Abstract
This study examined emergency department medical records to identify cases of inappropriately low trauma-level activation and factors associated with the risk of such undertriage.
Earlier recognition of severe traumatic injury and triage to the proper trauma level designation are essential factors in the safe and effective care of trauma patients.1 Trauma-level activation often dictates the personnel present at the initial trauma resuscitation, and undertriage has been associated with worse clinical outcomes.2
Traditionally, undertriage has been evaluated using the Injury Severity Score. The problem with using this approach to evaluate triage-level appropriateness is that the Injury Severity Score is determined either at the time of discharge or death and therefore cannot prospectively identify patients who were undertriaged.
After a review of 10 years (2004-2014) of data on adult trauma activations at a single institution, tachypnea (respiratory rate, >22 breaths per minute) and blunt thoracic injury were associated with undertriage and were added to higher-level trauma activation criteria at the institution.3 In this study, we sought to determine if other clinically relevant prehospital criteria could be used to accurately identify patients who are more likely to be undertriaged.
Methods
We performed a retrospective review of the prospective trauma database at a single institution to identify all lower-level adult activations from January 2014 through December 2016. Patient demographic factors, prehospital vital signs obtained during transport, Glasgow Coma Scale scores, Abbreviated Injury Scores, and urgent procedures were collected. Undertriage was defined as lower-level activations that occurred during incidents meeting higher-level criteria or requiring predefined life-saving interventions (cardiopulmonary resuscitation, resuscitative thoracotomy, tube thoracostomy, endotracheal intubation, surgical airway management, or blood transfusion) within 1 hour of arrival at the hospital. Rates of undertriage were calculated and odds ratios (ORs) with 95% CIs using multivariate analysis to identify factors associated with undertriage. Severe injury was defined as an Abbreviated Injury Scale score in a body region of 3 or more.
This study was approved by the institutional review board at Oregon Health & Science University. Informed consent for study participants was waived because of the retrospective nature of the study.
Data analysis was completed between October 2017 through December 2017 with JMP version 14 (SAS Inc). All P values less than .05 were considered significant.
Results
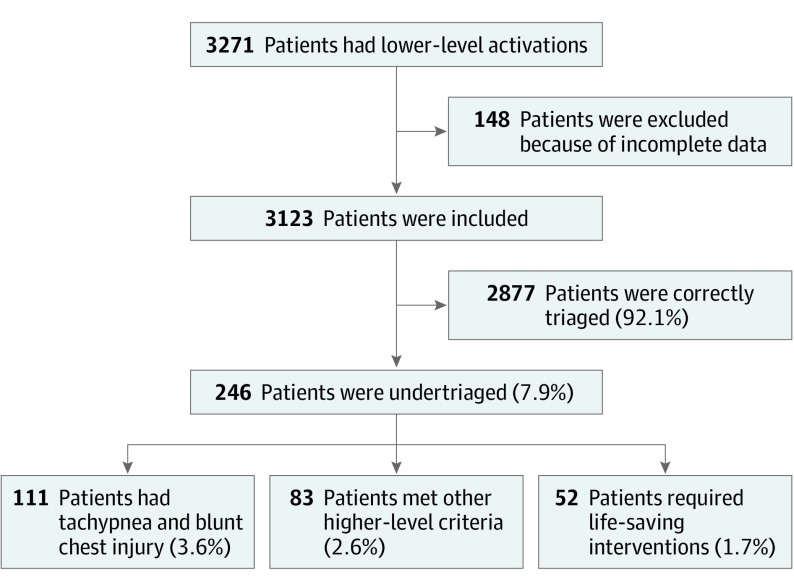
There were 3271 lower-level trauma activations from January 2014 through December 2016 at a level-1 trauma center. A total of 148 patients were excluded owing to incomplete data, leaving 3123 patients. Of these, 2877 patients (92.1%) were correctly triaged to the lower-level designation, while 247 patients (7.9%) were undertriaged. Of the 3123 total cases, 111 patients (3.6%) were undertriaged because they met the newly implemented higher-level criteria of tachypnea and blunt thoracic injury. An additional 83 patients (2.6%) were undertriaged because they met other higher-level triage criteria (ie, systolic blood pressure <90 mm Hg or Glasgow Coma Scale score <9 points). Finally, 52 patients (1.7%) were undertriaged because they required a life-saving intervention within 1 hour of arrival (Figure). Of the patients who required a life-saving intervention, 23 required tube thoracostomy, 16 required blood transfusion, and 13 required endotracheal intubation.
Figure. Flowchart of Lower-Level Trauma Activations.
On multivariate analysis, increased age (OR, 1.07 [95% CI, 1.03-1.10] per 1-year increment), male sex (OR, 1.39 [95% CI, 1.04-1.85]), lower Glasgow Coma Scale scores (OR, 1.62 [95% CI, 1.53-1.71] per 1-point increment), tachypnea (OR, 1.24 [95% CI, 1.19-1.28] per 1 breath more than 22 breaths per minute), and hypotension (OR, 1.14 [95% CI, 1.11-1.18] per 5–mm Hg reduction) were associated with significantly increased odds of undertriage (Table). When looking at the most severely injured patients (Abbreviated Injury Score ≥3 in a body region), 431 patients (28.5%) with a severe chest injury were undertriaged, which was significantly higher than those with severe injury to the abdomen or pelvis (109 patients [16.5%]; P < .001), extremities (389 patients [12.9%]; P < .001), or head (454 patients [9.9%]; P < .001).
Table. Multivariate Analysis of Characteristics Associated With Undertriage.
| Patient and Injury Characteristic | Odds Ratio (95% CI) | P Value |
|---|---|---|
| Glasgow Coma Scalea | 1.62 (1.53-1.71) | <.001 |
| Respiratory rateb | 1.24 (1.19-1.28) | <.001 |
| Systolic blood pressurec | 1.14 (1.11-1.18) | <.001 |
| Heart rated | 0.97 (0.91-1.04) | .45 |
| Agee | 1.07 (1.03-1.10) | <.001 |
| Male | 1.39 (1.04-1.85) | .02 |
| Blunt injury | 0.65 (0.40-1.05) | .08 |
| Packed red blood cells given in initial 4 hf | 1.11 (1.01-1.21) | .03 |
Per 1-point reduction.
Per 1 breath more than 22 breaths per minute.
Per 5–mm Hg reduction.
Per 10–beats per minute increase.
Per 5-year increase.
Per 1-unit increase.
Discussion
Proper triage of patients with traumatic injuries is essential for the safe treatment of trauma patients. At many institutions, including the one at which this study was conducted, lower-level activations are generally directly managed by a chief surgical resident, which in the setting of undertriage potentially exposes patients to increased morbidity and mortality.4,5,6 Because of this, clinically relevant and accurate triage criteria are crucial.
In this study, undertriage was mostly attributable to not following predetermined triage criteria. This is likely from a communication breakdown between prehospital and emergency department practitioners. Clear communication is essential in all aspects of trauma care, and review of these communications will help determine the next steps to continue improving undertriage rates.
We found that thoracic injury, hypotension, tachypnea, and lower Glasgow Coma Scale scores were prehospital variables associated with an increased risk of undertriage. These variables should be considered when developing triage criteria and in the evaluation of proper trauma triage designation.
References
- 1.Sasser SM, Hunt RC, Faul M, et al. ; Centers for Disease Control and Prevention (CDC) . Guidelines for field triage of injured patients: recommendations of the National Expert Panel on Field Triage, 2011. MMWR Recomm Rep. 2012;61(RR-1):1-20. [PubMed] [Google Scholar]
- 2.Rotondo MF, Cribari C, Smith RS; American College of Surgeons Committee on Trauma Resources for the optimal care of the injured patient. https://www.facs.org/~/media/files/quality%20programs/trauma/vrc%20resources/resources%20for%20optimal%20care.ashx. Published 2014. Accessed June 27, 2019.
- 3.Yonge JD, Bohan PK, Watson JJ, Connelly CR, Eastes L, Schreiber MA. The respiratory rate: a neglected triage tool for pre-hospital identification of trauma patients. World J Surg. 2018;42(5):1321-1326. doi: 10.1007/s00268-017-4353-4 [DOI] [PubMed] [Google Scholar]
- 4.Durham R, Shapiro D, Flint L. In-house trauma attendings: is there a difference? Am J Surg. 2005;190(6):960-966. doi: 10.1016/j.amjsurg.2005.08.028 [DOI] [PubMed] [Google Scholar]
- 5.Cox JA, Bernard AC, Bottiggi AJ, et al. Influence of in-house attending presence on trauma outcomes and hospital efficiency. J Am Coll Surg. 2014;218(4):734-738. doi: 10.1016/j.jamcollsurg.2013.12.027 [DOI] [PubMed] [Google Scholar]
- 6.Cohen R, Adini B, Radomislensky I, Givon A, Rivkind AI, Peleg K. Involvement of surgical residents in the management of trauma patients in the emergency room: does the presence of an attending physician affect outcomes? World J Surg. 2012;36(3):539-547. doi: 10.1007/s00268-012-1428-0 [DOI] [PubMed] [Google Scholar]