Summary
Background
Taking into account radiation doses, safety, and protection, we highlighted the features in which cone-beam computed tomography (CBCT) can offer an advantage compared to the conventional two-dimensional imaging in paediatric dentistry before orthodontic treatment.
Objective
The aim of this article was to conduct a systematic review to assess the diagnostic efficacy of CBCT in the paediatric population at a pre-orthodontic phase.
Search methods
MEDLINE via PubMed was searched to identify all peer-reviewed articles potentially relevant to the review until 1 July 2018. Relevant publications were selected by two reviewers independently.
Selection criteria
The literature selection for this systematic review was carried out according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement and was based on predetermined inclusion criteria.
Data collection and analysis
Data were collected on overall study characteristics and examination characteristics of the selected studies. Methodological quality of the selected studies was evaluated. Original studies were assessed using the Quality Assessment of Diagnostic Accuracy Studies (QUADAS) tool. Thereafter, levels of evidence were obtained according to Grading of Recommendations Assessment, Development and Evaluation criteria.
Results
As a result of the QUADAS assessment, a total of 37 articles were included in the protocol. Following a proper protocol, CBCT was regarded as a reliable tool for assessment and management of impacted canine and root fracture. It provided a better evaluation of normal and pathological condylar shape and volume. CBCT was a superior choice for pre-surgical diagnostic applications in cleft lip and/or palate over a medical computed tomography based on its lower radiation exposure, shorter investigation time, and low purchase costs.
Conclusions
CBCT is justified only in those cases where conventional radiography fails to provide a correct diagnosis of pathology. Therefore, it cannot be regarded as a standard method of diagnosis. CBCT imaging may also be justified when it positively affects treatment options or provides treatment optimization.
Registration
None.
Conflict of interest
None to declare.
Introduction
Rationale
Evidence-based and justified diagnostic imaging is a key factor that contributes to proper orthodontic diagnosis and treatment planning, together with clinical evaluation of the patient and digital/plaster cast analysis (1). Since the introduction of cone-beam computed tomography (CBCT) in dentistry (2), there has been a rapid evolution in CBCT technology, driven largely by the demands of each specialty for providing with accurate and reproducible three-dimensional (3D) images, and minimizing the radiation dose.
CBCT was designed to overcome some of the limitations of conventional computed tomography (CT), offering high-resolution 3D images at a relatively lower dose and cost. However, CBCT still delivers a higher dose than a two-dimensional (2D) scan. Together with the exponential advancement in CBCT technology, there is still a growing gap with the available scientific evidence for justified use of CBCT. This holds particularly true in children, who are more vulnerable to radiation dose and often present with challenging diagnostics (3,4). The three fundamental principles of radiation protection, that is justification, optimization, and dose limitation, should always be followed when considering radiation exposure for orthodontic reasons (5–7). On the basis of the high susceptibility to the ionizing radiation in children (8), exposure should be kept as low as reasonably achievable, while maintaining sufficient diagnostic information (9).
According to the SEDENTEXCT guidelines, it is impossible to differentiate between safe and harmful exposure because of the uncertainties related to the stochastic effects (7). Even the smallest amount of radiation can be associated with a potential risk. It is likely that as the technology advances and more evidence on the efficacy of CBCT is established, its role in orthodontic applications will increase or be modified. Thereby, enabling clinicians to diagnose and plan treatment in many more clinical scenarios than currently possible.
Objectives
The aim of this article was to conduct a systematic review for the justification of CBCT application in paediatric population and to provide evidence for diagnostic use of CBCT in a pre-orthodontic paediatric population. Therefore, Population Intervention Comparator Outcomes (PICO) approach was formulated as follows:
Population: paediatric patients; Intervention: CBCT; Control: conventional 2D radiography; Outcome: treatment changes due to 3D imaging.
Materials and methods
Protocol and registration
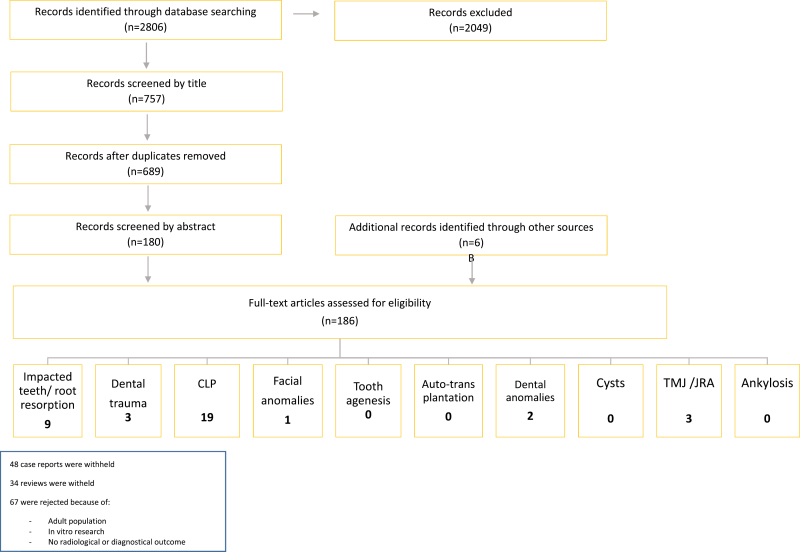
This systematic review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement (Figure 1) and was not registered (10).
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) flowchart. CLP, cleft lip palate; TMJ, temporomandibular joint.
Eligibility criteria
The selected publications had to describe the model of efficacy: diagnostic accuracy efficacy, diagnostic thinking efficacy, therapeutic efficacy, or any combination (11).
Diagnostic accuracy efficacy included the following:
Observer performance
Sensitivity, specificity, and predictive values
Diagnostic thinking efficacy included the following:
Percentage of cases in which CBCT was considered beneficial for the orthodontic treatment planning
Subjective estimation of difference in clinicians’ certainty on diagnostic outcome
Therapeutic efficacy included the following:
Percentage of times CBCT was found useful in treatment planning
Percentage of times treatment plan and therapeutic choices altered after obtaining CBCT information
Search methods, search strategy, and study selection
The period of search was limited till 1 July 2018. A detailed search was conducted in MEDLINE via the electronic database PubMed. Electronic search of the publications was carried out by using controlled index terms and relevant specific free text words without any language restrictions. Furthermore, manual screening of all references to earlier systematic reviews and selected full-text articles was accomplished for finding potentially useful articles. Specific strategies were applied for each subject. The search strategy encompassed appropriate variations in the keywords, following the syntax rules of the database (Supplementary Appendix I).
The PICO approach was applied to obtain data from the included articles independently by two review authors. Two reviewers analysed the list of titles and abstracts independently for inclusion. All the articles that fitted the review question were reviewed. Any disagreement between the reviewers was solved by means of consensus and when deemed appropriate, by consultation of a third reviewer. Risk of bias and quality assessment was also completed independently and in duplicate by the same two investigators. The reviewers were not blinded to the authors or the results of the research.
The following Medical Subject Headings (MeSH) were applied during the literature search: cone-beam computed tomography; root resorption; tooth, impacted; tooth, unerupted; transplantation, autologous; cleft lip; hypodontia; cyst, jaw; Arthritis, Juvenile; Congenital Abnormalities; Tooth, Supernumerary; Fused Teeth; wounds and injuries; Tooth Injuries; Tooth Ankylosis; not adult; not animal (Supplementary Appendix I).
Narrative reviews, case reports, letters to editor, in vitro studies, animal studies, studies without 2D comparison, and studies with sample size below 10 were excluded. Thereafter, complete text of the chosen publications were selected and assessed. If one of the authors found an abstract to be relevant, then the full text of publication was read. Next step involved manual search of the reference lists included in the selected publications and full text of relevant abstracts were read. Titles of the articles that contained a MeSH keyword were included.
Assessment of risk of bias
Assessment of the quality of publications selected for this review was carried out by applying a protocol. This protocol was based on the Quality Assessment of Diagnostic Accuracy Studies (QUADAS) tool (12,13). Information isolated from selected studies included type of studies, number of samples, reference method, specific method used in the study, number of observers, statistical method, and results according to authors.
Data analysis
All results were analysed descriptively.
Results
Study selection
The result of this systematic review was based on the PRISMA statement (10). We found a total of 2806 publications from the PubMed database. After first assessment and removal of duplicates, a total of 186 publications were selected. Sixty-seven articles were rejected based on exclusion criteria. Following QUADAS assessment, a total of 37 articles were included in the protocol (Figure 1). The period of search was limited from 1997 until 1 July 2018, since CBCT in dentistry was introduced in 1998 (2).
Currently, there is ample literature on the use of CBCT imaging for diagnosis and treatment planning of dentomaxillofacial deformities in paediatric patients, yet most of them are described in the form of case reports or case series due to the rarity of appearance. We did not want to withhold these reports and summarized them in Supplementary Table 1.
Study characteristics
Estimates of test accuracy were established on the assumption that the reference standard was 100 per cent sensitive. Specific disparities between the reference standard and index test resulted from incorrect classification by the index test. All studies were screened by diagnostic accuracy efficacy.
Impacted teeth and root resorption
Because root resorptions are usually related to impacted teeth, both subjects were analysed together (Table 1) (14,15). CBCT showed better detection rates (63 per cent) of root resorption associated with impacted canines when compared to plain film radiographs (16). It was also found to be superior to intra-oral radiography for detection and assessment of internal and external cervical root resorption, thereby leading to improved management (17). Management of root resorption depends on the extent of the resorption and can vary between no treatment (active monitoring), nonsurgical root canal therapy, external surgical repair, and extraction. When it came to treatment changes, Goodell et al. (18) found different results compared with Patel et al. (17). In the study conducted by Goodell et al., 56.7 per cent of treatment was proposed when analysing periapical radiographs, compared to 59.8 per cent treatment when CBCT analysis was done (18). In the study conducted by Patel et al. (17), 50.7 per cent repair was advised with periapical radiographs whereas only 21.2 per cent by CBCT imaging.
Table 1.
CBCT diagnosis of impacted teeth and root resorption. CBCT, cone-beam computed tomography; EDAG, early dental age group; LDAG, late dental age group; LI, lateral incisor; RR, root resorption; 2D, panoramic imaging; 3D, CBCT.
| Authors | Sample size | 2D/3D | Results in accordance to CBCT |
|---|---|---|---|
| Durack et al. (19) | 10 | 2D + 3D | CBCT > 2D radiographs*: - Sensitivity - Specificity - Inter-examiner agreement |
| Goodell et al. (18) | 56 | 2D + 3D | Treatment plan on 2D differed with 3D in majority of cases |
| Patel et al. (17) | 15 | 2D + 3D | Correct treatment option: CBCT > intra-oral radiographs* |
| Ren et al. (20) | 160 | 2D + 3D | CBCT > 2D: Highly significant difference between periapical radiography and CBCT in detection of mild and moderate RR lesions (P < 0.05) |
| Tsolakis et al. (21) | 20 | 2D + 3D | CBCT more accurate diagnostic compared to 2D |
| Jawad et al. (16) | 42 | 2D + 3D | Improved RR detection rates of 63% with the use of CBCT |
| Hadler-Olsen et al. (22) | 59 | 3D | Best predictor for RR: if location of the canine mesial to the midline of the LI root in panoramic images |
| Lai et al. (14) | 134 | 3D | High accuracy of location, prevalence, and degree of RR with high interrater correlation |
| Sun et al. (23) | 41 | 3D | Roots of impacted teeth are significantly shorter than homonym teeth Roots of impacted teeth in EDAG shorter than in LDAG Dilaceration occurs mainly in LDAG |
*Statistically significant.
A higher incidence of root resorption and dilaceration was observed with CBCT than with 2D radiography (19,20,23). CBCT was also found to be practicable for observing root resorption of maxillary incisors related to normal and ectopically erupting canines (22). Among 2D modalities, panoramic imaging seemed to offer the best sensitivity, and occlusal and periapical radiographs the best specificity when it comes to detection of root resorption (21). Moreover, when predicting the exact palato-buccal position of impacted canines, periapical radiography was considered as the most specific of the conventional techniques (21). Also, this study revealed that occlusal and periapical radiographs had a higher specificity when it comes to root resorption detection. When predicting the exact palato-buccal position of impacted canines, periapical radiographs were considered the most specific technique. Still conventional radiology has a lot of disadvantages such as overlaps, magnification, distortions, and deformations. At that point, CBCT can offer a solution because of higher accuracy of dimensions and localizations.
On the basis of our findings in accordance with the DIMITRA (dentomaxillofacial paediatric imaging investigation towards low-dose radiation) project (24), CBCT can be considered justified in children for diagnosis and treatment planning of impacted teeth and root resorption.
Trauma
Only three evidence-based articles on the use of 3D imaging were found within the limits of our inclusion criteria. All related articles found were in vitro studies on adult population and were rejected from this review.
According to Doğan et al. (25), root fractures are easily overseen on 2D radiographs, due to the direction of the X-ray beam. Evaluation of root fractures should be done by several periapical radiographs at different angles. An occlusal radiograph can add some additional information. However, in those cases, CBCT offers a 3D view and is superior in detecting vertical root fractures.
Due to limitations of 2D radiography, Bernardes et al. (26) compared detection rates of root fractures on periapical radiographs to CBCT. They concluded that only 30–40 per cent were diagnosed on periapical radiographs, but 90 per cent were found by the use of CBCT.
In a study by Bornstein et al. (27), 68.2 per cent of horizontal root fractures were located in the middle third of the root and extended towards the cervical third on the palatal aspect. These cervical third fractures are known to have a poor prognosis, which strongly speaks for CBCT, because a missed diagnosis of a cervical fracture extension can lead to unfavourable outcomes. According to the latest recommendations of the SEDENTEXCT guidelines and the DIMITRA project, we can agree that CBCT contributes to more precise evaluation of the root fracture (8,24).
Cleft lip and/or palate
CBCT was found to be an excellent tool for determining bone volume and morphology (28–32) compared to 2D radiographs that provided limited 2D information (Table 2) (16,33–40). Furthermore, it was also helpful for assessing root morphology, development of the adjacent teeth close to the cleft area, and quantification of soft-tissue depth (41–44). The volume rendering using CBCT was a reproducible and feasible method to assess the outcome of secondary alveolar bone grafting (45–47). CBCT was a superior choice over a medical CT as it required 8–10 times lower effective dose using standard protocol (48). Nevertheless, CBCT imaging should be optimized and correctly indicated at the right time for this specific group of paediatric patients to minimize the associated risks (24).
Table 2.
Use of CBCT for CLP diagnosis in children. BCLP, bilateral cleft lip palate; CBCT, cone-beam computed tomography; CEJ-AC, cementoenamel junction–alveolar crest; CG, control group (side); CLP, cleft lip palate; F, female; M, male; UCLP, unilateral cleft lip palate.
| Authors | Sample size | 2D/3D | Results in accordance to CBCT |
|---|---|---|---|
| Wriedt et al. (46) | 20 (16 M; 4 F) | 2D + 3D | CBCT only justified in special cases |
| Buyuk et al. (29) | 44 (26 M; 18 F) | 3D | Prevalence of dehiscence was found higher in the CLP group compared to the CG |
| CG: 51 (21 M; 30 F) | |||
| Celebi et al. (41) | 40 (20 M; 20 F) | 3D | Root volume assessment by using CBCT reveals smaller volume of roots on the cleft side compared to the non-cleft side |
| CG: 40 (20 M; 20 F) | |||
| Celikoglu et al. (37) | UCLP: 24 | 3D | UCLP and BCLP have insignificantly decreased values of mandibular volume compared to a normal occlusion group, evaluated by CBCT |
| BCLP: 17 | |||
| CG: 25 | |||
| Ercan et al. (31) | 31 (7 F; 24 M) | 3D | Bone thickness assessment by using CBCT: smaller bone thickness on the cleft side; mean CEJ-AC distance for central teeth: UCLP region > non-cleft region* |
| Garib et al. (28) | BCLP: 10 (5 M; 5 F) | 3D | CBCT is a useful method to assess alveolar bone plate thickness and bone dehiscence in teeth, adjacent to clefts |
| Janssen et al. (47) | 11 (6 M; 5 F) | 3D | CBCT is reliable at relatively low resolution for volumetric analysis |
| Lee et al. (38) | UCLP: 7 (3 M; 4 F) | 3D | Volume (bone graft) ~ volume(cleft) r = 0.96* |
| Lin et al. (33) | 30 (20 M; 10 F) | 3D | Facial asymmetry assessment by using CBCT showed more severe lower facial asymmetry: more asymmetrical positions and rotations of the condyles, with a positive correlation with chin deviation in UCLP patients |
| CG: 40 (16 M; 24 F) | |||
| Lin et al. (34) | 30 (18 M; 12 F) | 3D | UCLP patients had more retrusive maxillary and mandibular positions relative to the cranial base (P < 0.001 and P = 0.003, respectively); UCLP group had more severe vertical discrepancies* |
| CG: 30 (17 M; 13 F) | |||
| Linderup et al. (42) | 10 (6 M; 4 F) | 3D | CBCT is a reproducible and practical method for assessing the volumetric outcome of secondary alveolar bone grafting in UCLP patients |
| Oberoi et al. (45) | 21 (15 M; 6 F) | 3D | Volume rendering using CBCT is reproducible and practical method to assess preoperative alveolar cleft volume |
| Paknahad et al. (39) | 60 (20 UCLP; 20 BCLP; 20 controls) | 3D | CBCT evaluation showed that the mandible appears to be leading factor in facial asymmetry in CLP patients |
| Starbuck et al. (35) | 15 BCLP (11 M; 4 F) | 3D | 3D imaging allows increased access, assessment, and measurement of craniofacial structures; BCLP deformity alters facial skeletal morphology of the midface, the oronasal region, and the upper facial skeleton. All these results were statistically significant |
| CG: 15 (11 M; 4 F) | |||
| Starbuck et al. (36) | UCLP: 26 (17 M; 9 F) | 3D | UCLP congenital anomaly is strongly associated with dysmorphology and asymmetry of the nasal regions of the midface; morphometric differences were also found for the upper and lower facial skeletons |
| CG: 26 (17 M; 9 F) | |||
| Starbuck et al. (44) | 55 (40 M; 15 F) | 3D | Significant differences in tissue depth symmetry were found around the cutaneous upper lip and nose in unilateral CLP patients |
| Yang et al. (40) | UCLP: 21 (13 M; 8 F) | 3D | CBCT assessment of facial asymmetry concluded that significant differences between cleft and non-cleft sides only exist around the cleft, and not in deeper regions of maxillary complex |
| CG: 14 (6 M; 8 F) | |||
| Zhang et al. (43) | 40 (30 M; 10 F) | 3D | Significant delay in dental development in cleft patients |
| Zhou et al. (42) | 60 CLP (40 UCLP; 20 BCLP) | 3D | CBCT is a valid tool to evaluate developmental deficiency in teeth adjacent to the cleft; permanent upper incisors in CLP patients are underdeveloped |
| CG: 53 |
*Statistically significant.
Congenital dental anomalies
Only two studies were considered relevant in this review with regard to dental anomalies but did not show hard evidence-based characteristics (Table 3). Both studies observed CBCT to be a reliable tool in comparison to 2D radiographs for assessing supernumerary teeth and dens invaginatus (49,50).
Table 3.
CBCT diagnosis for congenital dental anomalies and congenital deformities. CBCT, Cone-beam computed tomography; F, female; M, male; PRS, Pierre Robin Sequence; TCS, Treacher Collins Syndrome; 2D, panoramic imaging; 3D, CBCT.
| Authors | Sample size | 2D/3D | Results in accordance to CBCT |
|---|---|---|---|
| Congenital dental anomalies | |||
| Jung et al. (49) | 193 (144 M; 49 F) | 2D + 3D | Supernumerary teeth were most frequently observed in the central incisor region, palatal position, inverted orientation, and most commonly conical shaped; 71%: delayed eruption of adjacent incisors; displacement of incisors: commonly observed |
| Capar et al. (50) | 300 | 2D + 3D | Visualization of DI: CBCT >> 2D*; CBCT provides an accurate representation of the external and internal dental anatomy |
| Congenital facial anomalies and syndromes | |||
| Tucunduva et al. (51) | 15 (6 M; 9 F) | 2D + 3D | Morphology of interforaminal region of the mandible showed no significant difference when compared to the controls; CBCT is important in surgical planning of interforaminal mandible region |
| 10 PRS | |||
| 10 TCS | |||
| 10 Controls | |||
*Statistically significant.
Congenital facial anomalies and syndromes
CBCT examination was vital for assessing morphology of the interforaminal region of mandible and for identifying anatomic variations of anterior loop and mandibular inferior canal in patients with Treacher Collins Syndrome and Pierre Robin Sequence (Table 3) (51). Because patients with congenital anomalies frequently show anatomic variations in the maxillofacial region, preoperative CBCT evaluation is of high importance for avoiding surgical complications.
Temporomandibular joint abnormalities
Regarding temporomandibular joint (TMJ) dysfunction, only three articles were included. CBCT was regarded as an accurate and reliable tool for assessing 3D condylar volume, shape, and angulation objectively in paediatric patients with bilateral cleft lip and palate, unilateral posterior crossbite, and juvenile idiopathic arthritis (Table 4) (52–54).
Table 4.
CBCT diagnosis of TMJ and juvenile rheumatoid arthritis in children. CBCT, cone-beam computed tomography; TMJ, temporomandibular joint; JIA, juvenile idiopathic arthritis; F, female; M, male; CG, control group.
| Authors | Sample size | 2D/3D | Results in accordance to CBCT |
|---|---|---|---|
| Huntjens et al. (54) | 20 (14 F; 6 M) | 3D | Condylar asymmetry is a common feature in children with JIA* |
| Illipronti-Filho et al. (55) | 20 | 3D | Difference between right and left condyles and in the crossed and non-crossed sides in sagittal and coronal cuts, in case of unilateral posterior crossbite (NS) |
| Ucar, et al. (56) | 17 (7 F; 10 M) | 3D | Condylar volume was slightly less in the bilateral cleft group compared to controls (P > 0.05); position of the mandibular condyle and temporomandibular fossa: similar in bilateral cleft group and controls |
| CG: 17 (6 F; 11 M) |
NS, non-significant.
*Statistically significant.
Discussion
The possibilities of CBCT application for orthodontic reasons range from impacted teeth to TMJ morphology. According to some studies, CBCT should not be considered as a routine and standard method of diagnosis and treatment planning, based on its high radiation dose compared with conventional radiographs and availability of limited supporting evidence (55,56). Supplementary Table 2 provides an overview of the radiation doses used in the selected articles compared to the panoramic equivalent. According to the American Academy of Oral and Maxillofacial Radiology selection criteria and SEDENTEXCT, small-field-of-view (FOV) CBCT can be indicated for pre-treatment assessment of dental structures or position anomalies (7,8). However, a small-FOV CBCT cannot be seen as a true alternative for panoramic radiograph as the latter covers the whole dentomaxillofacial region (48).
Recently, the DIMITRA position statement described indication-oriented and patient-specific recommendations regarding the main CBCT applications for children (24). Table 5 illustrates the summary of CBCT use for dental diseases based on the SEDENTEXCT guidelines and the DIMITRA position statement (7, 24).
Table 5:
Recommendations based on the SEDENTEXCT guidelines and the DIMITRA position statement. CBCT, cone-beam computed tomography
| Pathology | Use of CBCT | Except for | |
|---|---|---|---|
| SEDENTEXCT (7) | DIMITRA (24) | ||
| Impacted teeth | ⋎ | ⋎ | |
| Dental trauma | × | × | Root fractures; suspicion of condylar fracture |
| Facial trauma | ⋎ | ⋎ | |
| CLP | ⋎ | ⋎ | |
| Congenital anomalies and syndromes | ⋎ | ⋎ | |
| Dental anomalies | When 2D modalities do not answer the diagnostic question | ||
| Dens invaginatus | × | × | |
| External resorption | ⋎ | ⋎ | |
| Internal resorption | ⋎ | ⋎ | |
| Differentiation from normal anatomy | ⋎ | ⋎ | |
| Bone pathology | When 2D modality does not answer the diagnostic question; MSCT/MR: when evaluation of soft tissues is necessary; in case of inadequate information on MSCT/MR: CBCT | ||
| Dentigerous cysts | × | × | |
| Periapical lesions | × | × | |
| TMJ (bony pathology) | ⋎ | ⋎ | Disk visualization |
| Orthognathic surgery | ⋎ | ⋎ | |
| Periodontal assessment | × | × | infrabony defects and furcation lesions |
| Periapical disease | × | × | In case of negative findings on conventional radiographs and positive clinical signs |
⋎, justified; ×, not recommended; MSCT/MR, multi-slice computed tomography/magnetic resonance.
Impacted teeth and root resorption
We learned from past reviews that CBCT is commonly used to evaluate the exact position and localization of the impacted teeth (57–60). Studies show that CBCT was more feasible in detecting canine apices, lateral root resorption, and dilaceration compared to 2D radiographs (61). Therefore, it can be hypothesized that CBCT shows better outcome efficacy in complex cases (21,62). Also, in some studies, original treatment plans of more than 25 per cent cases were changed when consulting CBCT images compared to conventional 2D imaging (63–65).
However, there is still lack of evidence supporting CBCT application in paediatric patients for diagnosis, treatment planning, and improving outcomes. Future research has to be undertaken to compare the efficacy of CBCT with that of conventional radiographs in patients with multidisciplinary pathologies.
Trauma
In vivo studies of 3D imaging in paediatric trauma are very rare; for that reason, we included some in vitro and adult studies, although the exclusion criteria were set for these studies. This review suggested that CBCT is more accurate to assess vertical root fractures than 2D imaging, which is also in accordance with the included studies (25–27,66). Despite the advantages, a CBCT scan exposes the patient with additional radiation; hence, it should only be reserved for suspected root fractures diagnosed initially by clinical signs and 2D radiographs.
Cleft lip and/or palate
Many articles have been published concerning the use of CBCT in patients with cleft lip and/or (CL/P). Earlier, conventional medical CT was the most accepted method for assessing CL/P and the adjacent teeth. Now, CBCT can be assumed a better choice for assessing bone volume, deficiencies, and root development, because it provides a better image quality and a significantly lower radiation dose (28–47). No evidence is available showing that CBCT is more informative than 2D concerning facial soft-tissue analysis.
Congenital dental anomalies
Despite the limited evidence on this topic, we still support the superiority of CBCT above 2D radiographs for assessment and surgical planning of supernumerary teeth that are often accompanied by delayed eruption of adjacent teeth. Also, in case of dens invaginatus, fusion, or gemination, CBCT can be of great value for endodontic reasons (67). CBCT should be used only when 2D radiograph fails to provide appropriate information.
Congenital facial anomalies and syndromes
Because congenital deformities are not that common, studies with large samples were not available to our knowledge. Many case reports have been published on congenital deformities; however, not much information is available regarding the superiority of CBCT. On the basis of this review, CBCT should only be considered in cases where 2D imaging fails to provide enough information, and it should not be used as the first diagnostic tool.
TMJ abnormalities
For the assessment of osseous TMJ abnormalities, CBCT imaging is superior to magnetic resonance imaging (MRI) and conventional 2D radiographic methods. However, MRI is the method of choice for the assessment of inflammatory activity and soft-tissue abnormalities (68). Several case reports used CBCT as a first diagnostic aid instead of 2D radiograph. For that reason, it can be predicted that CBCT can have a beneficial role in the assessment of bony pathology of jaws. The results from the case reports showed that CBCT was mainly used for diagnostic and surgical reasons (Supplementary Table 1).
Conclusion
From this review, we can conclude that there is still lack of evidence considering optimization and justification for the use of CBCT in the paediatric population. CBCT can be regarded as a reliable diagnostic tool in both simple and complex cases where 3D assessment is mandatory for making the most appropriate therapeutic decision. The authors recommend strict adherence to the DIMITRA guidelines when selecting CBCT for paediatric examination.
Limitations
The limitations related to this study included the absence of randomized controlled trials, ethical issues related to study design of certain studies (69), and lack of specifically paediatric-oriented studies. According to systematic review requirements, in vitro and ex vivo studies were excluded. This study was not registered in advance.
Funding
No funding was available.
Supplementary Material
Acknowledgements
We would like to thank Marleen Michels, who helped us in the most professional way throughout the search strategy at the 2Bergen–Biomedical Library, Catholic University of Leuven, Belgium.
Conflict of interest
None declared.
References
- 1. Neilufar A., David R.M., Julian O. and Joseph H.N (2014)Digital versus plaster study models: how accurate and reproducible are they?Journal of Orthodontics, 39, 151–159. [DOI] [PubMed] [Google Scholar]
- 2. Arai Y., Tammisalo E., Iwai K., Hashimoto K. and Shinoda K (1999)Development of a compact computed tomographic apparatus for dental use. Dento Maxillo Facial Radiology, 28, 245–248. [DOI] [PubMed] [Google Scholar]
- 3. Berkhout W.E. (2015)[The ALARA-principle. Backgrounds and enforcement in dental practices]. Nederlands tijdschrift voor tandheelkunde, 122, 263–270. [DOI] [PubMed] [Google Scholar]
- 4. Jacobs R. (2011)Dental cone beam CT and its justified use in oral health care. JBR-BTR: organe de la Societe royale belge de radiologie (SRBR) = orgaan van de Koninklijke Belgische Vereniging voor Radiologie (KBVR), 94, 254–265. [DOI] [PubMed] [Google Scholar]
- 5. Frush D.P. (2011)Justification and optimization of CT in children: how are we performing?Pediatric Radiology. 41(Suppl 2), 467–471. [DOI] [PubMed] [Google Scholar]
- 6. Schulze D., Heiland M., Thurmann H. and Adam G (2004)Radiation exposure during midfacial imaging using 4- and 16-slice computed tomography, cone beam computed tomography systems and conventional radiography. Dento Maxillo Facial Radiology, 33, 83–86. [DOI] [PubMed] [Google Scholar]
- 7. European Commission(2012). Radiation protection No 172: cone beam CT for dental and maxillofacial radiology. Evidence based guidelines. www.sedentexct.eu/files/radiation_protection_172.pdf [Google Scholar]
- 8. International commission on Radiological Protection(2007). The 2007 recommendations of the International Commission on Radiological Protection. ICRP publication 103. Annals of ICRP, 37, 1–332. [DOI] [PubMed] [Google Scholar]
- 9. Khong, P-L., Ringertz, H., Donoghue, V., Frush, D., Rehani, M., Appelgate, K., Sanchez R, et al.(2013). ICRP Publication 121: radiological protection in paediatric diagnostic and interventional radiology. Annals of ICRP. 42, 1–63. [DOI] [PubMed] [Google Scholar]
- 10. Liberati A., Altman D.G., Tetzlaff J., Mulrow C., Gøtzsche P.C., Ioannidis J.P., Clarke M., Devereaux P.J., Kleijnen J. and Moher D (2009)The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. British Medical Journal (Clinical research ed.), 339, b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Fryback DG, Thornbury JR (1991)The efficacy of diagnostic imaging. Medical Decision Making, 11:88–94. [DOI] [PubMed] [Google Scholar]
- 12. Whiting P., Rutjes A.W., Reitsma J.B., Bossuyt P.M. and Kleijnen J (2003)The development of QUADAS: a tool for the quality assessment of studies of diagnostic accuracy included in systematic reviews. BMC Medical Research Methodology, 3, 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Jaeschke R., Guyatt G. and Sackett D.L (1994)Users’ guides to the medical literature. III. How to use an article about a diagnostic test. A. Are the results of the study valid? Evidence-Based Medicine Working Group. The Journal of the American Medical Association, 271, 389–391. [DOI] [PubMed] [Google Scholar]
- 14. Lai C.S., Bornstein M.M., Mock L., Heuberger B.M., Dietrich T. and Katsaros C (2013)Impacted maxillary canines and root resorptions of neighbouring teeth: a radiographic analysis using cone-beam computed tomography. European Journal of Orthodontics, 35, 529–538. [DOI] [PubMed] [Google Scholar]
- 15. Manne R., Gandikota C., Juvvadi S.R., Rama H.R. and Anche S (2012)Impacted canines: etiology, diagnosis, and orthodontic management. Journal of Pharmacy and Bioallied Sciences, 4, S234–S238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Jawad Z., et al. (2016)A review of cone beam computed tomography for the diagnosis of root resorption associated with impacted canines, introducing an innovative root resorption scale. Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology, 122, 765–771. [DOI] [PubMed] [Google Scholar]
- 17. Patel S., Dawood A., Wilson R., Horner K. and Mannocci F (2009)The detection and management of root resorption lesions using intraoral radiography and cone beam computed tomography—an in vivo investigation. International Endodontic Journal, 42, 831–838. [DOI] [PubMed] [Google Scholar]
- 18. Goodell K.B., Mines P. and Kersten D.D (2018)Impact of cone-beam computed tomography on treatment planning for external cervical resorption and a Novel Axial Slice-based Classification System. Journal of Endodontics, 44, 239–244. [DOI] [PubMed] [Google Scholar]
- 19. Durack C., Patel S., Davies J., Wilson R. and Mannocci F (2011)Diagnostic accuracy of small volume cone beam computed tomography and intraoral periapical radiography for the detection of simulated external inflammatory root resorption. International Endodontic Journal, 44, 136–147. [DOI] [PubMed] [Google Scholar]
- 20. Ren H., Chen J., Deng F., Zheng L., Liu X. and Dong Y (2013)Comparison of cone-beam computed tomography and periapical radiography for detecting simulated apical root resorption. The Angle Orthodontist, 83, 189–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Tsolakis A.I., Kalavritinos M., Bitsanis E., Sanoudos M., Benetou V., Alexiou K. and Tsiklakis K (2018)Reliability of different radiographic methods for the localization of displaced maxillary canines. American Journal of Orthodontics and Dentofacial Orthopedics, 153, 308–314. [DOI] [PubMed] [Google Scholar]
- 22. Hadler-Olsen S., Pirttiniemi P., Kerosuo H., Bolstad Limchaichana N., Pesonen P., Kallio-Pulkkinen S. and Lähdesmäki R (2015)Root resorptions related to ectopic and normal eruption of maxillary canine teeth—a 3D study. Acta Odontologica Scandinavica, 73, 609–615. [DOI] [PubMed] [Google Scholar]
- 23. Sun H., Wang Y., Sun C., Ye Q., Dai W., Wang X., Xu Q., Pan S. and Hu R (2014)Root morphology and development of labial inversely impacted maxillary central incisors in the mixed dentition: a retrospective cone-beam computed tomography study. American Journal of Orthodontics and Dentofacial Orthopedics, 146, 709–716. [DOI] [PubMed] [Google Scholar]
- 24. Oenning A.C., Jacobs R., Pauwels R., Stratis A., Hedesiu M. and Salmon B; DIMITRA Research Group , http://www.dimitra.be. (2018)Cone-beam CT in paediatric dentistry: DIMITRA project position statement. Pediatric Radiology, 48, 308–316. [DOI] [PubMed] [Google Scholar]
- 25. Doğan M.S., Callea M., Kusdhany L.S., Aras A., Maharani D.A., Mandasari M., Adiatman M. and Yavuz I (2018)The evaluation of root fracture with cone beam computed tomography (CBCT): an epidemiological study. Journal of Clinical and Experimental Dentistry, 10, e41–e48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Bernardes R.A., de Moraes I.G., Húngaro Duarte M.A., Azevedo B.C., de Azevedo J.R. and Bramante C.M (2009)Use of cone-beam volumetric tomography in the diagnosis of root fractures. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontics, 108, 270–277. [DOI] [PubMed] [Google Scholar]
- 27. Bornstein M.M., Wölner-Hanssen A.B., Sendi P. and von Arx T (2009)Comparison of intraoral radiography and limited cone beam computed tomography for the assessment of root-fractured permanent teeth. Dental Traumatology, 25, 571–577. [DOI] [PubMed] [Google Scholar]
- 28. Garib D.G., Yatabe M.S., Ozawa T.O. and Filho O.G (2012)Alveolar bone morphology in patients with bilateral complete cleft lip and palate in the mixed dentition: cone beam computed tomography evaluation. The Cleft Palate-Craniofacial Journal, 49, 208–214. [DOI] [PubMed] [Google Scholar]
- 29. Buyuk S.K., Ercan E., Celikoglu M., Sekerci A.E. and Hatipoglu M (2016)Evaluation of dehiscence and fenestration in adolescent patients affected by unilateral cleft lip and palate: a retrospective cone beam computed tomography study. The Angle Orthodontist, 86, 431–436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Oh T.S., Park J.S., Choi J.W., Kwon S.M. and Koh K.S (2016)Risk factor analysis of bone resorption following secondary alveolar bone grafting using three-dimensional computed tomography. Journal of Plastic, Reconstructive & Aesthetic Surgery, 69, 487–492. https://ec.europa.eu/energy/sites/ener/files/documents/172.pdf [DOI] [PubMed] [Google Scholar]
- 31. Ercan E., Celikoglu M., Buyuk S.K. and Sekerci A.E (2015)Assessment of the alveolar bone support of patients with unilateral cleft lip and palate: a cone-beam computed tomography study. The Angle Orthodontist, 85, 1003–1008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Linderup B.W., Küseler A., Jensen J. and Cattaneo P.M (2015)A novel semiautomatic technique for volumetric assessment of the alveolar bone defect using cone beam computed tomography. The Cleft Palate-Craniofacial Journal, 52, e47–e55. [DOI] [PubMed] [Google Scholar]
- 33. Lin Y., Chen G., Fu Z., Ma L. and Li W (2015)Cone-beam computed tomography assessment of lower facial asymmetry in unilateral cleft lip and palate and non-cleft patients with class III skeletal relationship. PLoS One, 10, e0130235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Lin Y., Fu Z., Ma L. and Li W (2016)Cone-beam computed tomography-synthesized cephalometric study of operated unilateral cleft lip and palate and noncleft children with Class III skeletal relationship. American Journal of Orthodontics and Dentofacial Orthopedics, 150, 802–810. [DOI] [PubMed] [Google Scholar]
- 35. Starbuck J.M., Ghoneima A. and Kula K (2015)A multivariate analysis of unilateral cleft lip and palate facial skeletal morphology. The Journal of Craniofacial Surgery, 26, 1673–1678. [DOI] [PubMed] [Google Scholar]
- 36. Starbuck J.M., Ghoneima A. and Kula K (2015)Bilateral cleft lip and palate: a morphometric analysis of facial skeletal form using cone beam computed tomography. Clinical Anatomy (New York, N.Y.), 28, 584–592. [DOI] [PubMed] [Google Scholar]
- 37. Celikoglu M., Ucar F.I., Buyuk S.K., Celik S., Sekerci A.E. and Akin M (2016)Evaluation of the mandibular volume and correlating variables in patients affected by unilateral and bilateral cleft lip and palate: a cone-beam computed tomography study. Clinical Oral Investigations, 20, 1741–1746. [DOI] [PubMed] [Google Scholar]
- 38. Lee D., Atti E., Blackburn J., Yen S., Lee D., Tetradis S. and Hong C (2013)Volumetric assessment of cleft lip and palate defects using cone beam computed tomography. Journal of the California Dental Association, 41, 813–817. [PubMed] [Google Scholar]
- 39. Paknahad M., Shahidi S., Bahrampour E., Beladi A. S., and Khojastepour L (2018). Cone beam computed tomographic evaluation of mandibular asymmetry in patients with cleft lip and palate. The Cleft Palate-Craniofacial Journal, 55, 919–924. [DOI] [PubMed] [Google Scholar]
- 40. Yang L., Chen Z. and Zhang X (2016)A cone-beam computed tomography evaluation of facial asymmetry in unilateral cleft lip and palate individuals. Journal of Oral Science, 58, 109–115. [DOI] [PubMed] [Google Scholar]
- 41. Celebi A.A., Ucar F.I., Sekerci A.E., Caglaroglu M. and Tan E (2015)Effects of cleft lip and palate on the development of permanent upper central incisors: a cone-beam computed tomography study. European Journal of Orthodontics, 37, 544–549. [DOI] [PubMed] [Google Scholar]
- 42. Zhou W., Li W., Lin J., Liu D., Xie X. and Zhang Z (2013)Tooth lengths of the permanent upper incisors in patients with cleft lip and palate determined with cone beam computed tomography. The Cleft Palate-Craniofacial Journal, 50, 88–95. [DOI] [PubMed] [Google Scholar]
- 43. Zhang X., Zhang Y., Yang L., Shen G. and Chen Z (2016)Asymmetric dental development investigated by cone-beam computed tomography in patients with unilateral cleft lip and alveolus. The Cleft Palate-Craniofacial Journal, 53, 413–420. [DOI] [PubMed] [Google Scholar]
- 44. Starbuck J.M., Ghoneima A. and Kula K (2014)Facial soft-tissue asymmetry in three-dimensional cone-beam computed tomography images of children with surgically corrected unilateral clefts. The Journal of Craniofacial Surgery, 25, 476–480. [DOI] [PubMed] [Google Scholar]
- 45. Oberoi S., Chigurupati R., Gill P., Hoffman W.Y. and Vargervik K (2009)Volumetric assessment of secondary alveolar bone grafting using cone beam computed tomography. The Cleft Palate-Craniofacial Journal, 46, 503–511. [DOI] [PubMed] [Google Scholar]
- 46. Wriedt S., Al-Nawas B., Schmidtmann I., Eletr S., Wehrbein H., Moergel M. and Jacobs C (2017)Analyzing the teeth next to the alveolar cleft: examination and treatment proposal prior to bone grafting based on three-dimensional versus two-dimensional diagnosis—a diagnostic study. Journal of Cranio-maxillo-facial Surgery, 45, 1272–1277. [DOI] [PubMed] [Google Scholar]
- 47. Janssen N.G., Schreurs R., Bittermann G.K.P., Borstlap W.A., Koole R., Meijer G.J. and Maal T.J.J (2017)A novel semi-automatic segmentation protocol for volumetric assessment of alveolar cleft grafting procedures. Journal of Cranio-Maxillo-Facial Surgery, 45, 685–689. [DOI] [PubMed] [Google Scholar]
- 48. Pauwels R. (2015)Cone beam CT for dental and maxillofacial imaging: dose matters. Radiation Protection Dosimetry, 165, 156–161. [DOI] [PubMed] [Google Scholar]
- 49. Jung Y.H., Kim J.Y. and Cho B.H (2016)The effects of impacted premaxillary supernumerary teeth on permanent incisors. Imaging Science in Dentistry, 46, 251–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Capar I.D., Ertas H., Arslan H. and Tarim Ertas E (2015)A retrospective comparative study of cone-beam computed tomography versus rendered panoramic images in identifying the presence, types, and characteristics of dens invaginatus in a Turkish population. Journal of Endodontics, 41, 473–478. [DOI] [PubMed] [Google Scholar]
- 51. Tucunduva R.M., Imada T.S., Lopes I.A., Rubira-Bullen I.R. and de Carvalho I.M (2016)Evaluation of interforaminal mandible region of individuals with Pierre Robin sequence and Treacher Collins syndrome through the cone-beam computed tomography. The Journal of Craniofacial Surgery, 27, 219–221. [DOI] [PubMed] [Google Scholar]
- 52. Huntjens E., Kiss G., Wouters C. and Carels C (2008)Condylar asymmetry in children with juvenile idiopathic arthritis assessed by cone-beam computed tomography. European Journal of Orthodontics, 30, 545–551. [DOI] [PubMed] [Google Scholar]
- 53. Uçar F.I., Buyuk S.K., Şekerci A.E. and Celikoglu M (2016)Evaluation of temporomandibular fossa and mandibular condyle in adolescent patients affected by bilateral cleft lip and palate using cone beam computed tomography. Scanning, 38, 720–726. [DOI] [PubMed] [Google Scholar]
- 54. Illipronti-Filho E., Fantini S.M. and Chilvarquer I (2015)Evaluation of mandibular condyles in children with unilateral posterior crossbite. Brazilian Oral Research, 29, 49. [DOI] [PubMed] [Google Scholar]
- 55. Garib D.G., Calil L.R., Leal C.R. and Janson G (2014)Is there a consensus for CBCT use in Orthodontics?Dental Press Journal of Orthodontics, 19, 136–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. van Vlijmen O.J., Kuijpers M.A., Bergé S.J., Schols J.G., Maal T.J., Breuning H. and Kuijpers-Jagtman A.M (2012)Evidence supporting the use of cone-beam computed tomography in orthodontics. Journal of the American Dental Association (1939), 143, 241–252. [DOI] [PubMed] [Google Scholar]
- 57. De Vos W., Casselman J. and Swennen G.R (2009)Cone-beam computerized tomography (CBCT) imaging of the oral and maxillofacial region: a systematic review of the literature. International Journal of Oral and Maxillofacial Surgery, 38, 609–625. [DOI] [PubMed] [Google Scholar]
- 58. Aps J.K. (2013)Cone beam computed tomography in paediatric dentistry: overview of recent literature. European Archives of Paediatric Dentistry, 14, 131–140. [DOI] [PubMed] [Google Scholar]
- 59. Van Acker J.W., Martens L.C. and Aps J.K (2016)Cone-beam computed tomography in pediatric dentistry, a retrospective observational study. Clinical Oral investigations, 20, 1003–1010. [DOI] [PubMed] [Google Scholar]
- 60. Kapila S.D. and Nervina J.M (2015)CBCT in orthodontics: assessment of treatment outcomes and indications for its use. Dento Maxillo Facial Radiology, 44, 20140282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Wriedt S., Jaklin J., Al-Nawas B. and Wehrbein H (2012)Impacted upper canines: examination and treatment proposal based on 3D versus 2D diagnosis. Journal of Orofacial Orthopedics = Fortschritte Der Kieferorthopadie: Organ/official Journal Deutsche Gesellschaft Fur Kieferorthopadie, 73, 28–40. [DOI] [PubMed] [Google Scholar]
- 62. Alqerban A., Jacobs R., Souza P.C. and Willems G (2009)In-vitro comparison of 2 cone-beam computed tomography systems and panoramic imaging for detecting simulated canine impaction-induced external root resorption in maxillary lateral incisors. American Journal of Orthodontics and Dentofacial Orthopedics, 136, 764.e1–11; discussion 764. [DOI] [PubMed] [Google Scholar]
- 63. Botticelli S., Verna C., Cattaneo P.M., Heidmann J. and Melsen B (2011)Two- versus three-dimensional imaging in subjects with unerupted maxillary canines. European Journal of Orthodontics, 33, 344–349. [DOI] [PubMed] [Google Scholar]
- 64. Haney E., Gansky S.A., Lee J.S., Johnson E., Maki K., Miller A.J. and Huang J.C (2010)Comparative analysis of traditional radiographs and cone-beam computed tomography volumetric images in the diagnosis and treatment planning of maxillary impacted canines. American Journal of Orthodontics and Dentofacial Orthopedics, 137, 590–597. [DOI] [PubMed] [Google Scholar]
- 65. Katheria B.C., Kau C.H., Tate R., Chen J.W., English J. and Bouquot J (2010)Effectiveness of impacted and supernumerary tooth diagnosis from traditional radiography versus cone beam computed tomography. Pediatric Dentistry, 32, 304–309. [PubMed] [Google Scholar]
- 66. Varshosaz M., Tavakoli M.A., Mostafavi M. and Baghban A.A (2010)Comparison of conventional radiography with cone beam computed tomography for detection of vertical root fractures: an in vitro study. Journal of Oral Science, 52, 593–597. [DOI] [PubMed] [Google Scholar]
- 67. Baumgart M., Hänni S., Suter B., Schaffner M. and Lussi A (2009)[Dens invaginatus. Review of the literature and diagnostic and therapeutic guidelines]. Schweizer Monatsschrift fur Zahnmedizin = Revue mensuelle suisse d’odonto-stomatologie = Rivista mensile svizzera di odontologia e stomatologia, 119, 697–714. [PubMed] [Google Scholar]
- 68. Larheim T.A., Abrahamsson A.K., Kristensen M. and Arvidsson L.Z (2015)Temporomandibular joint diagnostics using CBCT. Dento Maxillo Facial Radiology, 44, 20140235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Smith G.C. and Pell J.P (2003)Parachute use to prevent death and major trauma related to gravitational challenge: systematic review of randomised controlled trials. British Medical Journal (Clinical research ed.), 327, 1459–1461. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.