Abstract
Background: Breast cancer–related lymphedema (BCRL) is hard to control. Management may include lymphatic drainage, skin care, bandaging, or even surgery. Since acupuncture has been proven to affect the neurophysiology and neuroendocrine systems, it has the potential to control BCRL. Aim: To evaluate the effect of acupuncture in BCRL in randomized controlled trials. Design: A literature search was performed, following the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statement and without language restrictions. Data Sources: Five databases were searched from inception tthrough September 2018. Only studies that fulfilled the eligibility criteria of evaluating the effect of acupuncture on lymphedema in breast cancer were included. The methodological quality of these trials was assessed using the Cochrane criteria, and meta-analysis software (RevMan 5.3) was used for analysis. Results: We examined 178 breast cancer patients from 6 trials. All included randomized controlled trials had medium to high quality, based on the modified Jadad scale. The systematic review showed that acupuncture is safe and has a trend to improve symptoms, but trials did not consistently measure outcomes. The meta-analysis showed that acupuncture produced no significant improvement in the extent of lymphedema as compared with the control intervention (−1.90; 95% confidence interval = −5.39 to 1.59, P = .29). None of the studies reported severe adverse events. Conclusions: Acupuncture is safe and has a trend to improve the lymphedema related to breast cancer, yet it did not significantly change arm circumference in BCRL. Future studies should include both subjective and objective measurements and large-scale studies are warranted.
Keywords: breast cancer–related lymphedema, acupuncture, controlled clinical trials, randomized, systematic review
Introduction
Lymphedema is a term for lymphatic load that exceeds the transport capacity of the lymphatic system, causing filtered fluid to accumulate in the interstitium.1 Lymphedema may occur as a result of a primary lymphatic duct obstruction or secondary to treatment. Many breast cancer patients suffer from this troubling sign due to either obstruction of the lymphatic channels or lymph nodes, infiltration with tumor cells (lymphangitic carcinomatosis) or secondary to surgical removal of lymph nodes (lymphadenectomy) and radiation therapy.2 The incidence of lymphedema related to breast cancer ranges from 13.5% to 41.2% and increases with the number of lymph nodes removed.3,4 Axillary dissection, chemotherapy, radiation, and obesity will significantly increase its severity. Patients may also experience substantial functional impairment, psychological morbidity, and diminished quality of life.5
Since lymphedema is essentially incurable, many patients ask for complementary therapy beyond diuretics use and treatment of the underlying disease. From the research, up to 60% to 80% of those with breast cancer turn to complementary therapies. Types of complementary and alternative medicine therapy include low laser therapy,6,7 vitamin E supplements, yoga,8 acupuncture, and meditation.9 However, the efficacy of these is uncertain. Among these complementary therapies, acupuncture has been recognized as having much more evidence-based support, yet some physicians still question its efficacy and the increased risk of infection.
Acupuncture, in the real world, is widely used by breast cancer patients to improve symptoms such as pain, insomnia, joint pain, and the flushing related to hormone therapy.10,11 The mechanism by which acupuncture leads to physiological or clinical changes is still unclear, but traditional Chinese medicine (TCM) holds that it works through adjusting the neurophysiologic and neurohormonal activity that corresponds to regulating meridian energy (chi).12,13 Acupuncture has been postulated to affect the cardiovascular system via the autonomic nervous system to improve microvascular perfusion and the thermoregulation of the hands.14 Accordingly, acupuncture has been applied in edema based on the hypothesis that acupuncture increases the nitrous oxide level in treated regions and thereby increases local circulation.15 Acupuncture may also stimulate neuropeptides and hormones, including β-endorphin, serotonin, oxytocin, adrenocorticotropic hormone, gonadotropin-releasing hormone, and corticotrophin-releasing hormone, as well as having immunomodulation (anti-inflammation) and autonomic nerve activity.12 Despite the rationality of these arguments, it remains unclear whether acupuncture is effective in relieving the lymphedema associated with breast cancer. Therefore, we conducted this review and meta-analysis of the related trials to characterize the efficacy of acupuncture in treating breast cancer–related lymphedema (BCRL).
Methods
Data Sources and Search Strategy
The conduct of this systematic review adhered to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statement16,17 to ensure transparent and complete reporting. The structured search strategy was developed by an experienced librarian with retrieval from 5 databases (Embase, Ovid Medline, Cochrane CENTRAL, Scopus, and World Health Organization International Clinical Trials Registry Platform), with no language restrictions, from their inception dates to September 2018. Reference lists of eligible articles were also checked to identify additional studies.
The 2 key concepts used in the search, lymphedema and acupuncture, included their synonyms (32 free-text terms plus truncation symbols when appropriate) and controlled vocabulary (4 Emtree terms and 5 MeSH terms). We adopted Cochrane highly sensitive search filters to identify randomized controlled trials (RCTs).18 The complete search strategy is shown in Appendix 1 (available online).
Eligibility Criteria
All eligible studies examined women with breast cancer who were also diagnosed with lymphedema related to breast cancer. Only studies that used true needle acupuncture were enrolled; excluded were studies that adopted transcutaneous electrical nerve stimulation, laser acupuncture, acupressure, acupoints injection, or other acupoint stimulations such as moxibustion. For consistency, only studies that measured arm circumference were subjected to meta-analysis. Other results from different outcome measurements are presented in the article.
Study and Data Extraction
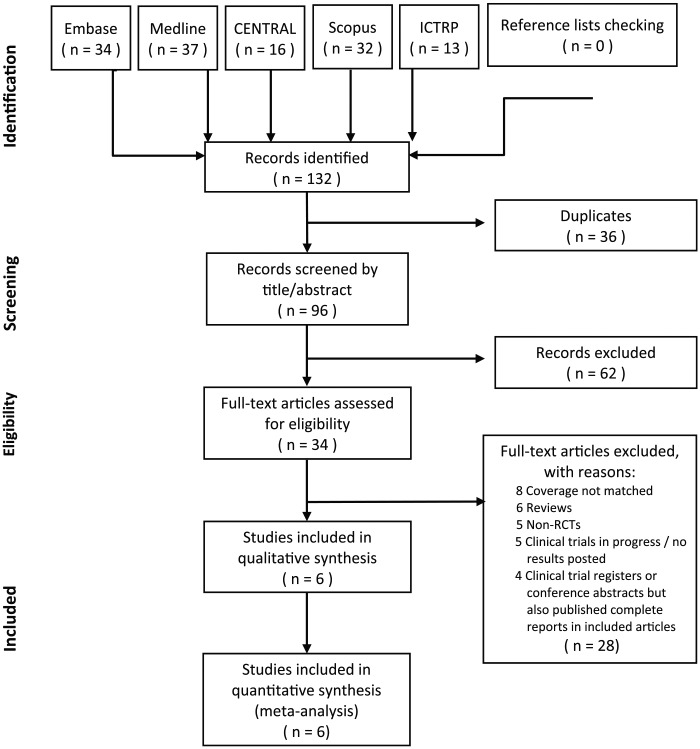
The searches of the 5 databases and additional sources led to the identification of 132 potentially relevant articles. The titles and abstracts that fulfilled the criteria of our study were independently reviewed by 2 reviewers (Chien and Liu), and the full texts of articles that met these criteria were obtained. Final decisions on inclusion were made after examination of the full articles. In cases of duplicate publications, the most recent and complete version was selected. Using these criteria, 126 of the 132 studies were excluded. Among the exclusions, 36 articles were duplicates, 62 titles/abstracts screened were not relevant, and 28 full-text articles assessed were “coverage not matched,” reviews, non-RCTs, clinical trials in progress, trial registers, or conference abstracts.
Six unique studies were ultimately included in the systematic review. Three studies were conducted in the United States: Bao et al19 and Cassileth et al20,21; 1 study was conducted in Austria: Smith et al22; and 2 studies were from Asia: one from China, Yao et al,23 and one from Korea, Jeong et al.24 Owing to the inconsistency of outcome measures, only 2 studies were included in the meta-analysis to evaluate arm circumference. The study selection flowchart is shown in Figure 1.
Figure 1.
Studies selection flowchart, which is based on PRISMA statement.
Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6:e1000100.
The Risk of Bias and Quality Assessment
The quality of each study was assessed independently by 2 reviewers, applying the criteria recommended in the Cochrane Handbook for Systematic Reviews of Interventions, version 5.1.0.25 We assessed 6 domains as follows: (1) generation of randomization, (2) allocation concealment, (3) blinding of participants and personnel, (4) blinding of outcome assessment, (5) incomplete outcome data, and (6) selective outcome reporting. The modified Jadad scale was used to evaluate the quality of the included studies.26,27
Statistical Analysis
To analyze the effects of acupuncture on outcomes (extent of lymphedema assessed using mean change in arm circumference between the affected and unaffected arms) after treatment compared with baseline, we estimated the weighted mean differences and 95% confidence intervals (CIs) from each study using Review Manager (RevMan) Version 5.3 for Windows (The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, Denmark). For weighted mean differences, a result of 0 reflected “no effect” and less than 0 favored the acupuncture intervention. Statistical heterogeneity was assessed by using χ2 test (P < .1). The I2 statistic was also calculated, and we considered I2 > 50% to indicate significant heterogeneity across studies.1 A random-effects model was used if significant heterogeneity was shown among trials. Otherwise, results were obtained from a fixed-effects model.
Results
Evaluation of Quality and Descriptions of the Included Trials
Table 1 shows the risk of bias in each of the 6 domains. Half of the studies were of high quality while half were categorized as being high risk due to lower level of evidence. The modified Jadad scale represents the quality of an RCT, and has a maximum of 5 points (1 point each for randomization, appropriate randomization method, describing dropouts, patient blinding, and assessor blinding).28 The 3 RCTs included in this systematic review were all of high quality; the others, albeit not RCTs, still have reference value as pilot studies in the emerging area of use of acupuncture in BCRL.
Table 1.
The Comparisons of the Characteristics of the Included Trials.
| Author (Year)/Trial Type | Sample Size/Control | Inclusion Criteria/Status About Lymphedema | Intervention (Primary Acupoints) | Course | Measurement Tools | Results |
|---|---|---|---|---|---|---|
| Bao et al19 (2018)/RCT | 73/wait-list | 1. Affected arm circumference >2 cm larger than the
unaffected arm in at least 1 of the 2 sites 2. The median duration of lymphedema was 2.5 years in experimental group (quartiles 1.4 and 3.4) and 2.2 years in the control group |
CV12 and CV3, and at bilateral TE14, LI15, LU5, LI4, ST36, and SP6 points | Twice weekly manual acupuncture for 6 weeks | Circumference and bioimpedance | 1. Compared lymphedematous arm versus unaffected
arm 2. No significant difference between the groups for arm circumference difference or bioimpedance difference |
| Yao et al23 (2016)/RCT | 30/diosmin 900 mg 3 times daily | 1. ≥3 cm circumference differences between the affected and
unaffected arms 2. Participants had met the clinical diagnostic criteria for between 6 months and 5 years |
30 minutes of acupuncture at 6 acupoints (Shousanli [LI.10], Quchi [LI.11], Binao [LI.14], Jianyu [LI.15], Waiguan [SJ.5], and Jianliao [SJ.14]) | Three times per week for 30 days | Arm circumference, QoL, clinical safety, and adverse events | 1. Compared lymphedematous arm versus unaffected
arm 2. BCRL improved by 51.46% in the experimental group and by 26.27% in the control group (P < .00001) |
| Jeong et al24 (2015)/pilot study | 9/nil | 1. ≥2 cm difference in a circumferential measurement of the
affected upper limb in comparison with the contralateral
limb 2. Clinical diagnosis of lymphedema for at least 6 months 3. Did not mention the duration postsurgery |
Saam acupuncture; the 5 Shu points | 3 times per week for 6 weeks | Stages of lymphedema, VAS, arm circumference, and QoL | 1. Compared lymphedematous arm versus the unaffected
arm 2. Reduction of lymphedema in VAS and circumferential measurements (P < .001) |
| Smith et al22 (2014)/a parallel randomized controlled feasibility study | 20/treatment as usual | 1. ≥10 cm segment by bioimpedance 2. Stable unilateral intransient lymphedema present for at least 6 months, no use of intensive therapy |
CV12, CV3, CV2; LI15, TE4, LU5, LI4, ST36, SP9, and SP6 | Twice weekly for 4 weeks then once weekly for 4 weeks; 8weeks | Extracellular fluid, lymphedema symptoms, well-being, and safety | 1. Compared pre- versus posttreatment 2. Acupuncture may stabilize symptoms yet no change in extracellular fluid or any patient-reported outcome measurement |
| Cassileth et al21 (2013)/pilot study | 37/nil | 1. ≥2 cm arm circumference differences between affected and
unaffected arms 2. Postsurgery 6 months to 5 years were included |
TE14, LI15, LU5, CV12, CV3, LI4, ST36, and SP6 | Twice weekly for 4 weeks | Arm circumference at 2 points | 1. Two-point circumference measurements of the affected and
unaffected arms were performed before and after each
treatment session 2. Mean reduction in arm circumference difference was 0.90 cm (95% CI = 0.72-1.07; P < .0005) |
| Cassileth et al20 (2011)/pilot study | 9/nil | 1. ≥2 cm arm circumference differences between the affected
and unaffected limbs 2. Clinical diagnosis of lymphedema for at least 6 months and no more than 5 years |
LI15, LI4, TE14, CV12, CV3, LU5, SP6, and ST36 | Twice a week for 4 weeks | Arm circumference (response was defined as at least a 30% reduction in the difference in size between the affected and unaffected arms after 4 weeks of treatment) | 1. Compared both the affected and unaffected limbs, before
and after each treatment 2. Acupuncture appears safe and may reduce lymphedema associated with breast cancer surgery |
Abbreviations: RCT, randomized controlled trial; QoL, quality of life; BCRL, breast cancer–related chronic lymphedema; VAS, Visual Analogue Scale; CI, confidence interval.
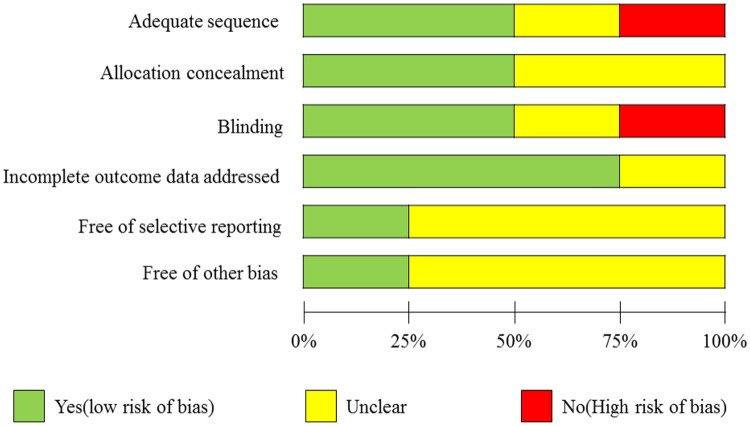
Figure 2 summarizes the risk of the included trials; 66% can be categorized as low risk. To be more complete, we also contacted authors to identify additional studies and asked them to provide methodological details when data were missing.
Figure 2.
The summary of risk od bias of the included trials.
The 6 prospective trials examined 169 patients with breast cancer (Table 2). The sample sizes ranged from 9 to 73 patients, and the average age was 58.3 years (range 41-79 years). The controlled treatments were wait-list, medication (diosmin), or current treatment; no sham acupuncture was applied in these trials to determine the placebo effect of acupuncture. However, most studies adopted objective measurements such as bioimpedance or change in arm circumference; some also measured symptoms by using a Visual Analogue Scale or quality of life assessment. The heterogeneity and limited number of studies may have contributed to some risk of bias. Because the included trials did not adopt a consistent outcome measurement, we could apply meta-analysis only to the 2 studies that measured change in arm circumference.
Table 2.
Risk of Bias in the Included Trialsa.
| Author (Year) | Randomization | Allocation Concealment | Patients Blinding | Assessor Blinding | Incomplete Outcome Data Addressed | Selective Outcome Reporting | Modified Jaded Scale |
|---|---|---|---|---|---|---|---|
| Bao et al19 (2018) | Low | Low | Low | Low | Low | Low | 5 |
| Yao et al23 (2016) | Low | Low | Low | Low | Low | Low | 5 |
| Jeong et al24 (2015) | High | Unclear | High | Unclear | Low | Low | 2 |
| Smith et al22 (2014) | Low | Low | Low | Low | Low | Low | 5 |
| Cassileth et al21 (2013) | High | Unclear | Unclear | Unclear | Low | Low | 2 |
| Cassileth et al20 (2011) | High | Unclear | Unclear | Unclear | Low | Low | 2 |
Modified Jadad Scale: Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17:1-12.
Effect of Acupuncture on the Extent of Lymphedema of BCRL
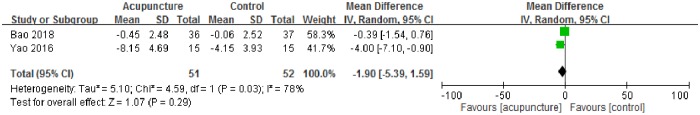
Due to the limited number of studies, we did not perform funnel plot analysis and publication bias cannot be excluded. We observed significant between-study heterogeneity in the effect of acupuncture on extent of lymphedema (change of arm circumference; I2 = 78%). For the 2 trials that reported the difference in arm circumference between the affected and unaffected arms, no significant improvement in extent of lymphedema was observed in subjects treated with acupuncture (−1.90; 95% CI =−5.39 to 1.59, P = .29; Figure 3) as compared with the control intervention.
Figure 3.
Effect of acupuncture on extent of lymphedema in acupuncture in breast cancer–related lymphedema (arm circumference).
Discussion
To date, BCRL remains an uncontrollable complication for breast cancer survivors and current treatments are suboptimal. For this reason, patients seek acupuncture or other complementary therapy for symptom relief. BCRL patients are not old and most are at Eastern Cooperative Oncology Group Performance Status 1 to 2. Lymphedema, therefore, represents a major obstacle to their ability to resume normal activities and to have improved quality of life. From the limited results of our study, we can only note that acupuncture is safe and probably has the effect of relieving lymphedema.
Consensus About How to Evaluate BCRL Severity
Many factors prevent firm conclusions at this time. First, the topic of acupuncture in BCRL is still new with few studies, only half with control arms. Second, there is no consensus on how to evaluate the severity of BCRL except for measuring arm circumference, the method adopted by most studies. Arm circumference is the most intuitive and measurable data to collect; nevertheless, there will be some bias in measuring in terms of the measure levels and timing. In this systematic review, we note that Bao et al23 chose bioimpedance between the affected and unaffected arms as an objective measurement. Bioimpedance, defined as the ability of biological tissue to impede an electric current, has been a reliable and accurate tool for documenting the presence of lymphedema since early 2000, with some studies even using it to detect subclinical BCRL before and after surgery.29 Although it is noninvasive, ways to interpret bioimpedance vary and bioimpedance has been applied in a wide range of clinical settings.25 Bioimpedance has been used clinically to estimate and evaluate body composition.30 Although only one study in our review adapted this method, it may be more widely used in the future to provide a more objective measure than arm circumference.
Symptom Measurement Beyond Arm Circumference
We note that the included trials did not consistently record the symptoms of BCRL. Each used different methods to monitor lymphedema-related symptoms. Smith et al24 chose the validated Lymphedema Symptom Intensity and Distress Survey–Arm and Trunk as a measurement,22 while Jeong et al24 used a Visual Analogue Scale to check symptoms. Yao et al23 used not only an effective index for upper-limb lymphedema but also the range of motion of the shoulder joint and quality of life as outcome measures. The distinct methods impeded meta-analysis. However, previous studies indicate that arm swelling may not be as important as the specific types of arm symptoms present, which may be more meaningful in terms of quality of life to survivors of breast cancer with lymphedema.31 Previous research has also indicated a significant correlation between symptoms and function.32 Likewise, Yao et al23 included the function assessment (shoulder range of motion) as an outcome measurement. However, it is important to recollect that using the presence of symptoms as a diagnostic indicator or prognosticator of lymphedema still has limitations.
Accordingly, in the study of BCRL, it is crucial to combine subjective symptomatic and quality of life self-reports with objective measures of the level of lymphedema, be they arm circumference, bioimpedance, or even water displacement.33 So far, no definite measurement exists to evaluate BCRL clinically. The methods most used were bioimpedance, water volumetry, tape measurement, and perometry, although only bioimpedance can detect alterations in the extracellular fluid from stage one lymphedema.34
Bias From Acupuncture Style
Another bias lies in the types of acupuncture used: warm acupuncture, saam acupuncture, manual (traditional) acupuncture, or even electro-acupuncture. Whether the adjunct stimulation, such as warm (moxibustion) or saam (Korean style), will affect outcomes is unknown. Each study design was distinct in the acupoints and practice intervals chosen; they agreed in that acupuncture was practiced based on the Meridian theory. According to TCM, BCRL is caused by meridian stagnation, with fluid retention beneath the upper arm skin because of injury at operation; through stimulation of the acupoints, the chi flows more smoothly along the meridians and thereby decreases the edema or inflammation reaction around the nearby tissue. Therefore, the style of acupuncture varied only in the amount of effect; the dredging of meridians was the same.
Heterogeneity From the Measurement of Lymphedema
Another bias lies in the fact that some studies compared the outcome (arm circumference) by comparing affected and unaffected arms in each subject, which is a between-arm design, while others chose within-arm analysis, which compares pre- versus posttreatment circumference for the affected arm only. This can lead to confusion in the description of studies. Since some studies were pilot studies, the true effect of acupuncture on BCRL is not completely confirmed in this systematic review because there are too few controlled studies. Furthermore, regarding the inclusion criteria for patients with lymphedema, since the interval after surgery is varied, most studies include patients suffering from lymphedema for at least 6 months but less than 5 years since it is debatable whether lymphedema is an acute effect. To this point, the studies that were included in the meta-analysis excluded acute-postoperative edema and thus are more convincing.
Why Choose Acupuncture in Dealing With BCRL
Although lymphedema is a devastating symptom of cancer, it has no cure. The goal of lymphedema therapy is to restore function, reduce physical and psychologic suffering, and prevent the development of infection. Current treatments include pharmacologic therapies, hygiene and skin care, physical therapy and compression, and palliative surgery. The benzopyrones (including coumarin and flavonoids), when combined with complex physical therapy, have been successful against the disease in a few studies. Diuretics are not effective in treating lymphedema. Physical therapy and compression, including special massage techniques and compression bandages, provides temporary relief. Palliative operations such as vascularized lymph node transfer and lymphaticovenular bypass surgery are the last choice of patients already suffering from operation-related lymphedema, since their efficacy is not guaranteed. Therefore, acupuncture, which can promote meridian circulation and metabolism in the region, is the most promising non-invasive treatment.35
The Potential of Acupuncture in BCRL
Previous research indicates that acupuncture can mediate the peripheral nervous system by increasing levels of various endogenous opioids, anti-inflammatory cytokines, and neuropeptides both systemically and locally.35 One study found that manual acupuncture produces a phenotypic switch in macrophages and increases interleukin (IL)-10 concentrations in muscle, reducing pain and inflammation.36 Others have shown reduced plasma levels of IL-1, IL-6, and tumor necrosis factor-α after acupuncture.37,38 The antioxidative and immune system regulation of acupuncture have been shown in edema, rheumatic arthritis, and menopause symptoms.11,39 On the other hand, from a TCM perspective, pain and swelling are due to stagnation of meridians; acupuncture, which promotes chi and circulation, will dredge the clots in blood vessels or lymph ducts, restoring the flow of meridians. It is difficult to interpret the meridian system in a Western medical form; yet, in our previous study, we demonstrated that the Yin-Yang theory of the meridian system is somehow compatible with the autonomic (vagal-sympathetic) nervous system.40,41 In this context, we can understand how acupuncture works to regulate cytokine activity and thereby affect the neuroendocrine and nervous systems, in turn, alleviating BCRL. The efficacy may not be obvious due to the experimental design or type of adjunct used with acupuncture, such as electrostimulation or warm stimulation or even laser stimulation; nevertheless, the ability of acupuncture to stimulate the meridian system is worthy of further large-scale investigation.
To our knowledge, this is the first systematic review of acupuncture in BCRL, although not only RCTs were included due to the limited number of clinical trials in this emerging area. From our review, we can only state the safety of acupuncture in BCRL with no side effects or infection reported. However, efficacy remains a matter of debate, since few patients were included in the meta-analysis. Even though acupuncture was shown to help reduce arm circumference in one individual study, the effect did not reach statistical significance in the meta-analysis. The extent of symptom improvement cannot be analyzed due to the variability between studies in the tools used to measure effects. To be more concise, further study is needed to achieve consensus in measuring the parameters germane to BCRL, no matter the objective measurement used or subjective symptoms and quality of life reported.
Limitations
This systematic review is the first to examine the role of acupuncture in BCRL; however, some limitations remain. First, not all studies were of high quality and some were not of RCT design. Second, the number of enrolled patients in each study was small. Third, variations between studies may have led to bias; these include use of different controls, treatment sessions, periods between treatments, acupoints, lymphedema status of patients, and blinding of test outcomes. Actually, since TCM does not advocate the use of a standardized, one-size-fits-all acupuncture regimen, standardization of results will always be an issue in this research. Last, this field lacks consensus about the measurement of lymphedema, which made concise meta-analysis problematic.
Conclusion
This systematic review of existent clinical trials demonstrates the safety of acupuncture in BCRL, yet the benefit in reducing arm circumference did not reach statistical significance and the effect on symptom relief is unknown due to the inconsistency of study design. The conduct of further large-scale RCTs is indicated. So far, the therapeutic effect of acupuncture on BCRL make it a low-cost, noninvasive part of lymphedema management.
Supplemental Material
Supplemental material, Appendix_1_Search_Strategy for The Effect of Acupuncture in Breast Cancer–Related Lymphoedema (BCRL): A Systematic Review and Meta-Analysis by Tsai-Ju Chien, Chia-Yu Liu and Ching-Ju Fang in Integrative Cancer Therapies
Acknowledgments
We thank all authors and participants in this study and the authors we have contacted who provided us with the information of their trials.
Footnotes
Authors’ Note: The datasets used for the current study are available on reasonable request from the corresponding author.
Author Contributions: Conception and design: Tsai-Ju Chien
Collection and assembly of data: Tsai-Ju Chien, Chia-Yu Liu, Ching-Ju Fang
Data analysis and interpretation: All authors
Manuscript writing: All authors
Final approval of manuscript: All authors
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was supported by grants from Ministry of Science and Technology 107-2635-B-010-002
ORCID iDs: Tsai-Ju Chien  https://orcid.org/0000-0001-9646-5272
https://orcid.org/0000-0001-9646-5272
Ching-Ju Fang  https://orcid.org/0000-0002-7892-8840
https://orcid.org/0000-0002-7892-8840
Supplemental Material: Supplemental material for this article is available online.
References
- 1. Smile TD, Tendulkar R, Schwarz G, et al. A review of treatment for breast cancer-related lymphedema: paradigms for clinical practice. Am J Clin Oncol. 2018;41:178-190. [DOI] [PubMed] [Google Scholar]
- 2. Nguyen TT, Hoskin TL, Habermann EB, Cheville AL, Boughey JC. Breast cancer-related lymphedema risk is related to multidisciplinary treatment and not surgery alone: results from a large cohort study. Ann Surg Oncol. 2017;24:2972-2980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Rebegea L, Firescu D, Dumitru M, Anghel R. The incidence and risk factors for occurrence of arm lymphedema after treatment of breast cancer. Chirurgia (Bucur). 2015;110:33-37. [PubMed] [Google Scholar]
- 4. Pereira ACPR, Koifman RJ, Bergmann A. Incidence and risk factors of lymphedema after breast cancer treatment: 10 years of follow-up. Breast. 2017;36:67-73. [DOI] [PubMed] [Google Scholar]
- 5. Tobin MB, Lacey HJ, Meyer L, Mortimer PS. The psychological morbidity of breast cancer-related arm swelling. Psychological morbidity of lymphoedema. Cancer. 1993;72:3248-3252. [DOI] [PubMed] [Google Scholar]
- 6. Baxter GD, Liu L, Tumilty S, Petrich S, Chapple C, Anders JJ; Laser Lymphedema Trial Team. Low level laser therapy for the management of breast cancer-related lymphedema: a randomized controlled feasibility study. Lasers Surg Med. 2018;50:924-932. [DOI] [PubMed] [Google Scholar]
- 7. Baxter GD, Liu L, Petrich S, et al. Low level laser therapy (photobiomodulation therapy) for breast cancer-related lymphedema: a systematic review. BMC Cancer. 2017;17:833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Mazor M, Lee JQ, Peled A, et al. The effect of yoga on arm volume, strength, and range of motion in women at risk for breast cancer-related lymphedema. J Altern Complement Med. 2018;24:154-160. [DOI] [PubMed] [Google Scholar]
- 9. Finnane A, Liu Y, Battistutta D, Janda M, Hayes SC. Lymphedema after breast or gynecological cancer: use and effectiveness of mainstream and complementary therapies. J Altern Complement Med. 2011;17:867-869. [DOI] [PubMed] [Google Scholar]
- 10. Chien TJ, Liu CY, Chang YF, Fang CJ, Hsu CH. Acupuncture for treating aromatase inhibitor-related arthralgia in breast cancer: a systematic review and meta-analysis. J Altern Complement Med. 2015;21:251-260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Chien TJ, Hsu CH, Liu CY, Fang CJ. Effect of acupuncture on hot flush and menopause symptoms in breast cancer—a systematic review and meta-analysis. PLoS One. 2017;12:e0180918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Yu JS, Zeng BY, Hsieh CL. Acupuncture stimulation and neuroendocrine regulation. Int Rev Neurobiol. 2013;111:125-140. [DOI] [PubMed] [Google Scholar]
- 13. Litscher G. Bioengineering assessment of acupuncture, part 6: monitoring—neurophysiology. Crit Rev Biomed Eng. 2007;35:1-36. [DOI] [PubMed] [Google Scholar]
- 14. Suter B, Kistler A. Does acupuncture modify skin circulation via the autonomic nervous system? [in German]. Schweiz Med Wochenschr Suppl. 1994;62:36-38. [PubMed] [Google Scholar]
- 15. Tsuchiya M, Sato EF, Inoue M, Asada A. Acupuncture enhances generation of nitric oxide and increases local circulation. Anesth Analg. 2007;104:301-307. [DOI] [PubMed] [Google Scholar]
- 16. Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6:e1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Higgins JPT, Green S. Cochrane handbook for systematic reviews of interventions version 5.1.0. http://handbook-5-1.cochrane.org/. Accessed July 15, 2019.
- 19. Bao T, Zhi WI, Vertosick EA, et al. Acupuncture for breast cancer-related lymphedema: a randomized controlled trial. Breast Cancer Res Treat. 2018;170:77-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Cassileth BR, Van Zee KJ, Chan Y, et al. A safety and efficacy pilot study of acupuncture for the treatment of chronic lymphoedema. Acupunct Med. 2011;29:170-172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Cassileth BR, Van Zee KJ, Yeung KS, et al. Acupuncture in the treatment of upper-limb lymphedema: results of a pilot study. Cancer. 2013;119:2455-2461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Smith CA, Pirotta M, Kilbreath S. A feasibility study to examine the role of acupuncture to reduce symptoms of lymphoedema after breast cancer: a randomised controlled trial. Acupunct Med. 2014;32:387-393. [DOI] [PubMed] [Google Scholar]
- 23. Yao C, Xu Y, Chen L, et al. Effects of warm acupuncture on breast cancer–related chronic lymphedema: a randomized controlled trial. Curr Oncol. 2016;23:e27-e34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Jeong YJ, Kwon HJ, Park YS, Kwon OC, Shin IH, Park SH. Treatment of lymphedema with Saam acupuncture in patients with breast cancer: a pilot study. Med Acupunct. 2015;27:206-215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Coroneos CJ, Wong FC, DeSnyder SM, Shaitelman SF, Schaverien MV. Correlation of L-Dex bioimpedance spectroscopy with limb volume and lymphatic function in lymphedema. Lymphat Res Biol. 2019;17:301-307. doi: 10.1089/lrb.2018.0028 [DOI] [PubMed] [Google Scholar]
- 26. Palys KE, Berger VW. A note on the Jadad score as an efficient tool for measuring trial quality. J Gastrointest Surg. 2013;17:1170-1171. [DOI] [PubMed] [Google Scholar]
- 27. Clark HD, Wells GA, Huet C, et al. Assessing the quality of randomized trials: reliability of the Jadad scale. Control Clin Trials. 1999;20:448-452. [DOI] [PubMed] [Google Scholar]
- 28. Berger VW. Is the Jadad score the proper evaluation of trials? J Rheumatol. 2006;33:1710-1712. [PubMed] [Google Scholar]
- 29. Kaufman DI, Shah C, Vicini FA, Rizzi M. Utilization of bioimpedance spectroscopy in the prevention of chronic breast cancer-related lymphedema. Breast Cancer Res Treat. 2017;166:809-815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Mialich MS, Martinez EZ, Jordao Junior AA. Application of body mass index adjusted for fat mass (BMIfat) obtained by bioelectrical impedance in adults. Nutr Hosp. 2014;30:417-424. [DOI] [PubMed] [Google Scholar]
- 31. Hormes JM, Bryan C, Lytle LA, et al. Impact of lymphedema and arm symptoms on quality of life in breast cancer survivors. Lymphology. 2010;43:1-13. [PubMed] [Google Scholar]
- 32. Hayes SC, Rye S, Battistutta D, Newman B. Prevalence of upper-body symptoms following breast cancer and its relationship with upper-body function and lymphedema. Lymphology. 2010;43:178-187. [PubMed] [Google Scholar]
- 33. Sagen A, Karesen R, Skaane P, Risberg MA. Validity for the simplified water displacement instrument to measure arm lymphedema as a result of breast cancer surgery. Arch Phys Med Rehabil. 2009;90:803-809. [DOI] [PubMed] [Google Scholar]
- 34. Hidding JT, Viehoff PB, Beurskens CH, van Laarhoven HW, Nijhuis-van der Sanden MW, van der Wees PJ. Measurement properties of instruments for measuring of lymphedema: systematic review. Phys Ther. 2016;96:1965-1981. [DOI] [PubMed] [Google Scholar]
- 35. Moffet HH. How might acupuncture work? A systematic review of physiologic rationales from clinical trials. BMC Complement Altern Med. 2006;6:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. da Silva MD, Bobinski F, Sato KL, Kolker SJ, Sluka KA, Santos AR. IL-10 cytokine released from M2 macrophages is crucial for analgesic and anti-inflammatory effects of acupuncture in a model of inflammatory muscle pain. Mol Neurobiol. 2015;51:19-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Jeong HJ, Hong SH, Nam YC, et al. The effect of acupuncture on proinflammatory cytokine production in patients with chronic headache: a preliminary report. Am J Chin Med. 2003;31:945-954. [DOI] [PubMed] [Google Scholar]
- 38. Cho SY, Yang SB, Shin HS, et al. Correction to: anti-inflammatory and immune regulatory effects of acupuncture after craniotomy: study protocol for a parallel-group randomized controlled trial. Trials. 2017;18:481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Xu Y, Hong S, Zhao X, et al. Acupuncture alleviates rheumatoid arthritis by immune-network modulation. Am J Chin Med. 2018;46:997-1019. [DOI] [PubMed] [Google Scholar]
- 40. Chien TJ, Liu CY, Ko PH, Hsu CH. A Chinese decoction, Kuan-Sin-Yin, improves autonomic function and cancer-related symptoms of metastatic colon cancer. Integr Cancer Ther. 2016;15:113-123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Chien TJ, Liu CY, Lu RH, Kuo CW, Lin YC, Hsu CH. Therapeutic efficacy of traditional Chinese medicine, “Kuan-Sin-Yin”, in patients undergoing chemotherapy for advanced colon cancer—a controlled trial. Complement Ther Med. 2016;29:204-212. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Appendix_1_Search_Strategy for The Effect of Acupuncture in Breast Cancer–Related Lymphoedema (BCRL): A Systematic Review and Meta-Analysis by Tsai-Ju Chien, Chia-Yu Liu and Ching-Ju Fang in Integrative Cancer Therapies