Abstract
Study Design:
Retrospective.
Objectives:
To evaluate complications and outcomes of halo immobilization in patients with cervical spine fractures treated at a level I trauma center.
Methods:
A retrospective evaluation of patients treated at a single institution with halo immobilization from August 2000 to February 2016 was performed. Demographic information, mechanism of injury, level and type of spine fracture, length of halo immobilization, complications associated with halo immobilization, and length of patient follow-up were collected.
Results:
A total of 189 patients treated with halos were identified. Of the 189 patients, 121 (64%) received halos for the management of cervical spine fractures and were included in the study. A total of 49.6% were males and 50.4% were females. The average age was 50.8 years (range 1-89 years). Overall, 10.7% sustained C1 fractures, 71.1% C2 fractures, and 18.2% subaxial spine (C3-C7) fractures. In all, 47.1% of the upper cervical fractures were either odontoid or hangman-type fractures. A total of 25.1% of patients had multiple cervical fractures. At latest follow-up, 81% had healed fractures with good alignment, minimal pain, and return to normal activities. There was an 8.3% mortality rate. The mortality group had an average age of 64.7 years (range 19-84 years). A total of 10.7% of patients failed halo immobilization and 46.3% of patients had complications such as pin site infections (5.8%), loose pins (1.7%), neck pain (20.7%), decreased range of motion (14%), thoracic skin ulcers (2.4%), and dysphagia (1.7%).
Conclusions:
The use of halo immobilization for cervical spine fractures resulted in clinical success in 81% of patients. Complication rates in geriatric patients were lower than previously reported in the literature.
Keywords: halo immobilization, halo vest, cervical spine fracture, outcomes, complications, mortality
Introduction
Cervical spine fractures may result in increased complications, morbidity, or mortality if not properly evaluated and treated.1–3 Relatively stable injuries can be managed in a rigid cervical collar. The most rigid immobilization device for nonoperative cervical trauma management is the cranial pin halo ring and thoracic jacket device (halo vest). Many spinal trauma surgeons consider the halo vest fracture management to be less involved and less morbid than operative fracture stabilization. However, the halo vest can be cumbersome and problematic especially in obese or geriatric patients.4 Jacqueline Perry, MD, and colleagues pioneered halo immobilization in the 1950s.5 Since that time, halo vests have become the hallmark of nonoperative care. Numerous studies have shown that halo immobilization can provide enough stability to avoid surgery in certain cervical spine fractures.6,7 Previous studies highlight very high halo complication rates.8,9 In elderly patients the use of halo immobilization has become debatable and not encouraged because of possible complications.4,10
The objective of this study is to evaluate morbidity, mortality, and clinical success rates of halo immobilization for consecutive patients who were treated for cervical spine fractures at a level I trauma center.
Methods
A retrospective evaluation of electronic medical records of patients treated with halo immobilization from August 2000 to February 2016 was performed. Institutional review board approval was obtained. Two authors evaluated the medical records of patients treated with a halo vest a level I trauma center. Demographic information (age, gender, race), mechanism of injury, level and type of spine fracture, length of halo immobilization, complications associated with halo immobilization, and length of patient follow-up were collected.
Results
A total of 189 patients treated with halos were identified. Of these, 121 (64%) patients involving halo immobilization were enrolled. Sixty-eight patients were excluded because of use of traction tongs, use of halo immobilization only for surgical management, loss to follow-up, or lack of cervical spine fractures. A total of 49.6% were males and 50.4% were females. The average age was 50.8 years with a range of 1 to 89 years. In all, 81.9% were Caucasian, 13.8% were Hispanic/Latino, 3.2% were African American, and 1.1% were Asian. Of the 121 patients: 30 were ≤30 years old (24.8%), 46 were 31 to 60 years old (38%), and 45 were >60 years old (37.2%) (Table 1).
Table 1.
Patient and Treatment Demographics.
| No. of males, n (%) | 60 (49.6) |
| No. of females, n (%) | 61 (50.4) |
| Age, years, mean (range) | 50.8 (1-89) |
| Age (years) breakdown, n (%) | |
| ≤30 | 30 (24.8) |
| 31-60 | 46 (38) |
| >60 | 45 (37.2) |
| Race, % | |
| Caucasian | 81.9 |
| Hispanic/Latino | 13.8 |
| African American | 3.2 |
| Asian | 1.1 |
| Mechanism of injury, % | |
| Motor vehicle collision | 58.7 |
| Fall | 41.3 |
| Length of halo immobilization, weeks, mean (range) | 10 (0.29-16) |
| Length of follow-up, months, mean (range) | 10.9 (0.07-111) |
A total of 10.7% sustained C1 fractures, 71.1% C2 fractures, and 18.2% for subaxial spine (C3-C7) fractures (Figures 1 and 2). Overall, 47.1% of the upper cervical fractures were either odontoid or hangman type fractures and 25.1% of patients had multiple cervical fractures (Tables 2 –4). Mechanism of injury included the following: 58.7% motor vehicle collisions and 41.3% were from falls. The average length of halo immobilization was 10 weeks (range 0.29-16 weeks). The average length of follow-up was 10.9 months (range 0.07-111 months).
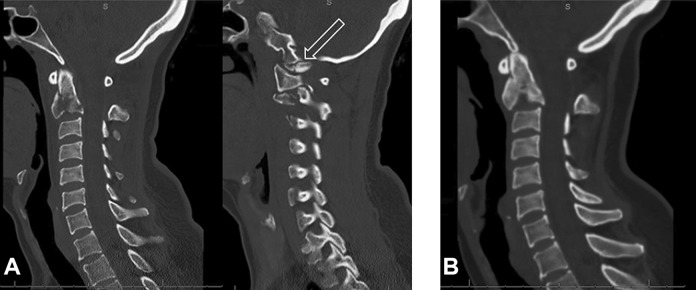
Figure 1.
(A) A 44-year-old woman involved in motor vehicle collision with C2 and occipital condyle fractures. Sagittal computed tomography (CT) of the cervical spine demonstrates the C2 and occipital condyle fractures (arrow). (B) She was treated with halo vest immobilization for 3 months and CT obtained prior to halo removal. Sagittal CT demonstrates healing of the C2 fracture.
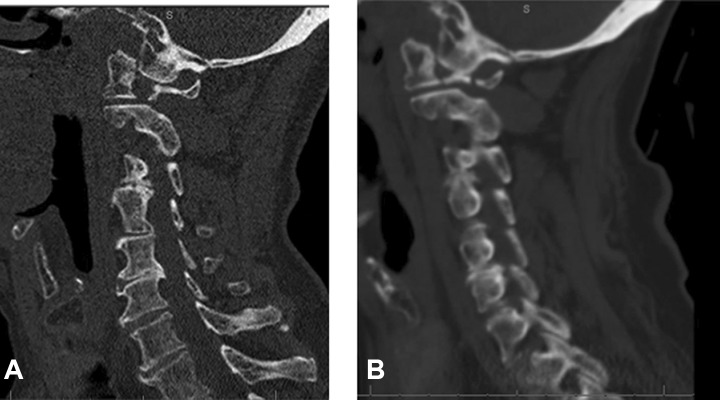
Figure 2.
(A) An 84-year-old woman who sustained a ground level fall with C1 lateral mass fracture as seen on sagittal computed tomography (CT) image. (B) She was treated with halo vest immobilization for 3 months and sagittal CT demonstrates fracture healing.
Table 2.
Classification of C1 and C2 Fractures.
| Type of Fracture | No. of Patients (% of Total) |
|---|---|
| C1 Jefferson type I | 1 (0.8) |
| C1 Jefferson type III | 1 (0.8) |
| C1 Jefferson displaced | 1 (0.8) |
| C1 Nondisplaced | 1 (0.8) |
| C2 Unspecified | 20 (16.5) |
| C2 Nondisplaced | 2 (1.6) |
| C2 Odontoid type II | 10 (8.3) |
| C2 Odontoid type III | 20 (16.5) |
| C2 Hangman’s unspecified | 10 (8.3) |
| C2 Hangman’s type I | 5 (4.1) |
| C2 Hangman’s type II | 7 (5.8) |
| C2 Hangman’s type III | 1 (0.8) |
| C2 Hangman’s atypical | 4 (3.3) |
Table 3.
Classification of Single Level Subaxial Fractures.
| Type of Fracture | No. of Patients (% of Total) |
|---|---|
| C3 | 1 (0.8) |
| C4 | 1 (0.8) |
| C6 | 3 (2.5) |
| C7 | 2 (1.6) |
Table 4.
Classification of Multilevel Fractures.
| Type of Fracture | No. of Patients (% of Total) |
|---|---|
| C1, C2 | 7 (5.8) |
| C1, C2, C7 | 1 (0.8) |
| C1, C2, C5, C6 | 1 (0.8) |
| C2, C3 | 5 (4.1) |
| C2, C3, C7 | 1 (0.8) |
| C2 (atypical type III), C5, C6 | 1 (0.8) |
| C2, C5 | 1 (0.8) |
| C2 (type II), C6 flexion-compression | 1 (0.8) |
| C4, C5 | 2 (1.6) |
| C4, C5, C6, C7 | 1 (0.8) |
| C5, C6 flexion-compression | 5 (4.1) |
| C5, C6, C7 | 1 (0.8) |
| C6, C7 | 4 (3.3) |
A total of 81% of patients had fracture healing with good alignment, minimal pain, and return to normal activities. There was an 8.3% mortality rate (1.7% died within 90 days of injury and 6.6% died within 1 year of injury). The mortality group had an average age of 64.7 years (range 19-84 years). Mechanisms for halo-related deaths included cardiac, respiratory, and renal complications. Halo immobilization may have exacerbated previous complications, leading to mortality. In all, 10.7% failed halo immobilization and 6.6% were treated surgically. Reasons for failing halo treatment included 5.8% having nonunion of cervical fracture and 0.8% for falling while wearing a halo. A total of 4.1% who failed halo immobilization were treated nonsurgically and reasons for failing included 2.5% with nonunion of cervical fracture, 0.8% with listhesis, and 0.8% with incapacitating pain and deemed medically unnecessary by institution in different city on patient’s relocation. Types of nonoperative management included autofusion, hard collar, use of Teriparatide (Forteo, Eli Lilly, Indianapolis, IN), referral to pain clinic, and halo removal. Perioperative or long-term complication rates included 5.8% for pin site infections, 1.7% for loose pins, 20.7% for neck pain, 14% for decreased range of motion, 2.4% for thoracic skin ulcers, and 1.7% for dysphagia with an overall complication rate of 46.3%. Breakdown by age for complications were 15.7% (≤30 years), 18.1% (range 31-60 years), and 12.4% (>60 years) (Tables 5 –11).
Table 5.
Outcome Demographics.
| Outcomes | No. of Patients (% of Total) |
|---|---|
| Total positive | 98 (81.0) |
| Total negative | 23 (19.0) |
| Mortality | |
| Total | 10 (8.3) |
| Within 90 days | 2 (1.7) |
| >90 days and <1 year | 8 (6.6) |
| Failed halo treatment | |
| Total | 13 (10.7) |
| Operative management | 8 (6.6) |
| Nonoperative management | 5 (4.1) |
Table 6.
Complication Demographics.
| Age | No. of Patients (Complication % of Total in Age Group) |
|---|---|
| Overall | 56 (46.3) |
| ≤30 years | 19 (63.3) |
| 31-60 years | 22 (47.8) |
| >60 years | 15 (33.3) |
| Complication: ≤30 years | |
| Pin infection | 5 (16.7) |
| Loose pin | 0 (0) |
| Pain | 11 (36.7) |
| Decreased range of motion | 2 (6.7) |
| Thoracic skin ulcers | 1 (3.3) |
| Dysphagia | 0 (0) |
| Complication: 31-60 years | |
| Pin infection | 2 (4.3) |
| Loose pin | 1 (2.2) |
| Pain | 9 (19.6) |
| Decreased range of motion | 9 (19.6) |
| Thoracic skin ulcers | 0 (0) |
| Dysphagia | 1 (2.2) |
| Complication: >60 years | |
| Pin infection | 0 (0) |
| Loose pin | 1 (2.2) |
| Pain | 5 (11.1) |
| Decreased range of motion | 6 (13.3) |
| Thoracic skin ulcers | 2 (4.4) |
| Dysphagia | 1 (2.2) |
Table 7.
Classification of Fracture Type and Complications.
| Complication | Type of Fracture | No. of Patients (% of Total Patients) |
|---|---|---|
| Pin infection | C1, C2 C2 unspecified C2 odontoid type II C2 odontoid type III C4 C5 |
1 (0.8) 2 (1.7) 1 (0.8) 1 (0.8) 1 (0.8) 1 (0.8) |
| Loose pin | C2 unspecified C2 type II |
1 (0.8) 1 (0.8) |
| Pain | C1, C2, C7 C2 unspecified C2 odontoid type II C2 odontoid type III C2 hangman’s unspecified C2 hangman’s type II C2, C3 C2 (type II), C6 flexion-compression C2, C3, C7 C4, C5, C6, C7 C5, C6, C7 C6, C7 C7 |
1 (0.8) 4 (3.3) 2 (1.7) 3 (2.5) 4 (3.3) 2 (1.7) 2 (1.7) 1 (0.8) 1 (0.8) 1 (0.8) 1 (0.8) 2 (1.7) 1 (0.8) |
| Decreased range of motion | C1 nondisplaced C1, C2 C2 unspecified C2 odontoid type II C2 odontoid type III C2 hangman’s unspecified C2 hangman’s type II C2 hangman’s atypical C2, C3 C2 (atypical type III), C5, C6 C5 |
1 (0.8) 1 (0.8) 1 (0.8) 1 (0.8) 3 (2.5) 5 (4.1) 1 (0.8) 1 (0.8) 1 (0.8) 1 (0.8) 1 (0.8) |
| Thoracic skin ulcers | C2 fracture, odontoid type III C2 fracture, nondisplaced C1, C2 |
1 (0.8) 1 (0.8) 1 (0.8) |
| Dysphagia | C1 and C2 fracture, unspecified C5-C6 flexion/compression fracture |
1 (0.8) 1 (0.8) |
Table 8.
Patients Who Failed Halo Treatment and Underwent Operative Management
| Reasons for Failing | No. of Patients (% of Patients for Operative Management) |
|---|---|
| Nonunion of fracture | 7 (87.5) |
| Fall while wearing halo | 1 (12.5) |
Table 9.
Fracture Classification for Those Who Failed Halo Treatment Followed by Operative Management.
| Type of Fracture | No. of Patients (% of Patients for Operative Management) |
|---|---|
| C2 unspecified | 3 (37.5) |
| C2 type II | 2 (25.0) |
| C2 hangman unspecified | 1 (12.5) |
| C1 (Jefferson unspecified), C2 (type II) | 1 (12.5) |
| C5, C6 | 1 (12.5) |
Table 10.
Patients Who Failed Halo Treatment Followed by Nonoperative Management.
| Reasons for Failing | Type of Nonoperative Management | No. of Patients (% of Patients for Nonoperative Management) |
|---|---|---|
| Nonunion of fracture | Autofusion Aspen collar Forteo |
3 (60) |
| Listhesis | Referral to pain clinic | 1 (20) |
| Deemed medically unnecessary by institution in different city | Halo removal | 1 (20) |
Table 11.
Fracture Classification for Those Who Failed Halo Treatment Followed by Nonoperative Management.
| Type of Fracture | No. of Patients (% of Patients for Nonoperative Management) |
|---|---|
| C2 type III | 3 (60) |
| C2, C3 | 1 (20) |
| C6, C7 | 1 (20) |
When evaluating complications per age group (Table 6): 19/30 patients in ≤30-year-old group (63.3%) had a complication, followed by 22/46 (47.8%) in the 31- to 60-year-old group, and the least number of complications were in the >60-year-old old group with 15/45 complications (33.3%).
Discussion
Spinal injuries are commonly associated with motor vehicle collisions and falls.11 Our findings confirmed this causality with 58.7% of the cervical injuries occurring from motor vehicle collisions and 41.3% resulting from falls. Injuries at C2 level tend to be the most common.12 The majority of the halo use in our study was for the treatment of C2 fractures (79.9%). The most common fracture patterns were odontoid and hangman injuries. A total of 25.1% of patients had multiple cervical fractures (Tables 2 –4).
High rates of complications of halo use have been previously reported in the literature. Tashjian et al8 demonstrated increased early morbidity and mortality in elderly patients with odontoid fractures who were treated with halo immobilization. The authors reported a 66% complication rate and a 42% mortality rate in 38 patients who were older than 65 years.8 More recently, DePasse et al13 reported an 11.1% in-hospital mortality rate for geriatric patients who had halo vest application for odontoid fracture treatment. In our study, there was an 8.3% mortality rate (1.7% died within 90 days of injury and 6.6% died after 90 days and within 1 year of injury) with an average age of 64.7 years (range 19-84 years). The lower mortality rate cited in our study is most likely due to the relatively younger age of our patients. Our study does show higher mortality with advancing age and halo use for cervical trauma as previously reported in the literature.4,8
Other studies have emphasized the high complication rates with halo use. Julien et al9 performed a meta-analysis and reported 36% complications and 35% pseudarthrosis in 265 adult patients who were treated with a halo vest. We report a similarly high rate of complications. In our study, 46.2% of patients experienced complications of halo vest treatment. Complications included pin site infections (5.8%), loose pins (1.7%), neck pain (20.7%), decreased range of motion (14%), thoracic skin ulcers (2.4%), and dysphagia (1.7%). When evaluated by age groupings, the highest rate of complications in our study was observed in younger patients, ≤30 years old (63.3%) followed by the 31- to 60-year-old group with 47.8%. Complication rates in patients older than 60 years averaged 33.3% and were lower than previously reported in the literature.4 While patients older than 60 years have the lowest complication rate, this age group has the highest rate of more severe complications such as thoracic skin ulcers and dysphagia at 20% compared to those less than 30 years old and 31- to 60-year-olds having 4.5% of severe complications (Table 7). While most halo complications involve pin site loosening or infection, the use of pinless halos also has significant complication rates. Bakshi et al14 reported a 21% complication rate using a pinless halo in the pediatric population. Other rare complications of halo use have been reported. Overtightening of halo pins may cause intracranial penetration, pneumocephalus, and epileptic seizure.15,16 Intracranial abscess has also been reported.17 Our study noted 3 patients with thoracic skin ulcers and 2 with severe prolonged swallowing problems after halo application (Table 6).
Sime et al18 recently published outcomes of 54 patients treated with a halo for subaxial cervical spine fractures. Overall, good 24-month function was achieved in 35% of patients, and 51% and 77% of patients reported good physical and mental health status, respectively. Ongoing moderate to severe neck pain was present in 19% of patients. The authors noted that poorer function was associated with compensable status, polytrauma, and a lower level of education. Poorer physical health status was associated with age ≥50 years, preexisting comorbidities, an Injury Severity Score >12, and a lower level of education.18
At latest follow-up, which averaged approximately 11 months in our study, 81% of patients had a clinical success rate, which was measured as healed fractures with good alignment, minimal pain, and return to normal activities. The most common injury types for halo management in our study were either type 3 odontoid or type 2 hangman’s fractures. Other studies have reported similarly high rates of clinical success for the treatment of C2 hangman’s fractures that may be treated nonoperatively using halo immobilization.19
Major complications in our study included the loss of fracture reduction and conversion of treatment to operative or nonoperative management (Tables 8 –11). Of patients who were initially treated with a halo 6.6% required subsequent surgical management and 4.1% required subsequent nonsurgical management due to loss of fracture reduction in the halo. One patient sustained a traumatic fall in the halo that caused halo loosening and loss of fracture alignment. An additional patient self-extricated from the halo within the first week of usage Our study confirms that after application, the halo has a moderate failure rate. Close patient follow-up and monitoring is required during the halo treatment period.
Minor complications of halo use were frequently observed in our study. These included pin loosening and pin-site infection. 46.2% of patients had minor perioperative complications or longer term complications such as pin site infections (5.8%), loose pins (1.7%), neck pain (20.7%), decreased range of motion (14%), thoracic skin ulcers (2.4%), and dysphagia (1.7%) (Tables 6 and 7). Similar rates of pin site complications and neck pain have been reported with halo use. Recommendations such as pin-site care and tightening of loose pins along with early halo removal physical therapy for neck range of motion may help decrease perioperative complications.20,21
Our study had several limitations. We did not use a historical control group. Also, some of the electronic medical records did not have all the information. For example, race/ethnicity was not listed in all the patients. We had a small sample size (n = 121) due to exclusion criteria such as loss to follow-up. Because the study spanned 16 years, patient-reported outcomes were not available for most of the study period and future studies evaluating the patient-reported outcomes in patients managed with halos would be useful.
Conclusion
The use of halo immobilization for cervical spine fractures resulted in clinical success in 81% of patients. Loss of fracture reduction and operative management occurred in 6.6% of patients who were initially treated with a halo versus 4.1% for nonoperative management. Early mortality rates remain high in the elderly population. Lesser complications of halo use also remain moderately high and mostly include loosening of infected pins, neck pain, or decreased range of motion. Complication rates in geriatric patients averaged 33.3% and were lower than previously reported in the literature.
Footnotes
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Dr. Addisu Mesfin reports research grant support from Corelink, LES Society, and Spine Surgery Fellowship support from AO Spine, OMeGA.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Cesar Hernandez, BA  https://orcid.org/0000-0001-8432-8887
https://orcid.org/0000-0001-8432-8887
Mohamed Salah Mahmoudi, BS  https://orcid.org/0000-0002-9686-5767
https://orcid.org/0000-0002-9686-5767
References
- 1. Fehlings MG, Vaccaro A, Wilson JR, et al. Early versus delayed decompression for traumatic cervical spinal cord injury: results of the Surgical Timing in Acute Spinal Cord Injury Study (STASCIS). PLoS One. 2012;7:e32037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Roberge RJ, Wears RC, Kelly M, et al. Selective application of cervical spine radiography in alert victims of blunt trauma: a prospective study. J Trauma. 1988;28:784–788. [DOI] [PubMed] [Google Scholar]
- 3. Goldberg W, Mueller C, Panacek E, et al. ; NEXUS Group. Distribution and patterns of blunt traumatic cervical spine injury. Ann Emerg Med. 2001;38:17–21. [DOI] [PubMed] [Google Scholar]
- 4. Sharpe JP, Magnotti LJ, Weinberg JA, Schroeppel TJ, Fabian TC, Croce MA. The old man and the C-spine fracture: impact of halo vest stabilization in patients with blunt cervical spine fractures. J Trauma Acute Care Surg. 2016;80:76–80. [DOI] [PubMed] [Google Scholar]
- 5. Nickel V, Perry J, Garrett A, Heppenstall M. The halo. A spinal skeletal traction fixation device. J Bone Joint Surg Am. 1968;50:1400–1409. [PubMed] [Google Scholar]
- 6. O’Donnell PW, Anavian J, Switzer JA, Morgan RA. The history of the halo skeletal fixator. Spine (Phila Pa 1976). 2009;34:1736–1739. [DOI] [PubMed] [Google Scholar]
- 7. Lauweryns P. Role of conservative treatment of cervical spine injuries. Eur Spine J. 2010;19(suppl 1):S23–S26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Tashjian RZ, Majercik S, Biffl WL, Palumbo MA, Cioffi WG. Halo-vest immobilization increases early morbidity and mortality in elderly odontoid fractures. J Trauma. 2006;60:199–203. [DOI] [PubMed] [Google Scholar]
- 9. Julien TD, Frankel B, Traynelis VC, Ryken TC. Evidence-based analysis of odontoid fracture management. Neurosurg Focus. 2000;8:e1. [DOI] [PubMed] [Google Scholar]
- 10. Bono CM. The halo fixator. J Am Acad Orthop Surg. 2007;15:728–737. [DOI] [PubMed] [Google Scholar]
- 11. Schouten R, Albert T, Kwon BK. The spine-injured patient: initial assessment and emergency treatment. J Am Acad Orthop Surg. 2012;20:336–346. [DOI] [PubMed] [Google Scholar]
- 12. Ryan MD, Henderson JJ. The epidemiology of fractures and fracture-dislocations of the cervical spine. Injury. 1992;23:38–40. [DOI] [PubMed] [Google Scholar]
- 13. DePasse JM, Palumbo JA, Ahmed AK, Adams CA, Jr, Daniels AH. Halo-vest immobilization in elderly odontoid fracture patients: evolution in treatment modality and in-hospital outcomes. Clin Spine Surg. 2017;30:E1206–E1210. doi:10.1097/BSD.0000000000000483 [DOI] [PubMed] [Google Scholar]
- 14. Bakhshi H., Kushare I, Banskota B, Nelson C, Dormans JP. Pinless halo in the pediatric population: indications and complications. J Pediatr Orthop. 2015;35:374–378. [DOI] [PubMed] [Google Scholar]
- 15. Kingma R, Peters JM, Coene LN. Intracranial penetration of a halo pin causing an epileptic seizure. J Bone Joint Surg Br. 2006;88:1654–1655. [DOI] [PubMed] [Google Scholar]
- 16. Glover AW, Zakaria R, May P, Barrett C. Overtightening of halo pins resulting in intracranial penetration, pneumocephalus, and epileptic seizure. Int J Spine Surg. 2013;7:e42–e44. doi:10.1016/j.ijsp.2013.01.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Gelalis ID, Christoforou G, Motsis E, Arnaoutoglou C, Xenakis T. Brain abscess and generalized seizure caused by halo pin intracranial penetration: case report and review of the literature. Eur Spine J. 2009;18(suppl 2):172–175. doi:10.1007/s00586-008-0759-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Sime D, Gabbe B, Liew S. Outcomes of halo immobilization in the management of subaxial cervical facet fractures. ANZ J Surg. 2017;87:159–164. doi:10.11111/ans.13656 [DOI] [PubMed] [Google Scholar]
- 19. Al-Mahfoudh R, Beagrie C, Woolley E, et al. Management of typical and atypical hangman’s fractures. Global Spine J. 2016;6:248–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Garfin SR, Botte MJ, Waters RL, Nickel VL. Complications in the use of the halo fixation device. J Bone Joint Surg Am. 1986;68:320–325. [PubMed] [Google Scholar]
- 21. van Middendorp JJ, Slooff WB, Nellestein WR, Oner FC. Incidence of and risk factors for complications associated with halo-vest immobilization: a prospective, descriptive cohort study of 239 patients. J Bone Joint Surg Am. 2009;91:71–79. [DOI] [PubMed] [Google Scholar]