Abstract.
Long-lasting insecticide-treated bednets are widely used and promoted for malaria control. Limitations in measurement methods have resulted in a poor understanding of how bednets are used in practice. We deployed a novel remote monitoring tool in Uganda to obtain, for the first time, a comprehensive characterization of bednet use in households at risk for malaria. Ten households each used one SmartNet adherence monitor over a commonly used sleeping area for 6 weeks. SmartNet continuously measures and records bednet use every 15 minutes. Bednet use was monitored for a total of 9,258 hours overall, with an average of 42 nights per household (SD: 3.5). Average duration of bednet use was 9 hours 49 minutes per night (SD: 1 hour 56 minutes), and adherence was 85–90% from 2100 to 0600. Bednets were not used at all on 4.5% (19/418) of observation nights. Overall, the average clock time that bednets were unfurled was 2034 (SD: 1 hour 25 minutes) and they were folded up at 0743 (SD: 43 minutes). The rate of interruptions per night observed in all households was 0.23 (86/369), with an average duration of 48 minutes (SD: 49 minutes). There was substantial heterogeneity between households, and some households had consistently poorer adherence relative to others. Variations in bednet use behaviors are a potentially important, and under-researched, component of long-lasting insecticide-treated bednet effectiveness. Remote bednet use monitors can provide novel insights into how bednets are used in practice, helping identify both households at risk of malaria due to poor adherence and also potentially novel targets for improving malaria prevention.
INTRODUCTION
Malaria is a serious health concern throughout the world, with an estimated 219 million cases and 435,000 deaths in 2017.1 Long-lasting insecticide-treated bednets (LLINs) have been a fundamental component of malaria prevention for almost 30 years.2,3 Since 2007, the WHO has recommended that every person at risk of malaria, 3.4 billion people worldwide, has access to an LLIN.4 Long-lasting insecticide-treated bednets accounted for an estimated 68% of the 40% reduction in malaria incidence between 2000 and 2015.5 Long-lasting insecticide-treated bednets are widely available and well understood by most people as an important tool for protection against malaria.
Recent studies suggest, however, that LLINs may no longer be as effective as previously thought.6–8 It is not clear why there is a change in the apparent effectiveness of LLINs. Leading explanations include changes in vector species prevalence or biting behaviors (e.g., earlier in the night),9,10 the development of insecticide resistance,11,12 or poor net durability.13 It is also possible that people are not using LLINs as frequently as reported.14,15 Addressing questions about the effectiveness of this widely used tool is particularly important, given recent evidence that progress in malaria control has stalled.1
Accurately measuring how bednets are used is a crucial first step in studying LLIN effectiveness, but measuring actual use is challenging. The most commonly used measure—self-reported bednet use the prior night—may be prone to social desirability and other biases, resulting in potentially inaccurate conclusions when characterizing bednet use.15 Other methods, such as surprise night visits, suffer from privacy and logistical issues. Furthermore, all current methods suffer from imprecision, as they are unable to capture temporal variations in hourly, nightly, or seasonal bednet use.16 These measurement challenges contribute to a lack of understanding about how bednets are used in practice. This may, in turn, lead to missed opportunities in public health campaigns seeking to promote bednet use and limit quality evidence available to inform evaluations of the role bednets should play in malaria prevention more broadly.
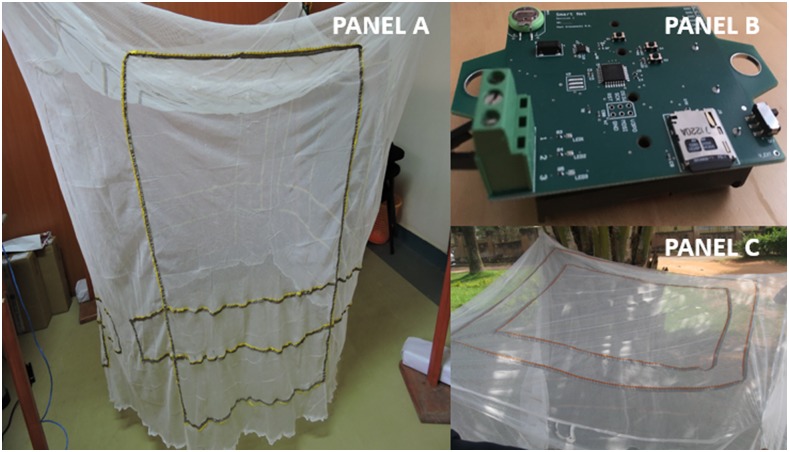
SmartNet is a novel electronic monitoring device designed to provide continuous, accurate, and objective measurements of bednet use. SmartNet uses conductive fabric sewn into a standard WHO-approved LLIN to form three electrical circuits, two on the sides and one on the top (Figure 1A and B). A microcontroller sends a current through the conductive fabric using insulated wires (Figure 1C). When the SmartNet is unfurled, and therefore considered in use, none of the conductive fabric touches any other and no circuit is detected. Alternatively, when the SmartNet is folded up or knotted during the day, the conductive fabric patterns come into contact and complete an electrical circuit which SmartNet defines as not in use. The time-stamped data are stored on a memory card for later retrieval. Laboratory tests show that SmartNet is > 98% accurate in determining whether the SmartNet is unfurled or folded up, and achieves 8 weeks of monitoring with 2 AA batteries logging at 15-minute intervals. SmartNet has been successfully deployed in feasibility trials in the United States and an acceptability study in Uganda.17,18
Figure 1.
SmartNet components: (A) Slide view of unfurled SmartNet; (B) SmartNet battery-powered microcontroller; (C) Top view of SmartNet. This figure appears in color at www.ajtmh.org.
In this study, we deployed SmartNet in 10 households for 6 weeks in western Uganda to obtain first-of-its-kind data, characterizing the use of bednets in actual practice. The overarching goal of this descriptive study was to explore how more precise and granular data on bednet use could contribute to answering important questions about LLIN effectiveness and inform the design of improved interventions to prevent malaria with this important public health tool.
MATERIALS AND METHODS
Ten households were recruited from the Kinoni Health Centre IV in Mbarara district, western Uganda. Women who had at least one child or who were pregnant were invited to participate. Women who elected to participate were visited in their homes for study consent and to install the SmartNet. At the initial home visit, following the consent process, demographic data were gathered about the household and one SmartNet was installed above a commonly used sleeping area. Households were requested to use the SmartNet bednet just as they would use a regular bednet/LLIN. Study personnel visited the household weekly for the first 4 weeks to gather SmartNet data and perform acceptability and adherence surveys. After an additional 2 weeks (6th week), study personnel performed a final survey, removed the SmartNet, and provided a new, standard, LLIN to the household. At each household visit, the SmartNet data were extracted from the embedded memory cards and compiled into a data set for later analysis.
We present demographic data and household characteristics such as main household occupation, number of rooms and bednets, ratio of occupants to bednets, and participant’s report of who used the SmartNet most frequently. SmartNet measures the state of the bednet at 15-minute intervals. We calculated the average duration of use by converting the average number of 15-minute intervals of use into minutes and subdividing this into hours and minutes. We present average SmartNet use during each hour and, separately, during 3-hour intervals from 1800 to 0900 by averaging the proportion of observations when the SmartNet was unfurled at each hour. We count nights during which the SmartNet was folded up (i.e., missed night of use) and unfurled for the entirety of 1800–0900. We report the average clock time that households unfurl the SmartNet at night and fold it up in the morning. We assume 0900 to be the time the bednet is folded up if it is not yet folded up. We report the number of interruptions, defined as folding up the SmartNet before definitively folding it up in the morning, and the average duration of interruptions per night in hours and minutes, following the conversion described earlier. To avoid the possibility that extremes (e.g., night with only 1 hour of use) might skew the data on regular use behaviors, both the analysis of the clock time that SmartNets are in use and the analysis of interruptions in use were restricted to nights with at least 4 cumulative hours of use between 1800 and 0900 (369/418).
All analyses were performed using Stata 14 (StataCorp. 2015. Stata Statistical Software: Release 14. College Station, TX: StataCorp LP.). Consent for the installation of SmartNet was obtained from the recruited mothers on behalf of the household. Study procedures were approved by Institutional Review Boards at the Mbarara University of Science and Technology in Uganda and Partners Healthcare in the United States. Additional approval was granted by the Uganda National Council for Science and Technology.
RESULTS
The 10 households had an average of 4.9 members (SD: 1.8; range: 3–8), 1.3 children younger than 5 years (SD: 0.5; range: 1–2), and 4 of the 10 households (40%) had one pregnant woman each. Households owned 2.5 bednets (SD: 0.8), with a ratio of occupants per bednet of 2.0 (SD: 0.3). Most bednets were obtained, presumably for free, through government distribution (15/25) or the health center (7/25). Six households reported that the SmartNet was used by one child and one adult. In 2 households, the SmartNet was used only by children (1 and 3), and in the remaining two households only by adults (2 and 7). (Table 1)
Table 1.
Demographic and bednet characteristics of 10 households in SmartNet pilot study
| Household members | Children younger than five years | Pregnant women | Mother’s education | Main income activity | Distance from health center (km) | Number of rooms | Number of bednets | Ratio of members/bednets | Source of bednet | Reported users of SmartNet | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Government distribution | Health center | Shop | |||||||||||
| Overall, mean (SD) | 4.9 (1.75) | 1.3 (0.5) | 0.4 (0.48) | – | – | 0.86 (0.12) | 2.2 (0.7) | 2.5 (0.8) | 1.95 (0.26) | 1.5 (1.2) | 0.7 (1.26) | 0.3 (0.45) | – |
| By household | |||||||||||||
| 1 | 4 | 2 | 0 | University | Banana farming | 1.8 | 2 | 2 | 2.0 | 2 | 0 | 0 | 1 child younger than 5 years |
| 2 | 8 | 1 | 1 | Primary | Trade | 0.2 | 3 | 4 | 2.0 | 0 | 4 | 0 | 2 adults (1 pregnant) |
| 3 | 8 | 1 | 0 | Primary | Farming | 1.7 | 3 | 4 | 2.0 | 4 | 0 | 0 | 2 children (1 younger than 5 years) |
| 4 | 4 | 1 | 1 | Primary | Farming | 1.7 | 1 | 2 | 2.0 | 1 | 0 | 1 | 1 adult + 1 child younger than 5 years |
| 5 | 4 | 2 | 0 | Primary | Butchery | 1.2 | 3 | 2 | 2.0 | 0 | 2 | 0 | 1 adult + 1 child younger than 5 years |
| 6 | 3 | 1 | 0 | University | Salary | 0.6 | 2 | 2 | 1.5 | 1 | 0 | 1 | 1 adult + 1 child younger than 5 years |
| 7 | 4 | 1 | 1 | Primary | Banana farming | 0.2 | 1 | 2 | 2.0 | 1 | 0 | 1 | 1 pregnant woman |
| 8 | 5 | 2 | 0 | Primary | Coffee growing | 0.5 | 2 | 2 | 2.5 | 1 | 1 | 0 | 1 adult + 1 child younger than 5 years |
| 9 | 3 | 1 | 0 | Primary | Farming | 0.4 | 2 | 2 | 1.5 | 2 | 0 | 0 | 1 adult + 1 child younger than 5 years |
| 10 | 6 | 1 | 1 | Primary | Farming | 0.5 | 3 | 3 | 2.0 | 3 | 0 | 0 | 1 adult + 1 child younger than 5 |
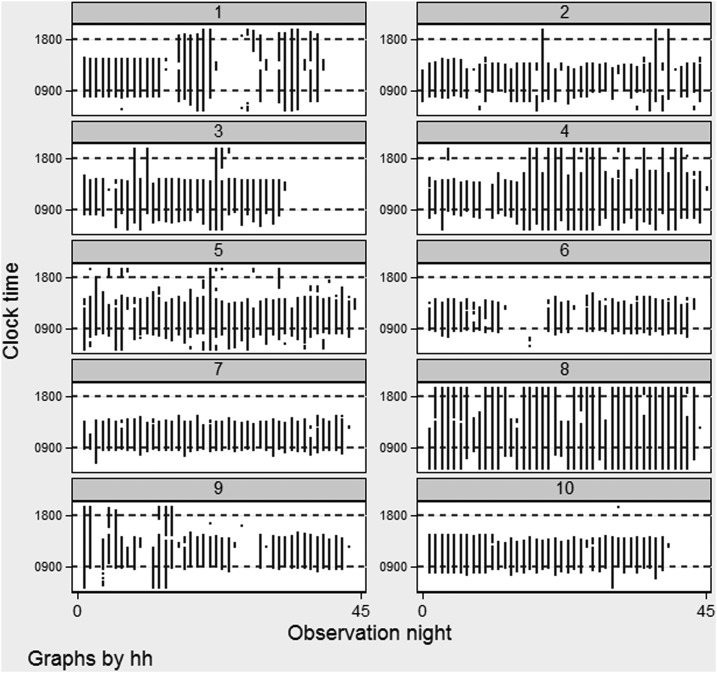
SmartNets were installed for an average of 42 nights (SD: 3.5; range: 33–45), and logged data for a total of 9,258 hours with an average of 925.8 hours per household (SD: 102.4; range: 742–1,024). An aggregate of the SmartNet records for each household over the observation period is displayed in Figure 2. From 1800 to 0900, the overall average duration of use was 9 hours 45 minutes (SD: 1 hour 56 minutes), ranging from 7 hours 6 minutes in household 6 to 13 hour 30 minutes in household 8. The average duration of use on nights with at least 4 hours total use (88.3% [360/418]) was 10 hours 59 minutes (SD: 1 hour 42 minutes) (Table 2).
Figure 2.
Household SmartNet use by night of observation.
Table 2.
Duration of SmartNet use
| All monitoring (n = 418) | Nights with ≥ 4 hours use (n = 369/418) | |
|---|---|---|
| Overall, mean (SD) | 9 hours 49 minutes (1 hour 56 minutes) | 10 hours 59 minutes (1 hour 42 minutes) |
| By household | ||
| 1 | 8 hours 45 minutes | 12 hours 39 minutes |
| 2 | 8 hours 51 minutes | 9 hours 54 minutes |
| 3 | 10 hours 51 minutes | 11 hours 29 minutes |
| 4 | 12 hours 20 minutes | 12 hours 54 minutes |
| 5 | 10 hours 52 minutes | 11 hours 14 minutes |
| 6 | 7 hours 6 minutes | 9 hours 7 minutes |
| 7 | 8 hours 34min | 8 hours 46 minutes |
| 8 | 13 hours 30 minutes | 13 hours 49 minutes |
| 9 | 7 hours 46 minutes | 9 hours 57 minutes |
| 10 | 9 hours 35 minutes | 10 hours 1 minute |
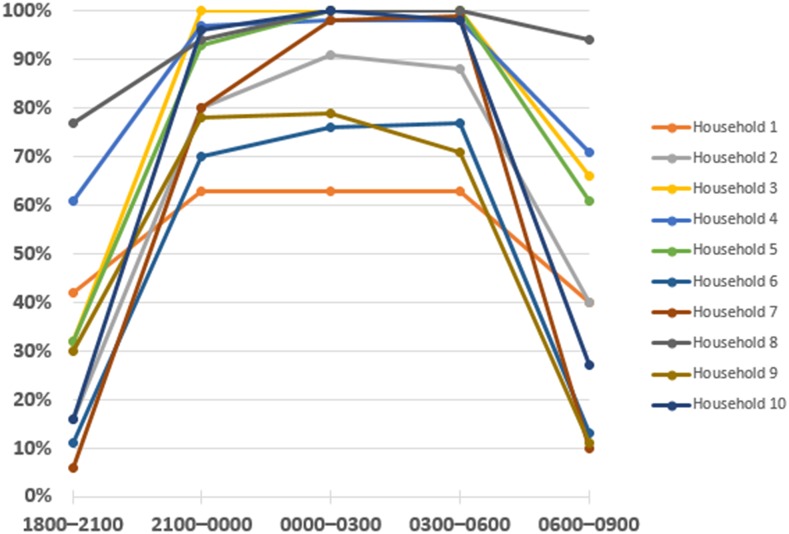
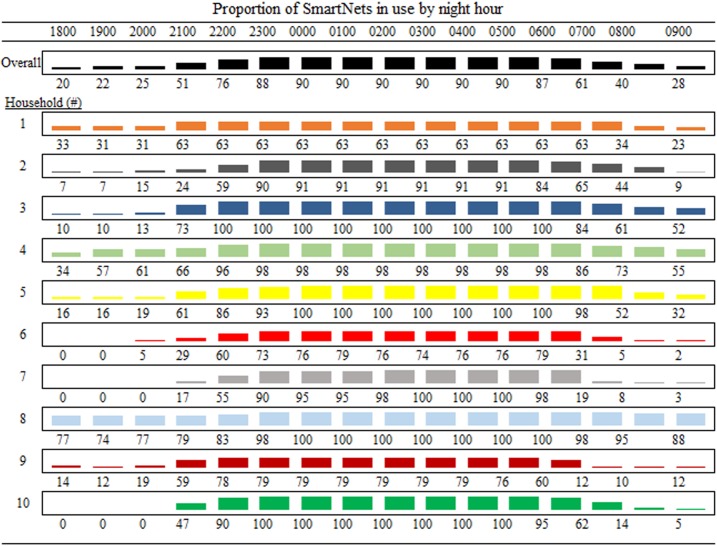
The peak proportion of SmartNet use was 90% during the late night (0000–0300), but use was similarly high in middle night (2100–0000) and early morning (0300–0600), with 85% and 89%, respectively (Table 3). Adherence during 3-hour intervals for each household are plotted together in Figure 3. There was substantial heterogeneity in use patterns between households. Household 8, for example, demonstrated high adherence beginning early in the night, whereas households 3, 7, and 10 unfurled their nets later, but still reached 95–100% adherence during 0000–0600 (Figure 4).
Table 3.
Proportion of SmartNets in use by select night hour intervals
| Whole night (1800–0900) | 1800–2100 | 2100–0000 | 0000–0300 | 0300–0600 | 0600–0900 | |
|---|---|---|---|---|---|---|
| Overall (%) | 65 | 33 | 85 | 90 | 89 | 43 |
| Household | ||||||
| 1 | 53% | 42% | 63% | 63% | 63% | 40% |
| 2 | 59% | 16% | 80% | 91% | 88% | 40% |
| 3 | 75% | 32% | 100% | 100% | 100% | 66% |
| 4 | 82% | 61% | 97% | 98% | 98% | 71% |
| 5 | 73% | 32% | 93% | 100% | 100% | 61% |
| 6 | 46% | 11% | 70% | 76% | 77% | 13% |
| 7 | 55% | 6% | 80% | 98% | 99% | 10% |
| 8 | 92% | 77% | 94% | 100% | 100% | 94% |
| 9 | 51% | 30% | 78% | 79% | 71% | 11% |
| 10 | 63% | 16% | 96% | 100% | 98% | 27% |
Figure 3.
Proportion of SmartNets in use by night intervals. This figure appears in color at www.ajtmh.org.
Figure 4.
Proportion of SmartNets in use by night hour. This figure appears in color at www.ajtmh.org.
Of a total of 418 nights of monitoring, the SmartNets were unused on 4.5% (19/418) of nights between 1800 and 0900. Missed nights were confined to households 1, 6, 9, and 4 who had 7, 6, 5, and one missed nights, respectively. SmartNets were unfurled continuously from 1800 to 0900 on 9.1% (38/418) of nights, led by household 8 that kept its SmartNet unfurled continuously on 18 nights (41% of total nights) (Table 4).
Table 4.
Nights from 1800–0900 with missed or continuous SmartNet use
| Missed nights of use | Continuous use | |
|---|---|---|
| Overall, % (n) | 4.6% (19/418) | 9.1% (38/418) |
| By household, % (n) | ||
| 1 | 18% (7/39) | 18% (7/39) |
| 2 | 0% (0/45) | 2% (1/45) |
| 3 | 0% (0/33) | 3% (1/33) |
| 4 | 2% (1/45) | 20% (9/45) |
| 5 | 0% (0/44) | 2% (1/44) |
| 6 | 14% (6/43) | 0% (0/43) |
| 7 | 0% (0/43) | 0% (0/43) |
| 8 | 0% (0/44) | 41% (18/44) |
| 9 | 12% (5/43) | 2% (1/43) |
| 10 | 0% (0/39) | 0% (0/39) |
Overall, the SmartNet was unfurled at an average time of 2034 (SD: 1 hour 25 minutes) and folded up in the morning at 0743 (43 minutes). Households 2 and 7 put their SmartNet down relatively late, at an average time of 2152 and 2146, respectively, compared with households 1, 4, and 8 who put theirs down earlier between 1847 and 1927 (Table 5).
Table 5.
Average clock time SmartNet unfurled and folded up*
| Time unfurled at night | Time folded up in morning | |
|---|---|---|
| Overall, mean (SD) | 20:34 (1 hour 25 minutes) | 07:43 (0 hour 43 minutes) |
| By household, % (n) | ||
| 1 | 19:14 (0 hour 59 minutes) | 08:14 (0 hour 13 minutes) |
| 2 | 21:46 (1hour 14 minutes) | 07:43 (0 hour 46 minutes) |
| 3 | 20:43 (0 hour 34 minutes) | 08:10 (0 hour 31 minutes) |
| 4 | 19:27 (1 hour 15 minutes) | 08:19 (0 hour 26 minutes) |
| 5 | 20:35 (1 hour 18 minutes) | 08:06 (0 hour 21 minutes) |
| 6 | 21:24 (0 hour 37 minutes) | 07:03 (0 hour 19 minutes) |
| 7 | 21:52 (0 hour 42 minutes) | 06:49 (0 hour 23 minutes) |
| 8 | 18:47 (1 hour 18 minutes) | 08:40 (0 hour 3minutes) |
| 9 | 20:29 (1 hour 13 minutes) | 06:38 (0 hour 38 minutes) |
| 10 | 21:13 (0 hour 23 minutes) | 07:18 (0 hour 30 minutes) |
* Restricted to nights with at least four total hours use between 1800 and 0900.
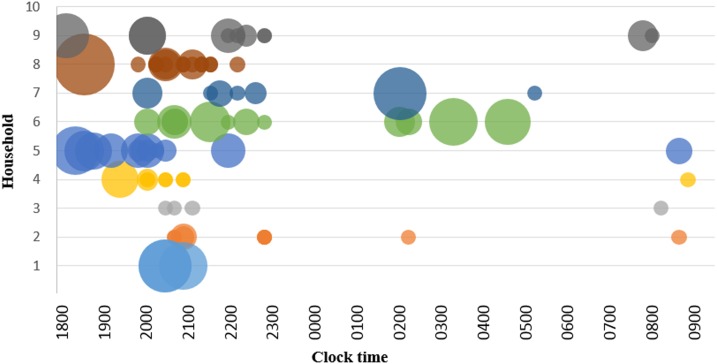
The analysis of interruptions in SmartNet use was restricted to nights with at least 4 hours of use. Over 369 nights, we detected a total of 86 interruptions for a nightly rate of 0.23 interruptions per night, with an average duration of 48 minutes (SD: 49 minutes). Figure 5 depicts all interruptions over the night, with the bubble size proportional to the duration. Household 10 had zero interruptions detected, whereas Households, 8, and 9 had significantly higher rates of interruptions. Despite a rate of only 0.12 interruptions per night (3/26), household 1 tended to have prolonged interruptions (2 hour 50 minutes; SD: 14 minutes). Meanwhile, household 8 had shorter average interruptions of 37 minutes (SD: 54 minutes), but had a more frequent rate of 0.4 interruptions per night (Table 6).
Figure 5.
Timing and duration of interruptions in bednet use by household. This figure appears in color at www.ajtmh.org.
Table 6.
Interruptions in use after unfurled for night*
| Interruption rate per night, rate (n) | Total nonuse due to interruptions (hour minutes) | Average duration of interruption (hour minutes [SD]) | |
|---|---|---|---|
| Overall | 0.23 (86/369) | 69 hours 15 minutes | 0 hour 48 minutes (49 minutes) |
| By household | |||
| 1 | 0.12 (3/26) | 8 hours 30 minutes | 2 hours 50 minutes (14 minutes) |
| 2 | 0.28 (11/39) | 4 hours 0 minutes | 0 hour 22 minutes (12 minutes) |
| 3 | 0.13 (4/31) | 1 hour 0 minutes | 0 hour 15 minutes (0 minutes) |
| 4 | 0.21 (9/43) | 3 hours 45 minutes | 0 hour 25 minutes (23 minutes) |
| 5 | 0.29 (12/42) | 13 hours 15 minutes | 1 hour 6 minutes (37 minutes) |
| 6 | 0.36 (12/33) | 13 hours 0 minutes | 1 hour 5 minutes (42 minutes) |
| 7 | 0.17 (7/42) | 6 hours 0 minutes | 0 hour 51 minutes (55 minutes) |
| 8 | 0.4 (17/43) | 10 hours 30 minutes | 0 hour 37 minutes (54 minutes) |
| 9 | 0.33 (11/33) | 9 hours 15 minutes | 0 hour 50 minutes (40 minutes) |
| 10 | 0 (0/37) | 0 hour 0 minutes | 0 hour 0 minutes (0 minutes) |
* Restricted to nights with at least four-hour use between 1800 and 0900.
DISCUSSION
In this study of 10 households using a remote and objective bednet adherence monitor for 6 weeks in rural Uganda, we were able to comprehensively characterize bednet use at high temporal resolution, leading to multiple insights. We discovered substantial heterogeneity in bednet adherence behaviors between users along various metrics with relevance for malaria prevention with LLINs.
Long-lasting insecticide-treated bednets are meant to be unfurled when individuals sleep and then folded up on awakening. Underlying differences in sleep timing and other nighttime behaviors among the billions of LLIN users worldwide may represent important variations in how LLINs are used in practice with potential relevance for malaria prevention.19,20 Only one other published study to our knowledge has used remote adherence monitors to assess bednet use. That study found 81% nightly adherence in Cote D’Ivoire, but they did not attempt to characterize bednet use in detail as we have done here.21 In our study, the average duration of LLIN use over 418 days of monitoring was 9 hours 49 minutes. However, some households used their LLINs substantially less, such as household 6 (average duration: 7 hours 6 minutes) and others, such as household 8, substantially longer (13 hours 30 minutes). It is reasonable to expect that this nearly 2-fold difference in protection between these households will have implications for their relative risks of acquiring malaria. Overall use from 2100 to 0600 was 85–90%, suggesting that this was a relatively adherent cohort. Besides the general emphasis on higher use that is inherent in the WHO policy of universal access, however, there is no consensus on what level of LLIN use is actually achievable and/or desirable in at-risk households. Future studies using electronic monitoring of LLIN use should correlate malaria outcomes with quantified measures of bednet use to determine what level of adherence is necessary to achieve malaria control goals in various transmission settings.
Some households tended to have consistently poor adherence. In particular, households 1, 6, and 9 had low adherence between 2100 and 0600, hours that are of highest risk for exposure to biting mosquitoes. Many studies have attempted to identify characteristics associated with poor bednet adherence.22,23 Remote adherence monitors could help identify poorly adherent users and facilitate deeper inquiries into the circumstances, leading to poor adherence which can then be used to improve malaria prevention programs.
Of 418 observation nights, we identified 4 households (1, 4, 6, and 9) that comprised all 19 instances when the SmartNet was not used the entire night. These events are high risk, because they expose individuals to many hours without protection. Anecdotal evidence suggests that some of these events may have been due to travel away from home, which is increasingly becoming recognized as a source of exposure risk.24,25 Ways to predict these missed nights, and mitigate their effects, should be explored in future studies.
Intra-night interruptions in use, for example, bathroom use, could represent an important risk of exposure to malaria vectors despite self-reported bednet adherence.15 We discovered a variety of different intra-night bednet use behaviors, including no interruptions at all (household 10), many short interruptions (household 8), and just a few long interruptions (household 1). Studying these sorts of overnight behaviors is challenging if not impossible using traditional methods. Remote adherence monitors may provide a feasible and acceptable alternative that reduces both the lack of reliability inherent in self-reports and also the privacy/logistical problems associated with direct observations or video capture. Future studies should explore how the full range of human bednet use behaviors implicate malaria risk.
The clock time bednets are unfurled has particular relevance, given evidence of earlier vector biting in response to control efforts.9 An average overall unfurling time of 2034 seems reasonable, but sunset occurs somewhere between 1830 and 1930.26 In addition, some households put their bednets down much later, nearer to 2200, likely exposing them to a significant number of mosquito bites that could be avoided with earlier use. Barriers to earlier bednet use should be explored, as these could represent important sources of residual risk despite apparent bednet coverage. Interestingly, households 2 and 7 had only adults using the SmartNet and also the latest unfurling times. Future studies will need to be powered to identify differences in use depending on the age and other characteristics of bednet users.
This study has important limitations. The small sample size makes generalization outside this population difficult. In addition, each household received only one SmartNet, making it difficult to identify differences in behaviors between household members. SmartNet detects bednet use based on the state of the net materials (i.e., folded up or unfurled); thus, we are unable to determine whether the unfurled bednet is providing actual protection to one or more individuals. Our reported intra-night interruptions are likely an underestimate because SmartNet cannot detect an individual simply slipping out from under a bednet without folding it up. Finally, given the appearance of the SmartNet, the monitoring itself may change behaviors. Studies of monitors for medication adherence in Uganda have found that this effect typically fades over time,27 but findings in this study should be correlated with SmartNet monitoring over longer time periods to look for evidence of a potential Hawthorne effect.
In conclusion, insecticide-treated bednets are a crucial pillar of malaria control. The main focus in studies of LLIN effectiveness has been on vector behaviors,10 insecticide resistance,11,12,28 and durability of bednet materials.13 In addition, there are multiple new LLINs being developed and tested, at significant cost.29,30 Quantifying the human behaviors underlying real-life bednet use is a potentially important, and under-researched, component in understanding how these very prevalent and critical public health tools function in malaria control. New electronic adherence monitors can provide novel insights into how bednets are used in practice and may also provide novel targets for malaria prevention programs to help regain the initiative in malaria control.
Acknowledgments:
This study was funded by the Massachusetts General Hospital Center for Global Health, the Thrasher Research Fund Early Career Award (P. J. K.), Consortium for Affordable Medical Technologies (CAMTech), Uganda, and Opportunity Solutions International. We thank the support staff in the CAMTech co-creation laboratory for their technical support. We are appreciative of the health staff of the Health Centre IV in Kinoni for their help in recruiting participants. We particularly would like to thank the 10 Ugandan households for being willing to participate in this study.
REFERENCES
- 1.WHO , 2018. World Malaria Report 2018. Geneva, Switzerland: World Health Organization. [Google Scholar]
- 2.Sexton JD, Ruebush TK, II, Brandling-Bennett AD, Breman JO, Roberts JM, Odera JS, Were JBO, 1990. Permethrin-impregnated curtains and bed-nets prevent malaria in western Kenya. Am J Trop Med Hyg 43: 11–18. [DOI] [PubMed] [Google Scholar]
- 3.Lengeler C, 2004. Insecticide-treated bed nets and curtains for preventing malaria. Cochrane Database Syst Rev CD000363. [DOI] [PubMed] [Google Scholar]
- 4.WHO , 2007. Insecticide-Treated Mosquito Nets: A WHO Position Statement. Geneva, Switzerland: World Health Organization. [Google Scholar]
- 5.Bhatt S, et al. 2015. The effect of malaria control on Plasmodium falciparum in Africa between 2000 and 2015. Nature 526: 207–211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Katureebe A, et al. 2016. Measures of malaria burden after long-lasting insecticidal net distribution and indoor residual spraying at three sites in Uganda: a prospective observational study. PLoS Med 13: e1002167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Raouf S, et al. 2017. Resurgence of malaria following discontinuation of indoor residual spraying of insecticide in an area of Uganda with previously high-transmission intensity. Clin Infect Dis 65: 453–460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wanzira H, Katamba H, Okullo AE, Agaba B, Kasule M, Rubahika D, 2017. Factors associated with malaria parasitaemia among children under 5 years in Uganda: a secondary data analysis of the 2014 malaria indicator survey dataset. Malar J 16: 191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sougoufara S, Thiaw O, Cailleau A, Diagne N, Harry M, Bouganali C, Sembène PM, Doucoure S, Sokhna C, 2018. The impact of periodic distribution campaigns of long-lasting insecticide-treated bed nets on malaria vector dynamics and human exposure in Dielmo, Senegal. Am J Trop Med Hyg 98: 1343–1352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Thomsen EK, Koimbu G, Pulford J, Jamea-Maiasa S, Ura Y, Keven JB, Siba PM, Mueller I, Hetzel MW, Reimer LJ, 2017. Mosquito behavior change after distribution of bednets results in decreased protection against malaria exposure. J Infect Dis 215: 790–797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Trape JF, et al. 2011. Malaria morbidity and pyrethroid resistance after the introduction of insecticide-treated bednets and artemisinin-based combination therapies: a longitudinal study. Lancet Infect Dis 11: 925–932. [DOI] [PubMed] [Google Scholar]
- 12.Toé KH, Jones CM, N’Fale S, Ismail HM, Dabiré RK, Ranson H, 2014. Increased pyrethroid resistance in malaria vectors and decreased bed net effectiveness, Burkina Faso. Emerg Infect Dis 20: 1691–1696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Morgan J, et al. 2015. Physical durability of two types of long-lasting insecticidal nets (LLINs) three years after a mass LLIN distribution campaign in Mozambique, 2008–2011. Am J Trop Med Hyg 92: 286–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zinszer K, Stone J, Mpaata JC, Muwanguzi S, Adler S, McGowan CL, Levy PD, 2017. Success and failure: a firsthand look into Ugandas most recent bednet distribution campaign. Lancet Infect Dis 17: 251–253. [DOI] [PubMed] [Google Scholar]
- 15.Krezanoski PJ, Bangsberg DR, Tsai AC, 2018. Quantifying bias in measuring insecticide-treated bednet use: meta-analysis of self-reported vs objectively measured adherence. J Glob Health 8: 010411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fernando SD, Abeyasinghe RR, Galappaththy GN, Gunawardena N, Ranasinghe AC, Rajapaksa LC, 2009. Sleeping arrangements under long-lasting impregnated mosquito nets: differences during low and high malaria transmission seasons. Trans R Soc Trop Med Hyg 103: 1204–1210. [DOI] [PubMed] [Google Scholar]
- 17.Krezanoski PJ, Campbell JI, Santorino D, Bangsberg DR, 2017. Objective monitoring of insecticide-treated bednet use to improve malaria prevention: SmartNet development and validation. PLoS One 12: e0168116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Krezanoski PJ, Santorino D, Nambogo N, Campbell JI, Bangsberg DR, 2016. Maternal attitudes about objectively monitored bednet use in rural Uganda. Malar Res Treat 2016: 8727131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Leake DW, Jr., Hii JL, 1994. Observations of human behavior influencing the use of insecticide-impregnated bednets to control malaria in Sabah, Malaysia. Asia Pac J Public Health 7: 92–97. [DOI] [PubMed] [Google Scholar]
- 20.Harvey SA, Lam Y, Martin NA, Olórtegui MP, 2017. Multiple entries and exits and other complex human patterns of insecticide-treated net use: a possible contributor to residual malaria transmission? Malar J 16: 265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Koudou BG, Malone D, Hemingway J, 2014. The use of motion detectors to estimate net usage by householders, in relation to mosquito density in central Cote d’Ivoire: preliminary results. Parasites Vectors 7: 96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Singh M, Brown G, Rogerson SJ, 2013. Ownership and use of insecticide-treated nets during pregnancy in sub-Saharan Africa: a review. Malar J 12: 268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pulford J, Hetzel MW, Bryant M, Siba PM, Mueller I, 2011. Reported reasons for not using a mosquito net when one is available: a review of the published literature. Malar J 10: 83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yukich JO, Taylor C, Eisele TP, Reithinger R, Nauhassenay H, Berhane Y, Keating J, 2013. Travel history and malaria infection risk in a low-transmission setting in Ethiopia: a case control study. Malar J 12: 33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Alemu K, Worku A, Berhane Y, Kumie A, 2014. Men traveling away from home are more likely to bring malaria into high altitude villages, northwest Ethiopia. PLoS One 9: e95341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Time and Date AS 1995–2019. Sunrise and Sunset Times in Kampala. Available at: https://www.timeanddate.com/sun/uganda/kampala. Accessed December 21, 2018.
- 27.Haberer JE, Kahane J, Kigozi I, Emenyonu N, Hunt P, Martin J, Bangsberg DR, 2010. Real-time adherence monitoring for HIV antiretroviral therapy. AIDS Behav 14: 1340–1346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Strode C, Donegan S, Garner P, Enayati AA, Hemingway J, 2014. The impact of pyrethroid resistance on the efficacy of insecticide-treated bed nets against African anopheline mosquitoes: systematic review and meta-analysis. PLoS Med 11: e1001619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Protopopoff N, et al. 2018. Effectiveness of a long-lasting piperonyl butoxide-treated insecticidal net and indoor residual spray interventions, separately and together, against malaria transmitted by pyrethroid-resistant mosquitoes: a cluster, randomised controlled, two-by-two factorial design trial. Lancet 391: 1577–1588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tiono AB, et al. 2018. Efficacy of Olyset Duo, a bednet containing pyriproxyfen and permethrin, versus a permethrin-only net against clinical malaria in an area with highly pyrethroid-resistant vectors in rural Burkina Faso: a cluster-randomised controlled trial. Lancet 392: 569–580. [DOI] [PubMed] [Google Scholar]