Abstract
Purpose
Orbital exenteration is a psychologically and anatomically disfiguring procedure which indicated in some patients with malignant or progressive diseases of orbital and periorbital area. In this study, we reviewed 176 patients that underwent orbital exenteration.
Methods
This was a retrospective study of medical records from all patients who underwent orbital exenteration from March 1991 to March 2014 in oculoplastic department at an eye care center. Demographic data, diagnosis, site of primary involvement and technique of surgery were determined in patients.
Results
One hundred seventy-six cases of orbital exenteration were included that had documented histopathology. The age of patients ranged from 1 to 91 years (mean age ± standard deviation, 55.43 ± 27 years). Ninety-seven (55.11%) males and 79 (44.88%) females were included. Fifteen different tumors were identified. The most common indication was patients with basal cell carcinoma 49 (28%) followed by 41 (23.5%) squamous cell carcinomas, 35 (20%) retinoblastoma, and 13 (7%) adenoid cystic carcinomas. In total, adnexal malignancies were the most common tumors, secondarily involving the orbit. Eyelids 89 (50.5%) and the globe 43 (24%) were the most frequent site of involvement. Three types of exenteration were performed, based on available data of 129 operation sheets, 46 (35.7%) subtotal, 62 (48.1%) total, and 21 (16.3%) cases of extensive exenterations. In total 97 cases were evaluated pathologically for perineural involvement, of which perineural invasion was noted in 9 (7%) reports.
Conclusions
Frequency of exenteration in our center has increased in past 3 years and the majority of cases were eyelid basal cell carcinoma. Patient education considering periocular lesions can help in earlier diagnosis of malignant lesions and therefore reducing the number of exenteration.
Keywords: Basal cell carcinoma, Orbital exenterartion, Perineural
The eye is a vital organ for cosmesis and its loss evokes emotional and psychosocial responses in affected individuals [1]. Orbital exenteration is more psychologically and anatomically disfiguring than other procedures performed in the orbit because this procedure includes the removal of the orbital contents, such as bones, orbital fat, the globe, and all or portions of the eyelid. Therefore, it is used infrequently and performed only if the removal of malignant tissue increases the chance of patient survival or for pain control in the setting of rapidly growing tumor [1].
This procedure was first described by Bartisch in 1583 [2], while the first report of modern total exenteration in the early 20th century was published by Golovine [3]. In recent years, several modifications such as eyelid-sparing techniques [4], retention of the conjunctiva [5], and preservation of the periorbita [6] have been introduced for use during exenteration to aid in facial rehabilitation.
One of the largest historical series of orbital exenteration cases was published in 1989 by the Mayo Clinic and includes 102 patients seen over a 20-year period [7]. Separately, Nagendran et al. [8] reported 25 cases of orbital exenteration performed at the Massachusetts Eye and Ear Infirmary over a 10-year period, while Rahman et al. [9] analyzed 69 cases of orbital exenteration performed during a 13-year period. Mohr and Esser [10] also reported their experiences with 77 cases and Levin and Dutton [11] had 99 cases, both over a period of 20 years. Also, Naquin [12] in a 25-year review described 48 cases and Rathbun et al. [13] presented 48 cases from a 30-year period.
In this study, we review 176 cases of orbital exenteration performed at a tertiary eye care center over a 23-year period to analyze indications, histopathologic findings, site of primary involvement, and type of exenteration technique used.
Materials and Methods
In this retrospective study, the medical records of patients who had undergone exenteration of the orbit at an eye care center were reviewed from March 1991 to March 2014. All surgical records were reviewed to determine demographic data, diagnosis, indications for exenteration, and the site of primary involvement. Histopathological diagnosis and perineural invasion were obtained from histology reports. The operation notes were used to determine the type of exenteration. Exenteration was categorized as “total” if it entailed removing the orbital contents and eyelids entirety, whereas a “subtotal” exenteration spared some portion of the posterior orbital soft tissues. In “extended” exenteration, removal of bone or adjacent structures was also performed. Medical records were used to determine recurrence rate in patients. Statistical analysis was performed using IBM SPSS Statistics ver. 19 (IBM Corp., Amonk, NY, USA) and data were reported as frequencies, percentages, means, and standard deviations. Informed consent for the publication was waived, and institutional review board approval was received.
Results
A total of 176 affected orbits from 176 patients were identified, including 97 (55.1%) males and 79 (44.9%) females. The age at exenteration ranged from one to 91 years (mean age ± standard deviation, 55.43 ± 27 years).
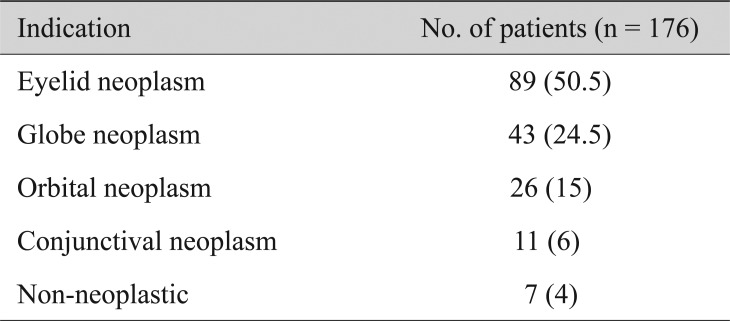
Eyelid malignancies were the most common cause of exenteration, followed by globe and orbital lesions. An overview of indications for exenteration based on primary site is presented in Table 1.
Table 1. Indications for orbital exenteration.
Values are presented as number (%).
Seven patients (4%) underwent exenteration for non-neoplastic diseases. Four patients had nonspecific orbital inflammation and three were documented (by culture) to have naso-orbital mucormycosis infections not responding to medical therapy involving the orbital apex.
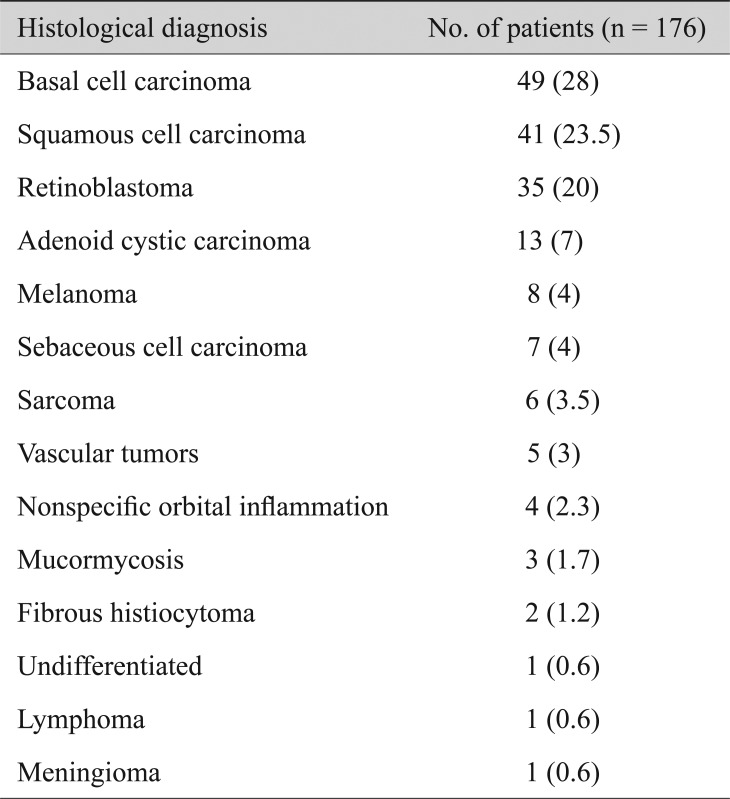
In the 176 histopathologic reports, basal cell carcinoma (BCC) was the most common finding, followed by squamous cell carcinoma (SCC), and retinoblastoma. The other tumor types are presented in Table 2.
Table 2. Histopathological diagnosis of patients undergoing exenteration.
Values are presented as number (%).
Of 89 eyelid malignancies, 49 patients had BCC, 31 had SCC, seven had sebaceous gland carcinoma (SGC), and two had malignant melanoma based on histopathologic report. Additionally, of 11 patients with conjunctival malignancies, 10 patients had SCC and one had malignant melanoma.
Case notes for tumor recurrence were available only in 47 patients. Of these patients, 23 (49%) cases of local or regional recurrence of tumors were documented. This group included eight (17%) BCC, seven (15%) SCCs, three (6%) SGC, two (4%) melanomas, one (2%) sarcoma, one (2%) retinoblastoma and one (2%) adenoid cystic carcinoma.
Data for surgical techniques were available only for 129 patients. Sixty-two (48%) patients underwent total exenteration, 46 (35.7%) patients required a subtotal exenteration and 21 (16.3%) cases underwent the extensive type of exenteration including removal of the bony orbit to ensure tumor clearance.
In total, 97 cases were evaluated pathologically for perineural involvement, of which perineural invasion was noted in nine reports (9%, 7 SCC and 2 SGC involving the eyelid). Exenterations were performed in 123 right orbits and 53 left orbits.
Discussion
Orbital exenteration is a severely disfiguring procedure that is indicated in primary orbital and adnexal malignancies that cannot be controlled by simple excision or radiotherapy. It is also occasionally indicated for nonmalignant progressive disease with intractable pain or orbital fungal infections, but the majority of cases are orbital malignancies [14]. The mean age of our patients was 55.43 ± 27 years. The mean age of patients undergoing orbital exenteration is commonly older than 50 years [8,11,15].
In our study, 169 of 176 surgeries were performed due to malignancy. Rahman et al. [9] reported that 64 of their 69 cases required exenteration for malignant disease. Other authors have published similar results in their studies: for example, Nagendran et al. [8] found 23 of 25 exenterations were for malignancies. Also, in the studies of Bartley et al. [7] (n = 100 / 102), Levin and Dutton [11] (n = 93 / 99), and Mohr and Esser [10] (n = 74 / 77), similar results were found.
Our results revealed secondary orbital invasion by eyelid neoplasms was the leading cause of exenteration (50.5%). As these malignancies are most often easily visible, patient education seems of paramount importance for the timely diagnosis and treatment of eyelid disorders, therefore reducing the rate of exenteration. The most common histopathologic report was BCC followed by SCC and retinoblastoma. This is comparable to the findings of other studies [7,9,11]. Although, in several studies concerning the Indian population, SCC and SGC were the most common adnexal tumors that needed exenteration [15,16,17], and in another study, conjunctival melanoma was the leading cause of exenteration [18]. Furthermore, in a different report, intraocular retinoblastoma was identified as the most frequent etiology (32.1%), followed by conjunctival SCC (17.9%) and BCC of the eyelid (10.7%), which probably is due to the distribution of age in the study [19]. It has been reported that the main causes of orbital exenteration vary between different geographic areas [20] and different ethnic groups due to better diagnosis or treatment [15]. In our study, 28% of exenterations were due to BCC. Varying rates of BCC have been reported in other studies: Bartley et al. [7] reported 21 of 100 (21%) cases, Mohr and Esser [10] reported six of 74 (8%) cases, Rathbun et al. [13] reported 14 of 48 (29%) cases, and Levin and Dutton [11] reported eight of 99 (8%) cases. The results of our study are consistent with these results from previous studies except in the Indian population.
As previously mentioned, orbital exenteration can be of value in some benign orbital diseases as a palliative measure. One Indication for exenteration in such cases is in patients with inflammatory orbital disease, such as nonspecific orbital inflammation, with chronic and uncontrollable pain or grossly disfiguring orbital abnormalities, such as teratomas, extensive varices, or massive optic nerve tumors as well as in patients with histologically benign tumors that may have malignant potential [1]. In our study, seven cases were exenterated for nonmalignant disease, specifically four for nonspecific orbital inflammation and three for mucormycosis. Nagendran et al. [8] reported four cases performed for palliative purposes (two orbital mucormycosis, two metastatic choroidal melanoma) and one completed to debulk a nonmalignant tumor (plexiform schwannoma).
Eighty cases of exenterations have been performed between 2011 and 2014 in our institution. This finding shows the number of cases requiring exenteration is still high and significant. Many of these patients may not have needed exenteration if their condition had been detected earlier. This may reflect the importance of patient education.
As exenteration is an anatomically and psychologically disfiguring operation with functional limitations, advances in the introduction of new and less-invasive techniques have taken place recently. For uveal melanoma, which is the most common primary ocular tumor in adults, some targeted drug therapies have been proposed [21]. Several epidermal growth factor receptor inhibitors have recently been developed and have shown efficacy in the treatment of SCC [22]. Vismodegib is a new drug that seems to have good results in treating periocular and orbital BCC [23]. Therefore, patients with advanced malignancies may soon have more treatment options than radical surgery.
As the eyes are the most important components of the face regarding aesthetics [24], the rehabilitation of patients undergoing exenteration is of importance. Patient confidence, self-esteem, and their return to normal social life are possible with the use of orbital prostheses [25]. All of our patients were consulted for rehabilitation, following near-complete epithelialization of the exposed area. Because most patients were operated on several years ago, the data for their rehabilitation are missing. Also, some patients did not have the financial support to get an orbital prosthesis. Of the patients that came for follow-up visits, 46 had prostheses. The most common type was an adhesive-retained silicone prosthesis in 40 patients, followed by six lightweight spectacle-retained acrylic prostheses.
The main limitation of our study was its retrospective design. Because exenteration is not a common surgical procedure, designing a prospective study for this topic is difficult. Some of the exenterations included were performed at least 20 years ago; therefore, obtaining detailed information was difficult and some data were missing.
In conclusion, the frequency of exenteration in our center has increased in the past three years and the majority of cases were eyelid BCC. Patient education considering periocular lesions can help in an earlier diagnosis of malignant lesions and therefore in reducing the number of exenterations performed.
Footnotes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
References
- 1.Rose GE, Wright JE. Exenteration for benign orbital disease. Br J Ophthalmol. 1994;78:14–18. doi: 10.1136/bjo.78.1.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bartisch G. Ophthalmodoulcia. Dresden. 1583;3:208. [Google Scholar]
- 3.Golovine SS. Orbito-sinus exenteration. Ann Ocul. 1909;141:413–431. [Google Scholar]
- 4.Shields JA, Shields CL, Suvarnamani C, et al. Orbital exenteration with eyelid sparing: indications, technique, and results. Ophthalmic Surg. 1991;22:292–297. [PubMed] [Google Scholar]
- 5.Frezzotti R, Nuti A. Repair after orbital exenteration. Personal technique. Acta Neurochir (Wien) 1982;60:119–124. doi: 10.1007/BF01401757. [DOI] [PubMed] [Google Scholar]
- 6.Shore JW, Burks R, Leone CR, Jr, McCord CD., Jr Dermis-fat graft for orbital reconstruction after subtotal exenteration. Am J Ophthalmol. 1986;102:228–236. doi: 10.1016/0002-9394(86)90150-9. [DOI] [PubMed] [Google Scholar]
- 7.Bartley GB, Garrity JA, Waller RR, et al. Orbital exenteration at the Mayo Clinic. 1967–1986. Ophthalmology. 1989;96:468–473. doi: 10.1016/s0161-6420(89)32872-7. [DOI] [PubMed] [Google Scholar]
- 8.Nagendran ST, Lee NG, Fay A, et al. Orbital exenteration: the 10-year Massachusetts Eye and Ear Infirmary experience. Orbit. 2016;35:199–206. doi: 10.1080/01676830.2016.1176210. [DOI] [PubMed] [Google Scholar]
- 9.Rahman I, Cook AE, Leatherbarrow B. Orbital exenteration: a 13 year Manchester experience. Br J Ophthalmol. 2005;89:1335–1340. doi: 10.1136/bjo.2004.062471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mohr C, Esser J. Orbital exenteration: surgical and reconstructive strategies. Graefes Arch Clin Exp Ophthalmol. 1997;235:288–295. doi: 10.1007/BF01739638. [DOI] [PubMed] [Google Scholar]
- 11.Levin PS, Dutton JJ. A 20-year series of orbital exenteration. Am J Ophthalmol. 1991;112:496–501. doi: 10.1016/s0002-9394(14)76848-5. [DOI] [PubMed] [Google Scholar]
- 12.Naquin HA. Exenteration of the orbit. AMA Arch Ophthalmol. 1954;51:850–862. doi: 10.1001/archopht.1954.00920040860011. [DOI] [PubMed] [Google Scholar]
- 13.Rathbun JE, Beard C, Quickert MH. Evaluation of 48 cases of orbital exenteration. Am J Ophthalmol. 1971;72:191–199. doi: 10.1016/0002-9394(71)91613-8. [DOI] [PubMed] [Google Scholar]
- 14.Kennedy RE. Indications and surgical techniques for orbital exenteration. Adv Ophthalmic Plast Reconstr Surg. 1992;9:163–173. [PubMed] [Google Scholar]
- 15.Maheshwari R. Review of orbital exenteration from an eye care centre in Western India. Orbit. 2010;29:35–38. doi: 10.3109/01676830903234020. [DOI] [PubMed] [Google Scholar]
- 16.Pushker N, Kashyap S, Balasubramanya R, et al. Pattern of orbital exenteration in a tertiary eye care centre in India. Clin Exp Ophthalmol. 2004;32:51–54. doi: 10.1046/j.1442-9071.2004.00757.x. [DOI] [PubMed] [Google Scholar]
- 17.Sihota R, Tandon K, Betharia SM, Arora R. Malignant eyelid tumors in an Indian population. Arch Ophthalmol. 1996;114:108–109. doi: 10.1001/archopht.1996.01100130104031. [DOI] [PubMed] [Google Scholar]
- 18.Shields JA, Shields CL, Demirci H, et al. Experience with eyelid-sparing orbital exenteration: the 2000 Tullos O. Coston Lecture. Ophthalmic Plast Reconstr Surg. 2001;17:355–361. doi: 10.1097/00002341-200109000-00010. [DOI] [PubMed] [Google Scholar]
- 19.Ben L, Aemero M, Gushchin AG, et al. Clinico-pathological patterns of patients who underwent orbital exenteration in a tertiary eye hospital of Nepal. Ethiop J Health Sci. 2016;26:543–548. doi: 10.4314/ejhs.v26i6.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kaur A, Khattri M, Jaiswal V. Pattern of orbital exenteration at a tertiary eye care centre in North India. Nepal J Ophthalmol. 2012;4:64–67. doi: 10.3126/nepjoph.v4i1.5853. [DOI] [PubMed] [Google Scholar]
- 21.Goh AY, Layton CJ. Evolving systemic targeted therapy strategies in uveal melanoma and implications for ophthalmic management: a review. Clin Exp Ophthalmol. 2016;44:509–519. doi: 10.1111/ceo.12688. [DOI] [PubMed] [Google Scholar]
- 22.El-Sawy T, Sabichi AL, Myers JN, et al. Epidermal growth factor receptor inhibitors for treatment of orbital squamous cell carcinoma. Arch Ophthalmol. 2012;130:1608–1611. doi: 10.1001/archophthalmol.2012.2515. [DOI] [PubMed] [Google Scholar]
- 23.Gill HS, Moscato EE, Chang AL, et al. Vismodegib for periocular and orbital basal cell carcinoma. JAMA Ophthalmol. 2013;131:1591–1594. doi: 10.1001/jamaophthalmol.2013.5018. [DOI] [PubMed] [Google Scholar]
- 24.Pathak C, Pawah S, Singh G, et al. Prosthetic rehabilitation of completely blind subject with bilateral customised ocular prosthesis: a case report. J Clin Diagn Res. 2017;11:ZD06–ZD08. doi: 10.7860/JCDR/2017/24434.9151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hatamleh MM, Haylock C, Hollows P, et al. Prosthetic eye rehabilitation and management of completely blind patients. Int J Prosthodont. 2012;25:631–635. [PubMed] [Google Scholar]