Abstract
The International Classification of High-resolution Computed Tomography for Occupational and Environmental Respiratory Diseases (ICOERD) has been developed for screening and diagnosis of occupational lung diseases. We evaluated the association of icoerd with the International Labor Organization (ILO) classification and respiratory functions in pneumoconiosis. Chest x-rays of patients with pneumoconiosis were classified with ilo and icoerd using hrct, irregular opacity, pleural pathology, and emphysema was detected in 78, 19, and 53 patients, and using chest x-rays in 47, 4, and 14 patients, respectively. There was a significant correlation between ILO categories and ICOERD grades. There was a negative correlation between ILO categories and FEV1% and FVC%, whereas, ICOERD grades were not correlated with FEV1% and FVC%. HRCT was superior to chest x-rays to detect pneumoconiosis in early stage, but not in evaluating pulmonary functions.
Keywords: Pneumoconiosis, High-resolution computed tomography, Ventilatory function
Introduction
Pneumoconiosis is defined by the International Labor Organization (ILO) as a preventable occupational disease caused by the accumulation of inorganic dust in the lungs and associated tissue reactions1). Analog radiographs recommended by the ILO are used to classify and record radiographic abnormalities caused by dust exposure2). New techniques are needed to identify pneumoconiosis at the subclinical stage and to visualize early changes to accurately predict disease progression3). High-resolution computed tomography (HRCT) is more specific and sensitive than chest x-rays in the early evaluation of pneumoconiosis4). The international expert meeting recommended the development of a HRCT reporting system for asbestos-related diseases5). Thereupon International Classification of HRCT for Occupational and Environmental Respiratory Diseases (ICOERD) was developed. The objective of this classification is asbestosis-related lung diseases and tobacco exposure-related respiratory diseases such as silicosis and emphysema used for screening, diagnosis, and epidemiological reporting4).
Pulmonary function tests (PFT), although not specific for diagnosing any cause, are used to assess dyspnea, to distinguish between obstructive and restrictive disorders, and to assess disease severity. Respiratory failure is a complication of severe pneumoconiosis6). A negative correlation between cumulative coal dust exposure and forced expiratory volume in 1 s (FEV1), forced vital capacity (FVC), and FEV1/FVC has been shown7, 8). There is often no correlation between silicosis functional changes and radiological involvement9). It has been reported that pulmonary functions are impaired by progressive massive fibrosis, mixed dust fibrosis, and emphysema10). Emphysema, large opacities, and bronchiectasis are reported in the ICOERD system4). Imaging methods and functional test correlation studies have shown that PFT results are influenced by a history of smoking and pulmonary emphysema11,12,13).
In this study, chest radiography and HRCT were compared at the early diagnosis stage of pneumoconiosis. We examined the relationship between ILO and ICOERD systems with PFT in determining the functional status of the disease.
Subjects and Method
Our study was planned as a retrospective, cross-sectional study. Ankara Keçiören Training and Research Hospital Clinical Research Ethics Board approved this study (approval number: 463/2014). Informed consent was not received from the participants because of the retrospective design. Three international criteria were used for the diagnosis of pneumoconiosis:
-
1
History of sufficient exposure to dust
-
2
Compatible radiological features
-
3
Exclusion of other competing diagnosis
In this way, patients who were diagnosed with pneumoconiosis from 2012–2014 and who had chest x-ray, HRCT, and PFT examinations at the time of diagnosis were included in the study. Those patients with other known diseases of the lung were not included. A total of 125 patients were screened, and 83 patients who met these criteria were included in the study.
In the patient evaluation form, demographic information, working environment and duration, environmental and occupational exposure, smoking, the time to diagnosis, and diagnostic methods used were recorded in detail.
Radiological studies
Pulmonary radiographs were taken using an Apelam device with Conica CR scanner and standard technique (180 cm, posteroanterior, 100 kV, Phot Timer 0.1sn). An automatic bath was used for all radiographs, and all were printed as 33 × 38 cm films as recommended by the ILO-2000 standard.
Pulmonary radiographs were evaluated according to the ILO-2000 classification by two pulmonologists with joint opinion consensus, both of whom were certified “B” reader of ILO and were not informed about the occupations of the patients. The complete set of 22 ILO radiographs was used in the classification.
Small opacities were coded as p, q, and r, corresponding to <1.5 mm, 1.5–3 mm, and 3–10 mm sizes respectively; irregular opacities were coded as s, t, and u, corresponding to <1.5 mm, 1.5–3 mm, and 3–10 mm sizes, respectively. Opacities larger than 1 cm were recorded as large opacities using the following code:
A was coded if the sum of the large diameters of these opacities was 1–5 cm,
B was coded if the sum was >5 cm and did not pass the right upper zone, and
C was coded if one or more opacities cross the equivalent area of the right upper zone.
Pleural abnormalities were reported as pleural plaque, costophrenic angle blunting, and diffuse pleural thickening. Symbols were used for additional features.
The HRCT was taken using a Siemens Emotion 6 device in a supine position (10 mm interval, 130 kV, mAS: 100) using 2 mm sections. Siemens scans were digitally evaluated on medical monitors.
The HRCT images were assessed by three radiologists, classified with joint opinion consensus, and based on the ICOERD classification. The density total grade for the well-defined round opacity (RO), irregular and/or linear opacity (IR), ground glass opacity (GGO), honeycomb grade (HC), and emphysema (EM) were established for each lung and each zone separately, calculated by taking the latest sums of 0 to 3 points one by one. Finally, the dominant lesion is selected according to the reader’s opinion and the score of the selected lesion is used. In our study, when comparing with the ILO categories, score of the lesion that was dominant among IR and RO was accepted as “small opacity grade” for ICOERD. On chest x-ray, round opacity and irregular opacity were categorized jointly and also the findings of emphysema and honeycomb were marked with original symbols; so, these categories were not individually compared within themselves.
Round opacities were classified according to size as P (<1.5 mm), Q (1.5–3 mm), and R (3–10 mm) in HRCT results. Linear and/or irregular opacities were reported as intralobular and interlobular opacities. Opacity was classified as a large opacity when the average of two perpendicular diameters was >1 cm. Large opacity findings were encoded as A if the sum of one or more opacities (one for each lung) was between the sizes of 1 cm and one-quarter of the area of the CT section at the level of the carina, as B if the size was greater than A and less than one-half of the area of the CT section at the level of the carina, and as C if the size was between one-half and the entire area of the CT section at the level of the carina.
Pleural pathologies were recorded as visceral and parietal types. Emphysema was reported as mild (1) for <15%, moderate (2) for 15–30%, and severe (3) for >30% for each zone.
In the PFT laboratory, pulmonary functions were evaluated using a current-sensitive spirometry device (Zan 100, nSpire Health Inc., Germany). The test was repeated three times and the best measurement was taken using FEV1, FEV1/FVC, FVC, forced expiratory flow at 25–75% (FEF25–75) values. Corrected values according to age, height, and weight were used and recorded with percentages. Pulmonary function was classified as normal, obstructive, restrictive, mixed type, and small airway obstruction according to the American Thoracic Society guidelines14).
Statistical analysis
The data obtained in this study were evaluated with the SPSS 16.0 for Windows program. Frequency and percentage distributions of the data were given. The Kolmogorov-Smirnov test was used for normality evaluation. The McNemar test was used to test the significance of the difference between the two percentages in the dependent groups. The Kruskal-Wallis test was used to compare the medians in independent multiple groups and Bonferroni correction was used for post hoc analysis of this test. The Spearman test was used to analyze the correlation of continuous variables in independent groups. For statistical significance, p<0.05 was used.
Results
All 83 patients included in the study were male, with a mean age of 44.46 (± 11.45) yr. Of the patients, 23 (27.71%) were nonsmokers, 30 (36.14%) were active smokers, and 30 (36.14%) were ex-smokers. Fifty-five (66.27%) patients had no environmental asbestos exposure, while 28 (33.73%) patients had been exposed to asbestos. The working period of patients ranged from 2–46 (M=16.48) yr.
The most frequent occupational groups were founder (n=25, 30.12%), welder (n=12, 14.46%), dental technician (n=11, 13.25%), and miner (n=9, 10.84%). The other 26 (31.32%) patients worked in sandblasting, grinding, stone quarrying, ceramics manufacturing, tunnel digging, polypropylene pipe fittings, heat insulation installation, bucket operation, and electrical installation occupations.
In the study, 79 patients were diagnosed radiologically and four patients were pathologically diagnosed by wedge resection, thoracotomy, transthoracic fine needle aspiration, or transbronchial biopsy.
The predominant lesion shown in HRCT results was found to be an irregular opacity in 28 (33.7%) patients and a round opacity in 33 (39.7%) cases, while 64 (77.1%) patients had a round opacity, and 8 (9.6%) patients had irregular opacities shown in chest x-rays. In 11 patients who were not evaluated as pneumoconiosis by chest x-ray, the dominant lesion shown in HRCT results was an irregular opacity in six cases, a round opacity in two cases, a ground glass opacity in one case, and emphysema in two cases.
Pneumoconiosis was detected in 72 (86.75%) patients using chest x-rays and 79 (95.18%) patients using HRCT. The distributions of RO and IR are shown in Table 1. HRCT showed a higher rate of IR compared to chest x-rays (47–78 cases) and the difference was statistically significant (p<0.05). In 36 patients without small irregular opacity lesions on CXR results, 20 patients had intralobular linear opacity and 14 patients had interlobular linear opacity in HRCT. Large opacities were found more often using HRCT (Table 1). Emphysema was detected in 14 patients using chest x-rays, and in 53 patients using HRCT. Emphysema and pleural pathology were significantly higher statistically in HRCT than chest x-ray results (p<0.001, p<0.001).
Table 1. Distribution of lesions (McNemar Test).
| Chest radiograph (ILO) n=83 |
HRCT (ICOERD) n=83 |
p value |
|
|---|---|---|---|
| Pneumoconiosis | 72 (86.75%) | 79 (95.18%) | 0.118 |
| Round opacity | 68 (81.93%) | 71 (85.54%) | 1.000 |
| Irregular opacity | 47 (56.63%) | 78 (93.98%) | <0.001 |
| Large opacity | 12 (14.46%) | 16 (19.28%) | 0.219 |
| Pleural pathology | 4 (4.82%) | 19 (22.89%) | <0.001 |
| Emphysema | 14 (16.87%) | 53 (63.86%) | <0.001 |
ILO: International Labor Organization; ICOERD: International Classification of High-resolution Computed Tomography for Occupational and Environmental Respiratory Diseases; HRCT: High-resolution computed tomography.
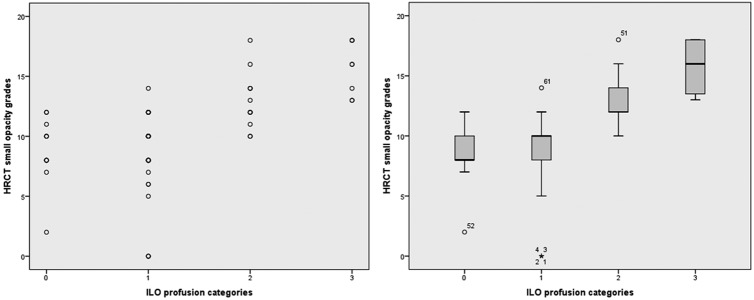
The correlation between the chest x-ray density category and the HRCT grades was statistically significant (rho=0.590; p<0.01).
HRCT grades were compared with the four groups according to the chest x-ray density categories, showing a statistically significant difference between the groups (p<0.01). With post hoc analysis we found that the difference originated from Groups 1 and 3 (Fig. 1). The ICOERD median score of patients in the ILO Category groups (0–1, 2–3) were 8 (2–12), 10 (0–14), 12 (10–18), and 16 (13–18) respectively, and found to be reported as IR.
Fig. 1.
ICOERD grades correlation graph with ILO categories (left) and box-plot (right).
The PFT test results evaluated 42 (50.6%) patients as normal, 4 (4.8%) as obstructive type, 8 (9.6%) as restrictive type, 22 (26.5%) as mixed type, 6 (7.2%) patients as small airway obstruction type, and 1 (1.2%) patient was incompatible with the test. Table 2 shows the analysis of 82 patients.
Table 2. PFT values.
| PFT | Mean n=82 |
Median n=82 |
|---|---|---|
| FEV1 (%) | 83.66 ± 22.37 | 88 (24–127) |
| FVC (%) | 86.35 ± 19.78 | 89 (43–127) |
| FEV1/FVC (%) | 78.98 ± 10.51 | 81 (37–102) |
| FEF25–75 (%) | 73.52 ± 33.72 | 72.5 (8–174) |
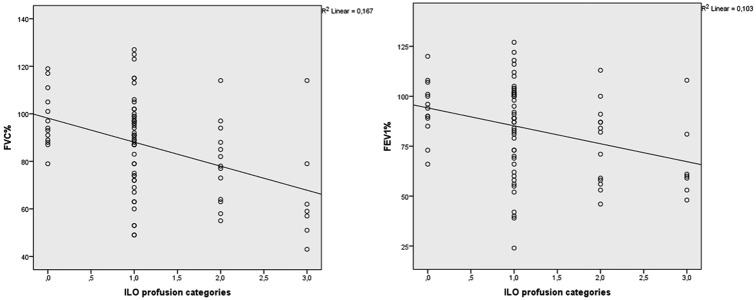
There was a negative correlation between small opacity-profusion categories on chest x-ray results with FEV1% and FVC% values (rho=−0.325, p<0.05; rho=−0.392, p<0.001) (Fig. 2).
Fig. 2.
Chest x-ray correlation graph of FEV1% and FVC% with density categories (Spearman).
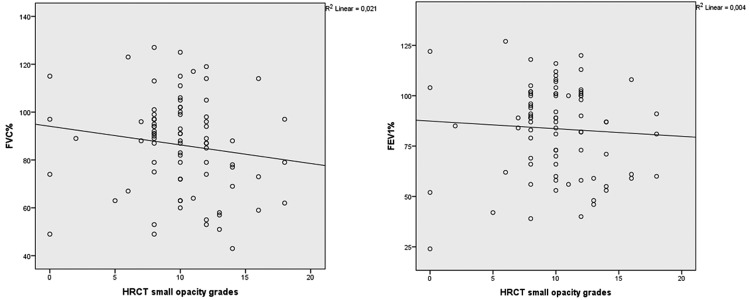
FEV1% and FVC% values decreased with the increase in HRCT small opacity grades, although there was no statistically significant correlation (rho=−0.207 p>0.05; rho=−0.128 p>0.05) (Fig. 3). The median (min–max) values of FEV1%, FVC%, and FEF25–75% of 19 patients with pleural thickening was found to be 60 (46–107), 69 (43–105) and 53 (22–128) respectively; additionally, the median values of 63 patients with no pleural thickening was found to be 91 (24–127), 92 (49–127) and 81 (8–174) respectively. These differences were statistically significant (p<0.001, p<0.001, p=0.009, respectively). There was no statistically significant difference in FEV1/FVC ratio between these two groups (p=0.304).
Fig. 3.
HRCT small opacity grades correlation graph with FVC% and FEV% (Spearman).
Discussion
The aim of our study was to compare the efficacy of chest x-ray and HRCT techniques to detect pneumoconiosis cases earlier and to investigate their relationships with pulmonary functional status. Diagnosis of pneumoconiosis was diagnosed using HRCT in seven of eleven patients without pneumoconiosis revealed by chest x-ray. In a study conducted by Lopes et al., pneumoconiosis was detected with HRCT in four cases with normal chest x-ray results15). In a similar study, 13 of 32 patients with silica exposure had normal chest radiographs while HRCT showed silicosis16). The superposition of many parenchymal regions in chest x-rays reduces the sensitivity and specificity, and in those with dust exposure, does not exclude the presence of silicosis as the chest x-ray is normal17). In our study, pneumoconiosis was reported in chest x-rays of four patients with no reported pneumoconiosis on HRCT. In our study, 44% of q opacities detected by chest x-rays were evaluated as P opacity using HRCT, thought to be related to reader diversity and superimpositions of different opacities on chest x-rays. In a study by Suganuma et al. it was shown that pulmonary specialists reported smaller opacities more often than radiologists18). In another study, it was found that cases reported as mild emphysema using HRCT may have been reported as p opacity on chest x-ray results depending on the collecting effect19).
One study showed that after occupational and environmental exposure, HRCT can detect early parenchymal changes starting from the secondary lobe and progressing to intralobular lines or subpleural curvilinear lines with the disease progression20). Similar studies demonstrated that HRCT is much more sensitive to early detection of parenchymal changes and small opacities in silicosis than are chest x-ray results21,22,23). In our work, while 47 (56.63%) of the patients had irregular opacity findings on their chest x-rays, 78 (93.98%) patients had irregular opacixxty findings using HRCT. Irregular opacity was the predominant lesion in 8 patients in the chest x-ray results, and irregular and/or linear opacity was the predominant lesion in 28 patients in the HRCT results. In 36 patients without small irregular opacity lesions on CXR results, 20 patients had intralobular linear opacity and 14 patients had interlobular linear opacity in HRCT. Pneumoconiosis can be detected with HRCT during the subclinical phase and the patient may be removed from exposure. In a similar study by Santos Antao et al., 91% of centrilobular branching was detected using HRCT and consequently the presence of small centrilobular branches in patients with silica exposure but without typical nodular patterns was reported to help early detection of pneumoconiosis24). In our study, three patients who revealed no evidence of pneumoconiosis using chest x-rays were diagnosed as pneumoconiosis using HRCT and were removed from exposure.
Large opacity lesions were more often found using HRCT but no statistical difference was found. Patients reported as having large areas of opacity using HRCT were noted to display coalescence symbols on chest x-ray films. Using HRCT, six cases with A opacity detected using chest x-rays were reported as B opacity, and four cases with B opacity were detected as C opacity. The large opacity lesions are measured in an anatomical region (at the carina level) in the ICOERD classification and are not affected like the x-ray zones by inspiration and expiration but may give more objective results. Using chest x-rays, anaphase pleural plaques may be considered as large opacities, which can be distinguished by using HRCT.
The superiority of using HRCT to chest x-rays in detecting large opacities and emphysema has been demonstrated in many studies15, 25, 26). In our study, more emphysema was detected statistically using HRCT. Emphysema was detected in 43 of 69 patients who were not reported with emphysema by use of chest x-rays. Since we included smokers in the study, we could not interpret the emphysema depending on the occupational exposure. However, 11 of 53 cases with emphysema found using HRCT had no smoking history. In the study conducted by Lopes et al., smokers were not included in the study and 61.4% of emphysema was detected using HRCT; in addition, progressive massive fibrosis presence or dense silica exposure has been demonstrated as a possible cause of emphysema15). In many other studies, the use of HRCT has been shown to be superior to using chest x-rays in determining emphysema detection and intensity10, 11).
In our study, there were no pleural pathologies other than costophrenic angle obliteration in four patients based on their chest x-ray results, but there was pleural thickening in 19 patients using HRCT. Lopes et al. found localized pleural thickening in 31.8% of patients using HRCT15). Arakawa et al. found pleural thickening (58.2% of patients) using HRCT and suggested that diffuse pleural thickening may be related to a restrictive pattern but did not achieve a definitive result27). Sun et al., in another study with 90 patients, detected pleural changes in five patients using chest x-rays and in 32 patients using HRCT17). In our study, when pleural thickening was detected in HRCT, FEV1, FVC, and FEF25-75 were significantly lower than those without pleural thickening (p<0.05).
We examined the association of spirometry results with ILO categories and ICOERD grades. On the chest x-ray, the FEV1 and FVC values decreased at a statistically significant amount as the intensity category increased; however, no correlation was found between ICOERD grades and these values. The reason for these findings is that parenchymal changes in HRCT have been detected at an early stage in which pulmonary function loss has not yet developed. Therefore, the absence of a relationship between spirometry results and ICOERD grades was considered as an expected result. Although not statistically significant, FEV1 and FVC values decreased as density increased. Chest X-ray shows small opacities at a later stage; an impairment in respiratory function is expected in this period. We thus interpreted the significant relationship between the ILO categories and FEV1 and FVC values in this way. Lopes et al. found there was no correlation between the density of small opacities and functional parameters15). In a similar study by Genevois et al., micronodular lesions detected using HRCT were not related to functional parameters28); similarly, in the study by Piirila et al., nodular lesions and functional parameters were found to be incompatible, unlike with many lesions found with HRCT29). In another study done by Santos Antao et al. there was a negative correlation between small opacity densities detected using HRCT with total lung capacity (TLC) and FVC24). In a study by Bégin et al., it was found that FVC and TLC decreased in patients with small opacity coalescence demonstrated by using HRCT30). Although density found using HRCT may be related to functional status, it may be interpreted that using HRCT does not have the advantage of evaluating respiratory functions as increased densities are also detected on chest x-ray results. In the study using the ICOERD classification, Meijer et al. reported that the presence of IR was associated with respiratory functions31). Also, in the study by Tamura et al. using ICOERD, there was no significant relationship between respiratory functions with RO and IR based on the results of multiple regression analysis, and the result of the ANOVA analysis suggested that the presence of RO is the cause of impairment of respiratory function32).
The heterogeneity of professional groups and working time in our study made it difficult to interpret the results. The fact that pulmonologists and radiologists interpreted different techniques constituted a limitation in the evaluation of classifications. Studies where all readers evaluate both techniques may give more consistent results in comparing the two techniques.
In conclusion, although the rate of detection of pneumoconiosis in early stages using HRCT is higher, when the cost, radiation exposure, and accessibility are considered there is not enough evidence to support the routine use of the ICOERD classification. Furthermore, using HRCT was not superior to chest x-rays in evaluating pulmonary functions.
Interest Statement
The authors report no conflict of interest.
References
- 1.Fraser RS, Müller NL, Colman N, Pare PD .(1999) Diagnosis of Disease of the Chest, 4th ed., 2386–484, WB Saunders Company, Philadelphia. [Google Scholar]
- 2.ILO (2000) Guidelines for the use of ILO International classification of radiographs of pneumoconioses, revised ed, International Labour Office Occupational Safety and Health Series No.22. International Labour Office, Geneva.
- 3.Akira M. (1995) Uncommon pneumoconioses: CT and pathologic findings. Radiology 197, 403–9. [DOI] [PubMed] [Google Scholar]
- 4.Kusaka Y, Hering KG, Parker JE .(2005) International Classification of HRCT for Occupational and Environmental Respiratory Diseases, 1–143, Springer Vering, Tokyo. [Google Scholar]
- 5.Tossavainen A. (2000) International expert meeting on new advances in the radiology and screening of asbestos-related diseases. Scand J Work Environ Health 26, 449–54. [PubMed] [Google Scholar]
- 6.Akgun M, Araz O, Akkurt I, Eroglu A, Alper F, Saglam L, Mirici A, Gorguner M, Nemery B. (2008) An epidemic of silicosis among former denim sandblasters. Eur Respir J 32, 1295–303. [DOI] [PubMed] [Google Scholar]
- 7.Attfield MD, Hodous TK. (1992) Pulmonary function of U.S. coal miners related to dust exposure estimates. Am Rev Respir Dis 145, 605–9. [DOI] [PubMed] [Google Scholar]
- 8.Qian QZ, Cao XK, Qian QQ, Shen FH, Wang Q, Liu HY, Tong JW. (2016) Relationship of cumulative dust exposure dose and cumulative abnormal rate of pulmonary function in coal mixture workers. Kaohsiung J Med Sci 32, 44–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hertzberg VS, Rosenman KD, Reilly MJ, Rice CH. (2002) Effect of occupational silica exposure on pulmonary function. Chest 122, 721–8. [DOI] [PubMed] [Google Scholar]
- 10.Ooi GC, Tsang KW, Cheung TF, Khong PL, Ho IW, Ip MS, Tam CM, Ngan H, Lam WK, Chan FL, Chan-Yeung M. (2003) Silicosis in 76 men: qualitative and quantitative CT evaluation—clinical-radiologic correlation study. Radiology 228, 816–25. [DOI] [PubMed] [Google Scholar]
- 11.Bégin R, Filion R, Ostiguy G. (1995) Emphysema in silica- and asbestos-exposed workers seeking compensation. A CT scan study. Chest 108, 647–55. [DOI] [PubMed] [Google Scholar]
- 12.Hnizdo E, Sluis-Cremer GK, Baskind E, Murray J. (1994) Emphysema and airway obstruction in non-smoking South African gold miners with long exposure to silica dust. Occup Environ Med 51, 557–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Talini D, Paggiaro PL, Falaschi F, Battolla L, Carrara M, Petrozzino M, Begliomini E, Bartolozzi C, Giuntini C. (1995) Chest radiography and high resolution computed tomography in the evaluation of workers exposed to silica dust: relation with functional findings. Occup Environ Med 52, 262–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.American Thoracic Society (1995) Standardization of spirometry: 1994 update. Am J Respir Crit Care Med 152, 1107–36. [DOI] [PubMed] [Google Scholar]
- 15.Lopes AJ, Mogami R, Capone D, Tessarollo B, de Melo PL, Jansen JM. (2008) High-resolution computed tomography in silicosis: correlation with chest radiography and pulmonary function tests. J Bras Pneumol 34, 264–72. [DOI] [PubMed] [Google Scholar]
- 16.Bégin R, Ostiguy G, Fillion R, Colman N. (1991) Computed tomography scan in the early detection of silicosis. Am Rev Respir Dis 144, 697–705. [DOI] [PubMed] [Google Scholar]
- 17.Sun J, Weng D, Jin C, Yan B, Xu G, Jin B, Xia S, Chen J. (2008) The value of high resolution computed tomography in the diagnostics of small opacities and complications of silicosis in mine machinery manufacturing workers, compared to radiography. J Occup Health 50, 400–5. [DOI] [PubMed] [Google Scholar]
- 18.Suganuma N, Kusaka Y, Hering KG, Vehmas T, Kraus T, Arakawa H, Parker JE, Kivisaari L, Letourneux M, Gevenois PA, Tuengerthal S, Crane MD, Shida H, Akira M, Henry DA, Nakajima Y, Hiraga Y, Itoh H, Hosoda Y. (2009) Reliability of the proposed international classification of high-resolution computed tomography for occupational and environmental respiratory diseases. J Occup Health 51, 210–22. [DOI] [PubMed] [Google Scholar]
- 19.Tamura T, Suganuma N, Hering KG, Vehmas T, Itoh H, Akira M, Takashima Y, Hirano H, Kusaka Y. (2015) Relationships (I) of International Classification of High-resolution Computed Tomography for Occupational and Environmental Respiratory Diseases with the ILO International Classification of Radiographs of Pneumoconioses for parenchymal abnormalities. Ind Health 53, 260–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Akira M, Higashihara T, Yokoyama K, Yamamoto S, Kita N, Morimoto S, Ikezoe J, Kozuka T. (1989) Radiographic type p pneumoconiosis: high-resolution CT. Radiology 171, 117–23. [DOI] [PubMed] [Google Scholar]
- 21.Mosiewicz J, Myśliński W, Złomaniec G, Czabak-Garbacz R, Krupski W, Dzida G. (2004) Diagnostic value of high resolution computed tomography in the assessment of nodular changes in pneumoconiosis in foundry workers in Lublin. Ann Agric Environ Med 11, 279–84. [PubMed] [Google Scholar]
- 22.Ferreira AS, Moreira VB, Ricardo HM, Coutinho R, Gabetto JM, Marchiori E. (2006) Progressive massive fibrosis in silica-exposed workers. High-resolution computed tomography findings. J Bras Pneumol 32, 523–8. [DOI] [PubMed] [Google Scholar]
- 23.Petrova E, Petkov D, Shoshkov P, Nachev C. (1995) The diagnostic value of conventional X-ray examination of the lungs in comparison with high-resolution computed tomography (HRCT), isotope perfusion scintigraphy and the diffusion capacity in patients with pneumoconiosis. Int J Occup Med Environ Health 8, 231–8. [PubMed] [Google Scholar]
- 24.Antao VC, Pinheiro GA, Terra-Filho M, Kavakama J, Müller NL. (2005) High-resolution CT in silicosis: correlation with radiographic findings and functional impairment. J Comput Assist Tomogr 29, 350–6. [DOI] [PubMed] [Google Scholar]
- 25.Ozmen CA, Nazaroglu H, Yildiz T, Bayrak AH, Senturk S, Ates G, Akyildiz L. (2010) MDCT findings of denim-sandblasting-induced silicosis: a cross-sectional study. Environ Health 9, 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Moreira VB, Ferreira A, Gabetto JM, Marchiori E, Lourenço PM. (2003) [Comparative study of high resolution computer-assisted tomography with chest radiograph in silicosis]. Rev Port Pneumol 9, 33–40 (in Portuguese). [DOI] [PubMed] [Google Scholar]
- 27.Arakawa H, Honma K, Saito Y, Shida H, Morikubo H, Suganuma N, Fujioka M. (2005) Pleural disease in silicosis: pleural thickening, effusion, and invagination. Radiology 236, 685–93. [DOI] [PubMed] [Google Scholar]
- 28.Gevenois PA, Sergent G, De Maertelaer V, Gouat F, Yernault JC, De Vuyst P. (1998) Micronodules and emphysema in coal mine dust or silica exposure: relation with lung function. Eur Respir J 12, 1020–4. [DOI] [PubMed] [Google Scholar]
- 29.Piirilä P, Kivisaari L, Huuskonen O, Kaleva S, Sovijärvi A, Vehmas T. (2009) Association of findings in flow-volume spirometry with high-resolution computed tomography signs in asbestos-exposed male workers. Clin Physiol Funct Imaging 29, 1–9. [DOI] [PubMed] [Google Scholar]
- 30.Bégin R, Ostiguy G, Cantin A, Bergeron D. (1988) Lung function in silica-exposed workers. A relationship to disease severity assessed by CT scan. Chest 94, 539–45. [DOI] [PubMed] [Google Scholar]
- 31.Meijer E, Tjoe Nij E, Kraus T, van der Zee JS, van Delden O, van Leeuwen M, Lammers JW, Heederik D. (2011) Pneumoconiosis and emphysema in construction workers: results of HRCT and lung function findings. Occup Environ Med 68, 542–6. [DOI] [PubMed] [Google Scholar]
- 32.Tamura T, Suganuma N, Hering KG, Vehmas T, Itoh H, Akira M, Takashima Y, Hirano H, Kusaka Y. (2015) Relationships (II) of International Classification of High-resolution Computed Tomography for Occupational and Environmental Respiratory Diseases with ventilatory functions indices for parenchymal abnormalities. Ind Health 53, 271–9. [DOI] [PMC free article] [PubMed] [Google Scholar]