Abstract
Regular physical activity (PA) is of central importance for healthy ageing. However, in Germany, only 42% of older adults currently reach the PA recommendations of the World Health Organization. The aim of this study was to examine the effects of two web-based interventions on PA in adults aged 65–75 years living in Northwestern Germany compared to a delayed intervention control group (CG). 589 older adults were randomized to one of the three groups. Participants in intervention group 1 (IG1) received access to a web-based intervention for ten weeks assisting them in self-tracking PA behavior. Participants in IG2 received the intervention of IG1 and additionally an activity tracker to objectively track PA behavior. To analyze differences in objectively measured moderate-to-vigorous PA and sedentary time between baseline and follow-up (12 weeks after baseline), linear mixed models were used. The interaction effects revealed a decrease in minutes spent on moderate-to-vigorous PA in bouts of 10 min by 11 min per week in IG1 participants (β = −11.08, 95% CI: (−35.03; 12.87)). In comparison, IG2 participants were 7 min more physically active at follow-up (β = 7.48, 95% CI: (−17.64; 32.60)). Sedentary time in bouts of 30 min per week increased in IG1 participants (β = 106.77, 95% CI: (−47.69; 261.23)) and decreased in IG2 participants at follow-up (β = −16.45, 95% CI: (−178.83; 145.94)). Participation in the two web-based interventions did not lead to significant increases in moderate-to-vigorous PA or significant decreases in sedentary time compared to the CG.
The study was registered at the German Clinical Trials Register (DRKS00010052, 07-11-2016).
Keywords: Physical activity, Exercise, Accelerometer, Older adults, eHealth, Intervention, Primary prevention, Healthy ageing
Highlights
-
•
Regular physical activity (PA) is central to healthy ageing.
-
•
In Germany, only 42% of older adults currently meet the WHO-recommended PA levels.
-
•
PROMOTE examined the effectiveness of web-based PA interventions in older adults.
-
•
Two ten week web-based PA interventions were compared to a control group.
-
•
We found no increases in moderate-to-vigorous PA or decreases in sedentary time.
1. Introduction
Regular physical activity (PA) is a key contributor to healthy ageing and associated with improvements in physical, psychological, and cognitive health (Hong et al., 2008; Hupin et al., 2015; Warburton et al., 2006). The World Health Organization (WHO) and the American College of Sports Medicine (ACSM) recommend moderate-to-vigorous endurance training for at least 150 min per week (in bouts of at least 10 min) for adults aged 65 years and above. In addition, adults aged ≥65 years should perform flexibility, strength, and balance training two times per week (World Health Organization, 2010; Nelson et al., 2007). In Germany, 42% of adults aged 65 years and above meet the recommendations for endurance and 26% for strength training (Finger et al., 2017).
PA interventions may help inactive older adults to initiate and maintain regular PA. It is known that interventions providing information on PA face-to-face or as print versions can effectively increase PA levels in older adults (Richards et al., 2013; Noar et al., 2007; Short et al., 2011). Further, in Germany, 44% of adults aged 60 years and above use the internet daily and 74% at least occasionally (Koch and Frees, 2017) suggesting that web- or other technology-based (eHealth) interventions may be of interest to this population.
Three systematic reviews examined the effectiveness of eHealth interventions for PA promotion in healthy older adults and found that they can effectively promote PA (Müller and Khoo, 2014; Muellmann et al., 2018; Jonkman et al., 2018). Focusing only on web-based interventions, Muellmann and colleagues (Muellmann et al., 2018) found that participation in these interventions led to increased PA levels (e.g., daily steps, daily moderate-to-vigorous PA (MVPA)) compared to controls in the short-term (<12 months). However, only two of the included web-based interventions used an objective method for assessing PA at baseline and follow-up (i.e., pedometer, accelerometer) (Bickmore et al., 2013; Wijsman et al., 2013). Wijsman and colleagues (Wijsman et al., 2013) compared a web-based intervention to a control group (CG) and found a significant increase in daily PA after two months. Bickmore and colleagues (Bickmore et al., 2013) compared a web-based intervention to a non-eHealth intervention (i.e., pedometer) and reported significant increases in steps after two, but not 12 months. In sum, only few studies used objective methods to examine the effectiveness of web-based PA interventions in older adults compared to a non-eHealth intervention group or CG; and none of these studies were conducted in Germany. In addition, previous evidence suggests that a web-based intervention with subjective PA monitoring (i.e., self-report) in combination with an objective PA monitoring via pedometer was effective in increasing objectively measured PA in adults in one study (Compernolle et al., 2015) and even more effective compared to the single-component intervention in another study (Vandelanotte et al., 2018). However, the effects of subjective PA monitoring (i.e., via a web-based PA diary) compared to a combination of subjective and objective PA monitoring (i.e., via web-based diary and PA tracking device) have not been systematically examined in older German adults.
Therefore, the main aim of this community-based controlled intervention trial (PROMOTE study) was to evaluate the effectiveness of two different web-based interventions, one including subjective PA monitoring and the other a combination of subjective and objective PA monitoring, for the initiation and maintenance of regular PA among older adults aged 65 to 75 years living in five communities in Northwestern Germany compared to a delayed intervention CG. We hypothesized that 1) both interventions would lead to increased PA compared to a CG, 2) the web-based intervention including both subjective and objective PA monitoring would be more effective for increasing PA than the web-based intervention with subjective PA monitoring only.
This study was embedded in the larger Physical activity and Health Equity: Primary Prevention for Healthy Ageing (AEQUIPA) research network (Forberger et al., 2017). The methods for the study have been described in detail elsewhere (Muellmann et al., 2017) and will only be briefly described in the following section. The CONSORT checklist for randomized controlled trials is provided in supplementary file 1.
2. Methods
2.1. Participants and procedures
2.1.1. Recruitment
Five communities in Northwestern Germany were selected for the implementation of the intervention. A random sample of persons between the ages of 65 and 75 years was drawn from the records of the residents' registration offices of these communities. In addition, the intervention was publicized in local newspaper articles, as well as during events of senior citizen organizations and sports clubs.
2.1.2. Inclusion and exclusion criteria
Eligibility for study participation was determined in subsequent telephone interviews with trained study nurses. Inclusion criteria were a) residence in one of the five selected communities, b) age between 65 and 75 years, c) basic knowledge of German, d) living independently, e) ability to walk without a walking aid, f) ability to participate in study assessments and weekly group meetings without external support, and g) internet access at home or at family members' or friends' houses. Participants were excluded if they have planned a vacation for more than one month during the intervention period, displayed cognitive impairment or other permanent medical impairments (e.g., stroke) or if there were any medical contraindications to program participation.
During the study, the age range was loosened to the ages 60 to 80 years because some of the potential participants were only willing to participate together with their spouse or partner who did not fulfil the inclusion criteria regarding age. However, during active recruitment via invitation letters, at events of senior citizen organizations or sport clubs, or in local newspaper articles, we applied the original inclusion criteria. Another modification was that we had initially intended to exclude persons who had some form of cognitive impairment meaning that they had a Mini-Mental-Score < 27. During the study, we realized that a lot more persons than expected had to be excluded due to this very conservative cut-off. Supported by results of a systematic review by Creavin and colleagues (Creavin et al., 2016) suggesting acceptable diagnostic accuracy when using the slightly less conservative cut-off of 25, we decided only to exclude persons if they had a Mini-Mental-Score < 25.
2.1.3. Randomization and procedures
After successful screening for study eligibility, study participants were assigned to one of three study arms by the study nurses: a) a web-based intervention with subjective PA self-monitoring (intervention group 1 (IG1)), b) a web-based intervention with subjective and objective PA monitoring (intervention group 2 (IG2)) or c) a delayed intervention CG. Each IG was randomly assigned to certain weeks of baseline assessment. Participants were free to choose from available time slots during the telephone interview with the study nurse but were only informed after their decision which IG they were assigned to during a particular week. Participants were invited to the study center for baseline and follow-up (12 weeks after baseline) assessments. At the study center, participants completed different anthropometric, physical, motor, and cognitive tests. After both assessments, participants received an accelerometer (GT3X+, ActiGraph, Pensacola, USA) to objectively measure PA and a self-administered questionnaire. One week after the baseline assessment, participants of IG1 and IG2 received separate introductions to the ten-week intervention during the first group meeting.
2.2. Interventions
The two web-based interventions were developed based on self-regulation theory (Fleig et al., 2011; Pomp et al., 2013) and principles of behavior change (e.g., shaping knowledge, feedback and monitoring, goals and planning, social support, comparison of behavior, rewards) (Michie et al., 2013). According to the PA recommendations of the WHO and ACSM, participants in IG1 and IG2 were instructed to engage in exercises to improve balance (two times per week), flexibility (two times per week), strength (on two or more nonconsecutive days per week involving major muscle groups), and endurance (for at least 150 min with moderate-to-vigorous intensity per week in bouts of 10 min). Depending on the individual baseline PA levels of participants and gender, participants received different printed brochures outlining exercises for different difficulty levels displayed by male vs. female older adults modeling the exercises. The brochures also included information about local PA offers in the respective community.
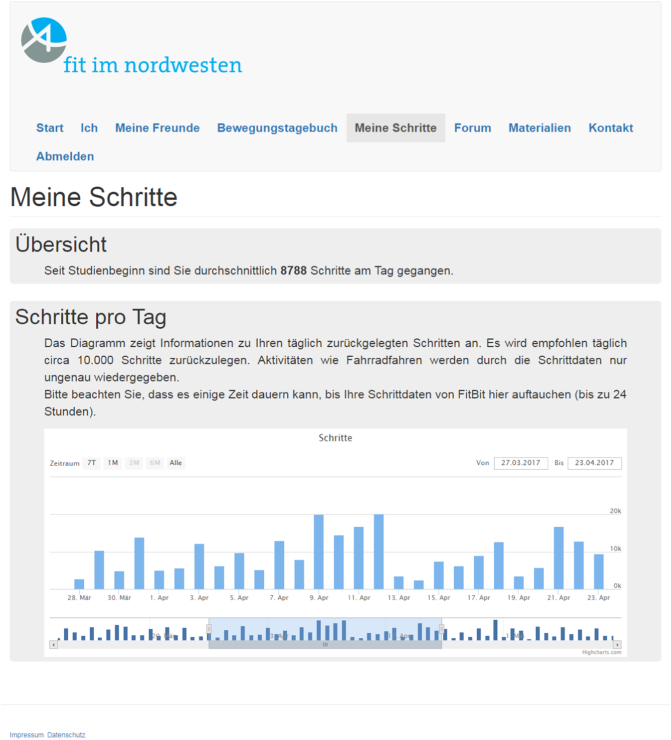
Participants in IG1 received access to a web-based PA diary to track their PA behavior over the ten-week intervention period (Fig. 1). Participants in IG2 additionally received a Fitbit Zip (Fitbit, San Francisco, USA) to objectively track PA; data of the Fitbit were synchronized with the website (Fig. 2). The website provided weekly feedback on whether PA goals (WHO and ACSM recommendations for moderate-to-vigorous endurance, balance, flexibility, and strength training) were reached. Moreover, participants received goal-specific rewards (digital cups) and the opportunity to network with other intervention participants via an invite friend's function and an online forum. In addition to the website, participants in IG1 and IG2 were offered weekly group meetings in their communities led by trained research assistants. During these 90-minute meetings, participants could resolve technical problems with the website and the Fitbit Zips, received health education regarding the role of PA for healthy ageing, discussed different factors which may enhance PA promotion (e.g., social support, the use of action planning, and strategies for PA maintenance), and practiced PA in groups (e.g., community walks). Participants assigned to the CG received no intervention during the ten-week intervention period but were offered participation in the web-based intervention of IG1 without weekly group meetings after follow-up.
Fig. 1.

Web-based PA diary for subjective self-monitoring of weekly PA behavior.
Fig. 2.
Synchronization of Fitbit and website for participants in intervention group 2.
2.3. Outcome measures
2.3.1. Physical activity and sedentary time
After baseline and follow-up assessments (12 weeks after baseline), all participants received an accelerometer (GT3X+, ActiGraph, Pensacola, USA) to objectively measure PA for one week. Participants were instructed to wear the accelerometer on the right hip and during the day for the following seven days. Accelerometer data were processed using the Actilife 6.8.0 software to identify non-wear times and classify PA levels into the categories described below. Valid wear-time was derived using the wear- and non-wear time classification algorithm by Choi and colleagues (Choi et al., 2011) and valid days were defined as having at least 8 h (480 min) of valid wear-time. Using 1 s epochs, counts were categorized into sedentary time (0–99 counts per minute (CPM)), according to Freedson and colleagues (Freedson et al., 1998) based on one axis, and light (0–2690 CPM), moderate (2691–6166 CPM), vigorous (6167–9642 CPM), moderate-to-vigorous (2691–9642 CPM), and very vigorous (>9642 CPM) PA, according to Sasaki and colleagues (Sasaki et al., 2011) considering the vector magnitude. Daily minutes for each category were averaged to derive PA levels at baseline and follow-up, if at least three valid days, including one weekend day, were available for each participant. In addition, sedentary time per week was calculated in bouts of at least 30 min and time spent in MVPA per week was calculated in bouts of at least 10 min. Further, total time of MVPA per week in bouts of 10 min was dichotomized into meeting the WHO recommendation (≥ 150 min/week MVPA in bouts of at least 10 min) or not. The season during accelerometer measurement was derived from the date of examination and categorized into autumn/winter for the months October to February and spring/summer for the months of March to September.
2.3.2. Demographic and baseline variables
Demographic information was collected using questionnaires at baseline. Country of birth, family status, and household income were assessed using items of the German Health Interview and Examination Survey for Adults (Robert-Koch-Institut, 2009). The variable need-weighted household income per capita was derived from the number of individuals living in the household and the monthly household income according to the German Microcensus (Boehle, 2015). The variable was then tertiled into low, middle, and high household income. Level of education was coded following the 2011 version of the International Standard of Education (ISCED). Persons with a higher educational status received a higher score (range 1–8) (Statistisches Bundesamt, 2016). Because only few participants had a low level of education (n = 8), the variable was dichotomized into low/medium level of education (ISCED-Score 1–4) and high level of education (ISCED-Score 5–8). Employment status was assessed using one item from a questionnaire for assessing seniors' demographic and socio-structural data in Germany (Berthelsmann Stiftung, 2018). Subjective health status was assessed using one item of the Short-Form (SF)-12 for health-related quality of life (Bullinger and Kirchberger, 1998). In addition, body mass index (BMI) was calculated based on the assessment of height (using stadiometers) and weight (using bioimpedance scales).
2.3.3. User satisfaction
Information on acceptance of the website and attendance of the weekly group meetings in the communities was collected from participants of both intervention conditions at follow-up, using a questionnaire with self-generated items.
2.4. Statistical analyses
Participants who provided none or invalid accelerometer measurements were excluded from the analyses (n = 20). In addition, participants with missing information on age (n = 6), gender (n = 16), BMI (n = 1), or with a Mini-Mental-Score < 25 (n = 17) were excluded from the analyses.
Descriptive statistics (i.e., mean and standard deviation (SD) or percentages for categories) were calculated for baseline and follow-up data. Differences in PA outcome variables (i.e., minutes of MVPA/day, minutes of MVPA/week in 10 min bouts, sedentary time/day, sedentary time/week in 30 min bouts), between baseline and follow-up, depending on the type of intervention, were analyzed using linear mixed models. Models were built for each outcome separately. We modeled fixed effects for IG (reference: CG) and assessment period (reference: baseline) to investigate overall group and time effects, as well as an interaction of group and assessment period to identify the intervention effect. Due to the flexibility of mixed models, data of participants with baseline but without follow-up data were used and repeated measurements were accounted for by means of a random effect. In order to assess differences in the intervention effect between IG1 and IG2, we estimated least-square means of the time difference in each outcome for both IGs which were then compared using an F-test. All models were adjusted for age, gender, BMI, level of education, family status, employment status, household income, subjective health status, community, season, WHO MVPA recommendation achieved at baseline, and valid wear-time. To explore whether participation in the interventions yielded different effects in subgroups (e.g., male vs. female participants), all models were stratified by gender, age, level of education, and whether the WHO MVPA recommendation was met (or not) at baseline.
Participants who did not complete the follow-up assessment were slightly more likely to still be employed, to have low or medium levels of education, and a low household income. By adjusting for these relevant covariates, mixed models were conducted under the assumption of missing at random.
Statistical analyses were conducted using SAS 9.3 (SAS Institute Inc., Cary, North Carolina, USA), the GLIMMIX procedure was used, in particular, to estimate linear mixed models.
3. Results
3.1. Participants
A total of 8474 adults were eligible for study participation (Fig. 3). In total, 7885 potential participants were excluded. Subsequently, 589 participants were randomized to one of the three study arms (IG1: n = 211, IG2: n = 198, CG: n = 180). Of these participants, 405 participants completed follow-up assessment (IG1: n = 146, IG2: n = 119, CG: n = 140). Attrition rates from baseline to follow-up were 22% in the CG, 31% in IG1, and 40% in IG2.
Fig. 3.
Participant flow.
Participants' demographic characteristics at baseline are displayed in Table 1. Overall, mean age was 69.7 years (SD = 3.3, range 62 to 79 years) and mean BMI was 27.7 (SD = 4.4). 299 (57%) participants were female, 500 (95%) were born in Germany, 245 (46%) had a high level of education, 380 (72%) were married, and 303 (57%) reported good health. There were no substantial differences in sociodemographic variables between study groups at baseline, except for country of birth (see Table 1 country of birth other than Germany: IG1 8%, IG2 1%, CG 7%).
Table 1.
Demographic characteristics of study sample at baseline.
| Characteristics | IG1 (n = 195) | IG2 (n = 172) | CG (n = 162) | Total (n = 529) |
|---|---|---|---|---|
| Age in years, mean (SD) | 69.6 (3.4) | 69.6 (3.2) | 69.8 (3.2) | 69.7 (3.3) |
| Gender, n (%) | ||||
| Male | 90 (46.2) | 71 (41.3) | 69 (42.6) | 230 (43.5) |
| Female | 105 (53.8) | 101 (58.7) | 93 (57.4) | 299 (56.5) |
| BMI, mean (SD) | 27.7 (4.3) | 27.2 (4.2) | 28.2 (4.6) | 27.4 (4.4) |
| Country of birth, n (%) | ||||
| Germany | 180 (92.3) | 170 (98.8) | 150 (92.6) | 500 (94.5) |
| Other than Germany | 15 (7.7) | 2 (1.2) | 12 (7.4) | 29 (5.5) |
| Community, n (%) | ||||
| Burglesum | 41 (21.0) | 13 (7.6) | 25 (15.4) | 79 (14.9) |
| Vahr | 18 (9.2) | 29 (16.9) | 24 (14.8) | 71 (13.4) |
| Obervieland | 55 (28.2) | 54 (31.4) | 42 (25.9) | 151 (28.5) |
| Osterholz-Scharmbeck | 63 (32.3) | 36 (20.9) | 36 (22.2) | 135 (25.5) |
| Achim | 18 (9.2) | 40 (23.3) | 35 (21.6) | 93 (17.6) |
| Season, n (%) | ||||
| Fall/Winter | 57 (29.2) | 42 (24.4) | 35 (21.6) | 134 (25.3) |
| Spring/Summer | 138 (70.8) | 130 (75.6) | 127 (78.4) | 395 (74.7) |
| Level of education, n (%) | ||||
| Low | 1 (0.5) | 1 (0.6) | 6 (3.7) | 8 (1.5) |
| Medium | 89 (45.6) | 90 (52.3) | 90 (55.6) | 269 (50.9) |
| High | 101 (51.8) | 79 (45.9) | 65 (40.1) | 245 (46.3) |
| Missing | 4 (2.1) | 2 (1.2) | 1 (0.6) | 7 (1.3) |
| Family status, n (%) | ||||
| Married | 140 (71.8) | 128 (74.4) | 112 (69.2) | 380 (71.8) |
| Married, not living with partner, or divorced or single or widowed | 51 (26.2) | 42 (24.4) | 49 (30.2) | 142 (26.8) |
| Missing | 4 (2.1) | 2 (1.2) | 1 (0.6) | 7 (1.3) |
| Employment status, n (%) | ||||
| Employed or retired and employed | 26 (13.3) | 22 (12.8) | 27 (16.7) | 75 (14.2) |
| Retired or other | 167 (85.6) | 147 (85.5) | 134 (82.7) | 448 (84.7) |
| Missing | 2 (1.0) | 3 (1.7) | 1 (0.6) | 6 (1.1) |
| Household income, n (%) | ||||
| Low | 50 (25.6) | 45 (26.2) | 55 (34.0) | 150 (28.4) |
| Middle | 62 (31.8) | 49 (28.5) | 42 (25.9) | 153 (28.9) |
| High | 68 (34.9) | 61 (35.5) | 57 (35.2) | 186 (35.2) |
| Missing | 15 (7.7) | 17 (9.9) | 8 (4.9) | 40 (7.6) |
| Subjective health status, n (%) | ||||
| Excellent or very good | 47 (24.1) | 50 (29.1) | 37 (22.8) | 134 (25.4) |
| Good | 114 (58.5) | 96 (55.8) | 93 (57.4) | 303 (57.3) |
| Less good or poor | 30 (15.4) | 23 (13.4) | 27 (16.7) | 80 (15.1) |
| Missing | 4 (2.1) | 3 (1.7) | 5 (3.1) | 12 (2.3) |
| WHO MVPA recommendation, n (%) | ||||
| Not achieved | 147 (75.4) | 128 (74.4) | 137 (84.6) | 412 (77.9) |
| Achieved | 48 (24.6) | 44 (25.6) | 25 (15.4) | 117 (22.1) |
| Wear-time (min/day), mean (SD) | 859.1 (95.0) | 863.5 (94.5) | 843.1 (77.4) | 855.6 (90.1) |
BMI: Body Mass Index; CG: Control group; IG: Intervention group; MVPA: Moderate-to-vigorous physical activity; SD: Standard deviation; WHO: World Health Organization.
3.2. Physical activity and sedentary time
At baseline and follow-up, participants were about 90 min moderately to vigorously physically active per day (Table 2). Minutes in MVPA per day decreased in IG1 participants at follow-up by 4 min compared to baseline and CG participants (β = −3.54, 95% Confidence Interval (CI): (−9.38; 2.29)). IG2 participants were approximately 2 min more physically active in MVPA per day at follow-up compared to baseline and CG participants (β = 1.73, 95% CI: (−4.40; 7.86)). Similar results were observed for total time in MVPA per week of 10min bouts for IG1 and IG2 participants (IG1: β = −11.08, 95% CI: (−35.03; 12.87); IG2: β = 7.48, 95% CI: (−17.64; 32.60)). Participants' baseline sedentary time was 720 min per day. There was no significant change in sedentary time per day in IG1 and IG2 participants at follow-up compared to baseline and CG participants (IG1: β = 6.27, 95% CI: (−1.32; 13.87); IG2: β = 0.32, 95% CI: (−7.67; 8.30)). Weekly sedentary time in bouts of 30 min increased in IG1 (β = 106.77, 95% CI: (−47.69; 261.23)) and decreased in IG2 participants at follow-up compared to baseline and CG participants (β = −16.45, 95% CI: (−178.83; 145.94)). In addition, differences in MVPA and sedentary time between IG2 and IG1 were observed favoring IG2. However, these results were only significant for weekly MVPA in 10minbouts (F = 3.31, p = 0.04). In depth analyses (see supplementary file 2) indicated that MVPA increased at follow-up in participants who were male, aged <70 years, had a high level of education, and reached the WHO recommendations for MVPA at baseline (not significant). For sedentary time, more mixed results were observed.
Table 2.
Results of the linear mixed regression models (time, group, intervention effects, and comparison of intervention effects in IG1 and IG2) for MVPA and sedentary time.
| Characteristics |
Assessment period mean (SD) |
Time difference β (95% CI) |
Group difference β (95% CI) |
Group-by-time interaction β (95% CI) |
Estimated difference in time for IGs Mean (95% CI) |
|
|---|---|---|---|---|---|---|
| Baseline | Follow-Up | Ref.: Baseline | Ref.: CG | Ref.: CG*Baseline | T1-T0 | |
| MVPAa (min/day)b | ||||||
| IG1 | 87.8 (33.1) | 86.7 (31.6) | 1.50 (−2.60; 5.60) | −2.06 (−8.06; 3.94) | −3.54 (−9.38; 2.29) | −2.04 (−6.31; 2.22) |
| IG2 | 89.2 (31.4) | 95.3 (33.8) | −1.33 (−7.43; 4.76) | 1.73 (−4.40; 7.86) | 3.23 (−1.40; 7.87) | |
| CG | 85.4 (34.1) | 88.5 (33.3) | F = 1.54, p = 0.22 | |||
| MVPAa in 10 min bouts (min/week)c | ||||||
| IG1 | 107.7 (132.8) | 83.6 (98.1) | −11.24 (−28.37; 5.89) | 2.63 (−14.56; 19.82) | −11.08 (−35.03; 12.87) | −22.32 (−39.41; −5.23) |
| IG2 | 103.8 (113.1) | 108.2 (107.0) | −1.40 (−18.88; 16.08) | 7.48 (−17.64; 32.60) | −3.76 (−22.38; 14.86) | |
| CG | 80.5 (112.0) | 83.1 (106.7) | F = 3.31, p = 0.04 | |||
| Sedentary timed (min/day)b | ||||||
| IG1 | 722.3 (93.5) | 693.8 (76.3) | −5.22 (−10.56; −0.12) | 4.31 (−3.52; 12.14) | 6.27 (−1.32; 13.87) | 1.05 (−4.50; 6.61) |
| IG2 | 723.9 (89.5) | 697.7 (104.1) | 3.82 (−4.13; 11.78) | 0.32 (−7.67; 8.30) | −4.90 (−10.94; 1.13) | |
| CG | 705.6 (75.3) | 703.1 (82.8) | F = 1.42, p = 0.24 | |||
| Sedentary timed in 30 min bouts (min/week)c | ||||||
| IG1 | 2384 (1175) | 1899 (839.5) | −63.83 (−172.38; 44.72) | −3.45 (−160.66; 153.75) | 106.77 (−47.69; 261.23) | 42.94 (−69.86; 155.75) |
| IG2 | 2410 (965.9) | 2047 (860.6) | 138.54 (−13.51; 306.19) | −16.45 (−178.83; 145.94) | −80.28 (−202.94; 42.38) | |
| CG | 2178 (932.8) | 2094 (890.0) | F = 1.22, p = 0.30 | |||
CI: Confidence Interval; CG: Control group; IG: Intervention group; MVPA: Moderate-to-vigorous physical activity; SD: Standard deviation; T1: Follow-Up; T0: Baseline.
Based on vector magnitude.
Adjusted for age, gender, BMI, level of education, family status, employment status, household income, subjective health status, community, season, WHO MVPA recommendation at baseline, and valid wear-time.
Adjusted for age, gender, BMI, level of education, family status, employment status, household income, subjective health status, community, season, WHO MVPA recommendation at baseline, valid wear-time, and calendar days.
Based on one axis.
3.3. User satisfaction
229 intervention participants (IG1: n = 127, IG2: n = 102) filled out the questionnaire assessing user satisfaction at follow-up. The intervention components of the website which were most commonly used by participants were the PA diary (n = 183, 80%) and the Fitbit step diagram (n = 87, 85%, only IG2 participants). The friend's function was not used by the majority of the participants (n = 167, 73%), as well as the online forum (n = 127, 56%). 160 (70%) participants used the PA diary daily or at least once every week and 156 (68%) found it (very) helpful to receive the PA recommendations. 71% (n = 163) of the participants attended the weekly group meetings in the communities (mean number of weekly group meetings attended 5.5, SD = 1.9). The majority of participants rated the group exercises during these weekly group meetings as (very) helpful for reaching PA recommendations (e.g., balance training was rated as (very) helpful by 127 (56%) participants). In contrast, only very few participants rated the health education delivered during these meetings as (very) helpful for reaching their PA goals (e.g., information on the role of social support in PA promotion was rated as (very) helpful by only 19% (n = 44) of participants).
4. Discussion
4.1. Principal findings
The aim of this community-based intervention trial was to examine the effectiveness of two different web-based interventions promoting PA in older adults compared to a CG. Intervention participants were instructed to track PA subjectively (IG1) or subjectively and objectively (IG2) over ten weeks. None of the investigated interventions led to significant increases in MVPA or decreases in sedentary time at follow-up compared to the CG. In addition, significant differences between IG1 and IG2 favoring IG2 were observed for MVPA but not for sedentary time.
4.2. Comparison to prior work
Our results are contrary to results of similar studies previously conducted. For example, results of a systematic review suggested that participation in web-based interventions led to increased PA in older adults at least over the short-term (<12 months) (Muellmann et al., 2018). However, the majority of the studies included in this review assessed PA subjectively (e.g., (Irvine et al., 2013; Mouton and Cloes, 2015; Peels et al., 2013)). Subjective assessment of PA often leads to an overestimation of actual PA behavior and studies which use a subjective PA assessment have a higher risk of bias than studies using an objective PA assessment (Prince et al., 2008; Kowalski et al., 2012). Another review aimed to give an overview of eHealth interventions focusing on PA promotion in community-dwelling older adults and used objective methods to assess PA at baseline and follow-up (Jonkman et al., 2018). Based on their findings, Jonkman and colleagues concluded that eHealth interventions offering objective methods to track PA yielded positive effects in older adults in the short-term (Jonkman et al., 2018). However, only three studies included in the review provided information on MVPA assessed by accelerometry (Wijsman et al., 2013; Lewis et al., 2017; Cadmus-Bertram et al., 2015) and none of the included studies provided information on sedentary time. Participants in the IGs increased MVPA by 11 min per day (Wijsman et al., 2013; Lewis et al., 2017) and 38 min per week in bouts of 10 min (Cadmus-Bertram et al., 2015). Compared to our study, intervention participants in the previous studies increased MVPA to a greater extent; however this effect was only statistically significant for the study by Wijsman and colleagues (Wijsman et al., 2013).
Participants in our study already engaged in approximately 90 min of MVPA per day at baseline suggesting that we recruited relatively active persons to our study. In comparison, other studies using objective methods (i.e., accelerometer, pedometer) for PA assessment in older adults reported much lower PA levels (approximately 20 min MVPA) at baseline (Wijsman et al., 2013; Alley et al., 2018; Suboc et al., 2014). This was, in part, due to stricter exclusion criteria meaning that persons with high levels of weekly PA were excluded from these studies (Wijsman et al., 2013; Alley et al., 2018).
A comparison of PA between the two IGs suggests that participants who subjectively and objectively tracked their PA behavior benefited more from the intervention than participants who only subjectively tracked their PA behavior. These findings are similar to findings by Vandelanotte and colleagues who found that a combination of subjective and objective PA monitoring was more effective in increasing MVPA in Australian adults than subjective PA monitoring only (Vandelanotte et al., 2018). Furthermore, the use of a website in combination with an activity tracker in already physically active older adults may support long-term maintenance of PA (Rasche et al., 2016).
4.3. Strengths and limitations
The two main strengths of our study were that PA was objectively measured using accelerometers and that two intervention arms were compared to a CG. However, our study had several limitations. We recruited a sample which was physically active at the onset of the study and with relatively high levels of education, which limited external validity of our findings. In addition, the awareness of participating in a study on PA promotion might explain participant's high baseline PA levels (Hawthorne effect). The intervention and follow-up period was relatively short in our study. Moreover, data collection took place in spring or during the summer where people tend to be more physically active than in autumn or winter. We controlled for seasonal effects in all statistical models but this might also explain the high baseline and follow-up PA levels we observed in this population.
Unfortunately, only 7% of older adults initially contacted participated in the study and 31% of participants were lost to follow-up. We did note a greater drop-out rate in the IGs compared to the CG. This may be because several participants did not feel capable of using the website and/or Fitbit Zips, despite the support of the intervention team suggesting that these intervention components were not easy enough to use for certain participants. There is evidence suggesting that older adults are highly motivated to use activity trackers for monitoring PA but that they have a higher demand for support during usage (Sullivan and Lachman, 2016). Further, personal preferences of the target group need to be taken into account when using activity trackers in PA intervention studies (Shin et al., 2019). In addition, we are not able to draw any conclusions with regard to the influence of the individual components of our web-based intervention or the added benefit of the face-to-face weekly group meetings. Another limitation was that blinding of participants was not possible. Also, we did not reach the initially calculated sample size (Muellmann et al., 2017), our results are therefore slightly underpowered and have to be interpreted with caution.
5. Conclusion
Participation in the two web-based interventions did not lead to increases in MVPA or decreases in sedentary time. Future studies should exclude initially active persons as they are not the focus of PA promotion. Further, additional research is necessary to investigate whether different modes of delivery or preferences of individual participants influence intervention participation and effects, particularly among different subgroups. Based on findings of this future research, researchers will be able to make more specific recommendations to the target group, intervention developers, and policy makers regarding the use (and further development) of different modalities for PA promotion and the tailoring of intervention content to individual preferences.
Abbreviations
- ACSM
American College of Sports Medicine
- AEQUIPA
Physical Activity and Health Equity: Primary Prevention for Healthy Ageing
- BMI
Body Mass Index
- CG
Control group
- CI
Confidence Interval
- CPM
Counts per minute
- IG
Intervention group
- ISCED
International Standard of Education
- MVPA
Moderate-to-vigorous physical activity
- PA
Physical activity
- SD
Standard Deviation
- SF
Short-Form
- WHO
World Health Organization
Human and animal rights
This study was approved by the Ethics Committee of the Chemnitz University of Technology (TU Chemnitz), Faculty of Behavioral and Social Sciences (number: V-099-17-HS-CVR-PROMOTE-03072015), and was registered at the German Clinical Trials Register (DRKS00010052, Date of registration 07-11-2016). Data collection took place in the federal states of Bremen and Lower Saxony, Germany, from May 2016 to November 2017. All study participants were fully informed about the study and provided informed consent.
Funding
This study was funded by the German Federal Ministry of Education and Research (BMBF; project numbers 01EL1422A, 01EL1422C, 01EL1422E, 01EL1422F, 01EL1522I). The content of this article only reflects the authors' views and the funder is not liable for any use that may be made of the information contained therein.
Declaration of Competing Interest
The authors declare that they have no competing interests.
Acknowledgments
The authors would like to thank Beate Schütte and all student assistants who helped out in recruiting participants and collecting the data. The authors would also like to thank all study participants. The publication of this article was funded by the Open Access Fund of the Leibniz Association.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.pmedr.2019.100958.
Contributor Information
Saskia Muellmann, Email: muellmann@leibniz-bips.de.
Christoph Buck, Email: buck@leibniz-bips.de.
Claudia Voelcker-Rehage, Email: claudia.voelcker-rehage@hsw.tu-chemnitz.de.
Inna Bragina, Email: inna.bragina@gmx.net.
Sonia Lippke, Email: s.lippke@jacobs-university.de.
Jochen Meyer, Email: jochen.meyer@offis.de.
Manuela Peters, Email: mpeters@leibniz-bips.de.
Claudia R. Pischke, Email: ClaudiaRuth.Pischke@med.uni-duesseldorf.de.
Appendix A. Supplementary data
CONSORT checklist.
Intervention effects stratified by gender, age, level of education, and WHO MVPA recommendation at baseline achieved.
References
- Alley S.J., Kolt G.S., Duncan M.J., Caperchione C.M., Savage T.N., Maeder A.J., Rosenkranz R.R., Tague R., Van Itallie A.K., Kerry Mummery W., Vandelanotte C. The effectiveness of a web 2.0 physical activity intervention in older adults - a randomised controlled trial. Int. J. Behav. Nutr. Phys. Act. 2018;15:4. doi: 10.1186/s12966-017-0641-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berthelsmann Stiftung Sozialplanung für Senioren. Fragebogen TF 1 Demografische und sozio-kulturelle Daten. 2018. http://www.sozialplanung-senioren.de/frageboegen-bausteine/frageboegen-nach-themenfeldern/index.html?L=0%2F%2F%2F%2F%27tyl
- Bickmore T.W., Silliman R.A., Nelson K., Cheng D.M., Winter M., Henault L., Paasche-Orlow M.K. A randomized controlled trial of an automated exercise coach for older adults. J. Am. Geriatr. Soc. 2013;61:1676–1683. doi: 10.1111/jgs.12449. [DOI] [PubMed] [Google Scholar]
- Boehle M. 2015. Armutsmessung mit dem Mikrozensus: methodische Aspekte und Umsetzung für Querschnitss- und Trendanalysen (GESIS Papers 2015/16). Köln: Leibniz-Insitut für Sozialwissenschaften. [Google Scholar]
- Bullinger M., Kirchberger L. Verlag für Psychologie; Hogrefe: 1998. Fragebogen zum Gesundheitszustand: SF-36; Handanweisung. [Google Scholar]
- Cadmus-Bertram L.A., Marcus B.H., Patterson R.E., Parker B.A., Morey B.L. Randomized trial of a Fitbit-based physical activity intervention for women. Am. J. Prev. Med. 2015;49:414–418. doi: 10.1016/j.amepre.2015.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi L., Liu Z., Matthews C.E., Buchowski M.S. Validation of accelerometer wear and nonwear time classification algorithm. Med. Sci. Sports Exerc. 2011;43:357–364. doi: 10.1249/MSS.0b013e3181ed61a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compernolle S., Vandelanotte C., Cardon G., De Bourdeaudhuij I., De Cocker K. Effectiveness of a web-based, computer-tailored, pedometer-based physical activity intervention for adults: a cluster randomized controlled trial. J. Med. Internet Res. 2015;17:e38. doi: 10.2196/jmir.3402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creavin S.T., Wisniewski S., Noel-Storr A.H., Trevelyan C.M., Hampton T., Rayment D., Thom V.M., Nash K.J., Elhamoui H., Milligan R. Mini-mental state examination (MMSE) for the detection of dementia in clinically unevaluated people aged 65 and over in community and primary care populations. Cochrane Database Syst. Rev. 2016:CD011145. doi: 10.1002/14651858.CD011145.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finger J.D., Mensink G.B.M., Lange C., Manz K. Gesundheitsfördernde körperliche Aktivität in der Freizeit bei Erwachsenen in Deutschland. J. Heal. Monit. 2017;2:37–44. [Google Scholar]
- Fleig L., Lippke S., Pomp S., Schwarzer R. Intervention effects of exercise self-regulation on physical exercise and eating fruits and vegetables: a longitudinal study in orthopedic and cardiac rehabilitation. Prev. Med. 2011;53:182–187. doi: 10.1016/j.ypmed.2011.06.019. [DOI] [PubMed] [Google Scholar]
- Forberger S., Bammann K., Bauer J., Boll S., Bolte G., Brand T., Hein A., Koppelin F., Lippke S., Meyer J. How to tackle key challenges in the promotion of physical activity among older adults (65+): the AEQUIPA network approach. Int. J. Environ. Res. Public Health. 2017;14 doi: 10.3390/ijerph14040379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedson P.S., Melanson E., Sirard J. Calibration of the computer science and applications, Inc. accelerometer. Med. Sci. Sports Exerc. 1998;30:777–781. doi: 10.1097/00005768-199805000-00021. [DOI] [PubMed] [Google Scholar]
- Hong S.Y., Hughes S., Prohaska T. Factors affecting exercise attendance and completion in sedentary older adults: a meta-analytic approach. J. Phys. Act. Health. 2008;5:385–397. doi: 10.1123/jpah.5.3.385. [DOI] [PubMed] [Google Scholar]
- Hupin D., Roche F., Gremeaux V., Chatard J.C., Oriol M., Gaspoz J.M., Barthelemy J.C., Edouard P. Even a low-dose of moderate-to-vigorous physical activity reduces mortality by 22% in adults aged ≥60 years: a systematic review and meta-analysis. Br. J. Sports Med. 2015;49:1262–1267. doi: 10.1136/bjsports-2014-094306. [DOI] [PubMed] [Google Scholar]
- Irvine A.B., Gelatt V.A., Seeley J.R., Macfarlane P., Gau J.M. Web-based intervention to promote physical activity by sedentary older adults: randomized controlled trial. J. Med. Internet Res. 2013;15:e19. doi: 10.2196/jmir.2158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jonkman N.H., van Schooten K.S., Maier A.B., Pijnappels M. eHealth interventions to promote objectively measured physical activity in community-dwelling older people. Maturitas. 2018;113:32–39. doi: 10.1016/j.maturitas.2018.04.010. [DOI] [PubMed] [Google Scholar]
- Koch W.F., Frees B. ARD/ZDF-Onlinestudie 2017: Neun von zehn Deutschen online. Media Perspektiven. 2017:434–446. [Google Scholar]
- Kowalski K., Rhodes R., Naylor P.J., Tuokko H., MacDonald S. Direct and indirect measurement of physical activity in older adults: a systematic review of the literature. Int. J. Behav. Nutr. Phys. Act. 2012;9:148. doi: 10.1186/1479-5868-9-148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis Z.H., Ottenbacher K.J., Fisher S.R., Jennings K., Brown A.F., Swartz M.C., Martinez E., Lyons E.J. The feasibility and RE-AIM evaluation of the TAME health pilot study. Int. J. Behav. Nutr. Phys. Act. 2017;14:106. doi: 10.1186/s12966-017-0560-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michie S., Richardson M., Johnston M., Abraham C., Francis J., Hardeman W., Eccles M.P., Cane J., Wood C.E. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann. Behav. Med. 2013;46:81–95. doi: 10.1007/s12160-013-9486-6. [DOI] [PubMed] [Google Scholar]
- Mouton A., Cloes M. Efficacy of a web-based, center-based or combined physical activity intervention among older adults. Health Educ. Res. 2015;30:422–435. doi: 10.1093/her/cyv012. [DOI] [PubMed] [Google Scholar]
- Muellmann S., Bragina I., Voelcker-Rehage C., Rost E., Lippke S., Meyer J., Schnauber J., Wasmann M., Toborg M., Koppelin F. Development and evaluation of two web-based interventions for the promotion of physical activity in older adults: study protocol for a community-based controlled intervention trial. BMC Public Health. 2017;17:512. doi: 10.1186/s12889-017-4446-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muellmann S., Forberger S., Möllers T., Bröring E., Zeeb H., Pischke C.R. Effectiveness of eHealth interventions for the promotion of physical activity in older adults: a systematic review. Prev. Med. 2018;108:93–110. doi: 10.1016/j.ypmed.2017.12.026. [DOI] [PubMed] [Google Scholar]
- Müller A.M., Khoo S. Non-face-to-face physical activity interventions in older adults: a systematic review. Int. J. Behav. Nutr. Phys. Act. 2014;11:35. doi: 10.1186/1479-5868-11-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson M.E., Rejeski W.J., Blair S.N., Duncan P.W., Judge J.O., King A.C., Macera C.A., Castaneda-Sceppa C. Physical activity and public health in older adults: recommendation from the American College of Sports Medicine and the American Heart Association. Med. Sci. Sports Exerc. 2007;39:1435–1445. doi: 10.1249/mss.0b013e3180616aa2. [DOI] [PubMed] [Google Scholar]
- Noar S.M., Benac C.N., Harris M.S. Does tailoring matter? Meta-analytic review of tailored print health behavior change interventions. Psychol. Bull. 2007;133:673–693. doi: 10.1037/0033-2909.133.4.673. [DOI] [PubMed] [Google Scholar]
- Peels D.A., Bolman C., Golsteijn R.H., de Vries H., Mudde A.N., van Stralen M.M., Lechner L. Long-term efficacy of a printed or a web-based tailored physical activity intervention among older adults. Int. J. Behav. Nutr. Phys. Act. 2013;10:104. doi: 10.1186/1479-5868-10-104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pomp S., Fleig L., Schwarzer R., Lippke S. Effects of a self-regulation intervention on exercise are moderated by depressive symptoms: a quasi-experimental study. Int. J. Clin. Health Psychol. 2013:1–8. [Google Scholar]
- Prince S.A., Adamo K.B., Hamel M.E., Hardt J., Connor Gorber S., Tremblay M. A comparison of direct versus self-report measures for assessing physical activity in adults: a systematic review. Int. J. Behav. Nutr. Phys. Act. 2008;5:56. doi: 10.1186/1479-5868-5-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rasche P., Schäfer K., Theis S., Bröhl C., Wille M., Mertens A. Age-related investigation of an activity tracker. Int. J. Hum. Factors Ergon. 2016;4:187–212. [Google Scholar]
- Richards J., Hillsdon M., Thorogood M., Foster C. Face-to-face interventions for promoting physical activity. Cochrane Database of Syst. Rev. 2013;(9) doi: 10.1002/14651858.CD010395.pub2. Art. No.: CD010392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robert-Koch-Institut . Robert-Koch-Institut; Berlin: 2009. Studie zur Gesundheit Erwachsener in Deutschland (DEGS): Gesundheitsfragebogen ab 65 Jahren. [Google Scholar]
- Sasaki J.E., John D., Freedson P.S. Validation and comparison of ActiGraph activity monitors. J. Sci. Med. Sport. 2011;14:411–416. doi: 10.1016/j.jsams.2011.04.003. [DOI] [PubMed] [Google Scholar]
- Shin G., Jarrahi M.H., Fei Y., Karami A., Gafinowitz N., Byun A., Lu X. Wearable activity trackers, accuracy, adoption, acceptance and health impact: a systematic literature review. J. Biomed. Inform. 2019;93 doi: 10.1016/j.jbi.2019.103153. [DOI] [PubMed] [Google Scholar]
- Short C.E., James E.L., Plotnikoff R.C., Girgis A. Efficacy of tailored-print interventions to promote physical activity: a systematic review of randomised trials. Int. J. Behav. Nutr. Phys. Act. 2011;8:113. doi: 10.1186/1479-5868-8-113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Statistisches Bundesamt . Statistisches Bundesamt; Wiesbaden: 2016. Demographische Standards Ausgabe 2016 Statistik und Wissenschaft. [Google Scholar]
- Suboc T.B., Strath S.J., Dharmashankar K., Coulliard A., Miller N., Wang J., Tanner M.J., Widlansky M.E. Relative importance of step count, intensity, and duration on physical activity's impact on vascular structure and function in previously sedentary older adults. J. Am. Heart Assoc. 2014;3 doi: 10.1161/JAHA.113.000702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan A.N., Lachman M.E. Behavior change with fitness Technology in Sedentary Adults: a review of the evidence for increasing physical activity. Front. Public Health. 2016;4:289. doi: 10.3389/fpubh.2016.00289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vandelanotte C., Duncan M.J., Maher C.A., Schoeppe S., Rebar A.L., Power D.A., Short C.E., Doran C.M., Hayman M.J., Alley S.J. The effectiveness of a web-based computer-tailored physical activity intervention using Fitbit activity trackers: randomized trial. J. Med. Internet Res. 2018;20 doi: 10.2196/11321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warburton D.E., Nicol C.W., Bredin S.S. Health benefits of physical activity: the evidence. CMAJ. 2006;174:801–809. doi: 10.1503/cmaj.051351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wijsman C.A., Westendorp R.G., Verhagen E.A., Catt M., Slagboom P.E., de Craen A.J., Broekhuizen K., van Mechelen W., van Heemst D., van der Ouderaa F., Mooijaart S.P. Effects of a web-based intervention on physical activity and metabolism in older adults: randomized controlled trial. J. Med. Internet Res. 2013;15 doi: 10.2196/jmir.2843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . 2010. Global Recommendations on Physical Activty for Health. Geneva. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
CONSORT checklist.
Intervention effects stratified by gender, age, level of education, and WHO MVPA recommendation at baseline achieved.