Abstract
Background: Routine imaging (“scan”) results contain key prognostic information for advanced cancer patients. Yet, little is known about how accurately patients understand this information, and whether psychological states relate to accurate understanding.
Objective: To determine if patients' sadness and anxiety, as well as results showing poorer prognosis, are associated with patients' understanding of scan results.
Design: Archival contrasts performed on multi-institutional cohort study data.
Subjects: Advanced cancer patients whose disease progressed after at least one chemotherapy regimen (N = 94) and their clinicians (N = 28) were recruited before an oncology appointment to discuss routine scan results.
Measurements: In preappointment structured interviews, patients rated sadness and anxiety about their cancer. Following the appointment, patients and clinicians reported whether the imaging results discussed showed progressive, improved, or stable disease.
Results: Overall, 68% of patients reported their imaging results accurately, as indicated by concordance with their clinician's rating. Accuracy was higher among patients whose results indicated improved (adjusted odds ratio [AOR] = 4.12, p = 0.02) or stable (AOR = 2.59, p = 0.04) disease compared with progressive disease. Patients with greater anxiety were less likely to report their imaging results accurately than those with less anxiety (AOR = 0.09, p = 0.003); in contrast, those with greater sadness were more likely to report their results accurately than those with less sadness (AOR = 5.23, p = 0.03).
Conclusions: Advanced cancer patients with higher anxiety and those with disease progression may need more help understanding or accepting their scan results than others.
Keywords: anxiety, delivery of health care, health knowledge, neoplasms, psycho-oncology
Introduction
For patients with advanced cancer to make informed health care decisions, they must understand the meaning of medical test results in the context of their disease.1,2 Routine imaging tests (hereafter, referred to as “scan results”) provide information regarding the patient's response to anticancer treatments, with implications for prognosis and treatment decision making. Results showing disease progression may suggest an important transition in a patient's illness trajectory, appropriately prompting a timely discussion of a patient's goals of care, end-of-life (EoL) preferences, and integrating palliative care. Accordingly, patients who understand their scan results accurately are likely better equipped to engage in informed medical decision making.
In addition, cancer patients frequently report nervousness about appointments and scans,3–5 which may influence their ability to engage fully in clinical discussions. Stress, sadness, and anxiety can influence information processing (e.g., by interfering with cognitive function6,7 or prompting avoidance of distressing information8). Furthermore, the extent to which patients' psychological states affect clinical discussions has been identified as a research priority among serious illness communication experts.9
Despite considerable research examining major medical consultations (e.g., regarding recurrence10) and EoL discussions,11–13 the extent to which patients understand and accurately summarize their scan results has been understudied. This is unfortunate given that scan results are frequently discussed in advanced cancer care and provide opportunities for discussing the patient's prognosis. We examined patients' accuracy regarding recently discussed scan results (i.e., their understanding of the gist of the results as progressive, improved, or stable disease). We compared patients' reports of the scan results with their oncology clinicians' reports as the criterion standard, given that clinicians routinely relay these results in clinical practice. To examine whether patients' psychological states may influence their understanding of this information, we tested whether cancer-related sadness and anxiety assessed before the discussion predicted patients' accuracy in reporting their scan results. Because results indicating progressive disease in this context may suggest a need to discuss overall prognosis and goals of care, we tested whether patient accuracy varied by the type of scan result.
Methods
Study sample
The study utilized data from Coping with Cancer-II (CwC-II), a multisite observational study conducted to examine clinical communication processes and outcomes in end-stage cancer care. Participants were adult cognitively intact patients with advanced/metastatic solid tumors refractory to at least one chemotherapy regimen.14 Institutional Review Boards at all participating sites approved the study procedures; all participants provided written informed consent.
Oncology clinicians were interviewed following patients' clinic visits in which routine disease-monitoring scan results were discussed. In preappointment structured interviews, patients reported their levels of cancer-related sadness and anxiety, as well as their overall psychological well-being as part of the McGill Quality of Life Questionnaire.15 In postappointment interviews, patients recalled the scan results discussed in the visit.
The analytic sample consisted of 94 advanced cancer patients recruited from five CwC-II sites where scan results were discussed (Meyer Cancer Center at Weill Cornell Medicine; Memorial Sloan Kettering Cancer Center; Yale Cancer Center; Dana-Farber Cancer Institute/Brigham and Women's Hospital; and Parkland Hospital) with a member of their oncology team (N = 28 unique clinicians) and had complete data on variables included in the analyses. Patients in the analytic sample were less likely to be black than other patients participating in CwC-II at these five sites (11% vs. 26% black; p < 0.01) but did not differ from other patients with respect to age, sex, education, or insurance status. Preappointment interviews were conducted a median of 33 (interquartile range: 15–60) days before their scan discussion clinic visit; postappointment interviews were conducted a median of 6 (interquartile range: 0–14) days following the visit.
Measures
Patient sociodemographic characteristics
Patients provided demographic information at baseline, including age, gender, race, ethnicity, education (years of formal schooling), and health insurance status.
Cancer-related sadness and anxiety
During preappointment interviews, patients rated the extent to which they felt sad or anxious about their cancer diagnosis. Response options included “not at all,” “somewhat,” “a great deal,” and “completely.” For analysis and ease of interpretation, we dichotomized anxiety and sadness variables into lower (“not at all” and “somewhat”) and higher (“a great deal” and “completely”) categories. The anxiety and sadness variables were correlated with the psychological well-being subscale of the McGill Quality of Life Questionnaire (r = −0.47, p < 0.001 and r = −0.43, p < 0.001, respectively).
Clinician assessment of imaging results
Following the clinic visit in which imaging results were discussed, the clinician was asked whether the scan indicated that the patient's disease was progressive, improved, or stable. This clinician assessment served as an indicator of the patient's disease trajectory.
Accuracy in patient understanding of imaging results
In postappointment interviews, patients were asked whether their oncologist said their cancer was worse, better, or stable; additional responses included “other” or “do not know.” Patient responses were coded as “accurate” or “inaccurate” based on concordance with the clinician's assessment of the scan results. Accurate patient responses were those that matched the clinician assessment (e.g., clinician indicated a “progressive” result and patient reported “My cancer is worse”). Inaccurate patient responses were those that differed from the clinician assessment (e.g., clinician reported a “progressive” result and patient reported the cancer was better, stable, other, or do not know). We included “other” and “do not know” responses in the inaccurate category, as they demonstrated that the patient's summary did not specifically match the clinician assessment.
Data analysis
Odds ratios between patient characteristics and accurate understanding of the scan results, accounting for nesting of patients within clinicians, were estimated using logistic regression models specified using generalized estimating equations. Single-predictor models evaluated bivariate associations between patient characteristics and patient accuracy for scan results. A multiple-predictor model, which included patient sociodemographic characteristics, times between the interviews and clinic visit, sadness and anxiety, and current disease trajectory as predictors, evaluated associations between each predictor and patient accuracy for scan results, independent of the effects of other predictors in the model. Statistical analyses were conducted in SAS version 9.4.
Results
Table 1 presents patient characteristics and their bivariate (unadjusted) and independent (adjusted) associations with having an accurate understanding of their scan results. Patients in the study sample were primarily white (89.4%), middle-aged to older (mean = 61.3 years, standard deviation [SD] = 9.6 years), female (72.3%), educated beyond high school (69.1%), and insured (85.1%). Most patients (68%) reported their scan results accurately, as indicated by agreement with their clinician's rating.
Table 1.
Patient Variables and Their Unadjusted (OR) and Adjusted (AOR) Associations with Patients' Accurate Understanding of Their Scan Results (N = 94)
| Accurate understanding | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Full sample | Yes | No | ||||||||
| 94 | 100% | 64 | 68% | 30 | 32% | |||||
| Variable | n | % | n | % | n | % | OR | p | AOR | p |
| Demographic | ||||||||||
| Age (years) | ||||||||||
| ≥65 | 34 | 36.2 | 27 | 42.2 | 7 | 23.3 | 2.42 | 0.058 | 1.33 | 0.610 |
| <65 | 60 | 63.8 | 37 | 57.8 | 23 | 76.7 | Ref. | Ref. | ||
| Sex | ||||||||||
| Male | 26 | 27.7 | 17 | 26.6 | 9 | 30.0 | 0.80 | 0.631 | 1.55 | 0.505 |
| Female | 68 | 72.3 | 47 | 73.4 | 21 | 70.0 | Ref. | Ref. | ||
| Race | ||||||||||
| Black | 10 | 10.6 | 5 | 7.8 | 5 | 16.7 | 0.45 | 0.158 | 0.39 | 0.274 |
| White | 84 | 89.4 | 59 | 92.2 | 25 | 83.3 | Ref. | Ref. | ||
| Education (years) | ||||||||||
| >12 | 65 | 69.1 | 43 | 67.2 | 22 | 73.3 | 0.73 | 0.419 | 0.26 | 0.041 |
| ≤12 | 29 | 30.9 | 21 | 32.8 | 8 | 26.7 | Ref. | Ref. | ||
| Insurance status | ||||||||||
| Insured | 80 | 85.1 | 59 | 92.2 | 21 | 70.0 | 5.01 | 0.002 | 8.24 | 0.002 |
| Not insured | 14 | 14.9 | 5 | 7.8 | 9 | 30.0 | Ref. | Ref. | ||
| Psychological | ||||||||||
| Sadness | ||||||||||
| Higher | 28 | 29.8 | 21 | 32.8 | 7 | 23.3 | 1.66 | 0.164 | 5.23 | 0.030 |
| Lower | 66 | 70.2 | 43 | 67.2 | 23 | 76.7 | Ref. | Ref. | ||
| Anxiety | ||||||||||
| Higher | 22 | 23.4 | 11 | 17.2 | 11 | 36.7 | 0.36 | 0.017 | 0.09 | 0.003 |
| Lower | 72 | 76.6 | 53 | 82.8 | 19 | 63.3 | Ref. | Ref. | ||
| Disease trajectory | ||||||||||
| Gist of test result | ||||||||||
| Better | 16 | 17.0 | 12 | 18.8 | 4 | 13.3 | 1.86 | 0.344 | 4.12 | 0.019 |
| Stable | 42 | 44.7 | 30 | 46.9 | 12 | 40.0 | 1.61 | 0.232 | 2.59 | 0.040 |
| Worse | 36 | 38.3 | 22 | 34.4 | 14 | 46.7 | Ref. | Ref. | ||
Accurate understanding of the scan results is based on the oncologist's interpretation of the scans. Both ORs and AORs account for patient nesting among oncology clinicians (N = 28). AORs adjusted for sociodemographic, psychological, and disease trajectory variables as well as time between previsit interview and test–result clinical visit, and for time between test–result clinical visit and postvisit interview.
AOR, adjusted odds ratio; OR, odds ratio.
In unadjusted analyses, patients who reported feeling “a great deal” or “completely” anxious about their cancer were less likely to have an accurate understanding of their scan results compared with those who felt “somewhat” or “not at all” anxious about their disease (OR = 0.36, p = 0.02).
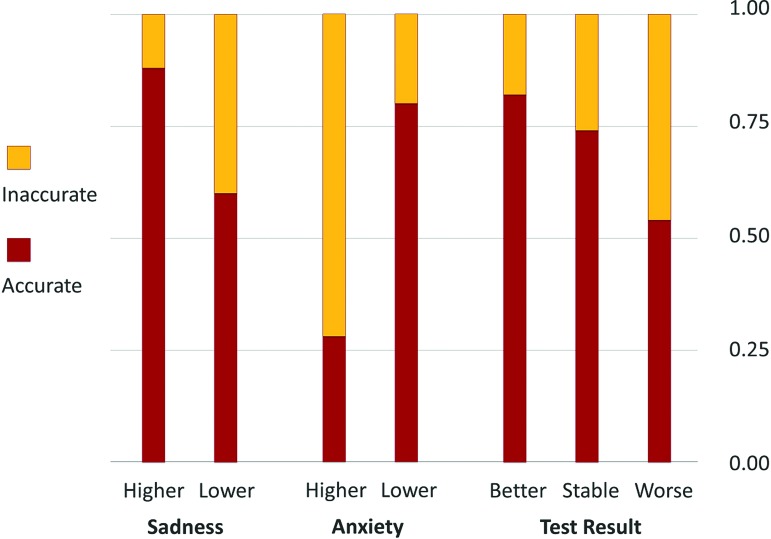
Accounting for other characteristics, greater anxiety was associated with lower (adjusted odds ratio [AOR] = 0.09, p < 0.01), and greater sadness was associated with higher (AOR = 5.23, p = 0.03), odds of a patient having an accurate understanding of the test results. Consistent with the depression and anxiety literature, cancer-related sadness and anxiety were significantly related (OR = 9.73, p < 0.001), yet each had distinct relationships with patients' understanding. Patients whose scans showed improved (AOR = 4.12, p = 0.02) or stable (AOR = 2.59, p = 0.04) disease were more likely to report results accurately compared with those whose scans showed disease progression. Figure 1 portrays the effects of sadness, anxiety, and current disease trajectory (test result) on the relative proportions of patients with accurate and inaccurate understanding of their scan results, adjusting for the other factors included in the final multivariable model.
FIG. 1.
Illustration of the effects of psychological factors and prognosis on the relative proportions of patients with accurate and inaccurate understanding of recently discussed scan results, as indicated by concordance with their clinician's rating. “Accurate understanding” bars indicate the probability that a person in the specified category (e.g., higher anxiety) reports an accurate understanding of the scan results, adjusting for the other factors included in the final multivariable model (age, sex, race, education, insurance status, time between interviews and clinical visit, and the other psychological or test result effects, respectively). Color image is available online.
Discussion
We compared advanced cancer patients' reports of their recently discussed scan results with their clinicians' interpretations to examine patients' accuracy about whether the scans showed progressive, improved, or stable disease. Overall, most patients (68%) accurately reported the interpretation given by their clinicians. For these patients, clinicians may capitalize on this understanding by broaching or continuing prior discussions about prognosis, treatment options, and care preferences. While some uncertainty may remain despite consultation, patients have a better understanding of their illness after recent prognostic discussions than in the absence of these discussions.13
Our results also highlight that a subset of patients do not share their clinicians' interpretation of scan results. Among patients whose scan results indicated progressive disease, 39% had an inaccurate understanding; these patients were significantly less likely to report their results accurately than those with improved or stable results in adjusted analyses. Furthermore, our results indicate that psychological states may influence how patients interpret information about their scan results, suggesting potential intervention targets. Patients who reported feeling “a great deal” or more anxiety about their cancer diagnosis were approximately 10 times less likely to identify their scan results accurately than those who were less anxious. Future studies should confirm these results using more comprehensive assessments of anxiety and depression.
In line with clinical communication guidelines,2 assessing patients' overall understanding (e.g., “What have you taken away from our conversation about these results?”) after delivering news will likely help to identify patients with inaccurate understanding of their results. This approach may be particularly important for those with progressive disease and those with anxiety, and could facilitate discussion about realistic expectations for outcomes of cancer treatments, the utility of palliative care, and patients' EoL care preferences. Accordingly, routine scan results provide opportunities for discussing overall prognosis, connecting patient goals of care with their values, facilitating family discussions, and enhancing overall illness understanding.
Acknowledgment
The authors thank the patients and clinicians who participated in this study.
The study and manuscript preparation were supported in part by the National Cancer Institute (CA106370, CA197730, CA008748), the National Institute on Minority Health Disparities (MD007652), the National Institute on Aging (AG049666), and the National Institute of Nursing Research (NR016905).
Author Disclosure Statement
No competing financial interests exist.
References
- 1. Reyna VF, Nelson WL, Han PK, Pignone MP: Decision making and cancer. Am Psychol 2015;70:105–11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Gilligan T, Coyle N, Frankel RM, et al. : Patient-clinician communication: American Society of Clinical Oncology Consensus Guideline. J Clin Oncol 2017;35:3618–3632 [DOI] [PubMed] [Google Scholar]
- 3. Peteet JR, Stomper PC, Ross DM, et al. : Emotional support for patients with cancer who are undergoing CT: Semistructured interviews of patients at a cancer institute. Radiology 1992;182:99–102 [DOI] [PubMed] [Google Scholar]
- 4. Bauml JM, Troxel A, Epperson CN, et al. : Scan-associated distress in lung cancer: Quantifying the impact of “scanxiety”. Lung Cancer 2016;100:110–113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Mehnert A, Berg P, Henrich G, Herschbach P: Fear of cancer progression and cancer‐related intrusive cognitions in breast cancer survivors. Psychooncology 2009;18:1273–1280 [DOI] [PubMed] [Google Scholar]
- 6. Dolcos F, McCarthy G: Brain systems mediating cognitive interference by emotional distraction. J Neurosci 2006;26:2072–2079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Shields GS, Sazma MA, Yonelinas AP: The effects of acute stress on core executive functions: A meta-analysis and comparison with cortisol. Neurosci Biobehav Rev 2016;68:651–668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. de Ruiter C, Brosschot JF: The emotional Stroop interference effect in anxiety: Attentional bias or cognitive avoidance? Behav Res Ther 1994;32:315–319 [DOI] [PubMed] [Google Scholar]
- 9. Tulsky JA, Beach MC, Butow PN, et al. : A research agenda for communication between health care professionals and patients living with serious illness. JAMA Intern Med 2017;177: 1361–1366 [DOI] [PubMed] [Google Scholar]
- 10. Bousquet G, Orri M, Winterman S, et al. : Breaking bad news in oncology: A metasynthesis. J Clin Oncol 2015;33:2437–2443 [DOI] [PubMed] [Google Scholar]
- 11. Wright AA, Zhang B, Ray A, et al. : Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. JAMA 2008;300:1665–1673 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Zhang B, Wright AA, Huskamp HA, et al. : Health care costs in the last week of life: Associations with end-of-life conversations. Arch Intern Med 2009;169:480–488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Epstein AS, Prigerson HG, O'Reilly EM, Maciejewski PK: Discussions of life expectancy and changes in illness understanding in patients with advanced cancer. J Clin Oncol 2016;34:2398–2403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Cohen SM, Maciejewski RC, Shah MA, et al. : Being present: Oncologists' role in promoting advanced cancer patients' illness understanding. Cancer Med 2018;7:1511–1518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Cohen SR, Mount BM, Strobel MG, Bui F: The McGill Quality of Life Questionnaire: A measure of quality of life appropriate for people with advanced disease. A preliminary study of validity and acceptability. Palliat Med 1995;9:207–219 [DOI] [PubMed] [Google Scholar]