Abstract
Objective
The American Urological Association guidelines recommend 24-hour urine testing in patients with urinary stone disease to decrease the risk of stone recurrence; however, national practice patterns for 24-hour urine testing are not well characterized. Our objective is to determine the prevalence of 24-hour urine testing in patients with urinary stone disease in the Veterans Health Administration and examine patient-specific and facility-level factors associated with 24-hour urine testing. Identifying variations in clinical practice can inform future quality improvement efforts in the management of urinary stone disease in integrated healthcare systems.
Materials and methods
We accessed national Veterans Health Administration data through the Corporate Data Warehouse (CDW), hosted by the Veterans Affairs Informatics and Computing Infrastructure (VINCI), to identify patients with urinary stone disease. We defined stone formers as Veterans with one inpatient ICD-9 code for kidney or ureteral stones, two or more outpatient ICD-9 codes for kidney or ureteral stones, or one or more CPT codes for kidney or ureteral stone procedures from 2007 through 2013. We defined a 24-hour urine test as a 24-hour collection for calcium, oxalate, citrate or sulfate. We used multivariable regression to assess demographic, geographic, and selected clinical factors associated with 24-hour urine testing.
Results
We identified 130,489 Veterans with urinary stone disease; 19,288 (14.8%) underwent 24-hour urine testing. Patients who completed 24-hour urine testing were younger, had fewer comorbidities, and were more likely to be White. Utilization of 24-hour urine testing varied widely by geography and facility, the latter ranging from 1 to 40%.
Conclusions
Fewer than one in six patients with urinary stone disease complete 24-hour urine testing in the Veterans Health Administration. In addition, utilization of 24-hour urine testing varies widely by facility identifying a target area for improvement in the care of patients with urinary stone disease. Future efforts to increase utilization of 24-hour urine testing and improve clinician awareness of targeted approaches to stone prevention may be warranted to reduce the morbidity and cost of urinary stone disease.
Introduction
Twenty-four-hour urine testing is employed in the metabolic evaluation and treatment of patients with urinary stone disease (USD). Clinicians use the 24-hour urine collection, along with chemical analysis of kidney stone composition, to diagnose urinary or systemic abnormalities responsible for kidney stone formation. The 24-hour urine collection can also be used to guide dietary and pharmacologic treatments for USD. Currently, the American Urological Association (AUA) guidelines recommend 24-hour urine testing for evaluating and treating recurrent stone formers and high-risk or interested first time stone formers [1].
While there is sound physiological rationale for incorporating 24-hour urine testing in assessing USD risk, variability in the application of, and effectiveness of strategies incorporating, 24-hour urine testing are not well characterized [2]. To address these gaps in evidence, we used a large national cohort of patients in the Veterans Health Administration (VHA) for the following objectives: 1) estimate the prevalence of 24-hour urine testing in Veterans with USD across the United States; 2) identify demographic, geographic, and clinical characteristics of patients with USD who are more or less likely to receive 24-hour urine testing; and 3) characterize healthcare utilization associated with 24-hour urine testing. We hypothesized that the prevalence of 24-hour urine testing remains low despite clinical practice guidelines recommending metabolic evaluation of patients with USD, and that application of 24-hour urine testing varies widely by patient-specific and facility-level characteristics.
Materials and methods
Data and study population
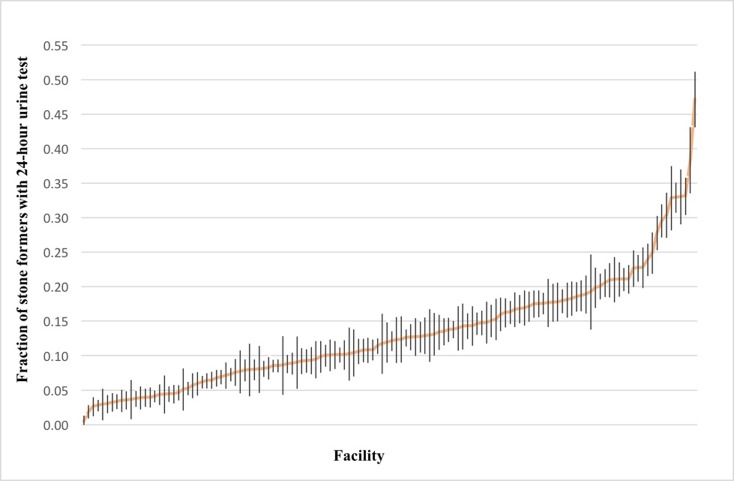
The Stanford Institutional Review Board and Veterans Administration Research and Development Committee (FWA00000929) approved this study and waived informed consent under the following protocol, IRB 6 Registration #4947. All records were fully anonymized before accessed. We accessed national VHA data stored in the Corporate Data Warehouse (CDW), hosted by the Veterans Affairs Informatics and Computing Infrastructure (VINCI), to identify patients with USD from 2007 through 2013. We defined “stone formers” as patients who had one or more inpatient ICD-9 codes for kidney or ureteral stones, two or more outpatient ICD-9 codes for kidney or ureteral stones, or one or more CPT codes for kidney or ureteral stone procedures in a single year [3]. We limited our cohort to patients who were free from a kidney or ureteral stone diagnosis or procedure in the two years before entry into the cohort to ascertain how clinicians respond to a new stone event episode (Fig 1). Each patient entered the cohort once, at the time of his or her first qualification as a stone former during the observation period.
Fig 1. Flow chart showing patient cohort selection and exclusion.
Primary outcome
We identified the fraction of stone formers who completed a 24-hour urine collection from time of entry into the observation period through 2014. We used Logical Observation Identifiers Names and Codes (LOINC) to define a 24-hour urine collection as the presence of a 24-hour urine measurement for calcium, oxalate, citrate or sulfate. We based our definition on the assumptions that 24-hour testing for urine calcium is a sensitive proxy for USD evaluation and that 24-hour urine testing for oxalate, citrate, or sulfate is a specific proxy. We chose not to define a 24-hour urine collection as requiring the presence of all parameters that are included in a 24-hour urine stone risk panel due to our concern that it would lead to under-ascertainment of 24-hour urine testing. To ascertain if VHA includes data from 24-hour urine collections processed by an outside laboratory, we queried 24-hour urine data from our local VHA facility, which sends out 24-hour urine samples to Quest Diagnostics for measurement of urine calcium, oxalate, citrate, and sulfate, and we confirmed that these test results were recorded in the VHA.
Patient characteristics
We compared demographic and clinical characteristics among stone formers who completed a 24-hour urine collection and those who did not. We examined the following factors we considered to be associated with stone risk: age, sex, race/ethnicity, history of cardiovascular disease (CVD), diabetes, cancer, hyperparathyroidism, paralysis, chronic obstructive pulmonary disease (COPD), dementia, prior 24-hour urine collection, and geographic region (broadly characterized as Northeast, Southeast, West, Midwest). To assess if a stone former received specialty stone care, we identified provider codes associated with a nephrology or urology clinic visit 6 months after their initial stone diagnosis (Table 1).
Table 1. Nephrology and urology clinic visit codes.
| Provider Codes | Clinic Stop Codes | |
|---|---|---|
| Nephrology | 070929, 151003,11512,181018,182515,040403, 150216 | 313 |
| Urology | 070951, 118200, 118000, 183400 | 414 |
Statistical analysis
We first categorized stone formers into those who had a 24-hour urine collection and those who did not. We compared continuous variables using Student’s t-tests, and we compared categorical variables with the x2 test. We used multivariable logistic regression to estimate the odds ratios (ORs) and 95% confidence intervals (95% CI) of having a 24-hour urine collection after adjusting for age, sex, race/ethnicity, geography, prior kidney stone procedure, prior 24-hour urine collection, study entry criteria (outpatient, inpatient, or kidney stone procedure), and Charlson comorbidity index. We used the location associated with stone diagnosis code to assign each patient to one of 150 facilities across the VHA. We then compared the use of 24-hour urine testing across VHA facilities. We considered 2-tailed p-values <0.05 as statistically significant. We conducted our analysis using SAS version 9.4 (Cary, NC, USA).
Results
We identified 130,489 patients with USD from 2007 through 2013 and found that 19,288 of these patients (14.8%) completed at least one 24-hour urine collection (Table 2). In both groups, male sex (92.7% and 94.9%) and White race (79.5% and 77.4%) were most common. Stone formers who completed a 24-hour urine collection were more likely to qualify for the cohort through two or more outpatient encounters (70.5% versus 61.1%, p<0.001), whereas those who did not complete a 24-hour urine collection were more likely to qualify for the cohort through an inpatient encounter (12.9% versus 7.9%, p<0.001) or stone procedure (26% versus 21.5%, p<0.001). Stone formers who completed 24-hour urine testing received more stone procedures compared to those who did not, with the median number of procedures being 1 (IQR 0–2) versus 0 (IQR, 0–1), respectively (p<0.001). Sixty-four percent of stone formers visited either a nephrologist or urologist 6 months after their initial stone diagnosis, and 18.7% of these stone formers completed a 24-hour urine collection (Table 3).
Table 2. Baseline characteristics of stone formers with and without a 24-hour urine collection.
| Characteristics | With 24-hour | Without 24-hour | p-value |
|---|---|---|---|
| (n = 19,288) | (n = 111,201) | ||
| Age (mean ± SD, years) | 58.3 ± 12.5 | 61.2 ± 13.8 | <0.001 |
| Sex (n,%) | |||
| Male | 17,884 (92.7) | 105,541 (94.9) | <0.001 |
| Female | 1404 (7.3) | 5660 (5.1) | <0.001 |
| Race/Ethnicity | |||
| White | 15,331 (79.5) | 86,013 (77.4) | <0.001 |
| Black | 1760 (9.1) | 12,301 (11.1) | <0.001 |
| Other or unknown | 1864 (9.7) | 9900 (8.9) | <0.001 |
| Stone Diagnosis | |||
| Inpatient | 1525 (7.9) | 14,326 (12.9) | <0.001 |
| Outpatient | 13,607 (70.5) | 67,931 (61.1) | <0.001 |
| Procedure | 4156 (21.5) | 28,944 (26) | <0.001 |
| Stone procedures (median, IQR) | 1 (0–2) | 0 (0–1) | <0.001 |
| Charlson Comorbidity Index (mean ± SD) | 2.1 ± 2.3 | 2.5 ± 2.6 | |
| Individual Conditions (n,%) | |||
| CVDa | 6405 (33.2) | 47,577 (42.8) | <0.001 |
| Diabetes Mellitus | 6042 (31.3) | 35,528 (31.9) | 0.08 |
| Cancer | 2580 (13.4) | 21,527 (19.1) | <0.001 |
| Paralysis | 574 (3.0) | 3527 (3.2) | 0.15 |
| COPD | 4617 (23.9) | 29,578 (26.6) | <0.001 |
| Dementia | 365 (1.9) | 4202 (3.8) | <0.001 |
| Hyperparathyroidism | 493 (2.6) | 324 (0.3) | <0.001 |
aCVD: includes cardiovascular disease, myocardial infarction, heart failure and peripheral vascular disease
Table 3. Stone specialty (Nephrology or Urology) provider care 6 months after stone diagnosis.
| Stone former (n,%) | Nephrology or Urology Visit (n = 84,086) |
No Specialty Visit (n = 46,393) |
p-value |
|---|---|---|---|
| With 24-hour | 15,722 (18.7) | 3556 (7.6) | <0.001 |
| Without 24-hour | 68,364 (81.3) | 42,837 (92.4) | <0.001 |
We assessed differences in comorbid illnesses between the two groups (Table 2). Stone formers who completed a 24-hour urine collection had fewer comorbid illnesses compared to those who did not (Charlson Comorbidity Index of 2.1 versus 2.5). In addition, specific diagnoses associated with USD were strongly associated with completion of a 24-hour urine collection. For example, patients with a history of hyperparathyroidism had 8.6-fold higher odds of completing a 24-hour urine collection compared to those who did not.
Using multivariable regression, we identified patient-specific factors associated with 24-hour urine testing in stone formers (Table 4). Stone formers who completed a 24-hour urine collection were more likely to be young or of White race. The odds of 24-hour urine testing were also directly related to the number of stone procedures (ORs are calculated in reference to a stone former without a stone procedure): 1–2 procedures (OR 1.91, 95% CI 1.84 to 1.99), 3–4 procedures (OR 2.89, 95% CI 2.72 to 3.06), or 5–6 procedures (OR 3.47, 95% CI 3.15 to 3.81). A stone former was much more likely to complete a 24-hour urine test if he or she completed a 24-hour urine test prior to the observation period (OR 3.06, 95% CI 2.80 to 3.34).
Table 4. Multivariable logistic regression reporting the odds of completing a 24-hour urine collection.
| Variable | Odds Ratio | Confidence Interval | p-value |
|---|---|---|---|
| Age (per decade) | 0.85 | 0.83–0.86 | <0.001 |
| Female vs. Male | 1.07 | 1.00–1.15 | .056 |
| White vs. Black | 1.28 | 1.20–1.36 | <0.001 |
| Stone Procedure | |||
| 0 | Ref | ||
| 1–2 | 1.91 | 1.84–1.99 | <0.001 |
| 3–4 | 2.89 | 2.72–3.06 | <0.001 |
| 5–6 | 3.47 | 3.15–3.81 | <0.001 |
| Charlson Comorbidity Index | |||
| 0 | Ref | ||
| 1 | 0.89 | 0.85–0.94 | <0.001 |
| 2 | 0.86 | 0.81–0.90 | <0.001 |
| 3 | 0.86 | 0.81–0.92 | <0.001 |
| 4 | 0.78 | 0.73–0.84 | <0.001 |
| > = 5 | 0.63 | 0.59–0.68 | <0.001 |
| Prior 24-hour urine test | 3.06 | 2.80–3.34 | <0.001 |
| Region | |||
| Midwest | Ref | ||
| West | 1.20 | 1.15–1.26 | <0.001 |
| Northeast | 0.71 | 0.67–0.75 | <0.001 |
| Southwest | 0.68 | 0.65–0.72 | <0.001 |
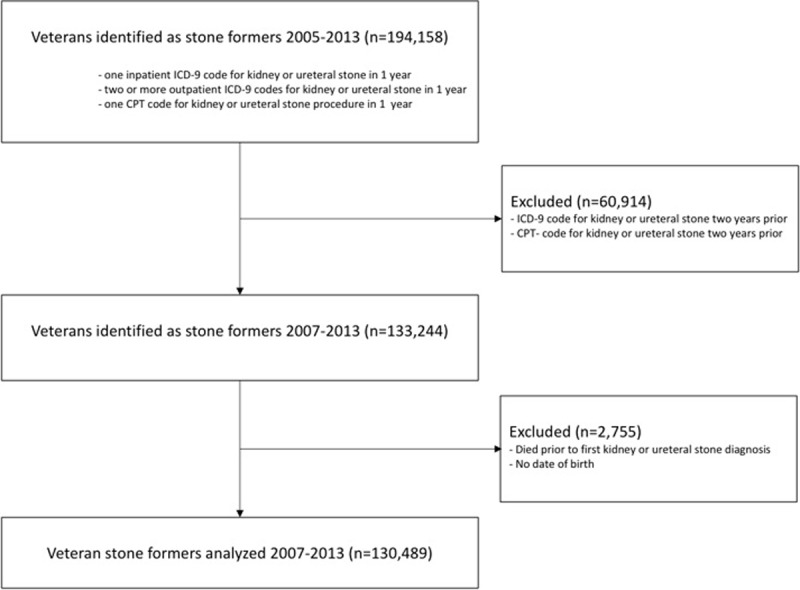
Next we examined geographic and facility-level variation in 24-hour urine testing in stone formers across the country (Table 4). Relative to stone formers in the Midwest, patients treated in the West were more likely (OR 1.20, 95% CI 1.15 to 1.26) and patients treated in the Northeast (OR 0.71, 95% CI 0.67 to 0.75) and Southeast (OR 0.68, 95% CI 0.65 to 0.72) were less likely to be tested. To further explore this geographic variation, we estimated the prevalence of 24-hour urine testing in stone formers at each of the VHA facilities. Among the 150 VHA facilities delivering care to stone formers, the unadjusted prevalence of 24-hour urine testing ranged between 1 and 40% (Fig 2). We also compared demographic and clinical characteristics of patients seen in the top and bottom decile of VHA facilities that administer 24-hour urine testing and found them to be similar (Table 5). While the volume of patients with USD was modestly higher in the top decile compared to the bottom decile of VHA facilities (9835 versus 7751 patients, respectively), the average number of stone procedures for each stone former within the observation period was similar (0.8 ± 1.4 versus 0.7 ± 1.3).
Fig 2. Prevalence of 24-hour urine testing by VHA facility.
Each bar reflects the standard error around the fraction estimate for each VHA facility.
Table 5. Baseline characteristics of stone formers with and without a 24-hour urine collection in the top and bottom decile of VHA facilities that administer 24-hour urine testing.
| Characteristics | Top Decile | Bottom Decile | p-valuea | ||||
|---|---|---|---|---|---|---|---|
| Total | With 24-hour | Without 24-hour | Total | With 24-hour | Without 24-hour | ||
| (n = 9835) | (n = 3052) | (n = 6783) | (n = 7751) | (n = 241) | (n = 7510) | ||
| Age (mean ± SD) | 60.6 ± 13.5 | 58.6 ± 12 | 61.5 ± 14.1 | 60.3 ± 13.6 | 55.5 ± 13.1 | 60.4 ± 13.6 | 0.79 |
| Sex (n,%) | |||||||
| Male | 9268 (94.2) | 2853 (93.5) | 6415 (94.6) | 7329 (94.6) | 217 (90) | 7112 (94.7) | 0.36 |
| Female | 567 (5.8) | 199 (6.5) | 368 (5.4) | 422 (5.4) | 24 (10) | 398 (5.3) | |
| Race (n,%) | |||||||
| White | 7437 (75.6) | 2395 (78.5) | 5042 (74.3) | 5415 (69.9) | 178 (73.9) | 5237 (69.7) | <0.001 |
| Black | 796 (8.1) | 188 (6.2) | 608 (9) | 934 (12.1) | 28 (11.6) | 906 (12.1) | |
| Other/Unknown | 1601 (16.3) | 469 (15.4) | 1133 (16.7) | 1402 (18) | 35 (14.5) | 1367 (18.2) | |
| Stone Diagnosis (n,%) | |||||||
| Inpatient | 1067 (10.8) | 242 (7.9) | 825 (12.2) | 844 (10.9) | 18 (7.5) | 826 (11) | <0.001 |
| Outpatient | 6740 (68.5) | 2309 (75.7) | 4431 (65.3) | 5114 (66) | 181 (75.1) | 4933 (65.7) | |
| Procedure | 2028 (20.6) | 501(16.4) | 1527 (22.5) | 1793 (23.1) | 42 (17.4) | 1751 (23.3) | |
| Number of procedures (mean ± SD) | 0.8 ± 1.4 | 1.2 ± 1.7 | 0.6 ± 1.2 | 0.7 ± 1.3 | 1.5 ± 2.1 | 0.7 ± 1.2 | <0.001 |
| Charlson Comorbidity Index (mean ± SD) | 2.3 ± 2.5 | 1.9 ± 2.1 | 2.4 ± 2.6 | 2.3 ± 2.5 | 1.9 ± 2.2 | 2.3 ± 2.6 | 0.13 |
| Region (n,%) | |||||||
| Midwest | 1219 (12.4) | 292 (9.6) | 927 (13.7) | 1270 (16.4) | 31 (12.9) | 1239 (16.5) | <0.001 |
| Northeast | 1285 (13.1) | 363 (11.89) | 922 (13.6) | 1405 (18.1) | 54 (22.4) | 1351(18) | |
| Southeast | 2870 (29.2) | 969 (31.8) | 1901 (28) | 3560 (45.9) | 108 (44.8) | 3452(46) | |
| West | 4461 (45.4) | 1428 (46.8) | 3033 (44.7) | 1516 (19.6) | 48 (19.9) | 1468 (19.6) |
ap-value compares characteristics between the total population in the bottom and top decile of facilities
Discussion
In this study, we found that fewer than one in six patients with USD completed 24-hour urine testing despite guidelines recommending its use for secondary prevention. The low prevalence of 24-hour urine testing in stone formers demonstrates that clinicians are not routinely incorporating this diagnostic tool and may be falling short of adopting targeted approaches to stone prevention. We identified patient-specific and facility-level factors associated with 24-hour urine testing to determine whether one set of factors dominated. Stone formers who completed a 24-hour urine collection were more likely to do so through an outpatient encounter and were healthier, with lower rates of cardiovascular disease, dementia, and cancer, suggesting that patients who are burdened by co-morbid illness are less likely to collect a 24-hour urine sample. Stone formers were also more likely to complete a 24-hour urine test if they had more than one stone procedure or if they had completed a 24-hour urine test prior to the observation period. These findings suggest that clinicians select patients for 24-hour urine testing who have an increased risk of stone recurrence; moreover, once patients are placed on a “metabolic care pathway” guided by 24-hour urine testing, they are more likely to undergo future testing.
We also found striking facility-level variation in 24-hour urine testing. Among the 150 VHA facilities delivering care to Veterans, the unadjusted proportion of stone formers receiving 24-hour urine testing ranged between 1 and 40%. This wide variation in 24-hour urine testing in stone formers across VHA facilities cannot be explained solely by differences in patient-level characteristics. For example, the average number of stone procedures performed for each stone former in the top and bottom decile of VHA facilities ordering 24-hour urine collections was nearly equal, indicating that stone formers in the top decile are not different from those in the bottom decile with respect to their need for USD procedures. Notably, even the top decile of VHA facilities ordering 24-hour urine collections do so at a rate that falls under 40% of patients with USD, highlighting a divide between recommended and real-world practice of incorporating 24-hour urine testing as a strategy for USD prevention.
To date, few studies have examined the role of 24-hour urine testing in secondary prevention of USD [4–7]. Milose et al. estimated the frequency of 24-hour urine testing to be between 7 and 7.9% in high risk stone formers [7]. Alruwaily et al. used Litholink Corporation data to assess follow-up 24-hour urine testing (i.e., a second 24-hour urine collection) and found the mean rate to be between 11 and 12% [4]. Our study examined a large national cohort of stone formers with varying stone risk profiles and found similarly low rates of testing. It is important to emphasize that our study may have included low risk or first time stone formers in our analytic cohort, which opens up the possibility that 24-hour urine testing may not have been indicated in some stone formers. Future studies are necessary to determine the reasons underlying the low observed rates and regional differences in 24-hour urine testing in stone formers.
Prior studies examining the relationship between 24-hour urine testing and specialty stone care have shown conflicting results. On the one hand, Milose et al. showed that the odds of receiving a 24-hour urine collection increases 2.9-fold when a stone former is seen by a nephrologist and increases more than 3-fold when a stone former is seen by a urologist [7]. On the other hand, Dauw et al. showed that the odds of receiving a repeat 24-hour urine collection decreases 0.76-fold when a stone former is seen by a urologist but increases 1.32-fold when a stone former is seen by a nephrologist [5]. In our study, we found that while 64% of stone formers visited a urologist or nephrologist, only 18.7% of these stone formers completed a 24-hour urine collection, suggesting that the low prevalence of 24-hour urine testing is more likely a function of individual provider preference or regional/facility-level differences rather than access to specialty stone care. These findings highlight the need for stone specialists, who typically care for high risk stone formers, to incorporate 24-hour urine testing in secondary prevention of USD.
This study has several strengths. First, the VHA is a relevant population for the study of USD. Veteran patients tend to be older than civilian patients and have higher rates of co-morbid illnesses that place them at particular risk for USD [8]. Second, we incorporated data from an integrated health system with both inpatient and outpatient claims. The patient sample was large and diverse in terms of age, race, geography and the presence or absence of multiple comorbid conditions. Third, the VHA may be an ideal setting for evaluating determinants of 24-hour urine testing because clinicians in the VHA do not require prior authorization from insurance companies to order 24-hour urine collections, which could reduce detection bias that may be present in civilian health care systems.
This study also has several limitations. First, our study population was comprised of Veterans, the majority of whom are men, which limits generalizability to women or persons unaffiliated with military service. Second, we defined a 24-hour urine collection to be a 24-hour urine measurement of calcium, oxalate, citrate, or sulfate, which is a subset of the measurements found in a typical 24-hour urine test. We included calcium which we believed to be a highly sensitive parameter as well as oxalate, citrate and sulfate which we believed to be a highly specific parameter to diminish false positives and negatives. We also limited our analysis to examining the rate of patients completing a 24-hour urine test rather than the rate of clinicians ordering a 24-hour urine test. It is possible that a discrepancy between these two rates exists in the VHA and could indicate patient or facility factors that impede successful completion of 24-hour urine testing. Currently the CDW dataset does not organize order names for 24-hour urine tests in a standardized format as it does for completed 24-hour tests, which are each associated with a specific set of LOINC codes. A lack of standardization in order names for 24-hour urine tests makes it difficult to know if order names used to query the CDW dataset will encompass all order names that are used for 24-hour urine tests across the 150 VHA facilities. Future studies are thus needed to estimate the rate of 24-hour urine test ordering in the VHA (or elsewhere) and to determine if this rate differs from the rate of 24-hour urine test completion. Third, we used ICD-9 codes to identify urinary stone disease diagnoses, which opens the possibility that a diagnosis could be either over-coded (e.g., emergency room visit for abdominal pain may be coded as a kidney stone) or under-coded (e.g. outpatient visit for multiple comorbid illnesses may not include a kidney stone code). Fourth, we could not specifically exclude stone formers for whom 24-hour urine testing was not indicated (e.g. un-interested first time or low risk stone formers). Fifth, it is possible that we may not have captured data from all VHA facilities that send 24-hour urine samples to an outside laboratory for processing. To address this concern, we queried 24-hour urine data from our local VHA facility, which sends out 24-hour urine samples to an outside laboratory for measurement of urine calcium, oxalate, citrate, and sulfate. We confirmed that these 24-hour urine test results were recorded in the VHA, but we acknowledge that we do not know if this would be the case for all VHA facilities. Finally, we did not capture medical care for stone formers who receive care outside the VHA.
Conclusions
In conclusion, the 24-hour urine collection is acknowledged to be a valuable diagnostic tool for clinicians aiming to identify and treat metabolic risk in stone formers, yet fewer than one in six patients with USD undergo testing. This low testing frequency does not appear to be due to lack of access to specialty care because the majority of stone formers visited either a urologist or nephrologist after a stone diagnosis. Moreover, 24-hour urine testing in stone formers varied widely by geographic region and VHA facility. These regional and facility-level differences in utilization of 24-hr urine testing appear to reflect fixed practice-patterns with respect to how clinicians approach USD prevention. Future efforts to increase utilization of 24-hour urine testing and improve clinician awareness of targeted approaches to stone prevention may be warranted to reduce the morbidity and cost of USD.
Data Availability
Data were sourced from the VA Corporate Data Warehouse, a third party database that houses electronic medical records of US VA patients. To maximize security of Veterans’ data, the US Department of Veterans Affairs (VA) developed the VA Informatics and Computing Infrastructure (VINCI). VA researchers must log onto VINCI via a secure gateway or virtual private network connection (VPN) to access and analyze VA data. By VA Office of Research and Development policy, VINCI does not allow the transfer of patient-level data out of its secure environment without special permission. All analyses performed for this study took place on the VINCI platform. For questions about data access, contact VINCI at: George E. Wahlen VA Medical Center, 500 Foothill Drive, Salt Lake City, Utah 84148, Email: VINCI@va.gov.
Funding Statement
This work received funding through the ASN Ben J. Lipps Research Fellowship Award and the NIH T32 Ruth L. Kirschstein Institutional National Research Service Award DK 7357-34 to CG. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Pearle MS, Goldfarb DS, Assimos DG, Curhan G, Denu-Ciocca CJ, Matlaga BR, et al. Medical management of kidney stones: AUA guideline. The Journal of urology. 2014;192(2):316–24. 10.1016/j.juro.2014.05.006 [DOI] [PubMed] [Google Scholar]
- 2.Hsi RS, Sanford T, Goldfarb DS, Stoller ML. The Role of the 24-Hour Urine Collection in the Prevention of Kidney Stone Recurrence. The Journal of urology. 2017;197(4):1084–9. 10.1016/j.juro.2016.10.052 [DOI] [PubMed] [Google Scholar]
- 3.Semins MJ, Trock BJ, Matlaga BR. Validity of administrative coding in identifying patients with upper urinary tract calculi. The Journal of urology. 2010;184(1):190–2. 10.1016/j.juro.2010.03.011 [DOI] [PubMed] [Google Scholar]
- 4.Alruwaily AF, Dauw CA, Bierlein MJ, Asplin JR, Ghani KR, Wolf JS Jr., et al. Geographic Variation in the Quality of Secondary Prevention for Nephrolithiasis. Urology. 2015;86(3):454–8. 10.1016/j.urology.2015.05.022 [DOI] [PubMed] [Google Scholar]
- 5.Dauw CA, Alruwaily AF, Bierlein MJ, Asplin JR, Ghani KR, Wolf JS Jr., et al. Provider variation in the quality of metabolic stone management. The Journal of urology. 2015;193(3):885–90. 10.1016/j.juro.2014.09.111 [DOI] [PubMed] [Google Scholar]
- 6.Ghiraldi EM, Reddy M, Li T, Lawler AC, Friedlander JI. Factors Associated with Compliance in Submitting 24-Hour Urine Collections in an Underserved Community. Journal of endourology. 2017;31(S1):S64–S8. 10.1089/end.2016.0594 [DOI] [PubMed] [Google Scholar]
- 7.Milose JC, Kaufman SR, Hollenbeck BK, Wolf JS Jr., Hollingsworth JM. Prevalence of 24-hour urine collection in high risk stone formers. The Journal of urology. 2014;191(2):376–80. 10.1016/j.juro.2013.08.080 [DOI] [PubMed] [Google Scholar]
- 8.Agha Z, Lofgren RP, VanRuiswyk JV, Layde PM. Are patients at Veterans Affairs medical centers sicker? A comparative analysis of health status and medical resource use. Archives of internal medicine. 2000;160(21):3252–7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data were sourced from the VA Corporate Data Warehouse, a third party database that houses electronic medical records of US VA patients. To maximize security of Veterans’ data, the US Department of Veterans Affairs (VA) developed the VA Informatics and Computing Infrastructure (VINCI). VA researchers must log onto VINCI via a secure gateway or virtual private network connection (VPN) to access and analyze VA data. By VA Office of Research and Development policy, VINCI does not allow the transfer of patient-level data out of its secure environment without special permission. All analyses performed for this study took place on the VINCI platform. For questions about data access, contact VINCI at: George E. Wahlen VA Medical Center, 500 Foothill Drive, Salt Lake City, Utah 84148, Email: VINCI@va.gov.