Abstract
Objective:
This study examined the degree to which the parent-child relationship uniquely predicted clinical outcomes in externalizing problems and adaptive skills in children meeting diagnostic criteria for oppositional defiant disorder and whether facets of this relationship moderated the effects of two unique psychosocial treatments.
Method:
We recruited 134 children and their parents (38.06% female, M age = 9.52 years, range 7–14; 83.58% white). Families were randomly assigned to one of two treatments: Parent Management Training (PMT; Barkley, 1997) and Collaborative and Proactive Solutions (CPS; Greene, 1998). We formed principal components from pre-treatment reports and behaviors of the parent-child relationship to predict within- and between-family outcomes in children’s externalizing problems and adaptive skills.
Results:
Four principal components were supported (parental warmth, parental monitoring, family hostility, and family permissiveness). Parental monitoring predicted fewer externalizing problems, whereas family permissiveness predicted more externalizing problems. Parental warmth predicted greatest improvements in children’s adaptive skills among families receiving PMT. Family hostility predicted more externalizing problems and poorer adaptive skills for children; however, families receiving CPS were buffered from the negative effect of family hostility on adaptive skills.
Conclusions:
The parent-child relationship can uniquely inform post-treatment outcomes following treatment for ODD. Certain treatment approaches may better fit unique relationships that emphasize warmth and/or hostility, allowing clinicians to anticipate and tailor treatments to families.
Keywords: Parenting, Intrusiveness, Rejection, Hierarchical Linear Modeling
Externalizing Problems among Children with ODD
Oppositional defiant disorder (ODD) is a childhood externalizing disorder characterized by disruptive and noncompliant behaviors that include loss of temper, defiance, and spiteful and vindictive behaviors (APA, 2013). These challenging behaviors have serious implications for children’s adaptive functioning at home, school, and with friends (see Burke, Loeber, & Birmaher, 2002; Murrihy, Kidman, & Ollendick, 2010) and place children at risk for the development of severe problems related to conduct disorder and mood disorders (Loeber, Burke, Lahey, Winters, & Zera, 2000; Loeber et al., 1998). Various evidence-based treatments have proven effective for reducing the behaviors associated with ODD (see Eyberg, Nelson, & Boggs, 2008; Murrihy et al., 2010). However, response to these treatments has been wide-ranging and highly individualized. As such, researchers have examined moderators of treatment outcomes, including parenting styles (e.g., Burke et al., 2002) and the broader relationships between children and their parents (Booker, Ollendick, Dunsmore, & Greene, 2016). Despite these efforts, questions remain regarding the ways the parent-child relationship informs a family’s compatibility with treatment approaches addressing ODD symptoms.
Adaptive Skills among Children with ODD
Children meeting diagnostic criteria for ODD have been shown to be lacking skills in multiple areas, including executive functioning skills, language processing and communication skills, emotion regulation skills, and social skills (Aebi et al., 2010; Dunsmore, Booker, & Ollendick, 2013; Greene et al., 2002; Hamilton & Armando, 2008). These lagging skills make it difficult for these youth to have adaptive social interactions and manage experiences of frustration that, in turn, increase the likelihood of rejection from peers and conflict with family members (APA, 2013; Burke et al., 2002; Burke, Pardini, & Loeber, 2008; Tung & Lee, 2014). Hence, these children face a challenging cycle where they lack the skills to relate with others and also receive fewer opportunities to improve these skills. Effective treatment has the potential to not only decrease the problematic behaviors associated with ODD but also to improve these crucial skills so as to permit these children to engage more adaptively with peers and caregivers.
The Parent-Child Relationship and Implications for Clinical Outcomes
Studies have shown that parents of children diagnosed with ODD are more likely to be critical, cold, rejecting, and to possess less supportive styles of parenting (Brown, Granero, & Ezpeleta, 2017; Burke et al., 2008; Nixon, Sweeney, Erickson, & Touyz, 2003; Pike, McGuire, Hetherington, Reiss, & Plomin, 1996). For example, parental intrusiveness—including unsolicited involvement in moments of frustration—is linked with more ODD symptoms in children (Hudson & Rapee, 2001; Kashdan et al., 2004). Further, harsh and ineffective parenting, including forms of rejection and dismissal of children’s emotional distress, is linked with increased oppositional symptoms (Hentges, Shaw, & Wang, 2017; Tung & Lee, 2014). In sum, a variety of negative parent-child relationship factors have been shown to place children at greater risk for oppositional problems (Barkley & Robin, 2014; Greene et al., 2002). Alternatively, warm and responsive parenting is considered to be a protective factor in the development of ODD in youth (Clark & Frick, 2016; Kashdan et al., 2004; Loeber, Burke, & Pardini, 2009). Indeed, presence of parental warmth has shown immediate and enduring benefits for children in community and clinical samples (e.g., de Haan, Deković, van den Akker, Stoltz, & Prinzie, 2013).
Significant heterogeneity in family interactions have been reported in families seeking treatment for behavior problems (Booker et al., 2016; Hawes, Price, & Dadds, 2014). Parents may enter treatment varying widely in the extent that they exhibit approaches of warmth, rejection, and intrusiveness. Such differences could impact post-treatment outcomes among these treatment-seeking families.
The Parent-Child Relationship and Treatment Compatibility
The fit or match between parental characteristics and psychosocial treatment has been referred to as parent-treatment compatibility (Greene & Doyle, 1998). Simply stated, families may enter treatment with parent-child relationship characteristics that are more or less compatible with specific treatments and/or which might be better or poorly addressed by specific treatments. Two treatments were examined in this study: Parent Management Training (PMT) and Collaborative and Proactive Solutions (CPS). PMT, sometimes referred to as “behavioral parent training,” aims to teach parents how to develop and implement structured contingency management programs with the primary focus of treatment being the decrease in disruptive behavior and the increase in child compliance. PMT’s treatment focus includes the use of direct and clear commands, differential attention, one-on-one time to increase positive reinforcement for prosocial child behaviors, and timeout from reinforcement for negative child behaviors (e.g., Barkley, 1997; Kazdin, 2005; Murrihy et al., 2010). PMT has been evaluated in randomized control trials (RCTs) for youth aged 2–14 and has shown considerable efficacy (Kazdin, 2017; Murrihy et al., 2010). PMT also results in significant declines in parenting stress and parent dysfunction, which are important factors that contribute to healthier parent-child relations (Kazdin, 2017). Furthermore, PMT has resulted in comparable results in “real world” clinical practice settings (Michaelson, Davenport, Barlow, & Day, 2013). Still, PMT has been characterized by some noteworthy limitations. For example, children with deviant behavior are still above the range of normative levels following treatment, treatment effects dissipate once treatment is removed, and there is some evidence that older youth and adolescents might not benefit as readily from such treatment (Frick, 2001; Kazdin, 2005; Ollendick et al., 2016). Despite these limitations, PMT is regarded as the gold standard for treating youth with ODD (Murrihy et al., 2010).
Collaborative and Proactive Solutions (CPS; Greene, 1998, 2010) focuses instead on helping parents and children collaboratively and proactively solve the problems that are contributing to behavior problems. In brief, CPS emphasizes the role of lagging skills (e.g., flexibility, problem solving, and adaptability) which contribute to the development and maintenance of ODD symptoms. CPS has demonstrated comparable efficacy to PMT in at least one large randomized clinical trial, resulting in significant reductions in aggressive and oppositional behaviors (Ollendick et al., 2016). In a second randomized clinical trial, CPS was shown to improve the quality of parent-child relationships, decrease parenting stress, and reduce problematic behaviors in the home (Greene et al., 2004), and there was some suggestion that the effects of CPS were more durable as compared to PMT.
The Current Study
In a secondary analysis of data involving families seeking treatment for their child’s ODD symptoms, we examined ways the parent-child relationship predicted post-treatment clinical outcomes in children diagnosed with ODD. In doing so, we addressed two major questions. First, can we predict improvements in externalizing problems and adaptive skills given multiple facets of the parent-child relationship? Second, do some facets of the parent-child interaction predict better clinical outcomes in the context of certain clinical treatments?
We hypothesized that facets of the parent-child relationship involving greater warmth (i.e., parental involvement), less rejection (i.e., family rejection), and less intrusiveness (i.e., family intrusiveness) would predict larger improvements in externalizing problems and adaptive skills following both treatments. Interactions were tested given assignment to PMT or CPS. For these interactions, specific hypotheses were not generated. However, we undertook these analyses to explore the possibility that one treatment would work better when families entered treatment incorporating warmth, rejection, and/or intrusiveness. If interactions were supported, such findings could inform ongoing efforts to improve “personalized” interventions and recommendations for some families. Finding ways to improve the potential responsiveness to treatments to ODD remains important and sought out by the field, as current approaches to treating these problems in youth and their families result in only about 45–55% of symptom improvement (Jones et al., 2013; Kimonis & Fleming, 2018; Ollendick et al., 2016). Hence, the current study focused not only on the implications of the parent-child relationship for clinical outcomes, but ways such approaches could further inform response given specific treatment assignment.
Method
Participants
Participants were 134 children and adolescents (M age = 9.52 years, SD = 1.77, range 7–14; 38.06% female) and their parents who were referred by university-affiliated clinics, print advertisements, mental health professionals, pediatricians, and local schools to participate in a randomized clinical control trial (RCT; citation omitted for masked review). Most families identified children’s ethnicities as White (83.58%), followed by families identifying as Black (7.46%), Hispanic (5.22%), and Asian American (1.48%). Mean mother age was 39.77 years (SD = 6.67) and mean father age was 42.21 years (SD = 7.78). Most parents had completed high school (96.27–97.01%), and a large proportion of parents had completed a four-year college degree (38.05–55.97%). While the range of family incomes varied widely, the mean income indicated the sample was typically upper-middle class (M = $66,781.96, SD = 38,215.70). Inclusion criteria for the study were as follows: a) participants were between the ages of 7.00-to-14.00 years of age; and b) youth met DSM-IV criteria for ODD, as established by a semi-structured diagnostic interview (see below). Exclusion criteria included a diagnosis of intellectual disability, autism spectrum disorder, and/or psychosis, as determined by parent report during a telephone screener. Although co-occurring psychological disorders were present in the sample, clinically significant ODD symptoms were the presenting problem in all cases.
Procedure
Following a telephone screener to determine eligibility, youth and their parents participated in two pre-treatment assessment sessions. Assent and consent were obtained during the first pre-treatment assessment session. During the pre-treatment assessment, parents and children completed two separate semi-structured diagnostic interviews (The Anxiety Disorders Interview Schedule for DSM-IV-Child and Parent Versions (ADIS-IV-C/P; Silverman & Albano, 1996) administered by trained doctoral level clinical psychology students. Diagnoses were based on the clinician severity ratings (CSRs) determined from the separate parent and child interviews. Consensus diagnoses were subsequently determined during a weekly clinical team conference that included the parent and child assigned clinicians as well as the project director (i.e., a licensed clinical psychologist). Parents and children also completed several questionnaires as part of the pre-treatment assessment sessions.
Following the pre-treatment assessment sessions, participants were randomly assigned to either PMT or CPS [see Masked for Review, for further treatment details]. PMT was based on Barkley’s (1997) manualized training program, improving parenting strategies to address children’s oppositional behaviors and ultimately uplift the parent-child relationship. Sessions were 75 minutes in duration and involved both the parents and their children. The sessions addressed specific topics including educating parents about ODD and providing parents with strategies and approaches for responding to defiant behavior within and beyond the home as well as role playing activities during the sessions (see Masked for Review for additional details). CPS was based on Greene’s (1998; 2010) family-based cognitive behavioral therapy (CBT) model and was similarly structured with 75-minute sessions for families and their children. CPS focuses on identifying and prioritizing the problems that are causing challenging behavior and on having children and caregivers collaboratively solve those problems. Preliminary data have suggested that this collaborative process also improves the skills often found lacking in children diagnosed with ODD (e.g., emotion regulation difficulties; Murrihy et al, 2016; see Ollendick et al., 2016 for additional details). Participants in both treatment conditions received weekly treatment sessions, with a maximum of 14 sessions [M PMT sessions = 10.28 (3.86); M CPS sessions = 9.87 (3.67)]. Post-treatment and follow-up sessions were conducted one week following treatment and six months following treatment. At the post-treatment and follow up sessions, parents and children completed the clinically endorsed modules of the ADIS-IV-C/P as well as several questionnaires. IRB approval was obtained for all data collection.
Measures
Tangram Puzzle Task.
Families completed the Tangram Puzzle Task at pre-treatment (Hudson & Rapee, 2001). This 5-minute task consisted of a series of puzzles which required the child to place geometric shapes on top of an outlined set of templates which form larger shapes. This task involved puzzles of varying difficulty such that most children were not able to complete the task in the allotted 5-minute interval. Before the task began, parents received answer keys to each puzzle and were instructed to assist the child in any way they pleased. The parent-child interaction during the task was of primary interest. While fathers were present in nearly one-fifth (19.40%) of Tangram tasks, mothers were most often present and were typically the primary parent involved (98.51%). Hence, scores involving mother-child interactions were used. Each parent-child interaction was rated on the degree of parental over-involvement and rejection using the coding manual developed by Hudson and Rapee (2001). Consistent with the manual, parent-child interactions were coded on a nine-point scale ranging from zero to eight. Two composite scores were formed from the 11 subscales. The intrusiveness factor consisted of (a) the general degree of parental help during the task; (b) the degree of unsolicited help (intrusiveness); (c) the degree to which the parent physically touched the tangram pieces; (d) the parent’s posture; and (e) the parent’s focus during the interaction (towards the child or towards the task). This composite represents an overall measure of the degree of help the parent provided during the task, with higher scores indicating more help and over-involvement. The rejection factor assessed the degree of coldness during the interaction and consisted of (a) parent’s degree of positive affect (reverse-scored); (b) parent’s tension; (c) parent’s degree of verbal and non-verbal criticism; (d) child’s degree of positive affect (reverse-scored); (e) child’s tension; and (f) child’s degree of verbal and non-verbal criticism. Two trained research assistants viewed audio-visual recordings of the tangram task and independently coded the 11 behaviors. Coders were first assigned a set of training videos and were considered reliable for independent coding when they achieved 80% agreement. The items forming each composite score showed acceptable internal consistency in a subset of 30% of the recordings (αs = .84-.86).
Alabama Parenting Questionnaire.
Mothers and fathers completed the Alabama Parenting Questionnaire at pre-treatment (APQ; Frick, 1991). The APQ is a 42-item parent-report questionnaire which measures parenting strategies using a 5-point Likert scale from 1 (Never) to 5 (Always). Subscales of the APQ include: Positive involvement, supervision and monitoring, use of positive discipline techniques, consistency in use of such discipline, and corporal punishment. However, the corporal punishment subscale was not used for the current study since items from it were rarely endorsed, leaving four subscales collected from both mothers and fathers. The APQ has demonstrated good criterion validity for predicting oppositional defiant disorder and conduct disorder in children (Dadds, Maujean, & Fraser, 2003). All subscales in the present study demonstrated acceptable internal consistency (αs = .70-.91).
Behavior Assessment System for Children, Second Edition.
Parents also reported on their children’s externalizing problems and adaptive skills on the Behavior Assessment System for Children, Second Edition (BASC-2; Reynolds & Kamphaus, 2004) at the pre-treatment assessment, post-treatment assessment, and six-month follow-up. The Externalizing Problems composite included the Hyperactivity, Aggression, and Conduct Problems subscales. The Adaptive Skills composite included Functional Communication, Activities of Daily Living, Social Skills, and Adaptability subscales. BASC-2 items were coded on a likert scale ranging from 0 (Never) to 3 (Always). This scale was T-scored. Internal consistency was acceptable across assessments (αs = .85-.86).
Results
Preliminary Analyses
Data imputation.
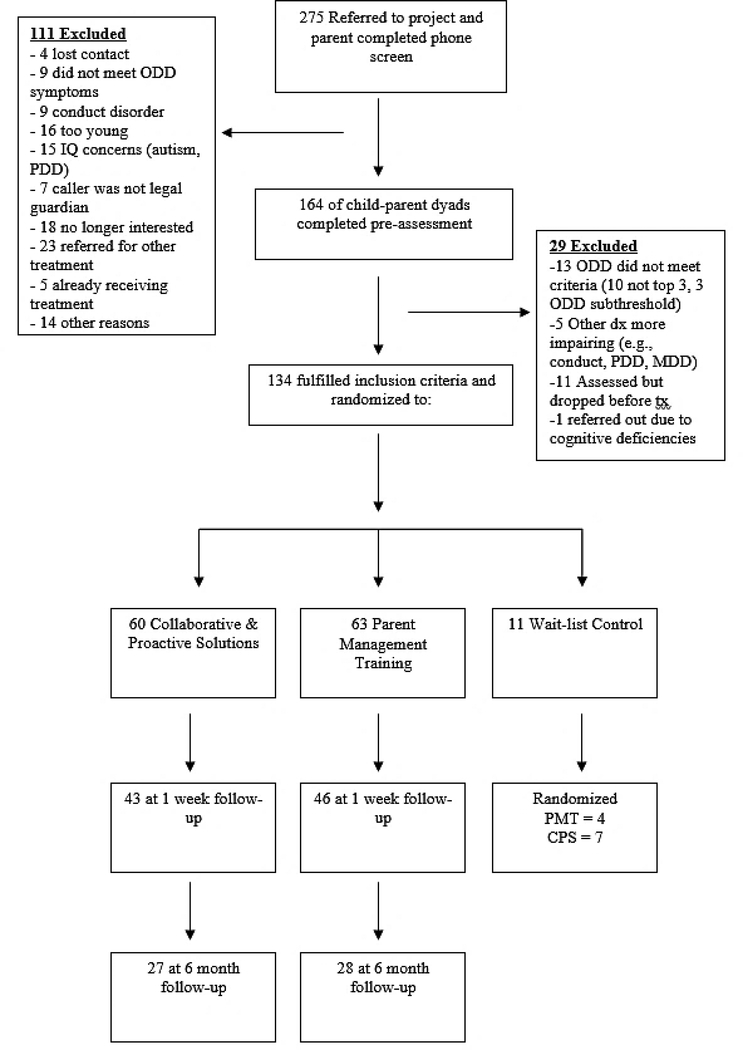
Given missing data across time points (see Table 1 and Figure 1), multiple imputation was conducted for all study variables. Using the R program (R Core Team, 2018) and Hmisc package (Harrell, 2018), 100 rounds of imputation were conducted, with up to 1,000 bootstrap resamples per imputation. The final imputed scores were used for all analyses. Table 1 presents the raw and imputed variables.
Table 1.
Variable Descriptives
| Pre-Treatment | Post-Treatment | Six-Month Follow-Up | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Variable | M | SD | N | M | SD | N | M | SD | N |
| APQ (Raw Data) | |||||||||
| Mom Involvement | 3.93 | .45 | 112 | -- | -- | -- | -- | -- | -- |
| Mom Positive Parenting | 4.16 | .54 | 112 | -- | -- | -- | -- | -- | -- |
| Mom Monitoring | 2.76 | 1.45 | 112 | -- | -- | -- | -- | -- | -- |
| Mom Inconsistent Discipline | 2.68 | .56 | 112 | -- | -- | -- | -- | -- | -- |
| Dad Involvement | 3.48 | .54 | 89 | -- | -- | -- | -- | -- | -- |
| Dad Positive Parenting | 2.84 | 1.54 | 89 | -- | -- | -- | -- | -- | -- |
| Dad Monitoring | 2.49 | .64 | 89 | -- | -- | -- | -- | -- | -- |
| Dad Inconsistent Discipline | 4.45 | 1.32 | 89 | -- | -- | -- | -- | -- | -- |
| Tangram Puzzle Task (Raw Data) | |||||||||
| Intrusiveness | 4.45 | 1.32 | 113 | -- | -- | -- | -- | -- | -- |
| Rejection | 3.73 | 1.15 | 113 | -- | -- | -- | -- | -- | -- |
| BASC (Raw Data) | |||||||||
| Externalizing Problems (Mom) | 72.89 | 10.56 | 123 | 60.26 | 10.34 | 66 | 59.71 | 8.39 | 35 |
| Adaptive Skills (Mom) | 36.11 | 6.06 | 123 | 40.44 | 7.26 | 66 | 38.33 | 6.32 | 35 |
| Externalizing Problems (Dad) | 67.39 | 10.60 | 104 | 60.54 | 10.24 | 50 | 59.17 | 8.39 | 24 |
| Adaptive Skills (Dad) | 36.58 | 7.01 | 103 | 38.20 | 6.98 | 50 | 38.33 | 6.32 | 24 |
| APQ (Imputed Data) | |||||||||
| Mom Involvement | 3.93 | .46 | 134 | -- | -- | -- | -- | -- | -- |
| Mom Positive Parenting | 4.16 | .53 | 134 | -- | -- | -- | -- | -- | -- |
| Mom Monitoring | 2.68 | 1.41 | 134 | -- | -- | -- | -- | -- | -- |
| Mom Inconsistent Discipline | 2.67 | .56 | 134 | -- | -- | -- | -- | -- | -- |
| Dad Involvement | 3.46 | .57 | 134 | -- | -- | -- | -- | -- | -- |
| Dad Positive Parenting | 3.84 | .63 | 134 | -- | -- | -- | -- | -- | -- |
| Dad Monitoring | 2.92 | 1.49 | 134 | -- | -- | -- | -- | -- | -- |
| Dad Inconsistent Discipline | 2.52 | .63 | 134 | -- | -- | -- | -- | -- | -- |
| Tangram Puzzle Task (Imputed Data) | |||||||||
| Intrusiveness | 4.47 | 1.29 | 134 | -- | -- | -- | -- | -- | -- |
| Rejection | 3.83 | 1.22 | 134 | -- | -- | -- | -- | -- | -- |
| BASC (Imputed Data) | |||||||||
| Externalizing Problems (Mom) | 72.84 | 10.58 | 134 | 62.10 | 10.77 | 134 | 57.73 | 10.02 | 134 |
| Adaptive Skills (Mom) | 36.29 | 5.99 | 134 | 39.84 | 7.23 | 134 | 40.96 | 7.29 | 134 |
| Externalizing Problems (Dad) | 68.92 | 11.05 | 134 | 63.93 | 11.20 | 134 | 62.03 | 11.38 | 134 |
| Adaptive Skills (Dad) | 35.48 | 7.33 | 134 | 36.95 | 6.99 | 134 | 36.27 | 6.86 | 134 |
Note.Tangram scores are based on mother-child interactions. APQ = Alabama Parenting Questionnaire. BASC = Behavior Assessment System for Children-2. BASC reports were T-scored.
Figure 1.
Numbers of Participants Meeting Study Protocol and Participating in Each Study Phase.
Bivariate correlations among family indicators.
Table 2 presents correlations among separate parent-child relationship variables. Many subscales on the APQ were significantly correlated and correlations were in the expected directions. There were fewer direct correlations between APQ reports and rated Tangram behaviors. However, family intrusiveness was positively correlated with father reports of involvement and inconsistent parenting. Further, family rejection was negatively correlated with mother reports of positive parenting and father reports of inconsistent parenting and was positively correlated with mother reports of inconsistent parenting.
Table 2.
Bivariate Correlations among Parent-Child Relationship Variables
| 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | |
|---|---|---|---|---|---|---|---|---|---|
| Mom APQ Reports | |||||||||
| 1. Involvement | .42** | .18* | −.12 | .35** | .22** | .20* | −.06 | .08 | .00 |
| 2. Positive Parenting | -- | .09 | −.23** | .30** | .32** | .14 | .05 | .01 | −.17* |
| 3. Monitoring | -- | .18* | .37** | .29** | .47** | .09 | .08 | −.01 | |
| 4. Inconsistent Parenting | -- | −.27** | −.03 | −.10 | .20* | −.04 | .27** | ||
| Dad APQ Reports | |||||||||
| 5. Involvement | -- | .64** | .32** | −.12 | .26** | −.07 | |||
| 6. Positive Parenting | -- | .20* | −.01 | .16 | −.15 | ||||
| 7. Monitoring | -- | −.01 | .01 | .03 | |||||
| 8. Inconsistent Parenting | -- | .18* | −.19* | ||||||
| Family Tangram Ratings | |||||||||
| 9. Intrusiveness | -- | .20* | |||||||
| 10. Rejection | -- |
Note.
p < .05
p < .01.
APQ = Alabama Parenting Questionnaire. Family Tangram Ratings are based on mother-child interactions.
Formation of Principal Components
Given the larger number of parent-child relationship variables across parental reports on the APQ and mother-child behaviors on the Tangram (k = 10), a data reduction approach was used in preparation of hypothesis testing. Principal components analysis (PCA) was used to represent as much item variance as possible within a smaller number of components. Reducing the number of independent variables for models was important to improve power for analyses, given interest in main effects and interaction effects. Components representing endorsements/displays of warmth, rejection, and intrusiveness were expected. Families with greater warmth were expected to report largest improvements in clinical outcomes (i.e., externalizing problems, adaptive skills) over time. Interactions with treatment assignment were tested, determining whether these family approaches predicted greater clinical outcomes given treatment assignment. Components were extracted using direct oblimin rotation, allowing correlations among components. The number of components was determined by Eigenvalues that equaled or were greater than one. Four components were supported, accounting for 65.13% of the variance among items. The structure matrix and correlations among components are presented in Table 3. The items with the largest loadings on the first component included mother involvement, mother positive parenting, mother inconsistent discipline, father involvement, and father positive parenting. This component was labeled Parental Warmth (PW). The items with the largest loadings on the second component included both mother and father monitoring. It was labeled as Parental Monitoring (PM). The third component had a high, positive loading from father inconsistent discipline and a high, negative loading from mother-child rejection behaviors. It was labeled Family Permissiveness (FP). The final component had high, positive loadings from the Tangram behaviors of intrusiveness and rejection. It was labeled Family Hostility (FH).
Table 3.
Principal Component Structure Matrix of Parent-Child Relationship Variables
| Parental Warmth | Parental Monitoring | Family Hostility | Family Permissiveness | |
|---|---|---|---|---|
| Component Loadings | ||||
| Mom Involvement | .54 | .26 | .11 | −.12 |
| Mom Positive Parenting | .70 | .08 | −.09 | .14 |
| Mom Monitoring | .01 | .86 | .13 | .13 |
| Mom Inconsistent Discipline | −.66 | .32 | .26 | .22 |
| Dad Involvement | .69 | .46 | .31 | −.07 |
| Dad Positive Parenting | .57 | .43 | .25 | .15 |
| Dad Monitoring | .15 | .73 | −.03 | −.13 |
| Dad Inconsistent Discipline | −.14 | .05 | .15 | .88 |
| Tangram Intrusiveness | .20 | .00 | .84 | .17 |
| Tangram Rejection | −.37 | .13 | .60 | −.53 |
| Component Correlations | ||||
| PW | -- | .17 | −.01 | .01 |
| PM | -- | .18 | .01 | |
| FH | -- | .01 | ||
Note. This table presents extracted principal components based on direct oblimin rotation.
Hypothesis Tests
Hierarchical linear models (HLM) were used for hypothesis tests, addressing between-family and within-family effects of parent-child relationship components approaches on reports of externalizing problems and adaptive skills. This analytical approach accounts for interdependent reports within groups and responses in this study were grouped by family (Osborne, 2000). HLM was selected rather than a repeated-measures ANOVA because interest was not on possible group effects among families (i.e., the main effect of treatment assignment; possible differences in mother and father reports within families), but on the continuous independent variable effects at the level of the family unit (i.e., parental warmth; family hostility). The effect of time (coded as 0, 1, 2) was included for each model, and a random effect of time was included for each model. Two models were tested for each outcome. A baseline model tested the between- and within-family effects of child age, child ADHD comorbidity, and family treatment assignment, as well as the effect of time on change within families. A final model added a) main effects between- and within-families for each principal component score, as well as b) interaction effects between- and within-families given each principal component score and treatment assignment. This final model addressed the two research questions: do parent-child relationship components uniquely predict clinical outcomes; and do these components moderate the effects of either PMT or CPS clinical interventions on clinical outcomes? Effect sizes were calculated given within- and between family variance in each model (Raudenbush & Liu, 2001). Table 4 presents the final model fixed effects for each outcome. For each outcome, the addition of principal component main effects and interaction terms between principal components and treatment assignment significantly improved model fit given changes in model complexity (ps ≤ .031).
Table 4.
Hierarchical Linear Model Fixed Effects for Externalizing Problems and Adaptive Skills
| Mother Externalizing | Mother Adaptive | Father Externalizing | Father Adaptive | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Est. | S.E. | d | p | Est. | S.E. | d | p | Est. | S.E. | d | p | Est. | S.E. | d | p | |
| Between-Family | ||||||||||||||||
| Intercept | 69.75 | 1.77 | -- | .000 | 38.64 | 1.01 | -- | .000 | 65.63 | 1.79 | -- | .000 | 36.51 | 1.17 | -- | .000 |
| Age | 1.92 | .93 | .47 | .041 | -.71 | .53 | −.28 | .184 | −.41 | .94 | −.06 | .666 | −.31 | .62 | .18 | .616 |
| ADHD | 3.78 | 1.82 | .92 | .040 | −3.27 | 1.04 | −1.31 | .002 | 5.48 | 1.84 | .81 | .003 | −1.79 | 1.21 | −.51 | .141 |
| Treatment (CPS) | −1.19 | 1.63 | −.29 | .469 | .63 | .03 | .25 | .498 | −2.09 | 1.65 | −.31 | .206 | .58 | 1.08 | .17 | .593 |
| PW | 1.75 | 1.20 | .43 | .147 | .97 | .69 | .39 | .159 | −.03 | 1.21 | .00 | .982 | .07 | .79 | .02 | .930 |
| PM | −.99 | 1.28 | −.24 | .439 | .51 | .73 | .20 | .483 | −3.29 | 1.29 | −.48 | .012 | .69 | .84 | .20 | .416 |
| FH | 1.54 | 1.23 | .38 | .215 | −1.74 | .71 | −.69 | .015 | 3.82 | 1.24 | .56 | .003 | −3.58 | .82 | −1.02 | .000 |
| FP | 3.98 | 1.11 | .97 | .000 | − .33 | .63 | −.13 | .599 | 3.78 | 1.12 | .56 | .001 | −.92 | .73 | −.26 | .208 |
| Treatment * PW | 2.52 | 1.68 | .61 | .137 | 1.95 | .96 | .78 | .044 | −1.21 | 1.70 | −.18 | .479 | 1.64 | 1.12 | .47 | .144 |
| Treatment * PM | .39 | 1.78 | .10 | .825 | .05 | 1.02 | .02 | .958 | .91 | 1.80 | .13 | .612 | −.45 | 1.18 | −.13 | .701 |
| Treatment * FH | −2.12 | 1.73 | −.52 | .224 | 2.16 | .99 | .86 | .031 | −2.60 | 1.75 | −.38 | .139 | 3.30 | 1.15 | .94 | .005 |
| Treatment * FP | −2.00 | 1.62 | −.49 | .219 | −.52 | .93 | −.21 | .576 | −.18 | 1.63 | −.03 | .913 | .21 | 1.07 | .03 | .844 |
| Within-Family | ||||||||||||||||
| Time | −8.35 | 1.26 | −2.04 | .000 | 3.56 | .74 | 1.42 | .000 | −4.74 | 1.26 | −.70 | .000 | .82 | .76 | .23 | .286 |
| Age | −.01 | .67 | .00 | .990 | .37 | .39 | .15 | .347 | .59 | .67 | .09 | .379 | −.52 | .40 | −.15 | .200 |
| ADHD | .86 | 1.30 | .21 | .512 | −1.02 | .76 | −.41 | .186 | 1.92 | 1.30 | .28 | .142 | −.30 | .79 | −.09 | .700 |
| Treatment (CPS) | .33 | 1.17 | .08 | .705 | −1.01 | .68 | −.41 | .139 | −.04 | 1.17 | −.01 | .970 | .25 | .71 | .07 | .719 |
| PW | −.32 | .86 | −.08 | .708 | .46 | .50 | .18 | .364 | .54 | .86 | .08 | .626 | −.23 | .52 | −.07 | .658 |
| PM | .32 | .91 | .08 | .728 | .53 | .53 | .21 | .324 | .66 | .91 | .10 | .470 | −.28 | .55 | −.08 | .616 |
| FH | −1.21 | .88 | −.29 | .172 | .70 | .52 | .28 | .178 | −1.41 | .88 | −.21 | .111 | .55 | .53 | .16 | .307 |
| FP | −1.29 | .79 | −.31 | .104 | −.04 | .46 | −.02 | .931 | −.16 | .79 | −.02 | .845 | .04 | .48 | .01 | .939 |
| Treatment * PW | 1.17 | 1.20 | .29 | .331 | −1.77 | .71 | −.71 | .013 | −.76 | 1.20 | −.11 | .529 | −.72 | .73 | −.21 | .323 |
| Treatment * PM | .09 | 1.28 | .02 | .944 | −.60 | .75 | −.24 | .353 | .67 | 1.27 | .10 | .601 | −.39 | .77 | −.11 | .612 |
| Treatment * FH | .65 | 1.24 | .16 | .599 | −.66 | .73 | −.26 | .366 | 1.57 | 1.24 | .23 | .206 | −1.18 | .75 | −.34 | .118 |
| Treatment * FP | .79 | 1.16 | .19 | .494 | .82 | .68 | .33 | .227 | −.30 | 1.16 | −.04 | .800 | .14 | .70 | .04 | .827 |
Note. PW = Parental Warmth. PM = Parental Monitoring. FH = Family Hostility. FP = Family Permissiveness.
Outcomes in externalizing problems.
For mothers’ reports of children’s externalizing problems, there were between-family effects of child age, ADHD comorbidity, and Family Permissiveness. Each of these variables predicted more severe externalizing problems. There was an effect of time. Specifically, mothers reported improvements in their child’s externalizing problems over time. There were no additional within-family effects.
For fathers’ reports of children’s externalizing problems, there were between-family effects of ADHD comorbidity, Parental Monitoring, Family Hostility, and Family Permissiveness. Monitoring from parents was associated with less severe reports of externalizing problems. ADHD comorbidity, family hostility, and family permissiveness predicted more severe reports of externalizing problems. There was also an effect of time. Fathers reported improvements in externalizing problems over time. There were no additional within-family effects.
Outcomes in adaptive skills.
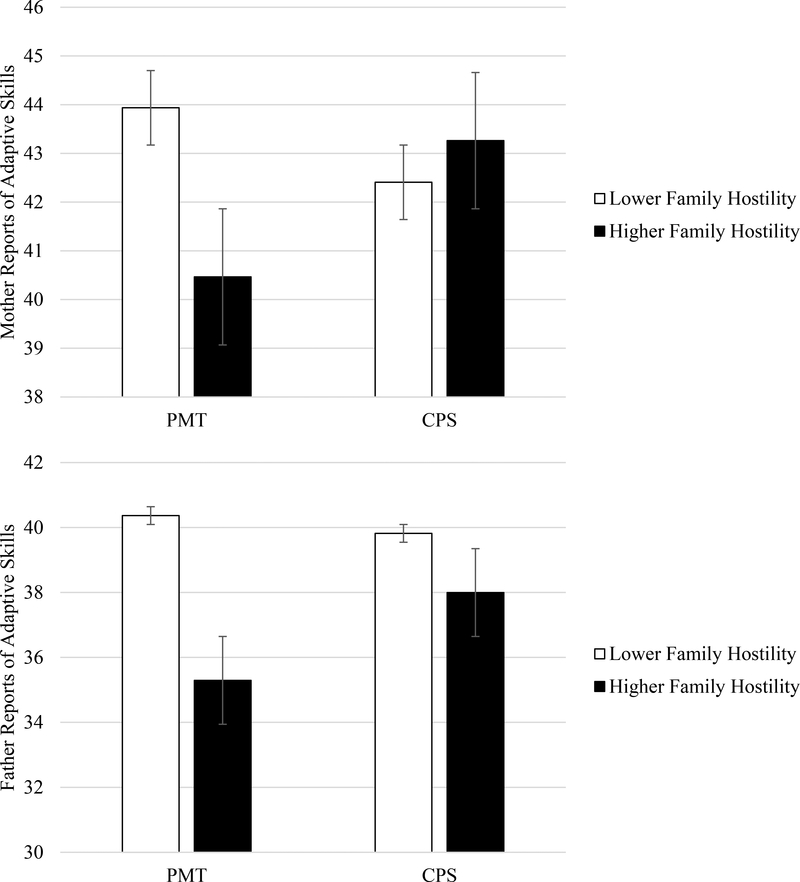
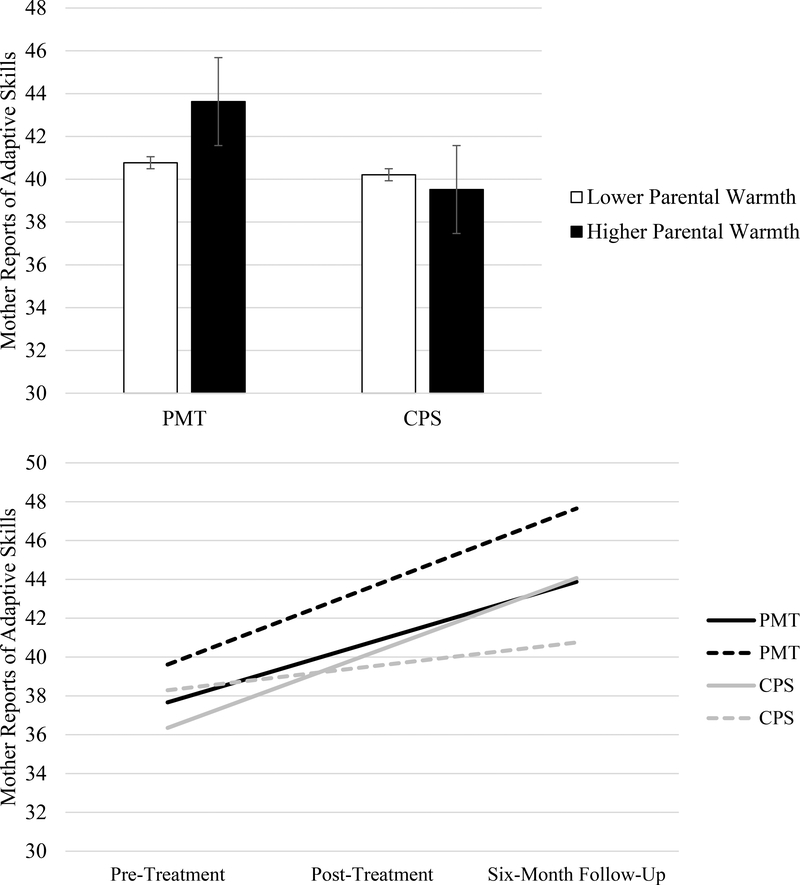
For mothers’ reports of children’s adaptive skills, there was a between-family main effect of ADHD comorbidity. Comorbidity predicted poorer adaptive skills. There was also a between-families interaction effect between treatment assignment and Family Hostility. This effect is depicted by Figure 2. For families receiving PMT, greater family hostility—intrusiveness and rejection displays in families—predicted poorer adaptive skills. However, families receiving CPS maintained relatively higher reports of mother-reported adaptive skills across levels of family hostility. Lastly, there were between-family and within-family interaction effects between treatment assignment and Parental Warmth. The between-family and within-family interaction effects are presented in Figure 3. Families with more parental warmth and who received the PMT intervention had the highest average endorsements of adaptive skills by mothers. Families lower in initial warmth reported improvements over time, but these improvements did not surpass warm PMT families. Further, families with more parental warmth and who received the CPS intervention reported the smallest improvements in adaptive skills over time.
Figure 2.
Mother (Top) and Father (Bottom) Reports of Adaptive Skills given Pre-Treatment Family Hostility and Treatment Assignment.
Note. Figures represent the two levels of treatment (PMT, CPS) and effects of principal component scores −1 SD and +1 SD from the mean.
Figure 3.
Mother Reports of Adaptive Skills given the Between-Family (Top) and Within-Family (Bottom) Interactions of Parental Warmth and Treatment Assignment.
Note. Figures represents the two levels of treatment (PMT, CPS) and effects of principal component scores −1 SD and +1 SD from the mean.
For fathers’ reports of children’s adaptive skills, there was a between-families interaction effect of treatment assignment and Family Hostility. This effect is depicted by Figure 2. Consistent with mothers’ reports, greater displays of family hostility were associated with lower father endorsements of children’s adaptive skills among families receiving PMT. Similarly, family hostility did not contribute to lower reports of adaptive skills among families receiving CPS. Father reports of adaptive skills did not significantly change over time and were not associated with any additional within-family effects.
Discussion
Building on existing findings, we expected pre-treatment facets of warmth, intrusiveness, and rejection in the parent-child relationship to inform clinical trajectories following ODD intervention. Multiple components emerged representing the parent-child relationship and uniquely predicted between- and within-family outcomes of externalizing problems and adaptive skills. Beyond covariate effects of child age and comorbid diagnosis of ADHD, endorsements of parental monitoring predicted fewer externalizing problems, whereas displays of family permissiveness (i.e., father inconsistency, low mother-child rejection) and hostile behaviors (i.e., higher mother-child intrusiveness and rejection) predicted more severe externalizing problems and poorer adaptive skills. These findings were in line with extant work (e.g., Burke et al., 2009; Greene et al., 2002). Also in line with previous findings (see Masked for Review), treatment assignment to either PMT or CPS did not show main effects, as assignment to each treatment was similarly efficacious for families. However, in the current re-analysis of data from that study, there were interaction effects between these components of the parent-child relationship and treatment assignment. Parent endorsements of adaptive skills were buffered from the negative effects of family hostility when families received CPS. Further, higher pre-treatment parental warmth showed greatest benefits for families receiving PMT.
Overall, the parent-child relationship did predict post-treatment clinical outcomes in children’s externalizing problems and their adaptive skills. This is important because these are two major problem areas for children with ODD (see Burke et al., 2002) and because psychosocial interventions for ODD have historically had high proportions of children who are not responsive to treatment (Jones et al., 2013; Kimonis & Fleming, 2018; Ollendick et al., 2016). By addressing multiple facets of this relationship—reflections of warmth, intrusiveness, and rejection—there may be ways to better anticipate the challenges to successfully implementing treatments and the ways in which certain treatments may be more or less compatible for specific families.
These findings could have implications for the selection of psychosocial treatments in youth diagnosed with ODD. PMT appeared better suited for families that entered intervention with warm and responsive parents—caretakers who may be appropriately equipped to incorporate firm, but fair rules and quality one-on-one time in the home (Barkley, 1997; Kazdin, 2005). Endorsements of warmth from mothers and fathers predicted larger gains in children’s adaptive skills, particularly among families receiving PMT. PMT emphasizes parent-driven structure and the development of parental strategies to promote compliance, remove reinforcers of oppositional behavior, and build a positive relationship with the child (Barkley, 1997; Kazdin, 2005). It is possible that PMT does not add significant parental warmth to the treatment equation, so parents demonstrating this characteristic before treatment may benefit from these treatment ingredients. These parents may gain more tools and strategies for promoting compliance with children than they would gain otherwise from approaches like CPS.
Alternatively, CPS appeared better suited for families where hostile interactions were more common and both parents and children were struggling to be able to display positive warmth with each other. Family hostility, reflecting problematic intrusive and rejecting behaviors in families, predicted poorer outcomes in adaptive skills among families receiving PMT. However, this was not found for families receiving CPS. CPS emphasizes the collaborative resolution of the problems contributing to problem behavior and recognition of children’s lagging skills. Thus, CPS may equip families to identify the underlying issues that contribute to hostile interactions between parents and children and begin working to address the causes and consequences of those hostile interactions. That is not to say that these families no longer had episodes of problematic parent-child interactions—hostility predicted more average externalizing problems. However, they could have more tools for redirecting these interactions and promoting constructive behaviors than youth with similar challenges who received PMT.
Support for interaction effects between treatment assignment and pre-treatment family approaches was limited to predictions of adaptive skills. These moderation effects did not extend to trajectories of externalizing problems. Given the primary emphasis of each of these interventions to reduce ODD symptoms in children, it is not entirely surprising that these treatments were similarly effective for externalizing problems and had similar benefits regardless of family heterogeneity. However, questions remain on how best to promote the rates of robust treatment response for families—to improve the current rates of approximately 45–55% symptom improvement (Jones et al., 2013; Kimonis & Fleming, 2018; Ollendick et al., 2016) for families with different approaches of warmth, intrusiveness, and rejection upon treatment entry.
Although not a primary question in this study, common covariates were also accounted for in addressing the major research questions. Child age and ADHD comorbidity were robust predictors of externalizing problems and adaptive skills. While findings regarding the prevalence and severity of ODD at different ages remain mixed (e.g., Loeber et al., 2000; Maughan, Rowe, Messer, Goodman, & Meltzer, 2004), additional disruptive behaviors beyond ODD symptoms are likely to become more prominent with age when ODD is untreated (Loeber et al., 2000). Hence, for families who are seeking treatment for older children and adolescents, particularly if youth have been displaying oppositional symptoms for an extended period, youth may enter treatment studies with initially more severe difficulties (i.e., increased externalizing problems and decreased adaptive skills). In the current study, older children did not differ in how their externalizing problems or adaptive skills changed over time. That is, older children were no less responsive to interventions of PMT and CPS than younger children. Further, in line with previous studies (Gadow & Nolan, 2002; Harvey, Breaux, & Lugo-Candelas, 2016), children with comorbid ODD and ADHD diagnoses were reported to have poorer outcomes on average. These findings further underscore the additional challenges children face when they enter treatment with comorbid diagnoses.
Limitations, Strengths, and Future Directions
Attrition is a common concern in multiphase studies with families dealing with oppositional symptoms (Murrihy et al., 2010), and we too were impacted by families withdrawing from later phases of study or not completing all requested study materials, leading to a reliance on data imputation. The current study was also limited by the demographic homogeneity of the sample (i.e., predominantly white and middle to upper-middle class families). The sample reflects the challenges of recruiting and maintaining participation from a diverse and representative sample of children and their parents for participation in multiphase clinical studies. Of course, our study is also limited by the two treatment programs we examined. Little is known about how these parenting variables might relate to other forms of parenting interventions or to interventions that are focused primarily on the child. Further, the use of PMT with a sample that extends into early adolescence (13–14 years) may have been problematic. In particular, as adolescents are typically renegotiating power and autonomy with their parents (see Collins & Laursen, 2004), there can be additional challenges in incorporating PMT that may not be present when working with children. However, we note that PMT has been used with early adolescents displaying severe disruptive and oppositional behaviors in other research studies (e.g., Kazdin, 1995, 2005; Kazdin, Siegel, & Bass, 1992; Murrihy et al., 2010). In addition, even as we accounted for child age in hypothesis tests, we continued to see overall improvement given treatment exposure and the roles of other family approaches for these children.
Overall, this study advances the field by addressing significant gaps in the extant literature. Few studies have examined the ways heterogeneity in family approaches relates to children’s clinical outcomes following treatment for ODD. The current study pointed to valuable insights of family approaches for families being assigned to one of two treatments to address ODD. We recognize that these are only two treatments among a broader set of empirically-supported interventions, with each placing different emphasis on strategies and tools for families to attain significant and lasting improvements. There is rich potential to consider the ways these (and possibly additional) facets of the parent-child relationship show particular fit and alignment with certain interventions and promote greater post-treatment improvements. There is also a need to understand the roles of family nuances beyond populations seeking treatment for ODD, extending methods to other disruptive behavior disorders (e.g., conduct disorder) and to internalizing disorders (e.g., specific phobias; social anxiety). Though these disorders reflect different challenges with self-regulation and skill deficits, family approaches remain salient for children’s clinical outlooks (see Bögels & Brechman-Toussaint, 2006). A separate, though related area of future inquiry involves the consideration of mechanisms of change that extend beyond the target child and involve the broader family unit. As active partners in the treatment process and individuals sharing proximal interactions with referred children, we know that other family members such as parents are influenced by children’s treatment outcomes (e.g., Booker et al., 2018; Kazdin, 2017). Given the ties between the parent-child relationship and treatment outcomes, and the ways family approaches can be shaped by certain treatments, there is value in testing processes of change in family approaches following treatment, understanding the nuances in change given assignment to different treatments, and the long-term implications of these changes for child outcomes and the family environment. Like many existing studies, we focused on homogenous effects of these facets of the parent-child relationship, expecting a similar benefit or drawback of each facet of the relationship (e.g., parental warmth) for all families. Future studies might benefit from considering systematic patterns in the parent-child relationship for a more holistic view of families (see Bergman, von Eye, & Magnusson, 2015). That is, there may be distinct and valuable insights given the ways some families emphasize only one relationship approach heavily (i.e., only high warmth, only high rejection) and the ways other families show more nuanced and mixed patterns (i.e., higher displays of warmth and rejection). These nuances may provide valuable insights for the field, and analyses focusing on family-level patterns (e.g., latent class analysis; growth mixture modeling) could provide additional insights for questions of family influences on post-treatment trajectories for children. As with questions on families’ fit with certain treatments, understanding areas where families are in broader need to address cohesion and conflict in the home, as well as interventions that may ultimately address those broader needs, could be determining factors in treatment selection and tailoring. With each of these considerations, there is a need to consider populations that represent diverse experiences given socioeconomic background, ethnic background, and geographic location for richer insights on the values of parent-child relationship patterns and other family characteristics may provide as families seek treatment for their children.
Acknowledgments
Funding Statement: Funding was provided by R01 MH076141 from NIMH and by the Institute for Society, Culture, and Environment at Virginia Tech. We wish to express appreciation to the graduate students and research scientists who assisted us with various aspects of this project, including data reduction, assessment, and treatment of these youth. We also wish to extend thanks to the many undergraduate students at Virginia Tech who assisted us with data coding, entry, and verification. Finally, we are grateful to the youth and families who participated in this clinical research. Please address correspondence to Jordan A. Booker, 213 McAlester Hall, Department of Psychological Sciences, University of Missouri, Columbia, MO, 65211, or bookerja@missouri.edu.
Footnotes
Conflict of Interest Statement: RWG: Received royalties related to work concerning Collaborative and Proactive Solutions. The remaining authors have no conflicts of interest.
Ethics Statement: All procedures performed in this study were in accordance with the ethical standards of the overseeing Institutional Review Board and with the 1964 Helsinki declaration and its later amendments.
Informed Consent Statement: All families completed informed consent and informed assent before participating.
Contributor Information
Jordan A. Booker, Email: bookerja@missouri.edu, jordan.booker@vt.edu.
Nicole N. Capriola-Hall, Email: cnicole@vt.edu.
Ross. W. Greene, Email: drrossgreene@gmail.com.
Thomas H. Ollendick, Email: tho@vt.edu.
References
- Aebi M, Muller UC, Asherson P, Banaschewski T, Buitelaar J, Ebstein R … Steinhausen HC (2010). Predictability of oppositional defiant disorder and symptom dimensions in children and adolescents with ADHD combined type. Psychological Medicine, 40, 2089–2100. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. (2013). DSM 5. Washington D.C.: American Psychiatric Association. [Google Scholar]
- Barkley RA (1997). Defiant children: A clinician’s manual for parent training (2nd ed.). New York: Guilford Press. [Google Scholar]
- Barkley RA, & Robin AL (2014). Defiant teens: A clinician’s manual for assessment and family intervention (2nd ed.). New York: Guilford Publications. [Google Scholar]
- Bergman LR, von Eye A, & Magnusson D (2015). Person-oriented research strategies in developmental psychopathology In Cicchetti D & Cohen DJ (Eds.), Developmental psychopathology: Volume one: Theory and method (2nd ed.; pp. 850–888). Hoboken, NJ: John Wiley & Sons. [Google Scholar]
- Bögels SM, & Brechman-Toussaint ML (2006). Family issues in child anxiety: Attachment, family functioning, parental rearing and beliefs. Clinical Psychology Review, 26, 834–956. [DOI] [PubMed] [Google Scholar]
- Booker JA, Capriola-Hall NN, Dunsmore JC, & Greene RW (2018). Change in maternal stress for families in treatment for their children with oppositional defiant disorder. Journal of Child and Family Studies, 27, 2552–2561. 10.1007/s10826-018-1089-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Booker JA, Ollendick TH, Dunsmore JC &, Greene RW (2016). Perceived parent-child relations, conduct problems, and clinical improvement following the treatment of oppositional defiant disorder. Journal of Child and Family Studies, 25, 1623–1633. 10.1007/s10826-015-0323-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown CA, Granero R, & Ezpeleta L (2017). The reciprocal influence of callous-unemotional traits, oppositional defiant disorder and parenting practices in preschoolers. Child Psychiatry & Human Development, 48, 298–307. 10.1007/s10578-016-0641-8 [DOI] [PubMed] [Google Scholar]
- Burke JD, Loeber R, & Birmaher B (2002). Oppositional defiant disorder and conduct disorder: A review of the past 10 years, part II. Journal of the American Academy of Child and Adolescent Psychiatry, 41, 1275–1293. 10.1097/01.CHI.0000024839.60748.E8 [DOI] [PubMed] [Google Scholar]
- Burke JD, Pardini DA, & Loeber R (2008). Reciprocal relationships between parenting behavior and disruptive psychopathology from childhood through adolescence. Journal of Abnormal Child Psychology, 36, 679–692. 10.1007/s10802-008-9219-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark JE, & Frick PJ (2016). Positive parenting and callous-unemotional traits: their association with school behavior problems in young children. Journal of Clinical Child & Adolescent Psychology. Advanced Online Publication. 10.1080/15374416.2016.1253016 [DOI] [PubMed] [Google Scholar]
- Dadds MR, Maujean A, & Fraser JA (2003). Parenting and conduct problems in children: Australian data and psychometric properties of the Alabama Parenting Questionnaire. Australian Psychologist, 38, 238–241. [Google Scholar]
- de Haan AD, Deković M, van den Akker AL, Stoltz SEMJ, & Prinzie P (2013). Developmental personality types from childhood to adolescence: associations with parenting and adjustment. Child Development, 84, 2015–2030. 10.1111/cdev.12092 [DOI] [PubMed] [Google Scholar]
- Dunsmore JC, Booker JA, & Ollendick TH (2013). Parental emotion coaching and child emotion regulation as protective factors for children with oppositional defiant disorder. Social Development, 22, 444–466. 10.1111/j.1467-9507.2011.00652.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eyberg SM, Nelson MM, & Boggs SR (2008). Evidence-based psychosocial treatments for children and adolescents with disruptive behavior. Journal of Clinical Child and Adolescent Psychology, 37, 215–237. 10.1080/15374410701820117 [DOI] [PubMed] [Google Scholar]
- Frick PJ (1991). The Alabama Parenting Questionnaire. Unpublished rating scale, University of Alabama. [Google Scholar]
- Frick PJ (2001). Effective interventions for children and adolescents with conduct disorder. The Canadian Journal of Psychiatry, 46, 597–608. [DOI] [PubMed] [Google Scholar]
- Gadow KD, & Nolan EE (2002). Differences between preschool children with ODD, ADHD, and ODD+ADHD symptoms. The Journal of Child Psychology and Psychiatry, 43, 191–201. 10.1111/1469-7610.00012 [DOI] [PubMed] [Google Scholar]
- Greene RW (1998). The explosive child: A new approach for understanding and parenting easily frustrated, “chronically inflexible” children. New York: Harper Collins. [Google Scholar]
- Greene RW (2010). The aggressive, explosive child In Zuckerman B, Caronna E, & Augustyn M (Eds.), Zuckerman and Parker’s Handbook of Developmental and Behavioral Pediatrics. (2nd Ed.). Baltimore: Lippincott, Williams, & Wilkins. [Google Scholar]
- Greene RW, Ablon JS, Goring JC, Raezer-Blakely L, Markey J, Monuteaux MC, … & Rabbitt S (2004). Effectiveness of collaborative problem solving in affectively dysregulated children with oppositional-defiant disorder: initial findings. Journal of Consulting and Clinical Psychology, 72, 1157–1164. 10.1037/0022-006X.72.6.1157 [DOI] [PubMed] [Google Scholar]
- Greene RW, Biederman J, Zerwas S, Monuteaux MC, Goring JC, & Faraone SV (2002). Psychiatric comorbidity, family dysfunction, and social impairment in referred youth with oppositional defiant disorder. The American Journal of Psychiatry, 159, 1214–1224. [DOI] [PubMed] [Google Scholar]
- Greene RW, & Doyle AE (1999). Toward a transactional conceptualization of oppositional defiant disorder: Implications for treatment and assessment. Clinical Child and Family Psychology Review, 2, 129–148. [DOI] [PubMed] [Google Scholar]
- Hamilton SS, & Armando J (2008). Oppositional defiant disorder. American Family Physician, 78, 861–866. [PubMed] [Google Scholar]
- Harrell FE (2018). Hmisc: Harrell miscellaneous. R package version 4.1–1. https://CRAN.R-project.org/package=Hmisc
- Harvey EA, Breaux RP, & Lugo-Candelas CI (2016). Early development of comorbidity between symptoms of attention deficit hyperactivity disorder and oppositional defiant disorder. Journal of Abnormal Psychology, 125, 154–167. 10.1037/abn0000090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawes DJ, Price MJ, & Dadds MR (2014). Callous-unemotional traits and the treatment of conduct problems in childhood and adolescence: A comprehensive review. Clinical Child and Family Psychology Review, 17, 248–267. 10.1007/s10567-014-0167-1 [DOI] [PubMed] [Google Scholar]
- Hentges RF, Shaw DS, & Wang M-T (2017). Early childhood parenting and child impulsivity as precursors to aggression, substance use, and risky sexual behavior in adolescence and early adulthood. Development and Psychopathology. 10.1017/S0954579417001596 [DOI] [PubMed] [Google Scholar]
- Hudson JL, & Rapee RM (2001). Parent–child interactions and anxiety disorders: An observational study. Behaviour Research and Therapy, 39, 1411–1427. [DOI] [PubMed] [Google Scholar]
- Jones DJ, Forehand R, Cuellar J, Kincaid C, Parent J, Fenton N, & Goodrum N (2013). Harnessing innovative technologies to advance children’s mental health: Behavioral parent training as an example. Clinical Psychology Review, 33, 241–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kashdan TB, Jacob RG, Pelham WE, Lang AR, Hoza B, Blumenthal JD, & Gnagy EM (2004). Depression and anxiety in parents of children with ADHD and varying levels of oppositional defiant behaviors: Modeling relationships with family functioning. Journal of Clinical Child and Adolescent Psychology, 33, 169–181. 10.1207/S15374424JCCP3301_16 [DOI] [PubMed] [Google Scholar]
- Kazdin AE (1995). Conduct disorders in childhood and adolescence (2nd ed.). Thousand Oaks, CA: Sage. [Google Scholar]
- Kazdin AE (2005). Child, parent, and family-based treatment of aggressive and antisocial child behavior In Hibbs ED & Jensen PS (Eds.), Psychosocial treatments for child and adolescent disorders: Empirically based strategies for clinical practice (pp. 445–476). Washington, DC, US: American Psychological Association. [Google Scholar]
- Kazdin AE (2017). Parent management training and problem-solving skills training for child and adolescent conduct problems In Weisz JR & Kazdin AE (Eds.), Evidence-based psychotherapies for children and adolescents (3rd Ed., pp. 142–158). New York: The Guilford Press. [Google Scholar]
- Kazdin AE, Siegel TC, & Bass D (1992). Cognitive problems-solving skills training and parent management training in the treatment of antisocial behavior in children. Journal of Consulting and Clinical Psychology, 60, 733–747. [DOI] [PubMed] [Google Scholar]
- Kimonis ER, & Fleming GE (2018). Disruptive and conduct disorder problems In Ollendick TH, White SW, & White BA (Eds.). Oxford handbook of clinical child and adolescent psychology. Oxford: Oxford University Press. [Google Scholar]
- Loeber R, Burke JD, Lahey BB, Winters A, & Zera M (2000). Oppositional defiant and conduct disorder: A review of the past 10 years, part I. Journal of the American Academy of Child and Adolescent Psychiatry, 39, 1468–1484. 10.1097/00004583-200012000-00007 [DOI] [PubMed] [Google Scholar]
- Loeber R, Burke J, & Pardini DA (2009). Perspectives on oppositional defiant disorder, conduct disorder, and psychopathic features. Journal of Child Psychology and Psychiatry, 50, 133–142. 10.1111/j.1469-7610.2008.02011.x [DOI] [PubMed] [Google Scholar]
- Loeber R, Keenan K, Russo MF, Green SM, Lahey BB, & Thomas C (1998). Secondary data analysis for DSM-IV on the symptoms of oppositional defiant disorder and conduct disorder In Widiger TA, Frances AJ, Pincus HJ, Ruth R, First MB, Davis W, & Kline M (Eds.), DSM-IV sourcebook, Vol. 4 (pp. 465–490). Washington, D.C., American Psychiatric Press. [Google Scholar]
- Maughan B, Rowe R, Messer J, Goodman R, & Meltzer H (2004). Conduct disorder and oppositional defiant disorder in a national sample: Developmental epidemiology. Journal of Child Psychology and Psychiatry, 45, 609–621. [DOI] [PubMed] [Google Scholar]
- Michaelson D, Davenport C, Dretzke J, Barlow J, & Day C (2013). Do evidence-based interventions work when tested in the “real world?” A systematic review and meta-analysis of parent management training for the treatment of child disruptive behavior. Clinical Child and Family Psychology Review, 16, 18–34. 10.1007/s10567-013-0128-0 [DOI] [PubMed] [Google Scholar]
- Murrihy RC, Kidman AD, & Ollendick TH (Eds.). (2010). Clinical handbook of assessing and treating conduct problems in youth. Springer Science & Business Media. [Google Scholar]
- Murrihy R, Wallace A, Ollendick TH, Greene RW, McAloon J, Gill S, Remond L, Ellis DM, & Drysdale S (2016). Parent Management Training and Collaborative & Proactive Solutions: A randomised comparison trial for oppositional youth within an Australian population. Presented at Symposium, Advances in conceptualisation and treatment of youth with oppositional defiant disorder: A comparison of two major therapeutic models, Eighth World Congress of Behavioural and Cognitive Therapies, Melbourne, Australia. [Google Scholar]
- Nixon RDV, Sweeney L, Erickson DB, & Touyz SW (2003). Parent-child interaction therapy: A comparison of standard and abbreviated treatments for oppositional defiant preschoolers. Journal of Consulting and Clinical Psychology, 71, 251–260. 10.1037/0022-006X.71.2.251 [DOI] [PubMed] [Google Scholar]
- Ollendick TH, Greene RW, Austin KE, Fraire MG, Halldorsdottir T, Allen KB, Jarrett MA, Lewis KM, Whitmore MJ, Cunningham NR, Noguchi RJP, Canavera K, & Wolff JC (2016). Parent Management Training (PMT) and Collaborative & Proactive Solutions (CPS): A randomized control trial for oppositional youth. Journal of Clinical Child and Adolescent Psychology, 45, 591–604. 10.1080/15374416.2015.1004681 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osborne JW (2000). Advantages of hierarchical linear modeling. Practical Assessment, Research & Evaluation, 7 Available online: http://PAREonline.net/getvn.asp?v=7&n=1 [Google Scholar]
- Pike A, McGuire S, Hetherington EM, Reiss D, & Plomin R (1996). Family environment and adolescent depressive symptoms and antisocial behavior: A multivariate genetic analysis. Developmental Psychology, 32, 590–603. [Google Scholar]
- R Core Team (2018). R: A language and environment for statistical computing R Foundation for Statistical Computing, Vienna, Austria: URL https://www.R-project.org/. [Google Scholar]
- Raudenbush SW, & Liu X (2001). Effects of study duration, frequency of observation, and sample size on power in studies of group differences in polynomial change. Psychological Methods, 6, 387–401. 10.1037//1082-989.X.6.4.387 [DOI] [PubMed] [Google Scholar]
- Reynolds CR, & Kamphaus RW (2000). Behavior assessment system for children (2nd ed.). Circle Pines, MN: American Guidance Service. [Google Scholar]
- Silverman WK, & Albano AM (1996). Anxiety Disorders Interview Schedule for DSM-IV (Child and Parent Versions). San Antonio, TX: Psychological Corporation. [Google Scholar]
- Tung I, & Lee SS (2014). Negative parenting behavior and childhood oppositional defiant disorder: Differential moderation by positive and negative peer regard. Aggressive Behavior, 40, 79–90. 10.1002/ab.21497 [DOI] [PubMed] [Google Scholar]