Short abstract
Background
Adolescent and young adult (AYA) cancer survivors are under-represented in research. Social media is increasingly used for recruitment given its ability to reach large audiences. Differences in participant characteristics and potential biases due to recruitment source are not well understood.
Purpose
This study aimed to: (a) compare recruitment strategies (hospital-based v. social media) in enrollment metrics, and (b) among enrolled participants, evaluate group differences in patient characteristics and patient reported outcomes (PROs).
Methods
Preliminary data from a cancer and fertility study with female AYAs were evaluated. Hospital-based recruitment used electronic medical records (EMR) to identify eligible patients. Social media recruitment involved posting on partner organizations’ social media outlets. PROs included validated measures related to the parent study. Descriptive statistics evaluated recruitment metrics. Independent samples t-tests and chi-square identified differences in participant characteristics and PROs based on recruitment.
Results
Social media yielded a higher enrollment rate (37%; n = 54/146) compared with hospital-based recruitment (7%; n = 21/289) and required fewer study resources. Compared with hospital-based recruitment, participants from social media were more likely to be White (p = 0.01), with a longer time since treatment (p = 0.03); and reported higher levels of reproductive concern (p = 0.004) and negative mood (p = 0.02), and more negative illness perceptions (ps < 0.05).
Conclusion
Recruitment via social media may be a more effective and efficient strategy compared with hospital-based methods. However, group differences were identified that could bias findings and limit generalizability. Advantages of social media should be considered with an understanding of how methodology may impact enrollment and results.
Keywords: Social media, social media recruitment, digital health, young adult, cancer, research methodology, patient organizations
Adolescent and young adult (AYA) cancer survivors are a ‘hard-to-reach’ group and are under-represented in research, which is due in part to recruitment challenges.1,2 Traditional recruitment methods include hospital- or clinic-based strategies during points of contact, provider referral and patient identification through the electronic medical records (EMR) to identify and contact patients already connected to a medical system. The use of Internet-based strategies, particularly within social media (e.g. Facebook), has become an increasingly common recruitment method given the advantages of reaching larger, potentially more diverse populations;3,7 with evidence suggesting it may be more efficient and effective than offline, hospital-based and in-person methods.8 Understanding the ways in which offline v. online recruitment may impact participant characteristics and study outcomes is critical to inform appropriate methodology and begin to identify potential biases that may result from varying recruitment strategies.
Several direct comparisons of offline and online recruitment methods have been conducted. Based on a sample of 8252 participants, Christensen et al.8 found that online recruitment (i.e. social media ads) was more efficient (total number of participants enrolled) and had an averaged lower cost per recruited participant, compared with offline methods (i.e. press releases, posters and flyers). Indeed, consensus around the advantages of online, social media recruitment appears to be well-established for its far-reach and low cost.9,10 In young adult cancer, Gorman et al.3 examined recruitment across four studies, in which online efforts using social media and Internet-based outreach were more successful than offline strategies when the study did not require local participation (e.g. in-person activities), citing that partnership with young adult cancer advocacy groups facilitated online recruitment and peer-to-peer dissemination of study information. Aside from enrollment metrics and cost calculations, however, limited research has evaluated whether different recruitment approaches lead to varying participant characteristics. Offline v. online recruitment may lead to over- or under-representation of the target population in different ways. For instance, social media may better capture geographic diversity, but lean towards a more highly distressed subgroup with online activity that connects to patient groups or online activity that identifies them as targets for recruitment ads. It is critical to evaluate recruitment-based differences to inform generalizability.
This study aimed to: (a) compare recruitment approaches (hospital-based v. social media) in enrollment metrics, and (b) among enrolled participants, evaluate differences in sociodemographic and medical characteristics and patient reported outcomes (PROs) by recruitment approach.
Methods
All study procedures were approved by the Northwell Health Institutional Review Board. This study was part of a larger study of AYA female cancer survivors’ fertility experiences and post-treatment decision-making and support needs related to family-building after cancer. This was a mixed methods study in which participants completed a one-time survey and a subgroup completed an additional one-time semi-structured interview (45–60 minutes). Participation in study activities was done remotely.
Participants
Eligibility criteria included: female gender, aged 15–45 years old, completed cancer treatment and a reported desire for future children or uncertainty about reproductive plans. The National Cancer Institute (NCI) defines AYA cancer as those diagnosed in individuals between the ages of 15–39 years old. Consistent with other studies of cancer and fertility,11 we expanded the age range to include survivors up to 45 years old, as parenthood desires may persist at older ages and family-building concerns are still relevant.
Recruitment strategies
Strategies to recruit participants used more traditional, hospital-based methods, as well as social media through partnership with patient organizations. These strategies were used cyclically over an 18-month period such that hospital-based recruitment was initiated first and was only followed by social media efforts once recruitment reached a lull, that is study staff focused on one recruitment strategy at a time. After the first round of social media posts, study staff re-focused on hospital-based recruitment. No more than two attempts were made to contact individuals if no response was obtained (i.e. ≤ two voicemails).
Hospital-based recruitment
Patients meeting initial eligibility criteria were identified using EMR data from the Northwell Health system. Study staff reviewed each chart to confirm eligibility. Oncology providers were contacted to give approval to contact their patients. Letters were mailed home describing the study and inviting participation. Follow-up phone calls were made one week later, with continued follow-up calls if needed, to have a discussion to confirm eligibility, obtain informed consent (phone or web-based consent) and complete study enrollment.
Social media recruitment
Four organizations (Stupid Cancer, The Samfund, Alliance for Fertility Preservation and Lacuna Loft) posted an Institutional Review Board (IRB)-approved message (see Supplemental Table 1) on Facebook and Instagram a total of six times (i.e. each organization posted once or twice). These organizations were chosen based on pre-existing relationships the authors had with the organizations (i.e. supporting organizational activities in volunteer and advisory roles, unpaid). The post provided a brief description of the study and link to provide contact information using a HIPPA-compliant platform. Those who provided information were contacted via email or phone, based on their preferred method for contact, to have a follow-up discussion about the study and to complete enrollment for those interested and eligible. There was no overlap between hospital-based recruitment and social media responses, such that those who responded to social media posts had not also received a recruitment letter.
Measures
Recruitment metrics across hospital-based and social media strategies were collected, including number of AYA cancer survivors approached, screened and enrolled. The number approached via social media was calculated based on the number that expressed interest by supplying their contact information, as we were unable to calculate the number of impressions or conversion to complete the contact information form. The yield of each strategy was calculated separately for the two groups by dividing the number of participants enrolled by the number of people approached.
A baseline survey collected sociodemographic and medical characteristics using a standard questionnaire and included measures of PROs aligned with the study objectives, including cognitive, emotional and financial factors related to infertility, coping and family-building decision-making after cancer. Investigator-designed questions assessed unmet fertility information needs (5 items, α = 0.82).12 Validated measures assessed mood (Profile of Mood States (POMS) subscales: Positive Mood, α = 0.83, and Negative Mood, α = 0.95),13 fertility-specific distress (Reproductive Concern After Cancer Scale (RCACS), α = 0.81),14 illness perceptions related to infertility/infertility risk (Illness Perceptions Questionnaire – Revised (IPQ-R), α = 0.70–0.90),15 coping (Impact of Events Scale – Revised (IES-R) Avoidance subscale, α = 0.85),16 cancer-related financial toxicity (Comprehensive Score for Financial Toxicity (COST), α = 0.72)17 and decision-making about family-building after cancer (Decisional Conflict Scale (DCS), α = 0.95; Decision Self-Efficacy (DSE) scale, α = 0.96).18,19
Analysis
Descriptive statistics compared recruitment metrics between hospital-based and social media groups. Comparisons were made with population-level statistics regarding sociodemographic characteristics. Group differences were evaluated for the number of individuals approached, screened and enrolled. Quantitative metrics were not tracked to examine differences in cost-effectiveness; however, observations regarding differences in study staff time and effort across recruitment methods are reported. To identify potential biases associated with recruitment source, independent samples t-tests and chi-square tests assessed differences in sociodemographic and medical characteristics and PROs by recruitment group. Group differences found to be significant (p < 0.05) or trending toward significance (p < 0.10) are reported.
Results
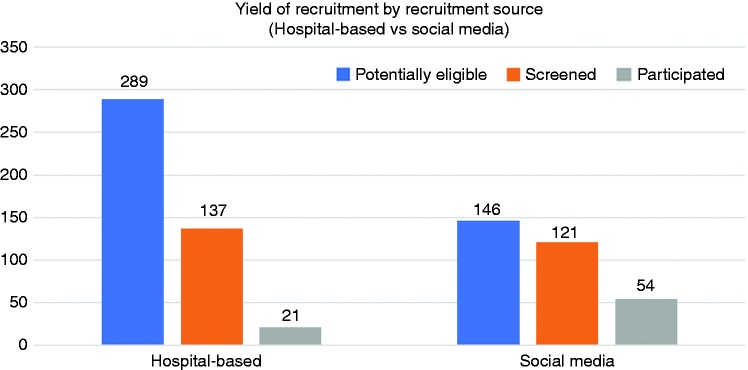
To achieve the first aim, we compared hospital-based v. social media recruitment strategies on enrollment metrics. Enrollment (n = 75) was greater for social media (n =54/75; 72%) than hospital-based (n = 21/75; 28%) recruitment (see Figure 1). Hospital-based recruitment included an EMR data abstraction, which identified 866 potentially eligible patients. After chart review to confirm eligibility, letters were sent home to 289 patients, 515 follow-up phone calls were made, 137 phone screens were completed and 21 participants were enrolled, resulting in an enrollment rate of a 7.3% (21 enrolled/289 patients identified as eligible using EMR data). Through social media, 146 forms were completed online, providing contact information and an initial assessment of eligibility. Follow-up efforts included 157 phone calls, 121 phone screens and 54 participants enrolled; equaling an enrollment rate of 37% (54 enrolled/146).
Figure 1.
Social media recruitment yielded the highest recruitment rate (37%; 54 enrolled/146 individuals who clicked the recruitment link and self-described as eligible by completing a contact and screener form), compared to hospital-based recruitment (7.3%; 21 enrolled/289 patients identified as eligible using electronic medical record data).
For the second aim, we evaluated differences in enrolled participants (n = 75) based on recruitment source. Overall, participants were primarily White (73%), employed (87%), mean (M) 31 years of age (standard deviation (SD) = 8.1), and 5.1 years post-treatment (SD = 4.5), and most common cancers were breast (27%) and leukemia (21%; see Table 1). Participants skewed toward older ages of the AYA age range with 49% in their 30s (n = 37); only 8% (n = 6) were in ‘adolescence/early young adulthood’ (15–25 years old). For comparison, the largest study of AYA cancer patients (the AYA HOPE study; n = 524) reported a racial/ethnic breakdown consisting of 63% non-Hispanic White, 19% Hispanic, 8% non-Hispanic Black and 10% Asian; and 44% were aged 30–39 years old.20
Table 1.
Sociodemographic and medical characteristics by recruitment source.
| Total n = 75 Mean (SD) or n (%) | Hospital-based n = 21 Mean (SD) or n (%) | Social media n = 54 Mean (SD) or n (%) | t-test or Chi square | p-value | |
|---|---|---|---|---|---|
| Age (years) | 31.18 (8.09) | 32.76 (9.10) | 30.57 (7.67) | 1.05 | 0.30 |
| Race | 10.44 | 0.005 | |||
| White, non-Hispanic | 48 (64%) | 7 (33%) | 41 (80%) | ||
| Black | 6 (8%) | 4 (19%) | 2 (4%) | ||
| Other | 14 (19%) | 7 (33%) | 7 (13%) | ||
| Hispanic | 16 (21%) | 7 (35%) | 9 (17%) | 2.90 | 0.09 |
| Education | 4.66 | 0.09 | |||
| High school/vocational | 13 (17%) | 6 (29%) | 7 (13%) | ||
| College | 35 (47%) | 11 (52%) | 24 (44%) | ||
| Graduate degree | 27 (36%) | 4 (19%) | 23 (43%) | ||
| Employed, full- or part-time | 65 (87%) | 17 (81%) | 48 (89%) | 0.82 | 0.45 |
| Income (household total)a | 3.98 | 0.14 | |||
| < US$50,000 | 24 (32%) | 9 (56%) | 15 (33%) | ||
| US$50,000–US$100,000 | 25 (33%) | 6 (38%) | 19 (41%) | ||
| > US$100,000 | 13 (17%) | 1 (6%) | 12 (26%) | ||
| Localityb | 13.44 | 0.004 | |||
| Urban | 24 (32%) | 10 (48%) | 14 (26%) | ||
| Suburban | 45 (60%) | 8 (38%) | 37 (68%) | ||
| Rural | 3 (4%) | 0 (0%) | 3 (6%) | ||
| Time since treatment (years) | 5.14 (4.46) | 3.71 (2.44) | 5.71 (4.93) | –1.72 | 0.03 |
| Cancer typec | 2.72 | 0.44 | |||
| Breast | 20 (26.7) | 8 (38.1) | 12 (22.2) | ||
| Leukemia | 16 (21.3) | 5 (23.8) | 11 (20.4) | ||
| Hodgkin Lymphoma | 12 (16) | 2 (9.5) | 10 (18.5) | ||
| Non-Hodgkin Lymphoma | 7 (9.3) | 2 (9.5) | 5 (9.3) | ||
| Ovarian | 4 (5.3) | -- | 4 (7.4) | ||
| Cervical | 3 (4.0 | 2 (9.5) | 1 (1.9) | ||
| Colon | 3 (4.0 | 1 (4.8) | 2 (3.7) | ||
| Sarcoma | 2 (2.7) | -- | 2 (3.7) | ||
| Rectal | 1 (1.3) | -- | 1 (1.9) | ||
| Uterine/Endometrial | 1 (1.3) | -- | 1 (1.9) | ||
| Other | 6 (8) | 1 (4.8) | 5 (9.3) |
aMissing data
bPrefer not to answer, n = 3
cChi-square test of group differences included the top four most common cancers.
Regarding sociodemographic and medial characteristics, participants from social media were more likely to be White (p = 0.01), with a longer time since treatment (p = 0.03), and trended toward more highly educated (p = 0.10); whereas hospital-based recruitment led to more minorities, more recent treatment and lower education. Participants through hospital-based recruitment were mostly from urban settings (48%), given the location of our institution, compared with social media participants primarily being from suburban settings (68%). Only three participants self-described as being from rural areas, but all were recruited through social media. Social media also led to more diverse cancer diagnoses, such that participants with ovarian, rectal, sarcoma and uterine/endometrial cancers were only represented in the social media group and not in the hospital-based group. No group differences in age or employment were identified (p range > 0.10).
With respect to baseline PROs, participants from social media, compared with hospital-based recruitment, reported higher levels of reproductive concern (t(71) = –2.94, p = 0.004) and negative mood (t(72) = –2.406, p = 0.02), more negative illness perceptions related to infertility risk/fertility problems (e.g. consequences, control, emotions; ps < 0.05) and trended toward greater unmet fertility information needs and lower positive mood (ps < 0.10). No group differences in decisional conflict or self-efficacy, coping, or cancer-related financial toxicity were identified (ps > 0.10) (Table 2).
Table 2.
Patient-reported outcomes by recruitment source.
| Total n = 75 M (SD) | Hospital-based n = 21 M (SD) | Social media n = 54 M (SD) | t-test or chi square | p-value | |
|---|---|---|---|---|---|
| Patient Reported Outcomesa,b | |||||
| Unmet information needs | 3.49 (1.78) | 2.75 (.46) | 3.78 (1.60) | –2.25 | 0.03 |
| Cognitive-emotional functioning | |||||
| Fertility distress (RCACS) | 61.21 (11.17) | 55.25 (8.25) | 63.45 (11.36) | –2.94 | 0.004 |
| Positive mood (POMS) | 2.93 (0.69) | 3.16 (0.59) | 2.84 (0.79) | 1.70 | 0.09 |
| Negative mood (POMS) | 2.72 (0.92) | 2.33 (0.84) | 2.88 (0.91) | –2.49 | 0.02 |
| Illness perceptions (IPQ-R) | |||||
| Consequences | 3.44 (0.81) | 2.98 (0.71) | 3.61 (0.79) | –3.19 | 0.002 |
| Personal control | 2.59 (0.76) | 3.01 (0.75) | 2.42 (0.70) | 3.19 | 0.002 |
| Treatment control | 2.75 (0.90) | 3.03 (0.59) | 2.63 (0.98) | 1.75 | 0.09 |
| Illness coherence | 2.98 (1.26) | 2.80 (1.28) | 3.04 (1.26) | –7.02 | 0.49 |
| Emotional representation | 3.66 (1.01) | 2.98 (0.96) | 3.94 (0.90) | –4.04 | < 0.001 |
| Coping | |||||
| Avoidance (IES-R) | 1.66 (0.92) | 1.78 (1.09) | 1.62 (0.85) | 0.68 | 0.50 |
| Financial toxicity (COST)c | 2.95 (0.69) | 3.01 (0.79) | 3.07 (0.85) | –0.26 | 0.79 |
| Decision-making processes | |||||
| Decisional conflict (DCS) | 46.96 (23.96) | 50.82 (25.74) | 45.42 (23.30) | 0.87 | 0.39 |
| Decision self-efficacy (DSE) | 67.94 (24.25) | 68.96 (29.69) | 67.53 (22.05) | 0.23 | 0.82 |
aSignificant group differences by recruitment source are bolded.
bHigher scores represent greater unmet information needs, more positive and negative mood (POMS), and greater fertility-specific distress (RCACS). With respect to the IPQ-R, higher scores represent more strongly held beliefs about the negative consequences of illness (Consequences subscale), more positive beliefs about controllability (Personal and Treatment Control) and a personal understanding of the health threat (Coherence), and more negative emotions related to health threat (Emotional Representation). Higher scores also represent greater use of avoidant strategies to cope (IES-R), greater cancer-related financial toxicity (COST), and decision making uncertainty (DCS) and confidence (DSE).
cOne item was removed based on reliability diagnostics; mean score calculated from remaining nine items.
Main outcome variables for the parent study were reproductive concern and decisional conflict about future family building. The social media group reported levels of reproductive concern that was slightly higher than levels reported in the literature (e.g. RCAC summary score, M = 58.3, SD = 10.9),21 whereas the hospital-based group reported lower levels. For every 5-unit increase in RCAC scores, there is 1.3 higher odds of experiencing moderate to severe depression,21 suggesting that the mean difference between social media and hospital-based groups of 5.96 may be clinically significant. Recruitment groups reported comparable levels of decisional conflict (DCS M = 49.96, SD = 23.96), which indicated clinically significant decision distress in both groups (DCS clinical cut-off score, M = 37.5); these scores have been associated with decision delay and feeling unsure about implementation.18
Discussion
Given the increasing use of social media for recruitment in health outcomes research, we sought to compare offline v. online strategies and evaluate whether recruitment source led to any bias in our participant sample. In this study, social media had a higher enrollment rate, compared with hospital-based recruitment, and required less time and effort per enrolled participant on the part of study support staff (e.g. follow-up phone calls). However, group differences were identified with social media yielding a less demographically diverse and generally more distressed sample than hospital-based recruitment.
Consistent with our findings, two reviews found that social media tended to lead to an over-representation of younger, White participants with higher education and income, and only 17% of studies found that social media and traditional recruitment methods led to comparable samples (2 of 12 studies).9,10 Keaver et al. compared a sample recruited via Twitter with a nationally representative sample of 1550 cancer survivors in NHANES (National Health and Nutrition Examination Survey) and similarly found that respondents to social media posts were younger and more likely to be female, non-Hispanic White, to have a higher education and to be within five years of their initial diagnosis.23 This may be due to the makeup of users on social media platforms, user activity or platform algorithms that determine exposure to study-relevant posts, effectiveness (or lack thereof) of targeted marketing to reach different groups, or differences in response rates across groups. Conversely, registry-based sampling and recruitment through cancer centers and clinics have been shown to be biased toward patients with private health insurance or Medicare and those who are in active or recent treatment and engaged with clinical care teams, with differences in ‘opt-out’ rates across demographic subgroups reported.24 Indeed, the lack of diversity in clinical research is not new and the under inclusion of racial/ethnic minority groups is a well-known problem for studies using more traditional recruitment methods as well.25 One limitation of our study was that we were unable to obtain an accurate estimate of the number of social media impressions or the characteristics of individuals who were exposed to social media posts. More in-depth exploration of how different groups perceive and engage with research ad postings may inform recruitment strategies to better engage diverse audiences.
The Internet and social media are powerful tools that offer significant opportunity to increase inclusion among under-represented groups. Findings suggest the need for researchers to make concerted efforts to access patient subgroups and employ methodology that leads to representative samples of the target population. Arigo et al.6 highlight the importance of understanding how the target population uses different social media platforms to best tailor recruitment campaigns, such as through the selection of keywords or hashtags that reflect the likes and interests of user subgroups. Monitoring recruitment campaigns via platform analytics may provide insight into factors that lead to successful enrollment (e.g. variation of ad postings across times of day, days of the week, or different keywords or photos used). We defined our target population as ‘adolescent and young adult cancer survivors’, however, more targeted approaches to understand and recruit participant subgroups may be necessary. Setting ads to target different zip codes and turning ads on and off based on accrual statistics has been shown to be an effective strategy to increase racial/ethnic minority recruitment and achieve equal representation across demographic groups.6 Other strategies may be to vary ad messaging and pictures or images to appeal to population subgroups.
Aside from sample demographic characteristics, even less research has examined how recruitment source may lead to biases with respect to psychological or behavioral outcomes. Similar to our findings, in a cohort study of cancer patients, participants recruited using Internet-based strategies reported higher levels of distress and lower quality of life than those recruited through a cancer registry.26 In our study, differences may reflect participants’ connection to the cancer organizations we partnered with, which largely determined their exposure to the recruitment ads posted. A self-selection bias based on participants’ online engagement with cancer organizations may have indicated greater difficulty or distress associated with their disease (and study PROs), compared to the hospital-based sample with no known connection to organizations.27 Had we partnered with organizations or digital community leaders (‘influencers’) with no connection to cancer, but large user followings matching this age group, results may have differed. Posting a recruitment ad through non-cancer channels may not apply to the majority of its viewers, but those that are enrolled may be more representative of the underlying population. For this line of research, identifying non-cancer digital touchpoints may be one way to expand recruitment strategies in the future. It may also be useful to better match digital platforms that are popular among age-based subgroups (e.g. Twitter or Snapchat).
Likewise, recruitment differences may have also been due to an interaction between recruitment source and enrollment. Although both recruitment strategies involved only remote interaction, it may be that individuals with lower distress and better quality of life were more likely to agree to participate when proactive attempts by study staff were made to contact them (i.e. phone calls); whereas social media posts required individuals to be proactive to provide contact information. PROs data was not available for those that did not enroll, and we were unable to compare the two populations that we recruited from.
Researchers should be thoughtful about which recruitment methods best match the objectives of the study and sampling needs with consideration to generalizability, particularly as findings suggested that clinically meaningful differences may result. Using a combination of multiple recruitment strategies is advocated, given the advantages and disadvantages of each. Clearly, researchers must balance the pressures of needing to successfully recruit the target sample size within budgetary, resource and time constraints, while addressing potential biases that are introduced with any one method. Initial approaches may use online methods as a feasible, low-cost strategy to start, with ongoing evaluation of the make-up and representation of the recruited sample. Strategies may be modified as the study progresses to target underrepresented subgroups as needed.
On the other hand, although online methods seem to offer a number of advantages, a recent review indicated that only 40% of studies using social media recruitment found it to be the best method and less than half found it to be cost-effective.10 In a comparison of time-efficiency and cost-effectiveness of six different recruitment strategies for eHealth clinical trials, Lattie et al.28 reported that digital recruitment yielded the highest number of participants, but registry-based recruitment yielded the highest conversion rate and was most cost-effective. In this study, we did not incur costs for social media posts and, given the higher enrollment rate and less time needed by study staff (e.g. fewer phone calls), social media was a more efficient strategy. However, we did not measure or track cost saving metrics. Our study may also differ from others as partnerships with patient organizations were an extension of longstanding collaborative work together. For other studies without pre-existing relationships with organizations, social media recruitment may be more costly, less efficient, and/or require greater time and resources for relationship building.
Our findings suggest researchers may need to be wary of overestimating cancer-related difficulties and psychosocial distress if recruiting solely from patient organizations or participants whose online behavior mark them for targeted recruitment messages. It has been shown that different social media recruitment strategies can influence the demographics and accrual of participants,6,10 indicating the need for ongoing evaluation, comparison to the literature when possible and efforts to reach underrepresented subgroups.
Our partnerships with patient organizations included bidirectional communication and collaboration throughout study development and procedures. This allowed us to learn from community leaders’ expertise with respect to community engagement tactics, buy-in from trusted stakeholders with public-facing evidence of partnership and collaboration, and access to established online patient communities. Advice from community leaders about language and picture/image use for study ads may impact the likelihood of viewers taking notice and engaging with the online content. Community-based participatory research (CBPR) methods advocate for this type of collaboration between researchers and the target population and have been shown to increase recruitment and retention of low-income and minority groups.29 Parallel guidelines for building inroads with virtual patient communities are needed. It may be useful to connect with digital community leaders outside the narrow scope of the research topic to engage broader audiences and connect with hard-to-reach and under-represented groups.
To improve participation rates, there is also a need for better communication to patients about the importance of research, opportunities to participate and dissemination of findings, whether through online or offline efforts. We previously found that AYA cancer survivors wanted to play an active role across the continuum of translational research and believed researchers should be more proactive in communicating with patients about study findings and scientific advances related to their disease.30 Partnering with patient organizations helps to overcome barriers, build trust and facilitate communication with patient communities.31,32 Building on this, efforts are needed to support meaningful engagement among patients, advocates, researchers and clinicians on a larger scale. There is evidence of this trend, as patient powered research networks and patient-partnered research are continuing to grow (e.g. CountMeIn, PatientsLikeMe),33,34 along with the rapid development of digital health tools to support innovative engagement among stakeholders. The EveryoneIncluded™ framework out of Stanford University was created to guide meaningful patient partnership during medical research events, based on values of mutual respect and inclusivity, and has set forth 10 guiding principles for digital health innovation in patient care and research (e.g. co-design with patients and healthcare stakeholders).35 The NCI also recognizes the need for evidence-based social media strategies to engage and educate diverse stakeholders.36 Paralleling the fundamental concept of precision medicine, ‘precision engagement’ aims to connect with patients at the right time, in the right place, with the right information based on their unique needs.37 These methods should be applied to research contexts as well as clinical care.
An important but sometimes overlooked aspect of patient-partnered research is the dissemination of findings back to participants and patient communities. Greater efforts to make participants aware of study results and scientific advancement is not only consistent with an overall philosophy of respect, but may also engender an attitudinal and cultural shift in which patients are able to recognize and be proud of their contribution to science. Creating a system in which patients feel good about their participation (often despite any personal benefit) may be akin to positive reinforcement. On an individual level, patients may be more open to future research opportunities. For AYA cancer survivors who are at increased risk for secondary health issues over the course of their lifetime, this is an important patient group to learn from and align with as long-term research partners and consumers of healthcare. Participants are also likely to share experiences with their social network, particularly as patient communities become more interconnected. Experiencing and then sharing a positive outlook on research participation may help to shift the overall landscape of patient involvement. In our study, we created a monthly newsletter we send to our participants; response to this simple outreach was overall positive, with many recipients expressing an interest in learning about where our research is heading and a desire to participate in future studies. Given low rates of participation among younger-aged cancer survivors,2 closing the communication loop in this way by sharing updates, study findings and plans for ‘next steps’ establishes a foundation of mutual respect and goodwill. Over time, such efforts may start to change patient perceptions of research and support genuine collaboration between research and patient communities.26
Finally, ethical and privacy concerns associated with social media recruitment should be addressed, as online methods may involve tracking, profiling and targeting of users. For example, simply clicking on a recruitment message may provide user data to online behavioral advertising companies, potentially leaving an identifiable trail. Bender et al.38 reviewed guidelines for risk mitigation and proposed a privacy-enhanced social media recruitment framework, including proactive and preventative measures to protect privacy and inform users of potential risks.38,39 Resources can also be found through the Connected & Open Research Ethics (CORE),40 including regulatory information, training webinars and thought leadership, and through published guidelines for online recruitment and methodology to inform study design and regulatory review.41,42 The absence of clear federal guidance regarding the appropriate use of social media in research generates uncertainty for both the researcher and IRB when considering ethical issues related to the management and mitigation of risks to human subjects. Gelinas et al.43 offer guidelines and an investigator checklist for social media recruitment; however, there remain gaps in regulatory guidance and widespread adoption of concrete, practical directives for investigators and IRBs is needed.
Limitations
This study evaluated recruitment methods for an AYA cancer and fertility study, including female participants between 15–39 years old, who were primarily White and well educated. However, minority participants represented 27% of our sample, which is similar to population-based estimates for this age group of survivor racial/ethnic representation.22,44 Similar to other cancer and fertility studies,11 the ages of participants skewed toward the older end of the ‘adolescent and young adult’ age range, which is consistent with our prior work demonstrating less fertility concern among adolescents and survivors in their early 20s, as they report a greater focus on higher priority tasks such as school achievement.45 We also evaluated PROs designed to meet our study objectives, which included measures specific to fertility and family-building experiences after cancer. Findings may not generalize to other patient subgroups or PROs. Common to social media research,3,23 we were unable to document more detailed social media metrics, such as number of ‘impressions’ or message views, making it difficult to quantify an appropriate denominator for social media recruitment or understand ‘passive refusal’ within this group (i.e. those who may have been eligible and saw the recruitment message, but did not click the link). Other offline and online recruitment strategies, such as attending patient conferences, creating a Facebook study page, or utilizing additional social media platforms (e.g. Twitter or Snapchat) may also be useful for recruitment but were not tested.
Conclusion
Findings suggested online, social media recruitment may be a more effective and efficient strategy compared to offline, hospital-based methods in terms of numbers of participants enrolled and use of study resources. However, group differences were identified that could bias findings and limit generalizability. Advantages of social media should be considered with an understanding of how methodology may impact enrollment and results, and measures should be taken to ensure best representation of the target population.
Supplemental Material
Supplemental Material for Recruitment via social media: advantages and potential biases by Catherine Benedict, Alexandria L Hahn, Michael A Diefenbach and Jennifer S Ford in Digital Health
Acknowledgements
We would like to thank the young adult cancer patient organizations for their help with social media recruitment: Stupid Cancer (Matthew Zachary), Lacuna Loft (Mallory Casperson), The Samfund (Samantha Watson and Michelle Landwehr) and GRYT Health (Dave Fuehrer).
Conflict of interest
The authors declare that there are no financial conflicts of interest. Catherine Benedict is a member of the Stupid Cancer Board of Directors, a Research Advisor to GRYT Health and a member of the Advisory Council for the Alliance for Fertility Preservation (unpaid positions with no financial relationships). None of these organizations were involved in the analysis or interpretation of data or in manuscript preparation.
Contributorship
CB and AH researched literature. CB, MD, and JF conceived the study. CB, AH, MD and JF were involved in protocol development, gaining ethical approval, patient recruitment and data analysis. CB wrote the first draft of the manuscript. AH, MD and JF contributed important intellectual content for the manuscript. All authors reviewed and edited the manuscript and approved the final version of the manuscript.
Ethical approval
The ethics committee of Northwell Health approved this study (REC number: 16-876)
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the National Cancer Institute [R03 CA212924].
Guarantor
CB
Peer review
This manuscript was reviewed by three reviewers, the authors have elected for these individuals to remain anonymous.
Supplemental material
Supplemental material for this article is available online.
References
- 1. Challenges conducting qualitative psychosocial research for adolescent and young adult patients and survivors. J Adolesc Young Adult Oncol 2011; 1: 71–76. [DOI] [PubMed] [Google Scholar]
- 2.Tonorezos ES and, Oeffinger KC. Research challenges in adolescent and young adult cancer survivor research . Cancer 2011; 117: 2295–2300. [DOI] [PubMed] [Google Scholar]
- 3.Gorman JR, Roberts SC, Dominick SA, et al. A diversified recruitment approach incorporating social media leads to research participation among young adult-aged female cancer survivors. J Adolesc Young Adult Oncol 2014; 3: 59–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Khatri C, Chapman SJ, Glasbey J, et al. Social media and internet driven study recruitment: evaluating a new model for promoting collaborator engagement and participation. PLoS One 2015; 10: e0118899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Burton-Chase AM, Parker WM, Hennig K, et al. The use of social media to recruit participants with rare conditions: Lynch syndrome as an example. JMIR Res Protoc 2017; 6: e12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Arigo D, Pagoto S, Carter-Harris L, et al. Using social media for health research: methodological and ethical considerations for recruitment and intervention delivery. Digit Health 2018; 4: 1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Burke-Garcia A, Scally G. Trending now: future directions in digital media for the public health sector. J Public Health 2014; 36(4): 527–534. [DOI] [PubMed] [Google Scholar]
- 8.Christensen T, Riis AH, Hatch EE, et al. Costs and efficiency of online and offline recruitment methods: a web-based cohort study. J Med Internet Res 2017; 19(3): e58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Whitaker C, Stevelink S, Fear N. The use of Facebook in recruiting participants for health research purposes: a systematic review. J Med Internet Res 2017; 19(8): e290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Topolovec-Vranic J, Natarajan K. The use of social media in recruitment for medical research studies: a scoping review. J Med Internet Res 2016; 18(11): e286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Logan S, Perz J, Ussher JM, et al. A systematic review of patient oncofertility support needs in reproductive cancer patients aged 14 to 45 years of age. Psychooncology. 2018; 27(2): 401–409. [DOI] [PubMed] [Google Scholar]
- 12.Benedict C, Thom B, Friedman D, et al. Young adult female cancer survivors' unmet information needs and reproductive concerns contribute to decisional conflict regarding posttreatment fertility preservation . Cancer 2016; 122(13): 2101–2109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shacham S. A shortened version of the profile of mood states. J Pers Assess 1983; 47(3): 305–306. [DOI] [PubMed] [Google Scholar]
- 14.Gorman JR, Su HI, Pierce JP, et al. A multidimensional scale to measure the reproductive concerns of young adult female cancer survivors. J Cancer Surviv 2014; 8(2): 218–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ashley L, Smith AB, Keding A, et al. Psychometric evaluation of the revised illness perception questionnaire (IPQ-R) in cancer patients: confirmatory factor analysis and Rasch analysis. J Psychosom Res 2013; 75(6): 556–562. [DOI] [PubMed] [Google Scholar]
- 16.Weiss DS. The impact of event scale: Revised In: Wilson JP, Tang CS. (eds) Cross-Cultural Assessment of Psychological Trauma and PTSD. International and Cultural Psychology Series. Boston, MA: Springer US, 2007, pp. 219–238. [Google Scholar]
- 17.de Souza JA, Yap BJ, Hlubocky FJ, et al. The development of a financial toxicity patient-reported outcome in cancer: the cost measure. Cancer 2014; 120(20): 3245–3253. [DOI] [PubMed] [Google Scholar]
- 18.O'Connor AM. Validation of a decisional conflict scale. Med Decis Making 1995; 15(1): 25–30. [DOI] [PubMed] [Google Scholar]
- 19.Ottawa Hospital Research Institute. Decision Self-Efficacy – Evaluation Measures – Patient Decision Aids, https://decisionaid.ohri.ca/eval_self.html (2017, accessed 12 June 2019).
- 20.Harlan LC, Lynch CF, Keegan THM, et al. Recruitment and follow-up of adolescent and young adult cancer survivors: the AYA HOPE Study. J Cancer Surviv 2011; 5(3): 305–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gorman JR, Su HI, Roberts SC, et al. Experiencing reproductive concerns as a female cancer survivor is associated with depression. Cancer 2015; 121(6): 935–942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.National Cancer Institute. SEER Cancer Statistics Review 1975–2015. Adolescent and Young Adult Cancer by Site Incidence, Survival, and Mortality, https://seer.cancer.gov/archive/csr/1975_2015/results_merged/sect_32_aya.pdf.
- 23.Keaver L, McGough A, Du M, et al. Potential of using Twitter to recruit cancer survivors and their willingness to participate in nutrition research and web-based interventions: a cross-sectional study. JMIR Cancer 2019; 5(1): e7850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Walsh MC, Trentham-Dietz A, Gangnon RE, et al. Selection bias in population-based cancer case-control studies due to incomplete sampling frame coverage. Cancer Epidemiol Biomarkers Prev 2012; 21(6): 881–886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Konkel L. Racial and ethnic disparities in research studies: the challenge of creating more diverse cohorts. Environ Health Perspect 2015; 123(12): A297–A302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Owen JE, Bantum EOC, Criswell K, et al. Representativeness of two sampling procedures for an internet intervention targeting cancer-related distress: a comparison of convenience and registry samples. J Behav Med 2014; 37(4): 630–641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fallon EA, Driscoll D, Smith TS, et al. Description, characterization, and evaluation of an online social networking community: the American Cancer Society’s Cancer Survivors Network(r). J Cancer Surviv 2018; 12(5): 691–701. [DOI] [PubMed] [Google Scholar]
- 28.Lattie EG, Kaiser SM, Alam N, et al. A practical do-it-yourself recruitment framework for concurrent eHealth clinical trials: identification of efficient and cost-effective methods for decision making (part 2). J Med Internet Res 2018; 20(11): e11050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nicholson LM, Schwirian PM and, Groner JA. Recruitment and retention strategies in clinical studies with low-income and minority populations: progress from 2004–2014. Contemp Clin Trials 2015; 45: 34–40. [DOI] [PubMed] [Google Scholar]
- 30.Benedict C, Victorson D, Love B, et al. The audacity of engagement: hearing directly from young adults with cancer on their attitudes, perceptions, and preferences of AYA cancer survivorship and cancer survivorship research. J Adolesc Young Adult Oncol 2018; 7(1): 103–111. [DOI] [PubMed] [Google Scholar]
- 31.Forsythe LP, Ellis LE, Edmundson L, et al. Patient and stakeholder engagement in the PCORI pilot projects: description and lessons learned. J Gen Intern Med 2016; 31(1): 13–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kirwan JR, de Wit M, Frank L, et al. Emerging guidelines for patient engagement in research. Value Health 2017; 20(3): 481–486. [DOI] [PubMed] [Google Scholar]
- 33.Count Me In. https://joincountmein.org/projects (accessed 6 December 2018).
- 34.Wicks P, Massagli M, Frost J, et al. Sharing health data for better outcomes on patientslikeme. J Med Internet Res 2010; 12(2): e19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Stanford Medicine X. Everyone included™, http://everyoneincluded.org (accessed 12 December 2018).
- 36.National Cancer Institute. At the crossroads of social media and clinical trials: A workshop on the future of clinician, patient and community engagement, 7 June 2018, Bethesda, MD, USA, https://videocast.nih.gov/launch.asp?23947 (accessed 15 October 2018).
- 37.Wagner JK, Peltz-Rauchman C, Rah AK, et al. Precision engagement: the PMI's success will depend on more than genomes and big data. Genet Med 2017; 19: 620–624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bender JL, Cyr AB, Arbuckle L, et al. Ethics and privacy implications of using the internet and social media to recruit participants for health research: a privacy–by-design framework for online recruitment. J Med Internet Res 2017; 19(4): e104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cavoukian A. Privacy by design in law, policy and practice. White paper for regulators, decision-makers and policy-makers, http://www.ontla.on.ca/library/repository/mon/25008/312239.pdf (2011, accessed 1 November 2018).
- 40.Connected and Open Research Ethics (CORE). https://thecore.ucsd.edu/ (accessed 15 October 2018).
- 41.Cavoukian A. Privacy by design: leadership, methods, and results In: Gutwirth S, Leenes R, de Hert P, et al. (eds) European Data Protection: Coming of age. New York, NY: Springer Netherlands, 2013, pp. 175–202. [Google Scholar]
- 42.Schaub F, Balebako R, Durity A, et al. A design space for effective privacy notices. Symposium on Usable Privacy and Security (SOUPS), 22–24 July 2015, Ottawa, Canada, https://www.usenix.org/conference/soups2015/proceedings/presentation/schaub (accessed 17 August 2018).
- 43.Gelinas L, Pierce R, Winkler S, et al. Using social media as a research recruitment tool: ethical issues and recommendations. Am J Bioeth 2017; 17(3): 3–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tai E, Buchanan N, Townsend J, et al. Health status of adolescent and young adult cancer survivors . Cancer 2012; 118: 4884–4891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Benedict C, Shuk E, Ford JS. Fertility issues in adolescent and young adult cancer survivors. J Adolesc Young Adult Oncol 2016; 5(1): 48–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material for Recruitment via social media: advantages and potential biases by Catherine Benedict, Alexandria L Hahn, Michael A Diefenbach and Jennifer S Ford in Digital Health