This pilot randomized clinical trial explores the effect of individualized coaching on physician burnout, job satisfaction, and well-being.
Key Points
Question
Does professional coaching result in measurable reductions in burnout and measurable improvements in quality of life, resilience, job satisfaction, engagement, and fulfillment in physicians?
Findings
In this pilot randomized clinical trial of 88 physicians, participants who received professional coaching had a significant reduction in emotional exhaustion and overall symptoms of burnout, as well as improvements in overall quality of life and resilience.
Meaning
Professional coaching may be an effective strategy to reduce burnout and improve well-being for physicians.
Abstract
Importance
Burnout symptoms among physicians are common and have potentially serious ramifications for physicians and their patients. Randomized studies testing interventions to address burnout have been uncommon.
Objective
To explore the effect of individualized coaching on the well-being of physicians.
Design, Setting, and Participants
A pilot randomized clinical trial involving 88 practicing physicians in the departments of medicine, family medicine, and pediatrics who volunteered for coaching was conducted between October 9, 2017, and March 27, 2018, at Mayo Clinic sites in Arizona, Florida, Minnesota, and Wisconsin. Statistical analysis was conducted from August 24, 2018, to March 25, 2019.
Interventions
A total of 6 coaching sessions facilitated by a professional coach.
Main Outcomes and Measures
Burnout, quality of life, resilience, job satisfaction, engagement, and meaning at work using established metrics. Analysis was performed on an intent-to-treat basis.
Results
Among the 88 physicians in the study (48 women and 40 men), after 6 months of professional coaching, emotional exhaustion decreased by a mean (SD) of 5.2 (8.7) points in the intervention group compared with an increase of 1.5 (7.7) points in the control group by the end of the study (P < .001). Absolute rates of high emotional exhaustion at 5 months decreased by 19.5% in the intervention group and increased by 9.8% in the control group (−29.3% [95% CI, −34.0% to −24.6%]) (P < .001). Absolute rates of overall burnout at 5 months also decreased by 17.1% in the intervention group and increased by 4.9% in the control group (−22.0% [95% CI, −25.2% to −18.7%]) (P < .001). Quality of life improved by a mean (SD) of 1.2 (2.5) points in the intervention group compared with 0.1 (1.7) points in the control group (1.1 points [95% CI, 0.04-2.1 points]) (P = .005), and resilience scores improved by a mean (SD) of 1.3 (5.2) points in the intervention group compared with 0.6 (4.0) points in the control group (0.7 points [95% CI, 0.0-3.0 points]) (P = .04). No statistically significant differences in depersonalization, job satisfaction, engagement, or meaning in work were observed.
Conclusions and Relevance
Professional coaching may be an effective way to reduce emotional exhaustion and overall burnout as well as improve quality of life and resilience for some physicians.
Trial Registration
ClinicalTrials.gov identifier: NCT03207581
Introduction
The prevalence of burnout symptoms among physicians is high,1 with those at the front lines of care2 at especially high risk. Symptoms of burnout are nearly twice as common among physicians than among US workers in other fields.1 Professional burnout has numerous adverse consequences, including effects on quality and safety, patient-physician relationships, productivity, and turnover.3,4,5,6,7,8,9 Workload (eg, work hours, overnight call frequency, and clerical burden), work-process inefficiencies (eg, computerized order entry), work-home conflicts, organizational culture (eg, leadership behaviors), and loss of autonomy, control, and meaning in work all are associated with work-related stress that leads to burnout.10,11,12,13,14
The degree to which stressors within the work environment affect well-being is influenced by personal and professional factors. Strategies to promote physician well-being are a shared responsibility between individual physicians, health care organizations, and external organizations (eg, Centers for Medicare & Medicaid Services, state medical boards, payers, regulators, and electronic health record vendors) and must involve optimization of the practice environment and organizational culture in addition to supporting individuals. As such, a holistic approach is necessary to address the problem; evidence-based approaches are necessary in all of these dimensions. Although recent meta-analyses have reported benefits for both individual-focused and structural or organizational interventions,15,16 the evidence on which interventions most effectively reduce burnout remains limited.
Coaching, mentorship, and peer support are 3 distinct approaches that have been proposed to reduce burnout. Mentorship, characterized by a relationship in which one individual who is more knowledgeable and experienced guides a less knowledgeable and less experienced individual, is widely considered essential to career development.17 Collegiality among and support from peers involves the sharing of knowledge, experience, and emotional and social support between individuals who have common experiences, with evidence indicating that interventions that support informal connections with colleagues can reduce burnout and improve career satisfaction.18 Formal peer support programs can also assist physicians after a medical error or a traumatic event involving the care of a patient.19,20 Both mentoring and peer support typically involve physicians or other individuals with direct experience in health care. Coaching is distinct from mentorship and peer support and involves inquiry, encouragement, and accountability to increase self-awareness, motivation, and the capacity to take effective action.21,22,23,24,25,26,27,28,29,30 Coaches do not need to be physicians or directly involved in health care. Professional coaching can be tailored to focus on the aspects desired by recipients and can assist individuals in their effort to navigate their professional life, their choices, and the direction of their career. Coaching, mentorship, and peer support are distinct from therapy, which is conducted by individuals trained to work with mental illness and conceptually relies on a medical model to diagnose and treat.
Professional coaching has been associated with improved retention, interpersonal relationships, job satisfaction, organizational commitment, ability to manage complexity, and communication skills.21,22,23,24,25,26,27,28,29,30,31 A limited number of randomized clinical studies of professional coaching have been conducted evaluating aspects of well-being.30 Studies on professional coaching published to date have substantial variability in their design, sample size, use of intention-to-treat analysis, and coaching intervention (number and length of sessions as well as time period), and findings have been mixed in regard to the effect on symptoms of depression, anxiety, and stress.30,32,33
Although there are few empirical data evaluating its effect on physicians, coaching has been proposed as a way to help physicians maximally access personal strengths and skills to handle work-related stressors, thereby reducing vulnerability to burnout and helping those who are burned out recover.23,25,34,35,36,37 We hypothesized that professional coaching would result in measurable improvements in well-being, job satisfaction, resilience, and fulfillment in physicians and measurable reductions in burnout. Here, we report the results of a pilot randomized clinical trial of a professional coaching intervention to test this hypothesis.
Methods
Study Design, Setting, and Participants
We conducted a multisite, single-institution pilot randomized clinical trial with a planned enrollment of 80 physicians who worked in the departments of medicine, family medicine, and pediatrics at Mayo Clinic in Rochester, Minnesota; Jacksonville, Florida; and Scottsdale, Arizona; or Mayo Clinic Health System campuses in Wisconsin and Minnesota (community-based hospitals and health care facilities). We chose a sample size of at least 40 participants in the intervention group and 40 participants in the control group to provide 80% power to detect a moderate 0.5-SD to 0.6-SD effect size, a level describing clinically significant outcomes.38 Subspecialists and generalists were recruited. The study was conducted between October 9, 2017, and March 27, 2018. Participants were recruited through e-mail and departmental announcements. Individuals who had been in practice for 5 to 30 years were eligible. From a population of 764 eligible physicians, we enrolled whoever responded first until our study recruitment goal was met. All of those who chose to participate in the trial provided written informed consent. The study was approved by the Mayo Clinic Institutional Review Board. The study protocol is available in Supplement 1.
Randomization, Allocation Concealment, and Follow-up
We used a computer-generated dynamic allocation algorithm to randomize participants into a coaching group and a control group. Randomization was stratified by years in practice, work site (Arizona, Florida, Minnesota, or Mayo Clinic Health System), and primary care (family medicine, general pediatrics, or general internal medicine) vs subspecialty practice. Participants completed a baseline and 5-month survey, corresponding to the end of the intervention.
Study Groups
Participants randomized to the coaching group received a 1-hour initial professional coaching session followed by five 30-minute professional coaching sessions occurring at a goal frequency of every 2 to 3 weeks within 5 months (total of 3.5 coaching hours; approximately $1400 per person). Credentialed professional coaches were provided by Bluepoint Leadership Development Inc, an established international professional coaching company with experience coaching physicians. All coaching sessions were performed by telephone. The initial coaching session focused on creating the relationship, assessing needs, identifying values, setting goals, and creating an action plan. Subsequent sessions followed the same general structure: (1) check in, debrief strategic action the participant had taken since the last session, manage progress, and review accountability; (2) plan and set goals; (3) design actions to incorporate into daily life; (4) commit to next steps; and (5) check out and summarize. The topics individuals could request coaching on were unscripted and individualized. Coaches made brief notes of the topics discussed. Participants randomized to the intervention group were expected to see the same number of patients as their colleagues who were not in the intervention group. Participants who scheduled their coaching during their clinical time were expected to make up the patient visits by seeing additional patients at other times (eg, adding extra patients before or after their standard clinical time on other days). Participants randomized to the control group received no intervention during the 5 months of the study but were provided with access to Bluepoint coaches for an equivalent number of coaching contact hours (3.5 hours) during the 5 months after the conclusion of the active study interval.
Study Outcomes
Baseline and end-of-study 5-month surveys were administered electronically by the Mayo Clinic Survey Research Center. The surveys contained multiple validated instruments to measure dimensions of distress, well-being, career satisfaction, and meaning in work.
Burnout, Quality of Life, and Resilience
Burnout was measured using the Maslach Burnout Inventory, the most commonly used instrument for assessment of physician burnout.39 Information on reliability coefficients, test-retest reliability, convergent validity, and discriminant validity among human service professionals can be found in the Maslach Burnout Inventory Manual,40 and validity data for the Maslach Burnout Inventory for physicians has recently been summarized.41 Respondents rate the frequency with which they experience various feelings or emotions on a 7-point Likert scale, with response options ranging from never (score of 0) to daily (score of 6). In multiple samples of physicians, a 1-point increase in the emotional exhaustion subscale score has been associated with a 7% increase in suicidal ideation and a 5% to 6% increase in perceived major medical errors.3,5,42 Similarly, a 1-point increase in the depersonalization subscale score has been associated with a 10% to 11% increase in suicidal ideation and a 9% to 11% increase in self-reported major medical errors.3,5,42 We used established thresholds specified in the index manual to define high emotional exhaustion (score ≥27) and high depersonalization (score ≥10).39,40 Consistent with other studies,5,43,44 we considered those who scored high on either the emotional exhaustion or depersonalization subscale to have at least 1 manifestation of professional burnout.
Quality of life was measured by a single-item linear analog scale. For this item, respondents rate their overall quality of life on a 10-point scale with response options ranging from “as bad as it can be” (score of 0) to “as good as it can be” (score of 10). Resilience was measured using the 10-item Connor-Davidson Resilience Scale. For this scale, respondents indicate how much a statement applies to them during the last month on a 0 to 4 scale ranging from “not true at all” to “true nearly all of the time” (range, 0-40), with higher scores suggesting greater resilience. The mean scores on the Connor-Davidson Resilience Scale in general population samples are 31.8 to 32.1.45,46 Although the minimal clinically important differences for the quality-of-life and resiliency measures have not been established for this population, a 0.25-SD to 0.5-SD change is a standard effect size considered to indicate meaningful change for such measures.47,48
Job Satisfaction, Engagement, and Meaning
We used the 12-item Global Job Satisfaction subscale of the Physician Job Satisfaction Scale, which measures 3 dimensions (job satisfaction, career satisfaction, and specialty satisfaction) and has Cronbach α values of 0.82 to 0.88.49 Respondents indicate their level of agreement on a 5-point scale, with response options ranging from strongly disagree to strongly agree (range, 1-5), with higher scores indicating greater satisfaction at work.
The Utrecht Work Engagement Scale was used to measure vigor, dedication, and absorption.50 Respondents rate the frequency with which they have various feelings about their work on a 0 to 6 scale ranging from never to always or every day. Vigor is assessed by 6 items that refer to high levels of energy, enthusiasm for work, and resilience, with a high score indicating energy and stamina when working. Dedication is measured by 5 items that refer to meaning, feeling inspired and challenged by work, and being enthusiastic about the work, with a high score indicating that work is experienced as meaningful, inspiring, and challenging. Lastly, absorption was measured by 6 items referring to being immersed in one’s work, with high scores indicating being happily engrossed by work and having difficulties detaching from work because it carries them away.
For the Empowerment at Work Scale, respondents rate 12 items on a 1 to 7 scale ranging from very strongly disagree to very strongly agree (range, 12-84).51 This scale has 4 dimensions: meaning, competence, self-determination, and impact. The 4 dimensions combine additively to create an overall construct of psychological empowerment at work, with higher scores suggesting a greater sense of empowerment, engagement, and meaning.
Statistical Analysis
Statistical analysis was conducted from August 24, 2018, to March 25, 2019, and was performed on an intent-to-treat basis. We calculated standard univariate statistics to characterize the sample. Baseline comparisons between the groups were made using standard Kruskal-Wallis or χ2 tests as appropriate. To evaluate the effect of the intervention, the changes in each measure from study baseline to study end were compared similarly. All P values were from 2-sided tests and results were deemed statistically significant at P < .05. Statistical analyses were performed using SAS, version 9.2 (SAS Institute Inc).
Results
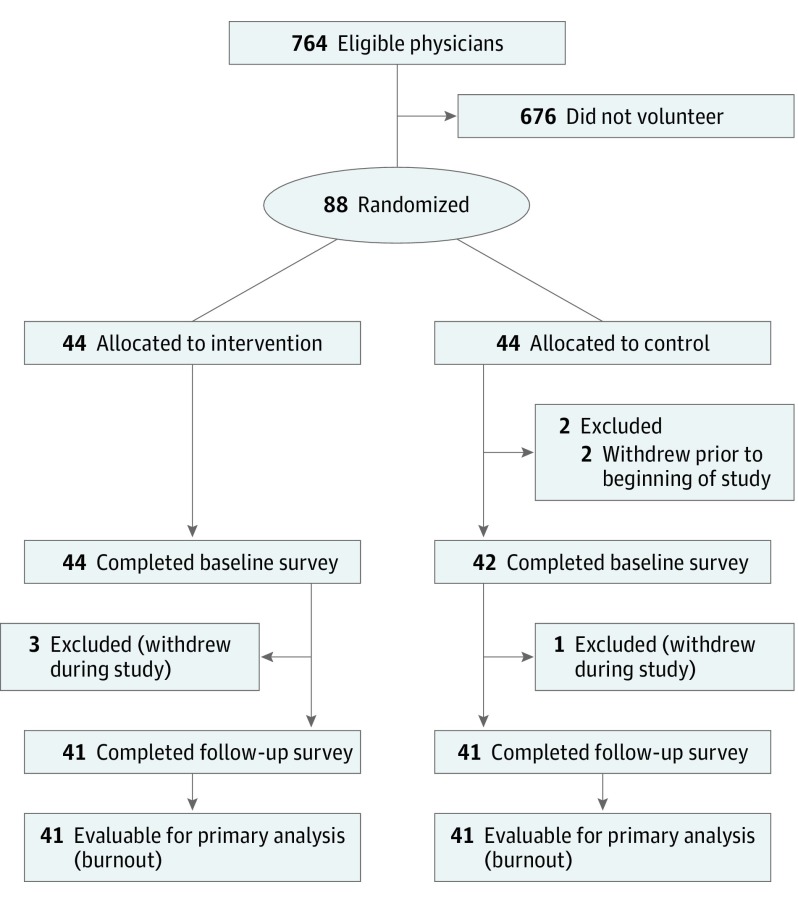
Of the 88 physicians who were the first to volunteer for the study and provide informed consent, 44 were randomly allocated to the coaching group (Figure). Most physicians (86 [97.7%]) completed the baseline survey. Professional characteristics (ie, work location, specialty, and number of years in practice) of study volunteers were similar to other physicians in the departments who were eligible for the study but did not volunteer to participate, with the exception that women were more likely to participate (48 of 88 study participants were women [54.5%] and 231 of 676 eligible physicians were women [34.2%]; P < .001). The baseline characteristics of participants randomized to the intervention group and the baseline characteristics of participants randomized to the control group were similar with respect to sex, age, relationship status, work location, specialty, number of years in practice, number of work hours, and time spent in direct patient care (Table 1). There were no statistically significant differences in baseline burnout symptoms, quality of life, resilience, job satisfaction, engagement, or meaning at work at baseline between individuals randomized to coaching and those randomized to the control group (Table 2).
Figure. Study Flowchart.
Table 1. Baseline Demographic Characteristics of Randomized Groups of the Study.
| Characteristic | Participants, No./Total No. (%) | P Value | |
|---|---|---|---|
| Intervention Group | Control Group | ||
| Women | 20/44 (45.5) | 28/44 (63.6) | .09 |
| Age, y | |||
| 31-40 | 7/44 (15.9) | 7/42 (16.7) | .32 |
| 41-50 | 25/44 (56.8) | 20/42 (47.6) | |
| 51-60 | 12/44 (27.3) | 12/42 (28.6) | |
| >60 | 0 | 3/42 (7.1) | |
| Missing data, No. | 0 | 2 | |
| Current relationship status | |||
| Single | 2/43 (4.7) | 2/42 (4.8) | .52 |
| Married | 36/43 (83.7) | 37/42 (88.1) | |
| Widowed | 1/43 (2.3) | 0 | |
| Divorced or separated | 2/43 (4.7) | 3/42 (7.1) | |
| Partner | 2/43 (4.7) | 0 | |
| Missing data, No. | 1 | 2 | |
| Work location | |||
| Rochester, Minnesota | 25/44 (56.8) | 24/43 (55.8) | .76 |
| Jacksonville, Florida | 4/44 (9.1) | 2/43 (4.6) | |
| Scottsdale, Arizona | 3/44 (6.8) | 5/43 (11.6) | |
| Mayo Clinic Health Systema | 12/44 (27.3) | 12/43 (27.9) | |
| Family medicine, general pediatrics, and general internal medicine specialties | 33/44 (75.0) | 34/43 (77.3) | .80 |
| No. of years in practice, mean (SD) | 15.8 (7.2) | 15.7 (8.3) | .73 |
| No. of hours worked per week, mean (SD) | 57.7 (14.1) | 54.2 (10.3) | .29 |
| Proportion of time spent in direct patient care, % | |||
| ≤24 | 1/41 (2.4) | 1/42 (2.4) | .59 |
| 25-49 | 8/41 (19.5) | 5/42 (11.9) | |
| 50-74 | 13/41 (31.7) | 9/42 (21.4) | |
| 75-99 | 12/41 (29.3) | 17/42 (40.5) | |
| 100 | 7/41 (17.1) | 10/42 (23.8) | |
Physicians working in community-based hospitals and health care systems in the Mayo Clinic Health System campuses in Wisconsin and Minnesota were invited to participate.
Table 2. Baseline Well-being, Job Satisfaction, Engagement, and Meaning at Work of Randomized Groups of the Study.
| Characteristic | Intervention Group (n = 44) | Control Group (n = 44) | P Value |
|---|---|---|---|
| Burnout | |||
| Subscale score, mean (SD) | |||
| Emotional exhaustiona | 32.8 (10.4) | 29.0 (12.1) | .15 |
| Depersonalizationb | 9.0 (5.7) | 7.8 (6.8) | .18 |
| Personal accomplishmentc | 40.6 (4.5) | 39.4 (5.7) | .46 |
| Overall burnout, No. (%)d | 32 (72.7) | 25/42 (59.5) | .20 |
| High emotional exhaustion, No. (%) | 31 (70.5) | 23/42 (54.8) | .13 |
| High depersonalization, No. (%) | 19 (43.2) | 14/42 (33.3) | .35 |
| Overall QOL score, mean (SD)e | 5.9 (1.6) | 6.5 (1.5) | .07 |
| Resilience score, mean (SD)f | |||
| CDRISC | 31.0 (6.3) | 30.6 (5.7) | .77 |
| Job satisfaction score, mean (SD)g | |||
| Global job satisfaction | 43.4 (10.7) | 42.8 (10.6) | .77 |
| Engagement and meaning at work | |||
| UWES score, mean (SD)h | |||
| Vigor | 3.9 (1.0) | 4.0 (1.2) | .62 |
| Dedication | 4.5 (1.1) | 4.6 (1.0) | .89 |
| Absorption | 4.2 (1.0) | 4.1 (1.1) | .62 |
| Empowerment at worki | 55.5 (11.9) | 57.3 (14.0) | .47 |
Abbreviations: CDRISC, Connor-Davidson Resilience Scale; QOL, quality of life; UWES, Utrecht Work Engagement Scale.
The score range is from 0 to 54; a higher score indicates greater burnout symptoms. The score was generated from the Emotional Exhaustion subscale of the Maslach Burnout Inventory.
The score range is from 0 to 30; higher score indicates greater burnout symptoms. The score was generated from the Depersonalization subscale of the Maslach Burnout Inventory.
The score range is from 0 to 48; lower score indicates greater burnout symptoms. The score was generated from the Personal Accomplishment subscale of the Maslach Burnout Inventory.
Positive for symptoms of overall burnout if had a high score (≥27) on the emotional exhaustion and/or high score (≥10) on the depersonalization subscale.
The score range is from 0 to 10, with higher scores indicating better quality of life. A single-item linear analog scale was used.
The score range is from 0 to 40, with higher scores suggesting greater resilience. Resilience was measured using the 10-item CDRISC.
The scale range is from 0 to 60, with higher scores indicating greater job satisfaction. The 12-item Global Job Satisfaction subscale of the Physician Job Satisfaction scale was used.
The scale range is from 0 to 6 for vigor, 0 to 5 for dedication, and 0 to 6 for absorption, with higher scores being more favorable.
The scale range is from 12 to 84, with higher score being more favorable. The Empowerment at Work Scale was used.
Participants randomized to the intervention group had a mean of 5.5 coaching sessions (range, 0-6 coaching sessions). The major themes discussed during coaching sessions are shown in Table 3. A total of 82 physicians (93.2%) completed the follow-up survey. Data in Table 4 show that participants randomized to the coaching intervention had greater reductions in emotional exhaustion scores from baseline than those in the control group (mean [SD], –5.2 [8.7] vs 1.5 [7.7]; relative change, –15.9% vs 5.2%; P < .001). The proportion of physicians with high emotional exhaustion at 5 months decreased by 19.5% in the intervention group and increased by 9.8% in the control group (relative change, –27.7% vs 17.9%; P < .001). There was no statistically significant change in depersonalization scores from baseline or in the proportion of physicians with high depersonalization at 5 months. The prevalence of symptoms of burnout at 5 months decreased by 17.1% in the intervention group and increased by 4.9% in the control group (relative change, –23.5% vs 8.2%; P < .001).
Table 3. Themes Discussed During Coaching Sessions.
| Theme | Example |
|---|---|
| Optimizing meaning in work | Aligning values and priorities with work-related tasks; ensuring work activities align with the aspects of work perceived as most meaningful; reconsidering nonclinical roles |
| Integrating personal and professional life | Sharing tasks with partner; meeting needs of aging parents; reducing work-home conflicts |
| Building social support and community at work | Strategies to network with colleagues; taking breaks at work with colleagues; building peer relationships; addressing stressful relationships with colleagues |
| Improving work efficiency | Steps to increase efficiency with email and other tasks: delegating tasks, setting boundaries with patients, collaborating with colleagues, and obtaining additional EHR training |
| Addressing workload | Prioritizing and saying “no”; avoiding overscheduling; setting expectations; setting goals; establishing roles and responsibilities |
| Building leadership skills | Building teams; changing management; influencing leaders; challenging conversations |
| Pursuing hobbies and recreation | Finding time; discovering interests |
| Engaging in self-care | Strategizing to get exercise; eating healthy, attending to medical needs |
| Strengthening relationships outside of work | Proactively scheduling social events with friends; spending more time with family; showing appreciation toward others; being grateful |
Abbreviation: EHR, electronic health record.
Table 4. Changes From Baseline to 5 Months After Randomization.
| Characteristic | Intervention Group (n = 44) | Control Group (n = 44) | Absolute Change, Intervention vs Control (95% CI) | P Value | ||
|---|---|---|---|---|---|---|
| Absolute Change | Relative Change | Absolute Change | Relative Change | |||
| Burnout | ||||||
| Subscale score, mean (SD) | ||||||
| Emotional exhaustiona | −5.2 (8.7) | −15.9 | 1.5 (7.7) | 5.2 | −6.7 (−10.3 to −3.2) | <.001 |
| Depersonalizationb | −0.9 (3.8) | −10.0 | 0.3 (3.8) | 3.8 | −1.2 (−2.7 to 0.5) | .23 |
| Personal accomplishmentc | −0.4 (4.9) | −1.0 | 0.8 (3.7) | 2.1 | −1.2 (−3.1 to 0.7) | .44 |
| Overall burnout score, %d | −17.1 | −23.5 | 4.9 | 8.2 | −22.0 (−25.2 to −18.7) | <.001 |
| High emotional exhaustion | −19.5 | −27.7 | 9.8 | 17.9 | −29.3 (−34.0 to −24.6) | <.001 |
| High depersonalization | −7.3 | −16.9 | −4.9 | −14.7 | −2.4 (−7.0 to 2.1) | .29 |
| QOLe | ||||||
| Overall QOL score, mean (SD) | 1.2 (2.5) | 20.3 | 0.1 (1.7) | 1.5 | 1.1 (0.04 to 2.1) | .005 |
| Resiliencef | ||||||
| CDRISC score, mean (SD) | 1.3 (5.2) | 4.2 | 0.6 (4.0) | 2.0 | 0.7 (0.0 to 3.0) | .04 |
| Job satisfactiong | ||||||
| Global job satisfaction scale score, mean (SD) | 1.0 (7.1) | 2.3 | 0.4 (6.0) | 0.9 | 0.6 (−2.3 to 3.6) | .79 |
| Engagement and meaning at work | ||||||
| UWES score, mean (SD)h | ||||||
| Vigor | 0.2 (1.0) | 5.1 | 0.2 (0.7) | 5.0 | 0 (−0.3 to 0.5) | .16 |
| Dedication | 0.1 (0.8) | 2.2 | 0.1 (0.6) | 2.2 | 0 (−0.3 to 0.3) | .73 |
| Absorption | −0.1 (0.9) | −2.4 | 0.1 (0.7) | 2.4 | −0.2 (−0.5 to 0.2) | .77 |
| Empowerment at Work Scale score, mean (SD)i | 2.7 (9.1) | 4.9 | 3.0 (7.8) | 5.2 | −0.3 (−3.9 to 3.4) | .95 |
Abbreviations: CDRISC, Connor-Davidson Resilience scale; QOL, quality of life; UWES, Utrecht Work Engagement scale.
The score range is from 0 to 54; a higher score indicates greater burnout symptoms. The score was generated from the Emotional Exhaustion subscale of the Maslach Burnout Inventory.
The score range is from 0 to 30; higher score indicates greater burnout symptoms. Score generated from the Depersonalization subscale of the Maslach Burnout Inventory.
The score range is from 0 to 48; lower score indicates greater burnout symptoms. The score was generated from the Personal Accomplishment subscale of the Maslach Burnout Inventory.
Positive for symptoms of overall burnout if participant had a high score (≥27) on the emotional exhaustion and/or high score (≥10) on the depersonalization subscale.
The score range is from 0 to 10, with higher scores indicating better quality of life. A single-item linear analog scale was used.
The score range is from 0 to 40, with higher scores suggesting greater resilience. Resilience was measured using the 10-item CDRISC.
The scale range is from 0 to 60, with higher scores indicating greater job satisfaction. The 12-item Global Job Satisfaction subscale of the Physician Job Satisfaction Scale was used.
The scale range is from 0 to 6 for vigor, 0 to 5 for dedication, and 0 to 6 for absorption, with higher scores being more favorable.
The scale range is from 12 to 84, with higher score being more favorable.
Participants randomized to the intervention group also had a significant improvement in overall quality of life compared with those in the control group (mean [SD], 1.2 [2.5] vs 0.1 [1.7]; relative change, 20.3% vs 1.5%; P = .005) and an increase in resilience (mean [SD], 1.3 [5.2] vs 0.6 [4.0]; relative change, 4.2% vs 2.0%; P = .04) (Table 4). No difference, however, was found in job satisfaction or measures of engagement and meaning at work between the intervention and control groups.
Discussion
In this pilot randomized clinical trial, participants who received 3.5 hours of professional coaching during a 5-month period had a significant reduction in emotional exhaustion and overall symptoms of burnout, as well as improvements in overall quality of life and resilience. The magnitudes of reduction in the emotional exhaustion score and in overall burnout were substantial and higher than in prior interventions15 and were likely to lead to a meaningful difference in rates of adverse outcomes.3,5,42 We did not observe statistically significant reductions in depersonalization or improvements in job satisfaction, engagement, or meaning in work, highlighting the reality that coaching, while useful, is not a replacement for organizational efforts to improve the practice environment and address the underlying drivers of burnout and dissatisfaction among physicians.
Improvement in some but not all aspects of well-being is consistent with findings from previous intervention studies.15,16 For example, a randomized intervention study of a facilitated physician small-group curriculum resulted in reductions in depersonalization and improvements in meaning and engagement in work, but no reduction in emotional exhaustion or change in job satisfaction.18 In that highly structured intervention, preselected topics were discussed in groups, allowing for building of collegiality through reflection and discussions of shared experiences. In contrast, in our study, coaching topics were unscripted, allowing individuals to tailor the session to their personal needs. The intervention in our study was designed to address a diverse range of individual physicians’ professional needs (eg, clinical work, career direction, leadership, work-life integration, and self-care)17 in a confidential setting devoid of traditional hierarchy. Identified needs, goals, and action plans could focus on modifying individual behavior to promote well-being and facilitate decisions regarding an individual’s career, as well as on individual action to change detrimental aspects of the work environment. It is likely that a range of approaches are needed to address various aspects adversely affecting physician well-being and career satisfaction.15,16
This study suggests that individual or institutional investment in professional coaching may be one useful approach to supporting the professional workforce. Professional coaching is widely used in industries outside of medicine and has been demonstrated in studies of other professionals to enhance leadership and managerial and interpersonal skills and to foster personal growth.21,22,23,24,25,26,27,28,29,30,31 The telephone-based coaching approach used in this study (as opposed to in-person coaching) is universally available to physicians in the United States, making it relevant to all practice settings. The use of professional coaches from outside the organization incurs cost, but then so would internal coaching (eg, by taking the coaches away from other activities in which they might generate revenue). In addition, external coaching by certified professionals may provide greater credibility and psychological safety.52 Regardless, the business case for investment in evidence-based strategies that improve physician well-being has been well articulated.53
External professional coaching can be complementary to mentorship and can overcome some of its challenges and limitations. An appropriate mentor or particular type of mentorship relationship may not always be available, particularly for physicians in community-based practices. Even within large practices, there are barriers to effective mentorship. For example, midcareer physicians, who have been reported to struggle the most with burnout,54 may not have access to more senior physicians to mentor them, or they may not feel comfortable engaging with mentors owing to the hierarchical structure. Also, the dimensions for which physicians need mentorship are diverse, and often no single individual is an appropriate mentor for all dimensions. Furthermore, the time for training internal mentors is often limited, and physicians may have confidentiality concerns regarding how open and vulnerable they should be with colleagues serving as mentors who may also be supervisors in some settings. Professional coaches are highly trained individuals who are credentialed, adhere to a professional code of ethics, and are prepared to address a diverse range of topics and needs. Thus, external professional coaching overcomes many of the barriers to traditional formal and informal mentorship relationships.
Professional coaching differs markedly from other commonly described individually focused offerings (eg, mindfulness, nutrition, exercise, and support groups). Most of the topics discussed during the coaching sessions in our study centered on professional dimensions. Hence, coaching provided an avenue to assist individuals in their effort to navigate their professional life, work choices, and career direction and to build a capacity to influence organizational systems that affect their well-being. As such, coaching expands the framework of the types of offerings that organizations can provide to assist physicians both personally and professionally.
Limitations
This study has a number of limitations. First, the sample size was modest. Second, trial participants volunteered. Some physicians who may benefit from coaching may not choose to access it, while other physicians may not find coaching to be an appealing modality to address burnout symptoms or other professional challenges. The factors associated with lower recruitment among men relative to women could be determined from this study and warrant further investigation. Apart from sex, the trial participants and the eligible physicians who did not volunteer to participate were similar with respect to the number of years in practice, practice location (academic and community-based), and specialty (generalist vs subspecialist). However, other important differences may exist between these 2 groups, including levels of distress. The baseline levels of burnout were higher for study volunteers than the baseline levels reported in other studies of physicians,1,55 which suggests that the study appealed to those in greatest need of the intervention. Third, although the study was a multisite study that enrolled physicians in both academic and community practice settings, it was conducted within a single organization and included only physicians who had been in practice for 5 to 30 years. Additional studies are needed to explore the efficacy of professional coaching for physicians in other practice models (eg, solo practitioners) and career stages. Fourth, we did not assess long-term or postintervention effects, and the durability of the benefit of coaching is unknown. Additional study is needed to determine if repeated coaching is needed to sustain or boost the effect on physician well-being. Fifth, although we reached our enrollment target, we could determine how much interest physicians as a whole have in coaching. Sixth, the study was not blinded. Seventh, coaching was delivered by 1 company, and the topics discussed were not scripted, potentially limiting reproducibility and generalizability. Professional coaching, however, is a well-defined discipline, and we used credentialed coaches. In that regard, it would be expected that similarly credentialed coaches from other agencies would yield a similar effect. Providing the individuals being coached with a choice in deciding what topics it would be most helpful for them to receive coaching on is a fundamental principle of coaching. Additional studies are needed to determine the optimal design of coaching sessions, including the number and length of sessions.
Conclusions
The results of this pilot randomized trial suggest that organizationally sponsored professional coaching for physicians can reduce emotional exhaustion, improve overall quality of life, and build resilience. This intervention adds to the growing literature of evidence-based approaches to promote physician well-being and should be considered a complementary strategy to be deployed in combination with other organizational approaches to improve system-level drivers of work-related stressors.
Study Protocol
Data Sharing Statement
References
- 1.Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014 [published correction appears in Mayo Clin Proc. 2016;91(2):276]. Mayo Clin Proc. 2015;90(12):1600-1613. doi: 10.1016/j.mayocp.2015.08.023 [DOI] [PubMed] [Google Scholar]
- 2.Shanafelt TD, Boone S, Tan L, et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med. 2012;172(18):1377-1385. doi: 10.1001/archinternmed.2012.3199 [DOI] [PubMed] [Google Scholar]
- 3.Shanafelt TD, Balch CM, Bechamps G, et al. Burnout and medical errors among American surgeons. Ann Surg. 2010;251(6):995-1000. doi: 10.1097/SLA.0b013e3181bfdab3 [DOI] [PubMed] [Google Scholar]
- 4.Shanafelt T, Sloan J, Satele D, Balch C. Why do surgeons consider leaving practice? J Am Coll Surg. 2011;212(3):421-422. doi: 10.1016/j.jamcollsurg.2010.11.006 [DOI] [PubMed] [Google Scholar]
- 5.West CP, Tan AD, Habermann TM, Sloan JA, Shanafelt TD. Association of resident fatigue and distress with perceived medical errors. JAMA. 2009;302(12):1294-1300. doi: 10.1001/jama.2009.1389 [DOI] [PubMed] [Google Scholar]
- 6.Wallace JE, Lemaire JB, Ghali WA. Physician wellness: a missing quality indicator. Lancet. 2009;374(9702):1714-1721. doi: 10.1016/S0140-6736(09)61424-0 [DOI] [PubMed] [Google Scholar]
- 7.Shanafelt TD, Dyrbye LN, West CP, Sinsky CA. Potential impact of burnout on the US physician workforce. Mayo Clin Proc. 2016;91(11):1667-1668. doi: 10.1016/j.mayocp.2016.08.016 [DOI] [PubMed] [Google Scholar]
- 8.Shanafelt TD, Mungo M, Schmitgen J, et al. Longitudinal study evaluating the association between physician burnout and changes in professional work effort. Mayo Clin Proc. 2016;91(4):422-431. doi: 10.1016/j.mayocp.2016.02.001 [DOI] [PubMed] [Google Scholar]
- 9.Dyrbye LN, Shanafelt TD. Physician burnout: a potential threat to successful health care reform. JAMA. 2011;305(19):2009-2010. doi: 10.1001/jama.2011.652 [DOI] [PubMed] [Google Scholar]
- 10.Shanafelt TD, Noseworthy JH. Executive leadership and physician well-being: nine organizational strategies to promote engagement and reduce burnout. Mayo Clin Proc. 2017;92(1):129-146. doi: 10.1016/j.mayocp.2016.10.004 [DOI] [PubMed] [Google Scholar]
- 11.Dyrbye LN, Shanafelt TD, Balch CM, Satele D, Sloan J, Freischlag J. Relationship between work-home conflicts and burnout among American surgeons: a comparison by sex. Arch Surg. 2011;146(2):211-217. doi: 10.1001/archsurg.2010.310 [DOI] [PubMed] [Google Scholar]
- 12.Shanafelt TD, Dyrbye LN, Sinsky C, et al. Relationship between clerical burden and characteristics of the electronic environment with physician burnout and professional satisfaction. Mayo Clin Proc. 2016;91(7):836-848. doi: 10.1016/j.mayocp.2016.05.007 [DOI] [PubMed] [Google Scholar]
- 13.Shanafelt TD, Gorringe G, Menaker R, et al. Impact of organizational leadership on physician burnout and satisfaction. Mayo Clin Proc. 2015;90(4):432-440. doi: 10.1016/j.mayocp.2015.01.012 [DOI] [PubMed] [Google Scholar]
- 14.Dyrbye LN, Shanafelt TD, Sinsky CA, et al. Burnout Among Health Care Professionals: A Call to Explore and Address This Underrecognized Threat to Safe, High-Quality Care. Washington, DC: National Academy of Medicine; 2017. [Google Scholar]
- 15.West CP, Dyrbye LN, Erwin PJ, Shanafelt TD. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet. 2016;388(10057):2272-2281. doi: 10.1016/S0140-6736(16)31279-X [DOI] [PubMed] [Google Scholar]
- 16.Panagioti M, Panagopoulou E, Bower P, et al. Controlled interventions to reduce burnout in physicians: a systematic review and meta-analysis. JAMA Intern Med. 2017;177(2):195-205. doi: 10.1001/jamainternmed.2016.7674 [DOI] [PubMed] [Google Scholar]
- 17.Sambunjak D, Straus SE, Marusić A. Mentoring in academic medicine: a systematic review. JAMA. 2006;296(9):1103-1115. doi: 10.1001/jama.296.9.1103 [DOI] [PubMed] [Google Scholar]
- 18.West CP, Dyrbye LN, Rabatin JT, et al. Intervention to promote physician well-being, job satisfaction, and professionalism: a randomized clinical trial. JAMA Intern Med. 2014;174(4):527-533. doi: 10.1001/jamainternmed.2013.14387 [DOI] [PubMed] [Google Scholar]
- 19.Shapiro J, Galowitz P. Peer support for clinicians: a programmatic approach. Acad Med. 2016;91(9):1200-1204. doi: 10.1097/ACM.0000000000001297 [DOI] [PubMed] [Google Scholar]
- 20.Shanafelt TD, Lightner DJ, Conley CR, et al. An organization model to assist individual physicians, scientists, and senior health care administrators with personal and professional needs. Mayo Clin Proc. 2017;92(11):1688-1696. doi: 10.1016/j.mayocp.2017.08.020 [DOI] [PubMed] [Google Scholar]
- 21.Thorn PM, Raj JM. A culture of coaching: achieving peak performance of individuals and teams in academic health centers. Acad Med. 2012;87(11):1482-1483. doi: 10.1097/ACM.0b013e31826ce3bc [DOI] [PubMed] [Google Scholar]
- 22.Askin WJ. Coaching for physicians: building more resilient doctors. Can Fam Physician. 2008;54(10):1399-1400. [PMC free article] [PubMed] [Google Scholar]
- 23.Gazelle G, Liebschutz JM, Riess H. Physician burnout: coaching a way out. J Gen Intern Med. 2015;30(4):508-513. doi: 10.1007/s11606-014-3144-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Honaman JC. Coaching emerging healthcare leaders. Healthc Exec. 2015;30(5):62–,64-65.. [PubMed] [Google Scholar]
- 25.Schneider S, Kingsolver K, Rosdahl J. Physician coaching to enhance well-being: a qualitative analysis of a pilot intervention. Explore (NY). 2014;10(6):372-379. doi: 10.1016/j.explore.2014.08.007 [DOI] [PubMed] [Google Scholar]
- 26.Yule S, Parker SH, Wilkinson J, et al. Coaching non-technical skills improves surgical residents’ performance in a simulated operating room. J Surg Educ. 2015;72(6):1124-1130. doi: 10.1016/j.jsurg.2015.06.012 [DOI] [PubMed] [Google Scholar]
- 27.McGovern J, Lindemann M, Vergara M, Murphy S, Barker L, Warrenfeltz R. Maximizing the impact of executive coaching: Behavioral change, organizational outcomes and return on investment. Manchester Review. 2001;6(1):1-9. [Google Scholar]
- 28.Coutu D, Kauffman C What can coaches do for you? Harvard Business Review Research Report. https://hbr.org/2008/12/what-can-coaches-do-for-you. Published January 2009. Accessed June 26, 2019.
- 29.Kauffman C, Coutu D The realities of executive coaching. Harvard Business Review Research Report. http://www.carolkauffman.com/images/pdfs/Kauffman_Coutu_HRB_survey_report.pdf. Published January 2009. Accessed June 26, 2019.
- 30.Theeboom T, Beersma B, van Vianen A. Does coaching work? a meta-analysis on the effects of coaching on individual level outcomes in an organizational context. J Posit Psychol. 2014;9(1):1-18. doi: 10.1080/17439760.2013.837499 26640507 [DOI] [Google Scholar]
- 31.Phillips JJ. Measuring the ROI of a coaching intervention: part 2. Perform Improv. 2007;46(10):10-23. doi: 10.1002/pfi.167 [DOI] [Google Scholar]
- 32.Grant AM, Curtayne L, Burton G. Executive coaching enhances goal attainment, resilience and workplace well-being: a randomised controlled study. J Posit Psychol. 2009;4(5):396-407. doi: 10.1080/17439760902992456 [DOI] [Google Scholar]
- 33.Grant AM, Green LS, Rynsaardt J. Developmental coaching for high school teachers: executive coaching goes to school. Consult Psychol J. 2010;62(3):151-168. doi: 10.1037/a0019212 [DOI] [Google Scholar]
- 34.Gardiner M, Kearns H, Tiggemann M. Effectiveness of cognitive behavioural coaching in improving the well-being and retention of rural general practitioners. Aust J Rural Health. 2013;21(3):183-189. doi: 10.1111/ajr.12033 [DOI] [PubMed] [Google Scholar]
- 35.Green DE, Maximin S. Professional coaching in radiology: practice corner. Radiographics. 2015;35(3):971-972. doi: 10.1148/rg.2015140306 [DOI] [PubMed] [Google Scholar]
- 36.Palamara K, Kauffman C, Stone VE, Bazari H, Donelan K. Promoting success: a professional development coaching program for interns in medicine. J Grad Med Educ. 2015;7(4):630-637. doi: 10.4300/JGME-D-14-00791.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Siegler J. Raising physician performance with coaching: respect, collaboration and unified expectations can catalyze future success. Healthc Exec. 2016;31(3):88–,90-91.. [PubMed] [Google Scholar]
- 38.Norman GR, Sloan JA, Wyrwich KW. The truly remarkable universality of half a standard deviation: confirmation through another look. Expert Rev Pharmacoecon Outcomes Res. 2004;4(5):581-585. doi: 10.1586/14737167.4.5.581 [DOI] [PubMed] [Google Scholar]
- 39.Maslach C, Jackson SE, Leiter MP. Maslach Burnout Inventory. 4th ed Menlo Park, CA: Mind Garden; 2016. [Google Scholar]
- 40.Maslach C, Jackson SE, Leiter MP. Maslach Burnout Inventory Manual. 3rd ed Palo Alto, CA: Consulting Psychologists Press; 1996. [Google Scholar]
- 41.National Academy of Medicine Validated instruments to assess work-related dimensions of well-being. https://nam.edu/valid-reliable-survey-instruments-measure-burnout-well-work-related-dimensions/. Accessed June 28, 2019.
- 42.Shanafelt TD, Balch CM, Dyrbye L, et al. Special report: suicidal ideation among American surgeons. Arch Surg. 2011;146(1):54-62. doi: 10.1001/archsurg.2010.292 [DOI] [PubMed] [Google Scholar]
- 43.Shanafelt TD, Bradley KA, Wipf JE, Back AL. Burnout and self-reported patient care in an internal medicine residency program. Ann Intern Med. 2002;136(5):358-367. doi: 10.7326/0003-4819-136-5-200203050-00008 [DOI] [PubMed] [Google Scholar]
- 44.Thomas NK. Resident burnout. JAMA. 2004;292(23):2880-2889. doi: 10.1001/jama.292.23.2880 [DOI] [PubMed] [Google Scholar]
- 45.Campbell-Sills L, Stein MB. Psychometric analysis and refinement of the Connor-Davidson Resilience Scale (CD-RISC): validation of a 10-item measure of resilience. J Trauma Stress. 2007;20(6):1019-1028. doi: 10.1002/jts.20271 [DOI] [PubMed] [Google Scholar]
- 46.Connor KM, Davidson JRT. Development of a new resilience scale: the Connor-Davidson Resilience Scale (CD-RISC). Depress Anxiety. 2003;18(2):76-82. doi: 10.1002/da.10113 [DOI] [PubMed] [Google Scholar]
- 47.Norman GR, Sloan JA, Wyrwich KW. Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Med Care. 2003;41(5):582-592. doi: 10.1097/01.MLR.0000062554.74615.4C [DOI] [PubMed] [Google Scholar]
- 48.Revicki DA, Cella D, Hays RD, Sloan JA, Lenderking WR, Aaronson NK. Responsiveness and minimal important differences for patient reported outcomes. Health Qual Life Outcomes. 2006;4:70. doi: 10.1186/1477-7525-4-70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Williams ES, Konrad TR, Linzer M, et al. ; SGIM Career Satisfaction Study Group; Society of General Internal Medicine . Refining the measurement of physician job satisfaction: results from the Physician Worklife Survey. Med Care. 1999;37(11):1140-1154. doi: 10.1097/00005650-199911000-00006 [DOI] [PubMed] [Google Scholar]
- 50.Schaufeli W, Bakker A UWES: Utrecht Work Engagement Scale: preliminary manual [version 1.1, December 2004]. https://www.wilmarschaufeli.nl/publications/Schaufeli/Test%20Manuals/Test_manual_UWES_English.pdf. Accessed June 28, 2019.
- 51.Spreitzer GM. Psychological empowerment in the workplace: Dimensions, measurement, and validation. Acad Manage J. 1995;38:1442-1465. [Google Scholar]
- 52.Rosenbaum L. Cursed by knowledge—building a culture of psychological safety. N Engl J Med. 2019;380(8):786-790. doi: 10.1056/NEJMms1813429 [DOI] [PubMed] [Google Scholar]
- 53.Shanafelt T, Goh J, Sinsky C. The business case for investing in physician well-being. JAMA Intern Med. 2017;177(12):1826-1832. doi: 10.1001/jamainternmed.2017.4340 [DOI] [PubMed] [Google Scholar]
- 54.Dyrbye LNVP, Varkey P, Boone SL, Satele DV, Sloan JA, Shanafelt TD. Physician satisfaction and burnout at different career stages. Mayo Clin Proc. 2013;88(12):1358-1367. doi: 10.1016/j.mayocp.2013.07.016 [DOI] [PubMed] [Google Scholar]
- 55.Shanafelt TD, West CP, Sinsky C, et al. Changes in burnout and satisfaction with work-life integration in physicians and the general US working population between 2011-2017 [published online February 13, 2019]. Mayo Clin Proc. doi: 10.1016/j.mayocp.2018.10.023 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Study Protocol
Data Sharing Statement