ABSTRACT
Background
Nutrients are added to the diet through fortification/enrichment and dietary supplements (DSs). Meeting the US Dietary Reference Intakes (DRIs) varies by nutrient and population subsegments.
Objective
The aim of this study was to assess the relative role of naturally occurring, enriched/fortified, and DS sources of 15 micronutrients with reference to the DRIs.
Methods
We used the NHANES 2009–2012 (≥2 y old, n = 16,975) data, the ILSI North America Fortification database, and the National Cancer Institute usual intake method.
Results
Prevalence of nutrient intake from naturally occurring sources below the Estimated Average Requirement (EAR) varied from 5% for vitamin B-12 to 100% for vitamin D, with ≥40% of the population below the EAR for 8 of the 14 nutrients (ages ≥2 y). With enrichment/fortification, the percentage below the EAR decreased to the following for vitamins A (35%), C (34%), and B-6 (7%), folate (8%), thiamin (5%), riboflavin (3%), niacin (1%), and iron (2%). Nutrients from DSs further improved intakes related to the EAR for 12 nutrients (ages ≥2 y). For 9–18-y-olds, the percentages of nutrient intakes below the EAR were 14–50% higher than for 2–8-y-olds. The Tolerable Upper Intake Level (UL) was exceeded among children aged 2–8 y for folate (41.7%), niacin (10.1%), and zinc (39.9%), whereas among ages ≥2 y and 9–18 y no prevalence of intakes over the UL exceeded 10%.
Conclusions
Fortification/enrichment constitutes a meaningful contribution to reducing the percentage of individuals with less than the EAR for their demographic. These data underscore the need to encourage better dietary patterns to improve the intake of nutrients at risk of low intake.
Keywords: NHANES, dietary, dietary supplements, fortification/enrichment, United States
Introduction
The US Dietary Guidelines for Americans 2015–2020 (1) recommend a healthy eating pattern with appropriate calorie intake that includes nutrient-dense foods and limited intake of sodium, saturated fats, and added sugar across the life span. However, Healthy Eating Index scores from 2010 show that only 57.8% of Americans adhere to the Dietary Guidelines (1). Four nutrients for which intakes are low (calcium, potassium, dietary fiber, and vitamin D) were reported to be of public health concern by the Dietary Guidelines Advisory Committee (DGAC) in 2015 (2). Low intake of iron is also of public health concern for young children and pregnant women or those of childbearing age (2).
The US food supply has long included foods that are enriched and/or fortified with specific nutrients to replace nutrients lost during processing (enrichment) and to increase nutrient amounts to reduce the risk of nutrient deficiencies (fortification) (3, 4). Earlier work has identified the important contribution of fortification to vitamin and mineral intakes in the United States (5, 6). More recent studies have discussed concern about excessive intakes as a result of fortification and called attention to the complexities of interpreting the Tolerable Upper Intake Level (UL) (4, 7), yet intake of some micronutrients in the United States continues to not meet national recommendations (4).
Fulgoni et al. (8) evaluated the contribution of 19 micronutrients from naturally occurring sources, as well as those added to foods through fortification and enrichment plus dietary supplements (DSs), among persons ≥2 y of age in the US population using the 2003–2006 NHANES. When comparing estimated usual intakes to the DRIs, these authors reported intakes from enriched and fortified foods below the Estimated Average Requirements (EARs) for vitamins A (45%), C (37%), D (93%), and E (91%), calcium (49%), and magnesium (55%) (8). When these authors also considered DS intake, a lower percentage of the population recounted intakes of specific nutrients below the EAR. These authors reported that meeting recommended intakes for vitamins A, C, and D, thiamin, iron, and folate was primarily due to enrichment and/or fortification (8). Fulgoni et al. (8) found that the prevalence of intakes of niacin and zinc were appreciably above the UL for the population (10.3% and 8.4%, respectively).
The objective of the current study was to estimate the relative contribution, in the US diet, of naturally occurring, enriched/fortified, and DS sources of 15 micronutrients in meeting or exceeding appropriate DRIs for various age groups using the 2009–2010 and 2011–2012 NHANES and the National Cancer Institute (NCI) usual intake estimation method. These results will provide an update of information on the contribution of fortification/enrichment and DS use (6, 8) to meeting the DRIs in the US diet.
Methods
Study population and nutrients
Dietary and individual DS intake information reported over two 24-h periods for 2 consecutive NHANES cycles (2009–2010, 2011–2012) (9) was coupled with the USDA food patterns equivalents database for analysis alone and in combination with the North American branch of the International Life Sciences Institute (ILSI North America) Fortification database (10).
The NHANES is a nationally representative cross-sectional survey that samples noninstitutionalized civilian US residents using a complex, stratified, multistage probability cluster sampling design and is collected by the National Center for Health Statistics (11). Food and beverage items reported consumed in the NHANES dietary interview component (What We Eat in America) were coded using the USDA's Food and Nutrient Database for Dietary Studies (FNDDS) and their estimated nutrient content was obtained (12).
The NHANES dietary data include two 24-h dietary recalls collected using a computer-assisted dietary interview software program: the USDA's automated multiple-pass method. The first 24-h dietary recall is conducted as an in-person interview and the second is administered by telephone 3–10 d later. At the time of the initial dietary interview, participants are asked to show the interviewer the DSs they are currently consuming and details of intake amount and frequency as well as product label information are recorded. Although complete 24-h dietary intake data were available for 20,293 participants, after exclusion of those <2 y of age (n = 1371) and participants whose data were deemed by the interviewer to be incomplete (n = 1947), the analytic sample included a total of 16,975 participants ≥2 y of age. Included in the total participants were children 2–8 y of age (n = 2871) and 9–18 y of age (n = 3238). In the total sample, 49.96% were male.
We also used the ILSI North America Fortification database (10), which contains estimates of nutrients available from 3 sources—as naturally occurring (i.e., intrinsic), enriched, and fortified—for those foods and beverages as reported in 2 NHANES cycles (2009–2010 and 2011–2012) and based on the USDA's FNDDS. The NHANES individual food intake files were merged with the ILSI North America Fortification database, which contained nutrient proportions according to the 3 sources. The total amount of each nutrient in the specified food/beverage level (naturally occurring, +enrichment/fortification, +DSs) for the analysis was calculated by multiplying the number of grams per nutrient from the NHANES food file and the nutrient proportion in the ILSI North America Fortification database, then dividing by 100. These values were then summed by level for each NHANES participant to yield the total intake by nutrient and amount per 100 g. During analyses we verified selected results with other published tables of NHANES data and found them to be comparable (13).
Usual intake estimation
Data obtained from the two 24-h recalls were used to estimate prevalence of intake using the NCI usual intake estimation methodology (14, 15). The NCI's MIXTRAN and DISTRIB computer macro enables usual intake estimation at the individual level. As part of our analysis, we incorporated/controlled for age, interview day (first compared with second), and weekend day (yes/no), to account for weekend effects in intake. Similarly to Fulgoni et al.’s study (8), for estimates of total nutrient intake, the usual intake macros were run before the addition of DS data to the enriched/fortified nutrient amounts.
Estimated usual intake data were generated from 1) foods and beverages only as naturally occurring, 2) foods and beverages including those with enrichment/fortification, and 3) all foods and beverages including enrichment/fortification and DSs for vitamins A, D, E, C, B-6, and B-12, folate, thiamin, riboflavin, niacin, iron, zinc, calcium, magnesium, and potassium, for each of which an EAR [or an Adequate Intake (AI) for potassium] was established. Percentage below the EAR as well as means and percentiles of intake for the nutrients of interest are presented. Percentage above the AI was estimated for potassium. DS data were not available for vitamins A and E for the NHANES cycles used in this analysis. Also estimated was percentage greater than or equal to the UL, as appropriate. Dietary folate equivalents were used for folic acid and folate (16). The ULs for the niacin, magnesium, and folate dietary folate equivalents were derived from nonfood sources (enrichment/fortification or supplements) (16, 17). DRI ULs have not been set for thiamin, riboflavin, potassium, and vitamins A, E, and B-12 (16, 18, 19).
For all other nutrients, the proportions of the population with intakes greater than or equal to the ULs were estimated using naturally occurring (all foods and beverages excluding enriched/fortified), enriched/fortified, and DS sources.
Statistical analysis
We accounted for the NHANES clustered sampling design and oversampling in all analyses and adjusted for differential noncoverage and nonresponse across the 2 continuous NHANES cycles (20–22). Frequencies, row percentages, and column percentages were reported for sample size. Means and SEs were calculated for average usual intake, percentage below the EAR, and percentage greater than or equal to the UL. SEs were estimated using Balanced Repeated Replication and NHANES weights were applied. The age groups analyzed include ≥2, 2–8, and 9–18 y of age for both sexes combined. All analyses were conducted using SAS version 9.4 and its complex survey-specific procedures (SAS Institute) and a P value < 0.05 was considered statistically significant. Because this study was a secondary data analysis of publicly available federal data, Human Subject Institutional Review Board approval was not required by the Medical University of South Carolina.
Results
Total nutrient intake from all food and beverage sources including DSs among individuals ≥2 y of age
Table 1 reports the national mean intake of 15 nutrients from food and beverage items among the US population ≥2 y of age over 2 d, by source (naturally occurring, enriched/fortified, enriched/fortified plus DSs) and percentage below the EAR. The percentage of the population ≥2 y of age with nutrient intakes from naturally occurring sources below the EAR varied from 5% for vitamin B-12 to 100% for vitamin D, with ≥40% of the population below the EAR for 8 of the 14 nutrients. With the addition of nutrients estimated as added by enrichment/fortification, the percentage of usual intakes below the EAR decreased for the population for all 14 nutrients, considerably so for vitamins A (65–35%), C (50–34%), and B-6 (15–7%), folate (81–8%), thiamin (41–5%), riboflavin (13–3%), niacin (9–1%), and iron (14–2%).
TABLE 1.
Usual intake from NHANES 2009–2012 for nutrients as naturally occurring, enriched/fortified, and DSs among individuals ≥2 y of age in the US population, compared with the DRIs1
| Percentiles | |||||||
|---|---|---|---|---|---|---|---|
| Nutrient | Usual intake2 | 10 | 25 | 50 | 75 | 90 | % < EAR3 |
| Vitamin A,4,5 μg RAEs/d | |||||||
| Naturally occurring | 433 ± 0.0 | 224 | 299 | 403 | 534 | 679 | 65.1 ± 9.0 |
| +Enriched/fortified | 646 ± 0.0 | 334 | 447 | 605 | 799 | 1011 | 35.1 ± 1.6 |
| Vitamin D,6,7 μg/d | |||||||
| Naturally occurring | 1.6 ± 0.0 | 0.8 | 1.0 | 1.5 | 2.0 | 2.7 | 100 ± 0.0 |
| +Enriched/fortified | 5.4 ± 0.0 | 2.3 | 3.3 | 4.9 | 6.9 | 9.2 | 92.9 ± 0.6 |
| +DSs | 1.2 ± 0.0 | 2.5 | 3.8 | 6.0 | 11.1 | 21.5 | 72.5 ± 0.6 |
| Vitamin E,5,8 mg AT/d | |||||||
| Naturally occurring | 7.2 ± 0.0 | 4.0 | 5.2 | 6.8 | 8.8 | 10.9 | 85.5 ± 0.6 |
| +Enriched/fortified | 7.9 ± 0.0 | 4.3 | 5.6 | 7.4 | 9.6 | 12.0 | 79.6 ± 0.6 |
| Vitamin C,8 mg/d | |||||||
| Naturally occurring | 62 ± 0.0 | 21 | 33 | 53 | 81 | 114 | 50.1 ± 1.2 |
| +Enriched/fortified | 85 ± 0.0 | 32 | 49 | 74 | 110 | 151 | 33.7 ± 0.8 |
| +DSs | 135 ± 0.2 | 35 | 55 | 88 | 137 | 212 | 26.7 ± 0.6 |
| Vitamin B-6,9 mg/d | |||||||
| Naturally occurring | 1.6 ± 0.0 | 0.9 | 1.2 | 1.5 | 1.9 | 2.3 | 14.7 ± 0.6 |
| +Enriched/fortified | 2.0 ± 0.0 | 1.2 | 1.5 | 1.9 | 2.4 | 2.9 | 6.7 ± 0.4 |
| +DSs | 3.8 ± 0.0 | 1.2 | 1.6 | 2.1 | 3.0 | 4.6 | 5.0 ± 0.4 |
| Vitamin B-12,9 μg/d | |||||||
| Naturally occurring | 4.1 ± 0.0 | 2.2 | 2.9 | 3.8 | 5.0 | 6.2 | 4.5 ± 0.4 |
| +Enriched/fortified | 5.3 ± 0.0 | 2.7 | 3.6 | 4.9 | 6.5 | 8.2 | 2.1 ± 0.2 |
| +DSs | 30.1 ± 0.2 | 2.9 | 4.0 | 5.6 | 8.6 | 16.0 | 1.6 ± 0.2 |
| Folate,9,10 μg DFEs/d | |||||||
| Naturally occurring | 207 ± 0.0 | 113 | 148 | 196 | 254 | 316 | 81.3 ± 0.6 |
| +Enriched/fortified | 548 ± 0.0 | 318 | 404 | 521 | 662 | 814 | 7.5 ± 0.6 |
| +DSs | 694 ± 0.0 | 336 | 434 | 581 | 830 | 1213 | 5.8 ± 0.4 |
| Thiamin,9 mg/d | |||||||
| Naturally occurring | 0.9 ± 0.0 | 0.6 | 0.7 | 0.9 | 1.1 | 1.4 | 41.2 ± 1.2 |
| +Enriched/fortified | 1.6 ± 0.0 | 1.0 | 1.2 | 1.6 | 1.9 | 2.3 | 5.0 ± 0.4 |
| +DSs | 3.5 ± 0.0 | 1.0 | 1.3 | 1.7 | 2.3 | 3.1 | 3.9 ± 0.2 |
| Riboflavin,9 mg/d | |||||||
| Naturally occurring | 1.5 ± 0.0 | 0.9 | 1.1 | 1.5 | 1.9 | 2.3 | 13.1 ± 0.8 |
| +Enriched/fortified | 2.1 ± 0.0 | 1.2 | 1.6 | 2.0 | 2.5 | 3.1 | 2.9 ± 0.2 |
| +DSs | 3.3 ± 0.0 | 1.3 | 1.7 | 2.2 | 3.0 | 4.0 | 2.4 ± 0.2 |
| Niacin,9 mg/d | |||||||
| Naturally occurring | 17.1 ± 0.0 | 9.8 | 12.7 | 16.4 | 20.8 | 25.2 | 8.7 ± 0.6 |
| +Enriched/fortified | 24.2 ± 0.0 | 14.6 | 18.4 | 23.3 | 29.0 | 34.8 | 1.2 ± 0.2 |
| +DSs | 30.0 ± 0.0 | 15.2 | 19.3 | 25.2 | 33.4 | 43.7 | 0.9 ± 0.2 |
| Iron,4 mg/d | |||||||
| Naturally occurring | 9.1 ± 0.0 | 5.6 | 7.0 | 8.8 | 10.8 | 12.9 | 13.8 ± 0.6 |
| +Enriched/fortified | 15.0 ± 0.0 | 9.2 | 11.4 | 14.4 | 18.0 | 21.7 | 1.8 ± 0.2 |
| +DSs | 17.6 ± 0.0 | 9.4 | 11.8 | 15.1 | 19.6 | 27.6 | 1.4 ± 0.2 |
| Zinc,4 mg/d | |||||||
| Naturally occurring | 10.0 ± 0.0 | 6.2 | 7.7 | 9.6 | 12.0 | 14.4 | 20.9 ± 1.0 |
| +Enriched/fortified | 11.1 ± 0.0 | 6.8 | 8.4 | 10.6 | 13.3 | 16.1 | 15.8 ± 0.8 |
| +DSs | 13.7 ± 0.0 | 7.1 | 8.9 | 11.6 | 15.7 | 22.9 | 12.7 ± 0.6 |
| Calcium,6,7 mg/d | |||||||
| Naturally occurring | 946 ± 0.0 | 553 | 704 | 904 | 1142 | 1391 | 46.4 ± 1.2 |
| +Enriched/fortified | 1026 ± 0.0 | 594 | 759 | 979 | 1241 | 1516 | 39.1 ± 1.0 |
| +DSs | 1122 ± 0.0 | 630 | 809 | 1052 | 1353 | 1696 | 32.5 ± 0.8 |
| Magnesium,7 mg/d | |||||||
| Naturally occurring | 281 ± 0.0 | 170 | 213 | 269 | 336 | 406 | 44.9 ± 0.8 |
| +Enriched/fortified | 284 ± 0.0 | 172 | 215 | 272 | 341 | 412 | 43.8 ± 1.0 |
| +DSs | 299 ± 0.0 | 175 | 221 | 282 | 357 | 438 | 39.8 ± 0.8 |
| Potassium,11,12 mg/d | % > AI | ||||||
| Naturally occurring | 2566 ± 1.0 | 1598 | 1990 | 2491 | 3059 | 3630 | 2.1 ± 0.2 |
| +Enriched/fortified | 2581 ± 1.0 | 1610 | 2003 | 2505 | 3076 | 3650 | 2.2 ± 0.4 |
| +DSs | 2590 ± 1.0 | 1615 | 2009 | 2514 | 3086 | 3662 | 2.2 ± 0.4 |
Source: reference 9 (n = 16,975 individuals ≥2 y of age, including pregnant and lactating women). SEM < 0.01 where SEM is 0.0 in the table. AI, Adequate Intake; AT, α-tocopherol; DFE, dietary folate equivalent; DS, dietary supplement; EAR, Estimated Average Requirement; RAE, retinol activity equivalent.
Values are mean ± SEM and percentiles for usual intakes are estimated using the National Cancer Institute method (14, 15).
For DRIs, see reference 19.
A supplements file is not currently available for vitamins A and E in NHANES for 2009–2012, and it will be released at a later date.
For DRIs, see reference 24.
For DRIs, see reference 17.
For DRIs, see reference 18.
For DRIs, see reference 16.
Folate EAR is presented as DFEs. 1 DFE = 1 μg food folate = 0.6 μg of folic acid from fortified food or supplement consumed with food = 5 μg of a supplement taken on an empty stomach.
For DRIs, see reference 23.
The AI approach was used for potassium (23).
After the addition of estimated nutrients from reported use of DSs into the total intake estimates, the percentage of estimated intakes below the EAR decreased further for 12 nutrients with the largest reduction observed for vitamin D (93–73%). However, for 4 nutrients ≥25% of the population had total estimated intakes below the EAR after the inclusion of estimated nutrients from DSs: vitamin D (73%), vitamin C (27%), calcium (33%), and magnesium (40%). The percentages of the population with total estimated intakes below the EAR were 13% for zinc, 6% for folate, 5% for vitamin B-6, and 4% for thiamin. Smaller proportions (<3%) of the population had total intakes below the EAR for vitamin B-12, riboflavin, niacin, and iron.
Only 2% of the population had total usual intakes that exceeded the AI for potassium. A small percentage of the population exceeded the AI for total usual intakes of potassium from naturally occurring sources (2.1%), and this increased only slightly to 2.2% after enrichment/fortification and did not change after the addition of DSs. These AI data can be interpreted as there being a low probability of inadequacy for the populations assessed (23).
Percentage of the population with mean intakes below the EAR by age group
Figure 1 and Supplemental Tables 1 and 2 include the relative estimated nutrient intakes from naturally occurring sources, enriched and fortified sources, and enriched and fortified sources plus DSs among US individuals by age groups including ≥2 y of age (Figure 1A), 2–8 y of age (Figure 1B), and 9–18 y of age (Figure 1C). The differences with enrichment/fortification/supplementation for the US population ≥2 y of age have already been described.
FIGURE 1.
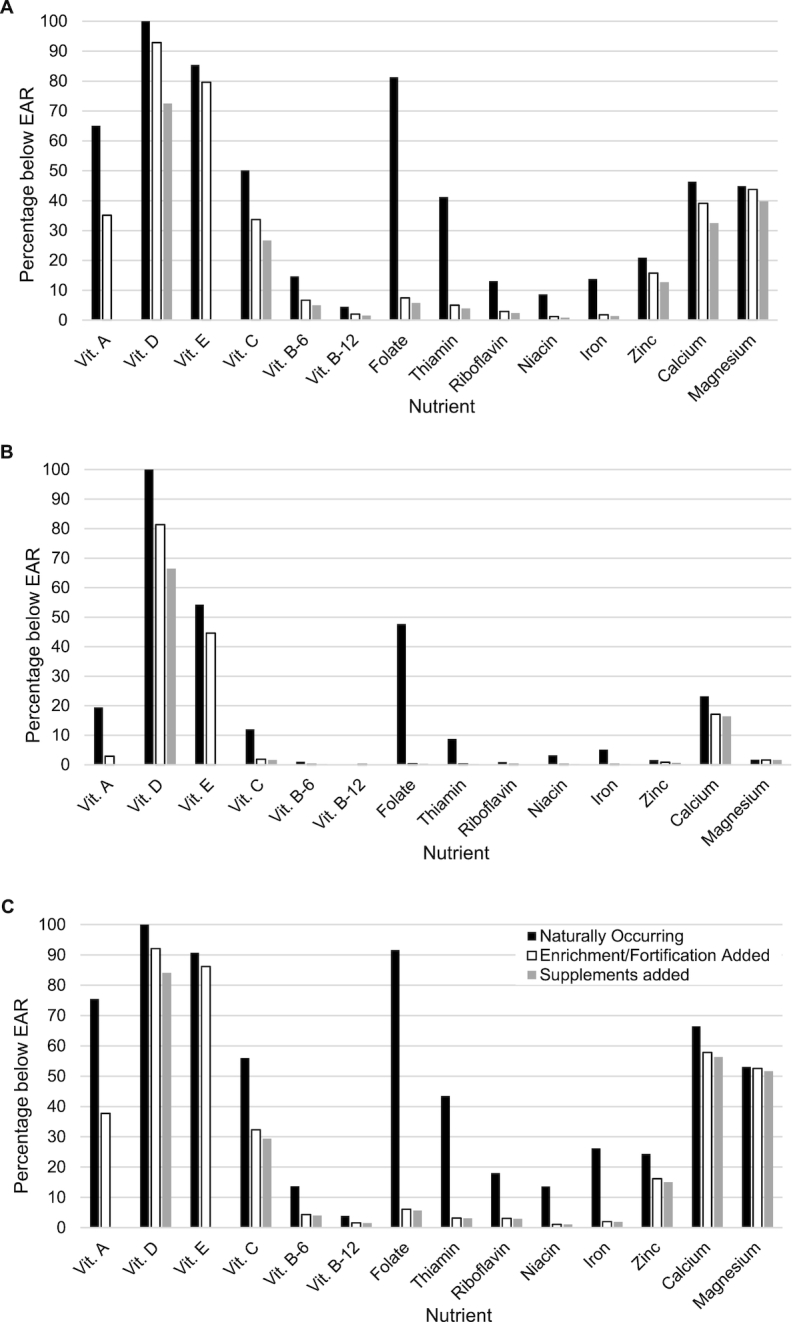
Percentage of the population with mean nutrient intakes from sources as naturally occurring, enriched/fortified, and DSs below the EAR by age group, among individuals ≥2 y of age including pregnant and lactating women (n = 16,975) (A), 2–8 y of age (n = 2871) (B), and 9–18 y of age (n = 3238) (C). Data are from reference 9. Values are mean ± SEM for the percentage below the EAR (16–19, 24). DS information is not currently available for vitamins A and E in NHANES for 2009–2012, and it will be released at a later date. Usual intakes were estimated using the National Cancer Institute method (14, 15). DS, dietary supplement; EAR, Estimated Average Requirement; Vit, vitamin.
Figure 1B illustrates the intake of younger children and Figure 1C that of older children and adolescents. The percentage of 2–8- and 9–18-y-olds with total usual intakes from naturally occurring sources below the EAR was consistent only for vitamin D (100%). Compared with 2–8-y-olds, the percentages of usual intakes below the EAR from naturally occurring sources were higher among 9–18-y-olds for all nutrients: vitamins A (76% compared with 19%), E (91% compared with 54%), C (56% compared with 12%), B-6 (14% compared with 1%), and B-12 (4% compared with 0.1%), folate (92% compared with 48%), thiamin (44% compared with 9%), riboflavin (18% compared with 0.9%), niacin (14% compared with 3%), iron (26% compared with 5%), zinc (24% compared with 2%), calcium (67% compared with 23%), and magnesium (53% compared with 2%).
After enrichment/fortification and the addition of reported DSs, the percentage of children with total usual intake of the 14 nutrients below the EAR remained higher for 9–18-y-olds than for 2–8-y-olds, and particularly for vitamins A (38% compared with 3%), D (84% compared with 67%), E (86% compared with 45%), and C (29% compared with 2%) as well as zinc (15% compared with 0.7%), calcium (56% compared with 16%), and magnesium (52% compared with 2%). The percentage of both 9–18-y-olds (92–84%) and 2–8-y-olds (81–67%) with usual intakes of vitamin D below the EAR declined more with the addition of DSs than with fortification/enrichment alone.
Children 2–8 y of age had a greater percentage of total usual intakes from naturally occurring sources exceeding the AI for potassium than 9–18-y-olds (6% and 0.4%, respectively) as well as usual intakes after enrichment/fortification and the addition of DSs.
Mean intakes above the ULs by age group
Table 2 displays the percentage of estimated nutrient intakes from naturally occurring sources, enriched and fortified sources, and enriched and fortified sources plus DSs among individuals that exceeded the ULs in the US population by the 3 age groups. For all age groups, for those nutrients where a UL is available, intake exceeding the UL from nutrients naturally occurring in food and beverages was only seen at a negligible level for calcium at 0.1% (≥2 y of age and 2–8 y of age). It was higher for zinc at 4.6% (≥2 y of age) with the highest percentage exceeding the UL among young children 2–8 y of age (27.2%), yet there was no evidence of zinc intake above the UL among older children 9–18 y of age. A UL is not available for naturally occurring sources of folate, niacin, or magnesium.
TABLE 2.
Usual intake from NHANES 2009–2012 compared with the ULs for intake of nutrients as naturally occurring, enriched/fortified, and DSs in the US population, by age group1
| % ≥ UL2 | |||
|---|---|---|---|
| Nutrient | ≥2 y of age | 2–8 y of age | 9–18 y of age |
| Vitamin D,3,4 μg/d | |||
| Naturally occurring | 0.0 ± 0.0 | 0.0 ± 0.0 | 0.0 ± 0.0 |
| +Enriched/fortified | 0.0 ± 0.0 | 0.0 ± 0.0 | 0.0 ± 0.0 |
| +DSs | 0.5 ± 0.0 | 0.0 ± 0.0 | 0.0 ± 0.0 |
| Vitamin C,5 mg/d | |||
| Naturally occurring | 0.0 ± 0.0 | 0.0 ± 0.0 | 0.0 ± 0.0 |
| +Enriched/fortified | 0.0 ± 0.0 | 0.0 ± 0.0 | 0.0 ± 0.0 |
| +DSs | 0.3 ± 0.0 | 0.4 ± 0.0 | 0.0 ± 0.0 |
| Vitamin B-6,6 mg/d | |||
| Naturally occurring | 0.0 ± 0.0 | 0.0 ± 0.0 | 0.0 ± 0.0 |
| +Enriched/fortified | 0.0 ± 0.0 | 0.0 ± 0.0 | 0.0 ± 0.0 |
| +DSs | 0.5 ± 0.0 | 0.0 ± 0.0 | 0.0 ± 0.0 |
| Folate,6,7 μg DFEs/d | |||
| Naturally occurring | — | — | — |
| +Enriched/fortified | 8.8 ± 0.6 | 41.7 ± 1.8 | 8.7 ± 1.4 |
| +DSs | 19.8 ± 0.4 | 52.4 ± 1.4 | 15.6 ± 1.2 |
| Niacin,6 mg/d | |||
| Naturally occurring | — | — | — |
| +Enriched/fortified | 1.9 ± 0.2 | 10.1 ± 0.6 | 0.8 ± 0.2 |
| +DSs | 6.9 ± 0.2 | 18.5 ± 0.6 | 4.3 ± 0.2 |
| Iron,8 mg/d | |||
| Naturally occurring | 0.0 ± 0.0 | 0.0 ± 0.0 | 0.0 ± 0.0 |
| +Enriched/fortified | 0.0 ± 0.0 | 0.0 ± 0.0 | 0.0 ± 0.0 |
| +DSs | 2.0 ± 0.0 | 0.9 ± 0.0 | 0.8 ± 0.0 |
| Zinc,8 mg/d | |||
| Naturally occurring | 4.6 ± 0.2 | 27.2 ± 0.8 | 0.0 ± 0.0 |
| +Enriched/fortified | 6.8 ± 0.2 | 39.9 ± 1.2 | 0.2 ± 0.0 |
| +DSs | 9.4 ± 0.2 | 46.3 ± 1.0 | 2.2 ± 0.0 |
| Calcium,3,4 mg/d | |||
| Naturally occurring | 0.1 ± 0.0 | 0.1 ± 0.0 | 0.0 ± 0.0 |
| +Enriched/fortified | 0.3 ± 0.0 | 0.2 ± 0.0 | 0.0 ± 0.0 |
| +DSs | 2.6 ± 0.2 | 0.3 ± 0.0 | 0.0 ± 0.0 |
| Magnesium,4 mg/d | |||
| Naturally occurring | — | — | — |
| +Enriched/fortified | 0.0 ± 0.0 | 0.0 ± 0.0 | 0.0 ± 0.0 |
| +DSs | 0.7 ± 0.0 | 0.1 ± 0.0 | 0.0 ± 0.0 |
Source: reference 9 (n = 16,975 individuals ≥2 y of age, including pregnant and lactating women; 2–8 y of age: n = 2871; 9–18 y of age: n = 3238). SEM < 0.01 where SEM is 0.0 in the table. DFE, dietary folate equivalent; DS, dietary supplement; UL, Tolerable Upper Intake Level.
Values are mean percentage ± SEM for the percentage equal to or above the UL. Usual intakes were estimated using the National Cancer Institute method (14, 15).
For DRIs, see reference 24.
For DRIs, see reference 17.
For DRIs, see reference 18.
For DRIs, see reference 16.
Folate EAR is presented as DFEs. 1 DFE = 1 μg food folate = 0.6 μg of folic acid from fortified food or supplement consumed with food = 5 μg of a supplement taken on an empty stomach.
For DRIs, see reference 19.
With enrichment/fortification, prevalence of intakes over the UL exceeded ≥10% primarily among the younger children 2–8 y of age for folate (41.7%), niacin (10.1%), and zinc (39.9%). Whereas, among those ≥2 y of age and 9–18 y of age, none of the intakes were as high as 10% above the UL.
When sources of enrichment/fortification and DSs were considered for individuals ≥2 y of age, 9% of the usual intakes were above the UL for folate, 2% above the UL for niacin, 7% above the UL for zinc, and 0.3% above the UL for calcium. With the addition of DSs, only slight increases were observed in the prevalence of intake exceeding the UL for vitamins B-6, C, and D, iron, and magnesium. Among children 9–18 y of age, percentages of nutrients with intakes above the UL were relatively low overall and the addition of reported DSs led to small percentage increases above the UL (enriched/fortified; enriched/fortified plus DSs): for folate (9%; 16%), niacin (1%; 4%), zinc (0.2%; 2%), and iron (0%; 0.8%). Whereas, children 2–8 y of age had much higher percentages of intakes exceeding the UL from enrichment/fortification and DS sources, respectively, for folate (42%; 52%), niacin (10%; 19%), and zinc (40%; 46%), with slight increases above the UL observed for vitamin C (0%; 0.4%), calcium (0.2%; 0.3%), magnesium (0%; 0.1%), and iron (0%; 0.9%).
Discussion
Our analysis including DS intake further supports the conclusions of the 2015 DGAC report (2) which identified vitamins A, D, E, C, folate, calcium, and magnesium as the most underconsumed nutrients by the US population ≥2 y of age. In our analysis of the at-risk nutrients identified by the DGAC, >25% of the US population ≥2 y of age did not meet the respective EAR for their demographic group for vitamins D and C, calcium, and magnesium, whereas only ∼6% of the US population were estimated to have intake amounts of folate lower than their respective EAR. A potential explanation for these differences is that we found some adults (>31 y old) reported consuming very high amounts of specific individual DSs.
Using the more recent NHANES 2009–2012 data, we found that a higher percentage of the US population ≥2 y of age reported nutrient intakes below the EAR for vitamins D and C, riboflavin, and zinc when naturally occurring, fortified/enriched foods and beverages, plus nutrients from reported DSs were included, than in the Fulgoni et al. (8) 2003–2006 analyses. Whereas, intake of vitamins A, B-6, and B-12, thiamin, niacin, folate, iron, calcium, and magnesium demonstrates a smaller proportion of the population ≥2 y of age not meeting the EAR than in the same earlier analyses (8). Results were mixed for the aforementioned nutrients when solely considering naturally occurring and enriched/fortified sources. We believe that the higher percentage of the population with reported nutrient intakes below the EAR in our analysis is a reflection of changes in the dietary patterns of the US population from 2006 to 2009 that have been reported for beverages and foods, cf. (25, 26). Similar to Fulgoni et al.’s results (8), we found that a greater percentage of 9–18-y-olds were at higher risk of not meeting the EARs for all nutrients studied than 2–8-y-olds.
As recognized globally (27), fortification/enrichment is a well-established and important approach to combating nutrient deficiency. Although the US population does not exhibit the level of widespread deficiency experienced by many low- and middle-income countries, similarly to other reports (5, 6, 8), our data further demonstrate that fortification/enrichment appreciably reduced the percentage of individuals who did not meet the EARs. Our data also indicated that the addition of nutrients through intake of DSs resulted in much less of an impact on meeting the EARs than did fortification/enrichment. Bailey et al. (28) also found that those who reported intake of DSs containing minerals had higher intake of minerals from food that potentially could contribute to risk of excessive intake. Yet, we found that the percentage of the population ≥2 y of age exceeding the UL was very low with the exception of folate, niacin, and zinc. We found the highest estimated percentage of total intake above the UL for these 3 nutrients among children 2–8 y of age, suggesting that the UL may be disproportionally too low in this age group. One would not expect children 2–8 y of age to be eating systematically differently than older children (9–18-y-olds). As the ULs for many nutrients were developed through extrapolation for children 2–18 y of age, the UL values may be unnecessarily conservative (29).
Food manufacturers in the United States may voluntarily fortify foods with vitamins and minerals with the understanding that there is some evidence of inadequacy of the particular nutrient in the target population and that the added nutrients are bioavailable, safe, and stable in the resulting product (4, 30, 31). US food fortification policies have slowly evolved since the 1940s when the FDA first identified specific nutrients and amounts as a standard of identity for “enriched” flour (30). At that time the FDA determined that it would not require mandatory fortification for any food product, but rather for every standard of identity for an enriched product there would be a parallel standard for a non-enriched product (30). The FDA's food fortification policy, published in 1980, that remains in effect today, includes a set of principles for addition of essential vitamins and minerals to foods (4, 30, 31). This policy includes standards of identity that specify amounts of nutrients which must be added (mandatory fortification) to a specific product for it to meet an “enriched” standard of identity, for example, folic acid, thiamin, riboflavin, niacin, and iron fortification of enriched cereal grains (4, 30, 31).
Although the interpretation of the UL for a number of nutrients is not clear for children (4), concern has been voiced by some (7) about the potential for excessive intakes among children due to fortification. Others also have demonstrated the specific positive contributions of fortification to meeting children's recommended nutrient intakes (6) and a recent international panel proposed a plan for global vitamin D food fortification to improve public health (32). Documentation of the higher than expected national estimated intake of folic acid due to mandatory fortification of cereal-grain products (33), coupled with uncertainty of application of the UL for some nutrients, has prompted recommendations for the continued evaluation of the risks and benefits of fortification (4, 7). However, in the present study, it was clear that fortification/enrichment were the main contributors to the reduction in percentage of individuals whose estimated intakes of specific nutrients were below the EAR, and not placing individuals at risk of exceeding the UL.
Our study is limited in that the nutrient intake estimation is based on dietary information from two 24-h NHANES recalls. Underreporting of portion size of food and drink items has been cited as an issue for NHANES 24-h recall data, and as this may affect nutrient amounts, the overall intake by US adults may be underestimated and in particular the regularity of DS intake (34). However, the NHANES and FNDDS are nationally representative databases that provide the most comprehensive dietary intake information for the US population and misreporting of food and beverage items in the NHANES has been reduced through use of the USDA's automated multiple-pass method approach for collecting dietary intake data (12, 13). Although newer NHANES data are available, the unique ILSI North America Fortification database was derived from NHANES and specifically created for the 2009–2010 and 2011–2012 NHANES cycles that are based on the USDA's FNDDS, thereby limiting our analysis to the same period. The database contains specific detailed fortification and enrichment data for the foods and beverages reported in the 2 NHANES cycles, allowing for identification of the sources of the nutrients within foods consumed by the US population.
In conclusion, these analyses further identify the need for improved intake of the key nutrients identified by the 2015 DGAC as the most underconsumed by the US population: vitamins A, D, E, and C, folate, calcium, and magnesium. Not unlike other countries globally, fortification/enrichment of the US diet clearly constitutes a major contribution to reducing the percentage of individuals whose estimated intake is less than the EAR for their demographic. Use of DSs further reduced the percentage of the US population whose intake was below the EAR, but not to the extent evidenced through fortification/enrichment. Although concern exists about fortification increasing intake above the UL, this analysis found an appreciable percentage of the US population reporting intakes that were deemed to be above the UL for only folate, niacin, and zinc, which were primarily due to higher intakes among children 2–8 y of age. However, the ULs for a number of nutrients for children are derived values, and as such may be artificially low (4, 29).
Overall, however, these data underscore the need to encourage better food choices to improve the intake by all individuals in the United States for vitamins A, D, E, and C, folate, calcium, and magnesium. The approach of the 2015 DGAC to focus on dietary patterns enables a wider possibility for education at all age levels. Compared with earlier approaches which focused on specific nutrient deficiencies, dietary pattern education not only fosters an improvement in the consumption of nutrients, such as these that are most underconsumed by the US population, but also promotes an overall more healthful approach to eating. Further modeling and quantitative studies of nutrient intakes of children, and refinement of the current ULs for all age groups, are needed before more fully considering global recommendations for nutrient fortification.
Supplementary Material
Acknowledgments
The authors’ responsibilities were as follows—JCN: analyzed the data and performed all the statistical analysis; KJH and BPM: provided scientific oversight; BPM, KJH, and AMM: wrote the manuscript; and all authors: designed the research and read, provided editorial changes to, and approved the final manuscript.
Notes
Supported by the North American branch of the International Life Sciences Institute (ILSI North America), grant agreement NA-MEDUNIVSCAROLINA-20170317 to the Medical University of South Carolina (to JCN). ILSI North America provided the fortification database necessary for the research.
Author disclosures: JCN, AMM, KJH, and BPM, no conflicts of interest.
ILSI North America is a public nonprofit foundation that provides a forum to advance understanding of scientific issues related to the nutritional quality and safety of the food supply by sponsoring research programs, educational seminars and workshops, and publications. ILSI North America receives support primarily from its industry membership.
Supplemental Tables 1 and 2 are available from the “Supplementary data” link in the online posting of the article and from the same link in the online table of contents at https://academic.oup.com/jn/.
Abbreviations used: AI, Adequate Intake; DGAC, Dietary Guidelines Advisory Committee; DS, dietary supplement; EAR, Estimated Average Requirement; FNDDS, Food and Nutrient Database for Dietary Studies; ILSI, International Life Sciences Institute; NCI, National Cancer Institute; UL, Tolerable Upper Intake Level.
References
- 1. United States Department of Health and Human Services and United States Department of Agriculture. Dietary Guidelines for Americans, 2015–2020. 8th ed Washington (DC): US Department of Health and Human Services and USDA; 2015. [Google Scholar]
- 2. Dietary Guidelines Advisory Committee. Scientific report of the 2015 Dietary Guidelines Advisory Committee. Washington (DC): USDA, Agricultural Research Service; 2015. [Google Scholar]
- 3. Backstrand JR. The history and future of food fortification in the United States: a public health perspective. Nutr Rev. 2002;60:15–26. [DOI] [PubMed] [Google Scholar]
- 4. Dwyer J, Woteki C, Bailey RL, Britten P, Carriquiry A, Gaine PC, Miller D, Moshfegh A, Murphy MM, Edge MS. Fortification: new findings and implications. Nutr Rev. 2014;72:127–41. [DOI] [PubMed] [Google Scholar]
- 5. Berner LA, Clydesdale FM, Douglass JS. Fortification contributed greatly to vitamin and mineral intakes in the United States, 1989–1991. J Nutr. 2001;131:2177–83. [DOI] [PubMed] [Google Scholar]
- 6. Berner LA, Keast DR, Bailey RL, Dwyer JT. Fortified foods are major contributors to nutrient intakes in diets of US children and adolescents. J Acad Nutr Diet. 2014;114:1009–22. e8. [DOI] [PubMed] [Google Scholar]
- 7. Sacco J, Dodd K, Kirkpatrick S, Tarasuk V. Voluntary food fortification in the United States: potential for excessive intakes. Eur J Clin Nutr. 2013;67:592–7. [DOI] [PubMed] [Google Scholar]
- 8. Fulgoni VL III, Keast DR, Bailey RL, Dwyer J. Foods, fortificants, and supplements: where do Americans get their nutrients?. J Nutr. 2011;141:1847–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. USDA Agricultural Research Service, Beltsville Human Nutrition Research Center. What We Eat in America, NHANES 2009–2010, 2011–2012. [Internet]. [cited 2018 Aug 5]. Available from: https://www.ars.usda.gov/ARSUserFiles/80400530/pdf/0910/tables_1-40_2009-2010.pdf. [Google Scholar]
- 10. ILSI North America. Fortification. [Internet]. Washington (DC): ILSI North America; 2018; [cited 2018 Dec 1]. Available from: http://ilsina.org/our-work/nutrition/fortification/. [Google Scholar]
- 11. NHANES. NHANES 2007–2010 is a stratified multistage probability sample of the civilian non-institutionalized population of the U.S. Dietary Interview (Individual Foods – First Day) (DR1IFF_E). 2007–2010. [Internet]. [cited 2007–2008]. Available from: https://www.cdc.gov/nchs/data/series/sr_01/sr02_160.pdf. [Google Scholar]
- 12. Ahuja JKA, Montville JB, Omolewa-Tomobi G, Heendeniya KY, Martin CL, Steinfeldt LC, Anand J, Adler ME, LaComb RP, Moshfegh AJ. USDA Food and Nutrient Database for Dietary Studies, 5.0. Appendix C. Dietary methods research: overview of What We Eat in America food categories: FSRG-defined food groups. [Internet]. Beltsville (MD): US Department of Agriculture, Agricultural Research Service, Beltsville Human Nutrition Research Center; 2012 October [cited 2012 Jan 1]. Available from: https://www.ars.usda.gov/ARSUserFiles/80400530/pdf/fndds/fndds5_doc.pdf. [Google Scholar]
- 13. Moshfegh AJ, Rhodes DG, Baer DJ, Murayi T, Clemens JC, Rumpler WV, Paul DR, Sebastian RS, Kuczynski KJ, Ingwersen LA et al.. The US Department of Agriculture Automated Multiple-Pass Method reduces bias in the collection of energy intakes. Am J Clin Nutr. 2008;88:324–32. [DOI] [PubMed] [Google Scholar]
- 14. Dodd KW, Guenther PM, Freedman LS, Subar AF, Kipnis V, Midthune D, Tooze JA, Krebs-Smith SM. Statistical methods for estimating usual intake of nutrients and foods: a review of the theory. J Am Diet Assoc. 2006;106:1640–50. [DOI] [PubMed] [Google Scholar]
- 15. Tooze JA, Midthune D, Dodd KW, Freedman LS, Krebs-Smith SM, Subar AF, Guenther PM, Carroll RJ, Kipnis V. A new statistical method for estimating the usual intake of episodically consumed foods with application to their distribution. J Am Diet Assoc. 2006;106:1575–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Food and Nutrition Board Institute of Medicine. Dietary Reference Intakes for thiamin, riboflavin, niacin, vitamin B6, folate, vitamin B12, pantothenic acid, biotin, and choline. Washington (DC): National Academies Press; 1998. [PubMed] [Google Scholar]
- 17. Institute of Medicine. Dietary Reference Intakes for calcium, phosphorus, magnesium, vitamin D, and fluoride. Washington (DC): National Academies Press; 1997. [PubMed] [Google Scholar]
- 18. Institute of Medicine. Dietary Reference Intakes for vitamin C, vitamin E, selenium, and carotenoids. Washington (DC): National Academies Press; 2000. [PubMed] [Google Scholar]
- 19. Institute of Medicine. Dietary Reference Intakes for vitamin A, vitamin K, arsenic, boron, chromium, copper, iodine, iron, manganese, molybdenum, nickel, silicon, vanadium, and zinc. Washington (DC): National Academies Press; 2001. [PubMed] [Google Scholar]
- 20. Johnson CL, Paulose-Ram R, Ogden CL, Carroll MD, Kruszon-Moran D, Dohrmann SM, Curtin LR. National Health and Nutrition Examination Survey: analytic guidelines, 1999–2010. Vit Health Stat 2. 2013;161:1–24. [PubMed] [Google Scholar]
- 21. CDC. National Health and Nutrition Examination Survey: analytic guidelines, 2011–2012. [Internet]. Atlanta (GA): National Center for Health Statistics, Division of Health and Nutrition Examination Surveys; 2013; [cited 2013 Sep 30]. Available from: https://www.cdc.gov/nchs/data/nhanes/analytic_guidelines_11_12.pdf. [PubMed] [Google Scholar]
- 22. CDC, National Center for Health Statistics. NHANES response rates. [Internet]. National Center for Health Statistics; 2011; [cited 2011 Dec 20]. Available from: https://www.cdc.gov/nchs/nhanes/responserates.aspx#response-rates. [Google Scholar]
- 23. Institute of Medicine. Dietary Reference Intakes for water, potassium, sodium, chloride, and sulfate. Washington (DC): National Academies Press; 2005. [Google Scholar]
- 24. Ross AC, Manson JE, Abrams SA, Aloia JF, Brannon PM, Clinton SK, Durazo-Arvizu RA, Gallagher JC, Gallo RL, Jones G et al.. The 2011 report on Dietary Reference Intakes for calcium and vitamin D from the Institute of Medicine: what clinicians need to know. J Clin Endocrinol Metab. 2011;96:53–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Dunford EK, Popkin BM. 37 year snacking trends for US children 1977–2014. Pediatr Obes. 2018;13:247–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Bleich SN, Vercammen KA, Koma JW, Li Z. Trends in beverage consumption among children and adults, 2003–2014. Obesity (Silver Spring). 2018;26:432–41. [DOI] [PubMed] [Google Scholar]
- 27. Osendarp SJM, Martinez H, Garrett GS, Neufeld LM, De-Regil LM, Vossenaar M, Darnton-Hill I. Large-scale food fortification and biofortification in low- and middle-income countries: a review of programs, trends, challenges, and evidence gaps. Food Nutr Bull. 2018;39:315–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Bailey RL, Fulgoni VL 3rd, Keast DR, Dwyer JT. Dietary supplement use is associated with higher intakes of minerals from food sources. Am J Clin Nutr. 2011;94:1376–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Zlotkin S. A critical assessment of the upper intake levels for infants and children. J Nutr. 2006;136:502S–6S. [DOI] [PubMed] [Google Scholar]
- 30. Institute of Medicine. Dietary Reference Intakes: guiding principles for nutrition labeling and fortification. Washington (DC): Institute of Medicine (US) Committee on Use of Dietary Reference Intakes in Nutrition Labeling; 2003. [PubMed] [Google Scholar]
- 31. Food and Drug Administration (FDA). Nutritional quality of foods; addition of nutrients. Final policy statement, Fed Regist. 1980;45:6314–24. [Google Scholar]
- 32. Pilz S, Marz W, Cashman KD, Kiely ME, Whiting SJ, Holick MF, Grant WB, Pludowski P, Hiligsmann M, Trummer C et al.. Rationale and plan for vitamin D food fortification: a review and guidance paper. Front Endocrinol (Lausanne). 2018;9:373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Choumenkovitch SF, Selhub J, Wilson PW, Rader JI, Rosenberg IH, Jacques PF. Folic acid intake from fortification in United States exceeds predictions. J Nutr. 2002;132:2792–8. [DOI] [PubMed] [Google Scholar]
- 34. Briefel RR, Sempos CT, McDowell MA, Chien S, Alaimo K. Dietary methods research in the third National Health and Nutrition Examination Survey: underreporting of energy intake. Am J Clin Nutr. 1997;65:1203S–9S. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


