Abstract
Objective:
Athletes who return to sport (RTS) after anterior cruciate ligament reconstruction (ACLR) demonstrate persistent biomechanical and neuromuscular deficits of the knee. There is limited evidence on what effect a neuromuscular training (NMT) program has on knee biomechanics in a cohort of athletes with ACLR. Therefore, the primary aim of this study was to quantify the effect of a NMT program on knee biomechanics in a cohort of ACLR athletes. Secondly, the post-training knee biomechanics were compared between the cohort of ACLR and control athletes.
Design:
Cohort study
Setting:
Controlled laboratory setting
Participants:
Eighteen athletes with ACLR and ten control athletes
Interventions:
Neuromuscular training
Main Outcome Measures:
Knee kinematics and kinetics during a double-limb jump-landing task.
Results:
There were no significant interactions (p>0.05) observed for the athletes with ACLR. However, there was a significant main effect of biomechanics testing session (p<0.05) for knee flexion angle and moments; athletes with ACLR demonstrated greater knee flexion angle and lower knee flexion moment during the post-training biomechanics testing session. Post-training comparison between the ACLR and control athletes demonstrated no significant interactions (p>0.05) between the groups. There was a significant main effect of group (p<0.05) for knee frontal angle, as athletes with ACLR landed with greater knee adduction than the control athletes.
Conclusions:
Significant improvements in knee sagittal plane biomechanical measures were observed following the NMT program by the athletes with ACLR. In addition, post-training comparison of the ACLR and control groups demonstrate comparable knee biomechanics.
INTRODUCTION
Young athletes who return to sport following anterior cruciate ligament (ACL) reconstruction (ACLR) have a greater propensity for poor outcomes.1 A systematic review on the current state of play following ACLR indicate that only 65% of ACLR athletes return to their preinjury level of activity and only 55% of these athletes return to competitive level of sports.2 However, the athletes who return to high levels of sport are highly susceptible to a second injury.3–5 The emerging evidence indicates that nearly one in three to four young, active athletes who return to their respective sport will sustain an ACL graft failure or injury to the contralateral ACL after.6, 7 These same ACLR athletes are 30 to 40 times more likely to suffer a second ACL injury than an uninjured counterpart is to sustain their first.5 These consequences pale in comparison to the long-term joint morbidity that a majority of ACLR athletes are confronted with. The early, pre-mature breakdown of the articular cartilage is reported in 50% to 90% of athletes in 10 to 20 years after ACLR.8–10 The etiology of these poor outcomes is possibly related and may be due to the chronic, abnormal movement patterns found in ACLR athletes.7, 11, 12
Deficits in lower extremity biomechanics and neuromuscular control following ACLR are commonly reported in these athletes. A recent systematic review on knee movement patterns during gait found that joint kinematics are on average restored six years following ACLR and other sagittal plane kinetic measures remain lower than a control population, which indicates that normal knee function may not ever be restored.13 Abnormal limb loading strategies are also observed in a range of functional activities including during squatting,14, 15 running,16 and landing7, 17–20 movements. Notably, these residual movement deficits persist at the time that athletes return to activity and are also directly associated with an elevated risk of second ACL injury.7, 21–23 A prospective study that screened ACLR athletes just prior to return of sport identified several hip and knee neuromuscular deficits which went on to predict second ACL injuries with high sensitivity and specificity.7 The pervasive functional deficits in this population indicate that rehabilitation of the athletes back to sport to pre-injury level of health may not be sufficient. This highlights the importance of augmenting post-operative rehabilitation with training programs to address residual movement deficits prior to athletes returning to sport.
The current evidence indicates that neuromuscular training (NMT) programs can address functional deficits in athletes.24 Previous studies that have implemented NMT in populations vulnerable to knee injuries have modified potential biomechanical risk factors, improved neuromuscular control, and decreased ACL injury incidence.25–28 Furthermore, a systematic review and meta-analysis on the effectiveness of ACL injury prevention training programs found strong evidence in support of these programs.26 The pooled estimates from this study found a risk reduction of 52% for female athletes and 85% for male athletes.26 These same benefits from NMT may allow ACLR athletes to safely and effectively return to sport. Ideally, this training program would be implemented at the end stage of rehabilitation or just prior to returning athletes back to sport. However, it is fist important to understand what effect a NMT program has on knee biomechanics in a group of young athletes with ACLR prior to returning to sport. The primary aim of this study was to quantify the effect of a NMT program on knee sagittal (knee flexion angle and moment) and frontal (knee abduction angle and moment) plane angle and moments in a cohort of ACLR athletes since these measures have been implicated in greater risk of ACL injury. Further, we compared the same knee kinematic and kinetic measures between a group of ACLR and control athletes after both groups completed the training program. The hypothesis tested was that the ACLR group and their limbs (involved and uninvolved) would demonstrate greater knee flexion angles, lower frontal plane knee angles, and decreased knee flexion and abduction moments after participation in the NMT program. The second hypothesis tested was that the ACLR group and their limbs would demonstrate sagittal and frontal plane knee angles and moments that were not significantly different than a group of uninjured controls and their limbs (dominant and non-dominant) after NMT.
METHODS
Subjects and Clinical Criteria to Enroll in Study
Eighteen (n=18) ACLR athletes and ten (n=10) uninjured controls were enrolled in this study (Table 1). The study was approved by the university’s Institutional Review Board and written informed consent was received from all athletes. Informed assents and parental permission were provided for athletes who were younger than 18 years old. All of the enrolled ACL-injured athletes in the study received a hamstring tendon autograft during ACLR. Post-operative rehabilitation was completed at the University’s affiliated Sports Medicine clinics. The athletes with ACLR were approximately 8 months (7.7±3.7 months) out from surgery at the beginning of the study. Prior to beginning baseline biomechanics testing, both ACL-injured and uninjured athletes were subject to a bilateral clinical evaluation conducted by a licensed physical therapist or athletic trainer. Clinical exams were performed by licensed physical therapists trained in the clinical examination protocol and criteria to perform the testing session. The purpose of the clinical exam is to ensure the health of the knee of each participant to safely participate in the high demand testing and training. The exam included measurements of active and passive knee joint range of motion, knee joint effusion, isokinetic knee extensor and flexor strength test (Biodex System 3, Biodex, Shirley, NY) at 60 deg/sec, and five continuous bilateral single-leg hops for maximum vertical height. In order to participate in the study, each athlete had to demonstrate: (1) pain free knee range of motion, (2) trace or no knee joint effusion,29 (3) <30% knee extensor strength deficit30, and (4) the willingness to single-leg hop in place without any pain or loss of balance. Athletes who demonstrated biomechanics excessively risky or unsafe (i.e. large medial-lateral knee excursion or little to no knee flexion) during the single-leg hop in place were referred back to their physical therapist.
Table 1:
Demographics of study cohorts. Note, there were no significant difference between groups.
| Group (males/females) | Age (years) | Weight (kg) | Height (m) |
|---|---|---|---|
| ACLR group (M:8; F: 10) | 19.4 ± 7.2 | 72.3 ± 15.4 | 1.68 ± 0.1 |
| Control group (M:4; F:6) | 16.0 ± 3.7 | 73.1 ± 24.4 | 1.66 ± 0.1 |
Biomechanical Testing and Neuromuscular Training
Biomechanical assessment was performed prior to enrollment in the NMT program and directly after completion. During this evaluation, athletes were fitted with 55 retro-reflective markers and performed three successful drop vertical jumps (DVJ) off a 30.5 cm plyometric box onto embedded force plates (Bertec Corp, Columbus, OH). Marker trajectories were sampled at 240Hz by a 12 camera motion-capture system (Motional Analysis Corporation, Santa Rosa, CA), and separate ground reaction force data were collected for each limb at 1200Hz.
Each athlete from the ACLR and control group completed the 12 session NMT program that focused on enhancing trunk stability, increasing and coordinating dynamic lower extremity joint flexion, and optimizing landing mechanics as described in detail by Di Stasi et al.31 The program was administered by study personnel trained specifically in the implementation of the NMT protocol by a licensed physical therapist (SD). These study personnel included athletic trainers, strength and conditioning specialists, physical therapists, and graduate students in the laboratory. In summary, the NMT program included seven separate progressions that involved both unilateral and bilateral lower limb exercises and core control and strengthening work-outs (Table 2). In addition, the seven progressions included 4 phases of increasing difficulty. Readiness to progress from one phase to the next was determined by the clinician or trainer on an exercise-by-exercise basis. Progression was based on the athlete’s ability to demonstrate proper form for at least 80% of the total repetitions.
Table 2:
A summary of the neuromuscular training program
| Exercise Progression | Tasks |
|---|---|
| Single leg hop | Phase I: Single leg lateral hop hold on Airex Mat Phase II: Single leg 90 degree hop hold on Airex Mat Phase III: Single-leg lateral BOSU (round) hop hold Phase IV: Single leg 90 degree Airex hop hold reaction ball catch |
| Single leg anterior | Phase I: Step-hold Phase II: Jump-single-leg hold Phase III: Hop-hold Phase IV: Hop-hop-hold |
| Romanian dead lift | Phase I: Single leg dead lift Phase II: Single leg dead lift on Airex Phase III: Single leg dead lift on Bosu Phase IV: Single leg dead lift with dumbbells |
| Lunge | Phase I: Walking lunges Phase II: Backward lunge walk Phase III: Lunge jumps Phase IV: Scissor jumps |
| Double leg jump | Phase I: Box butt touch Phase II: Squat jumps Phase III: Single tuck jump with hold Phase IV: Double tuck jumps with hold |
| Prone trunk stability | Phase I: Bosu (round) toe-touch swimmers Phase II: Bosu (round) with partner perturbation Phase III: Prone bridge (elbows and knees) hip extension w/ opposed shoulder flexion Phase IV: Prone bridge (elbows and toes) hip extension |
| Lateral trunk flexion | Phase I: Bosu (round) lateral crunch Phase II: box lateral crunch Phase III: Bosu (round) lateral crunch with ball catch Phase IV: Swiss ball lateral crunch |
Data Treatment and Statistical Analysis
Customized software was used to reduce and analyze kinematic and kinetic data. Marker position gaps that were within the 25 consecutive frames during the jump-landing task were filled using a cubic spline function in Cortex, a motion capture software (Cortex version 4.1, Motion Analysis Corp., Santa Rosa, CA). After all the markers were properly labeled and the gaps were filled, these data along with the ground reaction force data were exported to Visual 3D (C-motion Inc. Germantown, MD) where customized static models scaled were first generated to each participant’s anthropometric measurements. Subsequently, the marker position data and ground reaction force data were low-pass filtered using a bi-directional Butterworth filter at 12Hz and 50Hz, respectively. The hip joint centers were determined using a validated, anthropometric calculation32, and a virtual marker was created in post-processing based on the relative location of the calculated hip joint center to other markers on the pelvis segment. All data were time-normalized to 100% of stance. Cardan-Euler sequence for local coordinated systems (X-Y-Z) was used to calculated kinematic variables and inverse dynamics was used to calculate kinetic variables. Initial contact (IC) was defined when the vertical component of the ground reaction force exceeded 10N. The kinematic and kinetic calculations were processed using custom codes in Visual 3D and Matlab (Mathworks Inc Natick, MA).
The analysis of knee kinematic and kinetic variables was focused on initial contact and peak. Initial contact is of interest because injuries have been demonstrated to occur within approximately 20–50 milliseconds of landing.33 Repeated measures analysis of variance (ANOVA) was performed to assess interactions and main effects of session (pre- and post-training) and limb (involved/dominant and uninvolved/non-dominant) to understand the effects of NMT in the ACLR cohort. A two-way ANOVA was used to assess the interactions of group (ACLR vs control) and limb following the NMT intervention. Post-hoc paired and independent t-tests were used to test for significant differences between limb and session, and groups, respectively. Limb symmetry index ((LSI=involved/uninvolved)*100) was calculated for sagittal plane kinematic and kinetic variables during initial contact and peak for the athletes with ACLR prior to and after training. Paired t-tests were used to compare average LSI of athletes with ACLR prior to participating in the training and after completing the training program. The alpha level was set to 0.05 a priori to determine significant results.
RESULTS
Effect of NMT on Knee Biomechanics in ACLR Cohort
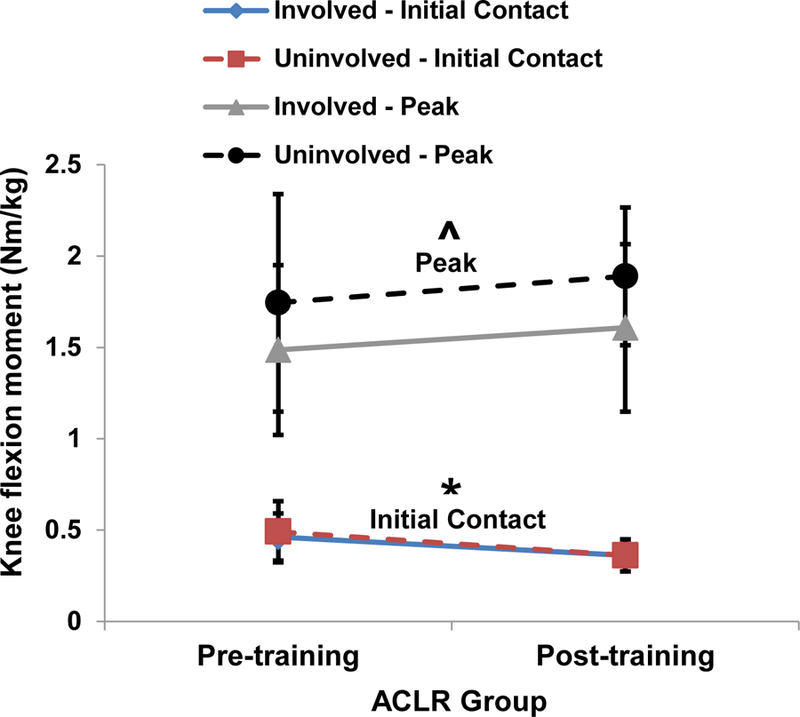
There were no significant interactions (p>0.05) between session and limb for knee flexion angle at initial contact (Figure 2), knee flexion moment initial contact (Figure 3), knee abduction angle at initial contact (Figure 4), and knee abduction moment at initial contact (Figure 5). A significant main effect of session was observed for knee flexion angle at initial contact (p=0.001; Figure 2) and knee flexion moment at initial contact (p=0.008; Figure 3). The ACLR group landed with greater knee flexion angle at initial contact (pre-training: 17.2±7.1 degrees; post-training: 24.3º±9.04 degrees) and lower knee flexion moment at initial contact (pre-training: 0.48 ± 0.14 Nm/kg; post-training: 0.36±0.10 Nm/kg) after participating in the NMT program. There were no significant main effects (p>0.05) observed for knee abduction angle at initial contact and knee abduction moment at initial contact.
Figure 2:
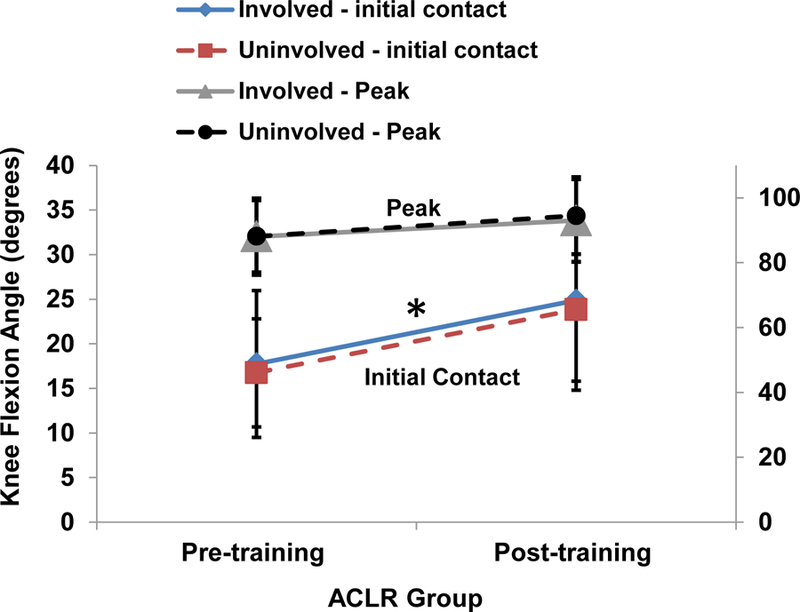
Changes in knee flexion angle at initial contact from pre- to post-training for the ACLR group.
Figure 3:
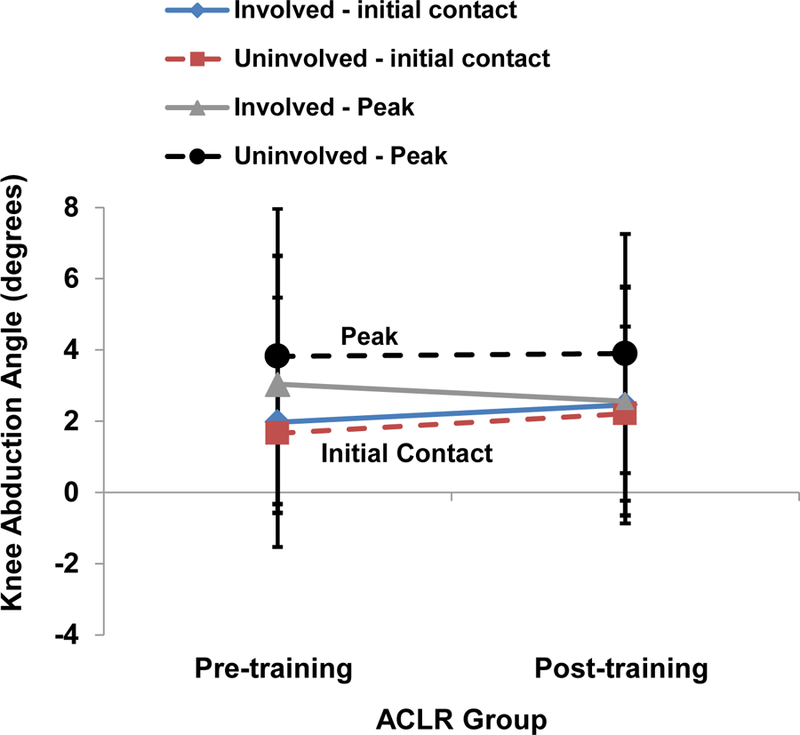
Changes in knee abduction angle at initial contact from pre- to post-training for the ACLR group.
Figure 4:
Changes in knee flexion moment at initial contact from pre to post-training for the ACLR group.
Figure 5:
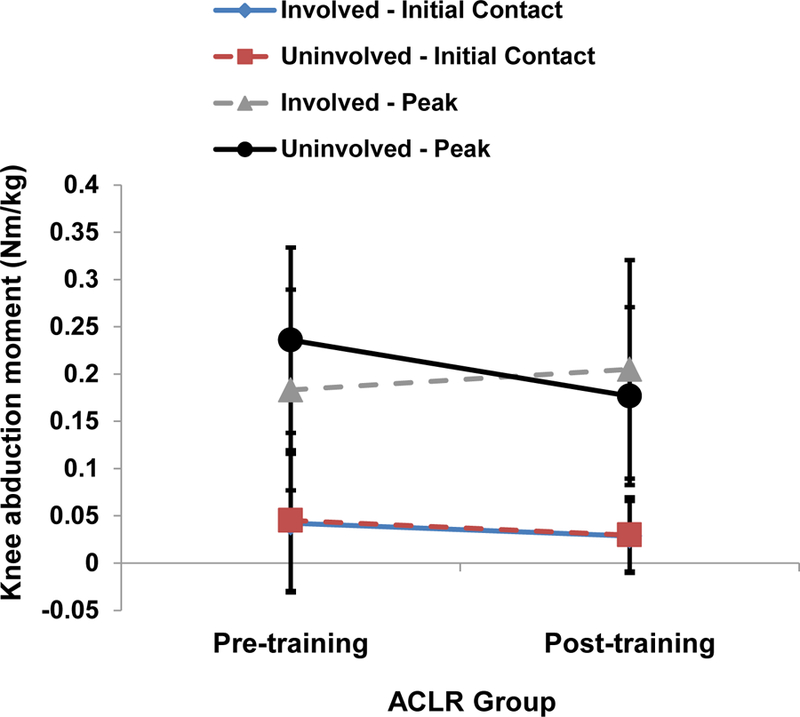
Changes in knee abduction moment at initial contact from pre to post-training for the ACLR group.
There were no significant interactions (p>0.05) for peak knee flexion angle, peak knee abduction angle, peak knee flexion moment, and peak knee abduction moment. A significant main effect of limb was observed for peak knee flexion moment (p=0.005). The uninvolved limbs (1.82±0.1 Nm/kg) demonstrated greater peak knee flexion moment than the involved limbs (1.55±0.01 Nm/kg). Otherwise, there were no significant main effects (p>0.05) or session or limb for peak flexion angle, peak knee abduction angle, and peak knee abduction moment.
There were no significant changes (p>0.05) in LSI from pre- to post-training for knee flexion angle at initial contact (pre-training: 107.0±35.7; post-training: 108.0±32.1; p=0.47), peak knee flexion angle (pre-training: 100.1±4.28; post-training: 98.5±3.5; p=0.11), knee flexion moment at initial contact (pre-training: 98.3±22.0; post-training: 102.8±18.4; p=0.28), and peak knee flexion moment (pre-training: 92.1±39.2; post-training: 85.6±18.5; p=0.27).
Post-NMT Comparison: Athletes post-ACLR vs. Controls
There were no significant interactions (p>0.05) between the factors group and limb for knee flexion angle, knee flexion moment, knee abduction angle, and knee abduction moment. A significant main effect of group was observed for knee frontal plane angle (p=0.002). The control group (post-training: 2.33±2.8 degrees) demonstrated a larger knee abduction angle than the ACLR group (post-training: −0.24±2.77 degrees). There was no significant main effect (p>0.05) of group or limb for the other biomechanical variables.
There were no significant interactions or main effects (p>0.05) between the factors group and limb for peak flexion angle, peak abduction angle, peak flexion moment, and peak abduction moment. Table 3 displays a summary of the post-training knee kinematic and kinetic variables for the ACLR and Control groups.
Table 3:
Post-training knee kinematic and kinetic variables of the ACLR and Control Group
| ACLR Group | Control Group | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Variables (angles: degrees moments: Nm/Kg) | Post-training Involved | Post-training Uninvolved | Post-Training Involved | Post-Training Uninvolved | Interactions/Main effects & P-values | |||||
| Knee flexion angle (initial contact & peak) | 24.9 ± 9.0 | 93.0 ± 11.9 | 23.8 ± 9.0 | 94.5 ± 12.7 | 22.0 ± 8.0 | 92.8 ± 9.7 | 23.5 ± 7.0 | 93.2 ± 9.8 | ||
| Knee abduction angle (initial contact & peak) | *2.4 ± 3.3 | 2.6 ± 3.2 | *2.2 ± 2.4 | 3.9 ± 3.4 | *−0.6 ± 2.5 | 4.4 ± 2.0 | *0.17 ± 3.2 | 5..6 ± 4.0 | *Main effect of group: p=0.002 | |
| Knee flexion moment (initial contact & peak) | 0.36 ± 0.05 | 1.61 ± 0.5 | 0.36 ± 0.08 | 1.89 ± 0.4 | 0.33 ± 0.08 | 1.82 ± 0.3 | 0.31 ± 0.07 | 1.70 ± 0.4 | ||
| Knee abduction moment (initial contact & peak) | 0.03 ± 0.04 | 0.20 ± 0.1 | 0.03 ± 0.04 | 0.18 ± 0.1 | 0.02 ± 0.02 | 0.24 ± 0.12 | 0.003 ± 0.03 | 0.23 ± 0.1 | ||
DISCUSSION
The athletes with ACLR demonstrated a significant improvement in sagittal plane knee biomechanics after completing the NMT program. The post-training comparison of knee biomechanics between the control and ACLR groups demonstrated comparable knee biomechanics. Participation in such training programs continues to be beneficial for populations vulnerable to lower extremity injury. Previous research on the efficacy of NMT programs has largely focused on uninjured athletes. However, in this study, we demonstrated that these training programs may augment athletes recovering from devastating knee injuries such as an ACL tear prior to returning to activity. Stiff kinematic and kinetic landing strategies in prospective biomechanical studies have shown to increase the risk of ACL injuries.34–37 The improvement of athletes with ACLR athletes who landed with greater knee flexion angle and less knee flexion moment after participating in the training program may help mitigate their risk of future ACL injury. The current literature contains limited evidence of the use of a NMT program in ACLR athletes to improve biomechanics and neuromuscular control. Recent studies have investigated the use of perturbation training, a particular type of NMT focused on eliciting coordinated muscle responses to surface perturbations, to resolve impairments in ACL-injured or ACLR athletes. Failla and colleagues38 compared the functional outcomes 2 years after ACLR in a cohort that underwent preoperative rehabilitation which included NMT and progressive strengthening with a non-experimental group. The group that was treated with the NMT and strength training preoperatively had greater functional outcomes as measured by the International Knee Documentation Committee (IKDC) subjective knee form and Knee Injury and Osteoarthritis Outcomes Score (KOOS) and return to sport rates 2 years following ACLR.38 In addition, recent reports from the Anterior Cruciate Ligament-Specialised Post-Operative Return to Sports trial, a single-blinded randomized clinical study of secondary prevention and return to sport, found similar outcomes for individual that were either randomized into the strengthening, agility, and secondary prevention (SAP) protocol or the SAP plus additional perturbation training (SAP+PERT).39, 40 Importantly, this secondary injury program is a combination of strengthening and movement training, including plyometric and agility exercises.39 From these studies, Arundale et al.39 found few differences in men assigned to either SAP or SAP+PERT in measures of quadriceps strength symmetry, single-legged hopping, and patient-reported outcomes. Capin et al.40 found that in the same group of men the SAP or the SAP+PERT group did not restore gait symmetry 1 or 2 years after ACLR. However, improvements in gait asymmetries were observed in this cohort between 1 and 2 years. The early evidence in the literature suggests that a training program the current data from this study suggest the potential role of NMT programs to improve self-reported outcomes and landing biomechanics.
Notably, the hypothesis that a significant change in frontal plane kinematics and kinetics would occur in the ACLR group after the NMT program was not supported. This is an unexpected finding because the NMT program was designed to target the frontal plane collapse of the knee during a jump-landing task. Increased knee valgus during a DVJ has been shown to be directly implicated in both primary and secondary ACL injury.36 The absence of significant measurable changes in the frontal plane after NMT may be due to the patient selection process. The study implemented strenuous clinical criteria to ensure participant safety, and we recognize this may have selectively biased our cohort of study to the highest functioning individuals post-ACLR. A part of the clinical criteria to participate in the study was that the athlete should demonstrate safe single-leg hopping in place without deleterious landing strategies. Athletes who demonstrated the deleterious medial collapse of the knee during the jumping task were excluded due to its association to increased risk of second ACL injury. Therefore, this ACLR cohort included athletes who already demonstrated frontal plane control of the knee. In addition, the ACLR athletes completed post-operative rehabilitation within the institution’s physical therapy department which practices evidence-based rehabilitation guidelines and addresses neuromuscular control of the knee within the frontal plane. These factors may have confounded the effect of training on knee frontal plane biomechanics. Regardless, the ACLR athletes still demonstrated an improvement in knee biomechanics after completing a NMT program prior to returning to sport.
There are a few limitations to the current study. There was a limited size within the control group. However, the literature has already shown that NMT is effective in modifying landing biomechanics in uninjured athletes. The aim was to demonstrate that the ACLR athletes after participating in the NMT are comparable to a group of control athletes who completed the same training program. Again, the strict clinical criteria to participate in the study may have restricted us from selecting some athletes who would have greatly benefited from the NMT. However, our first priority was the safety of the athletes and to perform some of the dynamic movements involved in the training the athletes were required to demonstrate some baseline health. The only requirement for the athletes participating in the study was to complete 12 training sessions. Therefore, the athletes did not complete all exercises within the training program. The decision to advance the athlete was made by the trainer and was based on their judgement of the athlete demonstrating proper technique of the exercise for at least three sets. Because of this performance based advancement, not all the athletes were at the same performance level at the end of the training program. Regardless, these athletes demonstrated improvement in landing biomechanics. Additionally, another control that will be considered in future studies is an ACLR group without any training because it is important to consider that individuals after ACLR might demonstrate improvements over time.
CONCLUSION
The purposes of this study were to: (1) investigate the effects of a NMT program on knee biomechanics in a cohort of ACLR athletes prior to returning to sport and (2) compare the post-training knee biomechanics of the ACLR cohort to a control cohort who also completed the same NMT program. The high-functioning ACLR group demonstrated an improvement in sagittal plane knee biomechanics and neuromuscular control after participation in the NMT program. Further, following the training the group of ACLR athletes demonstrated similar knee biomechanics and neuromuscular control to a group of uninjured, control athletes. Movement impairments may be the last of the residual deficits to normalize after ACLR and some athletes may never regain normal knee function.41 Recently, evidence in the literature has highlighted that those athletes may who wait to return to pre-injury level of activity until at least 9 months post-ACLR may mitigate their risk of second ACL injury.41, 42 A structured NMT program that exclusively focuses on improving biomechanics and neuromuscular control may remediate these aberrant movement patterns. Future work will be required to understand if NMT in the ACLR population mitigates the risk of a second ACL injury rates, and how it compares against strength training and home-based exercise programs.
Figure 1:
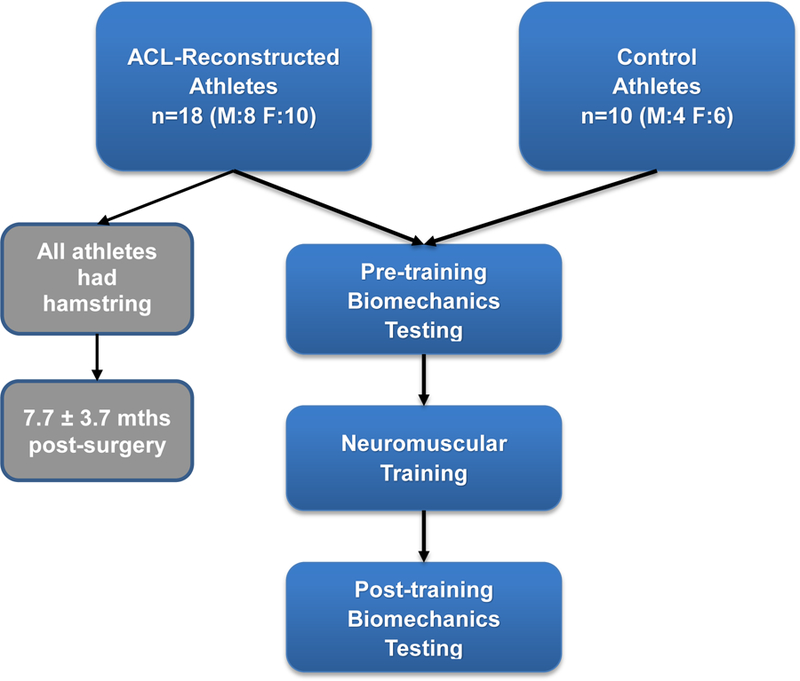
Flowchart of participants and study progression.
ACKNOWLEDGEMENTS:
The authors would like to thank the researchers and staff at The Ohio State University for their support with data collection. We acknowledge support from the National Institute of Arthritis and Musculoskeletal and Skin Diseases: T32AR56950 for CVN and R01AR056259 and R01AR055563 to TEH. We also acknowledge support from the Sports Physical Therapy Section of the American Physical Therapy Association.
FUNDING: We acknowledge support from the Sports Physical Therapy Section of the American Physical Therapy Association. We acknowledge CVN was supported by T32AR56680 and R01AR056259 and R01AR055563 to TEH.
Footnotes
ETHICAL CONSIDERATIONS
There are no ethical considerations for this particular study.
REFERENCES
- 1.Hewett TE, Di Stasi SL, Myer GD. Current concepts for injury prevention in athletes after anterior cruciate ligament reconstruction. Am J Sports Med 2013;41(1):216–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ardern CL, Taylor NF, Feller JA, et al. Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br J Sports Med 2014;48(21):1543–1552. [DOI] [PubMed] [Google Scholar]
- 3.Webster KE, Feller JA, Leigh WB, et al. Younger patients are at increased risk for graft rupture and contralateral injury after anterior cruciate ligament reconstruction. Am J Sports Med 2014;42(3):641–647. [DOI] [PubMed] [Google Scholar]
- 4.Lind M, Menhert F, Pedersen AB. Incidence and outcome after revision anterior cruciate ligament reconstruction: results from the Danish registry for knee ligament reconstructions. Am J Sports Med 2012;40(7):1551–1557. [DOI] [PubMed] [Google Scholar]
- 5.Wiggins AJ, Grandhi RK, Schneider DK, et al. Risk of secondary injury in younger athletes after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Am J Sports Med 2016;44(7):1861–1876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Allen MM, Pareek A, Krych AJ, et al. Are female soccer players at an increased risk of second anterior cruciate ligament injury compared with their athletic peers? Am J Sports Med 2016. [DOI] [PubMed]
- 7.Paterno MV, Schmitt LC, Ford KR, et al. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med 2010;38(10):1968–1978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Myklebust G, Holm I, Maehlum S, et al. Clinical, functional, and radiologic outcome in team handball players 6 to 11 years after anterior cruciate ligament injury: a follow-up study. Am J Sports Med 2003;31(6):981–989. [DOI] [PubMed] [Google Scholar]
- 9.Lohmander LS, Ostenberg A, Englund M, et al. High prevalence of knee osteoarthritis, pain, and functional limitations in female soccer players twelve years after anterior cruciate ligament injury. Arthritis Rheum 2004;50(10):3145–3152. [DOI] [PubMed] [Google Scholar]
- 10.Daniel DM, Stone ML, Dobson BE, et al. Fate of the ACL-injured patient. A prospective outcome study. Am J Sports Med 1994;22(5):632–644. [DOI] [PubMed] [Google Scholar]
- 11.Andriacchi TP, Mundermann A, Smith RL, et al. A framework for the in vivo pathomechanics of osteoarthritis at the knee. Ann Biomed Eng 2004;32(3):447–457. [DOI] [PubMed] [Google Scholar]
- 12.Chaudhari AM, Briant PL, Bevill SL, et al. Knee kinematics, cartilage morphology, and osteoarthritis after ACL injury. Med Sci Sports Exerc 2008;40(2):215–222. [DOI] [PubMed] [Google Scholar]
- 13.Kaur M, Ribeiro DC, Theis JC, et al. Movement Patterns of the Knee During Gait Following ACL Reconstruction: A Systematic Review and Meta-Analysis. Sports Med 2016;46(12):1869–1895. [DOI] [PubMed] [Google Scholar]
- 14.Neitzel JA, Kernozek TW, Davies GJ. Loading response following anterior cruciate ligament reconstruction during the parallel squat exercise. Clin Biomech (Bristol, Avon) 2002;17(7):551–554. [DOI] [PubMed] [Google Scholar]
- 15.Salem GJ, Salinas R, Harding FV. Bilateral kinematic and kinetic analysis of the squat exercise after anterior cruciate ligament reconstruction. Arch Phys Med Rehabil 2003;84(8):1211–1216. [DOI] [PubMed] [Google Scholar]
- 16.Hoshino Y, Fu FH, Irrgang JJ, et al. Can joint contact dynamics be restored by anterior cruciate ligament reconstruction? Clin Orthop Relat Res 2013;471(9):2924–2931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Paterno MV, Schmitt LC, Ford KR, et al. Effects of sex on compensatory landing strategies upon return to sport after anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther 2011;41(8):553–559. [DOI] [PubMed] [Google Scholar]
- 18.Paterno MV, Ford KR, Myer GD, et al. Limb asymmetries in landing and jumping 2 years following anterior cruciate ligament reconstruction. Clin J Sport Med 2007;17(4):258–262. [DOI] [PubMed] [Google Scholar]
- 19.Orishimo KF, Kremenic IJ, Mullaney MJ, et al. Adaptations in single-leg hop biomechanics following anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 2010;18(11):1587–1593. [DOI] [PubMed] [Google Scholar]
- 20.Gokeler A, Hof AL, Arnold MP, et al. Abnormal landing strategies after ACL reconstruction. Scand J Med Sci Sports 2010;20(1):e12–19. [DOI] [PubMed] [Google Scholar]
- 21.Schmitt LC, Paterno MV, Ford KR, et al. Strength asymmetry and landing mechanics at return to sport after anterior cruciate ligament reconstruction. Med Sci Sports Exerc 2015;47(7):1426–1434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schmitt LC, Paterno MV, Hewett TE. The impact of quadriceps femoris strength asymmetry on functional performance at return to sport following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther 2012;42(9):750–759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ithurburn MP, Paterno MV, Ford KR, et al. Young Athletes With Quadriceps Femoris Strength Asymmetry at Return to Sport After Anterior Cruciate Ligament Reconstruction Demonstrate Asymmetric Single-Leg Drop-Landing Mechanics. Am J Sports Med 2015;43(11):2727–2737. [DOI] [PubMed] [Google Scholar]
- 24.Hewett TE, Ford KR, Myer GD. Anterior Cruciate Ligament Injuries in Female Athletes Part 2, A Meta-analysis of Neuromuscular Interventions Aimed at Injury Prevention. The American Journal of Sports Medicine 2006;34(3):490–498. [DOI] [PubMed] [Google Scholar]
- 25.Hewett TE, Stroupe AL, Nance TA, et al. Plyometric Training in Female Athletes Decreased Impact Forces and Increased Hamstring Torques. The American Journal of Sports Medicine 1996;24(6):765–773. [DOI] [PubMed] [Google Scholar]
- 26.Sadoghi P, von Keudell A, Vavken P. Effectiveness of anterior cruciate ligament injury prevention training programs. J Bone Joint Surg Am 2012;94(9):769–776. [DOI] [PubMed] [Google Scholar]
- 27.Myer GD, Ford KR, Palumbo JP, et al. Neuromuscular training improves performance and lower-extremity biomechanics in female athletes. J Strength Cond Res 2005;19(1):51–60. [DOI] [PubMed] [Google Scholar]
- 28.Myklebust G, Engebretsen L, Braekken IH, et al. Prevention of anterior cruciate ligament injuries in female team handball players: a prospective intervention study over three seasons. Clin J Sport Med 2003;13(2):71–78. [DOI] [PubMed] [Google Scholar]
- 29.Sturgill LP, Snyder-Mackler L, Manal TJ, et al. Interrater reliability of a clinical scale to assess knee joint effusion. J Orthop Sports Phys Ther 2009;39(12):845–849. [DOI] [PubMed] [Google Scholar]
- 30.Adams D, Logerstedt DS, Hunter-Giordano A, et al. Current concepts for anterior cruciate ligament reconstruction: a criterion-based rehabilitation progression. J Orthop Sports Phys Ther 2012;42(7):601–614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Di Stasi S, Myer GD, Hewett TE. Neuromuscular training to target deficits associated with second anterior cruciate ligament injury. J Orthop Sports Phys Ther 2013;43(11):777–792, a771–711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bell AL, Brand RA, Pedersen DR. Prediction of hip joint centre location from external landmarks. Human Movement Science 1989;8(1):3–16. [Google Scholar]
- 33.Krosshaug T, Nakamae A, Boden BP, et al. Mechanisms of anterior cruciate ligament injury in basketball: video analysis of 39 cases. Am J Sports Med 2007;35(3):359–367. [DOI] [PubMed] [Google Scholar]
- 34.Leppanen M, Pasanen K, Krosshaug T, et al. Sagittal Plane Hip, Knee, and Ankle Biomechanics and the Risk of Anterior Cruciate Ligament Injury: A Prospective Study. Orthop J Sports Med 2017;5(12):2325967117745487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Leppanen M, Pasanen K, Kujala UM, et al. Stiff Landings Are Associated With Increased ACL Injury Risk in Young Female Basketball and Floorball Players. Am J Sports Med 2017;45(2):386–393. [DOI] [PubMed] [Google Scholar]
- 36.Hewett TE, Myer GD, Ford KR, et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. Am J Sports Med 2005;33(4):492–501. [DOI] [PubMed] [Google Scholar]
- 37.Padua DA, DiStefano LJ, Beutler AI, et al. The Landing Error Scoring System as a Screening Tool for an Anterior Cruciate Ligament Injury-Prevention Program in Elite-Youth Soccer Athletes. J Athl Train 2015;50(6):589–595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Failla MJ, Logerstedt DS, Grindem H, et al. Does Extended Preoperative Rehabilitation Influence Outcomes 2 Years After ACL Reconstruction? A Comparative Effectiveness Study Between the MOON and Delaware-Oslo ACL Cohorts. Am J Sports Med 2016;44(10):2608–2614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Arundale AJ, Cummer K, Capin JJ, et al. Report of the Clinical and Functional Primary Outcomes in Men of the ACL-SPORTS Trial: Similar Outcomes in Men Receiving Secondary Prevention With and Without Perturbation Training 1 and 2 Years After ACL Reconstruction. Clin Orthop Relat Res 2017. [DOI] [PMC free article] [PubMed]
- 40.Capin JJ, Zarzycki R, Arundale A, et al. Report of the Primary Outcomes for Gait Mechanics in Men of the ACL-SPORTS Trial: Secondary Prevention With and Without Perturbation Training Does Not Restore Gait Symmetry in Men 1 or 2 Years After ACL Reconstruction. Clin Orthop Relat Res 2017. [DOI] [PMC free article] [PubMed]
- 41.Nagelli CV, Hewett TE. Should Return to Sport be Delayed Until 2 Years After Anterior Cruciate Ligament Reconstruction? Biological and Functional Considerations. Sports Med 2017;47(2):221–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Grindem H, Snyder-Mackler L, Moksnes H, et al. Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: the Delaware-Oslo ACL cohort study. Br J Sports Med 2016;50(13):804–808. [DOI] [PMC free article] [PubMed] [Google Scholar]


