Abstract
Aims and objectives
To investigate uptake of a Chest Injury Protocol (ChIP), examine factors influencing its implementation and identify interventions for promoting its use.
Background
Failure to treat blunt chest injuries in a timely manner with sufficient analgesia, physiotherapy and respiratory support, can lead to complications such as pneumonia and respiratory failure and/or death.
Design
This is a mixed‐methods implementation evaluation study.
Methods
Two methods were used: (i) identification and review of the characteristics of all patients eligible for the ChIP protocol, and (ii) survey of hospital staff opinions mapped to the Theoretical Domains Framework (TDF) to identify barriers and facilitators to implementation. The characteristics and treatment received between the groups were compared using the chi‐square test or Fischer's exact test for proportions, and the Mann–Whitney U‐test for continuous data. Quantitative survey data were analysed using descriptive statistics. Qualitative data were coded in NVivo 10 using a coding guide based on the TDF and Behaviour Change Wheel (BCW). Identification of interventions to change target behaviours was sourced from the Behaviour Change Technique Taxonomy Version 1 in consultation with stakeholders.
Results
Only 68.4% of eligible patients received ChIP. Fifteen facilitators and 10 barriers were identified to influence the implementation of ChIP in the clinical setting. These themes were mapped to 10 of the 14 TDF domains and corresponded with all nine intervention functions in the BCW. Seven of these intervention functions were selected to address the target behaviours and a multi‐faceted relaunch of the revised protocol developed. Following re‐launch, uptake increased to 91%.
Conclusions
This study demonstrated how the BCW may be used to revise and improve a clinical protocol in the ED context.
Relevance to clinical practice
Newly implemented clinical protocols should incorporate clinician behaviour change assessment, strategy and interventions. Enhancing the self‐efficacy of emergency nurses when performing assessments has the potential to improve patient outcomes and should be included in implementation strategy.
Keywords: behaviour change, behaviour change wheel, chest injury, implementation evaluation, nursing, theoretical domains framework
What does this article contribute to the wider clinical community?
Even an isolated rib fracture is associated with significant consequences, particularly in the elderly but the majority of literature advises implementation of clinical protocols for patients with three or more rib fractures. Introduction of an early notification protocol for ALL blunt chest‐injured patients enabled multidisciplinary, tailored patient care that reduced the odds of patients developing pneumonia by 56%. The overall uptake of the protocol, however, is unknown, as are factors which hinder or help activation of the protocol.
Clinician behaviour change is central to evidence‐based practice and knowledge translation. Evaluation of clinical protocols for uptake and effectiveness is essential and should include staff perceptions and opinions. The behaviour change wheel can be used to revise and improve a clinical protocol in the ED context.
1. Introduction
Isolated blunt chest injury often results from a low energy mechanism (such as a fall from standing height), sporting collisions or assaults. Failure to treat blunt chest injuries in a timely manner with sufficient analgesia, physiotherapy and respiratory support, can lead to complications such as pneumonia and respiratory failure and/or death (Leone et al., 2008). Patients with at least three rib fractures have a significantly increased risk of in‐hospital mortality (Holcomb, McMullin, Kozar, Lygas, & Moore, 2003; Testerman, 2006), an effect even more pronounced in older patients (Kent, Woods, & Bostrom, 2008) in whom each additional rib fracture increases the risk of mortality by 19% and of pneumonia by 27% (Bulger, Arneson, Mock, & Jurkovich, 2000). Much of literature around blunt chest injury advises implementation of strategies such as clinical practice guidelines to improve the care and outcomes of these patients (Kerr‐Valentic et al., 2003; Testerman, 2006; Todd et al., 2006). However, the majority of pathways reported in the literature do not consider patients with less than three rib fractures, the elderly, or those with underlying respiratory disease, all of which are risk factors for morbidity and mortality (Menditto et al., 2012; Sahr, Webb, Renner, Sokol, & Swegle, 2013; Sesperez, Wilson, Jalaludin, Seger, & Sugrue, 2001; Todd et al., 2006). Given that pain caused by blunt chest injury is associated with restricted pulmonary function (Crandall, Kent, Patrie, Fertile, & Martin, 2000), which can lead to serious complications, the need for an effective early intervention in this patient group is critical.
Major difficulties arise when introducing clinical guidelines and protocols into clinical practice (Grol & Grimshaw, 2003), for example, clinician compliance with providing appropriate care for 22 conditions in a large cross‐sectional study in Australia, ranged from 32% to 86% (Runciman et al., 2012). Barriers to the implementation of evidence‐based care in the challenging context of competing priorities in the ED can include lack of time, lack of resources, poor access to guidelines, complex guidelines, capacity for interdisciplinary teamwork, a lack of continuing education and an unsupportive organisational culture (Haynes & Haines, 1998; Grol & Grimshaw, 2003; Wallis, 2012).
2. Background
To address the evidence‐practice gap in patients with blunt chest injury, the Trauma and Emergency Departments (ED) in our Level 1 Trauma Centre collaborated with the pain, physiotherapy and aged care teams to develop a Chest Injury Protocol (ChIP) that consolidated the best available evidence on treatment of blunt chest injury (Curtis et al., 2016; Unsworth, Curtis, & Asha, 2015). Comparable to a trauma team call (Davis et al., 2008) or “stroke page” (Batmanian et al., 2007), which are known to improve patient and health service outcomes, ChIP is an early activation protocol that facilitates individually tailored, multidisciplinary management of blunt chest injury, including multimodal analgesia to optimise respiratory function. Early notification enables rapid multidisciplinary assessment and care tailored to the individual needs dependent on their premorbid condition. Each member of the ChIP team (or their after‐hours delegate) received a message via their personal pager and was required to respond within 60 minutes. ChIP could be activated 24 h a day, 7 days a week. In a retrospective pre‐ to postcohort study, the likelihood of a patient who received a ChIP activation developing pneumonia was 56% lower than before ChIP introduction (Curtis et al., 2016). In the cohort that received ChIP, more patients received a pain team, physiotherapy and trauma team review and the use of high flow nasal prong oxygen (HFNP), multimodal analgesia including patient controlled analgesia (PCA) (Curtis et al., 2016).
2.1. Implementation of a new protocol
The planning and implementation of ChIP included the engagement of stakeholders in its development. As the success of any new protocol relies on senior clinician support, particularly around pain management and coordination of patient care (Bennetts, Campbell‐Brophy, Huckson, & Doherty, 2012), ChIP was developed with each of the clinical specialties involved in the care of patients with rib fractures and was approved by the hospital executive. Given the multidisciplinary nature of ChIP, a working party of key stakeholders developed a consensus plan to streamline its successful implementation. Success hinged on protocol education and compliance of seven clinical specialties (medical, nursing and allied health) and the hospital switch board. The consultative process involved all disciplines involved and feedback was incorporated. This process was facilitated by the authors being senior clinicians at the study site with significant corporate knowledge.
To raise awareness of the importance of this new protocol, regular and ongoing staff education around the pitfalls of inadequate analgesia and the benefits of early multimodal analgesia and physiotherapy was conducted by the trauma service. Australian research published in 2012 reported that staff perceptions of patients’ pain level and attitudes towards pain management were identified as barriers to the administration of analgesia (Shaban, Holzhauser, Gillespie, Huckson, & Bennetts, 2012). An education package was developed based on the aforementioned topics. The package explains the physiological effects of chest wall injury on respiration as well as the evidence around various clinical interventions to arrest or slow negative outcomes. The purpose and activation process of ChIP is also included. The trauma service has a regular clinical and educational presence throughout the hospital enabling access to staff immediately impacted as well as new clinicians as staff rotations occur. Regular (weekly) 45‐min education sessions occurred initially and ongoing sessions booked with the medical and nursing educators in the ED and surgical wards. Large laminated copies of the flow chart were mounted in the ED, as well as on the hospital intranet site, both of which are readily accessible by all hospital staff.
ChIP was implemented in 2012, yet the extent to which ChIP is activated by staff is unknown, particularly whether all eligible patients received a ChIP activation or staff opinion in terms of ease of use, relevance and applicability.
2.2. Aims
To describe and evaluate the implementation of ChIP, an early notification protocol for blunt chest injury. Specifically to:
Determine the incidence of uptake of the ChIP protocol
Identify facilitators and barriers to the protocol ChIP activation
Identify intervention strategies likely to be most feasible and effective in promoting uptake and optimising use of the ChIP protocol
3. Methods
ChIP was implemented in April 2012 at a large teaching and trauma hospital, the fourth busiest ED in New South Wales, the most populous state in Australia (over 70,000 patient visits in 2015), and 10% of the local population aged over 70 years.
3.1. Design
This is a mixed‐methods implementation evaluation study. We developed an implementation plan based on the Accelerated Implementation Methodology, the framework endorsed by the site health district, that focussed on engaging all stakeholders in the development of ChIP and educating impacted staff (NSW Agency for Clinical Innovation 2014). Two methods were used to evaluate the implementation of ChIP: Incidence of uptake of ChIP was calculated by identification and review of the characteristics of all patients eligible for ChIP; and facilitators and barriers to implementation were identified using a survey of hospital staff opinions mapped to the Theoretical Domains Framework (French et al., 2012).
3.2. Data collection
3.2.1. Incidence of uptake of the ChIP protocol
The data collection period was from May 2012 to July 2014, patients hospitalised during this period meeting the inclusion criteria were included in the study. A 3‐week “run in period” between protocol introduction (7th April 2012) and study inclusion was included to allow for implementation training and staff adjustment to the protocol. Patients were eligible for this study if they were adults, admitted to hospital, had isolated chest wall trauma and were eligible for ChIP activation (see Figure 1). Patients who received a ChIP call were identified from the hospital trauma registry. Potential patients that did not get a ChIP activation were identified by searching the hospital clinical information database using ICD‐10 codes related to thoracic trauma. This was cross‐checked with data from the trauma registry. The medical records were then retrieved and screened for inclusion and exclusion criteria. Patients were included if they would have fulfilled the ChIP eligibility criteria. These patients were allocated to the “No‐ChIP” group.
Figure 1.
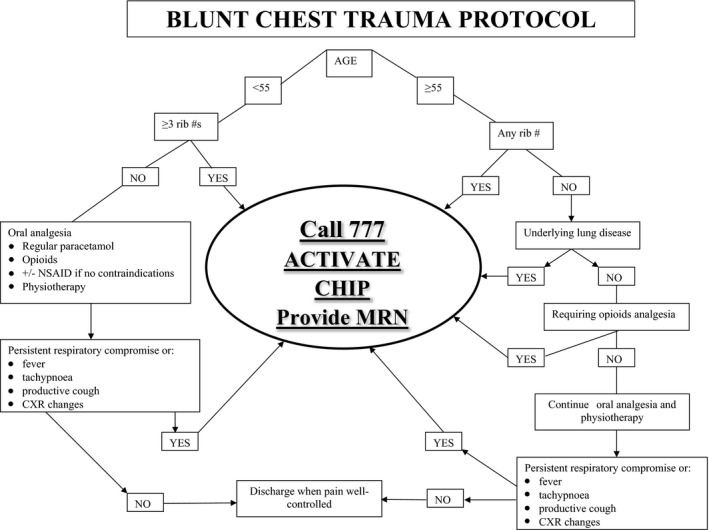
ChIP: Blunt chest injury protocol. #, fracture; ChIP, Chest Injury Protocol; CXR, Chest X‐ray; MRN, Medical Record Number; NSAID, Non‐steroidal anti‐inflammatory drug
Data for all patients were extracted using the same structured chart review method and data extraction template. Each data point was clearly defined and the section of the medical record from which the data item was to be obtained specified.
Demographic information included age and gender. Clinical information included Injury Severity Score (ISS), abbreviated injury score (AIS), the number of radiological rib fractures, time from injury to arrival, mechanism of injury and the Charlson Comorbidity Index. This Index is used to measure the burden of comorbid illness (Charlson, Pompei, Ales, & MacKenzie, 1987). A score ≥5 is considered severe and indicates a high risk of dying from comorbid illness within 1 year (Charlson et al., 1987). The AIS is an anatomical scoring system ranking injury severity and an AIS score greater than two signifies a serious injury (Copes et al., 1990). ISS is an anatomical diagnosis system derived from the Abbreviated Injury Scale that provides an overall score for patients with multiple injuries (Baker, O'Neill, Haddon, & Long, 1974). ISS was used to categorise injury severity as it is the most widely used injury scoring system (Curtis, Ramsden, & Lord, 2011).
Additional data were collected on patients who were eligible but did not receive a ChIP call. This included the medical team the patient was admitted under, time of day of presentation and the qualification level of the most senior ED medical staff member that was documented as reviewing the patient.
3.2.2. Facilitators and barriers to implementation
A survey was conducted in November and December 2014, on staff involved in activating, responding to and participating in ChIP. Survey participants were identified through points of contact in the trauma service, pain service, physiotherapy, ED and medical workforce. Participants were e‐mailed a participant information sheet outlining the aims of the survey and participation requirements. Clinicians agreeing to participate completed the survey on an online platform. Participation in the survey was voluntary and confidential. Participants were advised that they could withdraw their consent at any time. Reminder emails were sent out 2, 4 and 8 weeks after the initial invitation was distributed.
To identify and categorise any implementation problems, the survey (see Appendix S1) was designed and mapped to the Theoretical Domains Framework (TDF) (Cane, O'Connor, & Michie, 2012). The TDF was used as it identifies a wide range of barriers to change and provides a broader spectrum of potential intervention components to improve ChIP implementation should it be required (Cane et al., 2012; French et al., 2012). Questions that encompassed the barriers to implementing a protocol were also informed by the BARRIERs Scale (Légaré, 2009).
The survey consisted of the following areas of inquiry:
Clinician Demographics: including discipline, and role within the discipline.
TDF: includes knowledge; memory, attention and decision processes; behavioural regulation; professional/social role and identity; beliefs about capabilities; optimism; beliefs about consequences; reinforcement; and environmental context and resources
Additional comments: suggestions for changes and improvements to the protocol and any final comments
3.3. Ethical approval
Ethics approval was granted by the South Eastern Sydney Local Health District Human Research Ethics Committee (HREC 13/081 (LNR/13/POWH/175). Consent from staff was implied by survey completion.
3.4. Data analysis
3.4.1. Incidence of uptake of the ChIP protocol
Comparisons of characteristics between the groups, and the outcomes of time to pain team and physiotherapy review, proportion of patients receiving pain team, trauma team and physiotherapy review, and use of PCA and/or HFNP oxygen were compared using the chi‐square test or Fischer's exact test for proportions, and the Mann–Whitney U test for continuous data (continuous data were all non‐normally distributed). These outcomes were all components of ChIP and were presented to assess the effectiveness of protocol implementation. Therefore, no adjusted analyses were performed.
3.4.2. Facilitators and barriers to implementation
Survey analysis
Qualitative survey data were imported to and coded using NVivo 10. A coding guide was developed based on the definitions of the TDF domains(Cane et al., 2012). Qualitative survey data were coded using directed content analysis (Hsieh & Shannon, 2005). Exemplar quotes illustrating the themes were identified in this process. Quantitative survey data were imported to and analysed using descriptive statistics using spss (IBM v21), and mapped to the TDF domains.
Intervention design using the Behaviour Change Wheel
The Behaviour Change Wheel (BCW) was used as a framework for intervention design. The BCW is a well‐validated synthesis of 19 frameworks of behaviour change linked to a broad model of behaviour that can be applied to any behaviour in any setting. The BCW characterises the target behaviour in terms of Capability, Opportunity and Motivation (the COM‐B system), with Capability divided into psychological and physical capability, Opportunity divided into social and physical opportunity and Motivation divided into reflective and automatic motivation. Nine “intervention functions” exist in the BCW: (i) education, (ii) persuasion, (iii) incentivisation, (iv) coercion, (v) training, (vi) restriction, (vii) environmental restructuring, (viii) modelling and (ix) enablement. Intervention functions are functions served by an intervention targeting factors that influence behaviour (Michie, Atkins, & West, 2014). The intervention design consisted of three stages: Stage 1 involved selecting target behaviours, Stage 2 involved conducting a behavioural analysis and diagnosis, and Stage 3 involved identifying interventions to change target behaviours.
Selecting target behaviours
The authors discussed and considered ChIP activator and responder behaviours that could be targets for change. The behaviours of both activators and responders were considered as active participation by both of these groups is essential for the success of ChIP implementation and uptake. Behaviours were selected based on the impact they would make to ChIP implementation, the likelihood they could be changed and whether they would have positive spillover effects.
Conducting a behaviour analysis and diagnosis
To identify changes required for improved ChIP implementation, themes identified in the qualitative and quantitative data were mapped against the TDF domains. TDF domains considered to be targets for change were those that showed a disparity between reported behaviour and beliefs and/or were reported barriers/facilitators to ChIP implementation.
Identifying interventions to change target behaviours
TDF domains identified to be targets for change were mapped against the Behaviour Change Wheel (Michie et al., 2014). Identified intervention functions of the BCW were then linked to possible Behaviour Change Techniques Taxonomy Version 1 (BCTTv1) that could be employed (Michie et al., 2013). Face‐to‐face meetings with senior and junior members of each department required to activate or respond to ChIP were conducted to decide which of the proposed behaviour change techniques and modes of delivery would be most effective and feasible in the clinical setting to improve the implementation of ChIP. Further, the APEASE criteria were applied to the identified behaviour change techniques. The APPEASE criteria are a set of criteria used to make context‐based decisions on intervention content and delivery which consists of affordability, practicability, effectiveness and cost‐effectiveness, acceptability, side‐effects/safety and equity considerations.
4. Results
4.1. Incidence of uptake of the ChIP protocol
Of the 424 patients eligible for ChIP activation, only 68.4% (n = 290) received one. There was no meaningful clinical difference between patients who did and did not receive a ChIP call (Table 1). The largest group of treating clinicians of patients that did not receive a ChIP call was ED registrars (50.8%), followed by junior medical officers (31.4%). If at any time, a staff specialist saw the patient this was noted. If patients did not receive a ChIP call, they were predominantly admitted under general surgery (50.4%) or aged care (36.1%). Patients were more likely to receive a pain team review (p = .012), HFNP (p < .001) and a trauma team review (p < .001) if they received a ChIP call (Table 2).
Table 1.
Comparison of patient characteristics in the No ChIP (Review only and No ChIP) and Yes ChIP cohorts
| Characteristics | No ChIP (n = 134, 31.6%) | Yes ChIP (n = 290) | p value | ||
|---|---|---|---|---|---|
| Median | IQR | Median | IQR | ||
| Age (years) | 81.0 | 66–88 | 79.50 | 69–87 | <.001 |
| ISS | 4.0 | 2–9 | 5.00 | 2–9 | .466 |
| nISS | 4.0 | 2–9 | 5.00 | 2–10 | .281 |
| AIS score chest | 2.0 | 1–3 | 1.00 | 1–3 | .308 |
| Number of radiological rib fractures | 1.0 | 0–3 | 0.00 | 0–2 | .476 |
| Time from injury to arrival (hr) | 8.8 | 1.3–51.4 | 8.38 | 1.4–46.7 | .422 |
| Charlson Comorbidity Scoreǂ | 1.0 | 0–2 | 1.00 | 0–1 | .009 |
| n (%) | 95% CI | n (%) | 95% CI | p value | |
| Male | 56 (41.8) | 33.4–50.1 | 134 (46.2) | 40.5–51.9 | .395 |
| Mechanism of injurya | |||||
| Motor vehicle collision | 11 (8.2) | 3.6–12.9 | 8 (2.8) | 0.9–4.6 | .012 |
| Vulnerable road userb | 3 (2.2) | −0.3 to 4.7 | 6 (2.1) | 0.4–3.7 | .581 |
| Fall <1 m | 98 (73.1) | 65.6–80.6 | 247 (85.2) | 81.1–89.3 | .003 |
| Fall >1 m | 13 (9.7) | 4.7–14.7 | 17 (5.9) | 3.2–8.6 | .152 |
| Other | 9 (6.7) | 2.5–11 | 12 (4.1) | 1.8–6.4 | .255 |
| Time/day of arrivalb | |||||
| In Hour (0730 –2159 hours) | 111 (83.5) | 77.2–89.7 | 229 (79) | 74.3–83.7 | .280 |
| Out Hour (2200–0729 hours) | 22 (16.5) | 10.3–22.8 | 61 (21) | 16.3–25.7 | |
| Weekday (Mon–Fri) | 93 (69.4) | 61.6–77.2 | 192 (66.2) | 60.8–71.7 | .515 |
| Weekend (Sat–Sun) | 41 (30.6) | 22.8–38.4 | 98 (33.8) | 28.3–39.2 | |
Vulnerable road user: collision involving cyclist, motorbike or pedestrian. ChIP, chest injury protocol; IQR, interquartile range; ISS, injury severity score; nISS, new injury severity score; AIS, Abbreviated Injury Scale; CI, confidence interval.
Fisher Exact Test for Charlson Score, Vulnerable road user due to small cell size.
Table 2.
Hospital treatment characteristics in the combined No ChIP (Review Only and No ChIP) and Yes ChIP cohorts
| Characteristic | No ChIP (n = 134) | Yes ChIP (n = 290) | p |
|---|---|---|---|
| Pain Team Review, n (%, 95% CI) | 26 (19.5, 12.8–26.3) | 91 (31.4, 26–36.7) | .012 |
| Med time to pain team review (hr) (IQR) | 33.6 (22.6–39.9) | 26.3 (17.5–45.3) | .732 |
| Physiotherapy review, n (%, 95% CI) | 119 (88.8, 83.5–94.1) | 270 (93.1, 90.2–96) | .135 |
| Med time to physiotherapy review (hr) (IQR) | 23.5 (16.7–36.2) | 20.1 (7.4–27.3) | .001 |
| Trauma team review, n (%, 95% CI) | 82 (61.2, 53–69.4) | 273 (94.1, 91.4–96.8) | <.001 |
| PCA used, n (%, 95% CI) | 16 (11.9, 6.5–17.4) | 47 (16.2, 12–20.4) | .251 |
| HFNP used, n (%, 95% CI) | 32 (23.9, 16.8–31) | 123 (42.4, 36.8–48.1) | <.001 |
ChIP, chest injury protocol; CI, confidence interval; IQR, interquartile range; PCA, patient controlled analgesia; HFNP, high flow nasal prong oxygen.
4.2. Results of the staff survey
4.2.1. Sample characteristics
Ninety‐nine staff members completed the survey. The majority of respondents were from the ED (68.7%), just over an eighth of respondents were from the Trauma Service (14.1%) followed by physiotherapy (8.1%). About a quarter of respondents worked as a staff specialist/VMO (26.3%) or a fellow/registrar (24.2%). About one‐sixth of respondents worked as a clinical nurse consultant/clinical nurse specialist/nursing unit manager (16.2%) or a nurse (16.2%). The majority of staff had been in their role for more than 1 year: 41.4% for 1‐5 years and 41.4% >5 years.
4.2.2. Facilitators and barriers to ChIP
Twenty‐five themes were identified to influence the implementation of ChIP in the clinical setting, 15 classified as facilitators and 10 as barriers. These themes were linked to 10 of the 14 TDF domains: knowledge; memory, attention and decision processes; behavioural regulation; professional/social role and identity; optimism; beliefs about consequences; beliefs about capabilities; reinforcement; environmental context and resources; and social influences. The themes identified from the qualitative data are presented in Table 3 with illustrative quotes. The themes identified from the quantitative data are presented in Table 4 with percentage of participant agreement/disagreement. Behaviour of both ChIP activators and ChIP responders was identified as important targets for change.
Table 3.
Summary of relevant TDF domains—qualitative data
| Domains of the TDFa | Themes | Sample quote | Facilitator/barrier |
|---|---|---|---|
| Knowledge | Not knowing what ChIP is | A teaching session about [ChIP is needed] for JMO/RMOs | Barrier |
| Not knowing what happens after ChIP activation | I think most staff in ED are not aware there is a protocol following activation; analgesia/oxygen/aperients/DVT prophylaxis. For us in ED it has been advertised as more of a referral service | Barrier | |
| Memory, attention and decision processes | Memorising the ChIP criteria | I have memorised most of the pathway, but the age and number ribs were details I would sometimes need prompting with | Barrier |
| Behavioural regulation | Needs clearer activation criteria | I think a stricter criteria for activation. On the trauma rotation as a physio, I received many pages for people in their sixties sitting in the ED waiting room waiting to go home saturating on room air. I feel these patients were not appropriate for a physio review | Barrier |
| Professional/social role and identity | ChIP aligns with professional roles | I see my job as an ED Reg is to expedite the assessment, treatment and investigation of people with blunt chest trauma and to ensure early response from the inpatient teams | Facilitator |
| Beliefs about consequences | Improved response time |
I think that instituting a protocol will most likely improve the overall response time It reminds us to think of risk factors for potential deterioration/poor outcomes in patients and expedites their appropriate management. Helps to put patients as the priority not politics |
Facilitator |
| Appropriate care |
By following the ChIP protocol, the patient receives the appropriate care and reduces potential complications due to mismanagement I have seen poorly managed older patients with rib fractures at TSH with no ChIP. They got bounced around in ED, Aged Care and Respiratory before a long stand in HDU on Day 3 when all the complications occur. I am glad that the ChIP allows patients an avenue to inpatient care with being bounced around and blunt chest wall injuries managed appropriately before complications set in |
Facilitator | |
| Better access to services | We are able to assess patients that may otherwise not receive a formal pain review | Facilitator | |
| Activated when not required |
I often feel sometimes I respond to a page and the patient does not require any physiotherapy intervention at all As a physio some ChIP activations have gone out on patients sitting in the ED waiting room walking around on room air, I feel these patients do not need PT rx |
Barrier | |
| Reinforcement | Reminders | Seeing the large yellow sign… or reminder by someone else | Facilitator |
| Environmental context and resources |
Protocol complexity After hours a problem |
Make it simple, easy to read flow chart, abolish 2 tier system Pain team and physio not seen in ED after hours (physical capability) I work only nights and it is my understanding once CHIP activated patients are reviewed the following day |
Barrier Barrier |
| Lack of time | The shift is too busy to deal with extra pages | Barrier | |
| Responder resistance |
Generally encounter resistance from surgical teams/regs [A barrier is] the perceived ineffectiveness of response and attitude of responders |
Barrier | |
| Social influences | Colleague encouragement | The staff specialists encourage ChIP | Facilitator |
| Colleague discouragement | Other colleagues may state that shouldn't be activated at Triage | Barrier |
Domains not covered by qualitative data: physical skills, cognitive and interpersonal skills, beliefs about capabilities, intentions, goals, emotion, optimism.
Table 4.
Summary of relevant TDF domains—quantitative data
| Domains of the TDFa | Themes | Question and result | Facilitator/barrier |
|---|---|---|---|
| Knowledge | Not knowing what ChIP is |
Q4. Do you know what the Chest Injury Protocol (ChIP) is? Results: 94.9% (n = 94) know what it is Q5. How would you define the Chest Injury Protocol (ChIP)? Results: 24.2% (n = 23) did not select the correct definition |
Barrier |
| Not knowing what happens after ChIP activation |
Q17. Once ChIP has been activated, I am guided as to what clinical care to give Results: Less than half of respondents (46%, n = 40) indicated that once ChIP is activated, they are guided to what clinical care to give most or all of the time. |
Barrier | |
| Memory, attention and decision processes | Remembering to activate ChIP |
Q14. Are there times when you are likely to forget to activate the ChIP page? Results: 38.3% (n = 23) sometimes forget to activate the ChIP page but given the high rate of eligible patients not receiving a call this could be a potential problem |
Barrier |
| Behavioural regulation | Protocol complexity |
Q19. The ChIP protocol is too specific (not enough clinical discretion) Results: Response is mixed. About two‐thirds (67.1%, n = 57) of respondents disagree or somewhat disagree with this statement. 15.3% (n = 13) agree or strongly agree with this statement. Q20. The ChIP protocol is too complicated Results: About three quarters (75.3%, n = 64) of respondents disagree or somewhat disagree with this statement. |
Barrier |
| Professional/social role and identity | Recognising importance of own role in ChIP |
Q8. Do you think that your role in ChIP is important? Results: 90.9% (n = 90) of responders believe their role in ChIP is important |
Facilitator |
| Beliefs about capabilities | Not knowing how/when to activate ChIP |
Q9. Do you know when to active the ChIP page? Results: 98.3% (n = 59) responded they knew when to activate the ChIP page most of/all of the time however only 68.4% of eligible patients received a call Q10. Do you know how to activate the ChIP page? Results: 91.7% (n = 55) know how most of/all of the time. Q11. Do you feel confident in activating the ChIP page or suggesting it should be activated? Results: 91.4% (n = 64) feel confident in activating/suggesting ChIP be activated Q15. I am always certain when to activate ChIP Result: 73.3% (n = 44) are certain most/all of the time when to activate ChIP |
Barrier |
| Optimism | Expedited responses |
Q24. Do you think there is a need for an expedited (quick and early) response from the trauma or surgical team (less than 60 minutes) for patients with blunt chest injury? Results: 57.6% (n = 49) of respondents felt that patients with blunt chest injury require an expedited response Q25. Do you think there is a need for early intervention from a physiotherapist for patients with blunt chest injury? Results: 87.1% (n = 74) respondents felt that patients with blunt chest injury require an early intervention from a physiotherapist Q26. Do you think there is a need for a expedited (quick and early) response from the pain team for patients with blunt chest injury? Results: 71.8% (n = 61) of respondents felt that patients with blunt chest injury require an expedited response from the pain team |
Facilitator |
| Beliefs about consequences | Improved patient outcomes |
Q28. Do you think that ChIP has led to improved patient outcomes? Results: About two‐thirds of respondents (65.5%, n = 55) believe the ChIP protocol improves patient outcomes |
Facilitator |
| Improved response time |
Q27. Do you think that the ChIP protocol achieves an expedited response? Results: Three quarters of respondents (75.0%, n = 63) believe the ChIP protocol achieves an expedited response Q29‐36. Do you think ChIP has improved any of the following? Early analgesia/time to physiotherapy review/time to admitting team review/time to decision to admit/reducing length of time in the emergency department/time to pain team review/overall patient care/overall admission process Results: The majority of respondents saw improvements with ChIP for overall patient care (75.9%) most or all of the time, for example, early analgesia (57.8%, n = 48), time to physiotherapy review (55.4%, n = 46), time to admitting team review (60.2, n = 50), time to decision to admit (62.7, n = 52) and the overall admission process (71.1%, n = 59) |
Facilitator | |
| Appropriateness of service |
Q38. Do you ever feel that the surgical review is not necessary on ChIP patients? Results: Mixed response from responders (n = 20), 15% said N/A, 25% said never, 35% said rarely, 10% said sometimes, 15% said all the time. Q39. Do you ever feel that early physiotherapy review is not needed on ChIP patients? Results: Mixed response from responders (n = 20), 25% said N/A, 30% said never, 25% said rarely, 5% said sometimes, 15% said all the time. Q40. Do you ever feel that early pain team review is not needed on ChIP patients? Results: Most responders (75.0%, n = 15) said this is never or rarely the case |
Barrier | |
| Reinforcement | Reminders |
Q12. Do people you work with remind or suggest you activate the ChIP page? Results: 74.3% (n = 52) of respondents say work colleagues remind/suggest they activate the ChIP page sometimes, most of the time or all of the time Q13. Do you remind or suggest to others to activate the ChIP page? Results: 90.0% (n = 63) of respondents say they sometimes, most of the time or all of the time remind others activate the ChIP page |
Facilitator |
| False activation |
Q37. Do you experience false activations, that is, patients that do not meet ChIP criteria? Results: 82.6% (n = 19) believe that at some point they have experienced a false activation |
Barrier | |
| Environmental context and resources | Lack of prompt response |
Q21. When ChIP is activated, the required responders attend promptly Results: Less than half (47.1%, n = 40) of respondents felt that when ChIP was activated, the required responders attend promptly Q41. Are you able to respond to a ChIP page within the 60 minutes required? Results: 90.0% (n = 18) of responders unable to respond in 60 min |
Barrier |
Domains not covered by quantitative data: Physical skills, cognitive and interpersonal skills, intentions, goals, emotion, social influences.
4.2.3. Interventions for promoting uptake of ChIP
The ten TDF domains of behaviour requiring enhancement or modification to optimise the implementation of ChIP corresponded with all nine intervention functions in the BCW. Seven of these intervention functions met the APEASE criteria and were selected to address the target behaviours including: “training”; “education”; “environmental restructuring”; “enablement”; “persuasion”; “incentivisation”; and “modelling.” Behaviour change techniques in the BCTTv1 corresponded and overlapped with the selected interventions selected from the BCW. Behaviour change techniques, which met the APEASE criteria as well as relevant modes of delivery, were selected to implement the seven intervention functions. The modes of delivery although common to multiple behaviour change techniques and intervention functions were refined and mapped to specific targets behaviours for change. Face‐to‐face consultation around the suitability of each BCT was conducted with the heads of departments and senior and junior clinicians from each impacted service (Table 5—see Appendix S2).
5. Discussion
This study applied a systematic process to identify potential intervention options to improve the uptake of a blunt chest injury protocol known to improve patient outcomes. Only 68.4% of patients received a ChIP call. Comparison of patients that did and did not receive ChIP demonstrated no demographic or clinically relevant difference between the groups. This suggested that staff behaviour was the primary cause of the lack of activation. An analysis of quantitative and qualitative data obtained from a TDF‐based staff survey identified a range of influences on the target behaviour, that is, activating the ChIP protocol when appropriate. Seven domains were identified as priority targets for future intervention efforts: “training”; “education”; “environmental restructuring”; “enablement”; “persuasion”; “incentivisation”; and “modelling.” Both staff that activate, and staff that respond to the protocol were the targets for behaviour change.
5.1. Revising the protocol
One of the overwhelming themes identified from the survey respondents was around the structure and content of the protocol. In particular, it was too complicated, and, it did not provide information on what clinical treatments to initiate in the ED. Hence, a revision of the protocol was conducted to address the intervention functions of education, training and enablement. This process was multifaceted. First, a formal review of the literature was undertaken seeking any new evidence to inform the clinical management content of the protocol (Unsworth et al., 2015). Informed by the literature review and user feedback, the protocol was updated to include treatment recommendations to guide the responding clinician. The algorithm/flow chart summarising the protocol was updated to reflect the revised protocol and simplified (see Figure 2). This draft revision was then circulated to and revised by the heads of department. The heads of department consulted with their respective staff about the revised protocol. Further modifications were then conducted. For example, the physiotherapists reported that they often attend the ED to review the patient; however, the patient has not had sufficient time between administration of analgesia to be able to undergo chest physiotherapy. This resulted in the physiotherapist having to leave the ED and reassess later, wasting their time. To address this barrier to physiotherapy response and effective clinical intervention, the protocol now states that the physiotherapist should liaise with the treating trauma nurse prior to review of the patient to ascertain readiness of the patient for physiotherapy assessment and treatment.
Figure 2.
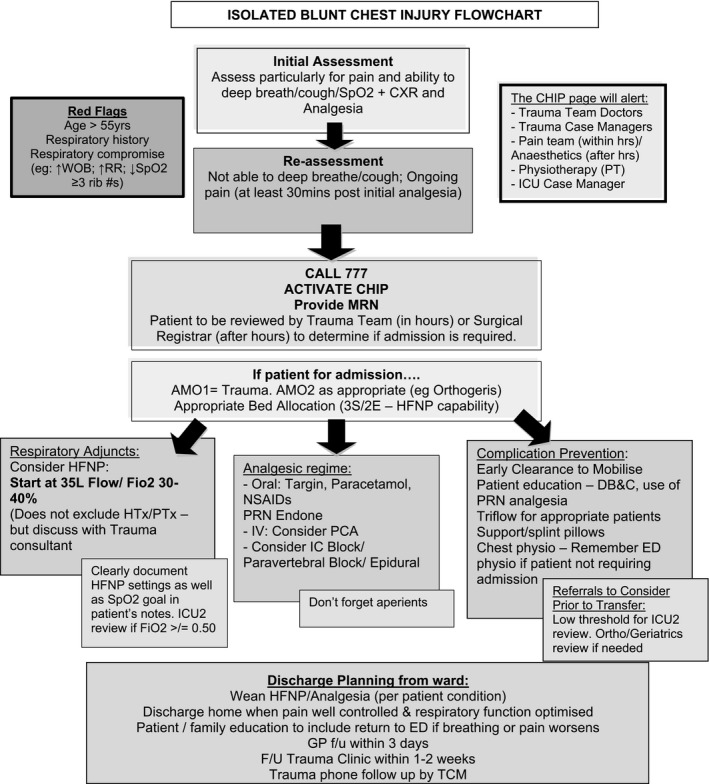
Revised Blunt Chest Injury Protocol informed by clinical evidence and behaviour change theory
5.2. Relaunch of the protocol
A strategy to relaunch and re‐implement the protocol was developed is based on the findings of this study. This strategy is also multifaceted with multiple targets and primarily focussed on the intervention functions of education, training, coercion, incentivisation, environmental restructuring and modelling and included a video https://www.youtube.com/my_videos?o=U.
The medical record review demonstrated that patients who did not receive the ChIP protocol were predominantly treated by junior emergency medical staff (registrars and residents). The reasons for this could be threefold. First, junior medical staff have a high rate of rotation, so may only work in the ED for three to six months. Although they attend orientation, there are myriad protocols to remember and act upon. Further, the demanding ED clinical environment makes the conduct of quality patient assessments challenging. Patients are more vulnerable to clinical error and adverse events due to excessive workload and time pressures (Flowerdew, Brown, Russ, Vincent, & Woloshynowych, 2012), frequent interruptions (Berg et al., 2013) and multitasking(Laxmisan et al., 2007) common to the ED. In Australia and worldwide, EDs are experiencing growing demands by the public for increased healthcare services. Studies across Europe, United States, Canada and Australia have similarly reported rapid increases in patient presentations to EDs and issues of overcrowding making it challenging to deliver high quality and safe patient care (Drummond, 2002; Forero et al., 2010; Hoot & Aronsky, 2008; Jayaprakash, O'Sullivan, Bey, Ahmed, & Lotfipour, 2009; Lowthian et al., 2011; Nagree et al., 2013; Pitts, Pines, Handrigan, & Kellermann, 2012; Sprivulis, Da Silva, Jacobs, Frazer, & Jelinek, 2006).
The relaunch of this protocol aims to reduce some of the workload and time pressures for junior medical staff by activating and expediting an automated multidisciplinary response by the clinicians who will provide the ongoing care for the patient following discharge from the ED. That activating the protocol will achieve a reduction in the junior medical staff workload, and improve patients outcomes will be regularly communicated by the senior ED and trauma medical and nursing staff. Monitoring of the activation of the protocol will continue; however, the trauma staff who oversee this monitoring have committed to providing more real‐time feedback and around junior medical staff behaviour.
5.3. Roles of nurses
Another strategy to enable junior medical staff is the empowerment of nursing staff to prompt or activate the protocol. Nursing staff are a more stable workforce in the ED and possess a broad knowledge base and range of assessment skills to competently assess and care for patients of different ages (Munroe, Curtis, Murphy, Strachan, & Buckley, 2015). Patients who present to the ED are frequently assessed and receive treatment commenced by emergency nurses before being seen by a medical officer (Scott, Considine, & Botti, 2015). Despite this, some early career nurses lack confidence in their clinical practice and ability to make decisions (Baumberger‐Henry, 2012), and, with nursing workforce shortages, there is an increasing number of new graduate nurses are seeking and gaining direct entry to ED (Baumberger‐Henry, 2012; Glynn & Silva, 2013).
Education, persuasion, social support and modelling will be used to empower and enhance the self‐efficacy of the ED nurses. Self‐efficacy is the belief in one's capability to perform a given behaviour or course of action and higher levels of self‐efficacy is associated with better assessment performance of emergency nurses (Hollingsworth & Ford‐Gilboe, 2006). Enhancing the self‐efficacy of emergency nurses when performing assessments has the potential to improve their ability to carrying out urgent tasks and improve patient outcomes. Likewise with the junior medical staff, the trauma staff who oversee monitoring of the protocol activation have committed to providing more real‐time feedback and around nursing staff behaviour.
5.4. Enhancing motivation and opportunity
Enhancement of the motivation and opportunity of activators and responders to ChIP is critical to the success of the revised protocol. Education is central to this, which is dependent on the support of the heads of departments. Each department has difference modes and availability of education for their staff and a plan will be developed in consultation with the heads of departments to ensure the revised protocol, and the rates of activation (as determined by the ongoing monitoring by the trauma service) features in education sessions, orientation and quality assurance meetings. Further to departmental clinical practice meetings and presentations, alternate forms of prompts will be implemented. For example, in the anaesthetics department tearoom, they use a 24/7 rotating slide show on a large screen as an adjunct to ongoing education. This slide show contains clinical updates, holiday photographs (to engage staff) and reminders. Each slide remains on the screen for 90 seconds. The protocol update will be included in this slide show. This mode of information sharing/prompting was unique to the Anaesthetic department, and the process of consultation with heads of departments around suitable BCTTv1 resulted in similar interventions being adapted for other departments. For example, this same concept will also be introduced to the ED tearoom, and has been approved by ED senior nurse manager and director. Purchasing of a screen by the ED is underway.
5.5. Limitations
There were some limitations to this study. The selection of intervention strategies was subject to some interpretation, and the selection of BCT limited to a core group of key stakeholders. Evaluation of the effectiveness of the selected implementation strategies and BCTs will overcome any subjectivity and generate evidence on the effectiveness of the proposed implementation strategy.
The revised protocol now includes a blunt chest injury “care bundle,” or a uniform set of evidence‐based practices specific to a clinical presentation to be considered by the attending team (Resar et al., 2005). The individual components of this bundle are well supported in the literature for improving outcomes in patients with blunt chest trauma (Unsworth et al., 2015). Further implementation and evaluation of ChIP could validate and formalise the blunt chest injury “care bundle” across difference care settings. Finally, the ongoing monitoring of the activation of the revised protocol will enable evaluation of effectiveness of revised protocol and implementation strategy. For example, monitoring in the four month period immediately following the launch of the revised protocol indicates appropriate uptake of CHIP increased from 68% to 91%.
6. Conclusions
This study has demonstrated how the behaviour change wheel may be used to revise and improve a clinical protocol in the ED context. Intervention strategies and behaviour change techniques have been integrated into the redesign, improvement and re‐ implementation strategy of an evidence‐informed early activation protocol known to expedite care and improve outcomes of patients with isolated blunt chest injury.
7. Relevance to Clinical Practice
Newly implemented clinical protocols should incorporate clinician behaviour change assessment, strategy and interventions. Enhancing the self‐efficacy of emergency nurses when performing assessments has the potential to improve patient outcomes and should be included in implementation strategy.
Conflict of Interest
All authors report no conflict of interest.
Contributions
KC, CV and SA conceived and designed the study. KC oversaw all aspects of the study. KC, SA and AU conducted data acquisition. AC oversaw implementation of the intervention. ML conducted the statistical data analysis. CV conducted the quantitative and qualitative survey analysis. KC, CV and LA conducted the behaviour change wheel analysis and interpretation. All authors have been actively involved in the drafting and critical revision of the manuscript.
Supporting information
Curtis K, Van C, Lam M, et al. Implementation evaluation and refinement of an intervention to improve blunt chest injury management—A mixed‐methods study. J Clin Nurs. 2017;26:4506–4518. 10.1111/jocn.13782
Funding information
KC is supported by a Translation of Research into Practice grant (GNT1067639_Curtis, 2013‐15) from the National Health and Medical Research Council
References
- Baker, S. P. , O'Neill, B. , Haddon, W. , & Long, W. B. (1974). The injury severity score: A method for describing patients with multiple injuries and evaluating emergency care. Journal of Trauma and Acute Care Surgery, 14(3), 187–196. [PubMed] [Google Scholar]
- Batmanian, J. J. , Lam, M. , Matthews, C. , Finckh, A. , Duffy, M. , Wright, R. , … Markus, R. (2007). A protocol‐driven model for the rapid initiation of stroke thrombolysis in the emergency department. Medical Journal of Australia, 187(10), 567–570. [DOI] [PubMed] [Google Scholar]
- Baumberger‐Henry, M. (2012). Registered nurses’ perspectives on the new graduate working in the Emergency Department or Critical Care Unit. The Journal of Continuing Education in Nursing & Health Care Perspectives, 43(7), 299–305. [DOI] [PubMed] [Google Scholar]
- Bennetts, S. , Campbell‐Brophy, E. , Huckson, S. , Doherty, S. , National Health & Medical Research Council's National Institute for Clinical Studies National Emergency Care Pain Management Initiative (2012). Pain management in Australian emergency departments: Current practice, enablers, barriers and future directions. Emergency Medicine Australasia, 24(2), 136–143. [DOI] [PubMed] [Google Scholar]
- Berg, L. M. , Källberg, A. S. , Göransson, K. E. , Östergren, J. , Florin, J. , & Ehrenberg, A. (2013). Interruptions in emergency department work: An observational and interview study. British Medical Journal Quality and Safety, 22(8), 565–663. [DOI] [PubMed] [Google Scholar]
- Bulger, E. M. , Arneson, M. A. , Mock, C. N. , & Jurkovich, G. J. (2000). Rib fractures in the elderly. The Journal of Trauma, 48(6), 1040–1046. [DOI] [PubMed] [Google Scholar]
- Cane, J. , O'Connor, D. , & Michie, S. (2012). Validation of the theoretical domains framework for use in behaviour change and implementation research. Implementation Science, 7(1), 37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charlson, M. E. , Pompei, P. , Ales, K. L. , & MacKenzie, C. R. (1987). A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. Journal of Chronic Diseases, 40(5), 373–383. [DOI] [PubMed] [Google Scholar]
- Copes, W. S. , Champion, H. R. , Sacco, W. J. , Lawnick, M. M. , Gann, D. S. , Gennarelli, T. , … Schwaitzberg, S. (1990). Progress in characterizing anatomic injury. The Journal of Trauma, 30(10), 1200–1207. [DOI] [PubMed] [Google Scholar]
- Crandall, J. , Kent, R. , Patrie, J. , Fertile, J. , & Martin, P. (2000) Rib fracture patterns and radiologic detection—A restraint‐based comparison. In Annual proceedings/association for the advancement of automotive medicine, Vol. 44 Association for the Advancement of Automotive Medicine, pp. 235. [PMC free article] [PubMed]
- Curtis, K. , Asha, S. E. , Unsworth, A. , Lam, M. , Goldsmith, H. , Langcake, M. , & Dwyer, D. (2016). ChIP: An early activation protocol for isolated blunt chest injury improves outcomes, a retrospective cohort study. Australasian Emergency Nursing Journal, 19, 127–132. [DOI] [PubMed] [Google Scholar]
- Curtis, K. , Ramsden, C. , & Lord, B. (2011). Emergency and trauma care: For nurses and paramedics. Sydney: Elsevier Australia. [Google Scholar]
- Davis, K. A. , Cabbad, N. C. , Schuster, K. M. , Kaplan, L. J. , Carusone, C. , Leary, T. , & Udelsman, R. (2008). Trauma team oversight improves efficiency of care and augments clinical and economic outcomes. The Journal of Trauma, 65(6), 1236–1242; discussion 1242–1244. [DOI] [PubMed] [Google Scholar]
- Drummond, A. (2002). No room at the inn: Overcrowding in Ontario's emergency departments. Canadian Journal of Emergency Medicine, 4(2), 91–97. [DOI] [PubMed] [Google Scholar]
- Flowerdew, L. , Brown, R. , Russ, S. , Vincent, C. , & Woloshynowych, M. (2012). Teams under pressure in the emergency department: An interview study. Emergency Medicine Journal, 29(12), e2. [DOI] [PubMed] [Google Scholar]
- Forero, R. , Hillman, K. , McCarthy, S. , Fatovich, D. M. , Joseph, A. P. , & Richardson, D. B. (2010). Access block and ED overcrowding. Emergency Medicine Australasia, 22(2), 119–135. [DOI] [PubMed] [Google Scholar]
- French, S. , Green, S. , O'Connor, D. , McKenzie, S. , Francis, J. , Michie, S. , … Grimshaw, J. (2012). Developing theory‐informed behaviour change interventions to implement evidence into practice: A systematic approach using the Theoretical Domains Framework. Implementation Science, 7, 38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glynn, P. , & Silva, S. (2013). Meeting the needs of new graduates in the emergency department: A qualitative study evaluating a new graduate internship program. Journal of Emergency Nursing, 39(2), 173–178. [DOI] [PubMed] [Google Scholar]
- Grol, R. , & Grimshaw, J. (2003). From best evidence to best practice: Effective implementation of change in patients’ care. Lancet, 362(9391), 1225–1230. [DOI] [PubMed] [Google Scholar]
- Haynes, B. , & Haines, A. (1998). Getting research findings into practice: Barriers and bridges to evidence based clinical practice. British Medical Journal, 317(7153), 273–276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holcomb, J. B. , McMullin, N. R. , Kozar, R. A. , Lygas, M. H. , & Moore, F. A. (2003). Morbidity from rib fractures increases after age 45. Journal of the American College of Surgeons, 196(4), 549–555. [DOI] [PubMed] [Google Scholar]
- Hollingsworth, E. , & Ford‐Gilboe, M. (2006). Registered nurses’ self‐efficacy for assessing and responding to woman abuse in emergency department settings. The Canadian Journal of Nursing Research, 38(4), 54–77. [PubMed] [Google Scholar]
- Hoot, N. , & Aronsky, D. (2008). Systematic review of emergency department crowding: Causes, effects and solutions. Annals of Emergency Medicine, 52(2), 126–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsieh, H. F. , & Shannon, S. E. (2005). Three approaches to qualitative content analysis. Qualitative Health Research, 15(9), 1277–1288. [DOI] [PubMed] [Google Scholar]
- Jayaprakash, N. , O'Sullivan, R. , Bey, T. , Ahmed, S. S. , & Lotfipour, S. (2009). Crowding and delivery of healthcare in emergency departments: The European perspective. The Western Journal of Emergency Medicine, 10(4), 233–239. [PMC free article] [PubMed] [Google Scholar]
- Kent, R. , Woods, W. , & Bostrom, O. (2008). Fatality risk and the presence of rib fractures. Annals of Advances in Automotive Medicine ‐ 52nd Annual Scientific Conference, 52, 73–82. [PMC free article] [PubMed] [Google Scholar]
- Kerr‐Valentic, M. A. , Arthur, M. , Mullins, R. J. , Pearson, T. E. , Mayberry, J. C. , Hicks, B. A. , … Barquist, E. (2003). Rib fracture pain and disability: Can we do better? The Journal of Trauma, 54(6), 1058–1064. [DOI] [PubMed] [Google Scholar]
- Laxmisan, A. , Hakimzada, F. , Sayan, O. R. , Green, R. A. , Zhang, J. , & Patel, V. L. (2007). The multitasking clinician: Decision‐making and cognitive demand during and after team handoffs in emergency care. International Journal of Medical Informatics, 76(11–12), 801–811. [DOI] [PubMed] [Google Scholar]
- Légaré, F. (2009) Section 3.4 Assessing barriers and facilitators to knowledge use In: Knowledge translation in health care: Moving from evidence to practice , Canadian Institutes of Health Research. Retrieved from http://www.cihr-irsc.gc.ca/e/42293.html on 13 July 2016
- Leone, M. , Brégeon, F. , Antonini, F. , Chaumoître, K. , Charvet, A. , Ban, L. H. , … Martin, C. (2008). Long‐term outcome in chest trauma. Anesthesiology, 109(5), 864–871. [DOI] [PubMed] [Google Scholar]
- Lowthian, J. , Curtis, A. , Cameron, P. , Stoelwinder, J. , Cooke, M. , & McNeil, J. (2011). Systematic review of trends in emergency department attendances: An Australian perspective. Emergency Medicine Journal, 28(5), 373–377. [DOI] [PubMed] [Google Scholar]
- Menditto, V. G. , Gabrielli, B. , Marcosignori, M. , Screpante, F. , Pupita, G. , Polonara, S. , … Pomponio, G. (2012). A management of blunt thoracic trauma in an emergency department observation unit: Pre‐post observational study. The Journal of Trauma and Acute Care Surgery, 72(1), 222–228. [DOI] [PubMed] [Google Scholar]
- Michie, S. , Atkins, L. , & West, R. (2014). The behaviour change wheel: A guide to designing interventions. London: Silverback Publishing. [Google Scholar]
- Michie, S. , Richardson, M. , Johnston, M. , Abraham, C. , Francis, J. , Hardeman, W. , … Wood, C. E. (2013). The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: Building an international consensus for the reporting of behavior change interventions. Annals of Behavioral Medicine, 46(1), 81–95. [DOI] [PubMed] [Google Scholar]
- Munroe, B. , Curtis, K. , Murphy, M. , Strachan, L. , & Buckley, T. (2015). HIRAID: An evidence‐informed emergency nursing assessment framework. Australasian Emergency Nursing Journal, 18(2), 83–97. [DOI] [PubMed] [Google Scholar]
- Nagree, Y. , Camarda, V. , Fatovich, D. , Cameron, P. A. , Dey, I. , Gosbell, A. D. , McCarthy, S. M. , & Mountain, D. (2013). Quantifying the proportion of general practice and low‐acuity patients in the emergency department. The Medical Journal of Australia, 198(11), 612–615. [DOI] [PubMed] [Google Scholar]
- NSW Agency for Clinical Innovation (2014) Centre for Healthcare Redesign. Retrieved from: http://www.aci.health.nsw.gov.au/centre-for-healthcare-redesign on 13 July 2016.
- Pitts, S. R. , Pines, J. M. , Handrigan, M. T. , & Kellermann, A. L. (2012). National trends in emergency department occupancy, 2001 to 2008: Effect of inpatient admissions versus emergency department practice intensity. Annals of Emergency Medicine, 60(6), 679–686. [DOI] [PubMed] [Google Scholar]
- Resar, R. , Pronovost, P. , Haraden, C. , Simmonds, T. , Rainey, T. , & Nolan, T. (2005). Using a bundle approach to improve ventilator care processes and reduce ventilator‐associated pneumonia. Joint Commission Journal on Quality and Patient Safety, 31(5), 243–248. [DOI] [PubMed] [Google Scholar]
- Runciman, W. B. , Hunt, T. D. , Hannaford, N. A. , Hibbert, P. D. , Westbrook, J. I. , Coiera, E. W. , … Braithwaite, J. (2012). CareTrack: Assessing the appropriateness of health care delivery in Australia. The Medical Journal of Australia, 197(2), 100–105. [DOI] [PubMed] [Google Scholar]
- Sahr, S. M. , Webb, M. L. , Renner, C. H. , Sokol, R. K. , & Swegle, J. R. (2013). Implementation of a rib fracture triage protocol in elderly trauma patients. Journal of Trauma Nursing, 20(4), 172–175. [DOI] [PubMed] [Google Scholar]
- Scott, B. M. , Considine, J. , & Botti, M. (2015). Unreported clinical deterioration in emergency department patients: A point prevalence study. Australasian Emergency Nurses Journal, 18(1), 33–41. [DOI] [PubMed] [Google Scholar]
- Sesperez, J. , Wilson, S. , Jalaludin, B. , Seger, M. , & Sugrue, M. (2001). Trauma case management and clinical pathways: Prospective evaluation of their effect on selected patient outcomes in five key trauma conditions. The Journal of Trauma, 50(4), 643–649. [DOI] [PubMed] [Google Scholar]
- Shaban, R. Z. , Holzhauser, K. , Gillespie, K. , Huckson, S. , & Bennetts, S. (2012). Characteristics of effective interventions supporting quality pain management in Australian emergency departments: An exploratory study. Australasian Emergency Nursing Journal, 15(1), 23–30. [DOI] [PubMed] [Google Scholar]
- Sprivulis, P. , Da Silva, J. , Jacobs, I. , Frazer, A. , & Jelinek, G. (2006). The association between hospital overcrowding and mortality among patients admitted via Western Australian emergency departments. The Medical Journal of Australia, 184(5), 208–212. [DOI] [PubMed] [Google Scholar]
- Testerman, G. M. (2006). Adverse outcomes in younger rib fracture patients. Southern Medical Journal, 99(4), 335–359. [DOI] [PubMed] [Google Scholar]
- Todd, S. R. , McNally, M. M. , Holcomb, J. B. , Kozar, R. A. , Kao, L. S. , Gonzalez, E. A. , … Moore, F. A. (2006). A multidisciplinary clinical pathway decreases rib fracture‐associated infectious morbidity and mortality in high‐risk trauma patients. American Journal of Surgery, 192(6), 806–811. [DOI] [PubMed] [Google Scholar]
- Unsworth, A. , Curtis, K. , & Asha, S. (2015). Treatments for blunt chest trauma and their impact on patient outcomes and health service delivery. Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine, 23(1), 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallis, L. (2012). Barriers to implementing evidence‐based practice remain high for U.S. nurses: Getting past “we've always done it this way” is crucial. The American Journal of Nursing, 112(12), 15. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials


