Abstract
High blood pressure (BP) is a highly prevalent modifiable cause of cardiovascular disease, stroke, and death. Accurate BP measurement is critical, given that a 5-mmHg measurement error may lead to incorrect hypertension status classification in 84 million individuals worldwide. This position statement summarizes procedures for optimizing observer performance in clinic BP measurement, with special attention given to low-to-middle-income settings, where resource limitations, heavy workloads, time constraints, and lack of electrical power make measurement more challenging. Many measurement errors can be minimized by appropriate patient preparation and standardized techniques. Validated semi-automated/automated upper arm cuff devices should be used instead of auscultation to simplify measurement and prevent observer error. Task sharing, creating a dedicated measurement workstation, and using semi-automated or solar-charged devices may help. Ensuring observer training, and periodic re-training, is critical. Low-cost, easily accessible certification programs should be considered to facilitate best BP measurement practice.
Keywords: blood pressure, blood pressure measurement, consensus statement, global health, hypertension, oscillometry
INTRODUCTION
High blood pressure (BP) is the leading modifiable risk factor for death and disability in the world, affecting an estimated 1.4 billion adults globally, and leading to over 10 million deaths per year [1,2]. It is a leading cause of heart disease, stroke, and chronic kidney disease and a major contributor to escalating healthcare costs [3]. With an overall global adult prevalence of 31%, high BP is highly prevalent in all major regions of the world [2]. However, in absolute numbers, it is low-to-middle income countries (LMICs) that bear the highest burden of illness, having over one billion individuals affected, and possessing awareness, treatment and control proportions that lag high-income countries to a considerable degree [2]. Accordingly, ongoing efforts to improve the diagnosis, prevention, treatment, and control of hypertension globally must include tailored interventions that prioritize reductions in regional disparities [4].
Accurate and reliable BP measurement is essential for the proper diagnosis and management of hypertension [5]. On a population-wide level, a 5-mmHg difference in SBP corresponds to an estimated 6% absolute and 30% relative change in hypertension prevalence [6]. Accordingly, the effect of a 5-mmHg error in BP measurement, assuming a global prevalence of 1.4 billion [2], could lead to the incorrect classification of hypertension status in 84 million individuals worldwide. Therefore, the ramifications of inaccurate measurement on a global level are profound.
Blood pressure is a physiological parameter that changes constantly in response to endogenous factors and exogenous stimuli [7]. This variability makes assessment of ‘usual’ BP, which is defined as an individual's true or genuine BP, challenging. BP measurement is perhaps the most commonly performed procedure in clinical medicine and, although, at first glance, it seems simple, in reality, many steps must be performed sequentially and optimally in order to produce a reproducible result reflective of usual BP. Accordingly, the individual responsible for measuring BP, herein referred to as the ‘observer’, must be meticulous in terms of following recommended techniques [8]. The challenges posed by the variable nature of BP were recognized over a century ago by Riva-Rocci et al.[9], who noted that taking multiple measurements and standardizing the measurement conditions could optimize use of the technique in clinical practice. He concludes, in his seminal paper written in 1896, that ‘… if the procedures are neglected, and the doctor is satisfied with a crude reading, the method will become useless and will be quickly abandoned as a scientists’ indulgence’ [9].
Unfortunately, in contemporary clinical practice, BP measurement is often suboptimally performed, and this type of unstandardized BP measurement leads to errors that can inappropriately alter management decisions in 20–45% of cases [10–13]. The problem of unstandardized BP measurement has persisted for decades despite extensive education and substantial efforts to raise awareness on the adverse consequences of inaccurate clinic BP measurement [5,14]. Time constraints and suboptimal technique leading to poorly performed auscultation are responsible for much of this error [10,15]. Potential solutions to minimize error, discussed below, include simplifying the measurement process by using automated devices and encouraging observers to undergo certified training and re-training to promote ongoing use of standardized measurement techniques.
The aim of the Lancet Commission on Hypertension was to identify key actions to improve the global management of BP both at the population and the individual levels, and to generate a campaign to adopt the suggested actions at national levels to reduce the impact of elevated BP globally [4]. The purpose of this position statement is to provide guidance towards optimizing observer-related clinic BP measurement performance for hypertension diagnosis and treatment, with special attention given to measurement in LMIC settings. We begin with a brief review of different measurement modalities, including a discussion of optimal measurement technique and the errors that result from deviating from standardized measurement practices. We then outline the impact of observer training on performance of BP measurement. Subsequently, we discuss BP measurement in LMIC settings, specifically the practical considerations that limit achievement of best practice. We close with recommendations for optimizing observer accuracy in clinic BP measurement and provide suggestions on future directions.
TYPES OF BLOOD PRESSURE MEASUREMENT USED IN CLINICAL PRACTICE AND OPTIMAL MEASUREMENT TECHNIQUE
Direct (or intra-arterial) and indirect (cuff-based) BP measurement are the two major methods employed in the clinical care setting and are summarized in Table 1. Indirect measurement is typically performed via auscultation or by using a semi-automated or fully automated device, which most often uses the oscillometric technique (Table 1). Although there are definitions in the literature for semi-automated and automated BP measurements, herein we refer to semi-automated as those devices that require a manual inflation (e.g. with using bulb compressions). Once inflation has been completed, these devices typically use an automated deflation process to determine BP. In contrast, fully automated devices have automated inflation and deflation – the user initiates a measurement, usually by pressing a button, and the remainder of the inflation–deflation process is automated. Automated office BP (AOBP) measurement is a subtype of automated measurement that involves taking sequential automated measurements rather than a single measurement at a time. In the oscillometric technique, arterial pulses are first sensed, filtered, processed and, then, a proprietary algorithm is applied to estimate BP [16].
TABLE 1.
Blood pressure measurement methods commonly used in clinical practice
| Measurement method | Comment |
| Direct (intra-arterial) | Commonly used in the critical care setting, where detecting short-term BP changes is essential. |
| Indirect | Commonly used outside of the critical care setting. Upper arm cuff BP measurement is preferred. |
| Auscultation | A good technique, if performed optimally, because SBP and DBP correspond to distinctly detectable physiological phenomena – the appearance and disappearance of the Korotkoff sounds, respectively. However, rarely performed properly in clinical practice, which is a major limitation. Can be performed using a mercury, aneroid, or electronic sphygmomanometer. Mercury has been banned in many jurisdictions and aneroid sphygmomanometers contain moving parts that require frequent calibration, which is often not performed, limiting accuracy over time. Simultaneous, two-observer, blinded, auscultatory measurement performed according to standardized methods using a mercury sphygmomanometer and a proper bladder size is the reference standard for BP validation studies but is too impractical for clinical practice. |
| Semi-automated or fully automated | Both approaches typically use the oscillometric technique, although, rarely, a fully automated device may employ electronic auscultation or both. Semiautomated devices are not commonly used but may be advantageous in LMIC settings as inflation is performed manually (obviating the need for a power source). Semiautomated deflation is device-controlled. Fully automated devices control both inflation and deflation. An important issue with automated devices is that many available on the market have not been properly validated for measurement accuracy. Major advantages of automated BP measurement that make it the preferred technique to use in the clinic include simplification of the measurement process and elimination of observer-related errors in auscultation. Automated office BP (AOBP) measurement offers the ability to take multiple, sequential, unobserved measurements (reducing white-coat effect), but these devices are relatively costly and may require more space and time in the clinical visit – further research to define their role is needed. Outside of the clinic setting, automated home and ambulatory BP measurement modalities provide superior diagnostic and prognostic capabilities relative to clinic measurements, including detection of white-coat and masked hypertension effect. If resources allow, use of AOBP, home and ambulatory BP measurement is recommended. A disadvantage is that the oscillometric technique indirectly estimates BP (i.e. no discrete ‘oscillometric’ physiological phenomena that herald the occurrence of systole and diastole exist) and is less accurate in some patients. In addition, the proprietary nature of the algorithm makes it difficult to consider oscillometry as a singular measurement method and makes device (and algorithm) validation a critically important consideration in automated device selection for clinical use. |
BP, blood pressure; LMIC, low-to-middle-income countries.
BP measurement should be performed carefully by a trained observer using standardized methodology (Table 2 and Fig. 1; Supplementary Figures S1–S5) [5]. The mean of multiple research quality auscultatory and, more recently, automated oscillometric measurements, sometimes taken over two or more clinical visits, was the method used to estimate the usual BP in many foundational prognostic and therapeutic studies in the field of hypertension [17–19]. Multiple readings over time are required to estimate the usual BP, allow for regression to the mean, and reduce the white-coat effect [20].
TABLE 2.
Essential elements of performing a standardized clinic blood pressure measurement
| Element | Comment |
| Device | |
| Use a calibrated (for aneroid devices) or clinically validated (for automated devices) instrument. | Mercury columns should be at zero when at rest and the mercury column should be fully intact and readable. Aneroid devices require regular calibration. Electronic devices should be validated against two-observer mercury-based auscultation in an independently performed clinical study using an internationally accepted protocol. Validated device listings are available at https://bihsoc.org/bp-monitors and https://hypertension.ca/hypertension-and-you/managing-hypertension/measuring-blood-pressure/devices/. |
| Preparation and positioning | |
| Aneroid devices or mercury columns should be clearly visible at eye level. | |
| The patient should be resting comfortably in a quiet environment for 5 min in a chair in the seated position, back-supported, legs uncrossed, feet flat on the floor, and the arm supported with the BP cuff at heart level. | There should be no talking by the patient or observer during the entire measurement procedure. The patient should have an empty bladder and not have eaten, ingested caffeine, smoked, or engaged in physical activity at least 30 min prior to the measurement. |
| Cuff | |
| Inflatable bladder width should be about 40% of arm circumference and bladder length should be about 80–100% of arm circumference. For electronic devices, select cuff size as recommended by the manufacturer. | Using too large a cuff leads to falsely low readings and using too small a cuff, falsely high readings. Markings on the cuff clearly indicate the ideal arm circumferences appropriate for the cuff size. |
| For auscultation, the lower edge of the cuff should be 2–3 cm above the elbow crease and the bladder should be centered over the brachial artery. For electronic devices, place the cuff as recommended by the manufacturer. | |
| Procedure | |
| For auscultation, increase the pressure rapidly to 30 mmHg above the level at which the brachial or radial pulse is extinguished, place the stethoscope head over the brachial artery, deflate the cuff by approximately 2 mmHg per heartbeat, and determine systolic (appearance of Korotkoff sounds) and diastolic (disappearance of Korotkoff sounds). If the Korotkoff sounds persist towards zero, use the point of muffling of the sounds to indicate DBP. For automated devices, initiate the measurement as per the device instructions. | Record the BP to the closest 2 mmHg for auscultation or exactly as displayed on the screen of an automated device. Avoid terminal digit preference (rounding up or down to a zero or five for the last digit). On the initial visit, readings should be taken in both arms and the arm with the higher BP should be used for subsequent measurements. Two or more readings should be taken at each visit and the mean calculated and used for making clinical decisions. |
Data from [5].
FIGURE 1.
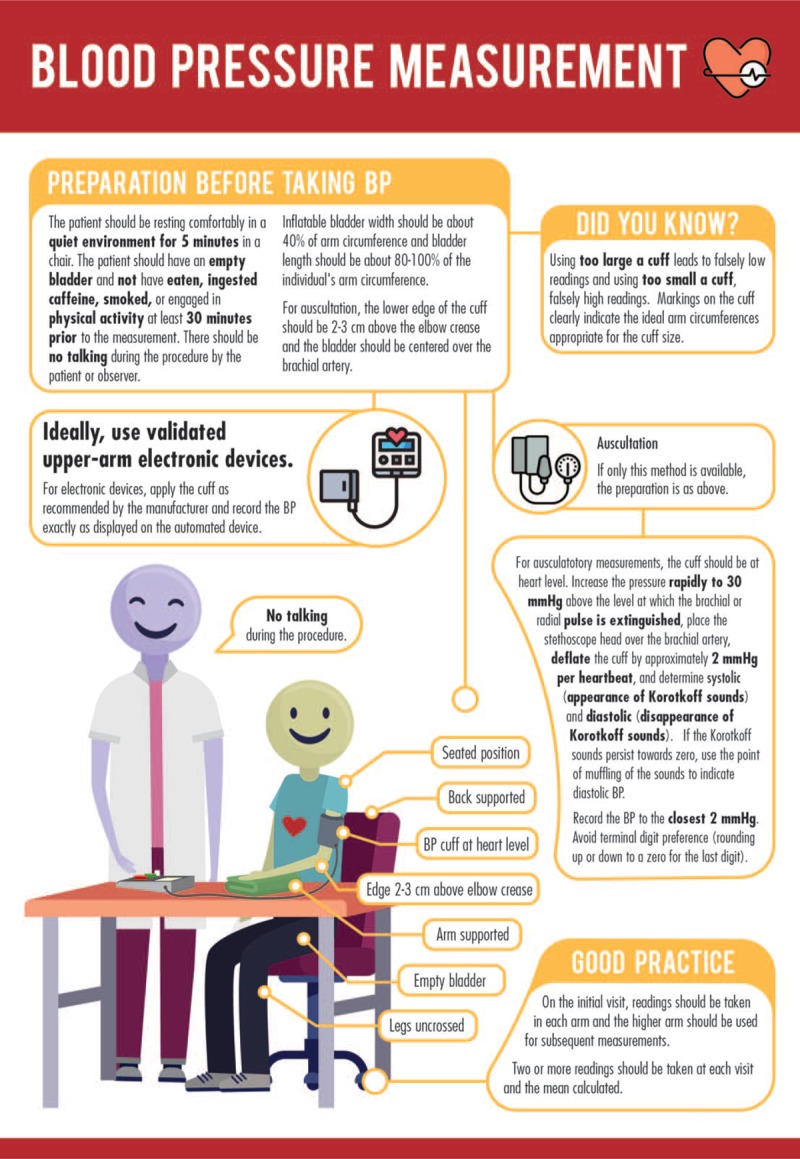
Standardized blood pressure measurement procedure.
CAUSES OF INACCURATE BLOOD PRESSURE MEASUREMENT IN CLINICAL PRACTICE
Unfortunately, standardized auscultatory measurement is not performed commonly in clinical practice [12,21]. It is also rarely performed by medical trainees [11,22]. Instead, ‘casual’ measurement, in which standardized methodology is not followed, is common. Casual measurement typically leads to higher variability, overestimation of SBP by 5–10 mmHg, and poorer correlation with hypertension related end-organ damage [10,11,15,23].
Multiple causes of inaccuracy exist and can be categorized into patient-related, procedure-related, equipment-related, or observer-related (Table 3) [24]. Poorly performed auscultation is responsible for much of the error [10,15]. Major barriers to standardized BP measurement include insufficient attention paid to optimal technique, lack of observer education, competing demands and observer time constraints, and use of inaccurate equipment [8,14,25]. Common observer-related errors in the clinical setting include failure to include a 5-min rest period, talking during the measurement procedure, using an incorrect cuff size, and failure to take multiple or bilateral measurements [12,23]. Time constraints are a particularly common reason for casual measurements, as a casual reading takes about 2 min to perform versus 8 min for a standardized measurement [12,26]. Physician readings are higher than nurse readings, which has been attributed to incremental white-coat effect [27]. Ultimately, the observer is responsible for performing a proper measurement and ensuring to the greatest extent possible that all of the potential causes of inaccuracy are avoided.
TABLE 3.
Major sources of error during blood pressure measurement
| Source | Range of mean error in SBP (mmHg) | Range of mean error in DBP (mmHg) |
| Patient-related | ||
| Acute meal ingestion | −6 | −5 to −2 |
| Acute caffeine use | +3 to +14 | +2 to +13 |
| Acute nicotine use | +3 to +25 | +3 to +18 |
| Bladder distension | +4 to +33 | +3 to +19 |
| White-coat effect | Up to +26 | Up to +21 |
| Procedure-related | ||
| Insufficient rest | +4 to +12 | +2 to +4 |
| Legs crossed at knees | +3 to +15 | +1 to +11 |
| Arm lower than heart level | +4 to +23 | +3 to +12 |
| Talking during measurement | +4 to +19 | +5 to +14 |
| Fast deflation rate | −9 to −3 | +2 to +6 |
| Equipment-related | ||
| Automated device variabilitya | −4 to +17 | −8 to +10 |
| Too small a cuff | +2 to +11 | +2 to +7 |
| Too large a cuff | −4 to −1 | −5 to −1 |
| Observer-related | ||
| Terminal digit preference for zero (rounding off during auscultatory measurements) | Up to 79% over-representation of terminal zero | Up to 79% over-representation of terminal zero |
| Reliance on a single measurement | +3 to +10 | −2 to +1 |
| Hearing deficit | −2 to −0.1 | +1 to +4 |
Data from [24].
aTo optimize automated device accuracy, use a validated device.
ADVANTAGES OF AUTOMATED BLOOD PRESSURE MEASUREMENT
Use of automated BP measurement is also supported by many foundational prognostic and therapeutic studies in the field of hypertension [17–19]. Its major advantage is that it reduces observer error by automating the BP measurement process. Accordingly, less observer expertise is needed, auscultatory training is not required, and the observer can focus on mastering a smaller number of essential aspects of BP measurement [28]. Automated BP could improve BP measurement technique even further if devices programmed to take BP in a guideline-concordant fashion were available. Examples include electronically displayed step-by-step instructions to remind observers of proper technique and auto-controlled initiation sequences that require a timed rest period before the first reading is performed.
An additional, and critically important advantage of automated BP, although beyond the immediate focus of this position paper, is that it enables many measurements to be taken in the out-of-clinic setting in the usual environment of each individual. Out-of-clinic measurement includes 24-h ambulatory monitoring and home BP monitoring and leads to much better assessment of usual BP because, in addition to eliminating observer error, it eliminates white-coat (high clinic but normal out-of-office BP) and detects masked hypertension (normal clinic but high out-of-office BP) phenomena. Indeed because of the existence of white-coat, and masked hypertension effect, which affect 9–24 and 9–17% of untreated and treated individuals, respectively, even meticulously performed standardized office BP may not be representative of usual BP [29]. Contemporary guidelines recommend confirming the diagnosis of hypertension with out-of-office BP measurements and treating masked, but not white-coat, hypertension [30].
Twenty-four-hour ambulatory and home BP monitoring are far superior to clinic measurements in terms of their ability to predict cardiovascular events [31,32]. 24-h BP monitoring is the gold standard for diagnosing hypertension and home BP monitoring is ideal for performing long-term follow-up monitoring of treated hypertensive patients, especially when coupled with nurse or pharmacist case management [33–36]. If resources allow, use of both of these measurement methods is highly recommended [30,35,37,38]. Both out-of-clinic measurement modalities require proper technique, and healthcare professionals must understand that home BP monitoring requires patient training in order to be effective in improving clinical decisions [33,36,39].
As mentioned above, AOBP offers the ability to perform three to five unattended, sequential BP measurements and auto-calculate the mean [40]. AOBP is a subtype of fully automated BP measurement; the critical distinction is that sequential readings are automated. Practically, this means the observer is required to initiate only the first reading of the sequence; she or he can then leave and return when the entire sequence is finished (as opposed to remaining in the room to initiate each sequential measurement). Use of AOBP, particularly when performed when the patient is alone in the room, facilitates a more standardized measurement process (e.g. no talking, multiple automated measurements taken sequentially). Consequently, the AOBP technique is associated with reduced white-coat effect [40,41,42–44]. AOBP requires additional space and time and the cost of AOBP devices is also 5-fold to 10-fold higher than regular automated (home) devices, which also limits use in the LMIC setting. However, if these barriers are not present, use of AOBP should be considered to enable greater standardization of in-clinic BP measurements.
Some automated devices have been specifically designed for use in the LMIC setting [45–47].
AUTOMATED DEVICE ACCURACY
An important issue with automated devices is that many have not been clinically validated for measurement accuracy [48]. Clinical validation involves demonstrating that the device meets the accuracy requirements of international BP measurement standards [49]. This process involves performing a protocol-based comparison using multiple measurements against a blinded, two-observer auscultatory reference standard. To maximize accuracy, only validated devices should be used in clinical practice [50].
In some individuals, even validated devices may produce BP measurements that differ substantially from auscultation; this may result from variations in algorithm performance and/or arterial wall properties [51,52]. For this reason, it is desirable to ensure that a specific device is performing well in a specific patient. Unfortunately, there is no consensus on how to do this in an efficient and feasible manner that is applicable in clinical practice. This issue is discussed in further detail elsewhere [53,54].
OBSERVER TRAINING TO IMPROVE CLINIC BLOOD PRESSURE MEASUREMENT
Observer training has been proposed as a solution to poor measurement technique. Training programs leading to short-term success in improving measurement technique have been described, all emphasizing the fundamentals of proper BP measurement (Table 2), and varying in their delivery format, from web-based to in-person, and in length, from 30 min to full-day sessions [55–57]. Clearly, shorter, web-based programs are preferred because of their practical advantages, lower cost and scalability. Beyond observer training alone, bundled quality improvement programs that combine use of automated office BP measurement with provider education on proper measurement and advice on clinical workflow improvement have been examined and shown to increase use of automated measurement and reduce terminal digit preference [58]. Additional approaches that have been proposed include training patients to recognize when their care providers are performing improper measurement and having regulatory agencies enforce use of standardized measurement, but the practical implementability of these propositions is uncertain [59,60].
A trained nurse with auscultatory expertise can approximate daytime ambulatory BP, a commonly used reference standard, better than automated devices [61]. However, the generalizability of this finding to an observer with less expertise undergoing a single training seminar, in the LMIC setting or otherwise, is likely to be low. Auscultation appears to be particularly difficult to perform in a uniform manner over time. The inter-observer variability of auscultatory BP measurements between expert observers was minimized by repeated training sessions, validating the importance of retraining [62]. However, following each training session, between-observer variability increased after just 1–2 months, indicating that very frequent re-training is required to maintain auscultatory skills. These data indicate that training requirements are greater over the short-term and long-term if the auscultatory technique is used, which is not feasible for widespread implementation, particularly in the LMIC setting. Accordingly, use of automated devices is recommended to minimize additional training requirements.
Overall, training improves BP measurement practices over the short term and retraining is required to maintain skills over the long term. The optimal frequency of retraining is unclear. As a practical compromise, to avoid a burdensome retraining schedule yet ensure relatively frequent refreshment of skills, retraining is recommended at least annually.
ADDITIONAL CHALLENGES TO OPTIMIZING CLINIC BLOOD PRESSURE MEASUREMENT IN THE LOW-TO-MIDDLE-INCOME SETTING
Additional challenges exist in LMIC settings and many are not easily solved. These are summarized in Table 4, together with proposed solutions.
TABLE 4.
Challenges to and potential solutions for optimizing clinic blood pressure measurement in the low-to-middle-income setting
| Challenges | Proposed solution |
| Lack of prioritization of and funding for hypertension care and proper BP measurement, including provider reimbursement, programmatic funding, and equipment. | Increased advocacy and recognition of the importance and scope of the problem. |
| Limited observer education and training in standardized BP measurement. | Training that is easily accessible and affordable. Eliminate the need for expertise in auscultation, and errors resulting from poorly performed auscultation, by using semi-automated or fully automated devices. |
| High provider workload and limited time to perform proper measurement, including between-patient cuff changes. Lack of dedicated clinic space to perform BP measurements. | Simplify measurement practices by modifying workplace ergonomics to facilitate best measurement practices (e.g. have a dedicated BP measurement station including a chair with arm-rest, even if not in a segregated clinical space, and arrange furniture to optimize patient and observer position). |
| Lack of availability of inexpensive, easily operable, clinically validated automated BP devices necessitating use of auscultation. | Increased advocacy and awareness of the need for clinical validation and low-cost devices. Encourage manufacturers to market low-cost clinic, home, and ambulatory devices. |
| Lack of availability of BP device accessories, including batteries and additional cuffs. Lack of proper environmentally responsible battery disposal mechanisms. Limited and/or lack of access to electrical power. | Choose validated semi-automated or solar-charged device overcome requirements for batteries or electrical power. A reasonable compromise if only one cuff size is available is to choose the cuff size that is considered optimal for most of the patients seen in that clinical setting. |
| Extremely high environmental temperatures in some regions that may theoretically affect the performance of BP devices. | Requires further study. |
BP, blood pressure.
RECOMMENDATIONS FOR OPTIMIZING OBSERVER PERFORMANCE IN BLOOD PRESSURE MEASUREMENT AND FOR STAKEHOLDER IMPLEMENTATION
Recommendations for optimizing observer performance in BP measurement and stakeholder implementation are listed in Fig. 2 and focus on performing simplified, standardized measurements using validated semi-automated or automated devices in a properly configured setting, and ensuring proper observer training and periodic retraining. Task-sharing by training nonphysician healthcare or lay providers, such as nurses and community health workers to perform measurement, is strongly advised because it frees physicians, who are in short supply relative to other healthcare providers, to perform other work and also reduces white-coat effect [27,63,64]. Task shifting alone may not improve BP control if clinics are overburdened, equipment is unreliable, or antihypertensive therapy is unavailable [65]. The core curricula of healthcare professional schools and postgraduate training programs should include standardized training and performance testing in blood pressure measurement.
FIGURE 2.
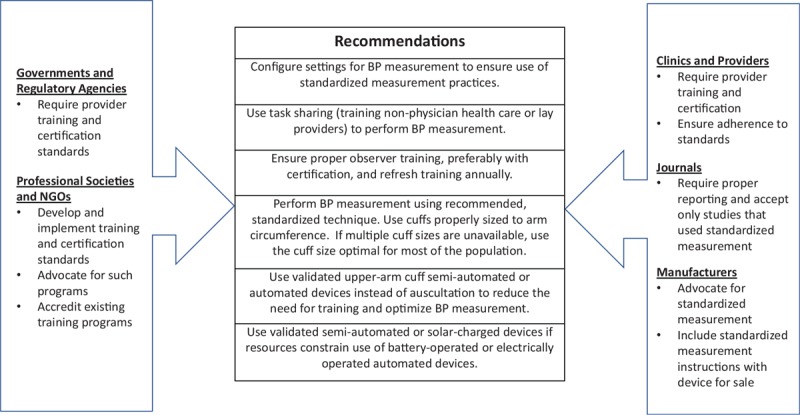
Recommendations for optimizing observer performance in clinic blood pressure measurement and for stakeholder implementation.
FUTURE DIRECTIONS
Given the importance of proper observer training, programs are needed to assist observers in acquiring the necessary skills to perform proper BP measurement. To this end, training courses that provide certification in standardized measurement, endorsed by prominent national and international organizations working in the field, would encourage and substantiate best measurement practices. The World Hypertension League has developed resources to assist providers to perform BP screening [66]. Proper BP measurement Certification programs should not be onerous and need to be simple, brief, multilingual, low-cost (ideally, free), easily repeatable and widely accessible. Research is needed to identify the best methods of delivering training, and further work is required to identify how and where training and certification could be best performed and if certification should be required.
CONCLUSION
Given the enormous, and increasing, global burden of hypertension, the need to improve all aspects of prevention, detection, treatment and control is clear [4]. The importance of proper BP measurement to optimal hypertension diagnosis and management cannot be overemphasized. Much of the error in BP measurement is within the control of the observer. Therefore, simplifying, standardizing, and automating measurement practices and ensuring proper observer education, training and certification is needed. Even these relatively straightforward recommendations can be challenging to implement, but they have the potential to markedly improve detection and management of hypertension across the world. Given the importance of accurate BP assessment, and the lack of impact of previous efforts to train healthcare workers, consideration should be given to regular certification in BP assessment.
ACKNOWLEDGEMENTS
This position statement is supported by the World Hypertension League, Artery Society, American Medical Association, American Heart Association, Hypertension Canada, Resolve to Save Lives, European Society of Hypertension Working Group on Blood Pressure Monitoring and Cardiovascular Variability.
Conflicts of interest
R.P. is a co-founder of a blood pressure measurement start-up company, mmHg Inc. No products are currently in the market. N.R.C.C. was a paid consultant to the Novartis Foundation (2016–2017) to support their program to improve hypertension control in low-to-middle-income countries, which includes travel support for site visits and a contract to develop a survey. N.R.C.C. has provided paid consultative advice on accurate blood pressure assessment to Midway Corporation (2017). M.K.R. is Vice President, Improving Health Outcomes at American Medical Association. G.W. is Director, Outcomes Analytics at American Medical Association. The remaining authors have no disclosures. G.S. is Chairman of European Society of Hypertension Working Group on BP Monitoring, ISO Sphygmomanometer committee member, and has conducted validation studies for various manufacturers of BP-measuring technologies and advised manufacturers on device and software development. J.K.C. is immediate past President of the Artery Society. A.E.S. received speaker fees from Novartis and Omron for scientific lectures on blood pressure and CV risk assessment, and Servier for presenting on raising awareness of blood pressure measurement. She a paid consultant to Abbott Pharmaceuticals on antihypertensive medication, and is President of the International Society of Hypertension.
Supplementary Material
Footnotes
Abbreviations: AOBP, automated office blood pressure; BP, blood pressure; LMIC, low-to-middle-income countries
REFERENCES
- 1.Global Burden of Disease Risk Factor Collaborators. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study, 2017. Lancet 2018; 392:1923–1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mills KT, Bundy JD, Kelly TN, Reed JE, Kearney PM, Reynolds K, et al. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation 2016; 134:441–450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Benjamin EJ, Virani SS, Callaway CW, Chamberlain AM, Chang AR, Cheng S, et al. American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics - 2018 update: a report from the American Heart Association. Circulation 2018; 137:e67–e492. [DOI] [PubMed] [Google Scholar]
- 4.Olsen MH, Angell SY, Asma S, Boutouyrie P, Burger D, Chirinos JA, et al. A call to action and a lifecourse strategy to address the global burden of raised blood pressure on current and future generations: the Lancet Commission on hypertension. Lancet 2016; 388:2665–2712. [DOI] [PubMed] [Google Scholar]
- 5.Pickering TG, Hall JE, Appel LJ, Falkner B, J G, Hill MN, et al. Recommendations for blood pressure measurement in humans and experimental animals: Part 1: blood pressure measurement in humans: a statement for professionals from the subcommittee of professional and public education of the American Heart Association Council on High Blood Pressure Research. Circulation 2005; 111:697–716. [DOI] [PubMed] [Google Scholar]
- 6.Joffres MR, Campbell NRC, Manns B, Tu K. Estimate of the benefits of a population-based reduction in dietary sodium additives on hypertension and its related healthcare costs in Canada. Can J Cardiol 2007; 23:437–443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Raven PB, Chapleau MW. Blood pressure regulation XI: overview and future research directions. Eur J Appl Physiol 2014; 114:579–586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pickering TG, Gerin W, Schwartz JE, Spruill TM, Davidson KW. Franz Volhard lecture: should doctors still measure blood pressure? The missing patients with masked hypertension. J Hypertens 2008; 26:2259–2267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Riva-Rocci S, Zanchetti A, Mancia G. A new sphygmomanometer. Sphygmomanometric technique. J Hypertens 1996; 14:1–12. [PubMed] [Google Scholar]
- 10.Campbell NR, Myers MG, McKay DW. Is usual measurement of blood pressure meaningful? Blood Press Monit 1999; 4:71–76. [PubMed] [Google Scholar]
- 11.McKay DW, Raju MK, Campbell NR. Assessment of blood pressure measuring techniques. Med Educ 1992; 26:208–212. [DOI] [PubMed] [Google Scholar]
- 12.Ray GM, Nawarskas JJ, Anderson JR. Blood pressure monitoring technique impacts hypertension treatment. J Gen Intern Med 2011; 27:623–629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.O’Brien E, Stergiou GS. The pursuit of accurate blood pressure measurement: a 35-year travail. J Clin Hypertens (Greenwich) 2017; 19:746–752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.O’Brien E, Dolan E, Stergiou GS. Achieving reliable blood pressure measurements in clinical practice: It's time to meet the challenge. J Clin Hypertens 2018; 20:1084–1088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Campbell NRC, Culleton BW, McKay DW. Misclassification of blood pressure by usual measurement in ambulatory physician practices. Am J Hypertens 2005; 18 (12 Pt 1):1522–1527. [DOI] [PubMed] [Google Scholar]
- 16.Alpert BS, Quinn D, Gallick D. Oscillometric blood pressure: a review for clinicians. J Am Soc Hypertens 2014; 8:930–938. [DOI] [PubMed] [Google Scholar]
- 17.Ettehad D, Emdin CA, Kiran A, Anderson SG, Callender T, Emberson J, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet 2015; 387:957–967. [DOI] [PubMed] [Google Scholar]
- 18.Chen Y, Lei L, Wang JG. Methods of blood pressure assessment used in milestone hypertension trials. Pulse (Basel) 2018; 6:112–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Giorgini P, Weder AB, Jackson EA, Brook RD. A review of blood pressure measurement protocols among hypertension trials: implications for ‘evidence-based’ clinical practice. J Am Soc Hypertens 2014; 8:670–676. [DOI] [PubMed] [Google Scholar]
- 20.Brueren MM, Petri H, van Weel C, van Ree JW. How many measurements are necessary in diagnosing mild to moderate hypertension. Fam Pract 1997; 14:130–135. [DOI] [PubMed] [Google Scholar]
- 21.Sebo P, Pechère-Bertschi A, Herrmann FR, Haller DM, Bovier P. Blood pressure measurements are unreliable to diagnose hypertension in primary care. J Hypertens 2014; 32:509–517. [DOI] [PubMed] [Google Scholar]
- 22.Rakotz MK, Townsend RR, Yang J, Alpert BS, Heneghan KA, Wynia M, et al. Medical students and measuring blood pressure: results from the American Medical Association Blood Pressure Check Challenge. J Clin Hypertens (Greenwich) 2017; 19:614–619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Minor DS, Butler KR, Jr, Artman KL, Adair C, Wang W, McNair V, et al. Evaluation of blood pressure measurement and agreement in an academic health sciences center. J Clin Hypertens (Greenwich) 2012; 14:222–227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kallioinen N, Hill A, Horswill MS, Ward HE, Watson MO. Sources of inaccuracy in the measurement of adult patients’ resting blood pressure in clinical settings. J Hypertens 2017; 35:421–441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.O’Brien E, Asmar R, Beilin L, Imai Y, Mancia G, Mengden T, et al. European Society of Hypertension Working Group on Blood Pressure Monitoring. Practice guidelines of the European Society of Hypertension for clinic, ambulatory and self blood pressure measurement. J Hypertens 2005; 23:697–701. [DOI] [PubMed] [Google Scholar]
- 26.Stergiou GS, Kyriakoulis KG, Kollias A. Office blood pressure measurement types: different methodology-different clinical conclusions. J Clin Hypertens (Greenwich) 2018; 20:1683–1685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Clark CE, Horvath IA, Taylor RS, Campbell JL. Doctors record higher blood pressures than nurses: systematic review and meta-analysis. Br J Gen Pract 2014; 64:e223–e232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Campbell NR, Berbari AE, Cloutier L, Gelfer M, Kenerson JG, Khalsa TK, et al. Policy statement of the world hypertension league on noninvasive blood pressure measurement devices and blood pressure measurement in the clinical or community setting. J Clin Hypertens 2014; 16:320–322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fagard RH, Cornelissen VA. Incidence of cardiovascular events in white-coat, masked and sustained hypertension versus true normotension: a meta-analysis. J Hypertens 2007; 25:2193–2198. [DOI] [PubMed] [Google Scholar]
- 30.Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens 2018; 36:1953–2041. [DOI] [PubMed] [Google Scholar]
- 31.O’Brien E, Parati G, Stergiou G, Asmar R, Beilin L, Bilo G, et al. European Society of Hypertension Working Group on Blood Pressure Monitoring. European Society of Hypertension position paper on ambulatory blood pressure monitoring. J Hypertens 2013; 31:1731–1768. [DOI] [PubMed] [Google Scholar]
- 32.Stergiou GS, Bliziotis IA. Home blood pressure monitoring in the diagnosis and treatment of hypertension: a systematic review. Am J Hypertens 2009; 24:123–134. [DOI] [PubMed] [Google Scholar]
- 33.Cloutier L, Daskalopoulou S, Padwal RS, Lamarre-Clich M, Bolli P, McLean D, et al. A new algorithm for the diagnosis of hypertension in Canada. Can J Cardiol 2015; 31:620–630. [DOI] [PubMed] [Google Scholar]
- 34.Duan Y, Xie Z, Dong F, Wu Z, Lin Z, Sun N, et al. Effectiveness of home blood pressure telemonitoring: a systematic review and meta-analysis of randomised controlled studies. J Hum Hypertens 2017; 31:427–437. [DOI] [PubMed] [Google Scholar]
- 35. [[Accessed 12 October 2018]]. National Institute for Health and Care Excellence. Hypertension in adults: diagnosis and management. Clinical guideline CG127. 2011 (updated 2016). Available at: https://www.nice.org.uk/guidance/cg127. [Google Scholar]
- 36.Parati G, Stergiou G, O’Brien E, Asmar R, Beilin L, Bilo G, et al. European Society of Hypertension practice guidelines for ambulatory blood pressure monitoring. J Hypertens 2014; 32:1359–1366. [DOI] [PubMed] [Google Scholar]
- 37.Nerenberg KA, Zarnke KB, Leung AA, Dasgupta K, Butalia S, McBrien K, et al. Hypertension Canada. Hypertension Canada's 2018 Guidelines for Diagnosis, Risk Assessment, Prevention, and Treatment of Hypertension in Adults and Children. Hypertension Canada's 2018 guidelines for diagnosis, risk assessment, prevention, and treatment of hypertension in adults and children. Can J Cardiol 2018; 34:506–525. [DOI] [PubMed] [Google Scholar]
- 38.US Preventive Services Task Force. Screening for high blood pressure: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med 2015; 163:778–786. [DOI] [PubMed] [Google Scholar]
- 39.Milot JP, Birnbaum L, Larochelle P, Wistaff R, Laskine M, Van Nguyen P, et al. Unreliability of home blood pressure measurement and the effect of a patient-oriented intervention. Can J Cardiol 2015; 31:658–663. [DOI] [PubMed] [Google Scholar]
- 40.Myers MG. Eliminating the human factor in office blood pressure measurement. J Clin Hypertens (Greenwich) 2014; 16:83–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Roerecke M, Kaczorowski J, Myers MG. Comparing automated office blood pressure readings with other methods of blood pressure measurement for identifying patients with possible hypertension. JAMA Intern Med 2019; 179: [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jegatheswaran J, Ruzicka M, Hiremath S, Edwards C. Are automated blood pressure monitors comparable to ambulatory blood pressure monitors? A systematic review and meta-analysis. Can J Cardiol 2017; 33:644–652. [DOI] [PubMed] [Google Scholar]
- 43.Ringrose JS, Cena J, Ip S, Morales F, Hamilton P, Padwal R. Comparability of automated office blood pressure to daytime 24-Hour ambulatory blood pressure. Can J Cardiol 2018; 34:61–65. [DOI] [PubMed] [Google Scholar]
- 44.Drawz PE, Pajewski NM, Bates JT, Bello NA. Effect of intensive versus standard clinic-based hypertension management on ambulatory blood pressure: novelty and significance. Hypertension 2017; 69:42–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.de Greeff A, Nathan H, Stafford N, Liu B, Shennan AH. Development of an accurate oscillometric blood pressure device for low resource settings. Blood Press Monit 2008; 13:342–348. [DOI] [PubMed] [Google Scholar]
- 46.Baker EC, Hezelgrave N, Magesa SM, Edmonds S, de Greeff A, Shennan A. Introduction of automated blood pressure devices intended for a low resource setting in rural Tanzania. Trop Doct 2012; 42:101–103. [DOI] [PubMed] [Google Scholar]
- 47.Parati G, Kilama MO, Faini A, Facelli E, Ochen K, Opira C, et al. A new solar-powered blood pressure measuring device for low-resource settings. Hypertension 2010; 56:1047–1053. [DOI] [PubMed] [Google Scholar]
- 48.O’Brien E, Stergiou GS, Turner MJ. The quest for accuracy of blood pressure measuring devices. J Clin Hypertens (Greenwich) 2018; 20:1092–1095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. [[Accessed 10 August 2013]]. Association for the Advancement of Medical Instrumentation. ANSI/AAMI/ISO 81060-2:2013 noninvasive sphygmomanometers - part 2: clinical investigation of automated measurement type. 2013. Association for the Advancement of Medical Instrumentation. Arlington, VA, 2013. Available at: www.aami.org. [Google Scholar]
- 50.Jung M-H, Kim G-H, Kim J-H, Moon K-W, Yoo K-D, Rho T-H, et al. Reliability of home blood pressure monitoring: in the context of validation and accuracy. Blood Press Monit 2015; 20:215–220. [DOI] [PubMed] [Google Scholar]
- 51.Stergiou GS, Lourida P, Tzamouranis D, Baibas NM. Unreliable oscillometric blood pressure measurement: prevalence, repeatability and characteristics of the phenomenon. J Hum Hypertens 2009; 23:794–800. [DOI] [PubMed] [Google Scholar]
- 52.Padwal R, Jalali A, McLean D, Anwar S, Smith K, Raggi P, et al. Accuracy of oscillometric blood pressure algorithms in healthy adults and in adults with cardiovascular risk factors. Blood Press Monit 2018; 24:33–37. [DOI] [PubMed] [Google Scholar]
- 53.Cohen JB, Padwal RS, Gutkin M, Green BB, Bloch MJ, Germino FW, et al. History and justification of a national blood pressure measurement validated device listing. Hypertension 2019; 73:258–264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Eguchi K, Kuruvilla S, Ishikawa J, Schwartz JE, Pickering TG. A novel and simple protocol for the validation of home blood pressure monitors in clinical practice. Blood Press Monit 2012; 17:210–213. [DOI] [PubMed] [Google Scholar]
- 55.Grim CM, Grim CE. A curriculum for the training and certification of blood pressure measurement for healthcare providers. Can J Cardiol 1995; 11 Suppl H:38H–42H. [PubMed] [Google Scholar]
- 56.Block L, Flynn SJ, Cooper LA, Lentz C, Hull T, Dietz KB, et al. Promoting sustainability in quality improvement: an evaluation of a web-based continuing education program in blood pressure measurement. BMC Fam Pract 2018; 19:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Dickson BK, Hajjar I. Blood pressure measurement education and evaluation program improves measurement accuracy in community-based nurses: a pilot study. J Amer Acad Nurse Pract 2007; 19:93–102. [DOI] [PubMed] [Google Scholar]
- 58.Boonyasai RT, Carson KA, Marsteller JA, Dietz KB, Noronha GJ, Hsu Y-J, et al. A bundled quality improvement program to standardize clinical blood pressure measurement in primary care. J Clin Hypertens 2017; 20:324–333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Appel LJ, Miller ER, Charleston J. Improving the measurement of blood pressure: is it time for regulated standards. Ann Intern Med 2011; 154:838–840. [DOI] [PubMed] [Google Scholar]
- 60.Umscheid CA, Townsend RR. Is it time for a blood pressure measurement ‘bundle’? J Gen Intern Med 2012; 27:615–617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Graves JW, Grossardt BR, Gullerud RE, Bailey KR, Feldstein J. The trained observer better predicts daytime ABPM diastolic blood pressure in hypertensive patients than does an automated (Omron) device. Blood Pres Monit 2006; 11:53–58. [DOI] [PubMed] [Google Scholar]
- 62.Bruce NG, Shaper AG, Walker M, Wannamethee G. Observer bias in blood pressure studies. J Hypertens 1988; 6:375–380. [PubMed] [Google Scholar]
- 63.World Health Organization. Global Health Observatory (GHO) data. Density of physicians (total number per 100 population, latest available year). Available at: http://www.who.int/gho/health_workforce/physicians_density/en/ [Accessed 4 November 2018] [Google Scholar]
- 64.World Health Organization. HEARTS Technical package for cardiovascular disease management in primary healthcare: team-based care. Geneva: World Health Organization; 2018 (WHO/NMH/NVI/18.4). Licence: CC BY-NC-SA 3.0 IGO. [Google Scholar]
- 65.Goudge J, Chirwa T, Eldridge S, Gómez-Olivé FXF, Kabudula C, Limbani F, et al. Can lay health workers support the management of hypertension? Findings of a cluster randomised trial in South Africa. BMJ Glob Health 2018; 3: e000577-e12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Mangat BK, Campbell N, Mohan S, Niebylski ML, Khalsa TK, Berbari AE, et al. Resources for blood pressure screening programs in low resource settings: a guide from the World Hypertension League. J Clin Hypertens (Greenwich) 2015; 17:418–420. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


