Abstract
Purpose of Review
To review the relevant literature and techniques regarding arthroscopic and open treatment of femoroacetabular impingement (FAI). To discuss both the senior authors’ preferred method of arthroscopic and open treatment of FAI.
Recent Findings
Routine treatment of FAI has moved away from open techniques and is more focused arthroscopic methods. Arthroscopic treatment of FAI has more recently focused on differing techniques of hip access and capsular management. Open techniques still have a role in FAI, but indications for open management are focused on cases with more severe pathology.
Summary
While arthroscopic techniques have shown better outcomes in the short term and higher return to play, it is not without risk and is a procedure with a steep learning curve. In cases of complex joint pathology, such as FAI coupled with dysplasia or Legg-Calve-Perthes, arthroscopy may be not indicated and an open approach preferred. We outline various techniques for both arthroscopic and open treatment of FAI and their outcomes when possible.
Keywords: Osteoplasty, Osteochondroplasty, Femoroacetabular impingement, Surgical hip dislocation, Hip arthroscopy
Introduction
Femoroacetabular impingement (FAI), first described by Ganz in 2001 [1], is a condition in which anatomic abnormalities of the femoral head (CAM lesion) and/or acetabular rim (pincer lesion) result in contact between the two during hip range motion leading to cartilage and labral damage, pain, and early hip osteoarthritis [2]. The cam deformity is defined by a femoral head-neck junction asphericity and decreased offset.
Numerous studies have examined the etiology of cam deformities as they are incidentally noted in about 15–25% of the asymptomatic population [3–5]. Although not completely understood, the development of cam deformities is multifactorial. Evidence suggests that idiopathic cam deformity develops during adolescence with modifications of the capital femoral epiphysis in response to prolonged vigorous athletic participation. Elongation of the femoral head physis has been seen in high level athletes including basketball, soccer, and hockey [3]. These athletes have been followed in their adolescent years and significant increases in the alpha angle can be noted before and after physeal closure.
While primary or idiopathic deformity develops from a variety of intrinsic and extrinsic factors, it is important to recognize secondary cam deformity due to other pathologic causes. The most common of these causes are Legg-Calve-Perthes disease (LCPD), slipped capital femoral epiphysis (SCFE), and deformities arising from trauma, infection, or osteoarthritis. These deformities may require a more vigilant workup and can sometimes be difficult to treat with standard arthroscopic techniques and necessitate and open approach.
Advancements in hip arthroscopy have shown good to excellent results in treating cam deformities with femoral osteoplasty. The surgeon must be mindful to correct the entire deformity, regardless of the technique used. Numerous studies have reported that the largest risk factor for revision hip arthroscopy is inadequate resection of the cam deformity when treating femoral-sided lesions [6–12].
Regardless of the technical approach, it is imperative to obtain adequate visualization of the cam lesion in order to perform a thorough cam decompression. Many techniques for capsular management during hip arthroscopy have been described to ensure satisfactory visualization. Some techniques prioritize the benefits of maintaining the biomechanical function of the iliofemoral ligament (IFL), while other approaches highlight adequate visualization and access to the entire cam lesion. These capsulotomy techniques will be described along with their strengths and weaknesses.
Capsulotomy Techniques
Extracapsular Capsulotomy
Under fluoroscopy and using anatomic landmarks of the ASIS and greater trochanter, standard anterolateral (AL), mid-anterior (MA), and distal anterolateral (DALA) portals are marked out in an equilateral triangle roughly 6 cm apart. After skin incision, a 30° arthroscope is introduced through the AL portal onto the femoral neck and into the pericapsular fat. A dissector is introduced through the MA portal and the pericapsular fat is dissected off of the capsule between the gluteus minimus, iliocapsularis, and vastus lateralis to expose the reflected head of rectus femoris tendon. Adhesions between the rectus tendon and capsule are removed using a radiofrequency ablation wand. The capsulotomy is performed parallel to the fibers of the IFL at the 12 o’clock position. Dissection through the capsule is continued until the labrum is exposed medially and through the zona laterally. Once the labrum is visible, traction is applied to access the central compartment.
The advantages of extracapsular capsulotomy are minimal violation of the IFL fibers. Biomechanical studies have reported the importance of the IFL in distraction, extension, and anterior translation [13, 14]. This technique may also offer a shorter rehabilitation period. The clinical significance and advantages of extracapsular capsulotomy in comparison to other techniques remains unclear.
The disadvantages to this technique mainly consist of inadequate visualization of the cam lesion. In one study, 17 of 100 cases required extension of the capsulotomy to an L or T shape to visualize the entire deformity [15•].
Interportal Capsulotomy
Similarly, under fluoroscopy and using anatomic landmarks, standard AL, MA, and DALA portals are marked out in an equilateral triangle roughly 6 cm apart. Traction is applied to distract the hip joint and fluoroscopy is used to ensure adequate distraction. A spinal needle is introduced through the AL portal into the joint and an air arthrogram is performed to ensure correct positioning. A nitinol wire is passed through the spinal needle and the scope sheath and blunt trocar is introduced over the nitinol wire and into the hip joint. Under direct visualization with a 70° arthroscope, the MA portal is then established. Surgeon’s preference of an arthroscopic knife or radiofrequency ablation probe can be used to carry out the capsulotomy. The capsulotomy is started from the MA portal and divided toward the AL portal. The arthroscope is switched into the MA portal and the ablation probe or knife is placed in the AL portal to complete the capsulotomy between the two portals. Once work in the central compartment is completed, traction is then discontinued and the osteoplasty is performed.
Advantages of this technique are a better visualization of the femoral head and neck to complete the osteoplasty, although in order to adequately achieve this, one must be comfortable manipulating the leg position to fully visualize and access the entire cam lesion. Disadvantages consist of violation of the IFL with theoretical risks of instability, although studies have shown repair of the capsulotomy restores joint stability [16•]. Other studies have noted increased heterotopic ossification associated with extensive capsule violation [17]. It is the author’s preference to perform an interportal capsulotomy [18•].
T-type Capsulotomy
The T-capsulotomy is an extension of the interportal capsulotomy [19•]. After completion of the interportal capsulotomy and the central compartment portion of the procedure is completed, the 70° arthroscope is moved into the peripheral compartment. The iliocapsularis is dissected off the IFL and the center of the femoral neck is identified. Similar to the extracapsular capsulotomy, a knife or radiofrequency ablation probe is used to create a capsulotomy parallel to the IFL fibers. A switching stick or retraction sutures can be used to manipulate the capsule to improve visualization [20].
The T-type technique provides the advantage of the largest exposure of the cam deformity. The same risks of capsular instability and defects associated with the interportal capsulotomy are largely the same with this technique [20].
Other Capsulotomy Techniques
The periportal or puncture capsulotomies have also been described and minimize take down of the capsule [21•, 22•]. These techniques require some expansion of the portals or slight debridement of the articular side of the capsule in order to improve visualization [21•, 22•]. These techniques may prove to be difficult in large lesions that extend more posterior than the 10 o’clock position.
Author’s Preferred Arthroscopic Osteoplasty Technique
The Trough Takedown Technique
The patient is placed in the supine position on either a post (Smith and Nephew) or a post-free traction table (Pivot Guardian Distraction System, Stryker). Distraction is placed and hip access is gained under fluoroscopy visualization using AL, MA, and DALA portals.
The interportal capsulotomy is performed as described above to gain access to the central compartment. Any central compartment pathology is addressed at this time and traction is discontinued to gain access to the peripheral compartment. Extracapsular fat is resected at this time to facilitate capsular closure at the end of the procedure. Adequate hemostasis and visualization are also performed preceding the osteoplasty. T-capsulotomy is not routinely done but can be considered if the cam lesion cannot be adequately visualized.
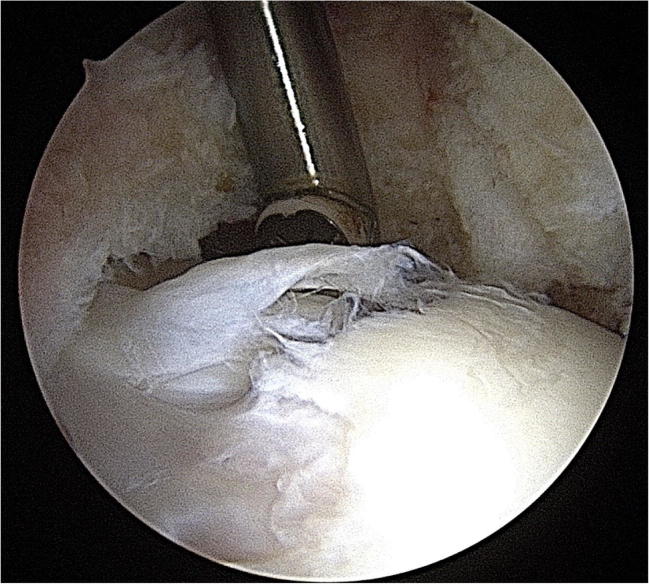
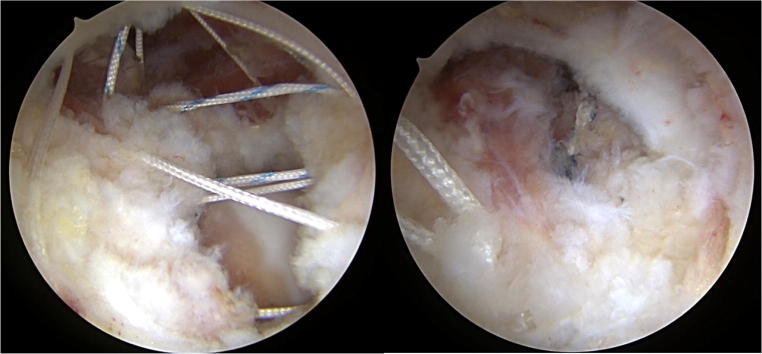
A 70° arthroscope is positioned in the anterolateral portal and is maintained in this position for the extent of the osteoplasty. Preoperative radiographs including an AP weight-bearing pelvis, modified false profile, and frog leg lateral are used to identify the extent of the cam deformity, and intraoperative fluoroscopy is used to confirm the findings. Intraoperative radiographs are also used to follow the progression of cam resection during the procedure. The cam deformity is identified with the arthroscope, as the lesion has a characteristic pattern of discoloration, surface fraying and occasionally a cartilage peel-off appearance in comparison to healthy cartilage (Fig. 1). The head may also have pathognomonic impingement signs of fibrocystic or sclerotic changes.
Fig. 1.
Direct Visualization of Cam Deformity
The hip is then flexed to 45° in neutral rotation to relax the capsule and visualize the deformity. Medial and lateral synovial folds are recognized as landmarks for the extent of the resection as to not damage the retinacular vessels. The soft tissue along the medial aspect of the cam is defined and electrocautery is used to clear the soft tissue from the deformity.
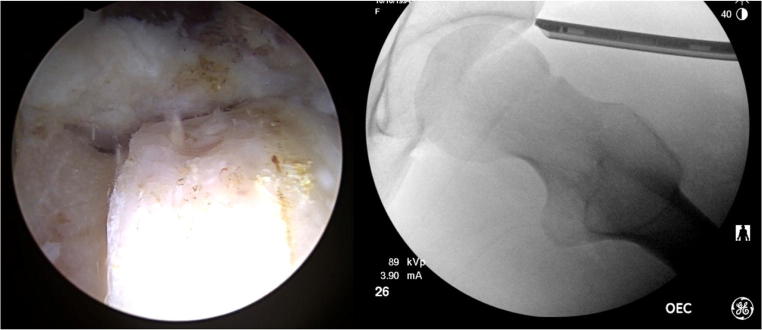
Using an arthroscopic burr, a trough is created approximately 8–10 mm away from the defined head neck junction (Fig. 2). The depth of the trough can be guided by pre-operative radiographs and intra-operative fluoroscopy. The subchondral sclerosis in the region of the cam lesion can also help guide the resection depth. By resecting the sclerotic bone in the region of the cam lesion, the shape can be restored to within submillimeter differences of normal hips. One study showed no difference in shape between cam deformity and normal hips when sclerosis was used as a guide for resection [23•]. This technique provides a reliable intraoperative boundary for the extent of cam resection. The trough is carried down inferiorly and superiorly through the entire lesion width and parallels the previously defined edge of the femoral head articular cartilage. Fluoroscopy may be used to ensure proper trough resection and placement (Fig. 2).
Fig. 2.
Arthroscopic and Fluoroscopic appearance of the Trough
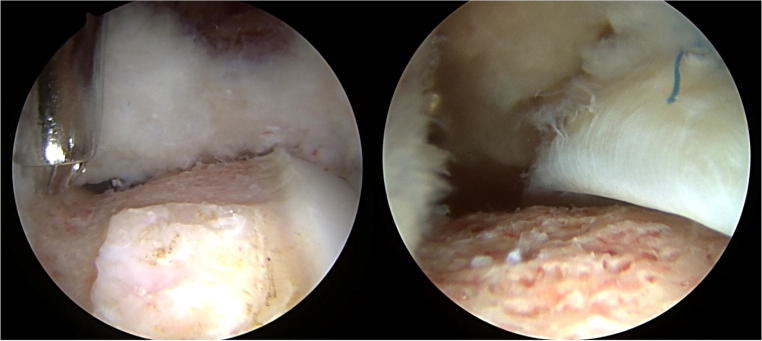
After adequate trough resection has been performed, the medially defined border is blended into the trough to create a smooth, contoured resection mimicking normal hip anatomy (Fig. 3). This is carried out from the inferior portion of resection to more superior and posterior being mindful of the retinacular vessels lying adjacent to the resection. Dynamic examination can be performed at this time to ensure clearance of the femoral head into the central compartment (Fig. 3). The hip is taken into 90° or more of flexion and rotated while the arthroscope is directly visualizing the labral rim. If impingement is still noted, the leg is brought back down and further resection is performed.
Fig. 3.
Arthroscopic View of Medial Cam Takedown and Dynamic Exam with Showing Proper Amount of Cam Resection
Once the medial osteoplasty is complete, the lateral bony deformity is then resected (Fig. 4). This is done with the hip in about 30–45° of flexion to allow for maximal capsular relaxation. The lateral prominence is blended to the extent of the trough resection to create a smooth, contoured neck to restore head-neck offset (Fig. 4).
Fig. 4.
Lateral Cam Takedown and Restoration of Head-Neck Offset
After completion of treating all central and peripheral compartment pathology, the capsule is closed. Three to four #2 non-absorbable sutures are passed using a Slingshot (Stryker - Kalamazoo, MI) with a figure of eight technique [18•]. This is done through the anterior portal using a cannula. After one suture is passed, the strands are brought outside of the cannula without being tied and the next figure of eight is performed. After passing all sutures, the sutures are individually tied using a sliding arthroscopic knot and backing half-hitches to ensure a water-tight capsular closure (Fig. 5).
Fig. 5.
Placement of “Figure of 8” Stitches and Resultant Water-Tight Capsular Closure
Technical Pearls
If visualization of the entire cam deformity is difficult, the interportal capsulotomy can be extended. It is better to extend a capsulotomy than to damage the capsule with instruments. Alternatively, conversion to T-capsulotomy will also improve exposure of the entire lesion.
When utilizing an interportal capsulotomy technique, the superolateral and anterior cam deformity is better visualized with the leg in extension. The inferomedial and lateral cam deformity is better visualized with the leg in flexion.
Arthroscopic techniques provide minimally invasive approaches to treating the majority of cam deformities. For large lesions due to secondary pathology, open approaches may be better utilized to correct the deformity.
Open Techniques
While there are advantages and disadvantages to the open and arthroscopic approach to FAI, many reports have seemingly equal patient reported outcomes when done in the hands of experts [24•, 25•, 26•, 27•]. Advantages to the open procedure mainly include the nearly 360° access to the hip joint. While the arthroscopic approach can address the more commonly located anterolateral cam deformity, complex cases extending beyond this especially to the more posterior aspect necessitate an open approach to navigate the vasculature of the femoral head to minimize the risk of postoperative osseous necrosis [28]. Further, the open technique is usually performed with the aid of spherical guides ensuring a perfect circular reshaping of the proximal femur, which is especially helpful in complex deformity as in the case of Legg-Calve-Perthes disease or post traumatic deformity. An open technique is more amendable to cartilage procedures of the femoral head and acetabulum [29–31]. However major disadvantages exist with an open technique. During a surgical hip dislocation, a trochanteric osteotomy is performed and is a risk for nonunion and revision surgery [32•]. Additionally, the ligamentum teres must be sacrificed which some have advocated plays a role in stability of the hip [33–35]. Finally, surgical hip dislocation is significantly more morbid with more extensive soft tissue disruption accompanied by increased scar formation, inpatient hospital stays, and longer rehabilitation after surgery [24•, 25•, 26•, 27•].
Modern Indications of Open Osteoplasty
Hip Dysplasia with Concomitant Femoroacetabular Impingement
Periacetabular osteotomy was initially developed by Ganz and has been shown in several long-term studies to be a successful operation in the treatment of hip dysplasia [36–40]. However, it has been shown by multiple authors that hip dysplasia does not always occur in isolation [41•, 42•, 43•]. In particular, he has been described that a combination of hip dysplasia with a cam type deformity may coexist in up to 75% in some cohorts [41•, 44•, 45]. Abnormalities of the femoral head and neck are common in patients with hip dysplasia. Unaddressed femoral acetabular impingement is also a frequent mechanism of failure following periacetabular osteotomy [46, 47]. Performing a cam osteoplasty in combination with periacetabular osteotomy has been shown to be safe and does not result in increased complications. This can be performed either arthroscopically or open. There are arguments that performing an arthroscopic osteoplasty will allow for better visualization of other intra-articular structures.
When performing a combined periacetabular osteotomy and cam decompression often the osteotomy is performed first. The surgeon then can assess range of motion deficits. If limited range of motion is detected after acetabular correction, specifically flexion and internal rotation, an open osteoplasty is indicated. To perform an osteoplasty decompression, the Smith-Peterson approach is extended distally and a capsulotomy is performed to expose the head-neck junction. As previously described above in the mini-open approach, the cam lesion is excised.
Proximal Femoral Deformities
Legg-Cave-Perthes (LCP) is a childhood disorder resulting in idiopathic femoral head osseous necrosis [48]. LCP can result in proximal femoral and acetabular changes resulting in pain, early osteoarthritis, femoroacetabular impingement, and abductor weakness resulting in significant disability [48, 49]. Imaging may demonstrate coxa magna, coxa vara, a shortened or widened femoral neck, trochanteric overgrowth, and acetabular changes such as dysplasia or retroversion [50]. These resultant deformities can result in complex intra-articular and extra-articular pathology [43, 49].
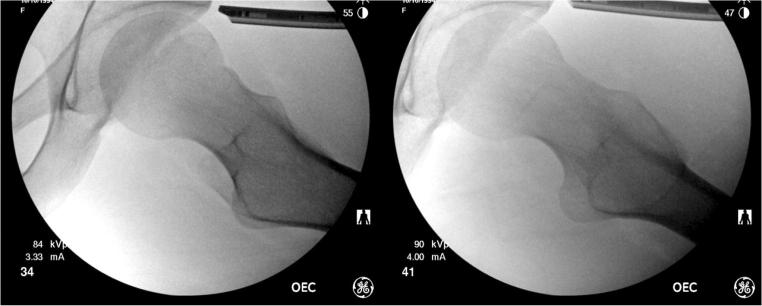
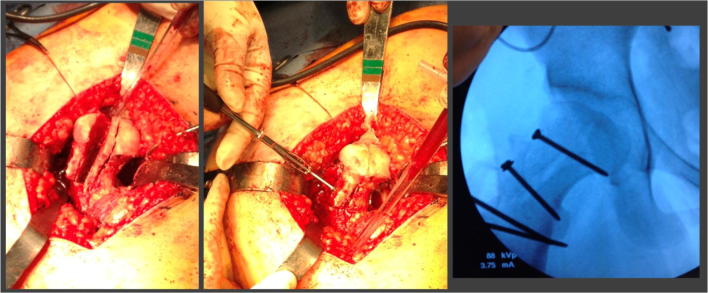
An open surgical hip dislocation is often indicated to address difficult pathology and is sometimes performed concomitantly with acetabular reorientation. Surgical hip dislocation allows access to address those structures contributing to both intra and extraarticular impingement. Further, it allows superb assessment of impinging structures through direct visualization. For intra-articular impingement, an open surgical dislocation provides access to perform an osteoplasty to address cam impingement, femoral head reduction (Fig. 6) for the treatment of coxa magna, as well as femoral osteotomy to address femoral version. For extra-articular impingement, relative femoral neck lengthening can decrease impingement from trochanteric overgrowth as well as optimize abductor biomechanics [28, 51]. Relative femoral neck lengthening involves creating an extended retinacular artery flap thereby separating the vessels from the proximal greater trochanter and femoral neck allowing debridement and distal translation of the osteotomized greater trochanter [28, 51].
Fig. 6.
Intraoperative and Fluoroscopic images of Femoral Head Reduction for Coxa Magna
Slipped Capital Femoral Epiphysis (SCFE)
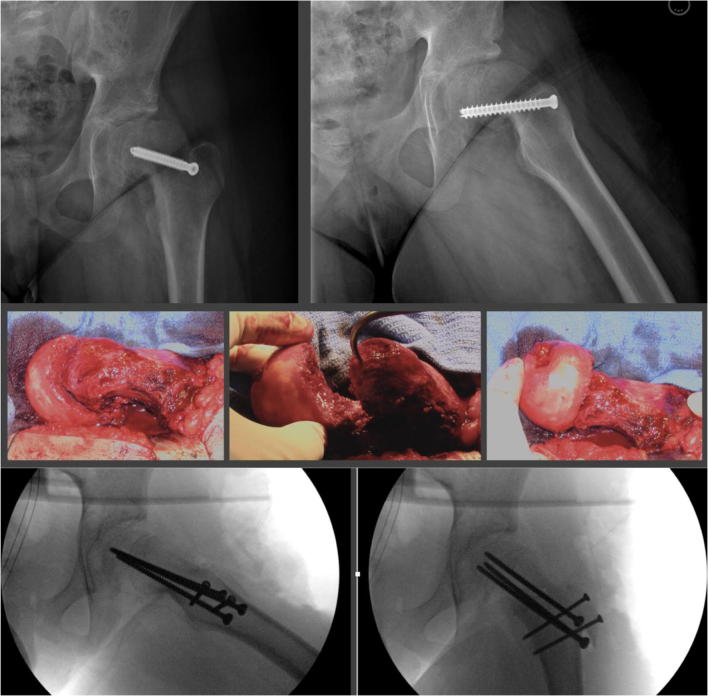
Relatively common in adolescents, SCFE is a condition of the femoral head in which there is pathologic translation through the growth plate [52, 53]. Initial treatment goals consist of stabilizing the epiphysis with in situ pinning. However, the SCFE deformity can lead to early, persistent femoroacetabular impingement and chondral injury in these patients [54–56]. While arthroscopic treatment is successful in lower grade slips, surgical hip dislocation is indicated in more severe deformities. For severe slips, Ganz et al. developed a modified Dunn technique to realign the epiphysis and minimize the post slip deformity that can cause further damage to the joint. This procedure involves creating an extended lateral retinacular flap to maintain blood supply while mobilizing the head under direct visualization, slightly reducing the neck length to avoid tension on the vessels, and pinning the fragment in place (Fig. 7). While this technique is relatively new, the results are pending and involve a steep learning curve.
Fig. 7.
Preoperative, intraoperative and final fixation of SCFE correction
Author’s Preferred Technique for Surgical Hip Dislocation with “Z Capsulotomy”
The patient is placed in the lateral decubitus position on a standard OR table. The use of hip positioners or a pegboard is helpful to stabilize the pelvis. The sterile field spans from the inferior thorax superiorly and the posterior superior iliac spine posteriorly, extending distally to the operative leg, which is prepped free into the sterile field allowing dynamic range of motion assessment during the procedure.
An incision centered over the greater trochanter approximately 20 cm in length is made. Dissection is carried down to the level of the fascia lata. The fascia lata is incised sharply. Care is taken to split the gluteus maximus bluntly and minimize muscular damage; distally the iliotibial band is sharply incised. This interval is held open with a Charnley retractor. The greater trochanter is palpated and a plane is made bluntly underneath the cephalad portion of the vastus lateralis usually with the use of a Cobb elevator. The cephalad border of the piriformis tendon is identified and care is taken to dissect just cephalad, elevating and preserving the gluteus medius and minimus attachments and developing a plane in between the gluteus minimus and the hip capsule. Once these planes are developed, the osteotomy is marked out. We take care to plan the osteotomy so the fragment will be approximately 1.5-cm thick leaving a 5-mm cuff of posterior border of gluteus medius attached to the medial portion of the trochanter which is intact to the femoral shaft. We routinely perform a step cut in the osteotomy as described by Ganz [1, 57, 58]. Once the osteotomy is completed, muscular attachments to the anterior capsule are bluntly elevated.
Once the fragment is mobilized, the anterior capsule is identified and the linear fibers of the iliofemoral ligament of Bigelow are identified. We perform a “Z” capsulotomy to preserve blood supply to the femoral head [1]. We begin the capsulotomy with a sharp incision along the linear fibers of the iliofemoral ligament. The key is to not disrupt the underlying acetabular labrum while performing the capsulotomy. This can be facilitated by applying a traction suture to the superior leaflet and applying traction during the superior limb portion of the “Z” capsulotomy. The inferior limb is also performed sharply taking care not to damage the underlying structures.
Once the capsulotomy is performed, the femoral head is subluxated with the use of a bone hook underneath the femoral neck with application of gentle abduction, flexion and external rotation. Curved scissors are utilized to release the ligamentum teres and the head is dislocated. It is our preference to address the cam morphology first then address any labral or acetabular lesions thereafter.
Once the femoral head is dislocated, the extent of the cam is marked out. We excise the cam preliminarily with the aid of curved osteotomes and then fine contouring is performed with a 5 mm round burr. We prefer to use the aid of spherical templates to help define regions of aspherical morphology.
At this time, any major femoral head cartilage lesions are corrected with either osteochondral autograft or allograft. Once the femoral head cam lesion is recontoured, we then address labral and acetabular pathology. Our preference is to debride unstable chondral lesions, and repair labral tissue with the use of suture anchors when possible.
The femoral head is then reduced. The capsule is closed with the aid of nonabsorbable #2 sutures. The trochanteric osteotomy is then repaired using two or three 3.5-mm cortical screws placed in a lag technique fashion. The fascia lata and wound are then closed in a layered fashion to the surgeon’s preference.
Mini Open Direct Anterior Approach
Parvizi et al. described a mini open technique with the patient positioned supine, while this approach does limit the access to the femoral and acetabular visualization [54].
A 3–4-cm incision over the tensor fascia lata muscle distal to the anterior superior iliac spine is made. The perimysium of the tensor fascia lata is identified and divided. The muscles are retracted laterally and the underlying perimysium is incised to expose the rectus femoris. The rectus is retracted laterally to expose the anterior hip capsule. Blunt retractors are then placed around the capsule, retracting the sartorius medially. If the lateral femoral circumflex is encountered it is ligated. To access the joint, an “I” capsulotomy is made. The anterior femoral head neck junction is then identified. This region can be identified by performing a dynamic exam by flexing and internally rotating the hip and by inspecting the anterior lateral cartilage which often has a reddish hue to define the impingement zone. The cam lesion is excised with the use of curved osteotomes and a pneumatic burr. To protect the weightbearing surface of the femoral head, the operative limb is released so that the head reduces within the acetabulum and the acetabular margin is used as a template for cam excision.
Discussion
Symptomatic pain relief and joint preservation are the surgical goals of FAI treatment. Both hip arthroscopy and open treatment have been well documented to correct the shape mismatch seen in FAI. Boster et al. [27] published a comparative review of open versus arthroscopic studies published prior to 2010 and found both techniques improved patient outcomes; however, elite athletes had a superior return to sporting activities following arthroscopic techniques. Matsuda et al. [59] similarly reviewed studies comparing both techniques published through 2009 and found similar clinical efficacy between both techniques; however, the complication rate for arthroscopy was lower. Nwachukwu et al. [25] performed a systematic review focusing on medium to long-term outcomes and found both techniques showed excellent equivalent outcomes and hip survival with no significant difference between the two techniques, but arthroscopy had a higher Health-Related Quality of Life (HRQoL) score. Zhang et al. [24•] performed a meta-analysis of studies through 2016 and found arthroscopy had significantly more favorable outcomes in Nonarthritic Hip Scores (NAHS) at 3 and 12 months as well as a lower reoperation rate, while open techniques had a significantly greater improved alpha angle measured on Dunn lateral radiographs.
While arthroscopic techniques have shown better outcomes in the short term and higher return to play, it is not without risk and is a procedure with a steep learning curve. In cases of complex joint pathology, such as FAI coupled with dysplasia or Legg-Calve-Perthes, arthroscopy may be not indicated and an open approach preferred. High quality literature that compares both techniques with randomized controlled trials and reports long-term outcomes is lacking. The approach taken to FAI must be individualized to reflect both patient anatomy and preference while at the same time accommodate surgeon comfort and technical skill.
Compliance with Ethical Standards
Conflict of Interest
Alex G. Dukas, Andrew S. Gupta, and Christopher L. Peters declare that they have no conflicts of interest.
Stephen K. Aoki is a paid consultant for Stryker (Kalamazoo, MI).
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on Femoroacetabular impingement/labral tears
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
- 1.Ganz R, Gill TJ, Gautier E, Ganz K, Krügel N, Berlemann U Surgical dislocation of the adult hip: a technique with full access to the f... J Bone Joint Surg Br. 2001. [DOI] [PubMed]
- 2.Ganz R, Parvizi J, Beck M, Leunig M, Notzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res 2003. [DOI] [PubMed]
- 3.Siebenrock KA, Behning A, Mamisch TC, Schwab JM. Growth plate alteration precedes cam-type deformity in elite basketball players. Clin Orthop Relat Res. 2013;471(4):1084–1091. doi: 10.1007/s11999-012-2740-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Anwander H, Beck M, Büchler L. Influence of evolution on cam deformity and its impact on biomechanics of the human hip joint. J Orthop Res. 2018;36(8):2071–2075. doi: 10.1002/jor.23863. [DOI] [PubMed] [Google Scholar]
- 5.Morris WZ, Li RT, Liu RW, Salata MJ, Voos JE. Origin of cam morphology in Femoroacetabular impingement. Am J Sports Med. 2018;46(2):478–486. doi: 10.1177/0363546517697689. [DOI] [PubMed] [Google Scholar]
- 6.Ricciardi BF, Fields K, Kelly BT, Ranawat AS, Coleman SH, Sink EL. Causes and risk factors for revision hip preservation surgery. Am J Sports Med. 2014;42(11):2627–2633. doi: 10.1177/0363546514545855. [DOI] [PubMed] [Google Scholar]
- 7.Kester BS, Capogna B, Mahure SA, Ryan MK, Mollon B, Youm T. Independent risk factors for revision surgery or conversion to total hip arthroplasty after hip arthroscopy: a review of a large statewide database from 2011 to 2012. Arthroscopy. 2018;34(2):464–470. doi: 10.1016/j.arthro.2017.08.297. [DOI] [PubMed] [Google Scholar]
- 8.Woodward RM, Philippon MJ. Persistent or recurrent symptoms after arthroscopic surgery for femoroacetabular impingement: a review of imaging findings. J Med Imaging Radiat Oncol. 2019;63(1):15–24. doi: 10.1111/1754-9485.12822. [DOI] [PubMed] [Google Scholar]
- 9.Heyworth BE, Shindle MK, Voos JE, Rudzki JR, Kelly BT. Radiologic and intraoperative findings in revision hip arthroscopy. Arthroscopy. 2007;23(12):1295–1302. doi: 10.1016/j.arthro.2007.09.015. [DOI] [PubMed] [Google Scholar]
- 10.Bogunovic, Gottlieb, Pashos, Baca, Clohisy. Why do hip arthroscopy procedures fail? Hip. Clin Orthop Relat Res 2013. [DOI] [PMC free article] [PubMed]
- 11.Sardana V, Philippon MJ, De Sa D, Bedi A, Ye L, Simunovic N, et al. Revision hip arthroscopy indications and outcomes: a systematic review. Arthroscopy. 2015;31:2047–2055. doi: 10.1016/j.arthro.2015.03.039. [DOI] [PubMed] [Google Scholar]
- 12.Domb BG, Stake CE, Lindner D, El-Bitar Y, Jackson TJ. Revision hip preservation surgery with hip arthroscopy: clinical outcomes. Arthroscopy. 2014;30:581–7. [DOI] [PubMed]
- 13.Abrams GD, Hart MA, Takami K, Bayne CO, Kelly BT, Espinoza Orías AA, et al. Biomechanical evaluation of capsulotomy, capsulectomy, and capsular repair on hip rotation. Arthroscopy. 2015;31(8):1511–7. [DOI] [PubMed]
- 14.Nepple JJ, Brophy RH, Matava MJ, Wright RW, Clohisy JC. Radiographic findings of femoroacetabular impingement in National Football League Combine athletes undergoing radiographs for previous hip or groin pain. Arthroscopy. 2012;28(10):1396–1403. doi: 10.1016/j.arthro.2012.03.005. [DOI] [PubMed] [Google Scholar]
- 15.Forster-Horvath C, Domb BG, Ashberg L, Herzog RF. A method for capsular management and avoidance of iatrogenic instability: minimally invasive capsulotomy in hip arthroscopy. Arthrosc Tech. 2017;6(2):e397–e400. doi: 10.1016/j.eats.2016.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Weber AE, Neal WH, Mayer EN, Kuhns BD, Shewman E, Salata MJ, Mather RC, Nho SJ. Vertical extension of the T-capsulotomy incision in hip arthroscopic surgery does not affect the force required for hip distraction: effect of capsulotomy size, type, and subsequent repair. Am J Sports Med. 2018;46(13):3127–3133. doi: 10.1177/0363546518800710. [DOI] [PubMed] [Google Scholar]
- 17.Amar E, Warschawski Y, Sampson TG, Atoun E, Steinberg EL, Rath E. Capsular closure does not affect development of heterotopic ossification after hip arthroscopy. Arthroscopy. 2015;31(2):225–230. doi: 10.1016/j.arthro.2014.08.026. [DOI] [PubMed] [Google Scholar]
- 18.Aoki SK, Karns MR, Hananouchi T, Todd DC. Hip arthroscopy capsular closure: the figure of eight technique. Arthrosc Tech. 2017;6(2):e505–e509. doi: 10.1016/j.eats.2016.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.• Ekhtiari S, de Sa D, Haldane CE, Simunovic N, Larson CM, Safran MR, et al. Hip arthroscopic capsulotomy techniques and capsular management strategies: a systematic review. Knee Surg Sport Traumatol Arthrosc. 2017; Reviews capsular management techniques in hip arthroscopy. [DOI] [PubMed]
- 20.Bedi A, Galano G, Walsh C, Kelly BT. Capsular management during hip arthroscopy: from femoroacetabular impingement to instability. Arthroscopy. 2011;27:1720–1731. doi: 10.1016/j.arthro.2011.08.288. [DOI] [PubMed] [Google Scholar]
- 21.• Chambers CC, Monroe EJ, Flores SE, Borak KR, Zhang AL. Periportal capsulotomy: technique and outcomes for a limited capsulotomy during hip arthroscopy. Arthroscopy. 2019; Highlights outcomes and technique of hip arthroscopy with minimal capsular disruption. [DOI] [PubMed]
- 22.Monroe EJ, Chambers CC, Zhang AL. Periportal capsulotomy: a technique for limited violation of the hip capsule during arthroscopy for femoroacetabular impingement. Arthrosc Tech. 2019;8:e205–e208. doi: 10.1016/j.eats.2018.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Aoki SK, Beckmann JT, Wylie JD. Arthroscopic femoral osteochondroplasty for cam-type femoroacetabular impingement: the trough technique. Arthrosc Tech. 2016;5(4):e743–e749. doi: 10.1016/j.eats.2016.02.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.• Zhang D, Chen L, Wang G. Hip arthroscopy versus open surgical dislocation for femoroacetabular impingement: a systematic review and meta-analysis. Medicine (Baltimore). 2016; Outlines outcomes of arthroscopic versus open treatment of FAI. [DOI] [PMC free article] [PubMed]
- 25.Nwachukwu BU, Rebolledo BJ, McCormick F, Rosas S, Harris JD, Kelly BT. Arthroscopic versus open treatment of femoroacetabular impingement. Am J Sports Med 2015; [DOI] [PubMed]
- 26.Büchler L, Neumann M, Schwab JM, Iselin L, Tannast M, Beck M. Arthroscopic versus open cam resection in the treatment of femoroacetabular impingement. Arthroscopy. 2013;29:653–60. [DOI] [PubMed]
- 27.Botser IB, Smith TW, Nasser R, Domb BG. Open surgical dislocation versus arthroscopy for femoroacetabular impingement: a comparison of clinical outcomes. Arthroscopy. 2011;27:270–8. [DOI] [PubMed]
- 28.Ganz R, Huff TW, Leunig M. Extended retinacular soft-tissue flap for intra-articular hip surgery: surgical technique, indications, and results of application. Instr Course Lect 2009; [PubMed]
- 29.Emmerson BC, Görtz S, Jamali AA, Chung C, Amiel D, Bugbee WD. Fresh osteochondral allografting in the treatment of osteochondritis dissecans of the femoral condyle. Am J Sports Med. 2007;35:907–914. doi: 10.1177/0363546507299932. [DOI] [PubMed] [Google Scholar]
- 30.Krych AJ, Lorich DG, Kelly BT. Treatment of focal osteochondral defects of the acetabulum with osteochondral allograft transplantation. Orthopedics. 2011; [DOI] [PubMed]
- 31.Leunig M, Tibor LM, Naal FD, Ganz R, Steinwachs MR. Surgical technique: second-generation bone marrow stimulation via surgical dislocation to treat hip cartilage lesions. Clin Orthop Relat Res. 2012;470:3421–3431. doi: 10.1007/s11999-012-2466-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.• Sink EL, Beaulé PE, Sucato D, Kim YJ, Millis MB, Dayton M, et al. Multicenter study of complications following surgical dislocation of the hip. J Bone Joint Surg Am. 2011; Highlights the complications following Surgical Hip Dislocation;93:1132–6. [DOI] [PubMed]
- 33.Bardakos N V., Villar RN. The ligamentum teres of the adult hip. J Bone Joint Surg (Br) 2008; [DOI] [PubMed]
- 34.Byrd JWT, Jones KS. Traumatic rupture of the ligamentum teres as a source of hip pain. Arthroscopy. 2004;20:385–91. [DOI] [PubMed]
- 35.Canga A, Dobado MC, Llopis E, Pérez-Carro L, Rolón A, Montero JA, et al. Anatomy, biomechanics, imaging, and management of ligamentum teres injuries. RadioGraphics. 2010; [DOI] [PubMed]
- 36.Ganz R, Klaue K, Vinh TS, Mast JW. A new periacetabular osteotomy for the treatment of hip dysplasias. Technique and preliminary results. Clin Orthop Relat Res. 1988;(232):26–36. [PubMed]
- 37.Zhu J, Chen X, Cui Y, Shen C, Cai G. Mid-term results of Bernese periacetabular osteotomy for developmental dysplasia of hip in middle aged patients. Int Orthop. 2013;37(4):589–594. doi: 10.1007/s00264-013-1790-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Peters CL, Erickson JA, Hines JL. Early results of the Bernese periacetabular osteotomy: the learning curve at an academic medical center. J Bone Joint Surg. 2006;88(9):1920. [DOI] [PubMed]
- 39.Matheney T, Kim Y-J, Zurakowski D, Matero C, Millis M. Intermediate to long-term results following the Bernese periacetabular osteotomy and predictors of clinical outcome. J Bone Joint Surg Am. 2010;92(Suppl 1):115–29. [DOI] [PubMed]
- 40.Lerch TD, Steppacher SD, Liechti EF, Tannast M, Siebenrock KA. One-third of hips after periacetabular osteotomy survive 30 years with good clinical results, no progression of arthritis, or conversion to THA. Clin Orthop Relat Res. 2017;475(4):1154–1168. doi: 10.1007/s11999-016-5169-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Goronzy J, Franken L, Hartmann A, Thielemann F, Postler A, Paulus T, Günther KP. What are the results of surgical treatment of hip dysplasia with concomitant cam deformity? Clin Orthop Relat Res. 2017;475(4):1128–1137. doi: 10.1007/s11999-016-5054-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nassif NA, Schoenecker PL, Thorsness R, Clohisy JC. Periacetabular osteotomy and combined femoral head-neck junction osteochondroplasty. J Bone Joint Surg Am. 2012;94(21):1959–66. [DOI] [PubMed]
- 43.Clohisy JC, Nepple JJ, Ross JR, Pashos G, Schoenecker PL. Does surgical hip dislocation and periacetabular osteotomy improve pain in patients with Perthes-like deformities and acetabular dysplasia? Clin Orthop Relat Res. 2015;473:1370–1377. doi: 10.1007/s11999-014-4115-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Anderson LA, Erickson JA, Swann RP, McAlister IP, Anderson MB, Sierra RJ, et al. Femoral morphology in patients undergoing periacetabular osteotomy for classic or borderline acetabular dysplasia: are cam deformities common? J Arthroplast. 2016;31:259–263. doi: 10.1016/j.arth.2016.01.066. [DOI] [PubMed] [Google Scholar]
- 45.Kohno Y, Nakashima Y, Hatano T, Akiyama M, Fujii M, Hara D, Kanazawa M, Haraguchi A, Iwamoto Y. High prevalence of cam deformity in dysplastic hips: a three-dimensional CT study. J Orthop Res. 2016;34:1613–1619. doi: 10.1002/jor.23147. [DOI] [PubMed] [Google Scholar]
- 46.Ziebarth K, Balakumar J, Domayer S, Kim YJ, Millis MB. Bernese periacetabular osteotomy in males: is there an increased risk of femoroacetabular impingement (FAI) after Bernese periacetabular osteotomy? In: Clinical Orthopaedics and Related Research. Association of Bone and Joint Surgeons; 2011. p. 447–53. [DOI] [PMC free article] [PubMed]
- 47.Myers SR, Eijer H, Ganz R. Anterior femoroacetabular impingement after periacetabular osteotomy. Clin Orthop Relat Res. 1999;363:93. doi: 10.1097/00003086-199906000-00012. [DOI] [PubMed] [Google Scholar]
- 48.Kim HKW. Pathophysiology and new strategies for the treatment of Legg-Calvé-Perthes disease. J Bone Joint Surg Am. 2012. [DOI] [PubMed]
- 49.Tannast M, Hanke M, Ecker TM, Murphy SB, Albers CE, Puls MLCPD. Reduced range of motion resulting from extra- and intraarticular impingement hip. Clin Orthop Relat Res. 2012;470:2431–2440. doi: 10.1007/s11999-012-2344-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Chaudhry S, Phillips D, Feldman D. Legg-Calvé-Perthes disease: an overview with recent literature. Bull Hosp Jt Dis 2014; [PubMed]
- 51.Leunig M, Ganz R. Relative neck lengthening and intracapital osteotomy for severe Perthes and Perthes-like deformities. Bull Hosp Jt Dis. 2011;69(Suppl 1):S62–7. [PubMed]
- 52.Lehmann CL, Arons RR, Loder RT, Vitale MG. The epidemiology of slipped capital femoral epiphysis: an update. J Pediatr Orthop. 2006;26:286–290. doi: 10.1097/01.bpo.0000217718.10728.70. [DOI] [PubMed] [Google Scholar]
- 53.Loder RT, Skopelja EN. The epidemiology and demographics of slipped capital femoral epiphysis. ISRN Orthop. 2011;2011:1–19. [DOI] [PMC free article] [PubMed]
- 54.Hesper T, Bixby SD, Maranho DA, Miller P, Kim YJ, Novais EN. Morphologic features of the contralateral femur in patients with unilateral slipped capital femoral epiphysis resembles mild slip deformity: a matched cohort study. Clin Orthop Relat Res. 2018;476:890–899. doi: 10.1007/s11999.0000000000000127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sankar WN, Novais EN, Lee C, Al-Omari AA, Choi PD, Shore BJ. What are the risks of prophylactic pinning to prevent contralateral slipped capital femoral epiphysis? Hip. In: Clin Orthop Relat Res 2013. [DOI] [PMC free article] [PubMed]
- 56.Millis MB, Lewis CL, Schoenecker PL, Clohisy JC. Legg-calvé-perthes disease and slipped capital femoral epiphysis: major developmental causes of femoroacetabular impingement. In: J Am Acad Orthop Surg. 2013. [DOI] [PubMed]
- 57.Leunig M, Ganz R. The evolution and concepts of jointpreserving surgery of the hip. Bone Joint J. 2014;96-B:5–18. [DOI] [PubMed]
- 58.Siebenrock KA, Hempfing A, Nötzli HP, Ramseier LE, Ganz R. Perfusion of the femoral head during surgical dislocation of the hip: monitoring by laser doppler flowmetry. J Bone Joint Surg. 2003; [DOI] [PubMed]
- 59.Matsuda DK, Carlisle JC, Arthurs SC, Wierks CH, Philippon MJ. Comparative systematic review of the open dislocation, mini-open, and arthroscopic surgeries for femoroacetabular impingement. Arthroscopy. 2011;27:252–69. [DOI] [PubMed]