Abstract
Objective
Approximately 55–76% of Service members use dietary supplements for various reasons; although such use has become popular, decisions are often driven by information that is not evidence-based. This work evaluates whether current research on dietary ingredients for chronic musculoskeletal pain provides sufficient evidence to inform decisions for practice and self-care, specifically for Special Operations Forces personnel.
Methods
A steering committee convened to develop research questions and factors required for decision-making. Key databases were searched through August 2016. Eligible systematic reviews and randomized controlled trials were assessed for methodological quality. Meta-analysis was applied where feasible. Grading of Recommendations, Assessment, Development and Evaluation was used to determine confidence in the effect estimates. The committee used a decision table to make evidence-informed judgments across decision-making factors and recommendations for practice and self-care use.
Results
Nineteen dietary ingredients were assessed. No recommendations were given for boswellia, ginger, rose hip, or s-adenosyl-L-methionine (SAMe); specifically, although ginger can be obtained via food, no recommendation is provided for use as a supplement due to unclear research. Further, there were insufficient strong research on boswellia and SAMe and possible compliance issues (i.e., high number of capsules required daily) associated with rose hip.
Conclusions
No recommendations were made when the evidence was low quality or trade-offs were so closely balanced that any recommendation would be too speculative. Research recommendations are provided to enhance the quality and body of evidence for the most promising ingredients. Clinicians and those with chronic pain can rely on evidence-based recommendations to inform their decisions.
Keywords: Systematic Review, Meta-analysis, Dietary Ingredients, Supplements, Chronic Pain, Musculoskeletal Pain, Special Operations Personnel, Practice Recommendations, Evidence-Based Practice
Introduction
The US military is exposed to extreme demands of physical training and combat missions and, as a result, may develop musculoskeletal (MSK) injuries. Such injuries are a leading cause of pain, medical encounters, lost duty time, and disability [1–3]. The challenges associated with pain are not only recognized by the military but are also a major public health concern in the United States [4]. Due to the complex nature of pain, our understanding of and approaches to pain management may be variable and may or may not be aligned with the patient’s or practitioner’s perspectives. In addition, advice on what approaches to invest in may or may not be evidence-based.
Pain management options primarily consist of medications (e.g., nonsteroidal anti-inflammatory drugs [NSAIDs]), injections, physical therapy, acupuncture, and other modalities [5]. Dietary ingredients are currently marketed for a wide range of pain conditions, including joint pain, osteoarthritis, chronic gout, and gastrointestinal disorders. In fact, research shows that about 70–74% of the general adult population and 55–76% of Service members use dietary supplements [6,7]. Despite their popularity, evidence surrounding their safety and efficacy is still unclear [8–11]. Further, although evidence-based research is meant to inform appropriate and safe decisions about supplement use, decisions to use such supplements are often driven by information that is not evidence-based (e.g., advice from peers, family members, and other sources).
As part of the US Special Operations Command’s Preservation of the Force and Family Behavioral Health Program, this project sought to determine whether current research on dietary ingredients for chronic MSK pain could provide the evidence needed to inform decisions for practice and self-care use. To achieve this, state-of-the-science evidence methodologies were applied to provide clear, comprehensive, and unbiased information to Special Operations Forces (SOF) personnel and enable key stakeholders and subject matter experts to make evidence-based recommendations to inform policy decisions regarding dietary ingredients for improving pain and pain-related (e.g., psychological health, quality of life) outcomes.
The aim of this article was to describe the ingredients for which no evidence-based use recommendations were made; in these cases, evidence was either low quality or trade-offs were so closely balanced that any recommendation would have been too speculative at this point. Factors causing the downgrading of quality or trade-offs are transparently described in the hopes of focusing and/or advancing research in these areas, where most appropriate. From a clinical standpoint, practitioners can rely on this evidence to assist patients with deciding which supplements are worth taking for pain. This paper is the third in a series of articles [12–14] that detail the relevance of this work to SOF, the evidence-based recommendations made, and the implications on how evidence-based information might impact policy decisions surrounding the use of dietary ingredients for improving pain and related outcomes. It is important to note that although formal processes were followed and recommendations made, this is not intended to serve as a formal clinical practice guideline.
Methods
The project’s full methodological approach is detailed within the first of this series of three articles and is included as Supplementary Data: Detailed Methodology [14]. Briefly, 1) the authors relied upon the Institute of Medicine guidelines to ensure transparent processes were followed and conflicts of interest were managed/mitigated in the selection and recruitment of a group of key stakeholders and subject matter experts [15]. The committee, named the Holistic Evidence Review Board (HERB), was convened to develop essential research questions and definitions (Table 1) and assess the factors required for decision-making (Supplementary Data: GRADE Grid) [5,16–20]; 2) a review team, independent of HERB, then conducted a series of systematic reviews to assess the current state of the evidence and to explore the safety and efficacy of various dietary ingredients for treating pain and related outcomes (Supplementary Data: Summary Report); 3) the gathered evidence was integrated with the expertise of these subject matter experts; and 4) modified Delphi methods were used to develop evidence-based recommendations for the use of dietary ingredients as well as priority areas in need of future research following the Grading of Recommendations, Assessment, Development and Evaluation (GRADE) evidence to decision framework [14,21–24]. The systematic review evidence used to inform recommendations is reported in Supplementary Data: Summary Report.
Table 1.
Focused PICOS used to define the narrowed research question: Are there dietary supplements/ingredients that can safely mitigate chronic pain in adults (18+ years old) with musculoskeletal disorders?
| Population | Adults (18+ years) with chronic pain due to musculoskeletal disorders. |
| Chronic pain was defined as ongoing or recurrent pain, lasting beyond the usual course of acute illness or injury (i.e., >3 months and occurring at least half of the days over the past 6 months), and which adversely affects the individual’s well-being [5,16]. | |
| Musculoskeletal pain was defined as pain affecting the bones, muscles, and ligaments, or disorders of the muscles, nerves, tendons, joints, and cartilage, and disorders of the nerves, tendons, muscles, and supporting structures of the upper and lower limbs, neck, and lower back that are caused, precipitated, or exacerbated by sudden exertion or prolonged exposure to physical factors such as repetition, force, vibration, or awkward posture [17,18]. Note that headaches/migraines and musculoskeletal pain conditions resulting from another disease or injury (e.g., fracture, contusion, abrasion, laceration) were excluded. | |
| Intervention | Any single or multiple (e.g., a combination of ingredients) dietary ingredient(s) [19,20]. |
| Control/comparison | Sham, no treatment, and/or active comparator. |
| Outcome(s) | Pain, physical function, sleep, mood (anxiety/depression), stress, cognitive performance, global health, health-related quality of life, behavior, resource use, adverse events. |
| Study design | Peer-reviewed systematic reviews/meta-analyses and/or randomized controlled trials presented in the English language. |
PICOS = Population, Intervention, Comparison, Outcomes and Study Designs.
Conditional recommendations were made when the desirable anticipated effects outweighed the undesirable effects but there was uncertainty about the trade-offs, either because the key evidence was of low quality or because the benefits and downsides were closely balanced. No recommendations were made either because the quality of the evidence was too low or trade-offs were so closely balanced that any recommendation would be too speculative. Recommendations against the current use of an ingredient, based on available evidence, were made when undesirable anticipated effects outweighed the desirable effects or the downsides clearly outweighed the benefits overall [21].
Results
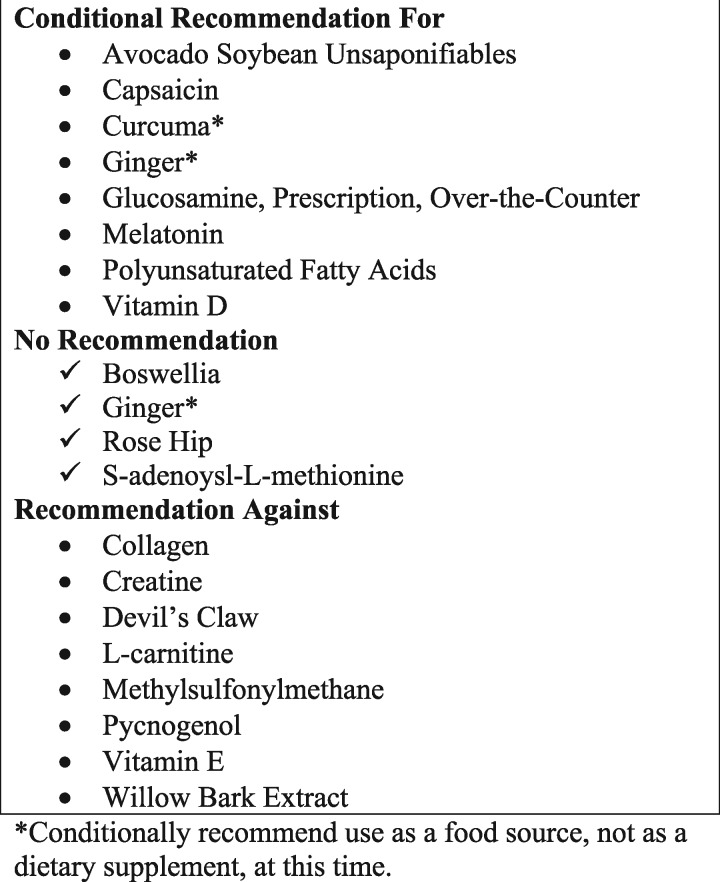
Nineteen dietary ingredients were identified and evaluated using systematic review methods (Supplementary Data: Detailed Methodology, Supplementary Data: Summary Report) [14]. Integrating the evidence with the HERB clinical acumen across the decision-making factors, three types of recommendations were ultimately made for these dietary ingredients (Figure 1).
Figure 1.
Recommendations. *Conditionally recommend use as a food source, not as a dietary supplement, at this time.
This article details dietary ingredients for which no recommendation was ultimately made. No recommendations were offered for boswellia [25–35], ginger [36–46], rose hip [47–51], or s-adenosyl-L-methionine (SAMe) [52–58]. Note that although ginger is conditionally recommended as a food source [13], use as a supplement was not recommended. Table 2 displays the ingredients where no practice recommendations were made, the graded evidence for efficacy and safety, and other considerations noted when making recommendations. Table 3 details the summary of judgments across factors and the resulting recommendations.
Table 2.
Summary of findings
| Ingredient Evaluated | Comparators | No. Studies/Participants | Populations | Outcomes | Evidence | Quality | Adverse Events | Considerations |
|---|---|---|---|---|---|---|---|---|
| Boswellia* | vs placebo | 4/225† | Osteoarthritis | Pain reduction, 1–3 mo | SMD (6 trials) = –3.34, 83.5 pts greater reduction than placebo | Very low ⊕◯◯◯ | Mainly minor gastrointestinal complaints in both groups |
|
| 100–7,200 mg/d over 1–6 mo | Physical function, 1–3 mo | SMD (4 trials) = –3.99 | Very low ⊕◯◯◯ | Risk to experience any AE: vs placebo: no significant differences vs drug: insufficient data |
|
|||
| Stiffness, 1–3 mo | SMD (5 trials) = –1.93 | Low ⊕⊕◯◯ | ||||||
| Global function, 1–3 mo | SMD (5 trials) = –0.90 | Moderate ⊕⊕⊕◯ | ||||||
| vs other | 3/195† | Osteoarthritis | One low-quality study, with methodological flaws, compared boswellia with valdecoxib and reported statistically significant effects favoring boswellia. Two studies also reported on different boswellia extracts. | |||||
| *Studies (N = 6) combining boswellia with other ingredients were heterogeneous. Some combination products appeared to be more effective than placebo and as effective as glucosamine sulfate, whereas others reported no significant differences compared with celecoxib. | ||||||||
| Ginger*,‡ | vs placebo† | 6/741 | Osteoarthritis | Pain reduction | SMD (5 trials) = – 0.30, 7.5 pts greater reduction than placebo | Moderate ⊕⊕⊕◯ | Bad taste or various forms of stomach upset; none “serious” but some resulted in trial discontinuation |
|
| Capsule: 250–1,000 mg/d over 3–12 wk | Self-reported disability | SMD (4 trials) = –0.22 | Moderate ⊕⊕⊕◯ | Risk to experience any AE: vs placebo: 12% greater risk for someone to experience an AE following ginger (RD = 0.12, 95% CI = 0.02 to 0.23, P = 0.02, I2 = 49.00%) vs drug: insufficient data | ||||
| Ointment: 6 g/d over 6 wk | vs other† | 2/187 | Osteoarthritis | Two studies compared ginger with ibuprofen and reported mixed results. The higher the dose (e.g., 1,000 mg), the more likely a positive benefit for ginger only. | ||||
| *Studies combining ginger (N = 4) with other ingredients were heterogeneous. Overall, combination products showed positive benefit for reducing pain and possibly overall health/quality of life but not for improving function. | ||||||||
| Rose hip‡ | vs placebo | 4/395 | Osteoarthritis, rheumatoid arthritis | Self-reported pain reduction | SMD (3 trials) = 0.37; 9.25 pts greater reduction than placebo | Moderate ⊕⊕⊕◯ | Mild gastrointestinal discomfort in both groups |
|
| 5 g/d over 3–6 mo | Self-reported use of analgesics | SMD (3 trials) = 0.28 | Moderate ⊕⊕⊕◯ | Risk to experience any AE: vs placebo: insufficient data vs drug: insufficient data | ||||
| No. of responders | OR (3 trials) = 2.13 | Moderate ⊕⊕⊕◯ | ||||||
| SAMe§ | vs placebo† | 3/849 | Osteoarthritis (hip, knee, spine, hand), fibromyalgia | Pain | P < 0.05¶ (3 trials) | Insufficient data to determine the quality of evidence | Relatively mild, primarily gastrointestinal complaints |
|
| 400–1,200 mg/d over 10 d–3 mo | Physical function | P < 0.05¶ (1 trial) | Risk to experience any AE: vs placebo: insufficient data vs drug: 14% greater risk for someone to experience an AE following pharmacological drug administration (RD = –0.14, 95% CI = –0.21 to –0.06, P = 0.0007, I2 = 39.00%) | |||||
| Sleep | P < 0.05‖ (3 trials) | |||||||
| Global health | P < 0.05¶,‖ (2 trials) | |||||||
| Mood | NS (2 trials) | |||||||
| Medication use | NS (1 trial) | |||||||
| vs other† | 5/1,127 | Osteoarthritis (hip, knee, spine, hand) | Five studies showed that SAMe was as effective as NSAIDs in improving pain, function, and general health/function. One study reported improvement in mood. | |||||
AE = adverse event; CI = confidence interval; MSK = musculoskeletal; NS = nonsignificant; NSAID = nonsteroidal anti-inflammatory drug; OR = odds ratio; RD = risk difference; SAMe = s-adenosyl-L-methionine; SMD = standardized mean difference.
Includes data from multiple arms (placebo and other comparators).
Data from existing meta-analysis used.
No meta-analysis conducted.
Between-group differences.
Within-group differences.
Table 3.
Judgments across factors for decision-making
| Ingredient Total Votes in Favor/Total Possible Votes* | Effect Size for Pain Reduction/Quality | Certainty of the Evidence Across all Outcomes | Desirable Effects Outweigh Undesirable | Justification of Resource Requirements | Acceptable to Stakeholders | Feasible/Suitable to Implement | Decision |
|---|---|---|---|---|---|---|---|
| Boswellia† | SMD = –3.34 | 4 4 0 0 0 | 0 3 1 3 1 | 0 3 1 4 0 | 0 6 1 1 0 | 1 3 1 3 0 | 75% weak, in favor |
| 12/40 | Very low ⊕◯◯◯ | VL L NS M H | N PN DK PY Y | N PN DK PY Y | N PN DK PY Y | N PN DK PY Y | 25% none |
| In favor = 0 | In favor = 4 | In favor = 4 | In favor = 1 | In favor = 3 | |||
| Ginger‡ | SMD = –0.30 | 0 2 0 6 0 | 0 1 0 7 0 | 0 3 0 5 0 | 0 5 1 2 0 | 0 6 0 2 0 | 37.5% weak, in favor |
| 22/40 | Moderate ⊕⊕⊕◯ | VL L NS M H | N PN DK PY Y | N PN DK PY Y | N PN DK PY Y | N PN DK PY Y | none 37.5% |
| In favor = 6 | In favor = 7 | In favor = 5 | In favor = 2 | In favor = 2 | 25% weak, against | ||
| Rose hip | SMD = 0.37 | 0 2 0 6 0 | 0 0 2 5 1 | 0 3 1 4 0 | 0 6 1 1 0 | 0 6 1 1 0 | 25% weak, in favor |
| 18/40 | Moderate ⊕⊕⊕◯ | VL L NS M H | N PN DK PY Y | N PN DK PY Y | N PN DK PY Y | N PN DK PY Y | 37.5% none |
| In favor = 6 | In favor = 6 | In favor = 4 | In favor = 1 | In favor = 1 | 37.5% weak, against | ||
| SAMe | Insufficient data | 0 6 2 0 0 | 0 1 2 5 0 | 0 2 2 4 0 | 2 3 0 3 0 | 0 4 0 4 0 | 37.5% weak, in favor |
| 16/40 | VL L NS M H | N PN DK PY Y | N PN DK PY Y | N PN DK PY Y | N PN DK PY Y | 25% none | |
| In favor = 0 | In favor = 5 | In favor = 4 | In favor = 3 | In favor = 4 | 37.5% weak, against |
DK = do not know; H = high; L = low; M = moderate; N = no; NS = no included studies; PN = probably no; PY = probably yes; SAMe = s-adenoysl-L-methionine; VL = very low; Y = yes.
Eight voting members judged factors to consider together to develop recommendations. A summary weight is provided for each ingredient, ranking the desirable consequences to the unknown or undesirable consequences across factors. The quality was not assigned a weight, as this was used to determine the weight of the certainty of the evidence across all outcomes assessed, and as supplied by the evidence review independently (Supplementary Data). Although the accumulated judgments of all factors were used to inform the recommendations ultimately made and displayed using the GRADE Grid (Supplementary Data) visually, they were not assigned a weighted summary score.
Recommended as a high-priority research area, not as a dietary supplement, at this time.
Conditionally recommended use as a food source, not as a dietary supplement, at this time.
Question 1. Can Boswellia Effectively Mitigate Chronic MSK Pain and Related Symptoms?
Extracts derived from resins of Boswellia species have been historically used both in African countries and Ayurvedic medicine in India to treat multiple diseases [59,60]. Boswellia is currently widely available and used in complementary medicine, particularly for inflammatory conditions; its resin oil and extracts can also be found in soaps, cosmetics, foods, and beverages [60].
Summary of Findings
A 2014 Cochrane systematic review reported evidence for various oral herbal therapies, including boswellia, for osteoarthritis; it revealed moderate-quality evidence for “trends of benefit” that warranted further investigation [61]. Following the 2014 review, Kessler et al. [62] reported in 2015 that boswellia was statistically more effective than placebo for improving pain and function, but that the statistically significant effects disappeared when only trials using the American College of Rheumatology diagnostic criteria were used. Inclusive of the studies captured in these recent reviews, 11 trials met the eligibility criteria and were included for this evidence evaluation to inform decision-making [25–35].
Included boswellia ingredients were labeled as aflapin [25,26], 5-loxin [25,27], Boswellia serrata extract [28,29], B. serrata extract combined with curcuma [30,33], methylsulfonylmethane [32,35], amlaki [34], and other dietary ingredients [31,32]. Boswellia was compared with placebo [25–28,30,31,35], NSAIDs [29,33,34], other dietary ingredients [32,34], and/or other types [25] or doses [27] of boswellia within osteoarthritis, primarily knee osteoarthritis, populations. Daily doses ranged from 100 to 7,200 mg/d over one to six months; however, one study [31] did not report the dose. All studies reported on pain and physical function, with few reporting on global function outcomes or medication use. No studies reported on health-related quality of life, sleep, mood, stress, or behavioral or resource use outcomes.
Six trials were included in the meta-analysis; two compared different types of boswellia extracts with placebo. Specifically, Sengupta et al. 2008 [27] compared low and high doses of 5-loxin and Sengupta et al. 2010 [25] compared alfapin and 5-loxin. This likely contributed to the large degree of heterogeneity and inconsistencies, which resulted in HERB members downgrading. Although the studies were directly related to the research question, the members downgraded for imprecision due to the overall small sample sizes being pooled in the analysis. The risk of bias associated with these studies appeared to be minimal; however, it was noted that some of the studies reported receiving funding from the same source that provided the ingredients for evaluation. The overall certainty of the evidence was judged to be very low to low.
Desirable vs Undesirable Effects
The meta-analysis showed very low-quality evidence for a large and statistically significant improvement in pain (six trials, N = 259 participants, standardized mean difference [SMD] = –3.34, 95% confidence interval [CI] = –4.86 to –1.82, P < 0.0001, I2 = 94.00%) and physical function (four trials, N = 183 participants, SMD = –3.99, 95% CI = –6.37 to –1.61, P < 0.001, I2 = 96.00%) compared with placebo. There is low- and moderate-quality evidence for a reduction in stiffness (Western Ontario and McMaster Universities Osteoarthritis Index subscale) and global function (five trials, N = 229 participants, Lequesne’s Functional Index), respectively. This evidence was based only on osteoarthritis populations. Further, studies that either combined boswellia with other ingredients or included other active comparators were quite heterogeneous. Although the noted effects were substantial across these outcomes, the desirable anticipated effects were judged by the members to be moderate to large.
All studies reported a similar number of adverse events—mainly gastrointestinal complaints—in both groups (Supplementary Data). No significant differences were noted between the boswellia and placebo groups; data comparing boswellia and pharmacological drug interventions were insufficient to analyze differences in the risk of experiencing any adverse event between groups. Members judged these undesirable effects as small to trivial. Members were divided about the balance between desirable/undesirable effects, given that the overall certainty of the evidence was very low to low.
Resource Requirements/Cost
A bottle of 100 capsules with 500 mg of boswellia extract costs anywhere from $10 to $20 depending on the brand. Because boswellia doses ranged from 100 to 7,200 mg across studies and boswellia was sometimes combined with other ingredients, members had divergent opinions about its required resources and whether resources were justified, given the uncertainty of the evidence and the desirable anticipated effects.
Other Considerations: Feasibility, Acceptability, Suitability, Values
The majority of members agreed that given the current quality of the evidence, boswellia did not warrant out-of-pocket costs and was not acceptable for implementation at this time. Feasibility was also an issue, with divergent opinions regarding the formulation of boswellia and its active ingredients.
Recommendations
The desirable anticipated effects reported in studies to date are substantial; however, the certainty of this evidence is questionable. Consequently, boswellia was recommended as a high-priority research area in need of study but was not recommended for use until more and higher-quality research could be produced, to include addressing strict reporting criteria, purity of the ingredients, bioavailability and dose requirements in larger clinical trials, and involving participants experiencing chronic MSK pain [14].
Question 2. Can Ginger Effectively Mitigate Chronic MSK Pain and Related Symptoms?
Ginger is a tropical plant widely used as a flavoring or fragrance in foods, beverages, soaps, and cosmetics [63]. It has been used to treat nausea and MSK-related pain [64]. Common forms of ginger include the fresh or dried root, tablets, capsules, liquid extracts, and teas.
Summary of Findings
In 2015, Bartels et al. [46] published a systematic review with meta-analysis across five trials (593 participants) and concluded that ginger compared with placebo was modestly efficacious and reasonably safe for the treatment of osteoarthritis. Significant reductions were shown for both pain and disability outcomes. The authors identified 10 randomized controlled trials (RCTs), including those evaluated by Bartels et al. [46], on ginger across chronic MSK populations. Studies assessed a variety of populations, including those with knee osteoarthritis [36–40], knee and hip osteoarthritis [41–43], rheumatoid arthritis [44], and chronic joint pain [45]. Ingredients were Zingiber officinale [36,42], Eurovita extract 33 [41], Zingiberis rhizoma [39], and EV Ext 77 [37], or dried, powdered ginger [38]. Different extracts of ginger were also combined (i.e., referred to as “ginger-plus” studies) with mastic and sesame oil [40], Zinaxin glucosamine [43,45], purified extracts of various plants [44], or multiple dietary ingredients [45]. Daily doses ranged from 250 to 1,000 mg/d (delivered as a capsule) and 6 g/d (delivered as an ointment) over three to 12 weeks. Ginger was compared with herbal [44], oral [43,44], and topical [40] pharmacologic interventions, or placebo capsules that were either undescribed [38,41,42] or contained maltodextrin [39], starch [36], coconut oil [37], or magnesium stearate [45]. Studies reported on outcomes including pain (N = 10), physical (N = 7) and global (N = 4) function, health-related quality of life (N = 3), and medication use (N = 1).
Outcome data were insufficient, other than pain and function to pool into a new meta-analysis (Supplementary Data: Summary Report). Therefore, the authors incorporated the evidence reported in the Bartels et al. [46] analyses into the GRADE framework [21]. Risk of bias was rated as high across studies. Whereas heterogeneity was not statistically significant compared with placebo, the authors downgraded for imprecision due to the overall small sample sizes. The members judged the overall certainty of the evidence to be moderate.
Desirable vs Undesirable Effects
The meta-analysis of five trials (593 participants) showed moderate-quality evidence for a statistically significant reduction in pain as compared with placebo (SMD = –0.30, 95% CI = –0.50 to –0.09, P = 0.005, I2 = 27%). The meta-analysis of four trials (513 participants) showed moderate-quality evidence for a statistically significant reduction in disability as compared with placebo (SMD = –0.22, 95% CI = –0.39 to –0.04, P = 0.01, I2 = 0.00%). The evidence comparing ginger with other active comparators and other conditions beyond osteoarthritis is limited. The members judged these desirable anticipated effects to be small.
Most studies reported adverse events, mainly citing gastrointestinal complaints, and none were classified as “serious” or causing lasting harm; some adverse events, however, did cause selected participants to discontinue the trial, as reported by Bartels et al. [46]. Compared with placebo, a 12% greater risk of experiencing an adverse event was noted following ginger (risk difference [RD] = 0.12, 95% CI = 0.02 to 0.23, P = 0.02, I2 = 49.00%) (Supplementary Data: Summary Report). However, adverse events appeared less frequent in ginger when compared with active controls, particularly ibuprofen (Supplementary Data: Summary Report). The HERB members judged these undesirable anticipated effects to be relatively small. Overall, the desirable effects probably outweigh the undesirable effects, and the certainty of this evidence overall appears to be moderate.
Resource Requirements/Cost
A bottle of 100 capsules with 550 mg of ginger on average costs anywhere from $5 to $10 depending on the brand, equating to much less than $1/d. Members judged these costs to be negligible or perhaps a moderate savings in some cases. Most members agreed that the cost would justify its use.
Other Considerations: Feasibility, Acceptability, Suitability
The majority of members questioned the feasibility, acceptability, and suitability of administering ginger as a dietary supplement for chronic MSK pain. Ginger is available in food, however, and could be incorporated into a nutrition planning checklist with proper nutritional education for trainers, dietitians, and Special Operators. Understanding and considering the operational environment and ingredient availability could help develop a long-term preventive plan rather than one solely focused on meeting caloric requirements.
Recommendations
Ginger is associated with minimal adverse events, and the desirable anticipated effects appear small, with moderate evidence. Because it is already available in tea/food, there would be no additional risk in obtaining ginger via food sources. Ginger could serve as a preventive nutritional agent if incorporated into the mission-planning process. Further research involving larger trials is required before definitive recommendations regarding use can be made. Research priorities include conducting more rigorously designed studies, exploring the optimal dose response of ginger as a dietary supplement, examining both pain and pain-related outcomes, and comparing ginger with other active ingredients.
Question 3. Can Rose Hip Effectively Mitigate Chronic MSK Pain and Related Symptoms?
Rose hips are the berry fruits of the dog rose or wild briar rose (Rosa canina L.), a scrambling rose species native to Europe, northwest Africa, and western Asia. Because rose hips contain a large amount of vitamin C, they have similar uses, including preventing and treating colds, flu and vitamin C deficiencies, and treating and preventing stomach disorders. They are often used in tea, jam, and soup, in both food and manufactured forms [65].
Summary of Findings
A high-quality 2008 systematic review [51] including three primary studies [48–50] reported that rose hip powder significantly reduced pain and rescue medication use in osteoarthritis patients. A 2010 study reported that rheumatoid arthritis patients may also benefit from rose hip powder [47]. Daily doses of rose hip powder were consistently reported at 5 g across all studies, though study duration ranged from three to six months. All studies compared the effect of rose hips with placebo and reported on pain, physical function, and medication use, as well as health-related quality of life (N = 2), global health (N = 2), sleep (N = 1), and mood (N = 1) outcomes (Supplementary Data: Summary Report).
Studies comparing rose hip with placebo had insufficient data on outcomes, other than pain and medication usage, to pool into a meta-analysis. Therefore, the authors incorporated the evidence reported in Christensen et al.’s [51] analyses into the GRADE framework. The risk of bias associated with these four studies was minimal. While the heterogeneity of the outcomes pooled was not a significant concern, the authors did downgrade for imprecision due to small sample sizes. The members judged the overall certainty of the evidence to be moderate.
Desirable vs Undesirable Effects
The meta-analysis of three trials (306 participants) showed moderate-quality evidence for a statistically significant reduction in pain (SMD = 0.37, 95% CI = 0.13 to 0.60, P = 0.0019, I2 = 0.00%) and the use of rescue medication compared with placebo (SMD = 0.28, 95% CI = 0.05 to 0.51, I2 = 0.00%). In addition, a patient allocated to rose hip was more than twice as likely to respond to therapy compared with placebo (odds ratio = 2.19, 95% CI = 1.38 to 3.48) [51]. Studies tended to show improvements in physical function, health-related quality of life, mood, sleep, and global health. Based upon this evidence, the members judged the desirable anticipated effects to be small to moderate.
Most studies reported on adverse events, with gastrointestinal complaints being the primary ones in both the rose hips and control groups (Supplementary Data: Summary Report). Data were insufficient to allow for pooling a risk difference for any comparators assessed. The members judged the undesirable effects to be trivial to small. The majority agreed that the desirable effects outweigh the undesirable.
Resource Requirements/Cost
A bottle of 100 capsules with 550 mg of rose hips costs anywhere from $5 to $10 depending on the brand. Based on the evaluated evidence, daily doses would consist of 10 (to achieve 5 g) capsules per day, a similar cost to that of ibuprofen 2,400 mg (i.e., $1/d). Although the HERB members agreed that the cost/savings would be negligible, there were divergent opinions regarding whether costs were justified.
Other Considerations: Feasibility, Acceptability, Suitability
There was concern about overall compliance with this ingredient given the large number of capsules required daily. Powder formulations should be taken with small amounts of liquid to avoid gastrointestinal complaints [66]. The members were unaware if rose hips could be formulated in a higher concentration to avoid the number of capsules required daily and whether that would affect the degree to which one may experience an adverse event. As such, most members voted that it would probably not be feasible, acceptable, or suitable for use among Special Operators in its current form as described in the literature.
Recommendations
Although moderate-quality evidence suggests that the desirable anticipated effects appear to outweigh the undesirable effects, various caveats precluded the members from making any definitive recommendations. Further research would be required to understand the formulation of rose hips and whether the suggested administered dose could be safely increased to decrease the burden of taking up to 10 capsules per day. Additionally, if the formulary were to be adjusted to increase compliance, larger trials would be required to enhance confidence in the estimate of the adjusted formulation’s effect. Trials with other active ingredient comparators across other pain-related outcomes would also be necessary, as none were identified through this effort (Supplementary Data: Summary Report).
Question 4. Can SAMe Effectively Mitigate Chronic MSK Pain and Related Symptoms?
SAMe is naturally formed in the body from homocysteine and 5-methylene tetrahydrofolate. It is a primary methyl group donor and contributes to the synthesis, activation, and/or metabolism of hormones, neurotransmitters, nucleic acids, proteins, phospholipids, and various drugs [67–69]. Taken orally, it has been used for several conditions, including depression, anxiety, and MSK pain [70].
Summary of Findings
In 2009, Rutjes et al. [71] published a systematic review evaluating the effects of SAMe on pain and function in knee and hip osteoarthritis populations involving four trials (656 patients). Results were inconclusive, and most of the studies assessed were small and of questionable methodological quality; the authors described the need for more research to understand SAMe and explain that although its effects on pain and function were likely to be small, they may still be clinically relevant. Seven RCTs, including the trials reported in Rutjes et al. [71], have been published comparing the effect of SAMe with either an NSAID [52,54,56–58] or placebo [53,55,56] across various MSK pain populations (fibromyalgia [53], knee [52,54–58], and/or hip [54,56], spine [56], and hand [56] osteoarthritis). Although oral and intravenous doses of SAMe ranged from 400 to 1,200 mg/d over 10 days to three months, oral doses were consistently 1,200 mg daily. Study outcomes included pain (N = 7), physical function (N = 7), global function/health (N = 6), mood (N = 3), medication use (N = 3), health-related quality of life (N = 1), sleep (N = 1), and behavioral effects (N = 1).
Meta-analysis was not feasible due to either the heterogeneity of outcomes/measures or missing data in the studies evaluated. Risk of bias was rated as high across two of the seven trials evaluated. Sample sizes comparing SAMe with placebo were small, and studies with drug comparators were wide ranging. The overall certainty of the evidence was judged to be low.
Desirable vs Undesirable Effects
Three trials comparing SAMe with placebo revealed significant between-group differences in pain, sleep, and overall global health, across both osteoarthritis [55,56] and fibromyalgia [53] patients. Based on five studies [52,54,56–58], SAMe appears to be as effective as other selected drugs (i.e., celecoxib, piroxicam, ibuprofen, naproxen, nabumetone). The HERB members judged these desirable anticipated effects to be moderate overall.
Reported adverse events were relatively mild and primarily consisted of gastrointestinal complaints. Analysis revealed a 14% greater risk for patients experiencing an adverse event following pharmacological drug administration compared with SAMe (RD = –0.14, 95% CI = –0.21 to –0.06, P = 0.0007, I2 = 39.00%) (Supplementary Data: Summary Report). HERB members judged these undesirable anticipated effects to be relatively trivial to small. Overall, the desirable effects probably outweighed the undesirable effects, but the certainty of the evidence was still low with no meta-analysis to rely upon.
Resource Requirements/Cost
Based on the range of doses in the reviewed studies (i.e., 400 to 1,200 mg/d), the cost of SAMe equates to ∼<$1 per day. Members judged these costs to be negligible, and some agreed that these costs could be justified given the desirable/undesirable effects.
Other Considerations: Feasibility, Acceptability, Suitability
Divergent opinions were expressed regarding the feasibility, acceptability, and suitability for use of SAMe, given the low quality and certainty of the evidence.
Recommendations
Although SAMe is associated with minimal adverse effects, the quality and certainty of the evidence remain low. Subsequently, no recommendations were made for the use of SAMe for pain and related symptoms. Research priorities include determining the specific efficacy of SAMe, compared with placebo, for pain and other patient-related outcomes in the MSK population, conducting dose studies to understand the specific formulations and preparations likely to produce an effect beyond that of placebo and comparing SAMe with other drug therapies in larger and multisite studies.
Discussion
No recommendations were made for the use of SAMe, ginger (as a supplement), rose hips, or boswellia as dietary supplements to alleviate chronic MSK pain, either because the quality of the evidence was too low or trade-offs were so closely balanced that any recommendation was judged to be overly speculative. However, the methodological steps taken allowed for transparency into the deficiencies of specific factors judged for decision-making and recommendations for next research steps.
Limitations in reviewing the evidence include the paucity in the number of RCTs and number of participants included in the trials. To include a trial’s evidence into a meta-analysis, data must be presented in the publication, and outcomes and comparators must be similar enough to pool. For a two-sample pooled t test with a statistical significance level of 0.05, a total sample size of 394 participants in each group would be required to obtain a power of at least 80.0%. The confidence in the estimate of the effect across outcomes assessed was, in most cases, downgraded due to inadequate sample sizes.
Another limiting factor is poor reporting in these trials, which leads to potential risk of bias and/or not understanding the context and setting well enough to generalize results across other populations of interest. Adhering to the suggested Standards for Reporting Interventions in Controlled Trials Essential to Nutritional Elements (STRICT-NE) [14] is also critical for these types of studies; this means a careful description of the preparation/treatment (e.g., formulation, preparer/supplier) of the dietary ingredient(s), analysis of baseline diet and whether diet was controlled during the experiment, and documentation of a quantitative analysis of the actual contents of the treatment provided to the participants. Such actions should be required when research is to be translated into actionable recommendations and decisions made for safe use of dietary ingredients. This currently is neither transparently nor consistently documented in the research published to date, which greatly limits the generalizability and utility for the end user.
Although some dietary ingredients had moderate evidence, the desirable anticipated effects were judged to be small in nature. Whether combination products and combining safe products could enhance a desirable anticipated effect for the participant should be open for discussion [14]. To date, several studies have used combination products and evaluated the evidence (Supplementary Data: Summary Report); however, heterogeneity precludes drawing any conclusions based on these study results.
In 2012, Stam et al. [72] published a mixed treatment comparison on the efficacy of several NSAIDs in the treatment of osteoarthritis and reported that the effect size for a reduction in pain relative to placebo was –0.41 (95% CI = –0.63 to –0.18) for 2,400 mg of ibuprofen. HERB used this dose as an anecdotal reference standard for “small to moderate” effect size according to Cohen’s d and similar to that of ginger and rose hip (noted in Table 2) as compared with placebo, although the confidence in this effect estimate was not large. More robust trials with evidence for efficacy of an ingredient compared with placebo and comparing dietary ingredients with a standard NSAID would help in the decision-making process. To date, studies of this nature are scant and do not evaluate all pain-related outcomes required for decision-making. Adverse events appear to be minor in nature across the evaluated ingredients. Given the current opioid crisis [73] and the need for better and alternative approaches to address the unknown complexity of pain, more rigorous research involving larger trials and considering the decision factors during initial trial design is required to produce impactful results that those in need can use as decision-making aids. Interestingly, when the National Institutes of Health Office of Dietary Supplement’s Dietary Supplement Label Database (https://www.dsld.nlm.nih.gov/dsld/index.jsp, accessed March 18, 2018.) was searched for products with the ingredients noted above and a label claim including the terms “muscle” and “pain,” 15 products were found with ginger, 21 with boswellia, and two with both boswellia and ginger. No products were found for rose hips or SAMe. When only the term “pain” and the ingredients were included, 151, 12, 50, and five were found for ginger, rose hips, boswellia, and SAMe, respectively. Thus, despite the limited evidence, manufacturers promote these ingredients, and claims are being made to support the use of these ingredients for improving pain. If someone wanted to purchase such products, we would urge them to only select those that have been either verified or certified by the United States Pharmacopeia or NSF, respectfully, to ensure that the contents are consistent with the label and the product has been prepared according to Food and Drug Administration (FDA) regulations.
Conclusions
The methodological processes and steps taken allowed for transparent and evidence-based recommendations to be made to inform policy decisions regarding the use of dietary ingredients for chronic MSK pain and other related symptoms. Whereas no recommendations were made for use of SAMe, ginger, boswellia, or rose hips as dietary supplements, the factors required to move the evidence toward better decisions are transparently documented. Stakeholders can use this evidence gained and factors considered as a decision aid, and when determining directions for the next steps in research. As noted in the second paper within this series, dietary ingredients are not intended to treat any particular health condition, and as MSK pain is a clinical condition, any ingredient or combination of ingredients would be required to go through the FDA Investigational New Drug Applications process.
Supplementary Material
Acknowledgments
The authors would like to acknowledge Lynn Teo, Charmagne F. Paat, Karin Meissner, and Cindy Lentino for their contributions to the systematic review and meta-analysis effort that informed the recommendations made.
The Holistic Evidence Review Board (HERB) consisted of the following individuals: Dr. Kevin Berry, Vice President, TLI Foundation; Dr. Robert Bonakdar, Academy of Integrative Pain Management and Director of Pain Management, Scripps Center for Integrative Medicine; SGM F. Bowling, Office of the Command Surgeon, US Special Operations Command and US Army Special Forces Medic; Dr. Patricia A. Deuster, Director of the Consortium for Health and Military Performance at the Uniformed Services University (CHAMP/USU); CAPT Scott Cota, Command Surgeon, US Special Operations Command; Dr. Rebecca Costello, Scientific Consultant, Office of Dietary Supplements, National Institutes of Health; Dr. Tonya Dodge, Associate Professor of Psychology, George Washington University; Dr. C. Douglas Forcino, Director of the US Special Operations Command Programs at CHAMP/USUHS; Dr. Travis Harvey, Program Development Manager, US Special Operations Command, Preservation of the Force and Family, Human Performance; COL (ret.) Jeffery Johnson, 88th Pharmacy Flight Commander AFMC/TeamRx Consultant 88th DTS/88th MDG/88th MDG/88th ABW/WPAFB and member of the Air Force Nutrition and Supplements Subcommittee; COL (ret.) Steven Swann, Independent Military Medicine Consultant and former Command Surgeon, US Special Operations Command; CAPT Necia Williams, Anesthesiologist and Command Surgeon, US Marine Corps Special Operations Command.
Funding sources: Funding for this work was provided by the Preservation of the Force and Family Behavioral Health Program, Uniformed Services University (award number HU0001-15-2-0053).
Disclosure: The opinions or assertions contained herein are the collective views of the authors and the Holistic Evidence Review Board and are not to be construed as official or as reflecting the views of the Uniformed Services University, US Special Operations Command, or the Department of Defense.
Conflicts of interest: No conflicts of interest existed at the time of the project for any authors or steering committee members making evidence-based recommendations.
Supplementary Data
Supplementary data are available at Pain Medicine online.
References
- 1. Armed Forces Health Surveillance Center. Absolute and relative morbidity burdens attributable to various illnesses and injuries, U.S. Armed Forces, 2013. MSMR 2014;21(4):2–7. [PubMed] [Google Scholar]
- 2. Bullock S, Jones B, Gilchrist J, Marshall S.. Prevention of physical training-related injuries recommendations for the military and other active populations based on expedited systematic reviews. Am J Prev Med 2010;38(Suppl 1):S156–81. [DOI] [PubMed] [Google Scholar]
- 3. Hauret K, Jones B, Bullock S, Canham-Chervak M, Canada S.. Musculoskeletal injuries description of an under-recognized injury problem among military personnel. Am J Prev Med 2010;38(Suppl 1):S61–70. [DOI] [PubMed] [Google Scholar]
- 4. Institute of Medicine. Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education and Research. Washington, DC: The National Academies Press; 2011. [PubMed] [Google Scholar]
- 5. Pain Management Task Force Report. Office of the Army Surgeon General: Pain Management Task Force; 2010. http://www.dvcipm.org/clinical-resources/pain-management-task-force/ (accessed March 18, 2019).
- 6. Knapik J, Steelman R, Hoedebecke S, et al. A systematic review and meta-analysis on the prevalence of dietary supplement use by military personnel. BMC Complement Altern Med 2014;14:143. doi: 10.1186/1472-6882-14-143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Council for Responsible Nutrition. CRN 2016 Annual Survey on Dietary Supplements. Available at: https://www.crnusa.org/resources/crn-2016-annual-survey-dietary-supplements (accessed March 18, 2018).
- 8. Buckenmaier C, Crawford C, Lee C, Schoomaker E.. Are active self-care complementary and integrative therapies effective for management of chronic pain? A rapid evidence assessment of the literature and recommendations for the field. Pain Med 2014;15(1):S1–113.24734855 [Google Scholar]
- 9. Complementary Medicine Research. Journal Club. Complement Med Res 2017;24:207–13. [Google Scholar]
- 10. De Silva V, El-Metwally A, Ernst E, Lewith G, Macfarlane GJ.. Evidence for the efficacy of complementary and alternative medicines in the management of osteoarthritis: A systematic review. Rheumatology (Oxford) 2011;50(5):911–20. [DOI] [PubMed] [Google Scholar]
- 11. National Academies of Sciences. Pain Management and Opioid Epidemic: Balancing Societal and Individual Benefits and Risks of Prescription Opioid Use. Washington, DC: The National Academies Press; 2017. [PubMed] [Google Scholar]
- 12. Cota S, Williams N, Neff R, Deuster P.. How Evidence-Based Recommendations May Direct Policy Decisions Regarding Appropriate Selection and Use of Dietary Ingredients for Improving Pain. Pain Med 2019;20(6):1063–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Boyd C, Crawford C, Berry K, Deuster P; HERB Working Group. Conditional Recommendations for Specific Dietary Ingredients as an Approach to Chronic Musculoskeletal Pain: Evidence-Based Decision Aid for Healthcare Providers, Participants and Policy Makers. Pain Med. 2019;20(7):1430–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Crawford C, Boyd C, Paat C, et al. Dietary Ingredients as an Alternative Approach for Mitigating Chronic Musculoskeletal Pain: Evidence-based Recommendations for Practice and Research in the Military. Pain Med 2019;20(6):1236–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Institute of Medicine. Clinical Practice Guidelines We Can Trust. Washington, DC: The National Academies Press; 2011. [Google Scholar]
- 16. Deyo R, Dworkin S, Amtmann D, et al. Report of the Task Force on Research Standards for chronic low-back pain. Phys Ther 2015;95(2):e1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Centers for Disease Control and Prevention. The National Institute for Occupational Safety and Health (NIOSH) Musculoskeletal Health Program. Available at: https://www.cdc.gov/niosh/programs/msd/default.html (accessed March 18, 2018).
- 18. Cleveland Clinic. Musculoskeletal pain. Available at: http://my.clevelandclinic.org/health/articles/musculoskeletal-pain (accessed March 18, 2018).
- 19. United States Special Operations Command. Policy memorandum 16-29: Policy on performance enhancing substance use for Special Operations Forces. United States Special Operations Command. September 27, 2016.
- 20. Office of Dietary Supplements. Available at: www.ods.od.nih.gov.
- 21. GRADE Working Group. Grading of Recommendations Assessment, Development and Evaluation (GRADE). Available at: http://www.gradeworkinggroup.org/ (accessed March 18, 2018).
- 22. Coulter I, Adams A.. Consensus methods, clinical guidelines, and the RAND study of chiropractic. Aca J Chiropr 1992;60–1. https://www.rand.org/pubs/external_publications/EP19920003.html (accessed March 18, 2019). [Google Scholar]
- 23. Coulter I, Shekelle P, Mootz R, Hansen D.. The Use of Expert Panel Results: The RAND Panel for Appropriateness of Manipulation and Mobilization of the Cervical Spine. Santa Monica, CA: RAND; 1997. [Google Scholar]
- 24. Jaeschke R, Guyatt G, Dellinger P, et al. Use of GRADE grid to reach decisions on clinical practice guidelines when consensus is elusive. BMJ 2008;337:a744.. [DOI] [PubMed] [Google Scholar]
- 25. Sengupta K, Krishnaraju AV, Vishal AA, et al. Comparative efficacy and tolerability of 5-loxin and aflapin against osteoarthritis of the knee: A double blind, randomized, placebo controlled clinical study. Int J Med Sci 2010;7(6):366–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Vishal AA, Mishra A, Raychaudhuri SP.. A double blind, randomized, placebo controlled clinical study evaluates the early efficacy of aflapin in subjects with osteoarthritis of knee. Int J Med Sci 2011;8(7):615–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Sengupta K, Alluri KV, Satish AR, et al. A double blind, randomized, placebo controlled study of the efficacy and safety of 5-loxin for treatment of osteoarthritis of the knee. Arthritis Res Ther 2008;10(4):R85. doi: 10.1186/ar2461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Kimmatkar N, Thawani V, Hingorani L, Khiyani R.. Efficacy and tolerability of Boswellia serrata extract in treatment of osteoarthritis of knee—a randomized double blind placebo controlled trial. Phytomedicine 2003;10(1):3–7. [DOI] [PubMed] [Google Scholar]
- 29. Sontakke STV, Pimpalkhute S, Kabra P, Babhulkar S, Hingorani L.. Open, randomized, controlled clinical trial of Boswellia serrata extract as compared to valdecoxib in osteoarthritis of knee. Indian J Pharmacol 2007;39:27–9. [Google Scholar]
- 30. Badria FA, El-Farahaty T, Shabana AA, Hawas SA, El-Batoty MF.. Boswellia-curcumin preparation for treating knee osteoarthritis: A clinical evaluation. Altern Complement Ther 2002;8(6):341–8. [Google Scholar]
- 31. Kulkarni RR, Patki PS, Jog VP, Gandage SG, Patwardhan B.. Treatment of osteoarthritis with a herbomineral formulation: A double-blind, placebo-controlled, cross-over study. J Ethnopharmacol 1991;33(1–2):91–5. [DOI] [PubMed] [Google Scholar]
- 32. Notarnicola A, Maccagnano G, Moretti L, et al. Methylsulfonylmethane and boswellic acids versus glucosamine sulfate in the treatment of knee arthritis: Randomized trial. Int J Immunopathol Pharmacol 2016;29(1):140–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Kizhakkedath R. Clinical evaluation of a formulation containing curcuma longa and Boswellia serrata extracts in the management of knee osteoarthritis. Mol Med Rep 2013;8(5):1542–8. [DOI] [PubMed] [Google Scholar]
- 34. Chopra A, Saluja M, Tillu G, et al. Ayurvedic medicine offers a good alternative to glucosamine and celecoxib in the treatment of symptomatic knee osteoarthritis: A randomized, double-blind, controlled equivalence drug trial. Rheumatology (Oxford) 2013;52(8):1408–17. [DOI] [PubMed] [Google Scholar]
- 35. Notarnicola A, Tafuri S, Fusaro L, et al. The “MESACA” study: Methylsulfonylmethane and boswellic acids in the treatment of gonarthrosis. Adv Ther 2011;28(10):894–906. [DOI] [PubMed] [Google Scholar]
- 36. Zakeri Z, Izadi S, Bari Z, et al. Evaluating the effects of ginger extract on knee pain, stiffness and difficulty in patients with knee osteoarthritis. J Med Plant Res 2011;5(15):3375–9. [Google Scholar]
- 37. Altman RD, Marcussen KC.. Effects of a ginger extract on knee pain in patients with osteoarthritis. Arthritis Rheum 2001;44(11):2531–8. [DOI] [PubMed] [Google Scholar]
- 38. Niempoog S, Pawa KK, Amatyakul C.. The efficacy of powdered ginger in osteoarthritis of the knee. J Med Assoc Thai 2012;95(Suppl 1): S59–64. [PubMed] [Google Scholar]
- 39. Wigler I, Grotto I, Caspi D, Yaron M.. The effects of Zintona EC (a ginger extract) on symptomatic gonarthritis. Osteoarthritis Cartilage 2003;11(11):783–9. [DOI] [PubMed] [Google Scholar]
- 40. Zahmatkash M, Vafaeenasab MR.. Comparing analgesic effects of a topical herbal mixed medicine with salicylate in patients with knee osteoarthritis. Pak J Biol Sci 2011;14(13):715–9. [DOI] [PubMed] [Google Scholar]
- 41. Bliddal H, Rosetzsky A, Schlichting P, et al. A randomized, placebo-controlled, cross-over study of ginger extracts and ibuprofen in osteoarthritis. Osteoarthritis Cartilage 2000;8(1):9–12. [DOI] [PubMed] [Google Scholar]
- 42. Haghighi M, Khalvat A, Toliat T, Jallaei S.. Comparing the effects of ginger (Zingiber officinale) extract and ibuprofen on patients with osteoarthritis. Arch Iran Med 2005;8(4):267–71. [Google Scholar]
- 43. Drozdov VN, Kim VA, Tkachenko EV, Varvanina GG.. Influence of a specific ginger combination on gastropathy conditions in patients with osteoarthritis of the knee or hip. J Altern Complement Med 2012;18(6):583–8. [DOI] [PubMed] [Google Scholar]
- 44. Chopra A, Saluja M, Tillu G, et al. Comparable efficacy of standardized ayurveda formulation and hydroxychloroquine sulfate (HCQS) in the treatment of rheumatoid arthritis (RA): A randomized investigator-blind controlled study. Clin Rheumatol 2012;31(2):259–69. [DOI] [PubMed] [Google Scholar]
- 45. Nieman DC, Shanely RA, Luo B, et al. A commercialized dietary supplement alleviates joint pain in community adults: A double-blind, placebo-controlled community trial. Nutr J 2013;12(1):154. doi: 10.1186/1475-2891-12-154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Bartels EM, Folmer VN, Bliddal H, et al. Efficacy and safety of ginger in osteoarthritis patients: A meta-analysis of randomized placebo-controlled trials. Osteoarthritis Cartilage 2015;23(1):13–21. [DOI] [PubMed] [Google Scholar]
- 47. Willich SN, Rossnagel K, Roll S, et al. Rose hip herbal remedy in patients with rheumatoid arthritis—a randomised controlled trial. Phytomedicine 2010;17(2):87–93. [DOI] [PubMed] [Google Scholar]
- 48. Winther K, Apel K, Thamsborg G.. A powder made from seeds and shells of a rose-hip subspecies (Rosa canina) reduces symptoms of knee and hip osteoarthritis: A randomized, double-blind, placebo-controlled clinical trial. Scand J Rheumatol 2005;34(4):302–8. [DOI] [PubMed] [Google Scholar]
- 49. Warholm O, Skaar S, Hedman E, Mølmen HM, Eik L.. The effects of a standardized herbal remedy made from a subtype of Rosa canina in patients with osteoarthritis: A double-blind, randomized, placebo-controlled clinical trial. Curr Ther Res Clin Exp 2003;64(1):21–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Rein E, Kharazmi A, Winther K.. A herbal remedy, Hyben Vital (stand. powder of a subspecies of Rosa canina fruits), reduces pain and improves general wellbeing in patients with osteoarthritis—a double-blind, placebo-controlled, randomised trial. Phytomedicine 2004;11(5):383–91. [DOI] [PubMed] [Google Scholar]
- 51. Christensen R, Bartels EM, Altman RD, Astrup A, Bliddal H.. Does the rose hip powder of Rosa canina (rosehip) reduce pain in osteoarthritis patients? A meta-analysis of randomized controlled trials. Osteoarthritis Cartilage 2008;16(9):965–72. [DOI] [PubMed] [Google Scholar]
- 52. Najm WI, Reinsch S, Hoehler F, Tobis JS, Harvey PW.. S-adenosyl methionine (SAMe) versus celecoxib for the treatment of osteoarthritis symptoms: A double-blind cross-over trial. BMC Musculoskelet Disord 2004;5:6. doi: 10.1186/1471-2474-5-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Volkmann H, Norregaard J, Jacobsen S, et al. Double-blind, placebo-controlled cross-over study of intravenous s-adenosyl-l-methionine in patients with fibromyalgia. Scand J Rheumatol 1997;26(3):206–11. [DOI] [PubMed] [Google Scholar]
- 54. Glorioso S, Todesco S, Mazzi A, et al. Double-blind multicentre study of the activity of s-adenosylmethionine in hip and knee osteoarthritis. Int J Clin Pharmacol Res 1985;5(1):39–49. [PubMed] [Google Scholar]
- 55. Bradley JD, Flusser D, Katz BP, et al. A randomized, double blind, placebo controlled trial of intravenous loading with s-adenosylmethionine (SAM) followed by oral SAM therapy in patients with knee osteoarthritis. J Rheumatol 1994;21(5):905–11. [PubMed] [Google Scholar]
- 56. Caruso I, Pietrogrande V.. Italian double-blind multicenter study comparing s-adenosylmethionine, naproxen, and placebo in the treatment of degenerative joint disease. Am J Med 1987;83(5a):66–71. [DOI] [PubMed] [Google Scholar]
- 57. Kim J, Lee EY, Koh EM, et al. Comparative clinical trial of s-adenosylmethionine versus nabumetone for the treatment of knee osteoarthritis: An 8-week, multicenter, randomized, double-blind, double-dummy, phase IV study in Korean patients. Clin Ther 2009;31(12):2860–72. [DOI] [PubMed] [Google Scholar]
- 58. Maccagno A, Di Giorgio EE, Caston OL, Sagasta CL.. Double-blind controlled clinical trial of oral s-adenosylmethionine versus piroxicam in knee osteoarthritis. Am J Med 1987;83(5A):72–7. [DOI] [PubMed] [Google Scholar]
- 59. Ammon HP. Boswellic acids in chronic inflammatory diseases. Planta Med 2006;72(12):1100–16. [DOI] [PubMed] [Google Scholar]
- 60. Boswellia serrata. Altern Med Rev 2008;13(2):165–7. [PubMed] [Google Scholar]
- 61. Cameron M, Chrubasik S.. Oral herbal therapies for treating osteoarthritis. Cochrane Database Syst Rev 2014;5:CD002947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Kessler CS, Pinders L, Michalsen A, Cramer H.. Ayurvedic interventions for osteoarthritis: A systematic review and meta-analysis. Rheumatol Int 2015;35(2):211–32. [DOI] [PubMed] [Google Scholar]
- 63. US National Institutes of Health, National Center for Complementary and Integrative Health. Ginger. Available at: https://nccih.nih.gov/health/ginger (accessed March 18, 2018).
- 64. Therapeutic Research Center. Ginger. Available at: https://naturalmedicines.therapeuticresearch.com/databases/food,-herbs-supplements/professional.aspx? productid=961 (accessed March 18, 2018).
- 65. Cohen M. Rosehip—an evidence based herbal medicine for inflammation and arthritis. Aust Fam Physician 2012;41(7):495–8. [PubMed] [Google Scholar]
- 66. Chrubasik C, Roufogalis BD, Muller-Ladner U, Chrubasik S.. A systematic review on the Rosa canina effect and efficacy profiles. Phytother Res 2008;22(6):725–33. [DOI] [PubMed] [Google Scholar]
- 67. Bottiglieri T. S-adenosyl-l-methionine (SAMe): From the bench to the bedside–molecular basis of a pleiotrophic molecule. Am J Clin Nutr 2002;76(5):1151s–7s. [DOI] [PubMed] [Google Scholar]
- 68. Bottiglieri T, Hyland K, Reynolds EH.. The clinical potential of ademetionine (s-adenosylmethionine) in neurological disorders. Drugs 1994;48(2):137–52. [DOI] [PubMed] [Google Scholar]
- 69. Friedel HA, Goa KL, Benfield P.. S-adenosyl-l-methionine. A review of its pharmacological properties and therapeutic potential in liver dysfunction and affective disorders in relation to its physiological role in cell metabolism. Drugs 1989;38(3):389–416. [DOI] [PubMed] [Google Scholar]
- 70. Therapeutic Research Center. S-adenosyl-l-methionine (SAMe). Available at: https://naturalmedicines.therapeuticresearch.com/databases/food,-herbs-supplements/professional.aspx? productid=786. (accessed March 18, 2018).
- 71. Rutjes AW, Nuesch E, Reichenbach S, Juni P.. S-adenosylmethionine for osteoarthritis of the knee or hip. Cochrane Database Syst Rev 2009;4:CD007321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Stam W, Jansen J, Taylor S.. Efficacy of etoricoxib, celecoxib, lumiracoxib, non-selective nsaids, and acetaminophen in osteoarthritis: A mixed treatment comparison. Open Rheumatol J 2012;6:6–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Brown R, Sloan P.. The opioid crisis in the United States: Chronic pain physicians are the answer, not the cause. Anesth Analg 2017;125(5):1432–4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.