Abstract
Background:
Multiligament knee injury (MLKI) is a complex orthopedic injury leading to the tear of at least two of the major knee ligaments. However, there is no consensus on the optimal management of this debilitating condition. Regarding this, the present study was performed to evaluate the outcomes of single-stage multiligament reconstruction surgery in patients with MLKI.
Methods:
This retrospective study was conducted on 41 consecutive MLKI patients who underwent surgical reconstruction. Objective evaluation of the outcome included active extension and flexion. Furthermore, the subjective evaluation of the outcome was accomplished using the Lysholm scoring scale and International Knee Documentation Committee (IKDC) form in Persian. Postoperative complications were also recorded for all patients.
Results:
The mean age of the participants was 31.95±7.82 years. In addition, the mean follow-up period and the mean time interval between the injury and surgery were recorded as 36.9±17.8 and 11.5±8.9 months, respectively. The mean Lysholm and IKDC scores were obtained as 86.9±11.5 and 70±18.7, respectively. The mean Lysholm and IKDC scores were not statistically different between the patients who underwent surgery less than 6 months after the injury and those subjected to reconstruction 6 months postinjury (P=0.07 and P=0.3, respectively). Seven patients showed postoperative restricted range of motion, which was resolved with physiotherapy. The only surgical complication was popliteal artery injury.
Conclusion:
As the findings indicated, the single-stage reconstruction of MLKI provided an acceptable outcome. However, several aspects of this reconstruction, such as the timing of the surgery, still remain to be resolved in future investigations.
Key Words: Complication, Multiligament knee injury, Outcome, Reconstruction surgery
Introduction
Multiligament knee injury (MLKI) is a complex orthopedic injury that usually occurs as a result of traumatic knee dislocation. However, knee dislocation is not the only factor accounting for MLKI. The MLKI is referred to the tear of at least two of the four major knee ligaments, including anterior cruciate ligament (ACL), posterior cruciate ligament (PCL), posteromedial corner including the medial collateral ligament (MCL), and posterolateral corner (PLC) including the lateral collateral ligament.
The MLKI can be further complicated by the concurrence of fracture and vascular or nerve damage (1, 2). Knee dislocation is associated with vascular injury in 30-35% of the cases in forms of arterial rupture or thrombosis, which may lead to the limb amputation in case of inadequate management (3). Therefore, the vascular injury should be inspected in all cases of knee dislocation, even in ultra-low velocity dislocations. The neural damage, especially peroneal nerve injury, is also a potential consequence of knee dislocation. Neurovascular injuries are commonly seen in PLC injuries [Figure 1] (4, 5).
Figure 1.
Anterior-posterior radiograph of a multiligament right knee injury under valgus stress test, complicated with peroneal nerve injury in association with posterolateral corner damage
The MLKI is associated with considerable morbidity. In this regard, the affected patients may experience pain and instability even several years after the initial injury (2, 3, 6). Given the serious consequences of a neglected injury, a high index of suspicion should be devoted to MLKI diagnosis. However, as the knee dislocation accounts for < 0.02% of all orthopedic injuries, the diagnosis of this condition could be difficult (7, 8).
Although a clinical examination is the cornerstone of determining the extent of the injury and formulating the treatment plan, it is not always reliable. Stress radiographs could be used to aid in the diagnosis of ligament injuries as reported by James et al. (9). Moreover, MLKI therapeutic options vary from conservative management to acute or chronic repair/reconstruction of the injured structures. Nonetheless, there is a paucity of high-level evidence on the optimal surgical management of this uncommon but debilitating condition.
Despite the lack of a clear consensus regarding the superiority of either single-staged or staged surgery of MLKI, some surgeons opt for the staged procedure in cases with concomitant injuries, such as fractures, vascular injuries, and life-threatening head, thoracic, or abdominal injuries (2, 10). Moreover, there are controversies regarding many aspects of MLKI management, such as the type of treatment (i.e., surgical versus non-surgical), type of surgery (i.e., repair versus reconstruction), and timing of treatment (i.e., early versus late) (2). Regarding this, further evidence is needed to resolve the existing controversies.
Implementation of cohort studies on the outcome of MLKI treatment is a valuable approach to reach a consensus regarding the best therapeutic option. With this background in mind, the present study was conducted to report the outcomes of single-stage multiligament reconstruction surgery among a cohort of patients with MLKI.
Materials and Methods
The present retrospective study was conducted on 41 consecutive MLKI patients who underwent surgical reconstruction at Shafa Orthopedic Hospital, Tehran, Iran, during 2011-2016. This study was approved by the Institutional Review Board of our university. In line with the principles of research ethics, informed consent was obtained from all patients.
The diagnosis of MLKI was mainly performed by magnetic resonance imaging (MRI) and stress radiography used for a complete evaluation of the damaged ligamentous knee restraints and establishment of the functional consequence of the MRI findings, respectively.
The inclusion criteria were: 1) affliction with MLKI, 2) reception of a single-staged surgical reconstruction, 3) age of > 18 years, 4) a minimum follow-up period of 10 months, and 5) availability of complete medical records. On the other hand, the exclusion criteria were: 1) presence of any malalignment, 2) concurrent fracture, and 3) past history of lower extremity ligament surgery, osteoarthritis-associated knee pain, systemic disease, and hip/spine problems. A total of 41 patients were identified as eligible for this study.
The patients’ clinical and demographic data were extracted from their electronic medical records. Preoperative evaluation of the patients was accomplished using plain radiography, stress radiography, MRI, duplex sonography, or computed tomography angiography if needed. The Schenck classification was used for the categorization of the knee dislocations based on the pattern of multiligamentous injury (11).
In this system the knee dislocations are classified into five types. Type I is referred to the injury of a single cruciate ligament (ACL or PCL). Type II is ascribed to the injury of both cruciate ligaments. Type III idicates the injury of the ACL, PCL, and collateral ligament (medial or lateral), as well as posteromedial corner. Type IV denotes the injury of the ACL, PCL, and collateral ligament (medial and lateral), as well as posteromedial corner. Type V represents the multiligamentous knee injury with periarticular fracture.
Objective evaluation of the outcome included active extension and flexion assessed in comparison with those of the contralateral knee. Subjective evaluation of the outcome was accomplished by means of the Tegner Lysholm knee scoring scale (Lysholm score) and the International Knee Documentation Committee (IKDC) form in Persian (12, 13). In both of the mentioned instruments, a higher score represents a higher level of function and a lower level of disability.
In this regard, Lysholm scores of 95-100, 84-94, 65-83, and < 63 are indicative of excellent, good, fair, and poor outcomes, respectively. In addition, the IKDC score was categorized into four subsets of IKDC A, B, C, and D representing normal, nearly normal, abnormal, and severely abnormal outcomes, respectively. All postoperative complications, such as neurovascular events, compartment syndrome, and infection, were also recorded for each of the patients.
Surgical technique
The surgery was performed after a preoperative period of one month to allow soft-tissue repair, reduce the possibility of fluid extravasation during arthroscopy and compartment syndrome, and reach an acceptable range of motion to prevent postoperative stiffness. To perform the surgery, the patients were placed in the supine position on the operating table under general anesthesia. Subsequently, the ligamentous injuries were re-assessed. The uninvolved limb was wholly placed on the table in full extension. Tourniquet was used for all patients but two, in whom the popliteal artery was repaired earlier.
The reconstruction of ACL and PCL was accomplished using the anatomic arthroscopic transtibial technique. In this regard, the correct positioning of the femoral and tibial tunnels was performed using ACUFEX Director PCL Tibia Aimer (Smith & Nephew ACUFEX instruments, USA). Then, the position was checked with radiography and cruciate grafts were fixed in the femoral side with a screw or Endobutton (ConMed, Linvatec or Smith & Nephew, USA).
Tibialis posterior allograft was used for the reconstruction of the majority of the PCL injuries. Furthermore, the reconstruction of most of the ACL and PLC injuries was performed using tibialis anterior allograft. Semitendinosus autograft was used for the reconstruction of MCL. Afterwards, the arthroscopic re-evaluation of the knee and arthroscopic gap test were performed on the tension position (14).
The gap sizes of > 8, > 10, and > 12 mm in the most medial part of the knee, medial compartment, and lateral part of the knee were considered normal, respectively (15). If the gap size was more than normal, the patient was subjected to medial and lateral reconstruction. Larson method was used for the reconstruction of PLC. Peroneal nerve was explored and protected in this procedure.
The ligament fixation was started with PCL, followed by PLC, ACL, and MCL (16). While all PLC injuries were managed with reconstruction surgery, the majority of the MCL injuries were managed nonsurgically. Surgical treatment of MCL was performed on seven cases using the open reconstruction technique. At the end of the surgery, the knee motion range was assessed to prevent the potential knee motion capture during the reconstruction process.
Postoperative rehabilitation
After the surgery, the limb was supported with a hinged knee brace in full extension. Isometric quadriceps exercises were started a few hours after the surgery, and the patients were advised to perform the passive full extension of the knee and straight leg raise. Strengthening of the hamstring muscles was scheduled 12 weeks postsurgery in the patients with PCL reconstruction. The day after the surgery, the crutch walk was begun in the form of toe-touch weight-bearing and progressive weight bearing was initiated in 4-6 weeks.
At the end of week 4, 0-90° flexion was planned for the patients in the presence of the knee brace. Three months after the surgery, a soft hinged knee brace was substituted and full-weight bearing was initiated. After 6 months, the brace was removed completely. Two patients received long leg casts for 4 weeks after the surgery due to their nonadherence to the postoperative protocol.
Statistical analysis
All statistical analyses were performed in SPSS for Windows (version 16). The data were descriptively presented as mean, standard deviation, number, and percentage. Parametric tests, including independent t-test and one-way ANOVA, or their non-parametric counterparts (i.e., Mann-Whitney U and Kruskal-Wallis tests, respectively) were used to evaluate the mean difference between two or more samples. P-value less than 0.05 was considered statistically significant.
Results
Demographic data
The study population consisted of a total of 41 patients, including 39 (95.1%) males and 2 (4.9%) females, with the mean age of 31.9±7.8 years (age range: 18-50 years). The mean time interval between the injury and surgery was 11.5±8.9 months (range: 1-36 months). Frank dislocation was present in three (7.3%) patients, which was reduced by primary care. In terms of the mechanism of injury, 38 (92.7%) and 3 (7.3%) patients had high-energy (motor-vehicle accidents) and low-energy (sports accidents) traumas, respectively. The mean follow-up period was 36.9±17.8 months in the patients (range: 10-72 months).
According to the Schenck classification, knee dislocation types I, II, III, and IV classes were identified in 15 (36.6%), 5 (12.2%), 16 (39%), and 5 (12.2%) patients, respectively. Table 1 presents the clinical and demographic characteristics of the patients. The preoperative concomitant injuries included meniscus tear (n=8, 20.5%), cartilage lesion (n=5, 12.8%), vascular lesion (n=2, 5.1%), peroneal nerve injury, partial sensory, and motor loss (n=3, 7.3%), as well as complete sensory and motor loss (n=1, 2.5%). Regarding the cartilage lesion, one case was grade I, and the remaining four cases were grade II lesions. None of the patients with cartilage lesions underwent chondroplasty. Meniscus tears were managed with partial meniscectomy and meniscus repair in five and three patients, respectively.
Table 1.
Clinical and demographic characteristics of the MLKI patients
| Variable | Number (%) |
|---|---|
| Age | |
| • <30 years • >30 years |
17 (41.5) 24 (58.5) |
| Gender | |
| • Male • Female |
39 (95.1) 2 (4.9) |
| Dominancy of the knee | |
| • Dominant • Non-dominant |
22 (53.7) 19 (46.3) |
| Time to surgery | |
| • <6 months • >6 months |
9 (22.5) 31 (77.5) |
| Etiology | |
| • Low-energy trauma • High-energy trauma |
3 (7.3) 38 (92.7) |
| Schenk type of classification | |
| • KD I • KD II • KD IIIM • KD IIIL • KD IV |
15 (36.6) 5 (12.2) 9 (22) 7 (17) 5 (12.2) |
| Treatment approach* | |
| • Medial-sided • Lateral- sided • Posterolateral-sided • Anterior- sided • Posterior- sided |
21 (51.2) 17 (41.4) 14 (34.1) 34 (82.9) 31(75.6) |
| Reconstruction surgery** | |
| • Medial • Lateral • Posterolateral • Anterior • Posterior |
7 out of 21 (33.3) 13 out of 17 (76.5) 13 out of 14 (92.9) 34 out of 34 (100) 31 out of 31 (100) |
The total number of each side of the knee that was treated, either surgically or non-surgically.
The number of reconstruction surgery in each side of the knee.
Subjective outcomes
The mean Lysholm score was obtained as 86.9±11.5 (range: 48-100). In this regard, 9 (22%), 21 (51.2%), 8 (19.5%), and 3 (7.3%) patients had excellent, good, fair, and poor Lysholm scores, respectively. The mean Lysholm score was not significantly different in various types of dislocations (P=0.58). Moreover, there was no significant difference between the patients with the age of < 30 years and those with the age of > 30 years in this regard (P=0.87).
The mean Lysholm score was not statistically different between patients undergoing surgery in the first 6 months after the initial injury and those subjected to surgery after 6 months (P=0.27). Moreover, no statistically significant difference was observed between the patients with high-energy traumas and those with low-energy traumas regarding this score (P=0.07). In addition, no association was detected between the Lysholm score and other clinicodemographic characteristics, including the knee dominancy and gender [Table 2].
Table 2.
IKDC and Lysholm score with respect to the clinical and demographic characteristics of the MLKI patients
| Variable | IKDC | P value | Lysholm | P value |
|---|---|---|---|---|
| Age | ||||
| • <30 years • >30 years |
73.1±20 68±17.9 |
0.38 | 86.9±12 87±11.2 |
0.87 |
| Gender | ||||
| • Male • Female |
70±19.2 72.4±11.6 |
0.44 | 87.1±11.8 84±11.4 |
0.16 |
| Dominancy of the knee | ||||
| • Dominant • Non-dominant |
73.4±18.8 66.1±18.4 |
0.21 | 89.2±9.2 84.3±13.4 |
0.16 |
| Time to surgery | ||||
| • <6 months • >6 months |
80.5±12 67.9±19.1 |
0.07 | 91.1±6.7 86.7±11.3 |
0.27 |
| Etiology | ||||
| • Low-energy trauma • High-energy trauma |
60.5±16.9 70.8±18.9 |
0.3 | 77±17.2 87.8±10.7 |
0.07 |
| Schenk type of classification | ||||
| • KD I • KD II • KD III • KD IV |
68.2±23.3 69.4±20.9 69.2±16.1 78.8±10.4 |
0.74 | 85.2±14.6 92±8.1 85.7±10.3 90.8±6.5 |
0.58 |
IKDC: International Knee Documentation Committee; MLKI: Multiligament knee injury.
P value of <0.05 is considered significant.
The mean IKDC was 70±18.7 (range: 25.3-98.2). In this regard, 2 (4.9%), 13 (31.7%), 14 (34.1%), and 4 (9.8%) patients had grades A, B, C, and D of IKDC, respectively. The mean IKDC was not statistically different among the patients subjected to surgery in the first 6 months after the initial injury and those subjected to surgery after 6 months from the initial injury (P=0.07). Furthermore, there was no statistically significant difference between the high-energy and low-energy trauma groups in terms of this score (P=0.3). The results revealed no significant association between IKDC and other clinicodemographic characteristics of the patients, including the knee dominancy, gender, and age [Table 2].
Clinical outcome
Seven patients had a restricted range of motion postoperatively. In this respect, 1 (2.4%) patient had an extension loss of up to 3-5°, while 4 (9.8%) and 2 (4.2%) patients had the flexion loss of up to 6-15° and 16-25°, respectively. At the last follow-up, all of the patients obtained a full or nearly full range of motion with regularly scheduled physiotherapy, and none of them needed manipulation or arthroscopic lysis for arthrofibrosis.
Medial-sided knee reconstruction was performed in seven patients with MCL injuries, while the other 14 MCL injuries were managed nonsurgically. The adoption of a surgical or nonsurgical approach for the management of MCL injuries was determined by the surgeon considering several factors. These factors included the number of the involved ligament, type of dislocation, location of the tear (i.e., distal or proximal), and extent of medial opening at valgus stress test after the reconstruction of other ligaments.
Moderate (i.e., a side-to-side difference of >9.8 mm in stress valgus test) and mild (i.e., a side-to-side difference of >3.8 mm in stress valgus test) medial joint space openings were observed in 1 (14.3%) and 2 (28.5%) patients undergoing surgery, respectively. In addition, 7 (50%) patients managed nonsurgically had a mild medial joint space opening. However, this difference was not statistically significant between these two groups (P=0.33).
Operative and postoperative complications
The only surgical complication was a popliteal artery injury, which occurred during PCL transtibial tunnel drilling. This patient underwent a popliteal artery bypass at another center. After a follow-up of 48 months, the patient returned to his work with no further complications. Nonadherence to the postoperative rehabilitation protocol led to a revision ligamentous reconstruction surgery in one patient, who referred with the trauma of the same knee.
This patient was first managed with anatomic ACL+PLC reconstruction, which failed 3 months later. After a year, the patient underwent ACL+PCL+PLC reconstruction with the Larson method. In addition, long leg cast was used to prevent the incidence of further complications [Figure 2]. No cases of deep vein thrombosis, compartment syndrome, wound problem, iatrogenic neurologic disorder, infection, and periarticular fracture after reconstruction were identified in our patients.
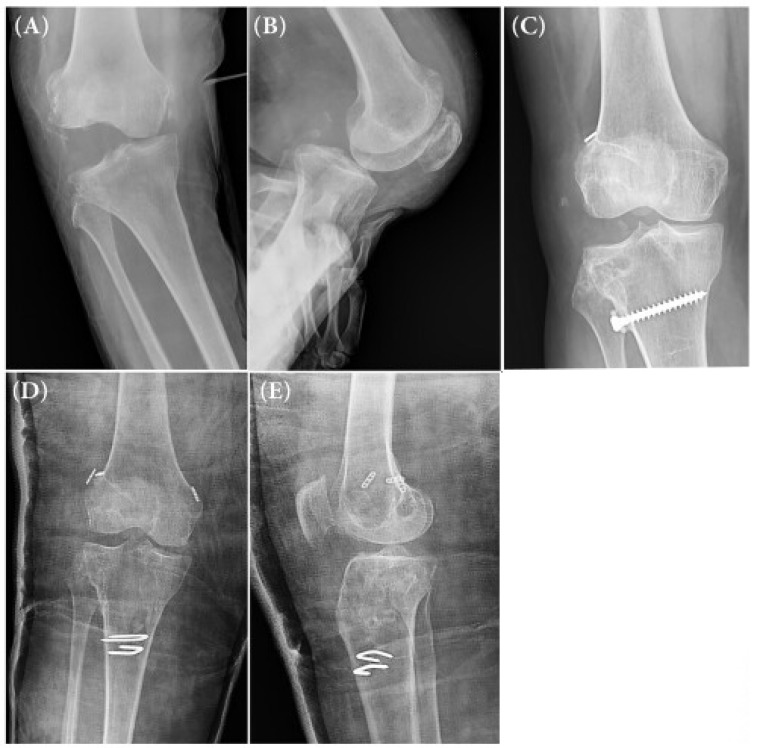
Figure 2.
(A) Anterior-posterior radiograph of the injured right knee under valgus stress test, (B) lateral radiograph of the same knee with manual posterior drawer test, (C) anterior-posterior plain radiograph of the same knee after reconstruction failure, (D) anterior-posterior plain radiograph of the same knee after the second surgery (anterior cruciate ligament+posterior cruciate ligament+posterolateral corner, and (E) lateral plain radiograph of the same knee after the second surgery
Discussion
The current study involved the investigation of the outcome of single-staged surgical reconstruction in the patients with MLKI. Based on our findings, the single-staged reconstruction of MLKI could result in an acceptable outcome, at least for a short period of time. The results indicated no significant difference between the patients undergoing the surgery in less than 6 months from the injury and those who were treated after 6 months in terms of the surgical outcome. Moreover, there was no significant association between the outcomes of the patients and other clinicodemographic characteristics, such as the type of dislocations, age, and gender.
Peskun et al. evaluated the outcomes of the surgical and nonsurgical treatment of MLKI in an evidence-based review. They compared the therapeutic outcomes of 855 patients from 31 studies who were managed with surgery with those of 61 patients from 4 studies undergoing nonsurgical management. Their results revealed the superiority of operative management over the nonoperative one in terms of several clinical and functional domains (17).
Similar results were reported in a study performed by Levy et al. who systematically reviewed the factors affecting decision-making process in the MLKI management (2). Our results were indicative of an acceptable functional outcome following the surgical management of MLKI, which is in accordance with the results of earlier investigations. In a prospective trial, Stannard et al. compared the results of repair versus reconstruction of the PLC in 57 knees, 44 (77%) cases of which had MLKI. In a minimum follow-up of 24 months, the failure rates of direct repair and reconstruction were reported as 37% and 9%. However, the mean Lysholm and IKDC scores were not statistically different between the two groups (18).
Mariani et al. demonstrated higher rates of flexion loss and posterior sag sign and a lower rate of resumption of the preinjury activity in the direct repair group in comparison with those in the reconstruction group. However, in the mentioned study, the two groups had similar Lysholm and IKDC scores (19). Based on these reports, in the present study, the researchers selected reconstruction over direct repair for the management of MLKI, which provided an acceptable outcome.
The timing of surgery is one of the most controversial topics in the MLKI management (20). Early surgery is generally performed during the first 3 weeks of the injury. In a systematic review addressing the outcomes of the early surgery of MLKI in 80 patients and late surgery in 50 patients, it was revealed that an early surgery is accompanied with higher mean Lysholm scores (90 vs. 82), as well as a higher percentage of excellent/good IKDC score (47% vs. 31%). However, there are multiple studies reporting favorable outcomes for the late surgery and demonstrating that it is accompanied with a significant improvement and the resumption of activity (21-23).
Karataglis et al. evaluated the outcomes of 35 patients who received surgical treatment within the mean time interval of 32 months from the initial injury and demonstrated that 60% of the patients had excellent or good outcomes during a mean follow-up of 40 months (21). Fanelli and Edson studied the outcomes of 41 patients with PCL/PLC injuries that received treatment within 4-240 months after the initial injury and obtained excellent functional results during a minimum follow-up of 24 months (22). In our study, the outcomes of 9 patients who were treated in less than 6 months from the injury were not significantly different from those in the patients managed after 6 months from the injury.
None of our patients underwent the surgery during the acute phase of the injury (i.e., the first 3 weeks). It is not suggested to adopt acute surgery for the management of combined ligament injury due to the high incidence of arthrofibrosis (20, 24, 25). In a systematic review, Mook et al. suggested that acute surgery was highly associated with deficits in the range of motion (26). However, Levy et al. did not find the same results as those of Mook et al (27). Therefore, the timing of the surgery needs to be more investigated in the future investigations.
Generally, low-energy injuries are accompanied with relatively fewer soft-tissue damages and better outcomes (28). However, the results of the present study revealed no statistically significant difference between the patients with high-energy and low-energy traumas regarding the outcome of MLKI. Nonetheless, it should be noted that only three low-energy traumas were included in our study; therefore, this result contains a low statistical power.
There is little consensus regarding the best strategy for the management of MCL injury. Some studies have suggested the adoption of early conservative management of the MCL with bracing, while others have proposed surgical approach (29). In the present stuy, the majority of the cases were subjected to the nonsurgical management of MCL injuries. Nonetheless, no significant difference was observed between the patients managed nonsurgically and those subjected to a surgical procedure in terms of the therapeutic outcome.
One of the weaknesses of the present study is that the short- to mid-term follow-up periods did not allow evaluating the long-term complications of MLKI, such as the incidence of degenerative joint disease. Moreover, the surgeries were performed by four different surgeons, which could have influenced the outcomes. In addition, some of the statistical analyses were not powered enough due to the small number of the patients in some groups, as mentioned earlier.
In accordance with the results of the previous investigations, our study revealed that the single-stage reconstruction surgery of MLKI was accompanied with acceptable outcomes in the affected patients. However, the inconsistencies among the results of different investigations regarding several aspects of MLKI treatment, such as the appropriate timing of the surgery, needs to be further investigated in future investigations with a larger sample size.
References
- 1.Riboh JC. Singapore: World Scientific Publishing Company. 2016. Multiligament knee injuries; pp. 359–67. [Google Scholar]
- 2.Levy BA, Dajani KA, Whelan DB, Stannard JP, Fanelli GC, Stuart MJ, et al. Decision making in the multiligament-injured knee: an evidence-based systematic review. Arthroscopy. 2009;25(4):430–8. doi: 10.1016/j.arthro.2009.01.008. [DOI] [PubMed] [Google Scholar]
- 3.Manske RC, Hosseinzadeh P, Giangarra CE. Multiple ligament knee injury: complications. N Am J Sports Phys Ther. 2008;3(4):226–33. [PMC free article] [PubMed] [Google Scholar]
- 4.Moatshe G, Dornan GJ, Løken S, Ludvigsen TC, LaPrade RF, Engebretsen L. Demographics and injuries associated with knee dislocation: a prospective review of 303 patients. Orthop J Sports Med. 2017;5(5):2325967117706521. doi: 10.1177/2325967117706521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pache S, Aman ZS, Kennedy M, Nakama GY, Moatshe G, Ziegler C, et al. Posterior cruciate ligament: current concepts review. Arch Bone Jt Surg. 2018;6(1):8–18. [PMC free article] [PubMed] [Google Scholar]
- 6.Jones RE, Smith EC, Bone GE. Vascular and orthopedic complications of knee dislocation. Surg Gynecol Obstet. 1979;149(4):554–8. [PubMed] [Google Scholar]
- 7.Rihn JA, Groff YJ, Cha PS, Harner CD. The acutely dislocated knee: evaluation and management. J Am Acad Orthop Surg. 2004;12(5):334–46. doi: 10.5435/00124635-200409000-00008. [DOI] [PubMed] [Google Scholar]
- 8.Hoover NW. Injuries of the popliteal artery associated with fractures and dislocations. Surg Clin North Am. 1961;41(4):1099–112. doi: 10.1016/s0039-6109(16)36451-9. [DOI] [PubMed] [Google Scholar]
- 9.James EW, Williams BT, LaPrade RF. Stress radiography for the diagnosis of knee ligament injuries: a systematic review. Clin Orthop Relat Res. 2014;472(9):2644–57. doi: 10.1007/s11999-014-3470-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Barfield WR, Holmes RE, Slone H, Walton ZJ, Hartsock LA. Acute versus staged surgical intervention in multiligamentous knee injuries: a review of the literature since 2009. Curr Orthop Pract. 2015;26(5):530–5. [Google Scholar]
- 11.Schenck RC Jr. The dislocated knee. Instr Course Lect. 1994;43(1):127–36. [PubMed] [Google Scholar]
- 12.Negahban H, Mostafaee N, Sohani SM, Mazaheri M, Goharpey S, Salavati M, et al. Reliability and validity of the Tegner and Marx activity rating scales in Iranian patients with anterior cruciate ligament injury. Disabil Rehabil. 2011;33(22-23):2305–10. doi: 10.3109/09638288.2011.570409. [DOI] [PubMed] [Google Scholar]
- 13.Ebrahimzadeh MH, Makhmalbaf H, Golhasani-Keshtan F, Rabani S, Birjandinejad A. The international knee documentation committee (IKDC) subjective short form: a validity and reliability study. Knee Surg Sports Traumatol Arthrosc. 2015;23(11):3163–7. doi: 10.1007/s00167-014-3107-1. [DOI] [PubMed] [Google Scholar]
- 14.Hadi H, Bagherifar A, Tayebi F, Ansari M, Shahsavaripour A, Qomashi I, et al. Anterior cruciate ligament reconstruction with hamstring tendons has no deleterious effect on hip extension strength. Arch Bone Jt Surg. 2019;7(3):278–83. [PMC free article] [PubMed] [Google Scholar]
- 15.Noyes FR, Barber-Westin SD. Posterolateral ligament injuries: diagnosis, operative techniques, and clinical outcomes. Noyes’ knee disorders: surgery, rehabilitation, clinical outcomes. New York: Elsevier; 2017. pp. 527–77. [Google Scholar]
- 16.Moatshe G, Chahla J, LaPrade RF, Engebretsen L. Diagnosis and treatment of multiligament knee injury: state of the art. J ISAKOS. 2017;2(3):152–61. [Google Scholar]
- 17.Peskun CJ, Whelan DB. Outcomes of operative and nonoperative treatment of multiligament knee injuries: an evidence-based review. Sports Med Arthrosc Rev. 2011;19(2):167–73. doi: 10.1097/JSA.0b013e3182107d5f. [DOI] [PubMed] [Google Scholar]
- 18.Stannard JP, Brown SL, Farris RC, McGwin G, Volgas DA. The posterolateral corner of the knee: repair versus reconstruction. Am J Sports Med. 2005;33(6):881–8. doi: 10.1177/0363546504271208. [DOI] [PubMed] [Google Scholar]
- 19.Mariani PP, Santoriello P, Iannone S, Condello V, Adriani E. Comparison of surgical treatments for knee dislocation. Am J Knee Surg. 1999;12(4):214–21. [PubMed] [Google Scholar]
- 20.Jari S, Shelbourne KD. Nonoperative or delayed surgical treatment of combined cruciate ligaments and medial side knee injuries. Sports Med Arthrosc Rev. 2001;9(3):185–92. [Google Scholar]
- 21.Karataglis D, Bisbinas I, Green MA, Learmonth DJ. Functional outcome following reconstruction in chronic multiple ligament deficient knees. Knee Surg Sports Traumatol Arthrosc. 2006;14(9):843–7. doi: 10.1007/s00167-006-0073-2. [DOI] [PubMed] [Google Scholar]
- 22.Fanelli GC, Edson CJ. Combined posterior cruciate ligament-posterolateral reconstructions with Achilles tendon allograft and biceps femoris tendon tenodesis: 2-to 10-year follow-up. Arthroscopy. 2004;20(4):339–45. doi: 10.1016/j.arthro.2004.01.034. [DOI] [PubMed] [Google Scholar]
- 23.Fanelli GC, Edson CJ. Arthroscopically assisted combined anterior and posterior cruciate ligament reconstruction in the multiple ligament injured knee: 2-to 10-year follow-up. Arthroscopy. 2002;18(7):703–14. doi: 10.1053/jars.2002.35142. [DOI] [PubMed] [Google Scholar]
- 24.Shelbourne KD, Wilckens JH, Mollabashy A, DeCarlo M. Arthrofibrosis in acute anterior cruciate ligament reconstruction: the effect of timing of reconstruction and rehabilitation. Am J Sports Med. 1991;19(4):332–6. doi: 10.1177/036354659101900402. [DOI] [PubMed] [Google Scholar]
- 25.Shelbourne K, Baele J. Treatment of combined anterior cruciate ligament and medial collateral ligament injuries. Am J Knee Surg. 1988;1(1):56–8. [Google Scholar]
- 26.Mook WR, Miller MD, Diduch DR, Hertel J, Boachie-Adjei Y, Hart JM. Multiple-ligament knee injuries: a systematic review of the timing of operative intervention and postoperative rehabilitation. J Bone Joint Surg Am. 2009;91(12):2946–57. doi: 10.2106/JBJS.H.01328. [DOI] [PubMed] [Google Scholar]
- 27.Levy BA, Dajani KA, Whelan DB, Stannard JP, Fanelli GC, Stuart MJ, et al. Decision making in the multiligament-injured knee: an evidence-based systematic review. Arthroscopy. 2009;25(4):430–8. doi: 10.1016/j.arthro.2009.01.008. [DOI] [PubMed] [Google Scholar]
- 28.Skendzel JG, Sekiya JK, Wojtys EM. Diagnosis and management of the multiligament-injured knee. J Orthop Sports Phys Ther. 2012;42(3):234–42. doi: 10.2519/jospt.2012.3678. [DOI] [PubMed] [Google Scholar]
- 29.Fanelli GC, Orcutt DR, Edson CJ. The multiple-ligament injured knee: evaluation, treatment, and results. Arthroscopy. 2005;21(4):471–86. doi: 10.1016/j.arthro.2005.01.001. [DOI] [PubMed] [Google Scholar]