Abstract
Background
Risk stratification in patients with asymptomatic Brugada Syndrome is challenging, and despite recent advances, there is no clear evidence. The first‐degree atrioventricular block was hypothesized to be a predictor of arrhythmic events. Measurement of the PR interval and diagnosing atrioventricular block from surface ECG is easy, noninvasive, and cost‐effective. We aimed to assess the latest evidence on PR interval or first‐degree atrioventricular block and major arrhythmic events related to Brugada Syndrome.
Methods
We performed a comprehensive search in PubMed for “atrioventricular block” OR “PR interval” and “Brugada syndrome.” We included studies that have a component of PR interval and/or first‐degree atrioventricular block and major arrhythmic events related to Brugada Syndrome including syncope/VT/VF/appropriate ICD shocks/ICD implantation.
Results
We included 1526 subjects from 7 studies. Pooled mean difference of PR interval in 4 studies showed a significant difference [MD 10.77 ms (2.97‐18.57) P = 0.007, moderate‐high heterogeneity I2 = 53% P = 0.08]. On sensitivity analysis by removing a study, it became MD 6.50 ms [1.97‐11.03], P = 0.005, heterogeneity I2 = 0% P = 0.52. Indicating that PR interval was prolonged by small margin. Pooled analysis of the association between a first‐degree atrioventricular block and major arrhythmic events was significant [OR 3.33 (2.02‐5.50) P < 0.001, low heterogeneity I2 = 0% P = 0.57].
Conclusion
First‐degree AV block is associated with more frequent major arrhythmic events in Brugada syndrome patients. PR interval seemed to be prolonged but is yet to be determined whether the PR interval association is still significant if it did not cross the first‐degree AVB threshold.
Keywords: atrioventricular block, Brugada syndrome, major arrhythmic event, PR interval, ventricular tachycardia/fibrillation
1. INTRODUCTION
Brugada syndrome is an autosomal dominant genetic disorder with a variable expression which is characterized by abnormal findings on the electrocardiograms. This finding typically consists of a pseudo right bundle branch block and ST elevation on lead V1 to V2. These alterations in electrocardiogram (ECG) findings are linked to SCN5A sodium channel mutation in the right ventricle outflow tract.1, 2
Currently, risk stratification Brugada patients rely on the morphology type of Brugada syndrome in ECG (type 1 vs 2) and history of sudden cardiac death or syncopes, with arrhythmia related syncope being the most significant risk factor. Patients with a type 1 ECG pattern and a history of syncope has a significantly higher risk of sudden cardiac death, implementation of Implantable cardiac defibrillator are warranted in this patients. However, these measures do not directly translate into a risk predictor for patients who are asymptomatic.3, 4
First‐degree atrioventricular (AV) block was hypothesized to be a predictor of arrhythmic events. Measurement of the PR interval and diagnosing atrioventricular block from surface ECG is easy, noninvasive, and cost‐effective. This meta‐analysis aims to analyze the relation of PR prolongation and AV block to major arrhythmic events in asymptomatic patients with Brugada syndrome. The authors believed this article would contribute positively to the advances of risk stratification in Brugada syndrome patients by providing a noninvasive, affordable, and widely available means of risk stratification.
2. METHODS
2.1. Search strategy
We performed a comprehensive search on studies that assess the association between prolonged PR interval and first‐atrioventricular degree block with major arrhythmic events in Brugada syndrome patients from studies published until January 2019. We searched [“atrioventricular block” OR “PR interval” and “Brugada syndrome”] and its synonyms using PubMed, EuropePMC, EBSCOhost, Cochrane Central Database, ClinicalTrials.gov, and snowballing from potential articles cited by other studies.
The association between prolonged PR interval and first‐atrioventricular degree block with major arrhythmic events in Brugada syndrome patients from studies published since inception up until January 2019. A broad strategy to maximize the initial scope of research with keyword [“atrioventricular block” OR “PR interval” and “Brugada syndrome”] and its synonyms using PubMed, EuropePMC, EBSCOhost, Cochrane Central Database, ClinicalTrials.gov, and snowballing from potential articles cited by other studies. The records were then systematically evaluated using inclusion and exclusion criteria. Two researchers (H.D and V.C) independently performed an initial search, discrepancies were resolved by discussion. A Preferred Reporting Items for Systematic Reviews and Meta‐Analyses flowchart of the literature search strategy of studies investigating the association between prolonged PR interval and first‐atrioventricular degree block with major arrhythmic events in Brugada syndrome was presented in Figure 1.
Figure 1.
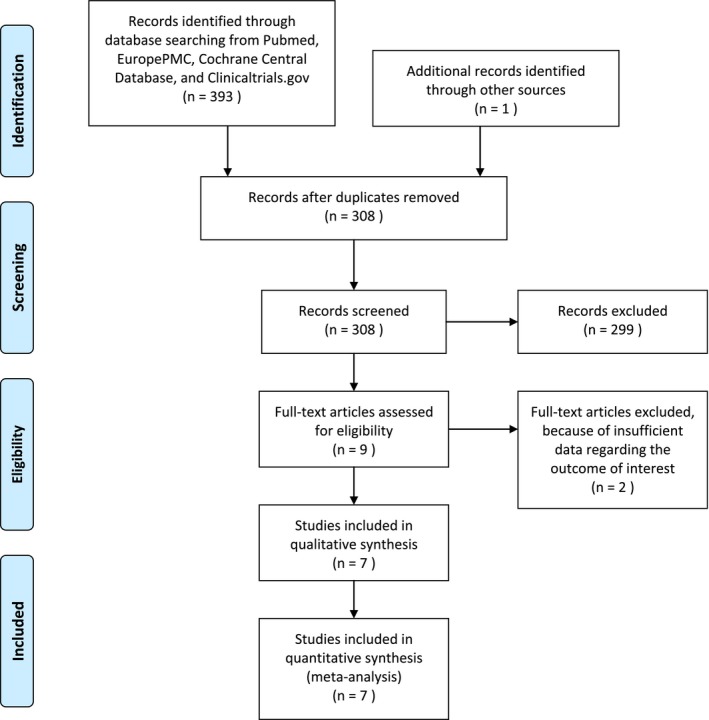
Study flow diagram
2.2. Selection criteria
The inclusion criteria for this study were all studies that assess the association between prolonged PR interval and first‐atrioventricular degree block with major arrhythmic events in Brugada syndrome patients. Major arrhythmic events were defined as syncope/VT/VF/appropriate ICD shocks/ICD implantation. Studies with insufficient data to assess the outcome of interest were excluded. We include all clinical researches/original articles and exclude case reports, review articles, and non‐English articles.
2.3. Data extraction
Data extraction and quality assessment were done by 2 independent authors (R.P and E.Y) using standardized extraction form which includes authors, year of publication, study design, sample size, prevalence of first‐atrioventricular degree block, major arrhythmic events, mean PR interval, and follow‐up period.
2.4. Statistical analysis
To perform the meta‐analysis, we used RevMan version 5.3 software (Cochrane Collaboration). We used the odds ratio (OR) and a 95% CI as a pooled measure for dichotomous data. We used mean difference (MD) and its standard deviation (DS) as a pooled measure for the continuous data. Inconsistency index (I2) test which ranges from 0% to 100% was used to assess heterogeneity across studies. A value above 50% or P < 0.05 indicates statistically significant heterogeneity. We used the Mantel‐Haenszel method (for OR), and the Inverse Variance method (for MD) with a fixed‐effect model for meta‐analysis and a random‐effect model was used in case of heterogeneity. All P values were 2‐tailed with a statistical significance set at 0.05 or below.
3. RESULTS
The search for studies that assess PR interval and/or first‐degree AV block and major arrhythmic events related to Brugada syndrome including syncope/VT/VF/appropriate ICD shocks/ICD implantation yielded a total of potential 393 articles. We removed 308 duplicates. We excluded 299 articles after screening the titles and abstracts. There were 9 potentially relevant articles. (Figure 1) We screened the full‐text articles, and after applying the inclusion criteria and exclusion criteria, 2 studies had insufficient data regarding the outcome of interest. We included 7 studies (6 cohorts and 1 case‐control) for qualitative synthesis (Table 1), and 7 studies were available for meta‐analysis. We included 1526 subjects from 7 studies.5, 6, 7, 8, 9, 10, 11
Table 1.
Summary of studies included in the systematic review
| Author | Study design | Sample size (n) | Measurement | 1st degree AVB prevalence | Outcome (major arrhythmic events) | Event [+]/event [−] | Mean PR intervalc (event [+]/event [−]) | Odds ratioc;95% CI; P‐value 1st degree AVB event [+]/event [−] | Follow‐up months |
|---|---|---|---|---|---|---|---|---|---|
| Corcia 2017 | Cohort | 95 | ECG | 16 (17%) | VT/VF/appropriate ICD shocks/ICD implantation | 24/71 | 181.6 ± 53.3/161.3 ± 30.5b | N/A | 33.8 |
| Corcia‐2 2017 | Cohort | 128 | ECG | 39 (30.5%) | VT/VF/appropriate ICD shocks | 40/88 | 181.35 ± 44.72/154.73 ± 29.64 | 3.42 (1.53‐7.64); 0.003 | 21 |
| Juntilla 2008 | Case‐Control | 200 | ECG | N/A | Syncope/VT/VF/appropriate ICD shocks | 66/134 | 181 ± 34/178 ± 39b | N/A | None |
| Maury 2013 | Cohort | 325 | ECG | 113 (35%) | Syncope/VT/VF/appropriate ICD shocks | 113/185 | N/A | 2.61 (1.16‐5.85); 0.02 | 48 |
| Migliore 2018 | Cohort | 272 | ECG | 45 (16.5%) | VT/VF/appropriate ICD shocks | 17/255 | N/A | 5.24 (1.90‐14.44); 0.001 | 85 |
| Morita 2018 | Cohort | 471 | ECG | 69 (14.64%)a | Syncope/VT/VF/appropriate ICD shocks | 145/326 | 180 ± 29/174 ± 26 | 1.34 (0.78‐2.28); 0.29a, b | 91 |
| Ohkubo 2011 | Cohort | 35 | ECG | N/A | Syncope/VT/VF | 10/25 | 178.9 ± 20/168 ± 19.6b | N/A | 84.5 |
Abbreviations: AVB, atrio‐ventricular block; ECG, 12‐lead electrocardiogram; N/A, not applicable/available; VF, ventricular fibrillation; VT, ventricular tachycardia; ICD, implantable cardioverter defibrillator.
Morita et al did not specify the type of atrioventricular block; it might not be first‐degree.
Not statistically significant (P > 0.05).
Calculated using RevMan 5.3.
3.1. PR interval and major arrhythmic events
Five studies reported the mean ± SD of PR interval in groups with and without major arrhythmic events. Corcia et al (2 studies) and Morita et al showed a longer PR interval in patients with major arrhythmic events.7, 9, 10 Juntilla et al, Ohkubo et al, and Corcia et al demonstrated that although the mean PR interval seemed to be higher, there was no significant difference in mean PR interval in Brugada syndrome patients with or without major arrhythmic events.8, 11 On meta‐analysis, the pooled mean difference of PR interval in 4 studies showed a significant difference [MD 10.77 ms (2.97‐18.57), P = 0.007, moderate‐high heterogeneity I2=53% P = 0.08]. (Figure 2A) Two remaining studies did not contain sufficient data about the mean PR interval. Upon sensitivity analysis by removing 1 study at a time, we found that a removal of Corcia‐2 et al study resulted in MD 6.50 ms [1.97‐11.03], P = 0.005, heterogeneity I2 = 0% P = 0.52. (Figure 2B).
Figure 2.
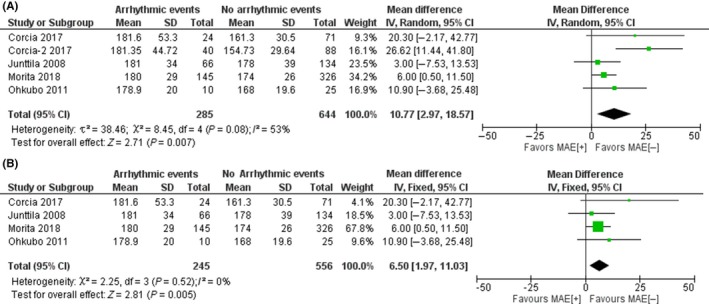
Pooled mean difference of PR interval and major arrhythmic events. Figure A shows a pooled mean difference (milliseconds) of PR interval and major arrhythmic events, PR interval is longer in those with MAE. Figure B shows that upon removal of Corcia‐2 et al. study upon sensitivity analysis, the heterogeneity became 0% with a longer pooled PR interval in those with MAE. Description: AVB = Atrioventricular Block; CI = Confidence Interval; IV = Inverse Variance; MAE = Major Arrhythmic Events; SD = Standard Deviation
3.2. First‐degree atrioventricular block and major arrhythmic events
Three studies reported the association between first‐degree AV and the major arrhythmic outcome. Corcia et al reported an odds ratio (OR) of 3.42 95% CI (1.53‐7.64); P = 0.003.10 Maury et al reported OR of 2.61 (1.16‐5.85); P = 0.02.5 Migliore et al demonstrated an OR of 5.24 (1.90‐14.44); P = 0.001. Morita et al study did not specify the type of AV block in his study, he reported that atrioventricular block was not associated with major arrhythmic outcome and is excluded from this section of meta‐analysis. Three remaining studies did not contain sufficient data about atrioventricular block.7
Pooled analysis of the association between first‐degree AV block and major arrhythmic events was significant [OR 3.33 (2.02‐5.50) P < 0.001, low heterogeneity I2 = 0% P = 0.57]. (Figure 3).
Figure 3.
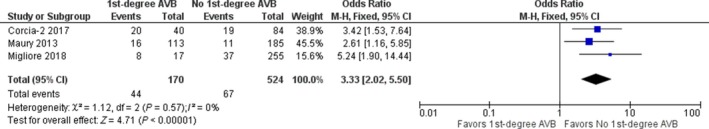
Pooled analysis of first‐atrioventricular degree block and major arrhythmic events. Forest‐Plot showing pooled analysis of first‐atrioventricular degree block and major arrhythmic events, incidence of major arrhythmic events was more frequent in those with 1st‐degree AVB. Description: AVB = Atrioventricular Block; CI = Confidence Interval; M‐H = Mantel‐Haenszel
4. DISCUSSION
Our study demonstrated that First‐degree AV block could be used to predict major arrhythmic events with OR of 3.33 (2.02‐5.50) and low heterogeneity from 3 studies with pooled 694 participants and 111 of them have major arrhythmic events. Our analysis showed that PR interval is longer MD 10.77 ms (2.97‐18.57) and moderate‐high heterogeneity; heterogeneity was reduced to 0% upon removal of Corcia‐2 et al study. Six studies are cohort, and 1 study is a case‐control, hence the latter study by Juntilla et al did not include the patient's follow‐up.11 Prevalence of first‐degree AVB is highest in Maury et al (35%) then Corcia et al (30.5% and 17%), Migliore et al (16.5%), and Morita et al (14.64%).5, 6, 10 The limitation of the studies was that most of the studies also assessed those who undergone provocative testing using sodium‐channel blocker which may cause prolongation of the PR interval. Migliore et al demonstrated the largest OR with first‐degree AVB compared to the other studies, Migliore assessed basal ECG without provocative testing in all of the subjects.6 This might explain that possibly AVB on basal ECG in the absence of provocative testing is a more powerful predictor. However, these studies did not assess the incidence of first‐degree AVB and magnitude of PR prolongation after provocative tests. Migliore et al have one of the smallest populations with AVB prevalence by percentage measurement, although the absolute count is similar to 2 studies by Corcia et al. The sample size and the number of events occurred were also limited, this is due to low prevalence of Brugada syndrome. One of the studies did not report follow‐up, and the others reported varying follow up length.
Among the studies with sufficient data to calculate the OR of first‐degree AVB and major arrhythmic outcome, all studies are significant with a heterogeneity of 0%.7 Study by Maury et al and Migliore et al showed that first‐degree AVB was an independent predictor of major arrhythmic outcome.5, 6 Corcia et al stated that first‐degree AVB but not SCN5A is an independent predictor in patients with Brugada syndrome ≤25 years old at the time of diagnosis.10 This study also assessed the most significant difference in PR interval in those experiencing major arrhythmic events. Morita et al and Juntilla et al also reported no association of SCN5A and the major arrhythmic events. A meta‐analysis by Rattanawong et al demonstrated an increased risk of major arrhythmic events in the Asian population, but not in the meta‐analysis by Raharjo et al who demonstrated no difference in ventricular fibrillation or syncope in their study.12, 13 Maury et al and Yamagata et al reported a higher mean PR interval and prevalence of first‐degree AVB in patients with SCN5A (+) which possibly means that there is a possible relation of SCN5A with first‐degree AVB.5, 14 Maury et al also demonstrated that first‐degree AVB is an independent predictor and SCN5A loss its significance after adjustment.5 Other studies did not assess the association between SCN5A and first‐degree AVB. Maury et al have the highest percentage, and absolute count of first‐degree AVB (there is also no other type of AV blocks in the study) prevalence in their study and their result might be likely reproducible. Future studies may explore the underlying mechanism of SCN5A association with major arrhythmic events, which may be due to other conduction abnormalities such as AVB or whether AVB is related to another mechanism causing an increased major arrhythmic event. Other ECG parameter that was hypothesized to be related to MAE includes QRS duration, fragmented QRS, QTc interval, and Tpeak‐Tend interval.14, 15, 16 However, studies investigating these parameters showed mixed results and high heterogeneity unlike the first‐degree AV block which is associated with MAE in all of the studies. QRS duration, QTc interval, Tpeak‐Tend interval, and Tp‐e dispersion may have different cut‐off points which may limit its practical application and fragmented QRS had a heterogeneity >50%. QRS duration and QTc interval were also shown to be related with SCN5A (+) and major arrhythmic events in several studies.14, 16
Only a study by Corcia‐2 et al individually showed a significant association between a longer PR interval and major arrhythmic outcome, this cause heterogeneity in the pooled PR interval analysis.10 This might be due to only their study specifies first‐degree AVB and their prevalence among other studies in the meta‐analysis of mean difference in PR interval. Hence, we did not know the prevalence of first‐degree AVB in the other 4 studies which might be smaller and reduces the difference in mean PR interval. Corcia et al only included those ≤25 years old at the time of diagnosis and is the cause of heterogeneity in pooled analysis of PR interval. Nevertheless, the pooled mean difference of PR interval was significant although by only small margin. Morita et al also reported a slightly higher mean PR interval in groups with the arrhythmic outcome; however, this value might change if only first‐degree AV block is included in the analysis. The other 3 studies reported that although the mean PR interval tends to be higher in groups with major arrhythmic outcome, they are not statistically significant. Possible causes include prolonged PR interval itself is not associated with major arrhythmic outcome unless it crosses the threshold for first‐degree AV block or the sample size is too small.
The limitation of this systematic review includes the small pooled number of events due to the scarcity of the study. Many of the studies investigating Brugada syndrome and the major arrhythmic outcome did not take account of the PR interval and first‐degree AV block. This is also possible that mean PR interval was not significantly different in these studies and the researchers were not interested in displaying their papers. Some of the studies included in our systematic review did not report either the first‐degree AVB or the mean PR interval of their subjects. Unfortunately, these studies reported PR interval and first‐degree AV block of both asymptomatic and symptomatic patients as a whole; it is not possible to obtain PR interval and first‐degree AV block data on the subgroup of patients that was symptomatic or asymptomatic on initial presentation. These authors presumably avoided subgroup analysis due to small number of events. Hence, we cannot measure the significance of PR interval and first‐degree AV block on these specific subgroups. We encourage further studies that assess PR interval, the status of AV block, and status of SCN5A gene mutation when investigating the ECG predictors of major arrhythmic events in Brugada syndrome. We also encourage subgroup analysis based on symptomatic or asymptomatic during initial presentation and their subsequent follow‐up.
5. CONCLUSION
First‐degree AV block is associated with more frequent major arrhythmic events in Brugada syndrome patients. PR interval seemed to be prolonged in those who experienced major arrhythmic events but is yet to be determined whether PR interval itself is associated with major arrhythmic outcome or only significant when it crosses the threshold for the diagnosis of first‐degree AV block. Presence of first‐degree AV block might be associated with SCN5A mutation although more research is needed.
CONFLICT OF INTEREST
The authors declare no conflict of interests for this article.
AUTHORS' CONTRIBUTION
Raymond Pranata conceived and designed the study and drafted the manuscript. Hadrian Deka and Veresa Chintya acquired the data and drafted the manuscript. Raymond Pranata and Emir Yonas interpreted the data. Sunu Budhi Raharjo performed extensive research and critically revise the manuscript. All authors contributed to the writing of manuscript. Raymond Pranata analyzed the data statistically.
ACKNOWLEDGEMENT
None.
Pranata R, Yonas E, Chintya V, Deka H, Raharjo SB. Association between PR Interval, First‐degree atrioventricular block and major arrhythmic events in patients with Brugada syndrome – Systematic review and meta‐analysis. J Arrhythmia. 2019;35:584–590. 10.1002/joa3.12188
REFERENCES
- 1. Brugada P, Brugada J. Right bundle branch block, persistent ST segment elevation and sudden cardiac death: a distinct clinical and electrocardiographic syndrome. A multicenter report. J Am Coll Cardiol. 1992;20(6):1391–6. http://www.ncbi.nlm.nih.gov/pubmed/1309182 [DOI] [PubMed] [Google Scholar]
- 2. Alings M, Wilde A. “Brugada” syndrome: clinical data and suggested pathophysiological mechanism. Circulation. 1999;99(5):666–73. http://www.ncbi.nlm.nih.gov/pubmed/9950665 [DOI] [PubMed] [Google Scholar]
- 3. Al‐Khatib SM, Stevenson WG, Ackerman MJ, et al. 2017 AHA/ACC/HRS guideline for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: executive summary. Circulation. 2018;138(13):e210–e271. 10.1161/CIR.0000000000000548 [DOI] [PubMed] [Google Scholar]
- 4. Priori SG, Wilde AA, Horie M, et al. Executive summary: HRS/EHRA/APHRS expert consensus statement on the diagnosis and management of patients with inherited primary arrhythmia syndromes. EP Eur. 2013;15(10):1389–406. 10.1093/europace/eut272 [DOI] [PubMed] [Google Scholar]
- 5. Maury P, Rollin A, Sacher F, et al. Prevalence and prognostic role of various conduction disturbances in patients with the Brugada syndrome. Am J Cardiol. 2013;112(9):1384–9. 10.1016/j.amjcard.2013.06.033 [DOI] [PubMed] [Google Scholar]
- 6. Migliore F, Testolina M, Zorzi A, et al. First‐degree atrioventricular block on basal electrocardiogram predicts future arrhythmic events in patients with Brugada syndrome: a long‐term follow‐up study from the Veneto region of Northeastern Italy. EP Eur. 2018;21(July);1–10. 10.1093/europace/euy144 [DOI] [PubMed] [Google Scholar]
- 7. Morita H, Watanabe A, Kawada S, et al. Identification of electrocardiographic risk markers for the initial and recurrent episodes of ventricular fibrillation in patients with Brugada syndrome. J Cardiovasc Electrophysiol. 2018;29(1):107–14. 10.1111/jce.13349 [DOI] [PubMed] [Google Scholar]
- 8. Ohkubo K, Watanabe I, Okumura Y, et al. Prolonged QRS duration in lead V2 and risk of life‐threatening ventricular arrhythmia in patients with brugada syndrome. Int Heart J. 2011;52(2):98–102. 10.1536/ihj.52.98 [DOI] [PubMed] [Google Scholar]
- 9. Gonzalez Corcia MC, Sieira J, Pappaert G, et al. A clinical score model to predict lethal events in young patients (≤19 years) with the Brugada syndrome. Am J Cardiol. 2017;120(5):797–802. 10.1016/j.amjcard.2017.05.056 [DOI] [PubMed] [Google Scholar]
- 10. Gonzalez Corcia MC, Sieira J, Sarkozy A, et al. Brugada syndrome in the young: an assessment of risk factors predicting future events. Europace. 2017;19(11):1864–73. 10.1093/europace/euw206 [DOI] [PubMed] [Google Scholar]
- 11. Junttila MJ, Brugada P, Hong K, et al. Differences in 12‐lead electrocardiogram between symptomatic and asymptomatic Brugada syndrome patients. J Cardiovasc Electrophysiol. 2008;19(4):380–3. 10.1111/j.1540-8167.2007.01050.x [DOI] [PubMed] [Google Scholar]
- 12. Rattanawong P, Chenbhanich J, Mekraksakit P, et al. SCN5A mutation status increases the risk of major arrhythmic events in Asian populations with Brugada syndrome: systematic review and meta‐analysis. Ann Noninvasive Electrocardiol. 2019;24(1):e12589 10.1111/anec.12589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Raharjo SB, Maulana R, Maghfirah I, et al. SCN5A gene mutations and the risk of ventricular fibrillation and syncope in Brugada syndrome patients: a meta‐analysis. J Arrhythmia. 2018;34(5):473–7. 10.1002/joa3.12097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Yamagata K, Horie M, Aiba T, et al. Genotype‐phenotype correlation of SCN5A mutation for the clinical and electrocardiographic characteristics of probands with Brugada syndrome. Circulation. 2017;135(23):2255–70. 10.1161/CIRCULATIONAHA.117.027983 [DOI] [PubMed] [Google Scholar]
- 15. Rattanawong P, Riangwiwat T, Prasitlumkum N, et al. Baseline fragmented QRS increases the risk of major arrhythmic events in Brugada syndrome: systematic review and meta‐analysis. Ann Noninvasive Electrocardiol. 2018;23(2):e12507 10.1111/anec.12507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Pranata R. Brugada syndrome: a brief review on diagnostic approach, risk stratification, and management. Int J Cardiovasc Acad. 2019;5(1):1 10.4103/IJCA.IJCA_31_18 [DOI] [Google Scholar]


