Abstract
Respiratory epithelial adenomatoid hamartoma (REAH) is a rare lesion in nasal cavity first reported by Wenig and Heffner in 1995. Most commonly seen in men in third to ninth decade of life. Majority of cases presents as a polypoidal mass in one or both nasal cavities. We experienced such a case of REAH originating from the nasal septum, in posterior aspect, treated by endoscopic approach. It is important to differentiate REAH from other sinonasal pathologies like inverted papilloma and low grade sinonasal adenocarcinoma. Complete surgical resection is the treatment of choice.
Keywords: nasal polyps, otolaryngology/ENT
Background
Respiratory epithelial adenomatoid hamartoma (REAH) is a benign glandular proliferation arising from surface epithelium of nasal cavity and sinonasal tract. It lack the ability to grow, resulting in self-limited proliferation.1–3 In 1995, Birt and Knight-Jones reported the first case of a hamartoma in the upper aerodigestive tract.4 5 A particular type of hamartoma first introduced by Weing and Heffner in 1995 and termed as REAH.1 Almost 70% of REAHs occur in the nasal cavity presenting as polypoidal mass over the posterior part of nasal septum. These lesions also have been reported to occur in paranasal sinuses and nasopharynx.6 7
Histopathological features remains gold standard for diagnosis. It is important to differentiate REAH from other sinonasal pathologies like inverted papilloma (IP) or low grade sinonasal adenocarcinoma which requires extensive surgical procedures.
Case presentation
A 62-year-old man presented with history of bilateral nasal obstruction, snoring causing social discomfort and anosmia since last 4 years. The patient had no history of allergy and any other medical and surgical history. On anterior rhinoscopy, polyps were seen in both the nasal cavities. A clinical diagnosis of sinonasal polyposis was made.
Investigations
CT paranasal sinus (PNS) (plain) revealed extensive soft tissue opacification involving bilateral paranasal sinuses with widened osteomeatal unit, causing expansion and near complete obliteration of the nasal cavities. Patient underwent endoscopic sinus surgery for sinonasal panpolyposis (figure 1A).
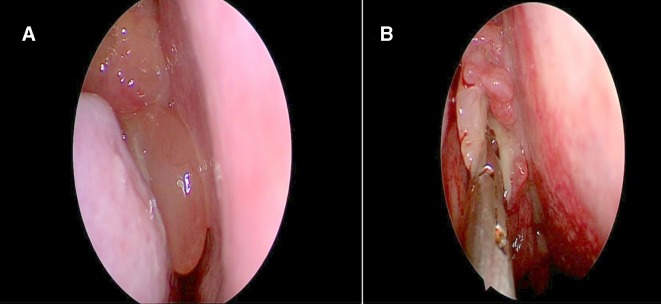
Figure 1.
(A) Diagnostic endoscopic picture of polyp on right side; (B) biopsy of polypoidal tissue with rubbery consistency medial to middle turbinate.
Intraoperatively, polypoidal tissue was found over the cribriform plate and septum medial to the middle turbinate, with smooth surface and rubbery consistency not mimicking a nasal polyp. Biopsy was taken and sent for histopathological examination (figure 1B).
Histological analysis revealed pseudostratified columnar epithelium with plenty of glands lined by ciliated epithelium, showing pseudostratification and oedematous stroma. The pathological findings were consistent with respiratory epithelial adenomatous proliferation (figure 2).
Figure 2.
(A) Histopathological examination revealed polypoidal tissue lined by pseudostratified columnar epithelium beneath are glands lined by ciliated epithelium. (B) Magnified photo microscopic picture.
CT PNS with contrast and MRI was done to look for erosion of the cribriform plate and intracranial extension of the tumour. It revealed a soft tissue mass over the cribriform area without any intracranial extension.
Differential diagnosis
REAH.
IP.
Low grade sinonasal adenocarcinoma.
Treatment
Complete endoscopic excision of the tumour was done.
Outcome and follow-up
Procedure was uneventful. Patient tolerated the procedure well without any postoperative complications and he is under regular follow-up since 1 year with no evidence of recurrence.
Discussion
Hamartomas are benign, glandular proliferation of one or more cellular components of a surface epithelium of aerodigestive tract.6 8 REAH is very rare and self-limiting lesions which do not regress spontaneously, first reported by Wenig and Heffner in 1995.1 8 Most commonly seen in men with age group being third to ninth decade of life.8 Majority of cases occurs in the nasal cavity presenting as polypoidal mass causing nasal obstruction, nasal stuffiness, and anosmia, resembling chronic rhinosinusitis. The mechanism for the occurrence of hamartomas is still unclear but few studies reported it to originate from the inflammatory polyps.1
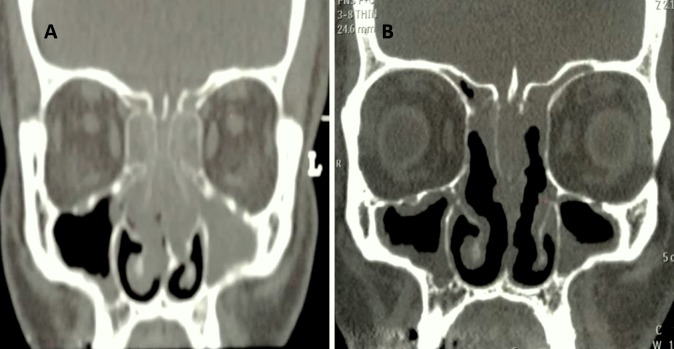
Radiographically, REAH presents as soft tissue density involving the sinuses and septum, giving the clinical picture of nasal polyposis as seen in our patient (figure 3). According to Lima et al, the most significant finding on imaging (CT PNS scan) to differentiate REAH from nasal polyps is enlargement of olfactory cleft.9 Majority of REAH occurs primarily on the nasal septum, especially in posterior area while IP arises almost exclusively on the lateral nasal wall.
Figure 3.
(A) Preoperation CT scan shows soft tissue sinus involving bilateral paranasal sinuses. (B) CT scan done after first surgery showing soft tissue density over the septum and in cribriform area.
REAH can be distinguished from IP and low grade sinonasal adenocarcinoma histologically. The main charateristic feature of REAH is, proliferation of glands, round to oval in shape, separated by stroma and glands distended by mucus. Basement membrane is invariably thickened with oedematous stroma with no metaplastic or atypical changes. In contrast, IPs predominately have proliferation of respiratory squamous epithelium with infiltration of neutrophils with basement membrane being thin and intact. Seromucinous glands are sparse to absent in IPs.10 Malignant transformation can occur rarely in IP.
Presence of intervening stroma between the ciliated glands in REAH is the most reliable way to distinguish it from low-grade sinonasal adenocarcinoma. Malignant features and dysplastic changes can often been seen in low grade sinonasal adenocarcinoma.
Treatment of this entity is complete local resection. Until, there is no evidence of recurrence. Malignant transformation also has never been reported.8
Patient’s perspective.
I had complaint of blocked nose from last few years. I took it as cold and consulted local physician for treatment. During early days I used to get relief but as time passed, I noticed for loss of my smell and started snoring which caused social discomfort to my spouse and relatives sleeping next to me.
Due to my working schedule and anxiety I did not consult to anyone. One day my wife told me to show to ear, nose, throat doctor for the same. About a month later I visited Mumbai for my work trip and finally I consulted to ear, nose and throat specialist. My mind perception was that it is just a cold and medical treatment will work.
Doctor examined me and asked to get CT scan done. CT scan was suggested of nasal polyps and will require surgery, which seems to be a routine operation. Surgery went well with endoscopy with no complication. Next day morning doctor briefed me about everything and explained me some tissue very near to the brain and looks like tumour. It was his judgement which could be identified as something else and he had sent it for examination. Hearing the word tumour, first thing came to my mind was ‘why me’. Report came as tumour but non-cancerous. As the tumour grows, it need come out without a doubt. He briefed me everything and made me aware of all the risks about cerebrospinal fluid (CSF) leak and repair. I decided to go through with it. Surgery went well and when I woke up after the operation I felt discomfort and headache due to nasal packing.
I am really grateful to the doctor and his team for alertness and judgement during surgery which helped me for my tumour diagnosis and complete removal of it.
He told me it is one of rare tumour not routinely seen in clinical practice. I’m regularly follow-up with him.
There is still loss of smell but snoring has really come down. My wife and children are really happy.
Learning points.
In our literature, Respiratory epithelial adenomatoid hamartoma (REAH) has received less attention due to uncommon clinical entity with its distinctive morphological features.
Diagnostic misinterpretation is a serious issue regarding this lesion.
Recognition and differentiation of REAH from other sinonasal pathologies is important in order to avoid excessive surgical procedures.
Footnotes
Contributors: RB and AAJ served as scientific advisors, critically reviewed the study proposal and proofread the article. ND helped in collecting data and SRA was involved with the idea of writing an article, technical editing, language editing and patient care.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Obtained.
References
- 1. Wenig BM, Heffner DK. Respiratory epithelial adenomatoid hamartomas of the sinonasal tract and nasopharynx: a clinicopathologic study of 31 cases. Ann Otol Rhinol Laryngol 1995;104:639–45. 10.1177/000348949510400809 [DOI] [PubMed] [Google Scholar]
- 2. Endo R, Matsuda H, Takahashi M, et al. Respiratory epithelial adenomatoid hamartoma in the nasal cavity. Acta Otolaryngol 2002;122:398–400. 10.1080/00016480260000085 [DOI] [PubMed] [Google Scholar]
- 3. Delbrouck C, Fernandez Aguilar S, Choufani G, et al. Respiratory epithelial adenomatoid hamartoma associated with nasal polyposis. Am J Otolaryngol 2004;25:282–4. 10.1016/j.amjoto.2004.02.005 [DOI] [PubMed] [Google Scholar]
- 4. Sangoi AR, Berry G. Respiratory epithelial adenomatoid hamartoma: diagnostic pitfalls with emphasis on differential diagnosis. Adv Anat Pathol 2007;14:11–16. 10.1097/PAP.0b013e31802efb1e [DOI] [PubMed] [Google Scholar]
- 5. Birt BD, Knight-Jones EB. Respiratory distress due to nasopharyngeal hamartoma. Br Med J 1969;3:281–2. 10.1136/bmj.3.5665.281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Himi Y, Yoshizaki T, Sato K, et al. Respiratory epithelial adenomatoid hamartoma of the maxillary sinus. J Laryngol Otol 2002;116:317–8. 10.1258/0022215021910672 [DOI] [PubMed] [Google Scholar]
- 7. Metselaar RM, Stel HV, van der Baan S. Respiratory epithelial adenomatoid hamartoma in the nasopharynx. J Laryngol Otol 2005;119:476–8. 10.1258/0022215054273124 [DOI] [PubMed] [Google Scholar]
- 8. Di Carlo R, Rinaldi R, Ottaviano G, et al. Respiratory epithelial adenomatoid hamartoma of the maxillary sinus: case report. Acta Otorhinolaryngol Ital 2006;26:225. [PMC free article] [PubMed] [Google Scholar]
- 9. Lima NB, Jankowski R, Georgel T, et al. Respiratory adenomatoid hamartoma must be suspected on CT-scan enlargement of the olfactory clefts. Rhinology 2006;44:264–9. [PubMed] [Google Scholar]
- 10. Barnes L. Schneiderian papillomas and nonsalivary glandular neoplasms of the head and neck. Mod Pathol 2002;15:279–97. 10.1038/modpathol.3880524 [DOI] [PubMed] [Google Scholar]