Abstract
Study Design:
Retrospective cohort study.
Objectives:
Examine pre- and postoperative outcomes between patients presenting with a central/paracentral versus a far lateral herniated nucleus pulposus (HNP) and assess whether significantly worse postoperative outcomes, assessed via patient self-reported survey, are associated with far lateral disc herniations.
Methods:
We performed a retrospective cohort analysis of patients who underwent primary lumbar decompression between January 2008 and December 2015. Groups were divided based on herniation type, central/paracentral or far lateral. Patients with 3 months, or longer, of follow-up were included. Variables analyzed included demographics, American Society of Anesthesiologists (ASA) Score, Charleston Comorbidity Index (CCI), Oswestry Disability Index (ODI) scores, Visual Analog Scales (VAS) scores for the back and leg, 12-Item Short Form Mental and Physical Survey (SF-12) scores, and Veterans RAND 12-Item Mental and Physical Survey (VR-12) scores.
Results:
A total of 100 patients met the inclusion criteria. Postoperative ODI scores for central/paracentral HNP were significantly lower compared to far lateral HNP. Patients with a far lateral disc herniation presented with significantly lower preoperative SF-12 and VR-12 scores. The improvement in ODI score from preoperative to final was significantly lower in the patients presenting with a far lateral HNP.
Conclusions:
Although patients with far lateral HNP present with worse preoperative outcome scores, they can expect similar symptom improvement to central or paracentral herniations following discectomy. This information can be used for future surgeons when weighing conservative versus surgical treatment of far lateral herniations.
Keywords: lumbar, far lateral, central, paracentral, herniated disc, nucleus pulposus
Introduction
Lumbar discectomy for the treatment of lumbar radiculopathy from nerve root compression is the most commonly performed neurosurgical procedure with more than 300 000 cases yearly in the United States.1,2 Lumbar disc herniation remains one of the main factors resulting in an estimated 80% of Americans experiencing low back pain during their lifetime. Lumbar disc herniations are often broadly classified based on their axial location, including central, paracentral, and far lateral.3,4
A far lateral herniated nucleus pulposus (HNP) represents anywhere from 0.7% to 11.7% of all lumbar disc protrusions.5 The clinical presentation of patients with far lateral disc herniations has subtleties that may distinguish them from central and paracentral herniations. Because far lateral lesions impinge on the nerve roots exiting at the same level of the herniation, more cephalad nerve root syndromes are observed as compared with central or paracentral herniations which compress the inferior root.6 Given the predisposition of far lateral HNP to directly compress the dorsal root ganglion, it may be surmised that far lateral HNP is associated with a worse postoperative course and outcome following lumbar discectomy compared with central/paracentral herniations.
Far lateral disc herniation is often associated with a more difficult surgical procedure as standard surgical approaches for more common lumbar herniations are not readily transferrable to far lateral variants because the lamina impedes access to the disc if a posterior approach is used.7 It follows that there is currently no consensus approach to surgical management. Current literature delves extensively into the various surgical approaches, management course, and outcomes of far lateral disc herniation.6-12 However, literature does not provide description of the comparative post-operative outcomes between those presenting with a far lateral HNP and those with a central or paracentral herniation. The goal of this study is to examine pre- and postoperative outcomes between patients presenting with a central/paracentral versus a far lateral HNP and assess whether significantly worse postoperative outcomes, assessed via patient-reported survey, are associated with far lateral disc herniation.
Methods
Patient Population
Following institutional review board (ORA# 16 251 619) approval, we retrospectively reviewed the records of consecutive patients who underwent a primary lumbar decompression between January 2008 and December 2015. All surgeries were performed by 1 of 2 senior orthopedic surgeons (HSA, EG) at a single quaternary referral medical center. Indication for surgery was radiculopathy and/or neurogenic claudication in the setting of failed conservative treatments. Patients were excluded from analysis if they were younger than 18 years at the time of surgery, if they had undergone a previous lumbar surgical procedure (decompression and/or fusion) or had follow-up less than 3 months. Groups were divided based on herniation type, central/paracentral or far lateral (Figure 1).
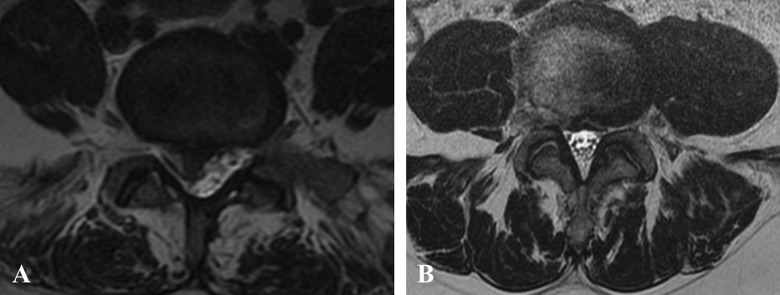
Figure 1.
Axial T2-weighted magnetic resonance imaging (MRI) slices of a paracentral/foraminal (A) and far lateral/extra-foraminal (B) herniated nucleus pulposus (HNP).
Surgical Procedure
Surgical procedures for both discs were carried out using a standard posterior approach. Following induction of general anesthesia, patients were positioned prone.
Central and Paracentral Disc Herniation
A midline incision was made and carried through the fascia. Cephalad and caudal dissection was performed subperiosteally and did not extend beyond the midpoint of the supra- and subjacent vertebrae. Care was taken to preserve target-level facet joints. A microscope was brought into the field for the decompression. A curette was used to separate the ligamentum flavum from the ventral surface of the lamina. A laminotomy was performed to allow for visualization of the traversing root and disc space. The thecal sac was then retracted to the contralateral side. A Penfield retractor was used to identify the disc space and annular defect. Once the defect was identified, disc fragments were removed. A nerve hook or Woodson were then used to mobilize any remaining disc material and deliver them to the annular defect. At the conclusion of our decompression, the nerve root was noted to be free and mobile.
Far Lateral Disc Herniation
A paramedian incision was used approximately 4 cm off the midline. This was localized to the appropriate level. A Wiltse approach to the spine was then used to access the lateral aspect of the facet joint and the transverse processes. Following radiographic confirmation of level, a microscope was used to complete the exposure of the intertransverse fascia. This fascia was divided to identify the nerve root. This is then traced back to the foramen; the lateral aspect of the facet was removed to improve visualization. The disc fragment was then identified and removed. Care was taken to avoid any excessive retraction of the nerve root and to avoid cautery around the dorsal root ganglion when possible.
Demographic and Outcome Measurements
Demographic information was collected for all patients that included age, sex, body mass index, diabetes, smoking status, and Charleston Comorbidity Index (CCI). Patient-reported outcomes were obtained in the form of Oswestry Disability Index (ODI) scores, Visual Analog Scales (VAS) scores for the back and leg, 12-Item Short Form Mental and Physical Survey (SF-12) scores, and the Veterans RAND 12-Item Health Mental and Physical Survey (VR-12) scores. Achievement of minimally clinically important difference (MCID) for VAS back, VAS leg, ODI, SF-12, and VR-12 were collected using threshold scores that have been previously established in literature: improvement in VAS back of 1.2, improvement in VAS leg of 1.71, improvement in ODI by 7.1%; improvement in SF-12 mental of 10.1; SF-12 physical in improvement of 2.52; improvement in VR-12 mental of 2.53, and improvement in VR-12 physical of 2.53.13-15 Duration of symptoms and reoperation rates were also collected.
Statistical Analysis
Baseline patient characteristics were compared using chi-squared analysis and independent-sample t tests for categorical and continuous data, respectively. Bivariate and multivariate regressions were subsequently used to compare clinical outcomes between procedure groups. Multivariate analyses controlled for differences in baseline patient characteristics, including duration of symptoms. Statistical significance was deemed as P ≤ .02 following Bonferroni correction for multiple statistical comparisons for each outcome.
Results
Overall, 100 patients who fulfilled our inclusion criteria were assessed. There were 85 patients who presented with a central or paracentral herniation, while 15 patients presented with a far lateral herniation (Table 1). For all patients included in the cohort, demographic variables, including age, gender, smoking history, diabetes (type I or type II), total number of spinal levels the herniation spanned, and duration of symptoms (months) were obtained. The American Society of Anesthesiologists Score (ASA) was also included. Statistically significant differences existed in patient age (48.79 ± 16.11 vs 46.92 ± 16.17 years, P = .01), and diabetes (9.41% vs 33.33%, P = .01).
Table 1.
Demographic Variables.
| Demographics | Central/Paracentral | Far Lateral | All Patients | P a |
|---|---|---|---|---|
| Overall, n | 85 | 15 | 100 | |
| Age, years, mean ± SD | 46.92 ± 16.17 | 59.4 ± 11.20 | 48.79 ± 16.11 | .005 |
| Female sex, % | 42.35 | 46.67 | 43.00 | .756 |
| Smoking, % | 5.88 | 6.67 | 6.00 | .906 |
| Diabetes (all), % | 9.41 | 33.33 | 13.00 | .011 |
| ASA score ≥3, % | 15.29 | 40.00 | 19.00 | .025 |
| BMI >30 kg/m2, % | 34.12 | 33.33 | 34.00 | .953 |
| No. of levels, % | .665 | |||
| 1 | 69.41 | 66.67 | 69.00 | |
| 2 | 28.24 | 26.67 | 28.00 | |
| 3 | 2.35 | 6.67 | 3.00 |
Abbreviations: ASA, American Society of Anesthesiologists; BMI, body mass index.
a Values in boldface indicate statistical significance (P ≤ .02).
Postoperatively, no statistically significant differences between the central/paracentral and far lateral groups were found in the following scores: VAS back (2.85 ± 2.65 vs 3.87 ± 3.33; P = .09), VAS leg (1.96 ± 2.56 vs 2.29 ± 3.33; P = .54), SF-12 mental (55.20 ± 8.38 vs 54.11 ± 12.70; P = .51), SF-12 physical (40.53 ± 13.34 vs 34.14 ± 16.82; P = .99), VR-12 mental (57.72 ± 10.92 vs 54.91 ± 12.14; P = .93), VR-12 physical (44.20 ± 13.93 vs 35.69 ± 16.44; P = .97). Postoperative ODI scores for the central/paracentral group were significantly lower compared with the far lateral group on bivariate and multivariate analysis (21.33 ± 18.93 vs 38.20 ± 20.05; P = .01). No significant difference in reoperation rates was found between central/paracentral and far lateral herniation cohorts (P = .05) (Table 2).
Table 2.
Comparing Clinical Outcomes and Reoperation Rates.a
| Bivariateb | Multivariateb | ||||||
|---|---|---|---|---|---|---|---|
| Central/Paracentral | Far Lateral | All Patients | β | P | β | P | |
| Preoperative | |||||||
| VAS back | 7.13 ± 3.21 | 7.72 ± 2.43 | 7.23 ± 3.07 | 0.59 | .628 | 0.63 | .660 |
| VAS leg | 6.64 ± 3.40 | 7.59 ± 1.71 | 6.81 ± 3.18 | 0.96 | .175 | 1.65 | .243 |
| ODI | 51.82 ± 18.81 | 47.57 ± 15.89 | 51.11 ± 18.29 | −4.26 | .529 | −8.19 | .274 |
| SF-12 mental | 55.08 ± 5.83 | 45.73 ± 16.04 | 52.74 ± 10.01 | −9.34 | .196 | −13.35 | .018 |
| SF-12 physical | 36.51 ± 10.39 | 24.75 ± 8.01 | 33.15 ± 11.04 | −11.76 | .008 | −8.60 | 0.137 |
| VR-12 mental | 57.02 ± 6.56 | 47.01 ± 13.58 | 53.81 ± 10.29 | −10.01 | .020 | −17.56 | .009 |
| VR-12 physical | 38.92 ± 11.82 | 25.86 ± 9.30 | 34.37 ± 12.53 | −13.06 | .013 | −9.42 | .366 |
| Postoperative | |||||||
| VAS back | 2.85 ± 2.65 | 3.87 ± 3.33 | 2.99 ± 2.74 | 1.02 | .334 | 1.93 | .094 |
| VAS leg | 1.96 ± 2.56 | 2.29 ± 3.33 | 2.01 ± 2.65 | 0.33 | .747 | 0.80 | .509 |
| ODI | 21.33 ± 18.93 | 38.20 ± 20.05 | 23.96 ± 19.93 | 16.87 | .013 | 20.50 | .006 |
| SF-12 mental | 55.20 ± 8.38 | 54.11 ± 12.70 | 54.91 ± 9.46 | −1.09 | .800 | 2.76 | .647 |
| SF-12 physical | 40.53 ± 13.34 | 34.14 ± 16.82 | 38.81 ± 14.30 | −6.39 | .322 | −0.15 | .985 |
| VR-12 mental | 57.72 ± 10.92 | 54.91 ± 12.14 | 56.83 ± 11.11 | −2.81 | .594 | 0.59 | .932 |
| VR-12 physical | 44.20 ± 13.93 | 35.69 ± 16.44 | 41.49 ± 14.94 | −8.51 | .222 | −0.05 | .977 |
| Reoperation | 12.94% | 20.00% | 14.00% | 1.68 | .468 | 7.93 | .048 |
Abbreviations: ODI, Oswestry Disability Index; SF-12, 12-Item Short Form Mental and Physical Survey; VAS, Visual Analog Scale; VR-12, Veterans RAND 12-Item Mental and Physical Survey.
aValues in boldface indicate statistical significance (P ≤ .02).
bCentral/Paracentral used as reference group.
On multivariate analysis, preoperative SF-12 mental (55.08 ± 5.83 vs 45.73 ± 16.04; P = .02) and VR-12 mental scores (57.02 ± 6.56 vs 47.01 ± 13.58; P = .01) were significant different between central/paracentral and far lateral patient groups. While on bivariate analysis, patients with a far lateral disc herniation presented with significantly lower preoperative SF-12 physical scores (36.51 ± 10.39 vs 24.75 ± 8.01; P = .01). Similarly, far lateral disc herniation presented with significantly lower preoperative VR-12 mental scores (57.02 ± 6.56 vs 47.01 ± 13.58; P = .02) and VR-12 physical scores (25.86 ± 9.30 vs 38.92 ± 11.82; P = .01). No statistically significant differences were found for preoperative VAS back, VAS leg, VR-12 physical, ODI scores, and SF-12 mental (Table 2).
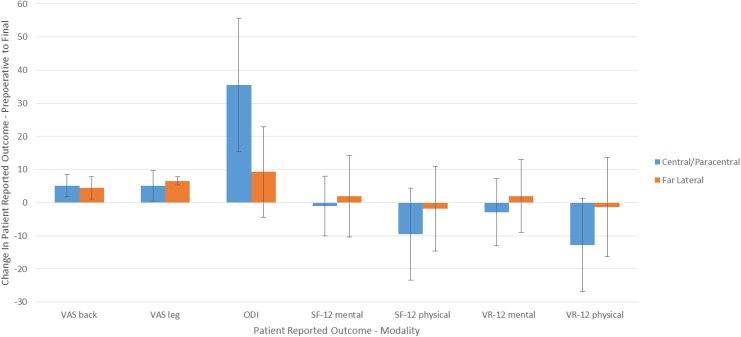
The improvement in ODI score from preoperative to final was significantly lower in the patients presenting with a far lateral disc herniation (35.53 ± 20.06 vs 9.26 ± 13.68; P = .01) (Table 3, Figure 2). No statistically significant changes in reported SF-12 and VR-12 scores were found from the preoperative to postoperative reported scores in both central/paracentral and far lateral herniations. No differences in achievement of MCID for VAS back, VAS leg, ODI SF-12, or VR-12 scores were found (Table 4).
Table 3.
Comparing Binary Clinical Outcomes.a
| Bivariateb | Multivariateb | ||||||
|---|---|---|---|---|---|---|---|
| Central/Paracentral | Far Lateral | All Patients | β | P | β | P | |
| Change preoperative to final | |||||||
| VAS back | 5.16 ± 3.28 | 4.47 ± 3.36 | 5.06 ± 3.26 | −6.98 | .633 | −0.05 | .977 |
| VAS leg | 5.09 ± 4.62 | 6.57 ± 1.22 | 5.30 ± 4.32 | 1.48 | .443 | 4.38 | .055 |
| ODI | 35.53 ± 20.06 | 9.26 ± 13.68 | 31.33 ± 25.25 | −26.27 | .001 | −24.50 | .010 |
| SF-12 mental | −1.04 ± 8.97 | 1.96 ± 12.26 | −0.375 ± 9.47 | 3.00 | .592 | −18.05 | .344 |
| SF-12 physical | −9.58 ± 13.88 | −1.81 ± 12.77 | 3.22 ± 13.68 | 7.77 | .331 | 11.86 | .612 |
| VR-12 mental | −2.86 ± 10.11 | 2.01 ± 10.92 | −1.56 ± 10.18 | 4.88 | .432 | −8.38 | .706 |
| VR-12 physical | −12.84 ± 14.01 | −1.41 ± 14.99 | −9.79 ± 14.69 | 11.43 | .192 | 27.19 | .195 |
Abbreviations: ODI, Oswestry Disability Index; SF-12, 12-Item Short Form Mental and Physical Survey; VAS, Visual Analog Scale; VR-12, Veterans RAND 12-Item Mental and Physical Survey.
aValues in boldface indicate statistical significance (P ≤ .02).
bCentral/Paracentral used as reference group.
Figure 2.
Change in clinical outcomes from preoperative to final.
Table 4.
Postoperative MCID Outcomes.
| Central/Paracentral (%) | Far Lateral (%) | P | |
|---|---|---|---|
| VAS back MCID | 92.94 | 86.67 | .344 |
| VAS leg MCID | 91.76 | 100.00 | .590 |
| ODI MCID | 100.00 | 93.33 | .150 |
| SF-12 mental MCID | 84.71 | 80.00 | .704 |
| SF-12 physical MCID | 85.88 | 86.67 | 1.000 |
| VR-12 mental MCID | 89.41 | 80.00 | .383 |
| VR-12 physical MCID | 88.24 | 86.67 | 1.000 |
Abbreviations: MCID, minimal clinically important difference; ODI, Oswestry Disability Index; SF-12, 12-Item Short Form Mental and Physical Survey; VAS, Visual Analog Scale; VR-12, Veterans RAND 12-Item Mental and Physical Survey.
VAS: Visual Analog Scales.
Discussion
Lumbar discectomy for treatment of lumbar radiculopathy remains one of the most common surgical procedures in the United States.1,2 The common place nature of this procedure makes it important to understand the outcomes expected after specific subtypes of lumbar disc herniation. While the natural course of paracentral and central disc herniations is well documented, less is known about outcomes following far lateral HNP. To our knowledge, this study represents the first study to compare outcomes of far lateral HNP to the more common central/paracentral HNP.
Our results suggest that patients with far lateral HNP have significantly higher levels of preoperative disability as measured by SF-12 mental and VR-12 mental scores. This is not surprising given that the far lateral HNP is anatomically predisposed to direct compression of the dorsal root ganglion, it may follow that far lateral HNP is associated with increased morbidity and post-surgical outcomes.16
Patients with far lateral HNP recorded significantly higher postoperative ODI scores, and patient recorded ODI scores reflected a significantly lower improvement in patients with far lateral HNP. While this contradicts our data found relative to the other scoring methodologies (VR-12 and SF-12), this may be explained by the mechanism of herniation. While improvement was undoubtedly realized for patients with far lateral herniation per their ODI scores, the difference in MCID ODI between the central or paracentral cohort and far lateral cohort was not found to be statistically significant. This lack of difference demonstrates that an improvement of 9 points may be statistically significant but is not clinically evident. Despite the lack of difference in MCID ODI between the central or paracentral cohort and far lateral cohort, it is important to discuss the reason for less improvement in ODI for patients with far lateral herniation. One reason for the inferior ODI scores in far lateral disc herniation may be the location of the herniation. Lateral HNP commonly occurs at higher lumber levels which have been shown to be associated with pseudoradicular pain. Resolving pseudoradicular symptoms can present as back pain and impact ODI in far lateral herniation more than central/paracentral herniation.17 Another possible explanation for lower ODI improvement for far lateral herniation may be the surgeon’s familiarity with the technique used to preform soft tissue dissection for lateral HNP as these are less common than central and paracentral HNP. MCID for VAS back, VAS leg, SF-12, and VR-12 scores was also not significantly different between the 2 cohorts. Reevaluating postoperative scores after a longer period of time has passed may be an opportunity for future research.
Furthermore, our patient population exhibited a median duration of symptoms of 9 months prior to surgery. While it must be acknowledged that outliers may prolong the mean duration of symptoms, the median helps to illustrate the accurate duration of symptoms in our study population. The duration of symptoms was also controlled for in the multivariate analysis and yielded no significant difference between the 2 cohorts. Additionally, all patients undergo the same conservative treatment prior to surgery; thus, this regimen may have been successful for some patients with prolonged duration of symptoms until they required surgery.
No significant differences were found in reoperation rates or postoperative SF-12 and VR-12 scores between far lateral and central/paracentral HNP groups. Previous literature comparing post-surgical outcomes of central/paracentral and far lateral HNP is scarce. However, literature assessing the difficulty associated with addressing far lateral HNP is extensive, and operative management remains controversial.12,16 Increased difficulty associated with lumbar discectomy of far lateral HNP may be attributed to their lower incidence, as well as their anatomical positioning compared with the more common central/paracentral herniations. In addition, inherently difficult anatomic access to the lateral interpedicular compartment may increase risk of causing nerve damage, or damaging the overlying facet joint, which can place the patient at risk of spine instability, resulting in spinal fusion surgery in the future.1,2 However, despite the notion that far lateral HNP may be associated with a technically more difficult surgical procedure, our study has found that patients presenting with far lateral disc herniations can expect similar outcomes to patients presenting with central/paracentral herniations with no increased risk of reoperation. This information can be used in support of surgical treatment for far lateral HNP, as previous literature has suggested that conservative management may result in relatively high non-operative success rates.18
The present study does have important limitations. While the present study explained the contradiction between the postoperative patient outcomes recorded per the ODI and VAS/SF-12/VR-12 measures, it is important to indicate that these do not measure the exact same domain. There is also evidence that these measures do not necessarily correlate.19 Thus this incongruence could partially explain the contradiction between patient-reported postoperative ODI and VAS/SF-12/VR-12 scores. In addition, a substantial difference in sample size exists between the far lateral (n = 15) and the central/para-central (n = 85) groups. Our sample size as a whole is also small, with a total of 100 patients. This may be attributed to the implementation of a 3-month follow-up cutoff postsurgery. Despite the small sample size, we were able to adequately analyze outcomes while factoring for MCID.
Conclusion
Despite the prevalence of lumbar microdiscectomy in treatment for lumbar disc herniation, literature is scare surrounding comparative postoperative outcomes of far lateral versus central/paracentral herniations. Given the anatomic predisposition to posterior root ganglion compression by far lateral herniations, these herniations are often associated with increased pain, radiculopathies, and burden on activities of daily life. Our study has found that although patients with far lateral lumbar disc herniations present with worse preoperative outcome scores, they can expect similar symptom improvement to central or paracentral herniations following discectomy. This information can be used for future surgeons when weighing conservative versus surgical treatment of far lateral herniations.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Al-Khawaja DO, Mahasneh T, Li JC. Surgical treatment of far lateral lumbar disc herniation: a safe and simple approach. J Spine Surg. 2016;2:21–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Gioia G, Mandelli D, Capaccioni B, Randelli F, Tessari L. Surgical treatment of far lateral lumbar disc herniation. Identification of compressed root and discectomy by lateral approach. Spine (Phila Pa 1976). 1999;24:1952–1957. [DOI] [PubMed] [Google Scholar]
- 3. Fardon DF, Milette PC, Combined Task Forces of the North American Spine Society; American Society of Spine Radiology; American Society of Neuroradiology. Nomenclature and classification of lumbar disc pathology. Recommendations of the Combined task Forces of the North American Spine Society, American Society of Spine Radiology, and American Society of Neuroradiology. Spine (Phila Pa 1976). 2001;26:E93–E113. [DOI] [PubMed] [Google Scholar]
- 4. Fardon DF, Williams AL, Dohring EJ, Murtagh FR, Gabriel Rothman SL, Sze GK. Lumbar disc nomenclature: version 2.0: recommendations of the combined task forces of the North American Spine Society, the American Society of Spine Radiology and the American Society of Neuroradiology. Spine J. 2014;14:2525–2545. [DOI] [PubMed] [Google Scholar]
- 5. O’Toole JE, Eichholz KM, Fessler RG. Minimally invasive far lateral microendoscopic discectomy for extraforaminal disc herniation at the lumbosacral junction: cadaveric dissection and technical case report. Spine J. 2007;7:414–421. [DOI] [PubMed] [Google Scholar]
- 6. Epstein NE. Different surgical approaches to far lateral lumbar disc herniations. J Spinal Disord. 1995;8:383–394. [PubMed] [Google Scholar]
- 7. Phan K, Dunn AE, Rao PJ, Mobbs RJ. Far lateral microdiscectomy: a minimally-invasive surgical technique for the treatment of far lateral lumbar disc herniation. J Spine Surg. 2016;2:59–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lew SM, Mehalic TF, Fagone KL. Transforaminal percutaneous endoscopic discectomy in the treatment of far-lateral and foraminal lumbar disc herniations. J Neurosurg. 2001;94(2 suppl):216–220. [DOI] [PubMed] [Google Scholar]
- 9. Hodges SD, Humphreys SC, Eck JC, Covington LA. The surgical treatment of far lateral L3-L4 and L4-L5 disc herniations. A modified technique and outcomes analysis of 25 patients. Spine (Phila Pa 1976). 1999;24:1243–1246. [DOI] [PubMed] [Google Scholar]
- 10. Siu TLT, Lin K. Direct tubular lumbar microdiscectomy for far lateral disc herniation: a modified approach. Orthop Surg. 2016;8:301–308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Darden BV, 2nd, Wade JF, Alexander R, Wood KE, Rhyne AL, 3rd, Hicks JR. Far lateral disc herniations treated by microscopic fragment excision. Techniques and results. Spine (Phila Pa 1976). 1995;20:1500–1505. [DOI] [PubMed] [Google Scholar]
- 12. Epstein NE. Evaluation of varied surgical approaches used in the management of 170 far-lateral lumbar disc herniations: indications and results. J Neurosurg. 1995;83:648–656. [DOI] [PubMed] [Google Scholar]
- 13. Kim EJ, Chotai S, Archer KR, Bydon M, Asher AL, Devin CJ. Need for two-year patient-reported outcomes score for lumbar spine surgery is procedure-specific: analysis from a prospective longitudinal Spine Registry. Spine (Phila Pa 1976). 2017;42:1331–1338. [DOI] [PubMed] [Google Scholar]
- 14. Parker SL, Mendenhall SK, Shau DN, et al. Minimum clinically important difference in pain, disability, and quality of life after neural decompression and fusion for same-level recurrent lumbar stenosis: understanding clinical versus statistical significance. J Neurosurg Spine. 2012;16:471–478. [DOI] [PubMed] [Google Scholar]
- 15. Kronzer VL, Jerry MR, Abdallah AB, et al. Changes in quality of life after elective surgery: an observational study comparing two measures. Qual Life Res. 2017;26:2093–2102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Maroon JC, Kopitnik TA, Schulhof LA, Abla A, Wilberger JE. Diagnosis and microsurgical approach to far-lateral disc herniation in the lumbar spine. J Neurosurg. 1990;72:378–382. [DOI] [PubMed] [Google Scholar]
- 17. Lee JH, Lee SH. Clinical and radiological characteristics of lumbosacral lateral disc herniation in comparison with those of medial disc herniation. Medicine (Baltimore). 2016;95:e2733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Rust MS, Olivero WC. Far-lateral disc herniations: the results of conservative management. J Spinal Disord. 1999;12:138–140. [PubMed] [Google Scholar]
- 19. Patel S, Hee SW, Mistry D, et al. Crosswalking between disability questionnaire scores In: Patel, ed. Identifying Back Pain Subgroups: Developing and Applying Aapproaches Using Individual Patient Data Collected Within Clinical Trials. Southampton, England: NIHR Journals Library; 2016. [PubMed] [Google Scholar]