Abstract
Background & aims
The province of British Columbia (BC), Canada has experienced a rapid increase in illicit drug overdoses and deaths during the last four years, with a provincial emergency declared in April 2016. These deaths have been driven primarily by the introduction of synthetic opioids into the illicit opioid supply. This study aimed to measure the combined impact of large-scale opioid overdose interventions implemented in BC between April 2016 and December 2017 on the number of deaths averted.
Design
We expanded on the mathematical modelling methodology of our previous study to construct a Bayesian hierarchical latent Markov process model to estimate monthly overdose and overdose-death risk, along with the impact of interventions.
Setting/Cases
Overdose events and overdose-related deaths in BC from January 2012 to December 2017.
Interventions
The interventions considered were take-home naloxone kits, overdose prevention/supervised consumption sites and opioid agonist therapy
Measurements
Counterfactual simulations were performed with the fitted model to estimate the number of death events averted for each intervention, and in combination.
Findings
Between April 2016 and December 2017, BC observed 2177 overdose deaths (77% fentanyl-detected). During the same period, an estimated 3 030 (2 900 – 3 240) death events were averted by all interventions combined. In isolation, 1 580 (1 480 – 1 740) were averted by take-home naloxone, 230 (160 – 350) by overdose prevention services, and 590 (510 – 720) were averted by opioid agonist therapy.
Conclusions
A combined intervention approach has been effective in averting overdose deaths during British Columbia’s opioid overdose crisis in the period since declaration of a public health emergency (April 2016 to December 2017). However, the absolute numbers of overdose deaths have not changed.
Introduction
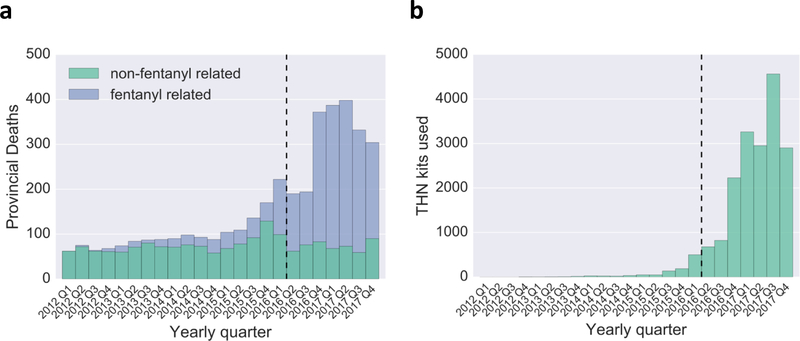
North America is currently experiencing an opioid overdose crisis, primarily driven by changes in the prescription of opioids and the introduction of highly potent, manufactured synthetic opioids into the illicit (street) drug market1–3. In British Columbia (BC), life expectancy has dropped between 2014– 2016, primarily driven by the large number of overdose deaths4. BC has seen a dramatically increased number of deaths from overdose due to illicit drugs since 2015 (Fig. [1a])5. Illicit drug overdose deaths now outnumber those due to suicide, motor vehicle accident and homicide combined6. In response to the escalating crisis, a provincial public health emergency was declared in April 20167,8. In BC, the crisis has been driven by the increasing presence of synthetic opioids, most notably illicitly-produced fentanyl, in the illicit drug supply. Fentanyl was first detected as a factor in overdose deaths by the Coroners Service of BC in 2012. The rate of fentanyl detection increased substantially in late 2015 (Fig. [1a]) and then increased significantly during 2016. There were 1 156 fentanyl-detected overdose deaths in 2017 representing a 73% increase over 20165.
Figure 1:
Provincial data summary. (a) Number of illicit-drug overdose related deaths in province broken down by fentanyl-detected and those not related to fentanyl. (b) Provincial take-home naloxone kits used. (c) Overdoses witnessed at an overdose prevention site or supervised consumption site (d) Estimated number of patients on opioid agonist therapy. Black dashed line represents when the provincial public health emergency was declared.
Provincial efforts to respond to the overdose crisis have initially focused on rapid scale-up of the take-home naloxone (THN) program and the establishment of overdose prevention service and supervised consumption service facilities (OPS/SCS), as well as supporting uptake of opioid agonist therapies (OAT) including buprenorphine/naloxone and methadone8,9. There are also continuing efforts to address contamination of supply, structural barriers and upstream factors, and to counter social stigma among people who use opioids8.
Naloxone is an opioid antagonist that can rapidly reverse opioid overdose and prevent death. The distribution of naloxone kits to the public has been shown to be cost-effective in certain settings10–14. The BC THN program has expanded rapidly since its inception in 2012. In 2012, only 269 kits were distributed, while 88 300 kits were distributed in 2017 (Fig. [1b]). THN kits are now distributed by all emergency departments, all provincial correctional facilities, and some community pharmacies. We previously used mathematical modeling to assess the impact of the BC THN program from January 2012 to June 2016 and found the THN program significantly reduced the number of overdose deaths during the earlier part of the current crisis14.
Overdose prevention sites are low-barrier facilities at which individuals can use drugs under supervision. In the event of an overdose, OPS can provide limited intervention. In BC, OPS were started by community members and approved by the BC Minister of Health in December 201615. By the end of 2017, 23 sites were operating, with a total of 3 476 non-fatal overdoses observed at an OPS (Fig. [1c]). For the purposes of this paper, we also include two supervised consumption sites within the OPS designation, which also provide enhanced access to addiction services and on-site medical professionals16. To date, few studies have examined the decrease in mortality due to supervised consumption sites and no studies have examined the benefits of overdose prevention sites17.
OAT is the first-line treatment for opioid use disorder and is available by prescription within BC. The number of people accessing OAT in BC has increased due to initiatives such as increased provider training, and referrals of people at risk of overdose to OAT, as well as the introduction of therapeutic alternatives such as buprenorphine/naloxone therapy in 201518, and more recently slow-release oral morphine19. Based on provincial pharmaceutical dispensations, the monthly average number of people receiving OAT during 2012–2015 was 18 095, this increased by 19%, to 22 191 in 2017 (Fig. [1d]).
Mathematical modeling has been extensively used to estimate the impact and cost-effectiveness of harm reduction interventions surrounding people who use drugs (PWUD)20–22, with particular application to naloxone10,14,23,24. In this paper, we expand on our previous validated model, supported by detailed administrative data, to estimate the impact of THN, OPS and OAT interventions prior to and during the 21-month period between the declaration of the provincial public health emergency (April 2016) and the end of 201714. Our method estimates the underlying monthly risk of overdose and probability of subsequent death by incorporating provincial surveillance data in a rigorous Bayesian inference framework14. The structure is event-based, allowing us to incorporate diverse datasets in an evidence-synthesis fashion, and is applicable when there are multiple interventions that are co-varying by time and geography25. After fitting the model and performing careful validation, we study a series of counterfactual scenarios to estimate the number of death events averted by each intervention.
Methods
Model Overview
The model is a rate-based Bayesian hierarchical Markov process which explicitly takes into account monthly and geographic variability in risk. As the model is fit using a Bayesian framework, each parameter and its uncertainty have initial priors based on available literature estimates or else guided by expert opinion. The prior distributions are then updated in the model fitting framework based on all available data. Every individual in the at-risk population in a given region has a per-month probability of experiencing an overdose, and each overdose can lead to a death. The probabilities of these events change over time, depend on the proportion of fentanyl in the illicit drug supply. The rate of overdosing for a given individual in a given month and region is the background (no-fentanyl) overdose rate, plus an additional risk due to contact with fentanyl. The total opioid overdose rate is then multiplied by the probability of an ambulance call-out, to give the ambulance-attended overdose rate. Death rates were informed by coroner-confirmed overdose deaths, which also indicate whether fentanyl was present. The overall (provincial) proportion of fentanyl contact is modelled as a latent (unobserved) time series that follows a random walk process from month to month (where the rate is dependent on the previous month only, with some random normally-distributed variation). Monthly regional fentanyl contact rates are permitted some variation around the provincial rate. We also allow the risk of death following an overdose to vary according to presence of fentanyl-analogues in the illicit-drug supply, and also according to monthly weather variables, which can also capture other seasonally-dependent risks. Risk of death following an overdose has previously been shown to be significantly dependent on ambient temperature within cocaine-use in New York city. We also found a small dependency on weather in our previous study of overdose deaths in British Columbia14,26. See Table S1 in the Supplementary Information for details on our initial priors for parameters.
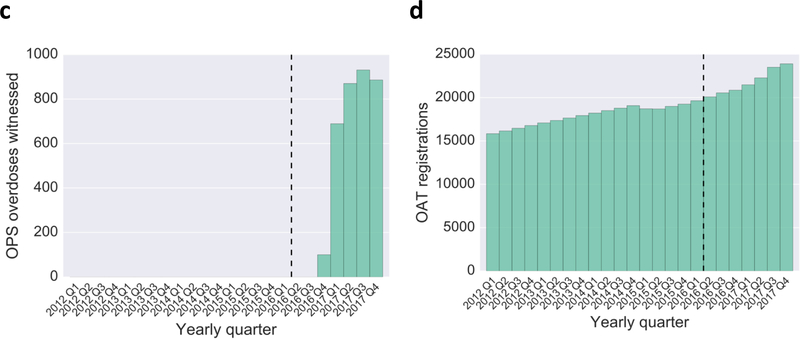
Interventions are then modelled individually as follows (Fig. [2]). First, if an individual in the PWUD population is on OAT then they are at reduced risk of an overdose, based on performance measures of the BC opioid substitution treatment program18. We additionally capture an increased rate of overdose for individuals relapsing from OAT. The elevated risk of overdose due to relapse was set at one month27. Second, there is a probability that THN will be administered following an overdose. This probability depends on the number of THN kits in circulation in the region, and a program effectiveness parameter with a uniform prior. Finally, there is a probability that the overdose occurs at an OPS/SCS, informed directly by the observed numbers of overdoses at sites in the region. We assume that all THN and OPS/SCS interventions result in survival. To date no deaths have occurred at an OPS/SCS and only in a rare handful of cases would THN have been administered once an individual is already deceased. If an overdose is not intervened then individual survival is based on a given probability as described above. Full details of all modelling assumptions are presented in the Supplementary Information.
Figure 2:
Flow-chart for incorporation of intervention into analysis. An individual who is not on OAT (or interrupting OAT treatment) is at risk of an overdose. During an overdose event there is a probability that THN is administered effectively and a probability that the overdose occurs at an OPS. If either event occurs then the individual survives the overdose as it is assumed THN was administered effectively and no overdose deaths have occurred at an OPS throughout the entire study period. If neither occurs then there is a certain probability the individual dies after an overdose.
Data
Data were collected as part of the ongoing monitoring of overdose events and associated interventions and outcomes, both at provincial and regional levels (based on all five regional health authorities in BC). See Table [1] for an overview of the data and its limitations.
Table 1. Data sources.
Surveillance and intervention data collected for study including model input, source of data, data collection method, case definition, and any known limitations.
| Model input | ||||
|---|---|---|---|---|
| Illicit-drug overdose deaths | BC Coroners Service | Autopsy reports | Street drugs (Controlled and illegal drugs: heroin, cocaine, MDMA, methamphetamine, illicit fentanyl etc.). Medications not prescribed to the decedent but obtained/purchased on the street, from unknown means or where origin of drug not known. Combinations of the above with prescribed medications. | |
| Fentanyl-detected overdose deaths | BC Coroners Service | Autopsy reports | Fentanyl or its analogues were detected, whether alone or in combination with other drugs, and the death resulted from illicit drug use. In the majority of deaths, fentanyl or its analogues were detected in combination with other drugs. Deaths were excluded if the fentanyl was known to be prescribed or the death was suspected to be due to intentional self-harm. | |
| Ambulance-linked overdoses | BC Ambulance Service | Administrative records | Codes associated with accidental opioid-overdose or probable overdose were selected | Overdoses where an ambulance was not called would not be accounted for |
| THN kits used | Provincial THN program | Kit replacement forms | The number of client re-fills due to client stating that a kit had be used | Only able to capture those clients who are returning a kit due to their use. Likely missing kits used where client does not return |
| THN kits distributed | Provincial THN program | THN request form | Registered THN sites are able to order THN kits for distribution to clients. Sites are expected to return distribution records on a regular basis. Distribution numbers represent the number of kits distributed according to records returned by THN sites | Numbers are reliant on reporting by THN sites and are likely an underestimate of the total number of kits given out to clients |
| OPS overdose | Provincial OPS | OPS staff | An overdose that is witnessed to have occurred within an OPS facility | |
| OPS site | Provincial OPS | Regional health authority | An OPS facility that is active in a given month | |
| Ambulance call-outs | Provincial THN program | kit forms | All returned forms where a kit was used and the question on whether an ambulance was called was answered | Only for kit forms returned, which may introduce a systematic bias |
| Patients registered on OAT | Provincial Health Officer report & Pharmanet | Composition of hospital discharges, community pharmacies, and the provincial medical services plan claims | Patient registered to receive methadone or suboxone/buprenorphine | Data prior to 2015 was retrieved from an opioid substitution treatment performance measure report commissioned by the Provincial Health Officer18. Data post 2017 was taken from the BCCDC reported statistics. Where data overlapped, an average of the two was taken. Typically data differed by 1–5% |
| Weather | World Weather Online30 | API | Monthly aggregated wind speed, precipitation and temperature located at most populous location in region | Weather statistics were taken from most densely populated urban area within each region |
| Fentanyl contaminant | LifeLabs | Urinalysis | Collected urine sample testing positive for fentanyl | Samples are requisition by OAT provider and hence represent a biased sample of the at-risk population. Testing only began in 2017. |
| Carfentanil contaminant | LifeLabs | Urinalysis | Collected urine sample testing positive for carfentanil | See above. |
| PWUD | Literature29 | Estimated | Methodology based on known indications of injection drug use | Only captures injection drug use |
Ambulance-attended overdoses and coroner-confirmed illicit drug-related overdose deaths (including deaths related to fentanyl) were collected by region from January 2012 to December 2017. BC has a province-wide ambulance service that provides a consistent and complete number of ambulance-attended overdoses: these were events where treatment by an ambulance crew included the use of naloxone or the paramedic impression codes indicated the use of illicit drugs and the corresponding dispatch code was consistent with possible drug overdose, although exact substances are not confirmed28. Toxicology was performed on all suspected illicit drug deaths in BC, with all cases under the jurisdiction of the BC Coroners Service and all tests performed at the BC provincial toxicology laboratory. The population prior of individuals at-risk to an overdose was derived from a regionally estimated number at a single time-point. This was an estimate of the number of persons who inject drugs, derived from the BC Hepatitis Testers Cohort, which captures all individuals who have tested for sexually-transmitted and blood-borne infections in BC29. This is likely an underestimate of the total at-risk population for our model. To mitigate this uncertainty, we performed a simple uncertainty analysis around the size of the at-risk population (Supplementary Information). We found that mis-specification makes minimal difference to our key model outputs. We found a similar lack of difference in our previous study14. For maximal flexibility, we also incorporated uncertainty into the prior for the population size. For the THN program we obtained monthly counts for the numbers of kits distributed to a client and used. When a kit is distributed, the client is asked the reason for obtaining the kit including if one had previously been used, which provides the kit use estimate. OPS/SCS data has been collected quarterly since December 2016, capturing the number of observed overdoses at each site, as well as the number of sites operating in each region. OPS/SCS indicators were provided directly by each regional health authority. OAT data was derived from prescription, physician billing and hospital discharge data18. We also used regional estimates of hospitalization rates for OAT patients on and off treatment18. Given previous analyses showing associations between overdose patterns and weather, data including monthly feels-like temperature, precipitation and wind strength were extracted from a publicly-available data source26,30.
Data collected at the provincial level included whether an ambulance was called at the time of an overdose during THN kit use (ambulance call-out rate). These were derived from administrative records obtained from clients who had used the THN program, and had responded to questions (n = 2350)31. We also collected and incorporated information on the presence of fentanyl and carfentanil in the illicit drug supply from urinalysis of OAT patients.
Model fitting & validation
Model fitting was performed within a Bayesian framework, which allowed the inclusion of prior knowledge to quantify the uncertainty in both data and parameters32–34. Where possible well-informed priors were implemented based on either literature-based estimates or data. Priors for geographic and time variance were fixed with moderate values. The likelihood used for calibration was a composition of, at the regional level, monthly ambulance-attended overdoses, monthly fentanyl/non-fentanyl overdose deaths, monthly THN kits used, and provincial monthly ambulance call-out survey data and monthly urinalysis. Fitting was performed using a variational Bayes methodology. See the Supplementary Information for full construction of likelihood and priors35.
Model validation was assessed using two standard measures: the root mean squared error of prediction (RMSE), and the mean absolute error of prediction (MAE). MAE is less sensitive to larger prediction errors, but each measure reflects how closely the model’s predictions agree with the actual observations; each measure will be larger when the model predicts poorly, and smaller when the model predicts well. Validation was performed on the model in a leave-one-out cross-validation scheme. The death, overdose, and kit use data were removed from the fitting for each region in turn and the resulting model was used to predict the missing data (see Supplementary Information). Model fitting, validation, and analysis were performed in Python 2.7 using the probabilistic programming library PyMC336,37.
Counterfactual Modelling
To assess the impact of interventions we performed counterfactual simulations. Individual intervention impacts were estimated by removing the specific intervention from the simulation and then comparing predicted numbers of deaths to the baseline estimate where data on intervention was included. Pair-wise counterfactual scenarios were estimated by removing two out of three interventions in turn: OPS & THN, OPS & OAT, and THN & OAT. The combined impact was estimated by removing all interventions from the counterfactual simulation. Each counterfactual scenario was simulated 10 000 times by drawing parameter samples from the fitted model posterior distributions and then simulating from the sampling distribution.
The statistic used to compare between scenarios was the estimated number of deaths averted. This was calculated by drawing a sample set of parameters from the posterior and simulating the counterfactual scenario. The cumulative difference between each scenario and the baseline was then summed for whole study period or split into before and after declaration of the provincial public health emergency (April 2016).
Sensitivity analysis
Sensitivity analysis was performed by examining the contribution of each data source to both model fit and deaths averted outcomes under each of the counterfactual modelling scenarios. See Supplementary Information for full details.
Results
Validation & Model fit
Our main strategy was to use the combined surveillance data to estimate the overdose rate and risk of death following an overdose. This analysis was stratified by month and region. The model likelihood was obtained by comparison with a combination of death, ambulance, THN kit, and urinalysis data. We found that the ambulance-attended overdose data combined with survey data on the number of ambulance callouts for an overdose event are the main determinants of the monthly regional overdose rate. We also found that the numbers of both fentanyl and non-fentanyl-related deaths determine the probability of a death following an overdose, along with the proportion of overdoses which are fentanyl-related. These estimates of overdose rate and probability of death following an overdose are then further refined with the incorporation of additional data. OAT prescription numbers provide information about the number of at-risk individuals, while urinalysis and weather data inform the probability of death following an overdose. Additionally, THN kit distribution and OPS overdose numbers both affect the probability of a death following an overdose. All parameters were updated simultaneously in a rigorous Bayesian analysis structure.
The model achieved validation RMSE of 33.6 (MAE 23.7) for overdoses, 7.4 (MAE 4.8) for deaths, and 6.4 (MAE 3.7) for fentanyl-related deaths. Validation error varied across each of the five regions, with the predictions broadly capturing the trend for each observation (see Supplementary Information). The predicted trends in deaths and overdoses deviates from the observed data for region one in 2017. Excluding region one the validation RMSE were 29.5 (MAE 20.2) for overdoses, 6.3 (MAE 4.2) for deaths, and 4.7 (MAE 2.7) for fentanyl-related deaths.
The full model fit predicts a 19.9-fold (95% credible interval [crI] 19.5–20.4) increase in risk of overdosing when fentanyl is present. In general, the estimated posterior fits well with the observed data in terms of the posterior predictive distribution. The RMSE of the full model were 12.3 (MAE 9.0) for overdoses, 3.8 (MAE 2.8) for deaths, and 3.0 (MAE 1.8) for fentanyl-detected deaths. Figs. S3–S6 in the Supplementary Information provide a graphical overview of the model fit.
The estimated probability that THN was administered during an overdose rose rapidly from 3% (95 crI 1%–5%) pre-emergency declaration, to 37% (95 crI 18%–55%) post-emergency. The probability of an overdose being observed at an OPS was 6% (95 crI 1%–17%) post-emergency. The probability of a death following an overdose without intervention increased from 8% (95 crI 7%–8%) pre-emergency to 10% (95 crI 9%–10%) post-emergency. The estimated probability of an ambulance call-out for an opioid overdose declined from 87% (95 crI 85%–89%) pre-emergency to 54% (95 crI 50%–59%) post-emergency.
Impact of interventions
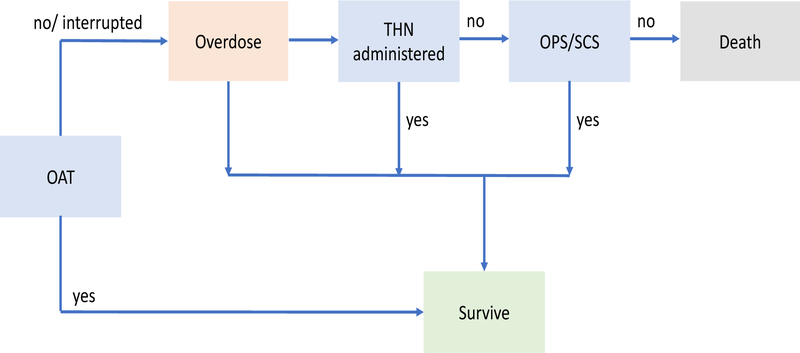
Counterfactual simulation provides an estimate of 3 650 (95 crI 3 490–3 910) death events averted by all interventions combined during the study period (Fig. [3]). Pre-emergency, 660 (95 crI 590–780) death events were averted, rising to 3 030 (95 crI 2 900–3 240) deaths averted post-emergency (Fig. [3]). Death events averted represents 52% (95 crI 50% – 54%) of all estimated possible deaths during the whole study period. This value was 31% (95 crI 28% – 35%) pre-emergency and 60% (95 crI 58%–62%) post-emergency.
Figure 3:
Total provincial annual deaths observed and averted broken down by each intervention. THN - Take Home Naloxone, OAT- Opioid Agonist Therapy, OPS - Overdose Prevention Site.
The total number of death events averted due to THN was estimated to be 1 650 (95 crI 1 540 – 1 850), corresponding to 11 (95 crI 10 – 13) kits used per death event averted. Of the total estimated possible deaths, these were 4% (95 crI 1% – 9%) pre-emergency (90 deaths (95 crI 20–200)) and 31% (30% – 34%) post-emergency (1 580 deaths (95 crI 1 480 – 1 740)).
The total estimated number of death events averted at OPS/SCS locations was 390 (95 crI 290 – 550), with 8% (95 crI 5% – 13%) of all potential deaths averted pre-emergency and 5% (crI 3% – 7%) post-emergency. The estimated number of deaths averted per site per month was 1.3 (95 crI 0.9–1.7, regional range 0.06–2.5).
The total estimated number of death events averted due to OAT was 960 (95 crI 860 – 1 150). Of these 390 (95 crI 320 – 500) were pre-emergency (18% of estimated possible deaths (95 crI 15% – 24%)) and 590 (95 crI 510 – 720) were post-emergency (12% of estimated possible deaths (95 crI 10% – 14%)).
The estimated number of deaths averted for the combined THN and OPS/SCS interventions were 260 (95 crI 190 – 360) pre-emergency and 1960 (1860 – 2130) post-emergency. For the combined OPS/SCS and OAT interventions the deaths averted in the pre-emergency period were 550 (95 crI 480 – 660), and 830 (95 crI 750 – 960) in the post-emergency period. For the combined THN and OAT interventions the deaths averted in the pre-emergency period were 480 (95 crI 420 – 600), and 2630 (95 crI 2520 – 2830). See Supplementary Information for quarterly summaries of scenarios.
Sensitivity analysis was performed to assess the impact of each data source on the results. Removal of ambulance call out survey data and fentanyl-related deaths from the fitting process inflated the number of deaths averted to 5013 (95 crI 4709 – 5328), and 4281 (95 crI 3971 – 4610). Removing illicit-drug overdose deaths, take-home naloxone kits used and ambulance attended overdoses decreased deaths averted to 3225 (95 crI 2920 – 3550), 2547 (95 crI 2326 – 2775), and 883 (95 crI 702 – 1068) respectively. See Supplementary Table S6 for full details.
Discussion
The complexity of factors driving the current North American opioid overdose crisis cannot be overstated. To be successful, the public health response must be multifaceted, rapid and responsive, and must reduce the numbers of overdoses and deaths, as well as address the root psychological and social causes of the crisis38,39. Here, we have estimated the individual and combined impact of three ongoing interventions in BC, Canada: the THN program, the introduction of OPS and the uptake of OAT. We estimate the number of overdoses that would have resulted in a death in the absence of these interventions would have been substantially higher. We find that the combined impact of all three interventions prevented an estimated 3 030 death events (95 crI 2 910–3 240) during the post-emergency period of April 2016 to December 2017. This represents 60% (95 crI 58%–62%) of the estimated deaths that would have occurred in the absence of these interventions. We also found that there was an increase in risk of death following an overdose due to the presence of fentanyl-analogues in the illicit drug supply (increase from 8% (95 crI 7–8) to 10% (95 crI 9 – 10)).
Our results were generated using a novel Bayesian hierarchical latent Markov process model, incorporating multiple interventions and data at different geographic scales14. The model estimates the underlying overdose and death due to overdose risk. This provides the ability to estimate the impact of interventions that target an overdose event or underlying overdose risk. The estimates are robust to missing data and misspecification of the underlying at-risk population (see Supplementary Information and Irvine et. al. 201814). This approach is also advantageous when a number of factors are co-varying together and may be inherently non-linear (e.g. naloxone introduction alongside increasing rates of fentanyl adulterant). This is a distinct advantage of this method over more traditional causal inference methods such as interrupted time-series40. The methodology also provides an estimate of historic impact as opposed to more speculative modelling approaches around future intervention scenarios41. We were able to take this approach due to BC’s highly detailed surveillance data and its particular public health focus on harm reduction. The model structure can be readily adapted to include other forms of surveillance data, and should be of value for other jurisdictions.
The main model outcome of deaths averted was determined by the incorporated observed data, including the number of illicit-drug related overdose deaths, number of fentanyl-related overdose deaths, number of THN kits used, and number of ambulance-attended overdoses. All data sources impacted the model outcomes substantially (Supplementary Information). This highlights the need to have comprehensive surveillance data when evaluating a complex epidemic such as the overdose crisis in BC. Nonetheless, the data providing the most information to support our estimate of deaths averted due to THN was found to be the number of THN kits used. Similarly, the data that was most important in terms of estimating the total deaths averted was the number of ambulance-attended overdoses. See Supplementary Information for further detail.
Naloxone has been shown to be highly effective as an overdose reversal agent when administered by a layperson and there is evidence that its use does not increase the risk behaviour of individuals who use heroin11,42. Our results indicate that the BC THN program substantially reduced mortality following declaration of the provincial emergency, with 1 580 (95 crI 1 480–1 740) death events averted, and when combined with OAT, we estimate that 2 630 (95 crI 2 520 – 2 830) deaths were averted. This corresponds to one averted death per 11 (95 crI 10–13) THN kits used. These results are very much in line with our previous findings of THN effectiveness in BC, where we estimated one death averted per 10 (95 crI 5–35) kits used14. This highlights the potentially powerful impact of multiple harm reduction programs being rolled out simultaneously within a single jurisdiction.
We estimated the total impact of the OPS/SCS program to be 230 (160–350) death events averted during the study period. This intervention started in December 2016 and was being scaled-up across the province during 2017. To date, not a single overdose death has occurred at an OPS or SCS. The OPS/SCS program has therefore already substantially reduced mortality and its long-term impact is likely to be very significant. Supervised injection facilities have also been shown to be associated with increased engagement in care for addiction as well as reductions in fatal overdoses43.
Uptake of OAT impacts mortality by reducing the risk of fatal overdose. Using the monthly risk of overdose and of death for each PWUD, we can estimate that OAT averted 590 (95 crI 510–720) death events during the study period. Long-term retention is necessary to avoid relapse, which can lead to increased risk of overdose44.
Our study has certain limitations. We were only able to analyze those interventions for which data exists. For example, general education of the at-risk population through informational campaigns, stigma reduction activities, provider training initiatives, or specific alerts cannot easily be modeled in our framework. All supervised facilities were treated as the same type of intervention for the purpose of our analysis. We focused on risk stratified by exposure to illicit opioids and geographic region, but are not able to assess the heterogeneity of risk in the population without more finely-grained data. We intend to address this limitation in future community-level studies. Heterogeneity in risk also leads to multiple death events averted for one individual. Future studies will seek to understand the impact of interventions on individual trajectories through a survival analysis. The size of the at-risk population was estimated through provincial tests for sexually-transmitted and other blood-borne infections29. It is likely that this is an underestimate of the total at-risk population, however, the total deaths averted is robust to this limitation as shown in the Supplementary Information and in keeping with findings reported in our previous study14.
Conclusion
The deployment of diverse interventions in BC such as THN, OPS, and OAT have significantly reduced the total mortality during the early stages of an opioid crisis driven primarily by the introduction of highly toxic illicit synthetic opioids.
We believe that a multi-intervention approach to the opioid overdose crisis is required. During a synthetic opioid crisis, the rapid scale-up of intervention was estimated to reduce the number of deaths by 60%. However, given that the majority of illicit drug overdose deaths in BC have occurred among people who use opioids alone, interventions that address the contaminated drug supply along with OAT are likely needed to further reduce overdose deaths.
The authors wish to acknowledge the ongoing collaboration of agencies who have provided data to the BC Centre for Disease Control and have supported this modeling work: BC Coroners Service, BC Emergency Health Services, Lifelabs, and the Ministry of Health. MG, MAI and DC acknowledge funding from the BC Government and the Canadian Institutes of Health Research for this work. DC was supported by a Natural Science and Engineering Research Council Discovery Grant (grant RGPIN-2015–04611). M-JM is supported by CIHR, MSFHR and the US NIH (U01-DA0251525). The authors wish to thank Mohammad Karamouzian for help in collection of the ambulance call-out data.
Supplementary Material
Footnotes
Declaration of competing interests: The authors declare no competing interests
References
- 1.Fischer B, Keates A, Bühringer G, Reimer J, Rehm J. Non-medical use of prescription opioids and prescription opioid-related harms: Why so markedly higher in North America compared to the rest of the world? Addiction. 2014;109(2):177–181. [DOI] [PubMed] [Google Scholar]
- 2.Guy JG, Zhang K, Bohm MK, et al. Vital signs: Changes in opioid prescribing in the united states, 2006–2015. MMWR Morbidity and mortality weekly report. 2017;66(26):697–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Janjua N, Islam N, Kuo M, et al. Identifying injection drug use and estimating population size of people who inject drugs using healthcare administrative datasets. 2018;55:31–39. [DOI] [PubMed] [Google Scholar]
- 4.Ye X, Sutherland J, Henry B, Tyndall M, Kendall PRW. Impact of drug overdose-related deaths on life expectancy at birth in british columbia. Health Promotion & Chronic Disease Prevention in Canada: Research, Policy & Practice. 2018;38(6). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Coroners Service of British Columbia. Fentanyl-Detected Illicit Drug Overdose Deaths January 1, 2012 to February 28, 2017. Coroners Service of British Columbia; 2017. http://www2.gov.bc.ca/gov/content/safety/public-safety/death-investigation/statistical-reports. [Google Scholar]
- 6.Coroners Service of British Columbia. Illicit Drug Overdose Deaths in Bc January 1, 2007 - March 31, 2017. Coroners Service of British Columbia; 2017. http://www2.gov.bc.ca/gov/content/safety/public-safety/death-investigation/statistical-reports. [Google Scholar]
- 7.British Columbia Observatory Population and Public Health. The Bc Public Health Opioid Overdose Emergency. BC Centre for Disease Control; 2017. http://www.bccdc.ca/resource-gallery/Documents/Educational\%20Materials/Epid/Other/Public\%20Facing\%20Surveillance\%20Report_Jan2017.pdf. [Google Scholar]
- 8.BCCDC, PHSA. BC Overdose Action Exchange II. Provincial Health Services Authority; 2017. http://www.bccdc.ca/resource-gallery/Documents/bccdc-overdose-action-screen.pdf. [Google Scholar]
- 9.Office of the Provincial Health Officer of British Columbia, Coroners Service of British Columbia, British Columbia Centre for Disease Control. British Columbia Overdose Action Exchange Meeting Report. British Columbia Centre for Disease Control; 2016. http://www.bccdc.ca/resource-gallery/Documents/BCOAE-Meeting-Report.pdf. [Google Scholar]
- 10.Coffin PO, Sullivan SD. Cost-effectiveness of distributing naloxone to heroin users for lay overdose reversalcost-effectiveness of distributing naloxone for heroin overdose reversal. Annals of internal medicine. 2013;158(1):1–9. [DOI] [PubMed] [Google Scholar]
- 11.McDonald R, Strang J. Are take-home naloxone programmes effective? Systematic review utilizing application of the Bradford Hill criteria. Addiction. 2016;111(7):1177–1187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bird SM, McAuley A, Perry S, Hunter C. Effectiveness of Scotland’s national naloxone programme for reducing opioid-related deaths: A before (2006–10) versus after (2011–13) comparison. Addiction. 2016;111(5):883–891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Somerville NJ. Characteristics of fentanyl overdose – Massachusetts, 2014–2016. MMWR Morbidity and Mortality Weekly Report. 2017;66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Irvine MA, Buxton JA, Otterstatter M, et al. Distribution of take-home opioid antagonist kits during a synthetic opioid epidemic in british columbia, canada: A modelling study. The Lancet Public Health. 2018;3(5):e218–e225. [DOI] [PubMed] [Google Scholar]
- 15.Office of the Provincial Health Officer of BC, BC Centre for Disease Control, BC Coroners Service. British Columbia Overdose Action Exchange Supplementary Material: Primers. BC Centre for Disease Control; 2017. http://www.bccdc.ca/resource-gallery/Documents/BCOAE-supplementary-materials.pdf. [Google Scholar]
- 16.Tyndall MW, Kerr T, Zhang R, King E, Montaner JG, Wood E. Attendance, drug use patterns, and referrals made from North America’s first supervised injection facility. Drug and alcohol dependence. 2006;83(3):193–198. [DOI] [PubMed] [Google Scholar]
- 17.Potier C, Laprévote V, Dubois-Arber F, Cottencin O, Rolland B. Supervised injection services: What has been demonstrated? A systematic literature review. Drug and alcohol dependence. 2014;145:48–68. [DOI] [PubMed] [Google Scholar]
- 18.Medical Beneficiary, Pharmaceutical Services Division, Public Health Division, British Columbia Ministry of Health. BC Opioid Substitution Treatment System: Performance Measures 2014/2015-2015/2016. British Columbia Ministry of Health; 2017. https://www2.gov.bc.ca/assets/gov/health/about-bc-s-health-care-system/office-of-the-provincial-health-officer/reports-publications/special-reports/bc-ost-system-measures-14-15-and-15-16.pdf. [Google Scholar]
- 19.BC Centre on Substance Use, BC Ministry of Health. A Guideline for the Clinical Management of Opioid Use Disorder. BC Centre on Substance Use; 2017. http://www.bccsu.ca/care-guidance-publications/. [Google Scholar]
- 20.Razali K, Thein HH, Bell J, et al. Modelling the hepatitis C virus epidemic in Australia. Drug and alcohol dependence. 2007;91(2):228–235. [DOI] [PubMed] [Google Scholar]
- 21.Razali K, Amin J, Dore G, Law M, HCV Projections Working Group, others. Modelling and calibration of the hepatitis C epidemic in Australia. Statistical Methods in Medical Research. 2009;18(3):253–270. [DOI] [PubMed] [Google Scholar]
- 22.Degenhardt L, Charlson F, Mathers B, et al. The global epidemiology and burden of opioid dependence: Results from the global burden of disease 2010 study. Addiction. 2014;109(8):1320–1333. [DOI] [PubMed] [Google Scholar]
- 23.Walley AY, Xuan Z, Hackman HH, et al. Opioid overdose rates and implementation of overdose education and nasal naloxone distribution in Massachusetts: Interrupted time series analysis. Bmj. 2013;346:f174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Keane C, Egan JE, Hawk M. Effects of naloxone distribution to likely bystanders: Results of an agent-based model. International Journal of Drug Policy. 2018;55:61–69. [DOI] [PubMed] [Google Scholar]
- 25.Jackson CH, Jit M, Sharples LD, De Angelis D. Calibration of complex models through bayesian evidence synthesis: A demonstration and tutorial. Medical decision making. 2015;35(2):148–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bohnert AS, Prescott MR, Vlahov D, Tardiff KJ, Galea S. Ambient temperature and risk of death from accidental drug overdose in New York city, 1990–2006. Addiction. 2010;105(6):1049–1054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sordo L, Barrio G, Bravo MJ, et al. Mortality risk during and after opioid substitution treatment: Systematic review and meta-analysis of cohort studies. bmj. 2017;357:j1550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.British Columbia Centre for Disease Control. Paramedic-Attended Illegal Drug Overdoses. British Columbia Centre for Disease Control; 2018. http://www.bccdc.ca/resource-gallery/Documents/Statistics\%20and\%20Research/Statistics\%20and\%20Reports/Overdose/BCAS_indicator_public.pdf. [Google Scholar]
- 29.The Centre for Global Public Health, University of Manitoba. Estimation of Key Population Size of People Who Use Injection Drugs (PWID), Men Who Have Sex with Men (MSM) and Sex Workers (SW) Who Are at Risk of Acquiring HIV and Hepatitis C in the Five Health Regions of the Province of British Columbia. BC Centre for Disease Control; 2016. http://www.bccdc.ca/resource-gallery/Documents/Statistics\%20and\%20Research/Statistics\%20and\%20Reports/STI/PSE\%20Project\%20Final\%20Report.pdf. [Google Scholar]
- 30.World weather online API. Accessed: 2017-06-06 https://api.worldweatheronline.com/
- 31.Karamouzian M, Kuo M, Crabtree A, Buxton JA. Correlates of seeking emergency medical help in the event of an overdose in british columbia, canada: Findings from the take home naloxone program. International Journal of Drug Policy. 2019. [DOI] [PubMed] [Google Scholar]
- 32.Elderd BD, Dukic VM, Dwyer G. Uncertainty in predictions of disease spread and public health responses to bioterrorism and emerging diseases. Proceedings of the National Academy of Sciences. 2006;103(42):15693–15697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jackson CH, Sharples LD, Thompson SG. Structural and parameter uncertainty in Bayesian cost-effectiveness models. Journal of the Royal Statistical Society: Series C (Applied Statistics). 2010;59(2):233–253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Spiegelhalter D, Myles JP, Jones DR, Abrams KR. An introduction to Bayesian methods in health technology assessment. British Medical Journal. 1999;319(7208):508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kucukelbir A, Ranganath R, Gelman A, Blei D. Automatic variational inference in Stan. In: Advances in Neural Information Processing Systems; 2015:568–576. [Google Scholar]
- 36.Pérez F, Granger BE. IPython: A system for interactive scientific computing. Computing in Science & Engineering. 2007;9(3):21–29. [Google Scholar]
- 37.Salvatier J, Wiecki TV, Fonnesbeck C. Probabilistic programming in python using PyMC3. PeerJ Computer Science. 2016;2:e55. doi: 10.7717/peerj-cs.55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.The Lancet Public Health. A public health approach to Canada’s opioid crisis. The Lancet Public Health. 2018. –5AD;3(5):e204. doi: 10.1016/S2468-2667(18)30078-1 [DOI] [PubMed] [Google Scholar]
- 39.Comiskey CM. Take-home naloxone: While good, it is far from good enough. The Lancet Public Health. 2018;3(5):e205–e206. [DOI] [PubMed] [Google Scholar]
- 40.Kontopantelis E, Doran T, Springate DA, Buchan I, Reeves D. Regression based quasi-experimental approach when randomisation is not an option: Interrupted time series analysis. bmj. 2015;350:h2750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pitt AL, Humphreys K, Brandeau ML. Modeling health benefits and harms of public policy responses to the us opioid epidemic. American journal of public health. 2018;108(10):1394–1400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jones JD, Campbell A, Metz VE, Comer SD. No evidence of compensatory drug use risk behavior among heroin users after receiving take-home naloxone. Addictive behaviors. 2017;71:104–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Marshall BD, Milloy MJ, Wood E, Montaner JS, Kerr T. Reduction in overdose mortality after the opening of north america’s first medically supervised safer injecting facility: A retrospective population-based study. The Lancet. 2011;377(9775):1429–1437. [DOI] [PubMed] [Google Scholar]
- 44.Mattick RP, Kimber J, Breen C, Davoli M. Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. Cochrane Database Syst Rev. 2008;2(2). [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.