Abstract
Introduction:
Opioid overdose deaths quintupled in Massachusetts between 2000 and 2016. Potentially inappropriate opioid prescribing practices (PIP) are associated with increases in overdoses. The purpose of this study was to conduct spatial epidemiological analyses of novel comprehensively linked data to identify overdose and PIP hotspots.
Methods:
Sixteen administrative datasets, including prescription monitoring, medical claims, vital statistics, and medical examiner data, covering >98% of Massachusetts residents between 2011–2015, were linked in 2017 to better investigate the opioid epidemic. PIP was defined by six measures: ≥100 morphine milligram equivalents (MMEs), co-prescription of benzodiazepines and opioids, cash purchases of opioid prescriptions, opioid prescriptions without a recorded pain diagnosis, and opioid prescriptions through multiple prescribers or pharmacies. Using spatial autocorrelation and cluster analyses, overdose and PIP hotspots were identified among 538 ZIP codes.
Results:
More than half of the adult population (n=3,143,817, ages 18 and older) were prescribed opioids. Nearly all ZIP codes showed increasing rates of overdose over time. Overdose clusters were identified in Worcester, Northampton, Lee/Tyringham, Wareham/Bourne, Lynn, and Revere/Chelsea (Getis-Ord Gi*; p< 0.05). Large PIP clusters for ≥100 MMEs and prescription without pain diagnosis were identified in Western Massachusetts; and smaller clusters for multiple prescribers in Nantucket, Berkshire, and Hampden Counties (p<0.05). Co-prescriptions and cash payment clusters were localized and nearly identical (p<0.05). Overlap in PIP and overdose clusters was identified in Cape Cod and Berkshire County. However, we also found contradictory patterns in overdose and PIP hotspots.
Conclusions:
Overdose and PIP hotspots were identified, as well as regions where the two overlapped, and where they diverged. Results indicate that PIP clustering alone does not explain overdose clustering patterns. Our findings can inform public health policy decisions at the local level, which include a focus on PIP and misuse of heroin and fentanyl that aim to curb opioid overdoses.
Keywords: Opioid overdose, prescription opioids, Massachusetts, hotspots, Getis-Ord Gi*, clusters, geographic information systems (GIS)
Introduction:
Since 2000, the opioid epidemic has taken a severe toll across the United States (US). Opioid prescription rates have increased nearly threefold in the last 15 years—alongside an increase in opioid related overdoses and deaths.1 In the US, drug overdose has become the leading cause of accidental death. Of the estimated 52,404 lethal drug overdoses in 2015, 20,101 were related to the use of prescription pain relievers.2
Massachusetts has been particularly afflicted by the opioid epidemic. Massachusetts is one of 19 states with a statistically significant increase in overdose deaths from 2014–2015.1 Opioid-related mortality rates in Massachusetts have increased by 478% between 2000 and 2016, a rate several times faster than any previously experienced in the state.3 All Massachusetts counties and municipalities have been affected by the opioid epidemic in some form, but impact varies by region.4 Between 2011 and 2015, the overall state rate for opioid overdose was 15.4 deaths per 100,000 residents, which was higher than the national rate of 10.4 per 100,000.2 Since 2013, the rising overdose death numbers have been driven by the introduction of illicitly produced fentanyl in the opioid drug supply.5,6
However, few people start using opioids by experimenting with heroin or illicit fentanyl. About 80% of people who use heroin report starting with the use of prescription opioids.7 Understanding prescription opioid acquisition patterns is important to prevent potential addiction.
In response to the dramatic increase in overdose deaths, political leaders across the US have begun to work together in an effort to curb the epidemic.8 In Massachusetts, the legislature and Governor Baker established a new legislative mandate. Chapter 55 of the Acts of 2015, enacted in August 2015, mandated the analysis of data from several Massachusetts government agencies to identify and report on trends among persons who suffered a fatal opioid overdose. This was later expanded to also include non-fatal overdose. This novel and comprehensive linkage across datasets at the individual level allowed analysts to gain a deeper understanding of the circumstances that influenced fatal and non-fatal opioid overdoses. Through this work, public health and other policymakers were able to gain greater insight on the opioid epidemic, guide policy development and inform programmatic decisions.9
Potentially inappropriate opioid prescribing (PIP) describes specific opioid prescribing practices that could lead to adverse drug events and health complications.10–12 PIP has been studied for many drug classes in elderly populations, where risk for PIP is high, but less is known about the specific role of PIP in the Massachusetts opioid epidemic.9 Identifying opioid related PIP and determining what role PIP plays in opioid overdose is important to improving the safety of pain treatment. Little is known about the geographic distribution of PIP and opioid overdose.
In this study, we used geographic information systems (GIS) and spatial epidemiological analyses to characterize the geographic distribution of fatal opioid overdoses and PIP across Massachusetts. Our objectives were to create descriptive and hotspot cluster analysis maps to better understand the landscape of opioid epidemic outcomes and predictors to test the hypothesis that opioid overdoses and PIP cluster geospatially, and to assess potential overlap between overdose and PIP hotspots to inform public health and clinical responses.
Methods:
Dataset and measures.
Through Chapter 55 of the Acts of 2015, the Massachusetts Department of Public Health linked sixteen administrative datasets, including prescription monitoring program (PMP), medical claims, vital statistics, and medical examiner data. The study population was defined as Massachusetts residents ages 18 and above with at least one opioid prescription throughout the 5-year study period, 2011–2015 (n=3,143,817), with the exclusion of those who had late stage cancer diagnoses recorded in the State’s cancer registry. We conducted analyses elsewhere focused on the associations between PIP, overdose deaths, and all-cause mortality.13
PIP Definitions
We defined opioid PIP in Massachusetts based on six criteria, established through literature review and consultation with experts in the field: (1) ≥100 morphine milligram equivalents (MMEs) per day in at least three months, (2) receipt of opioid prescriptions in three consecutive months without ever recording a pain diagnosis in claims data, (3) three or more cash purchases of opioid prescriptions, (4) opioid prescriptions obtained at four or more distinct pharmacies in a quarter (5) opioid prescriptions obtained from four or more distinct prescribers in a quarter, and (6) co-prescription of benzodiazepines and opioids in at least three months.14 Initial database linkage, data cleaning, and variable creation were performed in SAS Studio (v3.5, Cary, NC).
Geographic Analysis:
We aggregated all PIP and overdose events at the ZIP code level and joined these data to a geographic shapefile for all ZIP code tabulation areas in Massachusetts (n=538). To ensure confidentiality in descriptive maps, we suppressed PIP data for ZIP codes with small numbers following Massachusetts Department of Public Health (MDPH) conventions. Missing or suppressed data can hinder cluster analyses because they disrupt geographic neighborhoods. To combat this issue for variables with suppressed data, we substituted the midpoint value for the suppression range for each ZIP code in cluster analysis. Final cluster analyses cannot be traced back to the individual, thus maintaining confidentially.
Descriptive Statistics.
In Table 1, we present summary statistics for PIP and fatal opioid overdose rates in Massachusetts. We highlight our outcome categorization scheme to provide definitions for low, average, and high rates to place our thematic map cut points in context (Table 1).
Table 1.
Percent of People with PIP Occurrences and Rates of Fatal Opioid Overdoses per 100,000 population in Massachusetts ZIP Codes, 2011–2015.
| Cut Points | Excessive MME Dosing | Opioid Rx and No Pain Diagnosis | Multiple Prescribers | Co-Prescription of Opioids and Benzodiazepines | Cash Payments for Opioid Rx | Multiple Pharmacies | Fatal Opioid Overdose Rates per 100,000 | |
|---|---|---|---|---|---|---|---|---|
| Q1: Very Low Rates | 0−1.68% | 0−1.90% | 0−2.35% | 0−4.73% | 0−4.90% | 0−0.49% | No Overdoses | 0 |
| Q2: Low Rates | 1.69−2.39% | 1.91−2.48% | 2.36−3.13% | 4.74−6.00% | 5.00−6.10% | 0.5−0.74% | Below the MA Rate | <10.4 |
| Q3: Average Rates | 2.4−3.14% | 2.49−3.05% | 3.14−4.03% | 6.01−7.45% | 6.20−7.50% | 0.75−1.01% | >MA and <US Rates | 10.4−15.4 |
| Q4: High Rates | 3.15−4.87% | 3.06−4.12% | 4.04−5.94% | 7.46−4−10.14% | 7.60−11% | 1.02−1.43% | >US and MA Rates | >15.4 |
| Q5: Very High Rates | 4.88−24% | 4.13−18.45% | 5.95−13.45% | 10.15−24% | 11.10−36.80% | 1.44−6.72% | -- | |
Abbreviations and Definitions: PIP=Potentially inappropriate opioid prescriptions; MME=Morphine milligram equivalents; Rx=Prescription; Q1-Q5=Quintile 1-Quintile 5 for PIP variables; MA=Massachusetts; US=United States; cut points for fatal opioid overdose are based on Massachusetts rates and US opioid overdose rates per 100,000.
Descriptive Mapping.
We developed descriptive GIS maps to portray PIP and overdose counts, and the percent of the study population (adult residents with an opioid prescription) who experienced PIP. When appropriate, we calculated rates of overdose and PIP variables per 100,000 residents using ZIP code level population counts in the denominator. In these instances, our denominator was the 5-year estimate of the average population of each ZIP code over the five years, which we multiplied by five to account for study duration, in order to calculate a person-year denominator. We obtained the population denominator data from the U.S. Census Bureau’s American Community Survey (ACS).15 We excluded ZIP codes with a 5-year population estimate < 50 to avoid skewing rate calculations. We developed a reference map of Massachusetts, highlighting the 14 counties and 351 municipalities across the state helping to situate subsequent overdose and PIP maps (Appendix 1). All descriptive maps were created using ArcGIS version 10.4.1 (Esri, Redlands, CA).
Spatial Cluster Analyses:
We conducted hotspot cluster analyses to identify statistically significant clusters of opioid overdose deaths and PIP, using a five-step geoprocessing approach employed previously to assess disease clustering and public health unmet needs.16,17 We conducted local indicators of spatial autocorrelation (LISA) analyses to corroborate our hotspot cluster analyses, and to identify outlier communities with regard to opioid overdose deaths.18 Our hotspot cluster and LISA analytical methods are described in greater detail in Appendix 2.
Results:
More than half of the adult population (n=3,143,817) in Massachusetts were prescribed opioids at least once between 2011 and 2015. In trend analyses, we found that the number of fatal opioid overdoses among Massachusetts residents who received an opioid prescription rose steeply and consistently during the study period, from 614 in 2011 to 1590 in 2015. Fatal opioid overdose rates in this population also rose steadily and significantly over the course of the study period, from 19.5 deaths per 100,000 in 2011 to 50.5 deaths per 100,000 in 2015 (p<0.05) (Appendix 3).
Overdose Deaths.
Nearly all ZIP codes showed increasing rates of overdose deaths between 2011–2015, many well above national and state average rates. In Figures 1a–1e, we present descriptive maps that depict annual fatal overdose rates from 2011 to 2015, and in Figure 1f we show aggregated overdose rates across the entire timeframe. We noted steady increases in overdose death rates across an increasing number of ZIP codes between 2011 and 2015. By 2015, we found that 51.3% of ZIP codes (n=276) had fatal overdose rates that surpassed the national opioid overdose rate of 10.4 deaths per 100,000 residents (Figure 1e).
Figure 1. Fatal opioid overdose rates per 100,000 Massachusetts residents, 2011–2015.
Rates are aggregated at the ZIP code level. Overdose rates are categorized with reference to state (15.4 deaths/ 100,000 residents) and national (10.4 deaths/ 100,000 residents) overdose rates. The lightest reds represent ZIP codes with fatal overdose rates lower than that national average, whereas the darkest red accounts for rates higher than the national and Massachusetts state average. Town/city boundaries are outlined in black. A) 2011; B) 2012; C) 2013; D) 2014; E) 2015; F) Aggregated/average annual fatal overdose rate per 100,000 Massachusetts residents, 2011–2015.
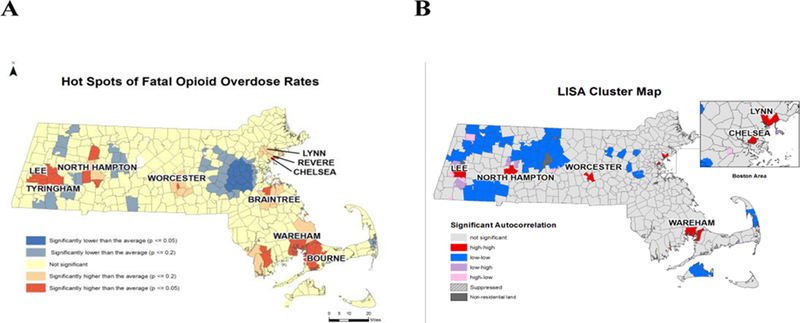
In Figure 2, we present results of our cluster analyses. We identified six statistically significant hotspot clusters for fatal overdose rates in the municipalities of Worcester, Northampton, Lee/Tyringham, Wareham/Bourne, Lynn, and Revere/Chelsea (p<0.05) (Figure 2). We identified communities that were spared from high overdose rates in Western Massachusetts and the Metro West area, to the west of Boston and East of Worcester, where we identified lower overdose rates (Figure 1) and the presence of overdose coldspots (p<0.05) relative to all other ZIP codes in the state (Figure 2). Hotspots and coldspots were defined as geographically contiguous regions of ZCTAs with statistically significant Getis-Ord statistics.
Figure 2. Clustering of fatal opioid overdose rates per 100,000 residents, by Massachusetts ZIP codes, 2011–2015.
A) Statistically significant clusters of opioid overdose rates. Red shading highlights significant clusters of ZIP codes with elevated overdose rates (p<0.5); orange shading highlights marginally significant clusters of ZIP codes with elevated overdose rates (p<0.2); yellow shading represents average opioid overdose rates; light blue highlights marginally significant clusters of ZIP codes with overdose rates that are lower than the state average (p<0.2); blue shading represents significant clustering of ZIP codes with lower overdose rates than the state average (p<0.05); B) Local Incremental Spatial Autocorrelation (LISA) cluster map highlighting ZIP codes with high fatal overdose rates per 100,000 population that are surrounded by neighboring ZIP codes with high overdose rates (red), ZIP codes with low overdose rates that are surrounded by neighboring ZIP codes with low overdose rates (blue), ZIP codes with high overdose rates that are adjacent to ZIP codes with low overdose rates (pink), and ZIP codes with low overdose rates that adjacent to neighboring ZIP codes with high overdose rates (p<0.05).
Potentially Inappropriate Prescribing (PIP).
We depict the spatial distribution of six subtypes of PIP across Massachusetts in Figure 3. In Figures 3a–3e, we noted initial patterns in the spatial distribution of PIP outcomes across Massachusetts, with lower percentages of people experiencing PIP in the Greater Boston area. The percentages of people experiencing PIP appeared to increase moving east to west across the state, as noted by darker shading, or entry into the upper quintiles for PIP rates.
Figure 3. Potentially inappropriate opioid prescription practices (PIP) in Massachusetts, 2011–2015.
A) Percent of people prescribed more than 100 morphine milligram equivalents per day for three or more months amongst those who received at least one opioid prescription, Massachusetts ZIP codes, 2011 −2015; B) percent of people with three consecutive months of opioid prescriptions without a pain diagnosis amongst those who received at least one opioid; C) percent of people with four or more prescribers per quarter amongst those who have received at least one opioid prescription; D) percent of people co-prescribed benzodiazepines and opioids for three or more months amongst those who received at least one opioid prescription; E) percent of people with an opioid prescription who have paid for a prescription with cash three or more times; F) percent of people with four or more pharmacies per quarter amongst those who received at least one opioid prescriptions.
In Figure 4, we present results from PIP hotspot analyses. We identified clusters for cash payments and co-prescription of opioids and benzodiazepines in North Adams, Lee, Blandford, Boxford, Martha’s Vineyard, and Nantucket (p<0.05). For multiple prescribers (i.e., “doctor shopping”), excessive MME dosing, and prescription without a documented pain diagnosis, we observed sizeable hotspot clusters in Western Massachusetts (p<0.05). Of note, we observed no clusters when analyzing the use of four or more pharmacies for opioid prescriptions.
Figure 4. Clustering of potentially inappropriate opioid prescription practices (PIP) in Massachusetts, 2011–2015.
a) Clustering of percent of people with an opioid prescription who have paid for opioid prescriptions three or more times with cash; b) clustering of percent of people with an opioid prescription and three months with a co-prescription of benzodiazepines and opioids; c) clustering of percent of people with an opioid prescription who received prescriptions from four or more prescribers per quarter; d) hotspots of rates of people with an opioid prescription for three months with an average daily MME > 100 mg; e) clustering of percent of people with a three consecutive months of opioid prescriptions and no pain diagnosis.
PIP and fatal opioid overdose clustering patterns were most similar when comparing cash payments for opioid prescriptions (Figure 4a), co-prescription of opioids and benzodiazepines (Figure 4b), and fatal overdoses (Figure 2). Cluster maps for all three of these outcomes portrayed hotspots in Cape Cod and Berkshire County.
Discussion:
Opioid prescriptions have been an increasing concern among public health officials during the past decade. GIS and spatial epidemiological analyses are an important tool to better understand opioid epidemic outcomes and risk factors. We employed a mix of descriptive GIS mapping techniques and spatial epidemiological analyses to better understand the geographic landscape of fatal opioid overdose deaths and PIP across the state of Massachusetts, using a novel comprehensively linked dataset that was created in response to a recent legislative mandate.9 Assessing the geographic distribution of opioid-related PIP can assist policymakers in identifying locations for targeted public health interventions.
Our findings provide a unique picture of the Massachusetts epidemic. A number of previous studies have presented maps of overdose in different parts of the US.5,19,20 Several studies have assessed PIP,10,11,21 and its associations with overdose deaths,14 but we are unaware of any that have juxtaposed opioid overdose deaths and PIP. Our study is one of the first to identify local geographic changes in overdose deaths over time during the recent acceleration of the opioid epidemic. Through our spatial cluster analyses, we have been able to pinpoint local areas of elevated concern, as well as areas of low risk relative to their surroundings.
We were able to map six PIP variables at the neighborhood level. Cash payments and opioid prescription without a documented pain diagnosis were two PIP subtypes that had not been examined by previous studies. We identified several PIP variables (multiple prescribers, excessive MME, opioid prescription with no pain diagnosis) that were characterized by systematic hotspot clustering in Western MA and coldspot clustering in Eastern MA, with exceptions in Boxford, Cape Cod, and its neighboring islands. While our descriptive maps highlighted the growing ubiquity of opioid overdose deaths across the state, we identified fatal overdose clusters in urban (Boston metro, Worcester, Fall River, New Bedford), suburban (Bourne, Wareham, Northampton), and rural locations of the state (Lee, Tyringham). We identified similar clustering patterns for fatal opioid overdoses and two PIP variables—cash payments for opioid prescriptions and co-prescription of opioids and benzodiazepines. However, the relationship between other PIP variable clusters and overdose clusters was not consistent throughout the state. This emphasizes the point that PIP is only one factor of many that may explain the geospatial variation in overdose rates across the state. Focusing on PIP alone from a geospatial perspective is not enough to inform all targeted overdose prevention interventions. Recent studies focused on Eastern Massachusetts found that the proportion of opioid overdose deaths attributed to fentanyl increased from 32% during 2013–2014 to 74% during early 2016,22 and that fentanyl was easily accessible at low cost.23 In other recent studies, we found that older adults were more likely to be exposed to PIP,24 and that younger adults were less likely to experience PIP prior to opioid overdose death,25 which may also contribute to differential spatial distributions of PIP and overdose clusters. In areas where fentanyl is prevalent in the drug supply, or where effective interventions have been implemented, geospatial PIP indicators may play a limited or more nuanced role in the geographic distribution of fatal opioid overdoses. Recent research also points to the “triple wave” theory to describe the opioid overdose crisis in the U.S.26 In testimony before the U.S. House of Representatives, Ciccarone described the three waves of the overdose epidemic, including: 1) the rise in opioid prescriptions (within which PIP is situated); 2) a “tightening” of opioid prescribing habits, resulting in less access to prescription opioids concurrent with an increase in heroin use and misuse;27 and, 3) the entry of fentanyl into opioid markets.26 The three waves of overdoses from prescription opioids to heroin to fentanyl build off of one another and they interact in complex ways, while social and economic factors may also come into play.28 The triple wave theory may help to explain the paradoxical relationship between PIP hotspots and overdose hotspots, where overdose clusters are driven largely by the entry of fentanyl into the drug market beginning in 2013.
In our LISA maps, in addition to identifying clusters, we were able to locate outliers— communities with high overdose rates surrounded by communities with low overdose rates, and communities with lower overdose rates surrounded by communities with higher overdose rates. Municipalities that are outliers on either extreme are worthy of further investigation to determine why they are different from their neighbors. Several ZIP codes surrounding Northampton, Lee, and in the northwest corner of Massachusetts appear as such outliers. In Northampton, formidable harm reduction programs may have helped to curb overdose deaths in some ZIP codes, despite high overdose rates in neighboring ZIP codes. Local and state departments of public health, as well as researchers, may be able to use this information to identify places in need of a greater response, and places to be studied for their successes in buffering the effects of the opioid epidemic.
Maps move the dial through their power as communication devices. It is, at times, easier for lay audiences to understand and engage when examining a map that visualizes a statistic rather than presenting statistics in tabular form. This is beneficial for two reasons. First, the information can reach a broader audience, increasing awareness of the problem and its contributing factors. Second, the visual aspect of maps facilitates discussion about next steps, leads to new questions from community members and stakeholders, and can help generate hypotheses for researchers. Maps that depict the geospatial landscape with regard to PIP risks and fatal overdose, for instance, allow community members to observe high risk activities and outcomes that impact their neighborhoods and families, which can spawn local organizing and policy actions. In a comprehensive approach, PIP maps can, in part, provide policymakers with findings that can facilitate targeted feedback and education to prescribers and pharmacists in areas identified as PIP hotspots. However, it is important to bear in mind that single policy efforts (e.g., opioid prescription reform) can have paradoxical effects if the intertwined aspects of the triple wave of opioid overdose deaths are not fully recognized, understood, or intervened upon in a comprehensive fashion. Thus, spatial epidemiological and statistical models that look at PIP (Wave 1), heroin (Wave 2), and fentanyl-related overdoses (Wave 3) in unison may provide the best opportunity to inform multifaceted responses that address the triple threat.
Our findings should be considered in light of several limitations. First, in reference to data, access to the Chapter 55 dataset allowed us to conduct analyses at the ZIP code level—a level of granularity not previously analyzed in Massachusetts. Although census tract level data would be preferable in terms of increased granularity, Chapter 55 stipulations prevented us from accessing data below the ZIP code level. Second, ZIP code boundaries vary over time with changing Postal Service distribution routes.29 We utilized ZIP code tabulation areas (ZCTAs) in our geographic analysis to control for this change over time. ZCTAs are calculated using census data and thus their boundaries only change every 10 years. However, because of the different methods by which the two boundaries are calculated, there are some instances when ZIP Codes are not represented by ZCTAs and data may not be included in the geospatial analysis.30 It is important to note that rates of opioid prescribing are calculated using ZIP Code level values in the numerator and ZCTA population values in the denominator, which may cause some slight mismatch. Third, it is possible that some deaths were misclassified and not considered opioid-related overdoses if they were not referred to the medical examiner for a final cause of death determination.31 It is probable, however, that potential misclassifications are non-differential across ZIP Codes in the state. Finally, the Chapter 55 Act and subsequent access to this linked data remains unique to Massachusetts. Results may not be generalizable to other states in the US. Future research that employs GIS and spatial analytical approaches from the current study should be replicated elsewhere with similarly linked data to compare results.
In future research we plan to identify geographic areas in greatest need of public health intervention with regard to overall opioid burden based on composite measures, as well as need for increased access to services (e.g., naloxone distribution, substance use treatment programs, medications for opioid use disorder, harm reduction programs, syringe services programs, pharmacies, prison release and re-entry programs). Additional data could strengthen these analyses, including spatially oriented data on overdose deaths by drug type (e.g., heroin, fentanyl, prescription opioids), PIP practices stratified by age,24 pharmaceutical marketing practices, proxies for illicit drug availability (e.g., arrests and drug seizures), and prevention/intervention capacity (e.g., naloxone utilization, proximity to emergency medical services, treatment or diversion services) to observe potential spatial associations with overdose. We intend to conduct this research through the development of statistical models to assess factors associated with overdose and other key outcomes to identify additional touchpoints for intervention.
Further research to develop predictive spatial and statistical analytical techniques (e.g., geographically weighted regression models; Bayesian spatiotemporal modeling) is needed to assess opioid epidemic burden and access to services that could facilitate the prediction of future hotspots and target future public health interventions. Future research should also explore different imputation methods for suppressed data to better understand its effect on hotspot analysis. Continued partnership with academic institutions, public health officials, and governments will aid in combating the opioid crisis in Massachusetts, the US, and globally.
Conclusion:
We used GIS mapping and spatial epidemiological analyses to pinpoint opioid overdose and PIP clusters between 2011 and 2015 using first of its kind comprehensively linked administrative data. We identified fatal overdose and PIP hotspots, as well as regions where the two overlapped, and where they diverged. Our results can inform public health policy decisions that include a focus on PIP and other components of the “triple wave” theory that aim to curb opioid overdose deaths.
Supplementary Material
Acknowledgments:
Conflicts of Interest Statements/Funding Sources:
Thomas Stopka received funding support from the GE Foundation (No: 33924399; PI: Stopka) and the National Institutes of Health, Clinical and Translational Science Award (UL1TR001064).
Harsha Amaravadi received funding support from the GE Foundation (No: 33924399).
Anna Kaplan received funding support from the GE Foundation (No: 33924399).
Rachel Hoh received funding support from the GE Foundation (No: 33924399).
Dana Bernson received funding support from the Massachusetts Department of Public Health.
Kenneth Chui received funding support from the GE Foundation (No: 33924399).
Thomas Land received funding support from the Massachusetts Department of Public Health.
Alexander Walley received funding support from the Massachusetts Department of Public Health.
Marc LaRochelle received funding support from the National Institute on Drug Abuse (NIDA K23 DA042168).
Adam Rose received funding support from the GE Foundation (No: 33924399).
The funder did not have any role in study design; collection, analysis, and interpretation of data; writing the report; and the decision to submit the report for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Publisher's Disclaimer: Disclaimer: The opinions expressed in this manuscript are those of the authors and do not represent the official views or policies of the study sponsor (The GE Foundation) nor the Massachusetts Department of Public Health or the Commonwealth of Massachusetts.
Preliminary findings from this study were presented at the 2017 annual meeting of the American Public Health Association, and to the Massachusetts Department of Public Health.
Financial Disclosures:
Thomas Stopka has no financial disclosures.
Harsha Amaravadi has no financial disclosures.
Anna Kaplan has no financial disclosures.
Rachel Hoh has no financial disclosures.
Dana Bernson has no financial disclosures.
Kenneth Chui has no financial disclosures.
Thomas Land has no financial disclosures.
Marc LaRochelle has no financial disclosures.
Alex Walley has no financial disclosures.
Adam Rose has no financial disclosures.
References
- 1.Sun EC, Dixit A, Humphreys K, Darnall BD, Baker LC, Mackey S. Association between concurrent use of prescription opioids and benzodiazepines and overdose: retrospective analysis. BMJ 2017;356:j760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rudd RA, Seth P, David F, Scholl L. Increases in Drug and Opioid-Involved Overdose Deaths - United States, 2010–2015. MMWR Morb Mortal Wkly Rep 2016;65(5051):1445–1452. [DOI] [PubMed] [Google Scholar]
- 3.MDPH. Current Statistics: Stop Addiction in its Tracks In: Services HaH, ed 2017. [Google Scholar]
- 4.MDPH. Number of Opioid-Related Deaths. All Intents by City and Town http://www.mass.gov/eohhs/docs/dph/stop-addiction/current-statistics/town-by-town-listings-may-2017.pdf In:2017.
- 5.Marshall BDL, Krieger MS, Yedinak JL, et al. Epidemiology of fentanyl-involved drug overdose deaths: A geospatial retrospective study in Rhode Island, USA. Int J Drug Policy 2017;46:130–135. [DOI] [PubMed] [Google Scholar]
- 6.Gladden RM, Martinez P, Seth P. Fentanyl Law Enforcement Submissions and Increases in Synthetic Opioid-Involved Overdose Deaths - 27 States, 2013–2014. MMWR Morb Mortal Wkly Rep 2016;65(33):837–843. [DOI] [PubMed] [Google Scholar]
- 7.Jones CM. Heroin use and heroin use risk behaviors among nonmedical users of prescription opioid pain relievers - United States, 2002–2004 and 2008–2010. Drug Alcohol Depend 2013;132(1–2):95–100. [DOI] [PubMed] [Google Scholar]
- 8.NGA. A Compact to Fight Opioid Addiction https://www.nga.org/news/a-compact-to-fight-opioid-addiction. Accessed November 25, 2018.
- 9.MDPH. An Assessment of Fatal and Non-Fatal Opioid Overdoses in Massachusetts (2011–2015) http://www.mass.gov/eohhs/docs/dph/stop-addiction/legislative-report-chapter-55-aug-2017.pdf In:2017.
- 10.Clyne B, Bradley MC, Hughes CM, et al. Addressing potentially inappropriate prescribing in older patients: development and pilot study of an intervention in primary care (the OPTI-SCRIPT study). BMC Health Serv Res 2013;13:307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rochon PA, Lane CJ, Bronskill SE, et al. Potentially inappropriate prescribing in Canada relative to the US. Drugs Aging 2004;21(14):939–947. [DOI] [PubMed] [Google Scholar]
- 12.Logan J, Liu Y, Paulozzi L, Zhang K, Jones C. Opioid prescribing in emergency departments: the prevalence of potentially inappropriate prescribing and misuse. Med Care 2013;51(8):646–653. [DOI] [PubMed] [Google Scholar]
- 13.Rose AJ, Bernson D, Chui KKH, et al. Potentially Inappropriate Opioid Prescribing, Overdose, and Mortality in Massachusetts, 2011–2015. J Gen Intern Med 2018. [DOI] [PMC free article] [PubMed]
- 14.Rose AJ, Bernson D, Chui KKH, et al. Potentially Inappropriate Opioid Prescribing, Overdose, and Mortality in Massachusetts, 2011–2015. J Gen Intern Med 2018;33(9):1512–1519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.United States Census Bureau. American FactFinder Available at: http://factfinder.census.gov. Accessed: August 3, 2011 Accessed.
- 16.Meyers DJ, Hood ME, Stopka TJ. HIV and Hepatitis C Mortality in Massachusetts, 2002–2011: Spatial Cluster and Trend Analysis of HIV and HCV Using Multiple Cause of Death. PLoS One 2014;9(12):e114822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stopka TJ, Krawczyk C, Gradziel P, Geraghty EM. Use of spatial epidemiology and hot spot analysis to target women eligible for prenatal women, infants, and children services. Am J Public Health 2014;104 Suppl 1:S183–189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Anselin L Local Indicators of Spatial Association - LISA. Geographical Analysis 1995;27(2):93–115. [Google Scholar]
- 19.Marshall BDL, Yedinak JL, Goyer J, Green TC, Koziol JA, Alexander-Scott N. Development of a Statewide, Publicly Accessible Drug Overdose Surveillance and Information System. Am J Public Health 2017:e1–e4. [DOI] [PMC free article] [PubMed]
- 20.Cerdá M, Gaidus A, Keyes KM, et al. Prescription opioid poisoning across urban and rural areas: identifying vulnerable groups and geographic areas. Addiction 2017;112(1):103–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bohnert AS, Valenstein M, Bair MJ, et al. Association between opioid prescribing patterns and opioid overdose-related deaths. JAMA 2011;305(13):1315–1321. [DOI] [PubMed] [Google Scholar]
- 22.Somerville NJ, O’Donnell J, Gladden RM, et al. Characteristics of Fentanyl Overdose - Massachusetts, 2014–2016. MMWR Morb Mortal Wkly Rep 2017;66(14):382–386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ciccarone D, Ondocsin J, Mars SG. Heroin uncertainties: Exploring users’ perceptions of fentanyl-adulterated and -substituted ‘heroin’. Int J Drug Policy 2017;46:146–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rose AJ, McBain R, Schuler MS, et al. Effect of Age on Opioid Prescribing, Overdose, and Mortality in Massachusetts, 2011 to 2015. J Am Geriatr Soc 2018. [DOI] [PMC free article] [PubMed]
- 25.Larochelle M, Bernson D, Land T, et al. Touchpoints to identify individuals at high risk for opioid overdose death. College on Problems of Drug Dependence (CPDD) 80th Annual Scientific Meeting; June 14, 2018; San Diego, CA. [Google Scholar]
- 26.Ciccarone D The Triple Wave Epidemic: Opioids, Heroin, and Fentanyl: Supply Issues and Public Health Consequences. Testimony Before the Committee on Foreign Affairs, Subcommittee on Africa, Global Health, Global Human Rights, and International Organizations, United States House of Representatives. Hearing: Tackling Fentanyl: The China Connection September 6, 2018. Accessed on: December 31, 2018 Available at: https://docs.house.gov/meetings/FA/FA16/20180906/108650/HHRG-115-FA16-Wstate-CiccaroneD-20180906-U2.pdf.
- 27.Kolodny A, Courtwright DT, Hwang CS, et al. The prescription opioid and heroin crisis: a public health approach to an epidemic of addiction. Annu Rev Public Health 2015;36:559–574. [DOI] [PubMed] [Google Scholar]
- 28.Dasgupta N, Beletsky L, Ciccarone D. Opioid Crisis: No Easy Fix to Its Social and Economic Determinants. Am J Public Health 2018;108(2):182–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhu L, Waller LA, Ma J. Spatial-temporal disease mapping of illicit drug abuse or dependence in the presence of misaligned ZIP codes. GeoJournal 2013;78(3):463–474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Grubesic TH, Matisziw TC. On the use of ZIP codes and ZIP code tabulation areas (ZCTAs) for the spatial analysis of epidemiological data. Int J Health Geogr 2006;5:58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rockett IR, Hobbs GR, Wu D, et al. Correction: Variable Classification of Drug-Intoxication Suicides across US States: A Partial Artifact of Forensics? PLoS One 2015;10(9):e0137933. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.