Abstract
Discussion of growing inequity in US life expectancy increasingly focuses on the popularized narrative that it is driven by a surge of “deaths of despair.” Does this narrative fit the empirical evidence? Using Census and Vital Statistics data, we apply life-table methods to calculate cause-specific years of life lost between ages 25 and 84, by sex and educational rank, for non-Hispanic blacks and whites in 1990 and 2015. Drug overdoses do contribute importantly to widening inequity for whites, especially men, but trivially for blacks. The contribution of suicide to growing inequity is unremarkable. Cardiovascular disease, non-lung cancers, and other internal causes are key to explaining growing life expectancy inequity. Results underline the speculative nature of attempts to attribute trends in life-expectancy inequity to an epidemic of despair. They call for continued investigation of the possible weathering effects of tenacious high-effort coping with chronic stressors on the health of marginalized populations.
Keywords: US, opioid epidemic, cancer, cardiovascular disease, growing life expectancy inequities, despair, weathering, John Henryism
Background
A variety of independent researchers, using different data sources and methodologies, have now established a troubling fact: the long-running trend of universal gains in life expectancy (LE) has come to a halt or, in some U.S. subpopulations, reversed (e.g., Bound et al. 2015; Case and Deaton 2015; Geronimus, Bound, and Colen 2011; Gross, Glied, and Muennig 2015; Hendi 2015; Meara, Richards, and Cutler 2008; Montez et al. 2011; Olshansky et al. 2012; Preston and Elo 1995; Sasson 2016). The disparity in life expectancy between higher- and lower-educated groups has been growing at least since 1990 in blacks and whites, men and women.
Although the advent of the opioid epidemic postdated the early growth in life expectancy inequity (Meara et al. 2008; Muennig et al. 2018), investigators have wondered whether rising opioid and other drug-related deaths are to blame. In fact, drug overdoses can explain a substantial fraction of growing inequity among whites, especially those ages 30–60 (Ho 2017). However, less is known about the importance of drug-related deaths among other subpopulations, such as nonwhites or older Americans. Furthermore, the literature has made little progress in placing the growth of drug-related deaths in context alongside other historically important causes of death, such as chronic diseases, that may also play an important role in recent trends in life expectancy. Without a more complete understanding of the drivers of this growing inequity, the research and policy communities are at risk of focusing too narrowly on this single currently prominent behavioral risk rather than consider more fundamental causes (Link and Phelan 1995).
Despite these gaps in the empirical evidence, much of the discussion of recent trends in life expectancy, both in the academic community and the popular press, has focused on the growth of drug-related deaths. One prominent narrative suggests that increased opioid and other drug deaths may be the consequence of growing existential despair among less educated Americans. This narrative suggests that economic stagnation and unresponsive social institutions induce despair among the less educated, who look to substance use to numb the pain or tedium of losing status, resources, meaningful work, and opportunities to build and support their families – i.e. as means of actual or slow suicide (Case and Deaton 2017). Proponents of this hypothesis have aggregated drug-related deaths together with deaths to suicide and alcoholic liver disease into a composite “Deaths of Despair” (DOD) classification (Case and Deaton 2017; Monnat 2016).
Empirically, the focus on DODs as a coherent composite category has been largely driven by the observation that rates of death due to this composite rose among whites ages 45–54 (Case and Deaton 2017), a cohort one might speculate would be highly affected by the economic stagnation of the last 30+ years, especially among its less educated members. However, this increase in crude death rates in one narrow age range for whites – an age/race group whose baseline death rate is low – does not in itself shed light on the extent to which increasing DOD explain the growing educational disparities in LE across demographic groups, overall or relative to other causes. And given the findings that drug overdose deaths alone are important contributors for working-age whites (Ho 2017), some have questioned whether the increases in crude death rates attributed to the composite DOD measure are primarily driven by opioid and other drug overdose deaths (Masters, Tilstra, and Simon 2018; Muennig et al. 2018).
The emphasis on and popularization of the DOD narrative also carries the risk of ignoring alternative explanations of recent trends in drug-related deaths and in growing educational life expectancy inequity. In interpreting what underlies the dramatic increase in opioid-related deaths, many investigators do not point to despair, per se, and instead point to the exuberant and deceptive marketing of OxyContin by Purdue Pharma (Van Zee 2009), the over-prescription of legal opioids by physicians (Guy et al. 2017), and an increased availability of heroin explicitly marketed to whites (Quinones 2016). Given their strong addictive quality, these changes in the availability of opioids could explain an increase in opioid deaths, whether or not they are socioeconomically patterned by despair. In addition, the contribution of opioids to growing educational inequities in LE could be explained by differential access to life-saving resources, should overdose occur, or the possibility that the less educated are more likely to use opioids that put them at greater risk of overdose – e.g. heroin laced with fentanyl, a synthetic opioid 50–100 times as potent as morphine (Katz 2017a, 2017b; Rubin 2017) – even if they do not use drugs more often or feel greater despair than their better-educated counterparts. Recent research found that the geographic patterns of increased drug deaths appear to be more closely related to patterns of supply of legal and illegal drugs than to patterns of economic decline (Ruhm 2018).
More fundamentally, the underlying assumption of the DOD narrative that populations are “giving up” in the face of economic or social adversity neglects a body of research on the great variety of positive coping mechanisms people use to deal with life challenges. James (1994) first hypothesized and found evidence for the health-harmful effects among working-class black men of the psychological predisposition to remain hopeful and relentless in their struggles to overcome racial subordination and economic insecurity that he called, “John Henryism.” Several studies have since provided evidence that among the working-class such a predisposition to high-effort coping with chronic hardship predicts higher mean blood pressure and obesity, and other risk factors for cardiovascular diseases and cancers (Booth and Jonassaint 2016; Godbout and Glaser n.d.; James et al. 2006; Khansari, Shakiba, and Mahmoudi 2009; Parente, Hale, and Palermo 2013; Seeman et al. 2010; Steptoe and Kivimäki 2013).
So too, the Weathering Hypothesis (Geronimus 1992; Geronimus et al. 2006, 2015) emphasizes health as an emergent capacity of human beings that dynamically develops over the life course in response to repeated or chronic and structurally-rooted material, psychosocial, or environmental stressors. Weathering theory recognizes health as dynamic across the full life course as biopsychosocial mechanisms link fundamental social causes (Link and Phelan 1995) to population distributions of health, disease, and longevity. Mechanistically, advances in stress physiology, human stress genomics, epigenetics, and the mechanisms of telomere attrition confer biological plausibility on, and suggest pathways for, causal links between high effort coping with chronic stress exposure and disease.
In brief, active coping with every-day adversities shaped by structural disadvantages activate the hypothalamic- pituitary-adrenal (HPA) axis and sympathetic nervous system (SNS) (Geronimus et al. 2006; McEwen 1998; Sapolsky, Romero, and Munck 2000). This feedback system prepares the body for responses to stressful situations, for example by signaling for increased cortisol secretion, in order to utilize stored energy and respond to threats (Traustadóttir, Bosch, and Matt 2005). But repeated or chronic exposure to and physiological coping with stress inhibits the body’s ability to efficiently turn off the HPA and SNS, a circumstance associated with dysregulation of glucocorticosteriods, neurotransmitters, and inflammatory cytokines (McEwen and Gianaros 2010). Persistent activation of allostatic systems due to structural disadvantages has detrimental effects on cellular systems, including pathogenic gene expression and dysregulation and acceleration of the normal cellular aging process (Linnenbringer, Gehlert, and Geronimus 2017). These pathways are thought to be especially important in the early onset of chronic stress-related diseases and cancers.
These lines of research suggest that the less-educated may be dying not only or primarily from hopelessness and maladaptive coping through alcohol or opioid abuse, but, perhaps, from engaging in high-effort coping with adversity reflecting the hopeful belief that their economic uncertainty can be overcome with effort and tenacity. On a population level, such biopsychosocial processes would develop into life-threatening chronic diseases over the life course. Because the weathering process can take years or decades to develop into pernicious disease, if this were the case, growth in educational inequity in life expectancy would be apparent at older ages (ages 65–84 years), and not only in the younger cohorts. Thus, it is important to study trends in educational inequity in LE in a broader age range than many extant studies and to place rises in educational LE inequity stemming from specific behaviors such as opioid and other drug overdoses in perspective with possible rises in other historically important stress-related causes such as cardiovascular diseases and cancers (Jemal et al. 2008).
The current investigation was designed to estimate the contribution to growing educational inequities in life expectancy of DOD, in the aggregate and for each underlying condition –opioid and other drugs, alcoholic liver disease, or suicide -- as well as a broad range of other historically important causes among blacks and whites ages 25–84, 1990–2015. We build on existing literature on the growth in educational inequity in life expectancy in several ways. First, we focus on a broader array of causes of death than most studies which focus on a single cause or smaller subset of potential causes. Second, we ask whether the distribution of causes of death responsible for growing LE inequities varies by race or gender. Much recent literature places a strong emphasis on trends in mortality among whites, and sometimes only white women (e.g. Ho and Fenelon 2015; Montez and Zajacova 2013), although educational gradients in mortality have historically been detected in all races and have also recently grown among blacks. Third, we ask whether the distribution of causes of death responsible for growing LE inequities varies by adult age-group (working compared to post-middle age). Recent literature often emphasizes a specific age group – often working-aged adults – although deaths at older ages are more common and may or may not reflect the same trends or causes of death as those distinctive of younger adults. Fourth, we update most closely related research – e.g. Meara et al. (2008), who studied increasing educational inequity in the 1980s and 1990s; or Sasson (2016), who studied deaths through 2010, but did not consider drug-related deaths in a separate category from all external causes. Fifth, by providing estimates through 2015, we are capturing an era in which opioid deaths continued to rise at an alarming rate, inclusive of the explosion of opioid-related deaths beginning in 2010 for heroin overdose deaths and in 2014 for deaths related to fentanyl and fentanyl analogs (synthetic opioids). Finally, by providing a more complete accounting of the drivers of growing LE inequality than has been possible in previous literature, we hope to shed new light on the biopsychosocial processes underlying recent trends in mortality, and in particular to spur critical examination of the popular theory that the deteriorating life expectancy of less educated Americans can be traced to an epidemic of hopelessness and despair.
By focusing on the growth in life expectancy inequity, our goal is different from providing an accounting of the primary causes of death, overall, or for specific demographic groups, or the causes of educational inequity in LE at a single time period. For example, cardiovascular disease is the leading cause of death overall, yet if rates of cardiovascular disease deaths did not change differentially by education between 1990 and 2015, they would not contribute to the growing educational inequities in LE. If differential changes have occurred, they could theoretically contribute either to growing educational inequity in LE over the study period or to lowering it.
Data and Methods
We analyze nonHispanic blacks and nonHispanic whites separately. For counts of deaths we used data from the Multiple Cause of Death public use files, which contain individual-level information on decedents in the U.S., including cause of death, age, sex, race, ethnicity, and educational attainment. To estimate the population at risk of death using the same covariates, we used data from the 1990 and 2000 decennial U.S. Census and the 2010 and 2015 American Community Survey. We start our analysis in 1990, the first year in which vital statistics data can be matched by educational attainment to population estimates constructed using appropriately large samples. Seven states were omitted because they did not report education on the death certificate in all four years of the analysis. We limit our analysis to the forty-three states and the District of Columbia that did. Strictly speaking, this exclusion implies that our results apply only to these forty-three states and the District of Columbia. However, since the states excluded (GA, LA, NY, OK, RI, SD and WA) collectively had somewhat lower opioid and other drug overdose death rates in 2015 than did the states included, our estimates are likely to show a somewhat larger effect for drug deaths than we would have shown had we been able to include these states. A sensitivity analysis suggests that this exclusion had minimal effects on our estimates. (See online Methodological Appendix for a more elaborate discussion of these data.)
We focus on ages 25 through 84. Education through high school will be completed in most cases before age 25, while issues of age misreporting and the identification of a primary cause of death when many conditions are present become problematic among those 85 and older (Preston and Elo 1999; Tinetti et al. 2012). We present estimates for the full age range (25–84), as well as separately for 25–64 and 65–84 year olds.
We categorized education by sex- and race-specific relative ranks (bottom quartile versus top three quartiles) in the overall distribution, rather than by credentials or years of education, to adjust for distributional changes in educational attainment across race/sex cohorts. To do so, we followed the methodology of Bound et al. (2015). To estimate the relative contributions of various causes of death to growing LE inequity, we calculated cause-specific mortality rates by race, sex, and five-year age group separately for those in the bottom quartile and top three-quartiles of the educational distribution. Using standard period life table methods, these mortality rates are used to construct measures of years of life lost (YLL) – overall and by cause – from ages 25 through 84. The all-cause version of this measure represents the difference between the life expectancy between two ages and the maximum number of years in that age range (e.g., 60 years from ages 25 through 84). The cause-specific version of this measure apportions the total years lost to the various causes based on the age at which individuals die of a particular cause. For example, a person dying on their 65th birthday due to cancer loses 20 years of life to cancer in the interval 25–84, and a person dying of a drug overdose on their 45th birthday loses 40 years to drug overdose in that interval. The population measures of YLL by cause represent aggregates of these cases.
When researchers decompose YLL or standardized death rates (SDR) using standard methods they are implicitly or explicitly making counterfactual assumptions about what would have happened had certain causes of death not occurred. Standard methods assume competing risks are independent. If, as seems plausible, risks are positively correlated (e.g., if the person who dies of a drug overdose is at increased risk of dying from other causes), the cause specific analysis will tend to overestimate the impact of any specific cause on YLL or SDR (Manton and Stallard 1984). This effect may be more pronounced for a death that occurs at age 25 than a death at age 80, since the overly optimistic counterfactual is effectively applied to more potential years of life in the former case than the latter. In the current context, this means the impact of causes that disproportionately affect younger populations – e.g. opioid deaths – is likely to be exaggerated and the estimated impact of causes that disproportionately affect older populations – e.g. cardiovascular disease – conservative.
To categorize deaths by cause, we used diagnostic categories of the 9th and 10th Revisions of the International Classification of Diseases, using standard concordances. Online Appendix Table A5 lists and defines the causes of death studied according to the ICD9 codes used in 1990 and ICD10 codes used in 2015. Validity studies have shown these to be highly comparable (Anderson et al. 2001). Limitations to using death certificate data are well understood. Of particular relevance to this study are concerns that deaths caused specifically by opioids may be undercounted on death certificates (Ruhm 2017a, 2017b). We therefore combine deaths attributed to opioids and other drugs into a single category1 and generally discuss our findings for the broad set of “deaths of despair,” which include other drug and alcohol related deaths, and suicides. More broadly, deaths may be misclassified and the death certificate may list as primary the proximate cause, even if there were other distal contributors or comorbidities (Manton and Stallard 1984). Despite such limitations, these data include important information and sample sizes for the subgroups of interest not found elsewhere.
Researchers studying the changes over time in the mortality gradient have either analyzed population level vital statistics matched to population level census data as we do (e.g., Bound et al. 2015; Case and Deaton 2015, 2017; Olshansky et al. 2012; Sasson 2016) or have used nationally representative survey data linked with mortality vital statistics data for the survey sample members (e.g., Hendi 2015; Ho 2017; Ho and Fenelon 2015; Meara et al. 2008). There are potential limitations with either source of data. However, the data we use provides the only data with sufficient sample sizes for the purposes of fulfilling our primary objectives of focusing on black and white populations stratified by education and considering a comprehensive set of causes of death, rather than simply a single cause or the most common ones. In contexts in which linked survey sample data can be compared to matched population-level vital statistics and census data, Sasson (2017) found the two showed similar results in terms of trends, though the linked survey sample data consistently show lower overall mortality rates than do the population level data. Lower rates in linked survey compared to population data are consistent with the exclusion of the incarcerated and the well-known underrepresentation of members of vulnerable groups, more generally, in survey samples (Brown, Lariscy, and Kalousová 2018; Sasson 2017).
Finally, for a variety of reasons, including the fact that entire populations are being used in calculations, researchers do not typically report confidence intervals for LE or YLL estimates. However, because sampling rates for census sources containing education information varied between years, we did calculations confirming the fact that confidence intervals are small enough that meaningful differences will, typically, be statistically distinct. (See online Methodological Appendix and Table A3.)
Results
Table 1 lists YLL from ages 25 through 84, separately for 1990 and 2015, overall and disaggregated by sex, race, and educational rank. In all cases, women’s longer life expectancy compared to men’s is reflected in fewer YLL, although the gender gap narrows between 1990 and 2015 because women experience smaller gains in life expectancy than men. Overall, differences in YLL between whites and blacks also decrease over time, falling from 6.31 to 3.18 years for men and from 3.98 to 2.00 years for women. In each year, whites have fewer YLL than their black same-sex counterparts, with one exception: In 2015, white women in the lowest educational quartile effectively converged with black women in terms of YLL (also see Figure 1).
Table 1.
Years of life lost between ages 25-84 by sex, race, and educational rank, 1990 and 2015
| Men | Women | |||
|---|---|---|---|---|
| 1990 | 2015 | 1990 | 2015 | |
| Non-Hispanic White | ||||
| Total | 11.71 | 9.81 | 7.30 | 6.74 |
| Low Education | 14.38 | 14.91 | 8.67 | 10.92 |
| High Education | 11.07 | 8.34 | 7.00 | 5.71 |
| Education gap | 3.31 | 6.57 | 1.67 | 5.21 |
| Non-Hispanic Black | ||||
| Total | 18.02 | 12.99 | 11.28 | 8.74 |
| Low Education | 19.07 | 16.43 | 11.49 | 10.77 |
| High Education | 17.69 | 12.09 | 11.18 | 8.23 |
| Education gap | 1.37 | 4.35 | 0.31 | 2.54 |
Note: Low Education refers to bottom 25 percent of education distribution, and High Education refers to the top 75% of the education distribution within cohorts defined by sex, race/ethnicity, and year of birth. Education Gap=YLL in Low Education group minus YLL in the High Education group. Data on education distribution and population counts derived from U.S. decennial Census, 1940-2000 and American Community Survey, 2010 and 2015, accessed via IPUMS (Ruggles et al. 2017). Sample sizes are 234,509, 79,131, 252,632, 265,482, 1,933,828, 2,093801, 1,784,705, 333,3260, and 345,176, respectively. Mortality data derived from the Centers for Disease Control and Prevention Multiple Cause of Death files for 1990 and 2015; sample sizes are 2,151,890 and 2,718,198, respectively.
Figure 1. Trends in Years of Life Lost, 1990-2015, by sex, race, and educational rank.
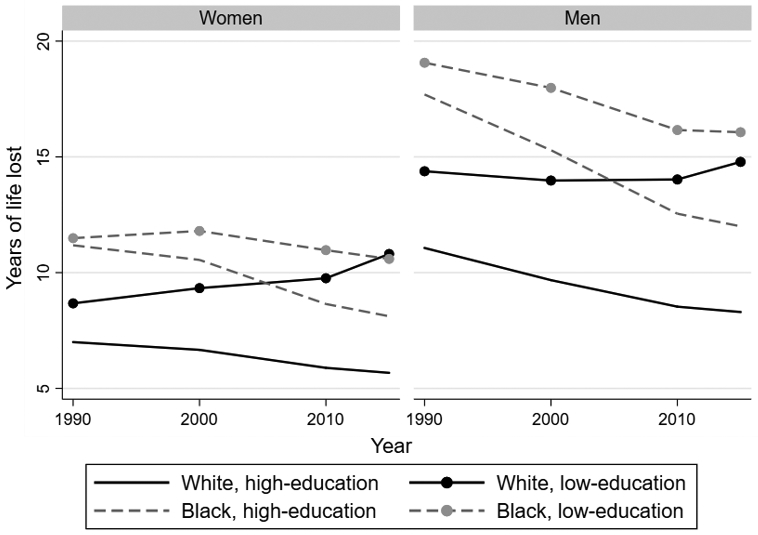
Note: Low education refers to bottom 25 percent of education distribution, and high education refers to the top 75 percent of the education distribution within cohorts defined by sex, race/ethnicity, and year of birth. Data on education distribution and population counts derived from U.S. decennial Census, 1940-2000 and American Community Survey, 2010 and 2015, accessed via IPUMS (Ruggles et al. 2017). Sample sizes are 234,509, 79,131, 252,632, 265,482, 1,933,828, 2,093801, 1,784,705, 333,3260, and 345,176, respectively. Mortality data derived from the Centers for Disease Control and Prevention Multiple Cause of Death files for 1990, 2000, 2010, and 2015; sample sizes are 2,151,890, 2,407,193, 2,472,542, and 2,718,198, respectively.
Both blacks and whites, men and women, show increased inequality in YLL between the lowest and higher education categories between 1990 and 2015. Among whites, both decreasing life expectancy among the lowest educational quartile, especially among women, and increasing life expectancy among the higher educational quartiles play important roles in widening the gap. Notably, for blacks, very small educational gaps in YLL in 1990 (only 1.37 years for men; .31 years for women) increased to sizeable gaps by 2015 (4.35 years for men; 2.54 years for women), largely due to increasing life expectancy among blacks in the higher educational quartiles, consistent with findings reported by Sasson (2016).
Table 2 shows the number of YLL for each educational group in 1990 and 2015; the change in YLL between 1990 and 2015 for each educational group, and the change in the educational YLL gap between 1990 and 2015, in total and broken down by cause, for each race/sex group. The final column of each panel shows the share of the total change in the size of the educational gap in YLL between 1990 and 2015 due to each specific cause. Thus, for example, we see that opioid and other drug deaths accounted for a small number of YLL for white men in 1990 (.29 or .13 years depending on educational rank),but became quantitatively more important in 2015 (1.57 or .63 years). This implies that opioid and other drug deaths account for .79 years or 24% of the growing educational inequity in YLL for white men. Deaths to cardiovascular diseases contributed 19% to the growth of this inequity among white men; however, this gap grew because CVD deaths declined more for white men in the high-education group than in the low-education group. Other [non-lung] cancers contributed 21% to the increasing educational inequity among white men. In this case, the growing inequity was a function of increases in YLL among white men in the low-education group and decreases in the high-education group.
Table 2.
Change in Years of Life Lost between ages 25 and 84, by race, sex, education, and cause of death, 1990-2015
| Non-Hispanic white men | Non-Hispanic black men | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Low Ed | High Ed | Change in gap |
Share of total |
Low Ed | High Ed | Change in gap |
Share of total |
|||||||||
| 1990 | 2015 | Chg | 1990 | 2015 | Chg | 1990 | 2015 | Chg | 1990 | 2015 | Chg | |||||
| Opioids & other drugs | 0.29 | 1.57 | 1.28 | 0.13 | 0.63 | 0.49 | 0.79 | 24% | 0.56 | 0.81 | 0.25 | 0.37 | 0.49 | 0.12 | 0.13 | 5% |
| Non-drug suicide | 0.61 | 0.82 | 0.21 | 0.37 | 0.47 | 0.10 | 0.11 | 3% | 0.27 | 0.26 | −0.01 | 0.24 | 0.19 | −0.05 | 0.04 | 1% |
| Alcoholic liver | 0.22 | 0.30 | 0.07 | 0.13 | 0.16 | 0.03 | 0.04 | 1% | 0.44 | 0.14 | −0.30 | 0.29 | 0.09 | −0.19 | −0.11 | −4% |
| Total Deaths of Despair | 1.12 | 2.68 | 1.56 | 0.63 | 1.25 | 0.62 | 0.94 | 29% | 1.27 | 1.21 | −0.06 | 0.90 | 0.77 | −0.12 | 0.06 | 2% |
| Cardiovascular disease | 5.03 | 3.63 | −1.39 | 4.14 | 2.13 | −2.00 | 0.61 | 19% | 5.38 | 4.71 | −0.67 | 5.77 | 3.77 | −2.00 | 1.33 | 45% |
| Lung cancer | 1.59 | 1.09 | −0.50 | 1.16 | 0.54 | −0.61 | 0.11 | 3% | 1.54 | 0.93 | −0.61 | 1.60 | 0.70 | −0.90 | 0.29 | 10% |
| Other cancer | 2.00 | 2.20 | 0.20 | 2.09 | 1.61 | −0.48 | 0.68 | 21% | 2.35 | 2.27 | −0.07 | 2.82 | 1.97 | −0.86 | 0.78 | 26% |
| HIV | 0.31 | 0.05 | −0.26 | 0.39 | 0.03 | −0.36 | 0.09 | 3% | 1.09 | 0.38 | −0.71 | 1.09 | 0.22 | −0.87 | 0.15 | 5% |
| Other infectious disease | 0.16 | 0.35 | 0.19 | 0.13 | 0.17 | 0.05 | 0.14 | 4% | 0.42 | 0.46 | 0.03 | 0.35 | 0.35 | 0.00 | 0.03 | 1% |
| Diabetes | 0.27 | 0.45 | 0.18 | 0.21 | 0.26 | 0.04 | 0.14 | 4% | 0.38 | 0.67 | 0.29 | 0.43 | 0.56 | 0.13 | 0.16 | 5% |
| Lower respiratory | 0.67 | 0.81 | 0.13 | 0.43 | 0.36 | −0.07 | 0.20 | 6% | 0.34 | 0.46 | 0.12 | 0.41 | 0.34 | −0.07 | 0.19 | 6% |
| Kidney disease | 0.09 | 0.18 | 0.09 | 0.06 | 0.10 | 0.04 | 0.05 | 2% | 0.20 | 0.39 | 0.19 | 0.20 | 0.31 | 0.11 | 0.08 | 3% |
| Other liver | 0.16 | 0.19 | 0.02 | 0.11 | 0.09 | −0.02 | 0.04 | 1% | 0.21 | 0.13 | −0.08 | 0.17 | 0.09 | −0.08 | 0.00 | 0% |
| Mental/behavioral | 0.08 | 0.12 | 0.04 | 0.04 | 0.08 | 0.04 | 0.00 | 0% | 0.15 | 0.15 | 0.00 | 0.10 | 0.12 | 0.03 | −0.02 | −1% |
| Other internal | 1.35 | 1.88 | 0.52 | 0.98 | 1.09 | 0.12 | 0.41 | 12% | 2.20 | 2.01 | −0.18 | 1.84 | 1.48 | −0.37 | 0.18 | 6% |
| Accidents/undetermined | 1.26 | 1.09 | −0.17 | 0.60 | 0.54 | −0.07 | −0.10 | −3% | 1.49 | 1.06 | −0.43 | 0.97 | 0.67 | −0.30 | −0.13 | −4% |
| Homicide | 0.26 | 0.16 | −0.10 | 0.08 | 0.05 | −0.03 | −0.07 | −2% | 2.00 | 1.56 | −0.45 | 1.01 | 0.71 | −0.30 | −0.15 | −5% |
| All other causes | 0.02 | 0.03 | 0.01 | 0.02 | 0.02 | 0.00 | 0.01 | 0% | 0.05 | 0.05 | 0.00 | 0.04 | 0.03 | −0.01 | 0.01 | 0% |
| Total | 14.38 | 14.91 | 0.53 | 11.07 | 8.34 | −2.72 | 3.26 | 19.07 | 16.43 | −2.63 | 17.69 | 12.09 | −5.61 | 2.98 | ||
| Non-Hispanic white women | Non-Hispanic black women | |||||||||||||||
| Low Ed | High Ed | Change in gap |
Share of total |
Low Ed | High Ed | Change in gap |
Share of total |
|||||||||
| 1990 | 2015 | Chg | 1990 | 2015 | Chg | 1990 | 2015 | Chg | 1990 | 2015 | Chg | |||||
| Opioids & other drugs | 0.12 | 0.96 | 0.84 | 0.07 | 0.34 | 0.27 | 0.57 | 16% | 0.24 | 0.41 | 0.17 | 0.11 | 0.22 | 0.11 | 0.06 | 3% |
| Non-drug suicide | 0.10 | 0.18 | 0.08 | 0.08 | 0.12 | 0.03 | 0.04 | 1% | 0.04 | 0.04 | 0.00 | 0.04 | 0.03 | −0.01 | 0.01 | 0% |
| Alcoholic liver | 0.07 | 0.15 | 0.08 | 0.05 | 0.08 | 0.03 | 0.06 | 2% | 0.22 | 0.09 | −0.13 | 0.12 | 0.05 | −0.06 | −0.07 | −3% |
| Total Deaths of Despair | 0.29 | 1.30 | 1.01 | 0.21 | 0.54 | 0.33 | 0.68 | 19% | 0.50 | 0.54 | 0.03 | 0.27 | 0.30 | 0.03 | 0.00 | 0% |
| Cardiovascular disease | 2.98 | 2.32 | −0.66 | 2.22 | 1.18 | −1.04 | 0.38 | 11% | 4.23 | 3.08 | −1.14 | 4.22 | 2.39 | −1.83 | 0.68 | 31% |
| Lung cancer | 0.78 | 0.92 | 0.14 | 0.66 | 0.46 | −0.20 | 0.34 | 10% | 0.52 | 0.55 | 0.04 | 0.66 | 0.44 | −0.22 | 0.25 | 11% |
| Other cancer | 1.99 | 1.99 | 0.00 | 2.10 | 1.43 | −0.67 | 0.67 | 19% | 2.05 | 2.07 | 0.02 | 2.61 | 1.92 | −0.69 | 0.71 | 32% |
| HIV | 0.03 | 0.02 | −0.01 | 0.01 | 0.00 | −0.01 | 0.00 | 0% | 0.45 | 0.25 | −0.19 | 0.17 | 0.10 | −0.08 | −0.11 | −5% |
| Other infectious disease | 0.11 | 0.32 | 0.21 | 0.09 | 0.15 | 0.06 | 0.15 | 4% | 0.29 | 0.39 | 0.10 | 0.26 | 0.28 | 0.02 | 0.08 | 3% |
| Diabetes | 0.31 | 0.33 | 0.02 | 0.19 | 0.16 | −0.03 | 0.05 | 1% | 0.56 | 0.57 | 0.01 | 0.54 | 0.41 | −0.14 | 0.15 | 7% |
| Lower respiratory | 0.44 | 0.89 | 0.45 | 0.33 | 0.37 | 0.05 | 0.41 | 12% | 0.23 | 0.37 | 0.14 | 0.23 | 0.28 | 0.05 | 0.09 | 4% |
| Kidney disease | 0.07 | 0.16 | 0.08 | 0.05 | 0.08 | 0.03 | 0.06 | 2% | 0.18 | 0.33 | 0.16 | 0.18 | 0.24 | 0.06 | 0.10 | 4% |
| Other liver | 0.09 | 0.13 | 0.05 | 0.07 | 0.06 | 0.00 | 0.05 | 1% | 0.14 | 0.08 | −0.06 | 0.10 | 0.05 | −0.04 | −0.02 | −1% |
| Mental/behavioral | 0.05 | 0.17 | 0.12 | 0.03 | 0.10 | 0.06 | 0.05 | 2% | 0.09 | 0.14 | 0.05 | 0.05 | 0.12 | 0.07 | −0.02 | −1% |
| Other internal | 1.03 | 1.83 | 0.81 | 0.76 | 0.92 | 0.17 | 0.64 | 18% | 1.47 | 1.86 | 0.39 | 1.35 | 1.38 | 0.03 | 0.36 | 16% |
| Accidents/undetermined | 0.40 | 0.44 | 0.05 | 0.24 | 0.22 | −0.02 | 0.07 | 2% | 0.38 | 0.33 | −0.05 | 0.30 | 0.21 | −0.09 | 0.03 | 1% |
| Homicide | 0.09 | 0.07 | −0.02 | 0.04 | 0.03 | −0.01 | 0.00 | 0% | 0.39 | 0.19 | −0.21 | 0.22 | 0.09 | −0.13 | −0.08 | −3% |
| All other causes | 0.01 | 0.02 | 0.00 | 0.01 | 0.01 | 0.00 | 0.01 | 0% | 0.02 | 0.02 | 0.00 | 0.02 | 0.02 | −0.01 | 0.01 | 0% |
| Total | 8.67 | 10.92 | 2.24 | 7.00 | 5.71 | −1.29 | 3.54 | 11.49 | 10.77 | −0.72 | 11.18 | 8.23 | −2.96 | 2.24 | ||
Note: Low Education refers to bottom 25 percent of education distribution, and High Education refers to the top 75 percent of the education distribution within cohorts defined by sex, race/ethnicity, and year of birth. Data on education distribution and population counts derived from U.S. decennial Census, 1940-2000 and American Community Survey, 2010 and 2015, accessed via IPUMS (Ruggles et al. 2017). Sample sizes are 234,509, 79,131, 252,632, 265,482, 1,933,828, 2,093801, 1,784,705, 333,3260, and 345,176, respectively. Mortality data derived from the Centers for Disease Control and Prevention Multiple Cause of Death files for 1990 and 2015; sample sizes are 2,151,890 and 2,718,198, respectively.
For white men, aggregated DOD account for 29% of the increase; yet for black men they account for only 2%. For white women, DOD account for 19%, while for black women DOD account for 0%. The convergence in YLL between low education blacks and whites seen in Figure 1 is only partially accounted for by the growth in drug-related deaths among white men and women.
Changes in CVD deaths are important in every group although the size of their contribution varies from 19% for white men to 45% for black men; and from 11% for white women to 31% for black women. Overall, the increase in the educational gap is a function of greater declines for high-education compared to low-education groups across race and gender. Changes in deaths from all cancers account for 24% (white men), 36% (black men), 29% (white women), and 43% (black women) of the growing educational LE disparity.
We also looked at changes in and contributors to YLL for working age adults (25–64) separately, where one would expect DOD to have their largest impact (see Table 3). We did find that DOD account for 82% of the widening gap in YLL between ages 25–64 among white men and 50% among white women, consistent with previous studies that find opioid and other drug deaths are the largest contributors to growth in educational inequity in LE for whites in this age group (Table 3). Yet, the total increase (across all causes) in the educational gap in YLL is small for white men in this younger age group (.57 years out of the total 3.76 years for all ages) and for white women (.67 years out of the total 3.46 years for all ages). Among blacks, DOD are not driving growing educational inequality in LE even at the younger ages.
Table 3:
Change in years of life lost between ages 25 and 64, by race, sex, education, and cause of death, 1990–2015
| Non-Hispanic white men | Non-Hispanic black men | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Low Ed | High Ed | Change in gap |
Share of total |
Low Ed | High Ed | Change in gap |
Share of total |
|||||||||
| 1990 | 2015 | Chg | 1990 | 2015 | Chg | 1990 | 2015 | Chg | 1990 | 2015 | Chg | |||||
| Opioids & other drugs | 0.14 | 0.81 | 0.67 | 0.06 | 0.31 | 0.26 | 0.42 | 73% | 0.28 | 0.36 | 0.09 | 0.16 | 0.20 | 0.04 | 0.05 | −39% |
| Non-drug suicide | 0.30 | 0.40 | 0.10 | 0.16 | 0.21 | 0.06 | 0.04 | 7% | 0.15 | 0.14 | −0.01 | 0.12 | 0.10 | −0.03 | 0.01 | −12% |
| Alcoholic liver | 0.08 | 0.10 | 0.02 | 0.04 | 0.05 | 0.01 | 0.01 | 1% | 0.20 | 0.04 | −0.16 | 0.11 | 0.02 | −0.08 | −0.07 | 61% |
| Total Deaths of Despair | 0.53 | 1.31 | 0.79 | 0.25 | 0.57 | 0.32 | 0.46 | 82% | 0.63 | 0.54 | −0.09 | 0.39 | 0.32 | −0.07 | −0.01 | 10% |
| Cardiovascular disease | 0.96 | 0.73 | −0.23 | 0.56 | 0.34 | −0.22 | −0.01 | −2% | 1.49 | 1.14 | −0.35 | 1.19 | 0.76 | −0.43 | 0.08 | −62% |
| Lung cancer | 0.29 | 0.15 | −0.14 | 0.16 | 0.06 | −0.10 | −0.04 | −7% | 0.37 | 0.14 | −0.23 | 0.30 | 0.08 | −0.21 | −0.02 | 13% |
| Other cancer | 0.41 | 0.41 | 0.00 | 0.34 | 0.25 | −0.09 | 0.09 | 16% | 0.59 | 0.45 | −0.14 | 0.54 | 0.32 | −0.23 | 0.09 | −73% |
| HIV | 0.18 | 0.02 | −0.16 | 0.21 | 0.01 | −0.20 | 0.04 | 6% | 0.63 | 0.15 | −0.47 | 0.59 | 0.08 | −0.51 | 0.03 | −28% |
| Other infectious disease | 0.05 | 0.08 | 0.03 | 0.03 | 0.03 | 0.00 | 0.03 | 6% | 0.16 | 0.11 | −0.05 | 0.11 | 0.06 | −0.04 | 0.00 | 4% |
| Diabetes | 0.07 | 0.10 | 0.03 | 0.04 | 0.04 | 0.01 | 0.03 | 4% | 0.11 | 0.16 | 0.06 | 0.10 | 0.11 | 0.02 | 0.04 | −33% |
| Lower respiratory | 0.07 | 0.08 | 0.01 | 0.03 | 0.03 | 0.00 | 0.01 | 2% | 0.07 | 0.08 | 0.00 | 0.06 | 0.04 | −0.02 | 0.02 | −17% |
| Kidney disease | 0.02 | 0.03 | 0.01 | 0.01 | 0.01 | 0.00 | 0.01 | 1% | 0.06 | 0.09 | 0.03 | 0.05 | 0.05 | 0.01 | 0.02 | −17% |
| Other liver | 0.05 | 0.05 | 0.00 | 0.03 | 0.02 | −0.01 | 0.00 | 0% | 0.09 | 0.03 | −0.06 | 0.06 | 0.02 | −0.04 | −0.02 | 15% |
| Mental/behavioral | 0.02 | 0.01 | −0.02 | 0.01 | 0.00 | 0.00 | −0.01 | −2% | 0.07 | 0.01 | −0.06 | 0.03 | 0.01 | −0.03 | −0.03 | 26% |
| Other internal | 0.35 | 0.46 | 0.11 | 0.17 | 0.19 | 0.02 | 0.09 | 15% | 0.83 | 0.57 | −0.27 | 0.53 | 0.34 | −0.19 | −0.08 | 65% |
| Accidents/undetermined | 0.63 | 0.48 | −0.15 | 0.26 | 0.21 | −0.06 | −0.09 | −16% | 0.75 | 0.48 | −0.27 | 0.43 | 0.29 | −0.15 | −0.12 | 101% |
| Homicide | 0.14 | 0.08 | −0.06 | 0.04 | 0.03 | −0.01 | −0.04 | −7% | 1.17 | 0.91 | −0.27 | 0.55 | 0.40 | −0.15 | −0.12 | 98% |
| All other causes | 0.01 | 0.01 | 0.01 | 0.00 | 0.00 | 0.00 | 0.00 | 1% | 0.02 | 0.02 | 0.00 | 0.01 | 0.01 | 0.00 | 0.00 | −2% |
| Total | 3.76 | 4.00 | 0.23 | 2.13 | 1.80 | −0.33 | 0.57 | 7.04 | 4.88 | −2.16 | 4.94 | 2.90 | −2.04 | −0.12 | ||
| Non-Hispanic white women | Non-Hispanic black women | |||||||||||||||
| Low Ed | High Ed | Change in gap |
Share of total |
Low Ed | High Ed | Change in gap |
Share of total |
|||||||||
| 1990 | 2015 | Chg | 1990 | 2015 | Chg | 1990 | 2015 | Chg | 1990 | 2015 | Chg | |||||
| Opioids & other drugs | 0.06 | 0.49 | 0.43 | 0.03 | 0.16 | 0.13 | 0.30 | 44% | 0.13 | 0.19 | 0.06 | 0.05 | 0.10 | 0.05 | 0.02 | 26% |
| Non-drug suicide | 0.05 | 0.09 | 0.04 | 0.04 | 0.05 | 0.02 | 0.02 | 3% | 0.02 | 0.02 | 0.00 | 0.02 | 0.02 | 0.00 | 0.00 | 5% |
| Alcoholic liver | 0.03 | 0.06 | 0.03 | 0.02 | 0.03 | 0.01 | 0.02 | 3% | 0.11 | 0.04 | −0.07 | 0.04 | 0.02 | −0.03 | −0.05 | −74% |
| Total Deaths of Despair | 0.14 | 0.64 | 0.51 | 0.08 | 0.24 | 0.16 | 0.35 | 50% | 0.26 | 0.24 | −0.01 | 0.11 | 0.13 | 0.02 | −0.03 | −42% |
| Cardiovascular disease | 0.41 | 0.39 | −0.02 | 0.21 | 0.16 | −0.05 | 0.03 | 5% | 0.95 | 0.69 | −0.26 | 0.68 | 0.43 | −0.25 | −0.01 | −13% |
| Lung cancer | 0.16 | 0.12 | −0.04 | 0.10 | 0.05 | −0.05 | 0.01 | 1% | 0.12 | 0.09 | −0.04 | 0.13 | 0.06 | −0.07 | 0.03 | 53% |
| Other cancer | 0.47 | 0.38 | −0.08 | 0.41 | 0.26 | −0.14 | 0.06 | 9% | 0.55 | 0.48 | −0.07 | 0.59 | 0.39 | −0.20 | 0.13 | 207% |
| HIV | 0.01 | 0.01 | −0.01 | 0.01 | 0.00 | −0.01 | 0.00 | 0% | 0.26 | 0.11 | −0.14 | 0.09 | 0.04 | −0.06 | −0.09 | −138% |
| Other infectious disease | 0.03 | 0.07 | 0.04 | 0.01 | 0.02 | 0.01 | 0.03 | 5% | 0.10 | 0.09 | −0.01 | 0.07 | 0.05 | −0.01 | 0.01 | 12% |
| Diabetes | 0.05 | 0.07 | 0.01 | 0.03 | 0.03 | 0.00 | 0.01 | 2% | 0.13 | 0.13 | 0.00 | 0.09 | 0.07 | −0.01 | 0.01 | 18% |
| Lower respiratory | 0.06 | 0.10 | 0.03 | 0.03 | 0.03 | 0.00 | 0.03 | 4% | 0.06 | 0.07 | 0.00 | 0.04 | 0.04 | 0.00 | 0.01 | 12% |
| Kidney disease | 0.01 | 0.02 | 0.01 | 0.01 | 0.01 | 0.00 | 0.01 | 1% | 0.04 | 0.07 | 0.03 | 0.03 | 0.04 | 0.01 | 0.03 | 42% |
| Other liver | 0.02 | 0.03 | 0.01 | 0.01 | 0.01 | 0.00 | 0.01 | 1% | 0.06 | 0.02 | −0.03 | 0.03 | 0.01 | −0.02 | −0.02 | −26% |
| Mental/behavioral | 0.01 | 0.01 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0% | 0.03 | 0.01 | −0.02 | 0.01 | 0.00 | −0.01 | −0.02 | −24% |
| Other internal | 0.24 | 0.41 | 0.18 | 0.12 | 0.15 | 0.03 | 0.14 | 20% | 0.51 | 0.55 | 0.04 | 0.34 | 0.32 | −0.02 | 0.06 | 98% |
| Accidents/undetermined | 0.18 | 0.18 | 0.00 | 0.09 | 0.08 | −0.01 | 0.01 | 2% | 0.18 | 0.14 | −0.05 | 0.11 | 0.08 | −0.04 | −0.01 | −14% |
| Homicide | 0.05 | 0.04 | −0.01 | 0.02 | 0.01 | −0.01 | 0.00 | −1% | 0.23 | 0.10 | −0.13 | 0.12 | 0.05 | −0.07 | −0.06 | −91% |
| All other causes | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0% | 0.01 | 0.01 | 0.00 | 0.01 | 0.00 | 0.00 | 0.00 | 4% |
| Total | 1.85 | 2.48 | 0.63 | 1.12 | 1.06 | −0.07 | 0.70 | 3.49 | 2.81 | −0.68 | 2.45 | 1.70 | −0.75 | 0.06 | ||
Note: Low Education refers to bottom 25 percent of education distribution, and High Education refers to the top 75% of the education distribution within cohorts defined by sex, race/ethnicity, year of birth. Data on education distribution and population counts derived from U.S. decennial Census, 1940-2000 and American Community Survey, 2010 and 2015, accessed via IPUMS (Ruggles et al. 2017). Sample sizes are 234,509, 79,131, 252,632, 265,482, 1,933,828, 2,093801, 1,784,705, 333,3260, and 345,176, respectively. Mortality data derived from the Centers for Disease Control and Prevention Multiple Cause of Death files for 1990 and 2015; sample sizes are 2,151,890 and 2,718,198, respectively.
Figure 2 displays the growth in the educational gap in YLL by cause. The black portion of each bar represents deaths at ages 25 through 64; the grey portion reflects deaths at ages 65 through 84. The figure clarifies that opioid and other drug overdose deaths for blacks did not contribute importantly to the growing educational gap as they did for whites—this despite a persistent black disadvantage in earnings and education throughout the period. Each of the component causes of DOD contributes to growing inequity among white women and men, although opioid and other drug overdoses make substantially larger contributions than suicide or alcoholic liver disease. To illustrate, while among whites DOD account for 29% and 19% of the growing educational inequity for men and women (Table 2), respectively, less than 5% of the gap is explained by suicide and alcoholic liver disease deaths. Even limiting the estimates to 25–64-year-old whites, where opioid and other drug deaths are the major contributors, only 8% of the gap for men and 6% for women (Table 3) are accounted for by suicide and alcoholic liver disease deaths, compared to 73% and 44% of the growing educational inequity due to opioids and other drugs for men and women, respectively.
Figure 2. Change in Education Gap in Years of Life Lost (YLL), 1990-2015, by race, sex, and age range.
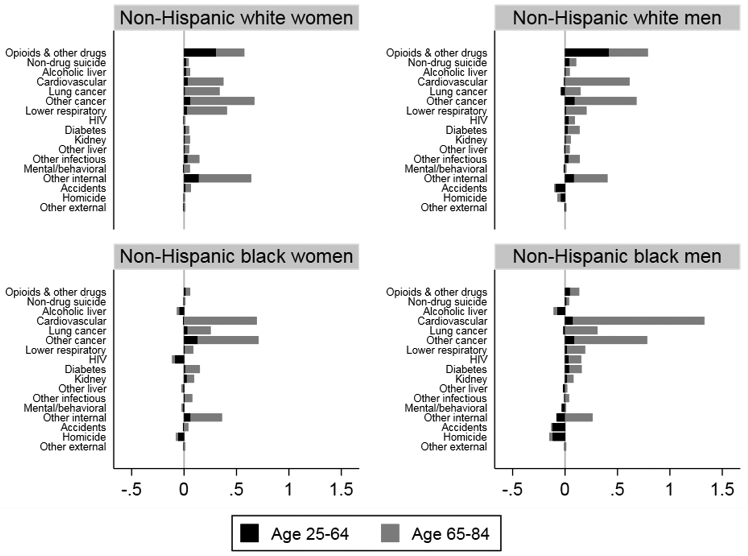
Note: Graph measures change in difference between High and Low-education groups, measured in years of life lost. Low Education refers to bottom 25 percent of education distribution, and High Education refers to the top 75 percent of the education distribution within cohorts defined by sex, race/ethnicity, and year of birth. Data on education distribution and population counts derived from U.S. decennial Census, 1940-2000 and American Community Survey, 2010 and 2015, accessed via IPUMS (Ruggles et al. 2017). Sample sizes are 234,509, 79,131, 252,632, 265,482, 1,933,828, 2,093801, 1,784,705, 333,3260, and 345,176, respectively. Mortality data derived from the Centers for Disease Control and Prevention Multiple Cause of Death files for 1990 and 2015; sample sizes are 2,151,890 and 2,718,198, respectively.
Among blacks, the contribution of each component cause of DOD is smaller than among their white counterparts. In the cases of alcoholic liver disease among black men and women, and other drug overdoses among black women, they work to narrow the educational inequity, not increase it. Declines in deaths to external causes including homicide and accidents – a category that some suggest includes misclassified suicides (Rockett, Samora, and Coben 2006)– also narrowed the gap for all groups except nonHispanic white women, for whom homicide made no contribution, while the contribution of accidents was very small. In all demographic groups studied, especially blacks, the contributions of growing educational inequities in cardiovascular disease and cancer deaths were substantial. Considering ages 25 through 64 alone, consistent with other researchers, we find opioid and other drug deaths are the largest contributors to growth in educational inequity in LE for whites. Other (non-lung) cancers are the largest contributor to the growth in educational inequity in LE for blacks in this age group. For whites and blacks, deaths at ages 25 through 64 explain relatively little of the growth in the educational inequity in YLL. Most of the growth in educational inequity in YLL occurs in the 65+ age range
Discussion
Our findings are consistent with other studies confirming that educational inequity in LE has grown for nonHispanic blacks and nonHispanic whites, men and women, and extend them to show continued, even accelerated, growth through 2015. Between 1990 and 2015, whites show larger growth in educational inequity in YLL than blacks, and white women show the largest growth. In all groups, only a small share of the growth in the educational gap in YLL occurs among 25–64 year olds, with the lion’s share occurring at ages 65–84 years.
Consistent with earlier researchers, we find the contribution of drug overdose deaths increased substantially over the study period for whites, particularly in the 25–64-year age group. However, in the specific context of growing LE inequities, our findings question the merit of aggregating opioid and other drug overdose deaths with suicide and alcoholic liver disease or viewing them all as a coalescent conceptualization of “deaths of despair.”
Conceptually, in assessing the DOD narrative, it is worthwhile to recall that the word despair is defined as “the complete loss or absence of hope.” Certainly, suicide deaths are likely to reflect the absence of hope, but is despair the dominant explanation of chronic liver disease or opioid overdose deaths? Death to chronic liver disease is the endpoint of decades-long alcoholism for which despair may be one contributor, along with Hepatitis C, exposure to other toxins, and genetic predisposition. And, as noted, the explosion in opioid deaths may be accounted for by changes in drug composition, supply and marketing.
Empirically, the contribution to the increasing educational gradient of opioid and other drug overdoses is substantial in whites, but the contribution of deaths to suicide or alcoholic liver disease is far less substantial, and in some cases is zero or negative. In all demographic groups studied, especially blacks, we found the contributions of growing educational inequities in CVD, cancer, and other internal causes of death larger than the contributions of inequities in suicide or alcoholic liver disease. For white and black women and for black men, lower respiratory diseases (emphysema, chronic bronchitis, and asthma) contributed a larger share than DOD to the inequitable growth in YLL by educational rank during the study period. Our findings are consistent with Phillips and Hempstead (2017), who found that the gap in suicide rates between high school and college graduates grew only slightly from 2005–2014 for middle-aged women, and not at all for men. Our findings also confirm the conclusion of Masters et al. (2018) and Meunnig et al. (2018) that opioid and other drug overdoses are driving the impact of DOD on the growth in educational inequity in life expectancy of whites ages 45–54, and extend these findings to a broader age group of US whites and to US blacks.
Our findings highlight the urgency of focusing on what might account for growing rates of excess death due to chronic disease among the less educated, in particular excess deaths to cardiovascular diseases and non-lung cancers. As noted, the Weathering (Geronimus 1992; Geronimus et al. 2006, 2015) and John Henryism (Bennett et al. 2004; James 1994) hypotheses may provide theoretical guidance. They emphasize the health costs of tenacious high-effort coping with adversity. The findings of an increasing number of social epidemiological studies incorporating biomeasures are suggestive that stress-related chronic disease risks may have grown among the less-educated, including in response to growing economic hardship and social inequity (Rodriguez et al. 2019). Seeman et al. (2018) found the 2008 Great Recession adversely impacted the blood pressure, fasting glucose, and medication usage of those study participants most likely to be affected. Studies find evidence that racial/ethnic (Geronimus et al. 2006; Rodriguez et al. 2019) and socioeconomic (Seeman et al. 2010) inequalities in allostatic load scores – an indicator of stress-mediated wear and tear across body systems – increase across young through middle adulthood, indicating the early onset of chronic diseases in disadvantaged populations that may lead to excess deaths, especially in medically underserved populations. In a 10-year prospective cohort study of midlife women, Moody et al. (2018) found that everyday discrimination contributed to increased central adiposity and elevated blood pressure. Miller et al. (2015) found that poor black youth in Georgia exhibiting higher self-control and academic resilience in the face of adversity show accelerated cellular aging compared to their peers. In sum, for the economically or socially most vulnerable, sustained experience with material, environmental and psychosocial stressors that activate harmful and cumulative biopsychosocial adaptations over the life-course may dysregulate and ultimately, exhaust neuro-endocrine, cardiovascular, metabolic, and immune systems and accelerate cellular aging, enhancing risk of early disease onset and ultimately, excess death (Cohen et al. 2015; Cohen, Janicki-Deverts, and Miller 2007; Epel and Lithgow 2014; Geronimus et al. 2006, 2015; Gruenewald et al. 2009; James et al. 1987; Janicki-Deverts et al. 2008; McEwen 1998; McEwen and Gianaros 2010; McEwen and Stellar 1993; Thoits 2010).
Race and Gender
Our findings also speak to trends in health inequities along the vectors of race and gender. While still substantial, black-white inequities in YLL have been reduced by about half over the study period, largely as a function of decreases among more-educated blacks and increases among less-educated whites. While decreasing YLL among blacks in the higher educational category is a positive development, it occurred against the baseline of little educational group differential in YLL for black men in 1990, and none for black women. An open question that deserves further study is the extent to which the decrease in YLL for blacks in the higher educational group relative to the low education group, reflects improved health status or greater access to health services that prevent incident cases of disease from becoming case fatalities (Geronimus et al. 2001).
Consistent with Sasson’s (2016) findings, between 1990 and 2010, highly educated black men showed a steeper decline in YLL than less educated black men. However, we found the less educated group experienced a reversal leading to greater YLL in 2015 than they had achieved in 2010 as well as greater within-race educational inequity in YLL. After modest ups and downs, less educated black women showed only a small improvement of .07 years in YLL between 1990 and 2015. Our findings also show that much of the narrowing of black/white inequities can be accounted for by reductions in homicide, accidents, and HIV deaths, for black men and women, together with the rise in drug deaths for white men and women.
The gender gap also declined during the study period, largely due to women experiencing increases, or smaller decreases, in YLL compared to men, depending on the specific race and age group. Of all groups, only white women have shown evidence of decreasing life expectancy throughout the 25-year period. Researchers who studied white women in the earlier sections of our study period found smoking rates to be an important contributor to women’s death rates (Ho and Fenelon 2015; Meara et al. 2008; Montez and Zajacova 2013b). Consistent with these studies, we found that smoking rates, while consistently higher for less educated white men than their female counterparts, declined in white men such that an estimated .6 fewer YLL between 1990 and 2015 could be accounted for by less smoking (see our calculations presented in the online Methodological Appendix). For less educated white women across the relevant cohorts, smoking behavior changed little. Thus, our calculations suggest gender differences in smoking trends can explain some of the white gender differences in trends in YLL. However, we found no trend in smoking rates for less educated white women that would have clear implications for their rising mortality rates to the level of less educated black women’s by 2015. Actually, inequities in lung cancer deaths narrowed the educational inequity in LE among black and white men, while making a small contribution among women. Deaths to non-lung cancers made a larger contribution to growing educational inequities in all race/sex groups.
Public Health Implications
The continued explosion and unequal distribution of overdose deaths adds urgency to the call for the opioid epidemic to be addressed. Reversing the growth of drug-related deaths will be especially beneficial in terms of life expectancy for working-age whites, and most emphatically so for white working-age men, with low education.
However, much like players of the classic “Whack-a-mole” arcade game, it is important we do not focus our attention on a single “mole” while the others go unattended. In a fundamental cause framework (Link and Phelan 1995), the successful suppression of a single mole only allows for another mole to rear its head. A broad examination of recent trends in life expectancy suggests that success in promoting health equity will be, at best, partial if we focus too narrowly on the opioid epidemic. Even among white men, addressing the opioid epidemic will not fully resolve the growing life expectancy inequities observed. Furthermore, opioid and other drug deaths played a lesser role in growing educational inequities in life expectancy among white women or blacks between 1990 and 2015. These are the groups that pose the biggest challenges for promoting health equity: Less-educated white women experienced the most consistent and alarming increases in YLL, while less educated blacks have the highest levels of YLL throughout the study period. While provisional evidence suggests growth in opioid deaths among blacks in 2016, they remain dramatically lower than among whites, and whether or to what extent they contribute to growing educational inequity in LE is unknown (Katz and Goodenough 2017). Finally, drug-related deaths explain little of the growing disparity in life expectancy at ages 65–84, where most of the overall growth in LE inequity occurred.
Thus, even as we tackle the opioid epidemic, we should not lose sight of the widening educational mortality gap attributed to CVD, cancers, and other internal causes. In this regard, we emphasize that the widely publicized “deaths of despair” narrative is speculative and imbued with untested motivational assumptions about individuals’ behaviors that may turn attention away from other reasonable explanations for the opioid epidemic, such as the role of the overselling and over-prescription of opioids, or the increasing use of fentanyl in street drugs. It overlooks black lives, for whom very little growth in life-expectancy inequity can be explained by opioid and other drug-related deaths.
Framing matters: the use and popularization of the DOD construct has important implications for agenda setting, guiding where research and intervention dollars are spent and on whom. Its popularization threatens to divert attention from other important entrenched drivers of health inequity, including cardiovascular disease, cancers and other internal causes. Without greater evidence, we recommend that researchers be cautious in their use of “deaths of despair” as a shortcut label to lend explanatory credibility to its underlying narrative of hopelessness. The DOD label implies that a lack of resilience explains LE inequities among whites even as a growing body of empirical evidence suggests that resilience is characteristic of many socioeconomically disenfranchised US populations facing structural oppression and that the process of persistent, high-effort coping itself can have adverse health repercussions.
Supplementary Material
Acknowledgements:
This work was supported by the Social Security Administration (SSA) Grant # RRC08098401–06-00 and by NIA Grant #s R01 AG059743 and T32 AG000221. The authors gratefully acknowledge use of the services and facilities of the Population Studies Center at the University of Michigan, funded by NICHD Center Grant # P2CHD041028. The findings and conclusions expressed are solely those of the authors and do not represent the views of the SSA, NIA, the University of Michigan, Claremont Graduate University, or the Urban Institute. The authors thank Abigail Norling-Ruggles for research assistance and three anonymous reviewers for comments on an earlier draft.
Footnotes
SUPPLEMENTAL MATERIAL
Additional supporting information may be found in the online version of this article.
The ICD9 codes for these deaths include 291, 303, 304, 965.00–965.09, E850-E858, E950.0-E950.5, E980.0-E980.5. ICD10 codes include F10-F19, X40-X44, X60-X64, X85, Y10-Y14.
Contributor Information
Arline T. Geronimus, School of Public Health, Research Professor, Institute for Social Research, University of Michigan, Member, National Academy of Medicine.
John Bound, George Johnson Collegiate Professor, Department of Economics, University of Michigan; &, Fellow, National Bureau of Economic Research.
Timothy A. Waidmann, Health Policy Center, Urban Institute.
Javier M. Rodriguez, Department of Politics and Government, Claremont Graduate University.
Mary Toepelt Nicolai, Department of Politics and Government, Claremont Graduate University.
George S. Blair, Department of Politics and Government, Claremont Graduate University.
Brenden Timpe, Doctoral Candidate, Department of Economics, University of Michigan.
REFERENCES
- Anderson Robert N., Miniño Arialdi M., Hoyert Donna L., and Rosenberg Harry M.. 2001. “Comparability of Cause of Death between ICD-9 and ICD-10: Preliminary Estimates.” National Vital Statistics Reports: From the Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System 49(2):1–32. [PubMed] [Google Scholar]
- Bennett Gary G., Merritt Marcellus M., Sollers John J. III, Edwards Christopher L., Whitfield Keith E., Brandon Dwayne T., and Tucker Reginald D.. 2004. “Stress, Coping, and Health Outcomes among African-Americans: A Review of the John Henryism Hypothesis.” Psychology & Health 19(3):369–83. [Google Scholar]
- Booth Jaime M. and Jonassaint Charles R.. 2016. “The Role of Disadvantaged Neighborhood Environments in the Association of John Henryism with Hypertension and Obesity.” Psychosomatic Medicine 78(5):552–61. [DOI] [PubMed] [Google Scholar]
- Bound John, Geronimus Arline T., Rodriguez Javier M., and Waidmann Timothy A.. 2015. “Measuring Recent Apparent Declines in Longevity: The Role Of Increasing Educational Attainment.” Health Affairs 34(12):2167–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown Dustin C., Lariscy Joseph T., and Kalousová Lucie. 2018. “Comparability of Mortality Estimates from Social Surveys and Vital Statistics Data in the United States.” Population Research and Policy Review 1–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Case Anne and Deaton Angus. 2015. “Rising Morbidity and Mortality in Midlife among White Non-Hispanic Americans in the 21st Century.” Proceedings of the National Academy of Sciences of the United States of America 112(49):15078–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Case Anne and Deaton Angus. 2017. Mortality and Morbidity in the 21st Century. Brookings Institution. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen Sheldon, Janicki-Deverts Denise, and Miller Gregory E.. 2007. “Psychological Stress and Disease.” JAMA 298(14):1685–87. [DOI] [PubMed] [Google Scholar]
- Cohen Sheldon, Janicki-Deverts Denise, Turner Ronald B., and Doyle William J.. 2015. “Does Hugging Provide Stress-Buffering Social Support? A Study of Susceptibility to Upper Respiratory Infection and Illness.” Psychological Science 26(2):135–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epel Elissa S. and Lithgow Gordon J.. 2014. “Stress Biology and Aging Mechanisms: Toward Understanding the Deep Connection between Adaptation to Stress and Longevity.” The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences 69 Suppl 1:S10–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geronimus Arline T. 1992. “The Weathering Hypothesis and the Health of African-American Women and Infants: Evidence and Speculations.” Ethnicity and Disease 2(3):207–21. [PubMed] [Google Scholar]
- Geronimus Arline T., Bound John, and Colen Cynthia G.. 2011. “Excess Black Mortality in the United States and in Selected Black and White High-Poverty Areas, 1980–2000.” American Journal of Public Health 101(4):720–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geronimus Arline T., Bound John, Waidmann Timothy A., Colen Cynthia G., and Steffick Diane. 2001. “Inequality in Life Expectancy, Functional Status, and Active Life Expectancy across Selected Black and White Populations in the United States.” Demography 38(2):227–51. [DOI] [PubMed] [Google Scholar]
- Geronimus Arline T., Hicken Margaret, Keene Danya, and Bound John. 2006. “‘Weathering’ and Age Patterns of Allostatic Load Scores among Blacks and Whites in the United States.” American Journal of Public Health 96(5):826–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geronimus Arline T., Pearson Jay A., Linnenbringer Erin, Schulz Amy J., Reyes Angela G., Epel Elissa S., Lin Jue, and Blackburn Elizabeth H.. 2015. “Race-Ethnicity, Poverty, Urban Stressors, and Telomere Length in a Detroit Community-Based Sample.” Journal of Health and Social Behavior 56(2):199–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Godbout Jonathan P. and Glaser Ronald. n.d. “Stress-Induced Immune Dysregulation: Implications for Wound Healing, Infectious Disease and Cancer. - PubMed - NCBI.” Retrieved April 12, 2019 (https://www.ncbi.nlm.nih.gov/pubmed/18040814). [DOI] [PubMed]
- Gross Tal, Glied Sherry, and Muennig Peter. 2015. “Widening Mortality Disparities by Educational Attainment among Native-Born Americans Adults over 3 Decades of Follow up: The Mystery Deepens.” International Journal of Healthcare 1(1). [Google Scholar]
- Gruenewald Tara L., Cohen Sheldon, Matthews Karen A., Tracy Russell, and Seeman Teresa E.. 2009. “Association of Socioeconomic Status with Inflammation Markers in Black and White Men and Women in the Coronary Artery Risk Development in Young Adults (CARDIA) Study.” Social Science & Medicine (1982) 69(3):451–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guy Gery P., Zhang Kun, Bohm Michele K., Losby Jan, Lewis Brian, Young Randall, Murphy Louise B., and Dowell Deborah. 2017. “Vital Signs: Changes in Opioid Prescribing in the United States, 2006–2015.” MMWR. Morbidity and Mortality Weekly Report 66(26):697–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendi Arun S. 2015. “Trends in U.S. Life Expectancy Gradients: The Role of Changing Educational Composition.” International Journal of Epidemiology 44(3):946–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho Jessica Y. 2017. “The Contribution of Drug Overdose to Educational Gradients in Life Expectancy in the United States, 1992–2011.” Demography 54(3):1175–1202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho Jessica Y. and Fenelon Andrew. 2015. “The Contribution of Smoking to Educational Gradients in U.S. Life Expectancy.” Journal of Health and Social Behavior 56(3):307–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- James, Sherman A, Strogatz David S., Wing Steven B., and Ramsey Diane L.. 1987. “Socioeconomic Status, John Henryism, and Hypertension in Blacks and Whites.” American Journal of Epidemiology 126(4):664–73. [DOI] [PubMed] [Google Scholar]
- James Sherman A. 1994. “John Henryism and the Health of African-Americans.” Culture, Medicine and Psychiatry 18(2):163–82. [DOI] [PubMed] [Google Scholar]
- James Sherman A., Angela Fowler-Brown Trevillore E. Raghunathan, and Van Hoewyk John. 2006. “Life-Course Socioeconomic Position and Obesity in African American Women: The Pitt County Study.” American Journal of Public Health 96(3):554–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janicki-Deverts Denise, Cohen Sheldon, Matthews Karen A., and Cullen Mark R.. 2008. “History of Unemployment Predicts Future Elevations in C-Reactive Protein among Male Participants in the Coronary Artery Risk Development in Young Adults (CARDIA) Study.” Annals of Behavioral Medicine: A Publication of the Society of Behavioral Medicine 36(2):176–85. [DOI] [PubMed] [Google Scholar]
- Katz Josh. 2017a. “The First Count of Fentanyl Deaths in 2016: Up 540% in Three Years.” The New York Times, September 2. [Google Scholar]
- Katz Josh. 2017b. “The Opioid Crisis Is Getting Worse, Particularly for Black Americans.” The New York Times, December 22. [Google Scholar]
- Katz Josh and Goodenough Abby. 2017. “The Opioid Crisis Is Getting Worse, Particularly for Black Americans.” The New York Times, December 22. [Google Scholar]
- Khansari Nemat, Shakiba Yadollah, and Mahmoudi Mahdi. 2009. “Chronic Inflammation and Oxidative Stress as a Major Cause of Age-Related Diseases and Cancer.” Recent Patents on Inflammation & Allergy Drug Discovery 3(1):73–80. [DOI] [PubMed] [Google Scholar]
- Link Bruce G. and Phelan Jo. 1995. “Social Conditions As Fundamental Causes of Disease.” Journal of Health and Social Behavior 35:80–94. [PubMed] [Google Scholar]
- Linnenbringer Erin, Gehlert Sarah, and Geronimus Arline T.. 2017. “Black-White Disparities in Breast Cancer Subtype: The Intersection of Socially Patterned Stress and Genetic Expression.” AIMS Public Health 4(5):526–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manton Kenneth G. and Stallard Eric. 1984. Recent Trends in Mortality Analysis. Academic Press. [Google Scholar]
- Masters Ryan K., Tilstra Andrea M., and Simon Daniel H.. 2018. “Explaining Recent Mortality Trends among Younger and Middle-Aged White Americans.” International Journal of Epidemiology 47(1):81–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McEwen Bruce S. and Stellar Eliot. 1993. “Stress and the Individual. Mechanisms Leading to Disease.” Archives of Internal Medicine 153(18):2093–2101. [PubMed] [Google Scholar]
- McEwen Bruce S. 1998. “Protective and Damaging Effects of Stress Mediators” edited by Flier JS and Underhill LH. New England Journal of Medicine 338(3):171–79. [DOI] [PubMed] [Google Scholar]
- McEwen Bruce S. and Gianaros Peter J.. 2010. “Central Role of the Brain in Stress and Adaptation: Links to Socioeconomic Status, Health, and Disease: Central Links between Stress and SES.” Annals of the New York Academy of Sciences 1186(1):190–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meara Ellen R., Richards Seth, and Cutler David M.. 2008. “The Gap Gets Bigger: Changes In Mortality And Life Expectancy, By Education, 1981–2000.” Health Affairs 27(2):350–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller Gregory E., Yu Tianyi, Chen Edith, and Brody Gene H.. 2015. “Self-Control Forecasts Better Psychosocial Outcomes but Faster Epigenetic Aging in Low-SES Youth.” Proceedings of the National Academy of Sciences of the United States of America 112(33):10325–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monnat Shannon M. 2016. Deaths of Despair and Support for Trump in the 2016 Presidential Election. The Pennsylvania State University Department of Agricultural Economics, Sociology, and Education. [Google Scholar]
- Montez Jennifer Karas, Hummer Robert A., Hayward Mark D., Woo Hyeyoung, and Rogers Richard G.. 2011. “Trends in the Educational Gradient of U.S. Adult Mortality from 1986 to 2006 by Race, Gender, and Age Group.” Research on Aging 33(2):145–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montez Jennifer Karas and Zajacova Anna. 2013a. “Explaining the Widening Education Gap in Mortality among U.S. White Women.” Journal of Health and Social Behavior 54(2):166–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montez Jennifer Karas and Zajacova Anna. 2013b. “Trends in Mortality Risk by Education Level and Cause of Death Among US White Women From 1986 to 2006.” American Journal of Public Health 103(3):473–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moody Danielle L. Beatty, Chang Yue-Fang, Pantesco Elizabeth J., Darden Taylor M., Lewis Tené T., Brown Charlotte, Bromberger Joyce T., and Matthews Karen A.. 2018. “Everyday Discrimination Prospectively Predicts Blood Pressure Across 10 Years in Racially/Ethnically Diverse Midlife Women: Study of Women’s Health Across the Nation.” Annals of Behavioral Medicine. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muennig Peter A., Reynolds Megan, Fink David S., Zafari Zafar, and Geronimus Arline T.. 2018. “America’s Declining Well-Being, Health, and Life Expectancy: Not Just a White Problem.” American Journal of Public Health e1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olshansky S. Jay, Antonucci Toni, Berkman Lisa, Binstock Robert H., Boersch-Supan Axel, Cacioppo John T., Carnes Bruce A., Carstensen Laura L., Fried Linda P., and Goldman Dana P.. 2012. “Differences in Life Expectancy Due to Race and Educational Differences Are Widening, and Many May Not Catch Up.” Health Affairs 31(8):1803–13. [DOI] [PubMed] [Google Scholar]
- Parente Victoria, Hale Lauren, and Palermo Tia. 2013. “Association between Breast Cancer and Allostatic Load by Race: National Health and Nutrition Examination Survey 1999–2008: Biomarkers of Breast Cancer.” Psycho-Oncology 22(3):621–28. [DOI] [PubMed] [Google Scholar]
- Phillips Julie A. and Hempstead Katherine. 2017. “Differences in U.S. Suicide Rates by Educational Attainment, 2000–2014.” American Journal of Preventive Medicine 0(0). [DOI] [PubMed] [Google Scholar]
- Preston Samuel H. and Elo Irma T.. 1995. “Are Educational Differentials in Adult Mortality Increasing in the United States?” Journal of Aging and Health 7(4):476–96. [DOI] [PubMed] [Google Scholar]
- Preston Samuel H. and Elo Irma T.. 1999. “Effects of Age Misreporting on Mortality Estimates at Older Ages.” Population Studies 53(2):165–77. [Google Scholar]
- Quinones Sam. 2016. Dreamland: The True Tale of America’s Opiate Epidemic. Paperback edition. New York: Bloomsbury Press. [Google Scholar]
- Rockett Ian R. H., Samora Julie B., and Coben Jeffrey H.. 2006. “The Black-White Suicide Paradox: Possible Effects of Misclassification.” Social Science & Medicine (1982) 63(8):2165–75. [DOI] [PubMed] [Google Scholar]
- Rodriguez Javier M., Karlamangla Arun S., Gruenewald Tara L., Dana Miller-Martinez Sharon S. Merkin, and Seeman Teresa E.. 2019. “Social Stratification and Allostatic Load: Shapes of Health Differences in the MIDUS Study in the United States.” Journal of Biosocial Science 1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin Rita. 2017. “Illicit Fentanyl Driving Opioid Overdose Deaths.” JAMA 318(22):2174. [DOI] [PubMed] [Google Scholar]
- Ruhm Christopher J. 2017a. “Drug Involvement in Fatal Overdoses.” SSM - Population Health 3:219–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruhm Christopher J. 2017b. “Geographic Variation in Opioid and Heroin Involved Drug Poisoning Mortality Rates.” American Journal of Preventive Medicine 53(6):745–53. [DOI] [PubMed] [Google Scholar]
- Ruhm Christopher J. 2018. Deaths of Despair or Drug Problems? Working Paper. 24188 National Bureau of Economic Research. [Google Scholar]
- Sapolsky Robert M., Romero L. Michael, and Munck Allan U.. 2000. “How Do Glucocorticoids Influence Stress Responses? Integrating Permissive, Suppressive, Stimulatory, and Preparative Actions.” Endocrine Reviews 21(1):55–89. [DOI] [PubMed] [Google Scholar]
- Sasson Isaac. 2016. “Diverging Trends in Cause-Specific Mortality and Life Years Lost by Educational Attainment: Evidence from United States Vital Statistics Data, 1990–2010” edited by Patra J. PLOS ONE 11(10):e0163412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sasson Isaac. 2017. “Reply to Trends in Education-Specific Life Expectancy, Data Quality, and Shifting Education Distributions: A Note on Recent Research.” Demography 54(3):1215–19. [DOI] [PubMed] [Google Scholar]
- Seeman Teresa, Epel Elissa, Gruenewald Tara, Karlamangla Arun, and McEwen Bruce S.. 2010. “Socio-Economic Differentials in Peripheral Biology: Cumulative Allostatic Load.” Annals of the New York Academy of Sciences 1186:223–39. [DOI] [PubMed] [Google Scholar]
- Seeman Teresa, Thomas Duncan, Stein Merkin Sharon, Moore Kari, Watson Karol, and Karlamangla Arun. 2018. “The Great Recession Worsened Blood Pressure and Blood Glucose Levels in American Adults.” Proceedings of the National Academy of Sciences 115(13):3296–3301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steptoe Andrew and Mika Kivimäki. 2013. “Stress and Cardiovascular Disease: An Update on Current Knowledge.” Annual Review of Public Health 34(1):337–54. [DOI] [PubMed] [Google Scholar]
- Thoits Peggy A. 2010. “Stress and Health: Major Findings and Policy Implications.” Journal of Health and Social Behavior 51(1_suppl):S41–53. [DOI] [PubMed] [Google Scholar]
- Tinetti Mary E., McAvay Gail J., Murphy Terrence E., Gross Cary P., Lin Haiqun, and Allore. Heather G. 2012. “Contribution of Individual Diseases to Death in Older Adults with Multiple Diseases.” Journal of the American Geriatrics Society 60(8):1448–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Traustadóttir Tinna, Bosch Pamela R., and Matt Kathleen S.. 2005. “The HPA Axis Response to Stress in Women: Effects of Aging and Fitness.” Psychoneuroendocrinology 30(4):392–402. [DOI] [PubMed] [Google Scholar]
- Van Zee Art. 2009. “The Promotion and Marketing of OxyContin: Commercial Triumph, Public Health Tragedy.” American Journal of Public Health 99(2):221–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


