spondylolisthesis found an overall complication rate of 1.6% and an overall reoperation rate of 4.5% [55]. Another systematic review exploring minimally invasive discectomy versus microdiscectomy and open discectomy in lumbar disc herniation cases found lower rates of surgical site infections and urinary tract infections, yet higher rates of rehospitalization for recurrent disc herniation [56].
Recently, minimally invasive spine surgery has extended beyond just novel methods for elective procedures to traumatic injuries. Percutaneous pedicle screw fixation (PPSF) has been shown to be a satisfactory management method for traumatic spine injuries, such as flexion-distraction injuries. Studies comparing open pedicle screw fixation and posterolateral fusion to minimally invasive PPSF in thoracolumbar flexion-distraction injuries found that the two methods had very similar efficacy, with minimally invasive methods resulting in decreased blood loss and tissue damage [57]. A meta-analysis comparing PPSF with open posterior pedicle screw placement for thoracolumbar fractures favored minimally invasive approaches, documenting decreased postoperative pain, blood loss, operating time, length of stay, and incision time, yet no significant difference in complications [58•, 59]. A large study retrospectively analyzing complication rates after PPSF in 781 patients suffering from thoracolumbar and lumbar fracture reported a complication in 5.9%, with complications such as blood vessel injury and poor vertebral reduction and internal fixation, guide wire breakage, screw breakage, and screw malposition [60]. There were also reported complications of screw malposition, cerebrospinal fluid leakage, guide wire rupture, and infection, similar to other minimally invasive spinal procedures.
Minimally invasive spine surgery techniques have revolutionized the management of common and serious spine pathologies, making surgery safer for many patients. Despite the intricacies of specific complication types and rates among varying minimally invasive spine procedures, all novel minimally invasive techniques share a common theme, in that there is a steep learning curve to mastering these innovative procedures [61]. Despite the need for mastering new procedural skills, minimally invasive spine surgical procedures have still been found to have decreased operation time, length of stay, and blood loss, suggesting that the skills associated with minimally invasive spine surgery require specialized surgical training in order to benefit patients [62].
There are several important limitations for this study. We utilized PubMed as the primary engine and attempted to include broad search terms, but it is possible that we did not identify all articles published meeting inclusion criteria. Additionally, the focus of this study is very narrow, systematically analyzing only articles concerning MI-TLIF among studies with at least 100 subjects. There were varying patient populations within the included articles, such as studies including only obese patients or using a distinct surgical technique, perhaps influencing the observed complication rates. Further systematic review of other minimally invasive spine surgeries will be necessary to better understand complication rates across alternative procedures, diagnoses, and patient populations. Future work should focus on a systematic review of all minimally invasive spinal procedures to optimize patient education and clinical preparation and insight into potential complications following minimally invasive spine surgery.
Conclusion
Minimally invasive spine surgery, although proven to have lower complication rates than traditional open methods, continues to have a distinct set of complications. These complications vary based on the exact minimally invasive procedure and indication. The majority of MI-TLIF complications based on current published literature are radiculitis, screw malposition, and incidental durotomy.
Compliance with Ethical Standards
Conflict of Interest
Hannah Weiss, Roxanna Garcia, Ben Hopkins, Nathan Shlobin, and Nader Dahdaleh declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on Minimally Invasive Spine Surgery
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.Deyo RA, Mirza SK, Martin BI. Back pain prevalence and visit rates: estimates from US national surveys, 2002. Spine. 2006;31:2724–2727. doi: 10.1097/01.brs.0000244618.06877.cd. [DOI] [PubMed] [Google Scholar]
- 2.Khan NR, et al. Surgical outcomes for minimally invasive vs open transforaminal lumbar interbody fusion: an updated systematic review and meta-analysis. Neurosurgery. 77:847–74 discussion 874 (2015). [DOI] [PubMed]
- 3.Phan K, Rao PJ, Kam AC, Mobbs RJ. Minimally invasive versus open transforaminal lumbar interbody fusion for treatment of degenerative lumbar disease: systematic review and meta-analysis. Eur Spine J. 2015;24:1017–1030. doi: 10.1007/s00586-015-3903-4. [DOI] [PubMed] [Google Scholar]
- 4.••.Xie L, Wu W-J, Liang Y. Comparison between Minimally Invasive Transforaminal Lumbar Interbody Fusion and Conventional Open Transforaminal Lumbar Interbody Fusion: An Updated Meta-analysis. Chin Med J. 2016;129:1969–86 This recent meta-analysis provides one of the most updated reviews of the literature on open-TLIF vs MIS-TLIF. The findings indicated that MIS-TLIF has fusion rates similar to open-TLIF, but with better functional outcome, decreased blood loss, decreased time to ambulation, and decreased length of hospital stay when compared with patients undergoing open-TLIF. [DOI] [PMC free article] [PubMed]
- 5.Maroon JC. Current concepts in minimally invasive discectomy. Neurosurgery. 2002;51(supplement 2):S137–S145. [PubMed] [Google Scholar]
- 6.Nerland US, Jakola AS, Solheim O, Weber C, Rao V, Lonne G, Solberg TK, Salvesen O, Carlsen SM, Nygaard OP, Gulati S. Minimally invasive decompression versus open laminectomy for central stenosis of the lumbar spine: pragmatic comparative effectiveness study. BMJ. 2015;350:h1603. doi: 10.1136/bmj.h1603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Perez-Cruet MJ, Fessler RG, Perin NI. Complications of minimally invasive spine surgery. Neurosurgery. 2002;51(supplement 2):S26–S36. [PubMed] [Google Scholar]
- 8.Karikari IO, Isaacs RE. Minimally invasive transforaminal lumbar interbody fusion: a review of techniques and outcomes. Spine. 2010;35(26S):S294–S301. doi: 10.1097/BRS.0b013e3182022ddc. [DOI] [PubMed] [Google Scholar]
- 9.Senker W, Gruber A, Gmeiner M, Stefanits H, Sander K, Rössler P, Pflugmacher R. Surgical and clinical results of minimally invasive spinal fusion surgery in an unselected patient cohort of a spinal care unit. Orthop Surg. 2018;10:192–197. doi: 10.1111/os.12397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fan G, Fu Q, Zhang J, Zhang H, Gu X, Wang C, Gu G, Guan X, Fan Y, He S. Radiation reduction of minimally invasive transforaminal lumbar interbody fusion with localisation system in overweight patients: practical technique. Bone Joint J. 2017;99-B:944–950. doi: 10.1302/0301-620X.99B7.BJJ-2016-0853.R1. [DOI] [PubMed] [Google Scholar]
- 11.Singh K, Bohl DD, Ahn J, Massel DH, Mayo BC, Narain AS, Hijji FY, Louie PK, Long WW, Modi KD, Kim TD, Kudaravalli KT, Phillips FM, Buvanendran A. Multimodal analgesia versus intravenous patient-controlled analgesia for minimally invasive transforaminal lumbar interbody fusion procedures. Spine. 2017;42:1145–1150. doi: 10.1097/BRS.0000000000001992. [DOI] [PubMed] [Google Scholar]
- 12.Li Y-B, Wang X-D, Yan H-W, Hao D-J, Liu Z-H. The long-term clinical effect of minimal-invasive TLIF technique in 1-segment lumbar disease. Clin Spine Surg. 2017;30:E713–E719. doi: 10.1097/BSD.0000000000000334. [DOI] [PubMed] [Google Scholar]
- 13.Liu C, Zhou Y. Percutaneous endoscopic lumbar Diskectomy and minimally invasive transforaminal lumbar interbody fusion for recurrent lumbar disk herniation. World Neurosurg. 2017;98:14–20. doi: 10.1016/j.wneu.2016.10.056. [DOI] [PubMed] [Google Scholar]
- 14.Tay KS, Bassi A, Yeo W, Yue WM. Associated lumbar scoliosis does not affect outcomes in patients undergoing focal minimally invasive surgery-transforaminal lumbar interbody fusion (MISTLIF) for neurogenic symptoms-a minimum 2-year follow-up study. Spine J. 2017;17:34. doi: 10.1016/j.spinee.2016.05.022. [DOI] [PubMed] [Google Scholar]
- 15.Bakhsheshian J, Khanna R, Choy W, Lawton CD, Nixon AT, Wong AP, Koski TR, Liu JC, Song JK, Dahdaleh NS, Smith ZA, Fessler RG. Incidence of graft extrusion following minimally invasive transforaminal lumbar interbody fusion. J Clin Neurosci. 2016;24:88–93. doi: 10.1016/j.jocn.2015.09.005. [DOI] [PubMed] [Google Scholar]
- 16.••.Wong AP, Smith ZA, Nixon AT, Lawton CD, Dahdaleh NS, Wong RH, et al. Intraoperative and perioperative complications in minimally invasive transforaminal lumbar interbody fusion: a review of 513 patients. J Neurosurg Spine. 2015;22:487–495. doi: 10.3171/2014.10.SPINE14129. [DOI] [PubMed] [Google Scholar]
- 17.Giorgi H, Prébet R, Delhaye M, Aurouer N, Mangione P, Blondel B, Tropiano P, Fuentes S, Parent HF. Minimally invasive posterior transforaminal lumbar interbody fusion: one-year postoperative morbidity, clinical and radiological results of a prospective multicenter study of 182 cases. Orthop Traumatol Surg Res. 2015;101:S241–S245. doi: 10.1016/j.otsr.2015.07.001. [DOI] [PubMed] [Google Scholar]
- 18.Klingler J-H, Volz F, Krüger MT, Kogias E, Rölz R, Scholz C, et al. Accidental durotomy in minimally invasive transforaminal lumbar interbody fusion: frequency, risk factors, and management. ScientificWorldJournal. 2015;2015:532628. doi: 10.1155/2015/532628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Scheer JK, Khanna R, Lopez AJ, Fessler RG, Koski TR, Smith ZA, Dahdaleh NS. The concave versus convex approach for minimally invasive lateral lumbar interbody fusion for thoracolumbar degenerative scoliosis. J Clin Neurosci. 2015;22:1588–1593. doi: 10.1016/j.jocn.2015.05.004. [DOI] [PubMed] [Google Scholar]
- 20.Park Y, Lee SB, Seok SO, Jo BW, Ha JW. Perioperative surgical complications and learning curve associated with minimally invasive transforaminal lumbar interbody fusion: a single-institute experience. Clin Orthop Surg. 2015;7:91–96. doi: 10.4055/cios.2015.7.1.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Eckman WW, Hester L, McMillen M. Same-day discharge after minimally invasive transforaminal lumbar interbody fusion: a series of 808 cases. Clin Orthop Relat Res. 2014;472:1806–1812. doi: 10.1007/s11999-013-3366-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Park Y, Ha JW, Lee YT, Sung NY. Minimally invasive transforaminal lumbar interbody fusion for spondylolisthesis and degenerative spondylosis: 5-year results. Clin Orthop Relat Res. 2014;472:1813–1823. doi: 10.1007/s11999-013-3241-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Perez-Cruet MJ, Hussain NS, White GZ, Begun EM, Collins RA, Fahim DK, Hiremath GK, Adbi FM, Yacob SA. Quality-of-life outcomes with minimally invasive transforaminal lumbar interbody fusion based on long-term analysis of 304 consecutive patients. Spine. 2014;39:E191–E198. doi: 10.1097/BRS.0000000000000078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Smith ZA, Sugimoto K, Lawton CD, Fessler RG. Incidence of lumbar spine pedicle breach after percutaneous screw fixation: a radiographic evaluation of 601 screws in 151 patients. J Spinal Disord Tech. 2014;27:358–363. doi: 10.1097/BSD.0b013e31826226cb. [DOI] [PubMed] [Google Scholar]
- 25.Wang J, Zhou Y. Perioperative complications related to minimally invasive transforaminal lumbar fusion: evaluation of 204 operations on lumbar instability at single center. Spine J. 2014;14:2078–2084. doi: 10.1016/j.spinee.2013.12.016. [DOI] [PubMed] [Google Scholar]
- 26.Wong AP, Shih P, Smith TR, Slimack NP, Dahdaleh NS, Aoun SG, el Ahmadieh TY, Smith ZA, Scheer JK, Koski TR, Liu JC, Fessler RG. Comparison of symptomatic cerebral spinal fluid leak between patients undergoing minimally invasive versus open lumbar foraminotomy, discectomy, or laminectomy. World Neurosurg. 2014;81:634–640. doi: 10.1016/j.wneu.2013.11.012. [DOI] [PubMed] [Google Scholar]
- 27.Kim M-C, Chung H-T, Cho J-L, Kim D-J, Chung N-S. Subsidence of polyetheretherketone cage after minimally invasive transforaminal lumbar interbody fusion. J Spinal Disord Tech. 2013;26:87–92. doi: 10.1097/BSD.0b013e318237b9b1. [DOI] [PubMed] [Google Scholar]
- 28.Lau D, Ziewacz J, Park P. Minimally invasive transforaminal lumbar interbody fusion for spondylolisthesis in patients with significant obesity. J Clin Neurosci. 2013;20:80–83. doi: 10.1016/j.jocn.2012.07.004. [DOI] [PubMed] [Google Scholar]
- 29.Silva PS, Pereira P, Monteiro P, Silva PA, Vaz R. Learning curve and complications of minimally invasive transforaminal lumbar interbody fusion. Neurosurg Focus. 2013;35:E7. doi: 10.3171/2013.5.FOCUS13157. [DOI] [PubMed] [Google Scholar]
- 30.Singh K, Nandyala SV, Marquez-Lara A, Cha TD, Khan SN, Fineberg SJ, Pelton MA. Clinical sequelae after rhBMP-2 use in a minimally invasive transforaminal lumbar interbody fusion. Spine J. 2013;13:1118–1125. doi: 10.1016/j.spinee.2013.07.028. [DOI] [PubMed] [Google Scholar]
- 31.Kim M-C, Chung H-T, Cho J-L, Kim D-J, Chung N-S. Factors affecting the accurate placement of percutaneous pedicle screws during minimally invasive transforaminal lumbar interbody fusion. Eur Spine J. 2011;20:1635–1643. doi: 10.1007/s00586-011-1892-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rouben D, Casnellie M, Ferguson M. Long-term durability of minimal invasive posterior transforaminal lumbar interbody fusion: a clinical and radiographic follow-up. J Spinal Disord Tech. 2011;24:288–296. doi: 10.1097/BSD.0b013e3181f9a60a. [DOI] [PubMed] [Google Scholar]
- 33.Matsumoto M, Hasegawa T, Ito M, Aizawa T, Konno S, Yamagata M, Ebara S, Hachiya Y, Nakamura H, Yagi S, Sato K, Dezawa A, Yoshida M, Shinomiya K, Toyama Y, Shimizu K, Nagata K. Incidence of complications associated with spinal endoscopic surgery: nationwide survey in 2007 by the committee on spinal endoscopic surgical skill qualification of Japanese Orthopaedic Association. J Orthop Sci. 2010;15:92–96. doi: 10.1007/s00776-009-1428-6. [DOI] [PubMed] [Google Scholar]
- 34.Rosen DS, Ferguson SD, Ogden AT, Huo D, Fessler RG. Obesity and self-reported outcome after minimally invasive lumbar spinal fusion surgery. Neurosurgery. 2008;63:956–960. doi: 10.1227/01.NEU.0000313626.23194.3F. [DOI] [PubMed] [Google Scholar]
- 35.Pereira C, Santos Silva P, Cunha M, Vaz R, Pereira P. How does minimally invasive transforaminal lumbar interbody fusion influence lumbar radiologic parameters? World Neurosurg. 2018;116:e895–e902. doi: 10.1016/j.wneu.2018.05.125. [DOI] [PubMed] [Google Scholar]
- 36.Ahn J, Massel DH, Mayo BC, Hijji FY, Narain AS, Aboushaala K, Bohl DD, Elboghdady IM, DiBattista JV, Singh K. The utility of routinely obtaining postoperative laboratory studies following a minimally invasive transforaminal lumbar interbody fusion. Clin Spine Surg. 2017;30:E1405–E1410. doi: 10.1097/BSD.0000000000000459. [DOI] [PubMed] [Google Scholar]
- 37.Kukreja S, Haydel J, Nanda A, Sin AH. Impact of body habitus on fluoroscopic radiation emission during minimally invasive spine surgery. J Neurosurg Spine. 2015;22:211–218. doi: 10.3171/2014.10.SPINE14163. [DOI] [PubMed] [Google Scholar]
- 38.Ahn J, Bohl DD, Elboghdady I, Aboushaala K, Mayo BC, Hassanzadeh H, Singh K. Postoperative narcotic consumption in Workman’s compensation patients following a minimally invasive transforaminal lumbar interbody fusion. Spine. 2015;40:1284–1288. doi: 10.1097/BRS.0000000000000994. [DOI] [PubMed] [Google Scholar]
- 39.Siemionow K, Pelton MA, Hoskins JA, Singh K. Predictive factors of hospital stay in patients undergoing minimally invasive transforaminal lumbar interbody fusion and instrumentation. Spine. 2012;37:2046–2054. doi: 10.1097/BRS.0b013e31825c6688. [DOI] [PubMed] [Google Scholar]
- 40.Tian N-F, Wu YS, Zhang XL, Xu HZ, Chi YL, Mao FM. Minimally invasive versus open transforaminal lumbar interbody fusion: a meta-analysis based on the current evidence. Eur Spine J. 2013;22:1741–1749. doi: 10.1007/s00586-013-2747-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wu RH, Fraser JF, Härtl R. Minimal access versus open transforaminal lumbar interbody fusion: meta-analysis of fusion rates. Spine. 2010;35:2273–2281. doi: 10.1097/BRS.0b013e3181cd42cc. [DOI] [PubMed] [Google Scholar]
- 42.Goldstein CL, Macwan K, Sundararajan K, Rampersaud YR. Comparative outcomes of minimally invasive surgery for posterior lumbar fusion: a systematic review. Clin Orthop Relat Res. 2014;472:1727–1737. doi: 10.1007/s11999-014-3465-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Foley KT, Gupta SK. Percutaneous pedicle screw fixation of the lumbar spine: preliminary clinical results. J Neurosurg. 2002;97:7–12. doi: 10.3171/spi.2002.97.1.0007. [DOI] [PubMed] [Google Scholar]
- 44.Mobbs RJ, Sivabalan P, Li J. Minimally invasive surgery compared to open spinal fusion for the treatment of degenerative lumbar spine pathologies. J Clin Neurosci. 2012;19:829–835. doi: 10.1016/j.jocn.2011.10.004. [DOI] [PubMed] [Google Scholar]
- 45.Scheer JK, Harvey MJ, Dahdaleh NS, Smith ZA, Fessler RG. K-wire fracture during minimally invasive transforaminal lumbar interbody fusion: report of six cases and recommendations for avoidance and management. Surg Neurol Int. 2014;5:S520–S522. doi: 10.4103/2152-7806.148009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Patel N, Bagan B, Vadera S, Maltenfort MG, Deutsch H, Vaccaro AR, Harrop J, Sharan A, Ratliff JK. Obesity and spine surgery: relation to perioperative complications. J Neurosurg Spine. 2007;6:291–297. doi: 10.3171/spi.2007.6.4.1. [DOI] [PubMed] [Google Scholar]
- 47.•.Xie Q, et al. Minimally invasive versus open Transforaminal lumbar Interbody fusion in obese patients: a meta-analysis. BMC Musculoskelet Disord. 2018;19:15. doi: 10.1186/s12891-018-1937-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Avila MJ, Walter CM, Baaj AA. Outcomes and complications of minimally invasive surgery of the lumbar spine in the elderly. Cureus. 2016;8:e519. doi: 10.7759/cureus.519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Fujita T, Kostuik JP, Huckell CB, Sieber AN. Complications of spinal fusion in adult patients more than 60 years of age. Orthop Clin North Am. 1998;29:669–678. doi: 10.1016/S0030-5898(05)70040-7. [DOI] [PubMed] [Google Scholar]
- 50.Dakwar E, Cardona RF, Smith DA, Uribe JS. Early outcomes and safety of the minimally invasive, lateral retroperitoneal transpsoas approach for adult degenerative scoliosis. Neurosurg Focus. 2010;28:E8. doi: 10.3171/2010.1.FOCUS09282. [DOI] [PubMed] [Google Scholar]
- 51.Phillips FM, Isaacs RE, Rodgers WB, Khajavi K, Tohmeh AG, Deviren V, Peterson MD, Hyde J, Kurd M. Adult degenerative scoliosis treated with XLIF: clinical and radiographical results of a prospective multicenter study with 24-month follow-up. Spine. 2013;38:1853–1861. doi: 10.1097/BRS.0b013e3182a43f0b. [DOI] [PubMed] [Google Scholar]
- 52.Castro C, Oliveira L, Amaral R, Marchi L, Pimenta L. Is the lateral transpsoas approach feasible for the treatment of adult degenerative scoliosis? Clin Orthop Relat Res. 2014;472:1776–1783. doi: 10.1007/s11999-013-3263-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Rahman M, Summers LE, Richter B, Mimran RI, Jacob RP. Comparison of techniques for decompressive lumbar laminectomy: the minimally invasive versus the ‘classic’ open approach. Minim Invasive Neurosurg. 2008;51:100–105. doi: 10.1055/s-2007-1022542. [DOI] [PubMed] [Google Scholar]
- 54.Mobbs RJ, Li J, Sivabalan P, Raley D, Rao PJ. Outcomes after decompressive laminectomy for lumbar spinal stenosis: comparison between minimally invasive unilateral laminectomy for bilateral decompression and open laminectomy: clinical article. J Neurosurg Spine. 2014;21:179–186. doi: 10.3171/2014.4.SPINE13420. [DOI] [PubMed] [Google Scholar]
- 55.Montano N, Stifano V, Papacci F, Mazzucchi E, Fernandez E. Minimally invasive decompression in patients with degenerative spondylolisthesis associated with lumbar spinal stenosis. Report of a surgical series and review of the literature. Neurol Neurochir Pol. 2018;52:448–458. doi: 10.1016/j.pjnns.2018.06.004. [DOI] [PubMed] [Google Scholar]
- 56.Rasouli MR, Rahimi-Movaghar V, Shokraneh F, Moradi-Lakeh M, Chou R. Minimally invasive discectomy versus microdiscectomy/open discectomy for symptomatic lumbar disc herniation. Cochrane Database Syst Rev. 2014;9:CD010328. 10.1002/14651858.CD010328. [DOI] [PMC free article] [PubMed]
- 57.Grossbach AJ, Dahdaleh NS, Abel TJ, Woods GD, Dlouhy BJ, Hitchon PW. Flexion-distraction injuries of the thoracolumbar spine: open fusion versus percutaneous pedicle screw fixation. Neurosurg Focus. 2013;35:E2. doi: 10.3171/2013.6.FOCUS13176. [DOI] [PubMed] [Google Scholar]
- 58.Tian F, et al. Percutaneous versus open pedicle screw instrumentation in treatment of thoracic and lumbar spine fractures: a systematic review and meta-analysis. Medicine (Baltimore) 2018;97:e12535. doi: 10.1097/MD.0000000000012535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wang B, Fan Y, Dong J, Wang H, Wang F, Liu Z, Liu H, Feng Y, Chen F, Huang Z, Chen R, Lei W, Wu Z. A retrospective study comparing percutaneous and open pedicle screw fixation for thoracolumbar fractures with spinal injuries. Medicine (Baltimore) 2017;96:e8104. doi: 10.1097/MD.0000000000008104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Zhao Q, Zhang H, Hao D, Guo H, Wang B, He B. Complications of percutaneous pedicle screw fixation in treating thoracolumbar and lumbar fracture. Medicine (Baltimore) 2018;97:e11560. doi: 10.1097/MD.0000000000011560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Sclafani JA, Kim CW. Complications associated with the initial learning curve of minimally invasive spine surgery: a systematic review. Clin Orthop Relat Res. 2014;472:1711–1717. doi: 10.1007/s11999-014-3495-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Lee JC, Jang H-D, Shin B-J. Learning curve and clinical outcomes of minimally invasive transforaminal lumbar interbody fusion: our experience in 86 consecutive cases. Spine. 2012;37:1548–1557. doi: 10.1097/BRS.0b013e318252d44b. [DOI] [PubMed] [Google Scholar]