Abstract
BACKGROUND:
There is a striking lack of long-term, prospective outcomes data for endoscopic sinus surgery (ESS) in chronic rhinosinusitis (CRS) using validated instruments. The primary objective of this study is to report long-term outcomes (>10 years) after ESS for CRS obtained by prospective data collection.
METHODS:
An observational cohort (n=59) of adult patients with CRS electing ESS was enrolled between 2004-2008. Long-term, disease-specific quality-of-life (QOL) outcomes, health utility values (HUV), revision surgery rate, development of asthma, and patient expectations/satisfaction with outcomes of ESS were examined using descriptive statistics and simple fixed-effects linear modeling.
RESULTS:
59 adult patients were followed for 10.9 years [±13.8 months] on average. Mean QOL significantly improved between baseline and 6 months and remained durable to 10 years. HUV improved to normal. A 17% revision surgery rate within the 10 year follow-up period was observed with a 25% revision rate in CRS with polyposis. New onset asthma after ESS occurred at a rate of 0.8%/year. Patient satisfaction with ESS outcomes was generally high.
CONCLUSIONS:
Ten year prospective outcomes of ESS for CRS demonstrate that the initial clinically significant improvements in QOL seen 6 months postoperatively are durable over the long term. Over 75% of patients reported clinically significant long term QOL and HUV improvement. HUV returned to normal. Revision surgery rates was 17% and worse postoperative endoscopy scores within 18 months of initial ESS were associated with higher likelihood of revision surgery. Most patients would pursue ESS again and recommend it to other patients considering this treatment option.
Keywords: Sinusitis, chronic disease, outcome assessment (health care), quality of life
INTRODUCTION
Chronic rhinosinusitis (CRS) is a common disease, with substantial morbidity identified by using quality of life (QOL) measures.1-3 More than 250,000 persons undergo endoscopic sinus surgery (ESS) for CRS in the United States (U.S.) each year.4 Despite this, there is a striking lack of long-term, prospective data using validated QOL instruments in the U.S. literature. Currently, the literature suggests that most patients will report symptomatic improvement after ESS with some suggestion that these improvements may dissipate over time.5,6 The prevailing literature is limited primarily by retrospective data collection, subjective definitions of patient “improvement” following surgery, secondary database analyses, and/or a 5 year maximum time frame for prospectively collected long-term follow-up results.5,7-10.
In 2004, we began to develop a prospective cohort of patients with CRS undergoing ESS, and to study disease-specific QOL, as well as other outcomes of interest using validated outcome measures. We have made a number of observations about short- to intermediate-term outcomes (eg. generally less than 2 years) in multiple prior publications.2,11-15 The majority of these patients experienced clinically significant improvement at 6 months that was durable to 18 months with follow-up evaluation. Although these studies suggest that ESS is efficacious, many patients want to know how long benefits are likely to last, whether additional procedures will be necessary, and ultimately whether they will be satisfied with the decision to pursue surgery. The primary objective of this study was to report long-term outcomes of ESS for CRS (average >10 years) obtained by prospective data collection. Specifically, we examined long-term, disease-specific QOL outcomes, health utility values (HUV), revision surgery rates, the incidence of new onset asthma, the impacts of nasal polyposis, and patient expectations/satisfaction with outcomes of ESS in the treatment of adult CRS.
MATERIALS and METHODS
Study Population
This investigation revisited an observational cohort of adult patients with CRS as part of a study funded by the National Institute on Deafness and Other Communication Disorders, one of the National Institutes of Health (Bethesda, MD).2 Patients were diagnosed with CRS, with and without nasal polyposis, by a fellowship trained Rhinologist following appropriate criteria established at the time16 and were considered surgical candidates following trials of medical therapy as directed by their physician. Patients were prospectively offered study enrollment to help evaluate surgical outcomes of CRS within an academic tertiary referral care setting.
Original enrollment of human subjects occurred between July, 2004 and December, 2008 within the Department of Otolaryngology-Head and Neck Surgery located at Oregon Health & Science University (OHSU, Portland, OR). Enrollment interviews, aimed at collecting extensive data for medical and social history, were completed for those patients who elected ESS. Study participants who provided informed, written consent were assured that voluntary study participation involved minimal risk and did not alter the standard of care. The Institutional Review Board at OHSU approved all study protocols (eIRB #658), conducted independent annual reviews and data safety monitoring. Surgical outcomes from the 18 month observational period have been previously described in the literature.17-19
Computed tomography (CT) imaging and sinonasal endoscopy of the sinus regions, collected during preoperative clinical evaluations, were used simultaneously for study purposes. Imaging was scored by the enrolling physician at OHSU in accordance with Lund-Mackay bilateral staging (range: 0–24).20 Bilateral paranasal sinuses were evaluated preoperatively using rigid sinonasal endoscopy and scored using the Lund-Kennedy bilateral staging system (range: 0–20).21 Higher scores on both scoring systems represent worse severity of sinus disease. Patients were categorized as CRS with nasal polyposis (CRSwNP) and CRS without nasal polyposis (CRSsNP) based upon endoscopy.
Surgical Intervention
Surgical intervention for the cohort was completed between August, 2004 and April, 2009. Study participants underwent surgical procedures consisting of either unilateral or bilateral maxillary antrostomy, partial or total ethmoidectomy, sphenoidotomy, and/or frontal sinusotomy per the judgement of the enrolling surgeon. Inferior turbinate reduction and/or septoplasty were performed as indicated per the judgement of the enrolling surgeon. Postoperative medical therapy was tailored to the extent of inflammation noted on postoperative clinic visits per the judgement of the treating surgeon.
Patient Reported Outcome Measures
Survey evaluations were completed by study participants both preoperatively and at 6-month postoperative intervals out to 18 months during either routine in-clinic appointments or using hard copy surveys distributed through the U.S. Postal service. Study participants were asked to complete a battery of openly accessible, patient reported outcomes measures (PROMs) including the Rhinosinusitis Disability Index (RSDI), the duration-based Chronic Sinusitis Survey (CSS-D), and the SF-6D (version 1.0) HUV survey, a derivation of the 36-item Medical Outcomes Study Short-Form instrument. The RSDI is a 30-item survey designed to measure self-reported symptom severity of CRS across a respondent’s global health, as well as the physical, functional, and emotional domains.22 Survey items of the RSDI utilized Likert scales ranging from a minimum score of 0 (“Never”) to a maximum score of 4 (“Always). Total RSDI scores are a summarization of all completed responses (range: 0–120), combining physical domain scores (range: 0–44), functional domain scores (range: 0–36), and emotional domain scores (range: 0–40). Lower RSDI scores reflect lower QOL impacts associated with CRS. A minimal clinically important difference (MCID) for RSDI total scores, as a measure of health-related QOL has been previously estimated as ½ of the standard deviation (SD) associated with the preoperative mean score.2,23
The CSS-D is a survey designed to measure the self-reported duration of sinusitis symptoms and medication usage within the 8 week period preceding survey completion.24 The CSS-D is a 6-item metric of symptom and medication duration using response categories ranging from “0 weeks” to “7–8 weeks”. Both the CSS-D total score (range: 0–100) and symptom and medication domain scores (range: 0–100) are calculated using transformed raw scale item scores. Higher CSS-D scores reflect lower QOL impacts associated with CRS. Values for the MCID of CSS-D total scores have been estimated using the same criteria of ½ SD of the preoperative mean score.
The SF-6D health utility value survey instrument is comprised of a subset of 6 questions extracted from either the 12-item or 36-item Medical Outcomes Study Short Form survey. The SF-6D survey items are transformed into standardized HUVs (range: 0.3–1.0), as described by Brazier, et al.25 The SF-6D describes a normalized value that a respondent ascribes to their particular health state at the time of survey completion, where a score of 1.0 represents perfect health and lower/worse scores reflect declining health states. Positive, within-subject score changes of at least 0.03 have been previously described as the MCID while scores of 0.81 have been defined as representative of the normal U.S. population.26,27
Long-Term Follow-up Procedures
Study participants enrolled in the original observational cohort at OHSU were contacted between October, 2017 and April, 2018 in order to provide additional follow-up responses to all PROMs, as well as supplementary questions regarding the need for revision ESS, new onset asthma diagnosis, and patient expectations/satisfaction with surgical intervention (Table 1). Electronic medical records (EPIC Systems, Verona, WI) were surveyed for most recent contact information. Study participants willing to participate provided additional informed consent and completed follow-up surveys using a secure, web-based survey application (n=45) (RedCap, Vanderbilt University Medical Center, Nashville, TN)28, hard copy surveys (n=11), or phone interview (n=3), per individual preference. Attempted collection of long-term follow-up was optimized through repeated study invitation and hard copy reminders at regular intervals.
Table 1:
Supplementary long-term follow-up survey questions surrounding patient expectation
| 1. Before you had sinus surgery, did you believe this treatment would completely resolve your sinus condition related symptoms? | ○ Strongly disagree ○ Disagree ○ Neither agree or disagree ○ Agree ○ Strongly agree |
| 2. The resolution of my symptoms following sinus surgery matched my expectations that I had prior to surgery. | ○ Strongly disagree ○ Disagree ○ Neither agree or disagree ○ Agree ○ Strongly agree |
| 3. Sinus surgery improved the symptoms most important to me. | ○ Strongly disagree ○ Disagree ○ Neither agree or disagree ○ Agree ○ Strongly agree |
| 4. I was satisfied that I was adequately informed about the issues important to my decision to receive sinus surgery. | ○ Strongly disagree ○ Disagree ○ Neither agree or disagree ○ Agree ○ Strongly agree |
| 5. If you had to do it again, would you pursue sinus surgery? | ○ Strongly disagree ○ Disagree ○ Neither agree or disagree ○ Agree ○ Strongly agree |
| 6. I would recommend sinus surgery to someone else who needed it. | ○ Strongly disagree ○ Disagree ○ Neither agree or disagree ○ Agree ○ Strongly agree |
Data Collection and Statistical Analyses
Analysis of all previous and newly collected study data was completed using SPSS statistical software (v24.0; IBM Corporation, Armonk, NY). Patient health information was protected using study identification number assignments and secure, HIPAA compliant data transfer methods. Scaled variables were assessed for assumptions of distribution normality while final study data was evaluated using appropriate descriptors including means, standard deviations, and frequency measures. Due to unequal numbers of repeated measures missing at random, simple fixed-effects linear modeling was used to evaluate longitudinal outcome scores for the RSDI, CSS, and SF-6D instruments, using time as a fixed effect. Unstructured covariance matrices were used due to differences in the variance of each follow-up time point and differences of within-subject correlation between time pairings for each outcome measure. Model fit was evaluated comparing −2 restricted log likelihood information criteria while the F-test was used to determine overall significance of simple fixed effects model. Within-subject, pairwise comparison t-testing was used to assess mean differences between study time points while either independent sample t-testing or Mann-Whitney U testing was used to compare between-subject results at discrete follow-up time points. A conventional 0.050 type-I error probability (p-value) determined statistically significant associations.
RESULTS
Final Study Population
A total of 227 study participants were identified as potential candidates for long-term follow-up. Current mailing addresses and/or phone contact information was not available for 58 (26%) potential respondents while 12 (5%) indicated they did not wish to participate and 3 patients were reported as deceased (1%). A total of 95 patients with contact information did not respond to our attempts to gather follow-up information. A total of 59/154 (38%) remaining subjects provided responses to additional follow-up surveys available for analysis with a mean long-term postoperative follow-up of 131 [±13.8] months (10.9 years; range: 105–160 months). Preoperative patient characteristics at the time of original enrollment are described in Table 2 while the prevalence of surgical procedures are described in Table 3. Only eight patients underwent partial ethmoidectomy and no patient had only single sinus intervention. We performed a baseline analysis of patients completing follow-up versus those unaccounted and no baseline differences were observed between the groups.
Table 2:
Preoperative demographic and health characteristics of final study population with CRS (n=59)
| Characteristic: | Mean [±SD] | Range [LL, UL] | N (%) |
|---|---|---|---|
| Age (years) | 53.8 [±10.8] | [27, 79] | ----- |
| Males | ----- | ----- | 33 (56%) |
| Female | ----- | ----- | 26 (44%) |
| Nasal polyposis | ----- | ----- | 32 (54%) |
| Asthma | ----- | ----- | 25 (42%) |
| Aspirin intolerance / AERD | ----- | ----- | 11 (19%) |
| Allergy (mRAST+/skin prick+) | ----- | ----- | 18 (31%) |
| COPD | ----- | ----- | 0 (0%) |
| Depression | ----- | ----- | 4 (7%) |
| Tobacco use | ----- | ----- | 2 (3%) |
| Alcohol use (Drinks/week) | 4.2 [±6.4] | [0, 25] | 35 (59%) |
| Corticosteroid dependency | ----- | ----- | 2 (3%) |
| Lund-Mackay CT score | 13.0 [±6.8] | [0, 24] | ----- |
| Lund-Kennedy endoscopy score | 8.2 [±4.8] | [0, 18] | ----- |
CRS, chronic rhinosinusitis; SD, standard deviation; LL, lower limit; UL, upper limit; mRAST, modified radioallergosorbent testing; +, positive; COPD, chronic obstructive pulmonary disease; CT, computed tomography; AERD, aspirin exacerbated respiratory disease.
Table 3:
Prevalence of surgical procedures during endoscopic sinus surgery (n=59 patients)
| Surgical procedures: | Left Side N(%) |
Right Side N (%) |
|---|---|---|
| Maxillary antrostomy | 51 (86%) | 52 (88%) |
| Partial ethmoidectomy | 7 (12%) | 8 (14%) |
| Total ethmoidectomy | 47 (80%) | 46 (78%) |
| Sphenoidotomy | 41 (70%) | 40 (68%) |
| Middle turbinate resection | 10 (17%) | 12 (20%) |
| Inferior turbinate reduction | 4 (7%) | 4 (7%) |
| Frontal sinusotomy | 43 (73%) | 39 (66%) |
| Septoplasty | 19 (32%) | |
| Image guidance | 41 (70%) | |
| Revision endoscopic sinus surgery | 41 (70%) | |
N, sample size.
Long-Term Postoperative Improvement in PROMs
Fixed-effect linear modeling was used to evaluate longitudinal trends in average PROM scores using study visit time points as the primary fixed effect of interest. Without adjustment for covariate effects, significant improvement for all mean PROM scores was reported (Table 4). For all PROM total scores the greatest magnitude of improvement was between preoperative and long-term postoperative follow-up measures (all p<0.001; Figures 1-2). No significant differences in any RSDI score or the CSS symptom domain score, between matched pairings of 18 month postoperative follow-up and long-term postoperative follow-up were reported (t< 1.47; p>0.15). Compared to 18 month postoperative averages, study participants reported additional significant improvement in CSS medication scores at long-term postoperative follow-up (t= −2.48; p=0.02; Figure 2) potentially reflective of long-term medication use reduction. Results from the CSS medication domain influenced similar findings for CSS total scores with comparable significant improvement between 18 month and long-term follow-up (t= −2.13; p=0.04). The majority of study participants (86%) reported clinically significant improvement through long-term changes in RSDI total scores, equaling or exceeding one MCID value (8.7 points). Similarly, a majority of participants (75%) also reported long-term postoperative improvements in CSS total scores, equaling or exceeding one MCID value (9.7 points; Table 4). Using independent samples ranking tests for nonparametric distributions, a comparison of average long-term follow-up RSDI and CSS total scores between patients with and without revision ESS during the 10 year follow-up demonstrates no significant differences in long-term RSDI and CSS total scores between groups (p= 0.82).
Table 4:
Average patient-reported outcome measures compared across all study visits (n=59).
| Study Visit Time Points | F-test Fixed Effect Model |
DF | p-value | |||||
|---|---|---|---|---|---|---|---|---|
| PROMs: | Preoperative | 6-Month Postoperative |
12 Month Postoperative |
18 Month Postoperative |
Long-term Postoperative Follow-up |
|||
| Mean [±SD] | Mean [±SD] | Mean [±SD] | Mean [±SD] | Mean [±SD] | ||||
| RSDI Physical | 18.1 [±7.3] | 9.3 [±7.9] | 8.8 [±7.6] | 9.7 [±7.4] | 9.4 [±7.3] | 27.2 | 4 | <0.001 |
| RSDI Functional | 15.2 [±6.1] | 8.2 [±7.2] | 6.5 [±6.5] | 7.2 [±6.9] | 6.0 [±7.2] | 26.1 | 4 | <0.001 |
| RSDI Emotional | 12.9 [±7.3] | 7.3 [±6.3] | 5.8 [±6.8] | 6.3 [±6.1] | 4.5 [±6.4] | 20.6 | 4 | <0.001 |
| RSDI Total | 46.2 [±17.4] | 24.8 [±20.1] | 21.1 [±19.6] | 23.2 [±18.6] | 19.9 [±19.0] | 32.6 | 4 | <0.001 |
| CSS Symptom | 31.8 [±28.4] | 69.4 [±23.0] | 68.0 [±31.9] | 59.0 [±30.8] | 63.5 [±28.6] | 26.7 | 4 | <0.001 |
| CSS Medication | 46.2 [±23.6] | 51.3 [±22.6] | 54.3 [±21.8] | 57.0 [±28.1] | 70.6 [±27.8] | 7.8 | 4 | <0.001 |
| CSS Total | 38.9 [±19.3] | 60.4 [±18.0] | 61.2 [±21.9] | 58.0 [±22.4] | 66.9 [±23.4] | 19.3 | 4 | <0.001 |
PROM, patient-reported outcome measure; SD, standard deviation; DF, degrees of freedom; RSDI, Rhinosinusitis Disability Index; CSS, Chronic Sinusitis Survey.
Figure 1:
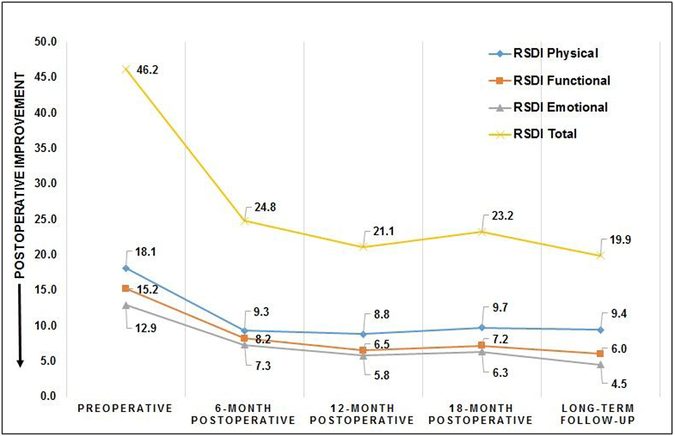
Within-subject trends in average scores of the RhinoSinusitis Disability Index (RSDI) compared across all study visits (n=59)
Figure 2:
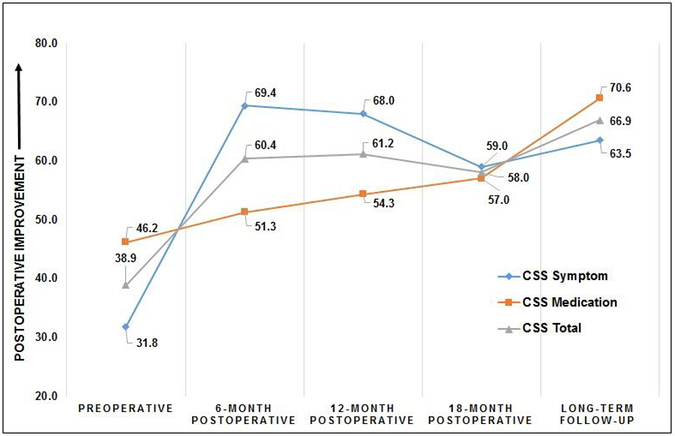
Within-subject trends in average scores of the Chronic Sinusitis Survey (CSS) compared across all study visits (n=59)
Long-Term Postoperative Improvement in Health Utility Values
Without adjustment for covariate effects in fixed effects modeling, significant improvement in SF-6D health utility scores was reported including long-term postoperative follow-up measures for the total observed time period (F=18.9; df=4, p<0.001; Figure 3). Similar to PROM findings, no significant differences in average SF-6D HUV scores between the matched pair of 18 month postoperative follow-up (0.77 [±0.12]) and long-term postoperative follow-up scores (0.79 [±0.12]) were reported (t= −1.02; p=0.31), with the average long-term postoperative SF-6D health state more closely approaching a normal health state represented within a non-institutionalized U.S. population.27 A majority of participants (76%) reported long-term improvement in SF-6D HUV, equaling or exceeding one MCID value.
Figure 3:
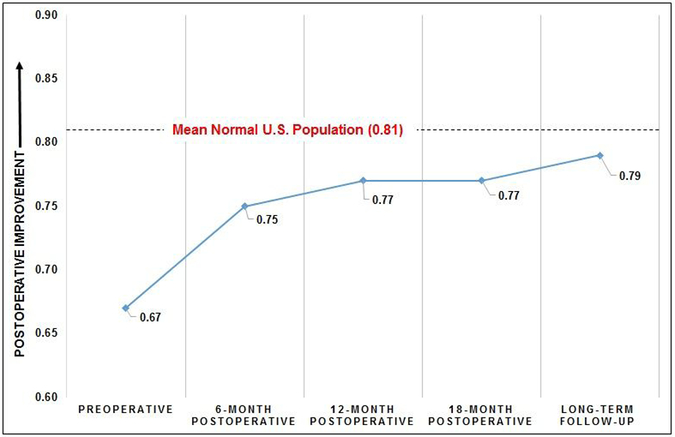
Within-subject trends in mean SF-6D health utility value scores compared across all study visits (n=59)
Need for Revision Surgery during Long-Term Follow-up
Subjects also provided information regarding the need for additional ESS since the time of the original surgical intervention. A total of 10/59 (17%) required additional sinus surgery within the long-term follow-up period, with 8/59 (14%) requiring one additional procedure and 2/59 (3%) patients requiring two additional revision procedures. Eighty percent (8/10) of the patients requiring revision sinus surgery had CRS with nasal polyposis and half of those (4/8) had aspirin exacerbated respiratory disease (AERD). A total of 51/59 (86%) patients were evaluated with postoperative endoscopy within the initial 18 month postoperative period. Those who required revision ESS between the 18 month and 10 years were found to have a significantly worse (p=0.03) Lund-Kennedy endoscopy score of 5.8 [±3.7] at their initial postoperative endoscopy exam (n=8), compared to 2.9 [±3.5] for patients not requiring revision ESS (n=43). Additionally, nasal polyp recurrence within 18 months of surgery was significantly higher in study participants requiring future revision ESS (50%) compared to patients who did not require revision (9%; p=0.004).The total follow-up duration time equated to 7742 observed person-months indicating a total incidence rate of 0.0013 cases / person-month or 0.015 cases / person-year.
Impact of Polyp Status
Stratified differences in long-term PROMs were compared between study participants with nasal polyposis (CRSwNP; n=32) and without nasal polyposis (CRSsNP; n=27). Both subgroups reported significant improvement in mean PROM scores over the study duration (F>6.8; df=4; p<0.003) with the exception of CSS medication scores in CRSwNP (F=2.5; df=4; p=0.08). Without adjustment for multiple bivariate comparisons, patients with CRSwNP experienced significantly less improvement in RSDI total score (t= −2.17; p=0.03; Figure 4) and CSS total score (t= 2.28; p=0.03; Figure 5) at 10 year follow-up though their improvement was still clinically significant exceeding one MCID.
Figure 4:
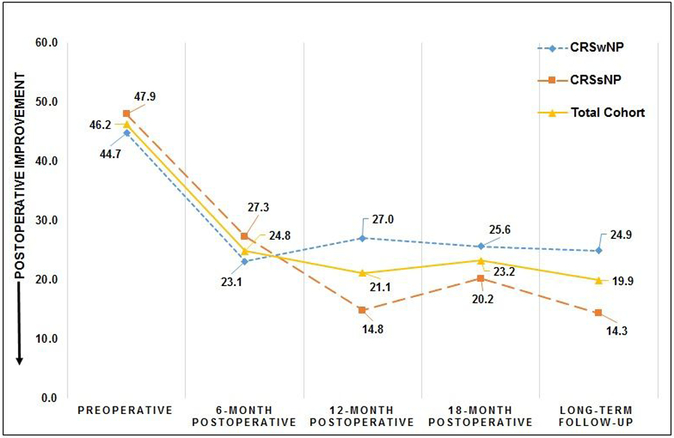
Average RSDI total scores compared across all study visits for patients with and without nasal polyposis.
Figure 5:
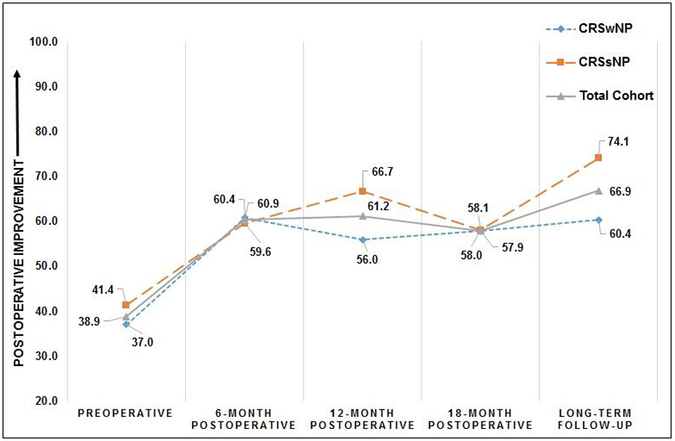
Average CSS total scores compared across all study visits for patients with and without nasal polyposis.
Similarly, both CRSwNP and CRSsNP subgroups reported clinically and statistically significant improvement in HUV over the long-term study period (F>10.0; df=4; p<0.001); however there was no significant difference between the two subgroups in mean score (t= 0.02; p=0.98; Figure 6) at long-term follow-up.
Figure 6:
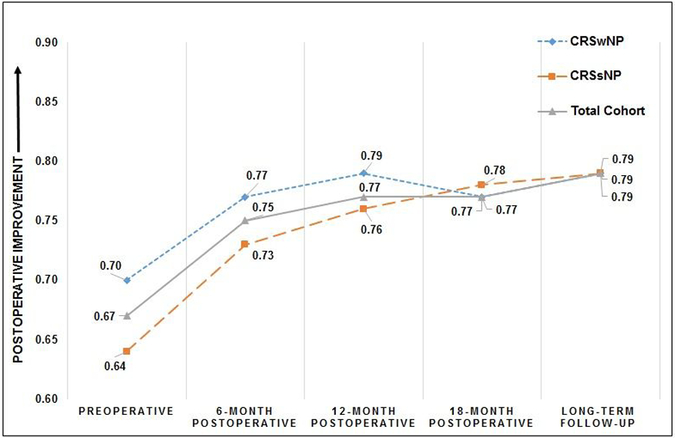
Average SF-6D health utility values compared across all study visits for patients with and without nasal polyposis.
Development of Asthma
A total of 25/59 (42%) of study participants reported comorbid asthma at the time of initial study enrollment. Of the remaining 34 participants without comorbid asthma, 3/34 (9%) reported new onset asthma during the 10 year follow-up period. With the total of 4544 observed person-months in this group without pre-existing asthma, the observed incidence rate of new onset asthma was 0.008 cases / person-year (0.8% per year).
Patient Expectations/Satisfaction
Responses to follow-up surveys regarding patient expectations of their original surgical intervention are summarized in Table 5. A large majority of participants (>85%) reported satisfaction with both their decision to pursue ESS as a treatment option and with how ESS improved symptoms most important to them. A majority of respondents agreed or strongly agreed that they would pursue ESS again, if needed, and would recommend the procedure to someone else experiencing symptoms of CRS.
Table 5:
Frequency of responses to long-term follow-up survey questions surrounding patient expectation of endoscopic sinus surgery (n=59)
| ‘Strongly disagree’ |
‘Disagree’ | ‘Neither agree or disagree’ |
‘Agree’ | ‘Strongly agree’ |
|
|---|---|---|---|---|---|
| N (%) | N (%) | N (%) | N (%) | N (%) | |
| 1. Before you had sinus surgery, did you believe this treatment would completely resolve your sinus condition related symptoms? | 0 (0%) | 10 (17%) | 16 (27%) | 26 (44%) | 7 (12%) |
| 2. The resolution of my symptoms following sinus surgery matched my expectations that I had prior to surgery. | 1 (2%) | 10 (17%) | 13 (22%) | 24 (41%) | 11 (19%) |
| 3. Sinus surgery improved the symptoms most important to me. | 2 (3%) | 4 (7%) | 9 (15%) | 27 (46%) | 17 (29%) |
| 4. I was satisfied that I was adequately informed about the issues important to my decision to receive sinus surgery. | 1 (2%) | 0 (0%) | 5 (9%) | 29 (49%) | 24 (41%) |
| 5. If you had to do it again, would you pursue sinus surgery? | 0 (0%) | 1 (2%) | 7 (12%) | 17 (29%) | 34 (58%) |
| 6. I would recommend sinus surgery to someone else who needed it. | 1 (2%) | 2 (3%) | 4 (7%) | 20 (34%) | 32 (54%) |
N, sample size.
DISCUSSION
Key Findings
We have reported prospective, long term outcomes of sinus surgery for CRS that suggest that the shorter term benefits previously reported are quite durable with regard to PROMs and HUV. The cohort demonstrated significant improvement in QOL at 6 months postoperatively and those improvements were durable up to nearly 11 years mean follow-up. In fact, the long-term QOL scores were the most improved relative to baseline than at any other time. HUVs also demonstrated significant improvement which, over the long term, approach normal HUVs for the U.S. population.27
Approximately 17% of patients required a revision surgical procedure during the long term follow-up period. Higher (worse) postoperative endoscopy scores within the first 18 months of surgery were associated with higher likelihood of revision surgery within 10 years. CRSwNP accounted for 80% of revision procedures and half of those patients suffered comorbid AERD. However, in total, only 25% of patients with CRSwNP required revision surgery during the long-term follow-up period. New onset asthma occurred at a rate of 0.8% / year during follow-up.
We also studied patient perceptions/satisfaction regarding their expectations of their surgical procedure. A majority of participants reported satisfaction with not only their decision to pursue ESS as a treatment option, but also with how ESS improved symptoms most important to them and the information they received surrounding their decision to pursue ESS. A majority of respondents agreed or strongly agreed that they would pursue ESS again, if needed, and would recommend the procedure to someone else experiencing symptoms of CRS. That said, approximately 20% of patients did not achieve the level of improvement they anticipated with surgery suggesting that patient counseling about expectations can be improved.
Existing Long-Term Literature
There are few reports that examine long-term ESS outcomes in adult patients. In a commonly referenced study on this topic, Senior et al, reported long term follow-up (mean 7.8 years) in a retrospective evaluation of non-validated measures in 72 patients while 98.4% of patients reported “improvement” and 18% required revision procedures.5 In a study primarily examining the effect of smoking on QOL after ESS, White, et al. reported 10 year outcomes by telephone interview on 53 patients.10 They found no difference between smokers and non-smokers in QOL improvement. Revision surgery and other outcomes were not examined. Hopkins et al. reported secondary data utilizing a national database and reported outcomes to 5 years.7 They reported no significant decline from 12 months follow-up outcomes to 60 months follow-up outcomes while a 20% revision surgery rate was reported. Smith, et al. recently reported a 16% revision rate with nearly 10 year follow-up using the Utah Population Database.29 Perhaps the most consistent findings among these studies and our study is the durable nature of the outcomes presented and a revision surgery rate that approximates 15–20% over the long term.
Health State Utility
Health state utility is an important measure of an individual patient’s preference for their current state of health and allows disease state comparisons. Further, HUV outcomes are important both to evaluate the effectiveness of interventions for chronic disease and to generate accurate long-term utility assumptions for economic evaluations.11 Significant decrements in health state utility have been demonstrated in CRS and are comparable to other chronic disease states such as chronic obstructive pulmonary disease, diabetes mellitus and Parkinson’s disease.11,17,30 Rudmik et al. and Scangas et al. have performed important economic analyses utilizing health state utility values and have demonstrated the cost effectiveness of ESS over continued medical therapy alone in appropriately selected patients.31,32 Our study has demonstrated that patients who undergo ESS for CRS experience HUV improvements over time and often continue to experience improvements past the initial shorter-term postoperative follow-up period. In fact, a clinically significant increase in HUV occurred between 6 month follow-up and the 10 year follow-up periods in our study population. This is particularly noteworthy given that health utility typically decreases as people age, with an average HUV decline of 0.016 – 0.018 per decade based on the SF-6D instrument.27 Furthermore, the mean long-term utility level following ESS approached US population norms and was within one MCID value (0.79 versus 0.81; MCID = 0.03) suggesting that ESS in combination with long term medical therapy can restore HUV to normal levels on average.
Impact of Polyps
In the current study, interesting trends were observed related to polyp status. Patients with CRSsNP experienced the largest improvements in PROMs and HUVs. While the final mean PROMs were statistically better in CRSsNP, final HUVs were identical on average at long-term follow-up regardless of polyp status while approaching the normal US population HUV. Interestingly, CSS-medication subscale scores suggested higher long term utilization of medical therapies in CRSwNP. It is unclear whether this is reflective of disease severity or surgeon medication recommendation bias given the propensity toward recurrent disease in this subgroup. Patients with polyps were more likely to require future revision surgery but only a minority required revision surgery (25%) and half of those patients had comorbid AERD. This suggests that patients with CRSwNP are not necessarily destined to multiple surgical procedures to remove polyps over the long-term, countering a prevailing opinion that suggests ESS is only a short term solution for patients with polyposis. Senior et al. suggested that patients with poor postoperative endoscopy evaluations 1.5 years after surgery were more likely to require revision surgery based on retrospective data.5 Our prospective data using postoperative endoscopy scores supports this concept in that higher (worse) mean postoperative endoscopy scores within 18 months of surgery were associated with a higher likelihood of revision sinus surgery within 10 years. Not surprisingly, nasal polyp recurrence on postoperative endoscopy within 18 months of surgery was also associated with a higher likelihood of revision surgery within 10 years, but it is important to recognize that not all patients with nasal polyp recurrence evident on endoscopy will require revision surgery. Prior studies have demonstrated that in CRSwNP, normal endoscopy findings can be achieved in approximately 1/3 of patients while 2/3 will continue to have evidence of inflammation on endoscopy.33,34 Our data suggest that even though abnormal endoscopy may be present in the majority, only a minority of CRSwNP will require revision surgery over the long term. We speculate that this may be due to a better understanding of topical therapy delivery and tailoring surgery to improve topical therapy access, as well and long term treatment of the inflammatory disease. Perhaps the introduction of biologics in the management of CRS will further decrease the need for revision surgery in this patient population.35
Risk of Developing Asthma
Prior studies utilizing large databases and secondary data have suggested that patients with long-term CRS (>5 years) prior to undergoing ESS have greater risk of developing asthma and that the risk declines after ESS. In fact, the incidence of asthma in patients with CRS increased 5% per year prior to ESS and leveled out to <1.0% / year after ESS.36 In the present study, we do not have information regarding the onset of CRS, time to ESS or incidence of asthma during that time frame. However, in our study, the observed incidence of new onset asthma was 0.008 cases / person-year (0.8% / year) after surgery during long-term follow-up which is very similar to the incidence reported in these other studies. The implication of these findings is that control of CRS may benefit patients beyond improvement in QOL and symptoms but also may reduce the risk of development of asthma. While our findings are consistent with the other published studies, our study was not specifically designed to answer this question and further study will be necessary to determine the role of ESS in reducing the risk of developing of asthma.
Patient Expectations/Satisfaction
Research examining patient expectations and satisfaction with treatment decisions is a nascent field with regard to CRS and ESS. Neubauer et al. performed a prospective study of 30 patients and identified a varied understanding of ESS including significant misconceptions about risks, anesthesia, and need for ongoing therapy, among others.37 They found that patients obtain their information from a variety of sources including peers, other doctors, and the Internet. They concluded that awareness of the gaps in patient knowledge and the sources of information will improve preoperative counseling. Yeung et al. prospectively studied 180 patients undergoing ESS and found that patients’ areas of greatest concern may not align with those perceived by the physician.38 Our study found that while 87% of patients would pursue ESS again and 88% would recommend sinus surgery to someone else, only 60% found that their resolution of symptoms matched their expectations while 22% found this question indeterminate and 19% did not agree that the outcomes of ESS matched their expectations prior to surgery. We have recently studied symptom importance and patient expectations/satisfaction in a subsequent cohort. We found that nasal, smell, and sleep-related symptoms were deemed most important and that meeting pre-operative expectations, and improving those symptoms most important to individual patients may be the most important drivers of satisfaction with the procedure.39
Limitations
Some issues and limitations should be considered when interpreting our data. With 10 year prospective data collection, our follow-up rate was 38% even after substantial attempts were used to contact all patients. This rate is less than our typical published studies with less than 2 years follow-up which approximates 70–80%.2,18,19,40 This long term follow-up rate is humbling and demonstrates the barriers to achieving 10 year prospective longitudinal data in CRS, however it is reasonably consistent with other published reports by Hopkins et al. (52% for 5 year follow-up),7 White et al. (22.5% for 10 year follow-up),10 Senior et al. (60% for 7.8 year follow-up).5 Given these follow-up rates, the reader should consider the possibility of follow-up bias in all of these studies. We performed a baseline analysis of patients completing follow-up versus those unaccounted and no baseline differences were observed between those following up and those lost to follow-up. Our results are from a single institution and the sample size is smaller relative to our other published studies. However, our sample size is consistent with the published literature of studies approaching 10 year follow-up including White et al. (n=42)10 and Senior et al. (n=72).5 To date, our study represents the longest-term prospective follow-up study with the largest sample size measuring outcomes in ESS for CRS. However, the sample size limits our ability to perform robust subset analyses. Our data are observational; when evaluating these data, it would be inappropriate to assume that all of the effects seen in this study are related to ESS alone. In fact, it is important to recognize the critical role that long term medical therapy has played in these cases and to consider our lack of understanding of the natural history of long term CRS. Recall bias may be present in our patient expectations/satisfaction results given the extended duration of follow-up. Finally, these patients were treated in a tertiary center by a fellowship trained sinus surgeon and outcomes may not be generalizable to the broad population of patients undergoing sinus surgery.
CONCLUSIONS
We report long term prospective outcomes of ESS for CRS with more than 10 years of follow-up on average. We found that the initial clinically significant postoperative improvements in QOL seen between 6–18 months after ESS are durable with further non-significant improvement over the long term and with more than 75% of patients reporting clinically significant improvement in the long term. ESS followed by long term medical therapy appears to restore HUVs to normal values. Revision surgery rates are 17% over the long term and worse postoperative endoscopy scores within the first 18 months of ESS were associated with higher likelihood of revision surgery within 10 years. CRSwNP accounted for 80% of revision procedures and half of those patients suffered comorbid AERD. However, only 25% of patients with CRSwNP required revision surgery during the long term follow-up period. New onset asthma occurred at a rate of 0.8% / year after ESS during follow-up. A large majority of patients would pursue ESS again and recommend it to other patients considering this treatment option. More research is needed to examine ways to increase long term follow-up rates and in appropriate counseling for patients considering sinus surgery regarding anticipated outcomes. In addition, comparative effectiveness studies examining long term outcomes of medical therapy alone versus ESS combined with continued medical therapy will further improve our understanding of the most appropriate role of ESS in CRS.
Acknowledgments
Funding disclosures: T.L.S., R.J.S., J.C.M., J.A.A. and Z.M.S. were supported for this investigation by a grant from the National Institute on Deafness and Other Communication Disorders (NIDCD), one of the National Institutes of Health, Bethesda, MD., USA (R01 DC005805; Co-PI: T.L.S./Z.M.S.). Public clinical trial registration (www.clinicaltrials.gov) ID# . This funding organization had no involvement in the design or conduct of this study; preparation, review, approval or decision to submit this manuscript for publication. There are no relevant financial disclosures for D.M.B., A.S.D, K.Y.D., or J.L.M.
Footnotes
Potential Conflicts of Interest: None
REFERENCES
- 1.Rosenfeld RM, Piccirillo JF, Chandrasekhar SS, et al. Clinical practice guideline (update): adult sinusitis. Otolaryngol Head Neck Surg 2015; 152(2 Suppl):S1–S39. [DOI] [PubMed] [Google Scholar]
- 2.Smith TL, Litvack JR, Hwang PH, et al. Determinants of outcomes of sinus surgery: a multi-institutional prospective cohort study. Otolaryngol Head Neck Surg 2010; 142(1): 55–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rudmik L, Hopkins C, Peters A, et al. Patient-reported outcome measures for adult chronic rhinosinusitis: A systematic review and quality assessment. J Allergy Clin Immunol 2015; 136(6): 1532–1540. [DOI] [PubMed] [Google Scholar]
- 4.Bhattacharyya N Ambulatory sinus and nasal surgery in the United States: demographics and perioperative outcomes. Laryngoscope 2010; 120(3): 635–638. [DOI] [PubMed] [Google Scholar]
- 5.Senior BA, Kennedy DW, Tanabodee J, et al. Long-term results of functional endoscopic sinus surgery. Laryngoscope 1998; 108(2):151–157. [DOI] [PubMed] [Google Scholar]
- 6.Young J, Frenkiel S, Tewfik MA, Mouadeb DA. Long-term outcome analysis of endoscopic sinus surgery for chronic sinusitis. Am J Rhinol 2007; 21(6):743–747. doi: 10.2500/ajr.2007.21.3108. [DOI] [PubMed] [Google Scholar]
- 7.Hopkins C, Slack R, Lund V, et al. Long-term outcomes from the English national comparative audit of surgery for nasal polyposis and chronic rhinosinusitis. Laryngoscope 2009; 119(12): 2459–2465. [DOI] [PubMed] [Google Scholar]
- 8.Cornet ME, Georgalas C, Reinartz SM, Fokkens WJ. Long-term results of functional endoscopic sinus surgery in children with chronic rhinosinusitis with nasal polyps. Rhinology 2013; 51(4): 328–334. [DOI] [PubMed] [Google Scholar]
- 9.Jiang XJ, Guo XY, Yuan W, et al. Long-term improvements in quality of life after functional endoscopic sinus surgery for adolescents with chronic rhinosinusitis. Acta Otolaryngol 2012; 132(8): 798–802. [DOI] [PubMed] [Google Scholar]
- 10.White LC, Kazi AA, Jang DW, et al. The effect of smoking on quality of life following sinus surgery: 10-year follow-up. ORL J Otorhinolaryngol Relat Spec 2015; 77(1): 39–43. [DOI] [PubMed] [Google Scholar]
- 11.Rudmik L, Mace J, Soler ZM, Smith TL. Long-term utility outcomes in patients undergoing endoscopic sinus surgery. Laryngoscope 2014; 124(1): 19–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Alt JA, Smith TL, Schlosser RJ, et al. Sleep and quality of life improvements after endoscopic sinus surgery in patients with chronic rhinosinusitis. Int Forum Allergy Rhinol 2014; 4(9): 693–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rudmik L, Mace JC, Smith TL. Smoking and endoscopic sinus surgery: does smoking volume contribute to clinical outcome? Int Forum Allergy Rhinol 2011; 1(3): 145–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Litvack JR, Mace J, Smith TL. Role of depression in outcomes of endoscopic sinus surgery. Otolaryngol Head Neck Surg 2011; 144(3): 446–451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Smith TL, Kern R, Palmer JN, et al. Medical therapy vs. surgery for chronic rhinosinusitis: a prospective, multi-institutional study with 1-year follow-up. Int Forum Allergy Rhinol. 2013; 3(1): 4–9. [DOI] [PubMed] [Google Scholar]
- 16.Lanza DC, Kennedy DW. Adult rhinosinusitis defined. Otolaryngol Head Neck Surg 1997; 117(3 Pt 2): S1–7. [DOI] [PubMed] [Google Scholar]
- 17.Soler ZM, Wittenberg E, Schlosser RJ, et al. Health state utility values in patients undergoing endoscopic sinus surgery. Laryngoscope 2011; 121(12): 2672–2678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Clinger JD, Mace JC, Smith TL. Quality-of-life outcomes following multiple revision endoscopic sinus surgery. Int Forum Allergy Rhinol 2012; 2(6): 444–452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rudmik L, Mace J, Smith TL. Low-stage computed tomography chronic rhinosinusitis: what is the role of endoscopic sinus surgery? Laryngoscope 2011; 121(2): 417–421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lund VJ, Mackay IS. Staging in rhinosinusitis. Rhinology 1993; 31(4): 183–184. [PubMed] [Google Scholar]
- 21.Lund VJ, Kennedy DW. Staging for rhinosinusitis. Otolaryngol Head Neck Surg 1997; 117(3 Pt 2): S35–40. [DOI] [PubMed] [Google Scholar]
- 22.Benninger MS, Senior BA. The development of the Rhinosinusitis Disability Index. Arch Otolaryngol Head Neck Surg 1997; 123(11): 1175–1179. [DOI] [PubMed] [Google Scholar]
- 23.Norman GR, Sloan JA, Wyrwich KW. Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Med Care 2003; 41(5): 582–592. [DOI] [PubMed] [Google Scholar]
- 24.Gliklich RE, Metson R. Techniques for outcomes research in chronic sinusitis. Laryngoscope 1995; 105(4 Pt 1): 387–390. [DOI] [PubMed] [Google Scholar]
- 25.Brazier J, Roberts J, Deverill M. The estimation of a preference-based measure of health from the SF-36. J Health Econ 2002; 21(2): 271–291. [DOI] [PubMed] [Google Scholar]
- 26.Walters SJ, Brazier JE. What is the relationship between the minimally important difference and health state utility values? The case of the SF-6D. Health Qual Life Outcomes 2003; 1: 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hanmer J, Lawrence WF, Anderson JP, et al. Report of nationally representative values for the noninstitutionalized US adult population for 7 health-related quality-of-life scores. Med Decis Making 2006; 26(4): 391–400. [DOI] [PubMed] [Google Scholar]
- 28.Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009; 42(2): 377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Smith KA, Orlandi RR, Oakley G, et al. Long-term revision rates for endoscopic sinus surgery. Int Forum Allergy Rhinol 2018. December 20. doi: 10.1002/alr.22264. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Smith TL. The 2017 13th Annual David W. Kennedy, MD, Lecture. The evolution of outcomes in sinus surgery for chronic rhinosinusitis: past, present, and future. Int Forum Allergy Rhinol 2017; 7(12): 1121–1126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rudmik L, Soler ZM, Mace JC, et al. Economic evaluation of endoscopic sinus surgery versus continued medical therapy for refractory chronic rhinosinusitis. Laryngoscope 2015; 125(1): 25–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Scangas GA, Su BM, Remenschneider AK, et al. Cost utility analysis of endoscopic sinus surgery for chronic rhinosinusitis. Int Forum Allergy Rhinol 2016; 6(6): 582–589. [DOI] [PubMed] [Google Scholar]
- 33.DeConde AS, Mace JC, Levy JM, et al. Prevalence of polyp recurrence after endoscopic sinus surgery for chronic rhinosinusitis with nasal polyposis. Laryngoscope 2017; 127(3): 550–555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Schlosser RJ, Storck K, Smith TL, et al. Impact of postoperative endoscopy upon clinical outcomes after endoscopic sinus surgery. Int Forum Allergy Rhinol 2016; 6(2): 115–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Beswick DM, Gray ST, Smith TL. Pharmacological management of chronic rhinosinusitis: current and evolving treatments. Drugs 2017; 77(16): 1713–1721. [DOI] [PubMed] [Google Scholar]
- 36.Benninger MS, Sindwani R, Holy CE, Hopkins C. Impact of medically recalcitrant chronic rhinosinusitis on incidence of asthma. Int Forum Allergy Rhinol 2016; 6(2): 124–129. [DOI] [PubMed] [Google Scholar]
- 37.Neubauer PD, Tabaee A, Schwam ZG, et al. Patient knowledge and expectations in endoscopic sinus surgery. Int Forum Allergy Rhinol 2016; 6(9): 921–925. [DOI] [PubMed] [Google Scholar]
- 38.Yeung JC, Brandt MG, Franklin JH, et al. Preoperative concerns of patients undergoing endoscopic sinus surgery. Int Forum Allergy Rhinol 2014; 4(8): 658–662. [DOI] [PubMed] [Google Scholar]
- 39.Mattos JL, Rudmik L, Schlosser RJ, et al. Symptom importance, patient expectations, and satisfaction in chronic rhinosinusitis. Int Forum Allergy Rhinol 2019; February 12. doi: 10.1002/alr.22309. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.DeConde AS, Mace JC, Alt JA, et al. Comparative effectiveness of medical and surgical therapy on olfaction in chronic rhinosinusitis: a prospective, multi-institutional study. Int Forum Allergy Rhinol 2014; 4(9): 725–733. [DOI] [PMC free article] [PubMed] [Google Scholar]


