Abstract
Background
Swallow or deglutition syncope is an unusual type of neurally-mediated syncope associated with life-threatening bradyarrhythmia and hypotension. It is a difficult condition to diagnose with commonly delayed diagnosis and management. There is lack of review articles that elucidate the basic demographics, clinical characteristics and management of this rare condition. This publication systematically reviews the 101 case reports published since 1793 on swallow syncope.
Case presentation
A 59-year-old man presented with the complaint of recurrent dizziness associated with meals. A 24-h ambulatory ECG recording confirmed an episode of p-wave asystole at the time of food intake. Oesophagogastroduodenoscopy with balloon inflation in the mid to lower oesophagus resulted in a 5.6 s sinus pause. The patient’s symptoms resolved completely following insertion of a permanent dual chamber pacemaker.
Conclusions
Swallow syncope is extremely rare, but still needs to be considered during diagnostic workup. It is commonly associated with gastro-intestinal disease. Permanent pacemaker implantation is the first line treatment.
Keywords: Swallow, Syncope, Deglutition, Bradycardia, AV block, Pacemaker
Background
Swallow syncope is a rare cause of a neurally mediated syncope that is frequently associated with life-threatening bradyarrhythmia [1]. The underlying mechanism is believed to be an exaggerated vagal stimulation during swallowing resulting in suppression of the cardiac conduction system. Swallow syncope has been reported in all age groups and occurs with or without underlying esophageal or cardiac pathology. A diagnosis of swallow syncope is frequently missed by physicians, often resulting in delayed diagnosis and treatment. The first case of swallow syncope was reported by Spens in 1793 [2]. Since then, another 117 cases have been reported in the literature.
We present a case of recurrent swallow syncope with a review and summary of the entire literature available regarding this rare condition.
Case presentation
A 59-year-old Chinese male presented with a 6-month history of intermittent dizziness. The dizziness occurred exclusively at meal times and was worst when swallowing large quantities of solid food, such as rice or bread. He initially was symptom free when consuming smaller quantities of solids or fluids, but his condition worsened progressively with presyncopal events occurring even while eating smaller quantities of solid food. The patient described a sensation of increasing difficulty in swallowing despite reducing the size of his meals. He denied any associated syncope or seizures. His past medical history and physical examination were unremarkable and blood investigations were within normal limits. Echocardiography revealed a structurally normal heart with normal systolic and diastolic function. 24-h electrocardiogram (ECG) monitoring recorded a sinus pause of 4.5 s at the time the patient had his meal (Fig. 1). A provisional diagnosis of swallow syncope was made and a permanent pacemaker (PPM) implantation was scheduled.
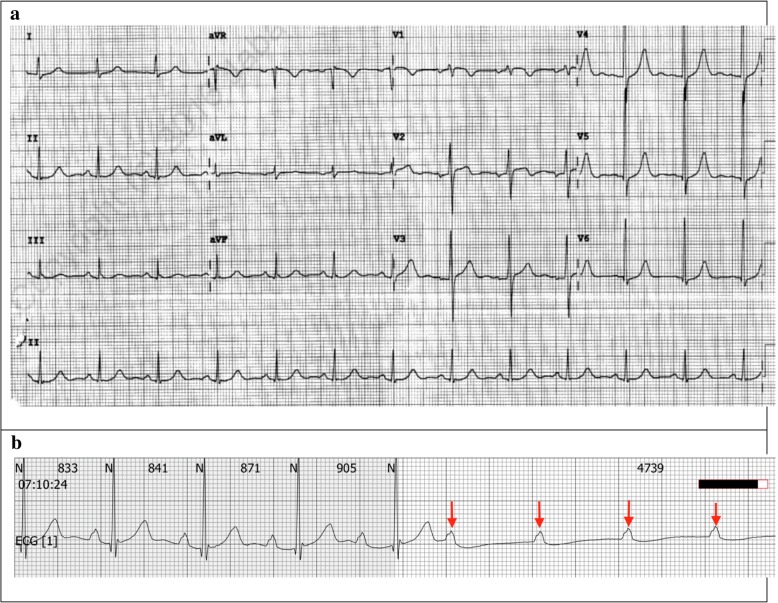
Fig. 1.
a 12-lead electrocardiogram with normal sinus rhythm during non-meal times. b 4.5 s episode of non-conducted p-waves during breakfast on a 24-h ECG. Arrow denotes p-waves
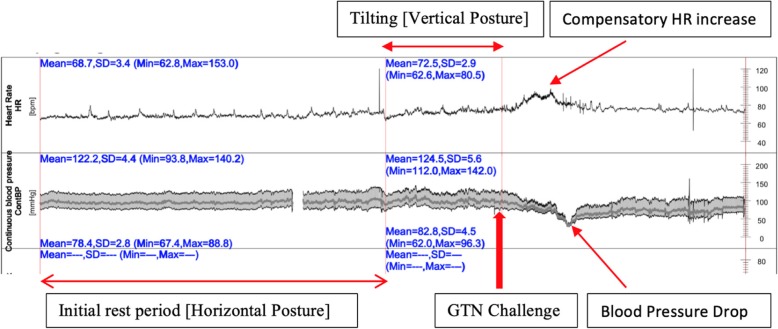
Tilt table testing prior to pacemaker insertion resulted in a hypotensive response 5 min after provocation with 400 micrograms of sublingual glycerin trinitrate administered sublingually, with reproduction of symptoms of syncope. The minimal blood pressure was 32.9/29.2 mmHg and the heart rate 75.3 bpm. No asystole was observed during tilt table testing (Fig. 2).
Fig. 2.
Tilt table test
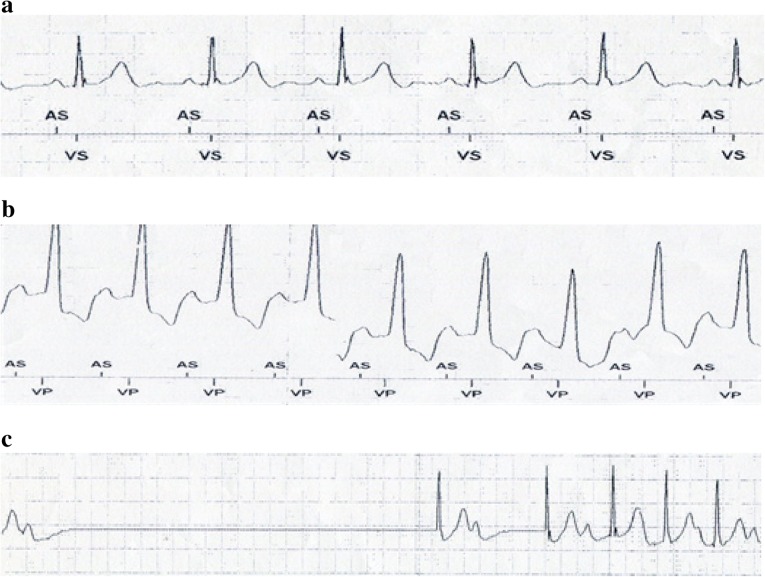
The patient’s symptoms resolved completely after implantation of a dual chamber PPM. A diagnostic workup to exclude gastrointestinal disease was performed. A barium swallow test was normal and effectively ruled out achalasia. The oesophagus appeared healthy with no structural disease on oesophagogastroduodenoscopy (OGD). The pacemaker was continuously interrogated during the OGD. Increased pacing requirements were noted when the endoscope was advanced into the esophagus (Fig. 3b). Subsequently, a 20 mm diameter TTS (through-the-scope), CRE™ (controlled radial expansion) balloon (Boston scientific) was sequentially inflated in the proximal, mid and distal esophagus while the pacemaker was programmed “OFF” to assess the physiologic response. Inflation in both distal and mid oesophagus resulted in significant sinus pauses of up to 5.6 s (Fig. 3c) confirming the cardio-inhibitory response to oesophageal distension as the underlying pathophysiological mechanism of this patient’s syncopal events.
Fig. 3.
a Pacemaker recording of patient in sinus rhythm prior to OGDS procedure, intrinsic heart rate 65 beats/min. b Pacemaker recording during advancement of endoscope into distal oesophagus (Pacemaker ON), increasing ventricular pacing. c Pacemaker recording when balloon inflation in distal oesophagus (Pacemaker OFF), 5.6 s pause
Discussion
Swallow syncope is more common in males (59.4%, n = 60), and in the older age group (55.4%, n = 56, more than 60 years old). The mean age at presentation was 57.5 years with the youngest patient described in the literature being 5 years old [3] and the eldest 89 years old [4]. All of the patient presented with either presyncope or syncope. Only one patient was diagnosed incidentally, when a high degree atrioventricular (AV) block associated with meal times was found during a diagnostic workup for lung carcinoma [5]. Swallow syncope is strongly associated with gastrointestinal diseases (32.7%, n = 33). Hiatal hernia (18.8%, n = 19), oesophageal stricture (3%, n = 3), achalasia (3%, n = 3) and oesophageal carcinoma are the most common associated gastrointestinal disorders. Thirty-three patients (32.7%) had underlying cardiac diseases including coronary artery diseases (13.9%, n = 14), atrial fibrillation (5%, n = 5), sick sinus syndrome (3%, n = 3), aortic aneurysm, rheumatic heart disease and digitalis toxicity. Twenty-eight patients (27.7%) had metabolic diseases like hypertension, diabetes mellitus, dyslipidaemia or obesity.
In most patients (54.5%, n = 55), any type of food – be it liquids or solids - triggered syncope. Atrioventricular conduction blocks (34.7%, n = 35) including first, second and third-degree AV blocks are the most common electrophysiological problems, followed closely by sinus node dysfunctions (33.7%, n = 34) including sinus bradycardia, sinus arrest and asystole. Second degree AV block, complete heart block (=3rd degree AV block) and asystole were the most frequently reported bradyarrhythmia in the literature. However, there are several cases where both sinus and atrioventricular dysfunction concurred. Paroxysmal atrial fibrillation and atrial tachycardia were rare causes of syncope. Table 1.
Table 1.
Literature review of 101 cases of Swallow Syncope from 1949 to 2018
| Author/ Reference | Age/ Gender | Presenting Symptom | Underlying Diseases | Trigger Factor | Type of arrhythmia | Management | Effectiveness |
|---|---|---|---|---|---|---|---|
| Padalia et al. 2018/ [6] | 65/ F | Presyncope, Dysphagia, Odynophagia/ | Candida Esophagitis, Metabolic Diseases | Solid and Liquid | Sinus bradycardia, Sinus arrest | Micafugin | Yes |
| Sammy et al. 2018/ [7] | 67/M | Syncope | End Stage Renal Failure | Ascension of Hyoid bone irritate carotid sinus | – | – | – |
| Yamaguchi et al. 2018/ [8] | 76/M | Syncope | No | Solid and Liquid (Citrus based) | Sinus arrest, AV block | PPM | Yes |
| Lipar et al. 2018/ [9] | 49/F | Syncope | Post whiplash neck injury | Solid and Liquid | – | PPM | Yes |
| Van Damme et al. 2017/ [10] | 39/M | Syncope | No | Solid and Liquid | 3rd degree AV block | PPM | – |
| Aydogdu et al. 2017/ [11] | 51/F | Presyncope, Syncope | No | Solid food | AV block | Rejected PPM | – |
| 65/F | Syncope | – | Liquid (Carbonated) | Sinus arrest, 3rd degree AV block | PPM | Yes | |
| 39/F | Presyncope, Syncope | No | Solid food | 3rd degree AV block | PPM | Yes | |
| 53/F | Presyncope, Syncope | No | Solid food | Asystole | Diet modification | – | |
| 68/M | Presyncope, Syncope | Atrial Fibrillation | Liquids | Asystole | PPM | Yes | |
| Patel et al. 2017/ [12] | 48/M | Syncope, Nausea, Tunnel vision | Hiatus Hernia | Solid and Liquid | Sinus arrest | Hiatus hernia repair surgery | Yes |
| Zaid et al. 2017/ [13] | 71/M | Syncope | Achalasia | Solid food | AV block | – | – |
| Bhogal et al. 2017/ [14] | 68/F | Presyncope | Hiatus Hernia, Metabolic Diseases | Solid food | Sinus Bradycardia, 1st degree AV block | Discontinuation of metoprolol + Proton Pump Inhibitor | No |
| 59/M | Pre-syncope & Syncope | No | Liquid diet | Premature atrial complexes & Asystole | PPM | Yes | |
| Trinco et al. 2016/ [15] | 83/ M | Syncope | Carotid endarterectomy, Metabolic diseases | Solid and Liquid | Sinus bradycardia, 3rd degree AV block | PPM | Yes |
| Islam et al. 2016/ [16] | 60/ F | Presyncope, Syncope | No | Solid food (Large chunk of bread) | AV block | Avoidance of trigger | Yes |
| Chhetri et al. 2016/ [17] | 71/M | Syncope | Fundoplication for GERD | Solid and Liquid (Fizzy drink) | Sinus arrest | PPM | NM |
| Tiffany et al. 2016/ [18] | 80/F | Syncope, palpation, facial flushing | Metabolic diseases, Hypothyrodism | Solid and Liquid | Atrial Tachycardia | Catheter ablation | Yes |
| Manu et al. 2016/ [19] | 13/F | Syncope | Superior sinus atrial septal defect | Solid and Liquid | 3rd degree AV block | PPM | Yes |
| Aaberg et al. 2015/ [20] | 62/M | Pre-syncope, Syncope | No | Solid and Liquid | 2nd and 3rd degree AV block | PPM | Yes |
| Kahn et al. 2015/ [4] | 89/M | Syncope | Transient Oesophageal dysmotility, Coronary artery diseases | Solid and Liquid (Carbonated) | 1st and 2nd degree AV block | PPM | Yes |
| Saitoh et al. 2015/ [21] | 70/M | Syncope | No | Solid food | Asystole | PPM | Yes |
| Erdogan et al. 2015/ [22] | 47/M | Syncope | Achalasia | Solid and Liquid | AV block, Asystole | Pneumatic dilation | Yes |
| Shashank et al. 2014/ [23] | 31/F | Presyncope & Syncope | No | Liquid (Carbonated) | Sinus bradycardia, Asystole | PPM | Yes |
| 78/ M | Presyncope | Sick sinus syndrome, Metabolic diseases | Solid food | – | PPM + Coffee before meals | Yes | |
| 80/M | Presyncope, Syncope | Hiatus Hernia AF, various cardiac comorbid | Solid food (Sticky food) | – | Avoidance of trigger | Yes | |
| Shah et al. 2014/ [24] | 57/M | Presyncope, Syncope | No | Swallow +Cold drink | Advanced heart block for 3–4 s | PPM | Yes |
| Witcik et al. 2014/ [25] | 70/M | Syncope, Weakness, Flushing | Mild AV regurgitation | Liquid (Carbonated) | Atrial Fibrillation with ventricular pause | PPM | Yes |
| Arihide et al. 2014/ [26] | 79/M | Syncope | Coronary artery disease, Metabolic diseases | Solid and Liquid | Sinus arrest | PPM | Yes |
| Moore et al. 2013/ [27] | 65/F | Presyncope, Syncope | No | Solid food | AV block | PPM | Yes |
| Lambiris et al. 2013/ [28] | 54/M | Presyncope, Shortness of breath | No | Solid and Liquid | 1st degree AV block | PPM | Yes |
| Rezvani et al. 2013/ [29] | 51/F | Syncope | Post Laparoscopic gastrectomy | Solid and Liquid | AV block | Atropine | Yes |
| Kim eat al. 2012/ [30] | 39/M | Syncope, Chest tightness | No | Liquid (Cold) | 3rd degree AV block | Avoidance of trigger | Yes |
| Knopke et al. 2012/ [31] | 49/F | Syncope, Dysphagia, Regurgitation | Hiatus hernia, Diffuse oesophageal spasm | Solid food | 3rd degree AV block | PPM | Yes |
| Foreman et al. 2011/ [32] | 52/F | Presyncope, Chest pain | No | Solid food | 2nd degree AV block | PPM | Yes |
| Vanerio et at. 2011/ [33] | 84/F | Syncope | Hiatus Hernia | Solid and Liquid (Carbonated) | – | Nissen’s Fundoplication | Yes |
| Mitra et al. 2011/ [34] | 60/F | Presyncope, Syncope | Metabolic Diseases | Solid food | Sinus Bradycardia, 3rd degree AV block | PPM | Yes |
| Marina et al. 2010/ [35] | 37/M | Syncope | Megaoesophagus, Extra Cardiac mass compressing left atrium | Solid and Liquid | – | Deflation of gastric band | – |
| GY Lee et al. 2010/ [36] | 62/M | Syncope, Dysphagia | Atrial Fibrillation, Metabolic diseases | Liquid | Asystole | PPM | Yes |
| Endean et al. 2010/ [37] | 61/ M | Syncope, Chest pain, Vision lost | Post Carotid entaterectomy | Solid food | – | Glycopyrrolate | Yes |
| Casella et al. 2009/ [38] | 66/ M | Syncope | Oesophageal dysmotility, Sick sinus syndrome | Liquid only | AV block | PPM | Yes |
| Karamitsos et al. 2009/ [39] | 82/F | Syncope | Hiatus hernia | Large meal | NM | – | – |
| Favaretto et al. 2008/ [40] | 63/M | Syncope, Odynophagia | Hiatus hernia | Solid and Liquid | Asystole | PPM | Yes |
| Bajwa et al. 2008/ [41] | 51/M | Presyncope, Syncope | Metabolic diseases, Inflammatory bowel diseases | Solid food | Atrial & Ventricular atopic beat | PPM | Yes |
| Christopher et al. 2008/ [42] | 25/F | Syncope | No | Solid and Liquid | 3rd degree AV block | PPM | Yes |
| Fahrner et al. 2008/ [43] | 75/M | Syncope | No | Solid and Liquid | AV block | – | – |
| Patsilinakos et al. 2007/ [44] | 86/F | Syncope | Oesophageal stenosis, Ascending aorta aneurysm, Hypothyroidism | Solid and Liquid | Sinus arrest | Avoidance of trigger | Yes |
| Tuzcu et al. 2007/ [45] | 16/F | Syncope, Visual disturbance | No | Solid food | 3rd degree AV block, Asystole | PPM | Yes |
| Omni et al. 2006/ [2] | 66/F | Syncope | Metabolic Diseases | Liquid | AV block | PPM | Yes |
| Gawrieh et al. 2005/ [46] | 63/M | Presyncope, Syncope, Dysphagia | Hiatus Hernia | Solid food | AV block, Asystole | PPM | Yes |
| 63/M | Presyncope, Syncope | Hiatus hernia, Coronary artery diseases, Metabolic diseases | Solid and Liquid | – | Refuse treatment | – | |
| 62/F | Presyncope, Syncope, Dysphagia | Nutcracker oesophagus, Coronary artery diseases | Solid and Liquid | Sinus bradycardia, Sinus arrest | PPM | Yes | |
| Turan et al. 2005/ [47], Kang et al. 2005/ [48] | 48/M | Syncope, Dysphagia | Achalasia | Solid food | Sinus bradycardia | PPM | Yes |
| 59/ M | Syncope | Metabolic diseases | Solid and Liquid | Sinus bradycardia | PPM | – | |
| 59/M | Syncope, Dysphagia | Compression fracture thoracic spine, Graves diseases | Solid food | Sinus bradycardia | Diet habit modification | – | |
| Sreekant et al. 2004/ [49] | 85/M | Syncope | Coronary artery diseases, Peripheral vascular diseases | Solid and liquid | Asystole | PPM | Yes |
| 61/ F | Presyncope | Metabolic diseases | Liquid (Carbonated) | Sinus Bradycardia | – | – | |
| Yoshifumi et al. 2004/ [50] | 76/F | Syncope | Hiatus hernia | Solid food | – | – | – |
| Srivathsan et al. 2003/ [51] | 26/M | Presyncope | No | Solid food | Systole | PPM | Yes |
| Mekawa et al. 2002/ [52] | 76/ F | Syncope | Hiatus hernia | Solid and liquid | – | Hernia repair surgery | Yes |
| Gordon et al. 2002/ [53] | 26/F | Syncope, Central chest discomfort | Hiatus hernia | Solid and liquid | Paroxysmal Atrial fibrillation, Ventricle atopic beat | Diet habit modification | Yes |
| Takeshi et al. 2002 [54] | 69/F | Presyncope, Syncope | Metabolic diseases | Solid food | Sinus arrest | – | – |
| Rasmi et al. 2001/ [55] | 16/M | Syncope | No | Liquid (Carbonated) | Asystole | PPM | Yes |
| Haumer et al. 2000/ [56] | 67/ M | Syncope | Coronary artery disease | Liquid | Sinus arrest | Temporary Pacemaker | Yes |
| Kakuchi et al. 2000/ [57] | 21/M | Syncope | Vasovagal syncope | Solid and liquid | AV block | PPM | – |
| Kazushi et al. 1999/ [58] | 69/M | Syncope, Facial flushing, Profuse diarrhoea | Metabolic disease, Stroke | Solid food | – | Cessation of Enalapril | Yes |
| Olshasky et al. 1999/ [59] | 72/M | Presyncope, Syncope | – | Liquid (Cold carbonated) | Sinus bradycardia | PPM | – |
| Dante et al. 1997/ [60] | 78/M | Syncope | Oesophageal carcinoma | Solid food | AV block, Asystole | PPM | Yes |
| Bellori et al. 1992/ [61] | 69/M | Syncope | – | Liquid | Sinus arrest | – | – |
| SY AO et al. 1991/ [5] | 70/M | Incidental | Lung carcinoma | Solid and Liquid | High grade AV block | Atropine before meal | Yes |
| Shapira et al. 1991/ [62] | 63/M | Presyncope, Syncope | Hiatus hernia, Coronary artery disease | Solid and Liquid | 2nd degree AV block | PPM | Yes |
| Kunimoto et al. 1990/ [63] | 65/M | Presyncope, Syncope | No | Liquid (Cold) | 2nd degree AV block, Asystole | PPM | Yes |
| Elam et al. 1989/ [64] | 44/M | Syncope | No | Solid and Liquid | 3rd degree AV block | PPM | Yes |
| Engelharbt et al. 1986/ [3] | 5/F | Syncope | No | Solid and Liquid/ Brush teeth | 3rd degree AV block | Close Observation | Yes |
| Ausubel et al. 1987/ [65] | 26/M | Syncope | Heart murmur | Solid food | Sinus bradycardia, AV block | PPM | Yes |
| Nakano et al. 1987/ [66] | 67/M | Syncope, Retrosternal discomfort | Aneurysm descending thoracic aorta | Solid and Liquid | Sinus bradycardia, Sinus arrest | Atropine before meal | Yes |
| Nakagawa et al. 1987/ [67], Guberman et al.1986/ [68] | 48/M | Syncope | No | Solid and Liquid | AV block | Atropine | – |
| 62/F | Syncope | No | Oesophageal balloon inflation | 2nd degree heart block | Propanthelene bromide | No | |
| 62/M | Syncope | Congestive heart failure | Solid food | 2nd degree heart block | Discontinuation of digoxin | Yes | |
| Alan et al. 1986/ [69] | 56/M | Syncope | Inferior myocardial infarction | Liquid | 1st degree heart block | PPM | Yes |
| Golf et al. 1986/ [70] | 15/ F | Syncope | No | Solid and Liquid | SA node blockade with junctional escape rhythm | – | – |
| Armstrong et al. 1985/ [71] | 53/F | Syncope, Dyspnoea, Retrosternal discomfort | Hiatus hernia | Liquid | Sinus bradycardia | PPM | Yes |
| 58/F | Syncope, Pulseless, Apnoea | Myocardial infarction, Atrial Fibrillation, Stroke | Solid and Liquid | Sinus bradycardia and Asystole | PPM | No | |
| 58/F | Presyncope | No | Solid and Liquid | 3rd degree AV block and Asystole | PPM | Yes | |
| 81/F | Syncope | Hiatus hernia, Metabolic disease | Liquid (Hot) | Sinus bradycardia | PPM | Yes | |
| 53/M | Syncope | Myocardial infarction | Liquid (Cold) | 2nd degree AV block | PPM | Yes | |
| Kunis et al. 1985/ [72] | 60/M | Presyncope, Syncope, Chest pain | Metabolic diseases | Solid food (Hot) | 3rd degree AV block, Asystole | PPM | Yes |
| Drake et al. 1985/ [73] | 76/F | Syncope | Myocardial infarction, Metabolic disease | Sight of food | 3rd degree AV block | PPM | Yes |
| Mauro et al. 1985/ [74] | 65/ F | Presyncope, syncope | Myocardial ischemia | Solid and Liquid | 2nd degree AV block | Atropine | No |
| Golf et al. 1977 [75] | −/ M | Syncope, Convulsion | No | Solid and Liquid | 2nd degree AV block | PPM | Yes |
| Weaddington et al. 1975/ [76] | 71/M | Syncope | Hiatus hernia, Oesophagus carcinoma, Atrial Fibrillation | Solid food | Sinus bradycardia and Asystole | Surgical removal of Oesophageal Carcinoma | Yes |
| B Wik et al. 1975/ [77] | 43/ M | Syncope, Retrosternal chest pain | Rheumatic heart diseases | Liquid (Carbonated) | AV block | PPM | – |
| Poul et al. 1973/ [78] | 64/ F | Syncope | Hiatus hernia, Abnormal oesophageal motility | Solid and Liquid | Sinus bradycardia, AV block | Hernia Repair | Yes |
| Edgar et al. 1972/ [79] | 84/M | Syncope | Hiatus hernia, Metabolic diseases | Solid and Liquid | 2nd degree AV block | Atropine | Yes |
| Keith et al. 1971/ [80] | 45/M | Syncope, Dysphagia, Heart burn | Hiatus hernia, Oesophageal stricture | Solid and Liquid | Sinus bradycardia | Dilation of oesophageal stricture | Yes |
| Rajendra et al. 1971/ [81] | 29/ F | Syncope | No | Solid and Liquid | Asystole | Surgical cauterization vagal nerve | Yes |
| Edgardo et al. 1970/ [82] | 73/M | Syncope, Chest pain | Myocardial infarction, Metabolic disease | Solid and Liquid | AV block, Asystole | Atropine | Yes |
| R P Sapru et al.1968/ [83] | 29/F | Presyncope | No | Solid and Liquid | AV block, Asystole | Atropine | Yes |
| George et al. 1958/ [84] | −/− | Syncope | No | Liquid | – | Discontinuation of digitalis | Yes |
| Correll et al. 1949/ [85] | 67/M | Syncope, Chocking sensation | Oesophageal diverticulum, Digitalis medication | Solid and Liquid | 3rd degree AV block | Atropine | Yes |
F Female, M Male, (−) Not Stated, AV Atrioventricular, PPM Permanent Pacemaker
Pacemaker implantation is the most popular treatment modality. More than half of the patients (55.5%, n = 56) were treated with a permanent pacemaker. Almost all (98.1%, n = 52) of the patients treated with pacemakers reported resolution of syncopal symptoms. One patient passed away shortly following a PPM implant due to asystole despite a reportedly normal functioning pacemaker [71]. Treatment of an underlying causative factor (15.8%, n = 16) was the second most common treatment modality. Treatment of an underlying gastrointestinal disorder has been shown to carry a good likelihood of resolving the swallow syncope. For example, all four cases of hiatal hernia that were corrected surgically had a complete resolution of the swallow syncope. Likewise, dilatation of an oesophageal stricture and an achalasia resulted in complete resolution of swallow syncope. Other reported successful treatments of underlying gastrointestinal diseases included surgical cauterisation of the vagal nerve, long term proton pump inhibitors and surgical excision of an oesophageal carcinoma. Pharmacological management was the preferred treatment option in the 19th and early twentieth century prior to the era of pacemakers. From the limited numbers, atropine was the most widely used, with about 90% efficacy. Table 2.
Table 2.
Characteristics of 101 reviewed cases of swallow syncope
| Frequency (n=) | Percentage (%) | |
|---|---|---|
| Age Group (n = 101) | ||
| Childhood/Adolescent [0–19 years] | 6 | 5.9 |
| Younger adults [20–59 years] | 37 | 36.6 |
| Older adults [60 years and above] | 56 | 55.4 |
| Not stated | 2 | 2.0 |
| Gender (n = 101) | ||
| Male | 60 | 59.4 |
| Female | 40 | 39.6 |
| Not Stated | 1 | 1.0 |
| Clinical Presentation (n = 101) | ||
| Syncope | 100 | 99.0 |
| Dysphagia | 12 | 11.9 |
| Asymptomatic (incidental diagnosis) | 1 | 1.0 |
| Underlying Diseases (n = 100) | ||
| Gastrointestinal Diseases | 34 | 33.7 |
| Hiatal Hernia | 19 | 18.8 |
| Achalasia | 3 | 3.0 |
| Esophageal stricture | 3 | 3.0 |
| Cardiac Diseases | 33 | 32.7 |
| Coronary artery diseases | 14 | 13.9 |
| Atrial Fibrillation | 5 | 5.0 |
| Sick Sinus Syndrome | 3 | 3.0 |
| Comorbiditiesa | 28 | 27.7 |
| Trigger Factor (n = 101) | ||
| Any (Solid and Liquid) | 55 | 54.5 |
| Solid only | 23 | 22.8 |
| Liquid only | 23 | 22.8 |
| Type of Arrhythmia (n = 101) | ||
| Sinus Dysfunctionb | 34 | 33.7 |
| Atrioventricular Dysfunctionc | 35 | 34.7 |
| Combination Sinus and AV Dysfunction | 16 | 15.8 |
| Not Stated | 13 | 12.9 |
| Othersd | 3 | 3.0 |
| Management (n = 101) | ||
| Pacemaker Implantation | 56 | 55.5 |
| Pharmacotherapy | 11 | 10.9 |
| Atropine | 9 | 8.9 |
| Treatment of Underlying causative factor | 16 | 15.8 |
| Surgical correction of hiatal hernia | 4 | 4.0 |
| Dilation of achalasia | 1 | 1.0 |
| Dilation of esophageal stricture | 1 | 1.0 |
| Conservative Management | 9 | 8.9 |
| Avoidance trigger/ diet modification | 7 | 6.9 |
| Close observation/ refused treatment | 2 | 2.0 |
| Not Stated | 9 | 8.9 |
| Documented efficacy of resp. treatment | Effective (n=) | Efficacy rate (%) |
| Pacemaker (n = 53) | 52 | 98.1 |
| Atropine treatment (n = 8) | 7 | 87.5 |
| Surgical correction of Hiatal hernia (n = 4) | 4 | 100 |
| Dilation of Achalasia (n = 1) | 1 | 100 |
| Dilation of esophageal stricture (n = 1) | 1 | 100 |
| Avoidance trigger/ diet modification (n = 5) | 5 | 100 |
aComorbidities defined as hypertension or diabetes mellitus or dyslipidemia or obesity or chronic kidney disease
b Sinus Bradycardia, Sinus Arrest, Asystole; c First, Second, Third degree Atrioventricular block; d Atrial Tachycardia, Atrial Fibrillation and others
Various mechanisms regarding the pathogenesis of swallow syncope have been postulated.
The most common postulated mechanism is increased and excessive vagal reflex activation during swallowing causing cardio inhibition [86]. During swallowing, the afferent impulses from the oesophageal plexus travel via the vagus nerve to the nucleus solitarius tract in the medulla oblongata. Subsequently, a corresponding signal that regulates involuntary peristalsis will travel down the parasympathetic efferent fibers through the oesophageal branch of the vagus nerve [87]. The presence of reflex arcs between afferent sensory fibers and efferent parasympathetic fibers of the cardiac branch results in inappropriate vagal activation with bradycardia, disturbance to the conduction system and hypotension secondary to vasodilation [27, 88]. The exact mechanism remains to be elucidated, however, excessive parasympathetic stimulation to the heart seems to be the central mechanism. The fact that atropine, a potent anticholinergic agent, prevents bradyarrhythmia effectively in cases of swallow syncope supports the theory of excessive vagal stimulations [5, 29, 66, 79].
Abnormal oesophageal mechanoreceptors have been postulated to be the primary cause of swallow syncope in individuals with underlying structural and functional disorders of the gastrointestinal system. We demonstrated a reproducible cardio-inhibition with balloon inflation in the mid to lower oesophagus in our patient [48, 89]. The bradyarrhythmia was terminated upon deflation of the balloon suggesting that mechanoreceptors in the mid-lower oesophagus may play a role in the pathogenesis of swallow syncope.
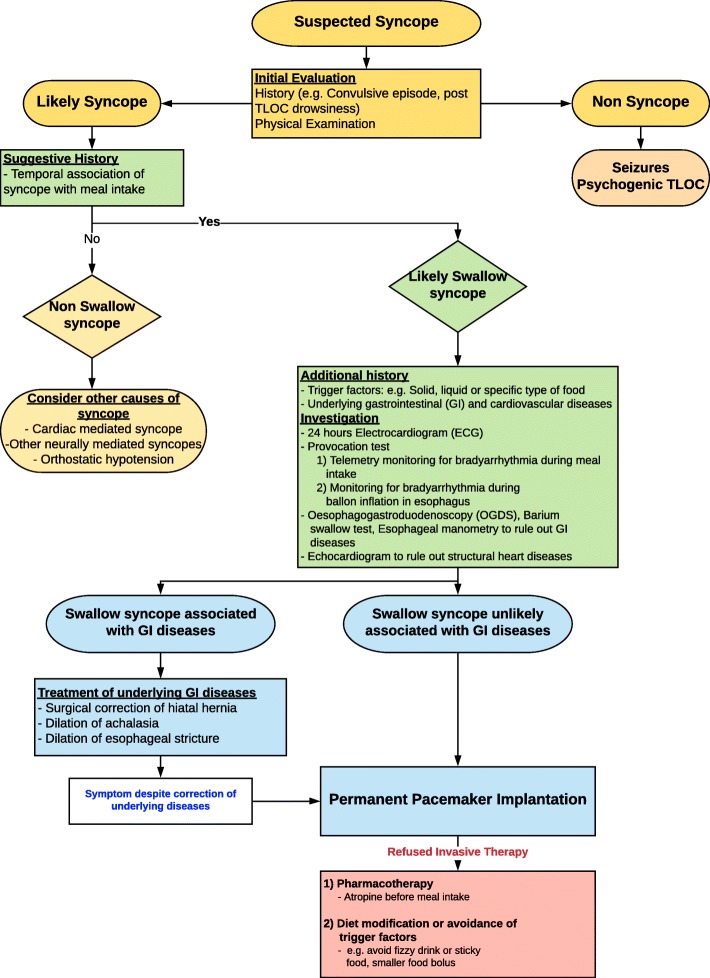
Investigations of neurally-mediated syncope should be tailored based on actual precipitants. While a tilt-table test confirmed the presence of a vasovagal response with reproduction of syncope, it did not demonstrate any periods of asystole. The diagnosis in this case was confirmed during OGD with cardiac monitoring and hence investigation with an OGD with haemodynamic monitoring should be considered for individuals with suspected swallow syncope. A diagram depicting a proposed approach to the diagnostic work-up and management of patients with symptoms suggestive of swallow syncope is depicted in (Fig. 4).
Fig. 4.
Approach to the diagnostic work-up and management of patients with symptoms suggestive of swallow syncope
Conclusions
Swallow syncope is a rare cause for syncopal events and should be considered as part of the diagnostic workup. Pacemakers are a safe and efficacious therapeutic option for all patients with that condition. In patients with associated gastrointestinal disease, specific treatment of the underlying disease has a high likelihood of resolving the swallow syncope without the need for permanent pacing.
Acknowledgments
This publication was presented as an abstract at the European Society of Cardiology, Heart Failure 2019 and the World Congress on Acute Heart Failure, 25th – 28th May 2019, Athens, Greece.
Abbreviations
- AV block
Atrioventricular block
- ECG
Electrocardiogram
- OGD
Oesophagogastroduodenoscopy
- PPM
Permanent pacemaker
Authors’ contributions
KSSW and AL prepared the manuscript and are responsible for the overall content as guarantors. TMP and INH reviewed the manuscript. All authors read and approved the final manuscript.
Funding
Not applicable.
Availability of data and materials
The datasets used and/or analysed in the literature review are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Kelvin Shenq Woei Siew, Phone: 006(0)3 7949 4422, Email: ksiewsw@gmail.com.
Maw Pin Tan, Email: mptan@ummc.edu.my.
Ida Normiha Hilmi, Email: i_hilmi@hotmail.com.
Alexander Loch, Email: alexanderloch@gmx.de.
References
- 1.Parry SW, Tan MP. An approach to the evaluation and management of syncope in adults. Bmj. 2010;340:c880. doi: 10.1136/bmj.c880. [DOI] [PubMed] [Google Scholar]
- 2.Omi W, et al. Swallow syncope, a case report and review of the literature. Cardiology. 2006;105(2):75–79. doi: 10.1159/000089543. [DOI] [PubMed] [Google Scholar]
- 3.Engelhardt W, Kotlarek F, von Bernuth G. Deglutition syncope in childhood with complete atrioventricular block. Am J Cardiol. 1986;58(11):1113–1114. doi: 10.1016/0002-9149(86)90128-1. [DOI] [PubMed] [Google Scholar]
- 4.Kahn A, Koepke LM, Umar SB. Deglutition syncope: a case report and review of the literature. ACG Case Rep J. 2015;3(1):20–22. doi: 10.14309/crj.2015.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sy AO, Plantholt S. Swallowing-induced atrioventricular block. South Med J. 1991;84(10):1274–1275. doi: 10.1097/00007611-199110000-00028. [DOI] [PubMed] [Google Scholar]
- 6.Padalia Kishan J., Padalia Arjun J., Parikh Milind G. Dysphagia, Hyperglycemia, and Presyncope. Dysphagia. 2018;33(6):866–868. doi: 10.1007/s00455-018-9932-5. [DOI] [PubMed] [Google Scholar]
- 7.Tawk S, Desuter G, Jamali S. Recurrent syncope upon deglutition. J Belg Soc Radiol. 2018;102(1):55. doi: 10.5334/jbsr.1584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yamaguchi Y, et al. Citrus fruits induced swallow syncope with atrioventricular block or sinus arrest. J Electrocardiol. 2018;51(4):613–616. doi: 10.1016/j.jelectrocard.2018.04.012. [DOI] [PubMed] [Google Scholar]
- 9.Lipar L, et al. Swallow syncope after whiplash neck injury. Heart Surg Forum. 2018;21(2):E084–e086. doi: 10.1532/hsf.1933. [DOI] [PubMed] [Google Scholar]
- 10.Van Damme A, De Backer T, Vanderheeren P. Swallow presyncope in an athletic patient caused by third-degree atrioventricular block. Acta Clin Belg. 2018;73(6):403-7. [DOI] [PubMed]
- 11.Aydogdu I, et al. Swallow-induced syncope in 5 patients: Electrophysiologic evaluation during swallowing. Neurol Clin Pract. 2017;7(4):316–323. doi: 10.1212/CPJ.0000000000000376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Patel N, et al. Deglutition syncope. Proc (Baylor Univ Med Cent) 2017;30(3):293–294. doi: 10.1080/08998280.2017.11929619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zaid EA, et al. Swallow-induced syncope and carotid sinus hypersensitivity: coincident or associated conditions? J Electrocardiol. 2017;50(4):523–525. doi: 10.1016/j.jelectrocard.2017.03.011. [DOI] [PubMed] [Google Scholar]
- 14.Bhogal S, et al. Deglutition syncope: two case reports attributed to vagal hyperactivity. Case Rep Cardiol. 2017;2017:2145678. doi: 10.1155/2017/2145678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Trinco P, et al. A case of swallow syncope. Rev Med Liege. 2016;71(7–8):360–363. [PubMed] [Google Scholar]
- 16.Islam Z, Warricker F, Shah BN. Swallow (deglutition) syncope. Postgrad Med J. 2016;92(1090):489–490. doi: 10.1136/postgradmedj-2016-133998. [DOI] [PubMed] [Google Scholar]
- 17.Chhetri SK, Khan S, Nixon J. Swallow syncope unravelled by fizzy drink challenge. Qjm. 2016;109(5):341–342. doi: 10.1093/qjmed/hcw024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hu TY, et al. Swallow-induced syncope: a case report of atrial tachycardia originating from the SVC. HeartRhythm Case Rep. 2016;2(1):83–87. doi: 10.1016/j.hrcr.2015.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Manu S, Aziz PF. Syncope with swallowing. J Pediatr. 2016;172:209–211. doi: 10.1016/j.jpeds.2016.01.053. [DOI] [PubMed] [Google Scholar]
- 20.Aaberg AM, Eriksson AE, Madsen PL, Dixen U. Swallow syncope caused by third-degree atrioventricular block. BMJ Case Rep. 2015;2015. [DOI] [PMC free article] [PubMed]
- 21.Saitoh T, et al. Swallow syncope. Acute Med Surg. 2015;2(2):145–146. doi: 10.1002/ams2.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Erdogan HI, Gok H, Karanfil M. Swallowing-induced atrioventricular block and syncope in a patient with achalasia. Turk J Gastroenterol. 2015;26(1):75–76. doi: 10.5152/tjg.2015.5312. [DOI] [PubMed] [Google Scholar]
- 23.Garg S, et al. Swallow syncope: clinical presentation, diagnostic criteria, and therapeutic options. Saudi J Gastroenterol. 2014;20(4):207–211. doi: 10.4103/1319-3767.136932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shah R, et al. Dangerous cold beverages: a case of swallow syncope. Am J Med. 2014;127(7):e3–e4. doi: 10.1016/j.amjmed.2014.01.021. [DOI] [PubMed] [Google Scholar]
- 25.Witcik M, Meskin J. Pop and drop. Wmj. 2014;113(4):162–163. [PubMed] [Google Scholar]
- 26.Okahara A. Blackout during meals: a case report of swallow syncope due to sinus arrest. J Cardiol Cases. 2014;10(3):91–93. doi: 10.1016/j.jccase.2014.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Moore PK, et al. A case of swallow syncope. Tex Heart Inst J. 2013;40(5):606–607. [PMC free article] [PubMed] [Google Scholar]
- 28.Lambiris Irene, Mendoza Ivan, Helguera Marcelo, Escudero Jose Baez, Bonilla Cesar. Thirty years of blackouts: a case report of swallow syncope. Journal of Community Hospital Internal Medicine Perspectives. 2013;3(1):20323. doi: 10.3402/jchimp.v3i1.20323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rezvani M, Casillas SG, Antanavicius G. Swallow syncope after laparoscopic vertical sleeve gastrectomy. Surg Obes Relat Dis. 2013;9(5):e77–e78. doi: 10.1016/j.soard.2013.03.002. [DOI] [PubMed] [Google Scholar]
- 30.Kim C, et al. A case of swallow syncope associated with cold beverage ingestion. Korean Circ J. 2012;42(3):212–215. doi: 10.4070/kcj.2012.42.3.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Knopke S, et al. Fainting during ingestion. Deglutition syncope. Hno. 2012;60(3):279–281. doi: 10.1007/s00106-011-2405-x. [DOI] [PubMed] [Google Scholar]
- 32.Foreman J, Vigh A, Wardrop RM., 3rd Hard to swallow. Am J Med. 2011;124(3):218–220. doi: 10.1016/j.amjmed.2010.10.009. [DOI] [PubMed] [Google Scholar]
- 33.Vanerio G. Syncope caused by huge hiatal hernia. Case Rep Cardiol. 2011;2011:560734. doi: 10.1155/2011/560734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mitra S, et al. Swallow syncope: a case report and review of the literature. Clin Med Res. 2011;9(3–4):125–129. doi: 10.3121/cmr.2010.969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Leitman M, et al. A 37-year-old man with recurrent fainting: a short communication. Eur J Echocardiogr. 2010;11(7):E30. doi: 10.1093/ejechocard/jeq038. [DOI] [PubMed] [Google Scholar]
- 36.Lee GY, et al. Deglutition syncope associated with ventricular asystole in a patient with permanent atrial fibrillation. Korean Circ J. 2010;40(2):99–101. doi: 10.4070/kcj.2010.40.2.99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Endean ED, et al. Deglutition syncope: a manifestation of vagal hyperactivity following carotid endarterectomy. J Vasc Surg. 2010;52(3):720–722. doi: 10.1016/j.jvs.2010.04.012. [DOI] [PubMed] [Google Scholar]
- 38.Casella F, et al. When water hurts. Pacing Clin Electrophysiol. 2009;32(11):e25–e27. doi: 10.1111/j.1540-8159.2009.02521.x. [DOI] [PubMed] [Google Scholar]
- 39.Karamitsos TD, et al. Massive hiatus hernia impeding transoesophageal echocardiography in a patient with swallow-syncope syndrome. Hell J Cardiol. 2009;50(3):216–217. [PubMed] [Google Scholar]
- 40.Favaretto E, et al. An uncommon case of right-sided throat pain and swallow syncope. J Cardiovasc Med (Hagerstown) 2008;9(11):1152–1155. doi: 10.2459/JCM.0b013e32830f42b1. [DOI] [PubMed] [Google Scholar]
- 41.Bajwa S, et al. Swallow syncope: reflex or reflux? Postgrad Med J. 2008;84(989):160–162. doi: 10.1136/pgmj.2007.062869. [DOI] [PubMed] [Google Scholar]
- 42.John C. Dangerous sandwiches. Lancet. 2008;372(9656):2164. doi: 10.1016/S0140-6736(08)61932-7. [DOI] [PubMed] [Google Scholar]
- 43.Fahrner A, et al. Swallow syncope. Eur J Emerg Med. 2008;15(2):122–123. doi: 10.1097/MEJ.0b013e3282f213ad. [DOI] [PubMed] [Google Scholar]
- 44.Patsilinakos SP, et al. Swallow syncope in a patient with esophageal stenosis caused by an ascending aorta aneurysm: differential diagnosis from postprandial hypotension: a case report. Angiology. 2007;58(1):126–129. doi: 10.1177/0003319706295514. [DOI] [PubMed] [Google Scholar]
- 45.Tuzcu V, Halakatti R. Swallow syncope associated with complete atrioventricular block in an adolescent. Pediatr Cardiol. 2007;28(5):409–411. doi: 10.1007/s00246-006-0167-0. [DOI] [PubMed] [Google Scholar]
- 46.Gawrieh S, et al. Swallow syncope in association with Schatzki ring and hypertensive esophageal peristalsis: report of three cases and review of the literature. Dysphagia. 2005;20(4):273–277. doi: 10.1007/s00455-005-0024-y. [DOI] [PubMed] [Google Scholar]
- 47.Turan I, Ersoz G, Bor S. Swallow-induced syncope in a patient with achalasia. Dysphagia. 2005;20(3):238–240. doi: 10.1007/s00455-005-0014-0. [DOI] [PubMed] [Google Scholar]
- 48.Kang KH, et al. Cases of swallow syncope induced by the activation of mechanorecepters in the lower esophagus. Korean J Intern Med. 2005;20(1):68–71. doi: 10.3904/kjim.2005.20.1.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Cherukuri S, Gardner GM. Deglutition syncope. Otolaryngol Head Neck Surg. 2004;130(1):145–147. doi: 10.1016/S0194-5998(03)01597-3. [DOI] [PubMed] [Google Scholar]
- 50.Oishi Y, et al. Syncope upon swallowing caused by an esophageal hiatal hernia compressing the left atrium: a case report. Echocardiography. 2004;21(1):61–64. doi: 10.1111/j.0742-2822.2004.03005.x. [DOI] [PubMed] [Google Scholar]
- 51.Srivathsan K, Lee RW. Swallow syncope. Pacing Clin Electrophysiol. 2003;26(3):781–782. doi: 10.1046/j.1460-9592.2003.00135_26_3.x. [DOI] [PubMed] [Google Scholar]
- 52.Maekawa T, et al. Unusual swallow syncope caused by huge hiatal hernia. Intern Med. 2002;41(3):199–201. doi: 10.2169/internalmedicine.41.199. [DOI] [PubMed] [Google Scholar]
- 53.Gordon J, et al. Swallow syncope associated with paroxysmal atrial fibrillation. Eur J Cardiothorac Surg. 2002;21(3):587–590. doi: 10.1016/S1010-7940(01)01172-1. [DOI] [PubMed] [Google Scholar]
- 54.Shirayama T, et al. Swallowing syncope: complex mechanisms of the reflex. Intern Med. 2002;41(3):207–210. doi: 10.2169/internalmedicine.41.207. [DOI] [PubMed] [Google Scholar]
- 55.Magadle R, et al. Recurrent deglutition syncope. Isr Med Assoc J. 2001;3(3):222–223. [PubMed] [Google Scholar]
- 56.Haumer M, et al. Transient swallow syncope during periods of hypoxia in a 67-year-old patient after self-extubation. Crit Care Med. 2000;28(5):1635–1637. doi: 10.1097/00003246-200005000-00064. [DOI] [PubMed] [Google Scholar]
- 57.Kakuchi H, Sato N, Kawamura Y. Swallow syncope associated with complete atrioventricular block and vasovagal syncope. Heart. 2000;83(6):702–704. doi: 10.1136/heart.83.6.702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Deguchi K, Mathias CJ. Continuous haemodynamic monitoring in an unusual case of swallow induced syncope. J Neurol Neurosurg Psychiatry. 1999;67(2):220–222. doi: 10.1136/jnnp.67.2.220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Olshansky B. A Pepsi challenge. N Engl J Med. 1999;340(25):2006. doi: 10.1056/NEJM199906243402517. [DOI] [PubMed] [Google Scholar]
- 60.Antonelli D, Rosenfeld T. Deglutition syncope associated with carotid sinus hypersensitivity. Pacing Clin Electrophysiol. 1997;20(9 Pt 1):2282–2283. doi: 10.1111/j.1540-8159.1997.tb04251.x. [DOI] [PubMed] [Google Scholar]
- 61.Bellorini M, et al. Recurrent syncope during deglutition. An uncommon form of sinusal dysfunction. Arch Mal Coeur Vaiss. 1992;85(7):1039–1041. [PubMed] [Google Scholar]
- 62.Shapira Y, Strasberg B, Ben-Gal T. Deglutition syncope with coexistent carotid sinus hypersensitivity. Chest. 1991;99(6):1541–1543. doi: 10.1378/chest.99.6.1541. [DOI] [PubMed] [Google Scholar]
- 63.Kunimoto S, et al. A case of swallow syncope induced by vagovagal reflex. Jpn J Med. 1990;29(2):199–202. doi: 10.2169/internalmedicine1962.29.199. [DOI] [PubMed] [Google Scholar]
- 64.Elam MP, et al. Swallow syncope associated with complete atrioventricular block: a case report and review of the literature. Mil Med. 1989;154(9):465–466. doi: 10.1093/milmed/154.9.465. [DOI] [PubMed] [Google Scholar]
- 65.Ausubel K, Gitler B. Swallow syncope in an otherwise healthy young man. Am Heart J. 1987;113(3):831–832. doi: 10.1016/0002-8703(87)90730-7. [DOI] [PubMed] [Google Scholar]
- 66.Nakano T, et al. Swallow syncope after aneurysmectomy of the thoracic aorta. Heart Vessel. 1987;3(1):42–46. doi: 10.1007/BF02073646. [DOI] [PubMed] [Google Scholar]
- 67.Nakagawa S, et al. A case of swallow syncope induced by vagotonic visceral reflex resulting in atrioventricular node suppression. J Electrocardiol. 1987;20(1):65–69. doi: 10.1016/0022-0736(87)90010-0. [DOI] [PubMed] [Google Scholar]
- 68.Guberman A, Catching J. Swallow syncope. Can J Neurol Sci. 1986;13(3):267–269. doi: 10.1017/S0317167100036416. [DOI] [PubMed] [Google Scholar]
- 69.Kadish AH, Wechsler L, Marchlinski FE. Swallowing syncope: observations in the absence of conduction system or esophageal disease. Am J Med. 1986;81(6):1098–1100. doi: 10.1016/0002-9343(86)90418-3. [DOI] [PubMed] [Google Scholar]
- 70.Golf S, Forfang K. Congenital swallowing-induced symptomatic heart block: a case report of a probably hereditary disorder. Pacing Clin Electrophysiol. 1986;9(4):602–605. doi: 10.1111/j.1540-8159.1986.tb06619.x. [DOI] [PubMed] [Google Scholar]
- 71.Armstrong PW, McMillan DG, Simon JB. Swallow syncope. Can Med Assoc J. 1985;132(11):1281–1284. [PMC free article] [PubMed] [Google Scholar]
- 72.Kunis RL, et al. Deglutition syncope and atrioventricular block selectively induced by hot food and liquid. Am J Cardiol. 1985;55(5):613. doi: 10.1016/0002-9149(85)90274-7. [DOI] [PubMed] [Google Scholar]
- 73.Drake CE, et al. Visually provoked complete atrioventricular block: an unusual form of deglutition syncope. Am J Cardiol. 1984;53(9):1408–1409. doi: 10.1016/0002-9149(84)90106-1. [DOI] [PubMed] [Google Scholar]
- 74.Bortolotti M, Cirignotta F, Labo G. Atrioventricular block induced by swallowing in a patient with diffuse esophageal spasm. Jama. 1982;248(18):2297–2299. doi: 10.1001/jama.1982.03330180057033. [DOI] [PubMed] [Google Scholar]
- 75.Golf S. Swallowing syncope. A case report. Acta Med Scand. 1977;201(6):585–586. [PubMed] [Google Scholar]
- 76.Waddington JK, et al. Letter: carcinoma of the oesophagus with “swallow syncope”. Br Med J. 1975;3(5977):232. doi: 10.1136/bmj.3.5977.232-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Wik B, Hillestad L. Deglutition syncope. Br Med J. 1975;3(5986):747. doi: 10.1136/bmj.3.5986.747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Alstrup P, Pedersen SA. A case of syncope on swallowing secondary to diffuse oesophageal spasm. Acta Med Scand. 1973;193(4):365–368. doi: 10.1111/j.0954-6820.1973.tb10594.x. [DOI] [PubMed] [Google Scholar]
- 79.Lichstein E, Chadda KD. Atrioventricular block produced by swallowing, with documentation by his bundle recordings. Am J Cardiol. 1972;29(4):561–563. doi: 10.1016/0002-9149(72)90450-X. [DOI] [PubMed] [Google Scholar]
- 80.Tolman KG, Ashworth WD. Syncope induced by dysphagia. Correction by esophageal dilatation. Am J Dig Dis. 1971;16(11):1026–1031. doi: 10.1007/BF02235016. [DOI] [PubMed] [Google Scholar]
- 81.Sapru RP, et al. Syncope on swallowing. Br Heart J. 1971;33(4):617–622. doi: 10.1136/hrt.33.4.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Ragaza EP, Rectra EH, Pardi MT. Intermittent complete heart block associated with swallowing as a complication of acute myocardial infarction. Am Heart J. 1970;79(3):396–400. doi: 10.1016/0002-8703(70)90427-8. [DOI] [PubMed] [Google Scholar]
- 83.Sapru R. An unusual cause of syncope. Proc R Soc Med. 1968;61(10):955–956. [PMC free article] [PubMed] [Google Scholar]
- 84.James AH. Cardiac syncope after swallowing. Lancet. 1958;1(7024):771–772. doi: 10.1016/S0140-6736(58)91578-2. [DOI] [PubMed] [Google Scholar]
- 85.Correll HL, Lindert MC. Vagovagal syncope; report of a case apparently induced by digitalization. Am Heart J. 1949;37(3):446–454. doi: 10.1016/0002-8703(49)91065-0. [DOI] [PubMed] [Google Scholar]
- 86.Howland RH. Vagus nerve stimulation. Curr Behav Neurosci Rep. 2014;1(2):64–73. doi: 10.1007/s40473-014-0010-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Steele CM, Miller AJ. Sensory input pathways and mechanisms in swallowing: a review. Dysphagia. 2010;25(4):323–333. doi: 10.1007/s00455-010-9301-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Benditt DG. Neurally mediated syncopal syndromes: pathophysiological concepts and clinical evaluation. Pacing Clin Electrophysiol. 1997;20(2 Pt 2):572–584. doi: 10.1111/j.1540-8159.1997.tb06211.x. [DOI] [PubMed] [Google Scholar]
- 89.Carey BJ, de Caestecker J, Panerai RB. More on deglutition syncope. N Engl J Med. 1999;341(17):1316–1317. doi: 10.1056/NEJM199910213411716. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed in the literature review are available from the corresponding author on reasonable request.