Abstract
Objectives. To explore US geographic areas with limited access to HIV preexposure prophylaxis (PrEP) providers, PrEP deserts.
Methods. We sourced publicly listed PrEP providers from a national database of PrEP providers from 2017 and obtained county-level urbanicity classification and population estimates of men who have sex with men (MSM) from public data. We calculated travel time from census tract to the nearest provider. We classified a census tract as a PrEP desert if 1-way driving time was greater than 30 or 60 minutes.
Results. One in 8 PrEP-eligible MSM (108 758/844 574; 13%) lived in 30-minute-drive deserts, and a sizable minority lived in 60-minute-drive deserts (38 804/844 574; 5%). Location in the South and lower urbanicity were strongly associated with increased odds of PrEP desert status.
Conclusions. A substantial number of persons at high risk for HIV transmission live in locations with no nearby PrEP provider. Rural and Southern areas are disproportionately affected.
Public Health Implications. For maximum implementation effectiveness of PrEP, geography should not determine access. Programs to train clinicians, expand venues for PrEP care, and provide telemedicine services are needed.
In the United States, men who have sex with men (MSM) account for a disproportionate proportion of HIV transmission.1 Easily accessible combination prevention strategies are needed to effectively address the HIV pandemic.2 HIV preexposure prophylaxis (PrEP), the provision of antiretroviral medication as a prophylactic measure for at-risk, HIV-uninfected individuals, is highly effective in preventing HIV transmission in clinical trials and clinical practice settings.3–5 Implementation of PrEP programs for populations with highest incidence is critical to reducing new infections in the United States; however, challenges have been observed in translating PrEP interest into PrEP uptake.6,7
The US Public Health Service provides guidelines for PrEP that recommend 4 annual visits with a licensed provider for HIV testing and prescription refill,8 making physical access to providers an important component of PrEP access. A number of factors are strongly associated with uptake of and retention in PrEP care, such as cost for medical services,6,9,10 race,9 and insurance.7 To ensure that PrEP reaches less advantaged groups that are often most in need of the service, novel programs and research will be needed.11
Several systematic reviews have found negative associations between length of travel and health outcomes.12–14 One covered 108 publications spanning a broad array of health domains, from dental care to sleep apnea to HIV care; it found that more than three quarters of the studies identified an association between greater distance or travel time to care and negative health outcomes.13 A review of 27 cancer studies with more than 700 000 patients concluded that greater distance was associated with more advanced disease at diagnosis (potentially indicating lower use of preventive services), less appropriate treatment strategies, and worse prognoses.14 One HIV care study found that an intervention that decreased transit time to care resulted in a 10% absolute increase in the number of patients achieving the targeted number of annual HIV clinic visits.15 Geographic proximity may be especially impactful for prevention services such as PrEP relative to treatment services considered by many previous studies; treatment services that yield immediate, more visible benefits are likely to have higher demand than the invisible benefits of prevention services.12
We previously described the density of PrEP-providing clinics at state and county levels, finding that counties with higher proportions of residents living in poverty, lacking health insurance, or identifying as African American or Latino had lower PrEP clinic density when epidemic burden was taken into account.16 Using a national database of PrEP providers and public data sources, we sought to build on this work by identifying geographic areas without nearby PrEP providers and providing minimum estimates of the number of PrEP-eligible MSM facing geographic barriers to accessing PrEP. This study defines these limited-access areas as PrEP deserts, identifying geographic and sociodemographic correlates to explicate and highlight access inequities.
METHODS
We obtained data for PrEP-providing clinics from PrEP Locator, a national, publicly available database.17,18 We collected an initial list of PrEP providers from more than 50 different data sources, including state and local health department directories and surveys conducted by HIV-related medical organizations. We added supplementary, publicly listed PrEP clinics through Web searches. After we launched the PrEP Locator Web site in September 2016, viewers, including clinic staff, public health practitioners, and the public, entered information for additional clinics. Research staff verified eligibility for inclusion in the database using the following criteria: a working phone number, a unique address (for institutions with multiple locations, each separate address that prescribed PrEP received a separate entry in the database), at least 1 practitioner with appropriate professional licensure to prescribe PrEP, telephone confirmation that the clinic actively prescribed PrEP, and acceptance of new patients. The analytic sample included all PrEP providers vetted by late 2017.
Preexposure Prophylaxis Eligibility for Men Who Have Sex With Men
We calculated PrEP-eligible MSM population estimates by applying a US Centers for Disease Control and Prevention (CDC)-generated PrEP eligibility estimate for MSM (24.7%) to all county-level MSM population estimates.19 The CDC PrEP eligibility estimate includes adult, HIV-negative MSM if they had more than 2 sex partners in the past 12 months and either an STI diagnosis or any condomless anal intercourse in the past 12 months.8 The present analysis used total MSM population estimates that included transgender persons assigned male at birth. Our analysis did not include other PrEP-eligible populations such as at-risk women, people who inject drugs, or transgender persons assigned female at birth, because requisite data were not available for these groups.
Demographic and Geographic Methods
Analysis data included geographic shapefiles of census tracts and corresponding population-weighted centroids, defined as the point at which “an imaginary, weightless, rigid [surface] would balance” if population members were each assigned an equal mass.20 We obtained data from the US Census Bureau, joined to 2016 county-level estimates of the population of men who had sex with other men in the past 12 months21 and census tract–level socio-contextual demographics from the 2011–2015 American Community Survey (ACS) 5-year estimates (ACS tables B01001, B01001B, B01001I, B15002, B15003, B17001, B17001B, B17001I, B19013, B19083, and B27001); we exported these data to ArcGIS 10.4 (ESRI, Redlands, CA). The MSM population estimates were adjusted for differences in concentration of MSM (e.g., urban vs rural) by adding into the algorithm estimates based on ACS data of the number of male–male households in each county.21 We restricted the analytic data set to the 48 contiguous states because of challenges in calculating travel time in Alaska and Hawaii. County urbanicity, region, and division classifications were based on the 2013 National Center for Health Statistics Urban–Rural Classification Scheme: large central metro (principal city areas of metropolitan statistical areas [MSAs] with population ≥ 1 million); large fringe metro (nonprincipal areas of MSA with population ≥ 1 million); medium metro (MSA with population = 250 000–999 999); small metro (MSA with population < 250 000); micropolitan (areas with an urban core population = 10 000–49 000); and noncore (areas with urban core population < 10 000).22 Because subcounty MSM population estimates were unavailable, we allocated county-level estimates down to the census tract level by weighting tracts by the total number of men in the census tract divided by the total men in the county containing the census tract.
We geocoded a total of 1973 vetted PrEP providers in our database and exported them to ArcGIS 10.4. We overlaid and displayed geographic data using the USA Contiguous Lambert Conformal Conic projected coordinate system. We used population-weighted centroids to measure travel time and distance from census tracts to the nearest PrEP providers. We gathered data on driving time between tract-level population-weighted centroids and the nearest PrEP providers with an R-based call to the Google Maps application programming interface (API) similar to that used in previous studies.23 We conducted subanalyses that included only PrEP providers who offered services in Spanish, care to those without health insurance, and PrEP navigation services. We displayed these data using choropleth maps.
To define driving deserts, we selected a cutpoint of 30-minute drive time. This cutpoint has been proposed as a standard for nonemergency clinical care: stated willingness-to-travel time is generally lower than this threshold, and it is a cutpoint used by state and local health departments for planning purposes.24–26 The Department of Defense health care program (TRICARE) recently adopted a 30-minute drive time threshold for primary care, with those enrolled able to select a civilian provider if no TRICARE provider is within this driving time limit.27 Increasingly, studies are also assessing 60-minute drive time thresholds, so we provide data regarding this threshold for additional context.
Statistical Analysis
We described census tract–level demographic and spatial characteristics, as well as clinic characteristics, using proportions, medians, and interquartile ranges, with quartiles calculated for tract-level sociodemographic variables. We performed multivariable logistic regression analyses, presented as adjusted odds ratios (AORs) with associated 95% confidence intervals (CIs), for 30-minute or 60-minute desert tracts on census tract–level variables of educational attainment, poverty, income inequality, health insurance, median household income, race/ethnicity, urbanicity, and geography. To determine whether use of estimates for adjusted relative risks would affect our findings, we conducted an additional modeling approach: conditional margins regression using SAS-callable SUDAAN (Research Triangle Institute, Research Triangle Park, NC). We performed data analysis in SAS version 9.4 (SAS Institute, Cary, NC) and R version 3.4.2 (R Foundation for Statistical Computing, Vienna, Austria).
RESULTS
In one quarter of census tracts (18 609/72 344; 26%) in the contiguous United States, there was a 1-way drive of more than 30 minutes to the nearest PrEP provider (i.e., 30-minute desert; Table 1). An estimated population of 440 318 MSM (13%) and 108 758 PrEP-eligible MSM reside in these tracts classified as 30-minute deserts. One in 10 tracts (8008/72 344; 11%) were classified as 60-minute deserts, with an estimated population of 157 103 MSM and 38 804 PrEP-eligible MSM.
TABLE 1—
Population of Men Who Have Sex With Men (MSM) and Preexposure Prophylaxis (PrEP)-Eligible MSM Population by Driving Time From Population-Weighted Centroid: Contiguous United States, 2017
| No. of Census Tracts, No. (%) | MSM Population Estimate, No. (%) | CDC PrEP-Eligible MSM Population Estimate, No. (%) | |
| All census tracts | 72 344 (100.0) | 3 419 328 (100.0) | 844 574 (100.0) |
| Driving time to any clinic, min | |||
| 0–15 | 39 846 (55.1) | 2 317 852 (67.8) | 572 510 (67.8) |
| 16–30 | 13 889 (19.2) | 661 157 (19.3) | 163 306 (19.3) |
| 31–60 | 10 601 (14.7) | 283 215 (8.3) | 69 954 (8.3) |
| 61–90 | 4 677 (6.5) | 91 894 (2.7) | 22 698 (2.7) |
| 91–120 | 1 926 (2.7) | 37 588 (1.1) | 9 284 (1.1) |
| > 120 | 1 405 (1.9) | 27 621 (0.8) | 6 822 (0.8) |
Note. CDC = Centers for Disease Control and Prevention.
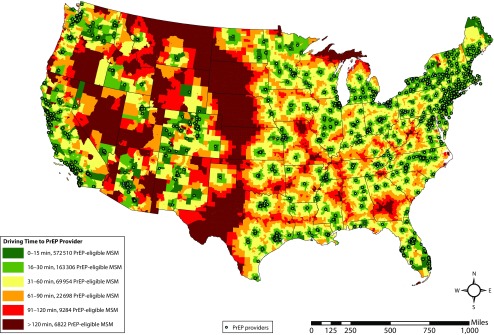
The geographic distribution of deserts and corresponding PrEP-eligible population estimates are displayed in Figure 1. PrEP providers clustered in urban population areas, particularly around major cities. Large areas with the lowest levels of geographic access (driving time > 90 minutes) were common in low-population areas in the West and Midwest, although low-access areas were also found in more populated areas in the South, such as substantial portions of Georgia and Texas. Supplementary tables and figures (available as supplements to the online version of this article at http://www.ajph.org) display the following additional analyses: comparisons of median values for census tract demographic characteristics among those living in desert tracts and nondesert tracts, population estimates stratified by driving time, population estimates stratified by PrEP provider service characteristics such as Spanish-language capability, PrEP provision to uninsured patents, and financial navigation assistance. Each of these additional analyses provided more strict criteria for clinics to be included in the analyses, leading to more persons being classified as living in a PrEP desert. For instance, 142 947 PrEP-eligible MSM lived in 30-minute deserts when we restricted the analysis to providers that include PrEP financial navigation assistance services, a 31% increase in the estimated number of MSM living in 30-minute PrEP deserts relative to analyses inclusive of all PrEP providers.
FIGURE 1—
Driving Time to Nearest Preexposure Prophylaxis (PrEP) Clinic for PrEP-Eligible Men Who Have Sex With Men (MSM): Contiguous United States, 2017
PrEP deserts existed in every geographic area and urban classification (Table 2). Less-urban areas (small metro or smaller) accounted for the majority of the PrEP-eligible population living in 30-minute deserts (55%; 59 928/108 755) and in 60-minute deserts (84%, 32 658/38 801). This is disproportionate to the population size for less urban areas, which accounted for only 11% (93 361/844 570) of all PrEP-eligible men. As expected, few census tracts in large central metro areas were classified as PrEP deserts. However, a substantial number of large fringe metro areas were classified as 30-minute deserts, accounting for 23% of persons living in PrEP deserts (25 127/108 755). Conversely, large central and large fringe areas together accounted for only 4.5% of all persons living in 60-minute PrEP deserts (1731/38 801).
TABLE 2—
Population of Men Who Have Sex With Men (MSM) and Preexposure Prophylaxis (PrEP)-Eligible MSM Population, in All Census Tracts and in PrEP Deserts, by County Urbanicity and Census Division: Contiguous United States, 2017
| All Census Tracts |
30-Minute Deserts |
60-Minute Deserts |
|||||||
| Census Tracts, No. (%) | Population Estimate, No. (%) | PrEP-Eligible Population Estimate, No. (%) | Census Tracts, No. (%) | Population Estimate, No. (%) | PrEP-Eligible Population Estimate, No. (%) |
Census Tracts, No. (%) | Population Estimate, No. (%) | PrEP-Eligible Population Estimate, No. (%) |
|
| All census tractsa | 72 341 (100) | 3 419 313 (100) | 844 570 (100) | 18 606 (100) | 440 303 (100) | 108 755 (100) | 8 005 (100) | 157 088 (100) | 38 801 (100) |
| County urbanicity | |||||||||
| Large central metro | 22 655 (31.3) | 1 812 618 (53.0) | 447 717 (53.0) | 284 (1.5) | 26 816 (6.1) | 6 624 (6.1) | 33 (0.4) | 1 738 (1.1) | 429 (1.1) |
| Large fringe metro | 16 555 (22.9) | 832 775 (24.4) | 205 695 (24.4) | 2 353 (12.6) | 101 728 (23.1) | 25 127 (23.1) | 115 (1.4) | 5 270 (3.4) | 1 302 (3.4) |
| Medium metro | 14 607 (20.2) | 395 940 (11.6) | 97 797 (11.6) | 2 952 (15.9) | 69 137 (15.7) | 17 077 (15.7) | 805(10.1) | 17 864 (11.4) | 4 412 (11.4) |
| Small metro | 6 576 (9.1) | 159 724 (4.7) | 39 452 (4.7) | 3 436 (18.5) | 79 748 (18.1) | 19 698 (18.1) | 1 704 (21.3) | 40 924 (26.1) | 10 108 (26.1) |
| Micropolitan | 6 538 (9.0) | 137 716 (4.0) | 34 016 (4.0) | 4 892 (26.3) | 96 696 (22.0) | 23 884 (22.0) | 2 469 (30.8) | 52 809 (33.6) | 13 044 (33.6) |
| Nonmetro | 5 410 (7.5) | 80 540 (2.4) | 19 893 (2.4) | 4 689 (25.2) | 66 178 (15.0) | 16 346 (15.0) | 2 879 (36.0) | 38 484 (24.5) | 9 506 (24.5) |
| County Census Division | |||||||||
| West | 15 575 (21.5) | 974 858 (28.5) | 240 790 (28.5) | 2 527 (13.6) | 104 109 (23.6) | 25 715 (23.6) | 1 301 (16.3) | 46 613 (29.7) | 11 513 (29.7) |
| Pacific | 10 325 (14.3) | 705 280 (20.6) | 174 204 (20.6) | 1 208 (6.5) | 62 446 (14.2) | 15 424 (14.2) | 423 (5.3) | 19 352 (12.3) | 4 780 (12.3) |
| Mountain | 5 250 (7.3) | 269 578 (7.9) | 66 586 (7.9) | 1 319 (7.1) | 41 663 (9.5) | 10 291 (9.5) | 878 (11.0) | 27 261 (17.4) | 6 733 (17.4) |
| Midwest | 17 027 (23.5) | 624 986 (18.3) | 154 372 (18.3) | 5 345 (28.7) | 80 236 (18.2) | 19 818 (18.2) | 2 188 (27.3) | 23 527 (15) | 5 811 (15.0) |
| West North Central | 5 283 (7.3) | 157 602 (4.6) | 38 928 (4.6) | 2 314 (12.4) | 28 241 (6.4) | 6 976 (6.4) | 1 400 (17.5) | 14 149 (9.0) | 3 495 (9.0) |
| East North Central | 11 744 (16.2) | 467 384 (13.7) | 115 444 (13.7) | 3 031 (16.3) | 51 995 (11.8) | 12 843 (11.8) | 788 (9.8) | 9 378 (6.0) | 2 316 (6.0) |
| South | 26 230 (36.3) | 1 353 008 (39.6) | 334 193 (39.6) | 9 564 (51.4) | 230 846 (52.4) | 57 019 (52.4) | 4 387 (54.8) | 83 942 (53.4) | 20 734 (53.4) |
| West South Central | 8 126 (11.2) | 447 402 (13.1) | 110 508 (13.1) | 3 095 (16.6) | 64 157 (14.6) | 15 847 (14.6) | 1 681 (21.0) | 28 694 (18.3) | 7 087 (18.3) |
| East South Central | 4 453 (6.2) | 151 399 (4.4) | 37 396 (4.4) | 2 376 (12.8) | 47 389 (10.8) | 11 705 (10.8) | 1 151 (14.4) | 20 326 (12.9) | 5 021 (12.9) |
| South Atlantic | 13 651 (18.9) | 754 207 (22.1) | 186 289 (22.1) | 4 093 (22) | 119 300 (27.1) | 29 467 (27.1) | 1 555 (19.4) | 34 922 (22.2) | 8 626 (22.2) |
| Northeast | 13 512 (18.7) | 466 476 (13.6) | 115 220 (13.6) | 1 173 (6.3) | 25 127 (5.7) | 6 206 (5.7) | 132 (1.6) | 3 021 (1.9) | 746 (1.9) |
| Middle Atlantic | 10 131 (14) | 353 830 (10.3) | 87 396 (10.3) | 924 (5.0) | 19 642 (4.5) | 4 851 (4.5) | 97 (1.2) | 2 241 (1.4) | 553 (1.4) |
| New England | 3 381 (4.7) | 112 646 (3.3) | 27 824 (3.3) | 249 (1.3) | 5 486 (1.2) | 1 355 (1.2) | 35 (0.4) | 781 (0.5) | 193 (0.5) |
Column sums may differ slightly from those of Table 1 because of missing data due to stratifying and re-summing across different covariates.
Each region had a substantial number of PrEP-eligible individuals living in 30-minute PrEP deserts. There was a considerable range across regions in the proportion of PrEP-eligible population living in a desert relative to total regional PrEP-eligible population: Northeast, 5.4% (6206/115 220); West, 10.7% (25 715/240 790); Midwest, 12.8% (19 818/154 372); and South, 17.1% (57 019/334 193). The corresponding proportions for 60-minute deserts were as follows: Northeast, 0.6% (746/115 220); West, 4.8% (11 513/240 790); Midwest, 3.8% (5811/154 372); and South, 6.2% (20 734/334 193). Six of the 9 geographic census divisions had more than 10 000 PrEP-eligible MSM living in 30-minute deserts and 4 of the 9 divisions (3 of which were in the South) had more than 5000 PrEP-eligible MSM living in 60-minute deserts.
Urbanicity, geographic census region, and demographic characteristics were associated with a tract being classified as a 30-minute desert in a regression model (Table 3). A model adjusting for all of these census tract–level characteristics found urbanicity and census region substantially correlated with being in a 30-minute PrEP desert. Compared with census tracts in small metro counties, tracts in more urban areas (large central: AOR = 0.01; 95% CI = 0.01, 0.01; large fringe: AOR = 0.18; 95% CI = 0.16, 0.19; medium: AOR = 0.21; 95% CI = 0.20, 0.23) were less likely to be deserts, whereas tracts in more rural areas, such as micropolitan (AOR = 2.81; 95% CI = 2.60, 3.04) and nonmetro counties (AOR = 5.40; 95% CI = 4.90, 5.96) were more likely to be deserts. Compared with the Northeast census region, tracts in all other regions had increased odds of being deserts (Midwest: AOR = 3.49; 95% CI = 3.21, 3.80; South: AOR = 7.84; 95% CI = 7.20, 8.54; West: AOR = 2.74; 95% CI = 2.49, 3.02). There were small negative associations between the outcome of being in a 30-minute desert and percentage increases in residents with high school education or who were African American or Hispanic. We found small positive associations in the same model for increases in income inequality, poverty, and lack of health insurance. A regression model for 60-minute deserts, as well as the additional regression approach, found similar associations (see the supplemental tables and figures).
TABLE 3—
Logistic Regression on 30-Minute Preexposure Prophylaxis (PrEP) Desert Classification With Census Tract–Level Demographic Correlates: Contiguous United States, 2017
| AOR (95% CI) |
||||
| Correlates | Basea | Base + NCHSb | Base + Regionc | Base + NCHS + Regiond |
| % with high school education: 5% increase | 0.74 (0.73, 0.75) | 0.89 (0.88, 0.91) | 0.74 (0.72, 0.75) | 0.89 (0.88, 0.91) |
| % living in poverty: 5% increase | 1.04 (1.03, 1.05) | 0.99 (0.97, 1.00) | 1.08 (1.06, 1.09) | 1.04 (1.02, 1.06) |
| Income inequality (Gini coefficiente): 0.05 increase | 1.03 (1.02, 1.05) | 1.04 (1.01, 1.08) | 1.03 (1.01, 1.05) | 1.00 (0.98, 1.02) |
| % without health insurance: 5% increase | 1.28 (1.26, 1.30) | 1.22 (1.19, 1.24) | 1.10 (1.08, 1.11) | 1.03 (1.01, 1.05) |
| Median household income: $1000 increase | 0.99 (0.99, 1.00) | 1.00 (1.00, 1.00) | 1.00 (0.99, 1.00) | 1.00 (1.00, 1.00) |
| % African American: 5% increase | 0.84 (0.83, 0.84) | 0.95 (0.94, 0.96) | 0.81 (0.81, 0.82) | 0.91 (0.90, 0.92) |
| % Hispanic: 5% increase | 0.75 (0.75, 0.76) | 0.94 (0.94, 0.95) | 0.78 (0.78, 0.79) | 0.97 (0.96, 0.97) |
| Urbanicity | ||||
| Large central metro vs small metro | . . . | 0.01 (0.01, 0.01) | . . . | 0.01 (0.01, 0.01) |
| Large fringe metro vs small metro | . . . | 0.17 (0.16, 0.19) | . . . | 0.18 (0.16, 0.19) |
| Medium metro vs small metro | . . . | 0.23 (0.22, 0.25) | . . . | 0.21 (0.20, 0.23) |
| Micropolitan vs small metro | . . . | 2.50 (2.32, 2.70) | . . . | 2.81 (2.60, 3.04) |
| Nonmetro vs small metro | . . . | 5.07 (4.61, 5.57) | . . . | 5.40 (4.90, 5.96) |
| Census region | . . . | |||
| Midwest vs Northeast | . . . | . . . | 4.32 (4.02, 4.64) | 3.49 (3.21, 3.80) |
| South vs Northeast | . . . | . . . | 7.26 (6.76, 7.80) | 7.84 (7.20, 8.54) |
| West vs Northeast | . . . | . . . | 2.66 (2.46, 2.88) | 2.74 (2.49, 3.02) |
Note. AOR = adjusted odds ratio; CI = confidence interval; NCHS = National Center for Health Statistics.
Base model adjusts for the following variables at the census tract level: education, poverty, income inequality, health insurance, median household income, and race/ethnicity.
Base + NCHS adjusts for the following variables at the census tract level: education, poverty, income inequality, health insurance, median household income, race/ethnicity, NCHS county urbanicity (6-category 2013 National Center on Health Statistics Urban–Rural Classification scheme for counties classification; https://www.cdc.gov/nchs/data_access/urban_rural.htm).
Base + Region adjusts for the following variables at the census tract level: education, poverty, income inequality, health insurance, median household income, race/ethnicity, US Census Region (4-category Census Bureau Region Classification; https://www.census.gov/geo/reference/gtc/gtc_census_divreg.html).
Base + NCHS + Region adjusts for the following variables at the census tract level: education, poverty, income inequality, health insurance, median household income, race/ethnicity, NCHS county urbanicity, US Census Region.
The Gini coefficient is a statistical measure of distribution of wealth or income, used as a measure of income inequality (range is 0 [minimum] to 1 [maximum]).
DISCUSSION
Using a database of publicly listed PrEP service providers, we explored disparities in geospatial access to care for this essential HIV prevention service. This study of PrEP deserts illustrates that a substantial number of individuals for whom PrEP would be recommended have limited geographic access to care: more than 100 000 would need to travel more than 60 minutes roundtrip per PrEP care visit, and more than 38 000 would travel more than 120 minutes. The majority of those facing longer commute times to care reside in rural areas. Transit barriers to care may especially affect PrEP use, because PrEP is a prevention service and the benefits therefore accrue less immediately than those for treatment.28 These results bolster a recent random forest modeling analysis of data from the PrEP Demo Project, which determined that access to a PrEP provider is a rate-limiting step to scale-up of access to PrEP.7 The findings build on previous work that found disparities in the geographic distribution of PrEP clinics29 by providing estimates of the number of persons affected by lengthy travel time to care, an important consideration for policy and programs.
The substantial number of persons residing in PrEP service deserts points to the need to develop interventions to increase PrEP care access for individuals in rural areas. Some promising approaches are provider training, alternative venue models (e.g., pharmacies or health departments), and telemedicine.30,31 Census tracts in the South were nearly 8 times more likely to be classified as PrEP deserts than were census tracts in the Northeast. This is especially striking because the South is a substantial area for HIV transmission in the United States, accounting for more than half of new HIV diagnoses in 2016 (https://www.cdc.gov/hiv/library/reports/hiv-surveillance.html). Even in models that adjusted for population density by including urbanicity as a covariate, the South had a disproportionate share of PrEP deserts. Low PrEP access in the South is probably partially because of lower concentrations of PrEP-providing clinics per capita and per new HIV diagnosis than in the Northeast.16 Policy also affects PrEP availability. For instance, states that did not expand Medicaid under the Affordable Care Act had only half as many PrEP users per new HIV diagnosis as states that adopted Medicaid expansion.29
The majority of PrEP-eligible persons living in PrEP deserts resided in rural areas, indicating a need to target service availability to more remote areas. Associations between travel time to health care and rural residence are well documented for a variety of health conditions, as are the negative impacts on health outcomes that result from such transit barriers.12 Persons living in rural areas were more likely to reside in PrEP deserts; however, the role of urbanicity is more complex than a dichotomy. Nearly one quarter of the estimated PrEP-eligible population in 30-minute PrEP deserts resided in suburban areas (large fringe metros). Individuals residing in deserts located in suburban areas may have substantially higher transit times than the 30-minute threshold, because our analysis used ideal traffic conditions that likely underestimates urban transit time. Enhanced PrEP geographic availability is therefore needed not only for rural areas but also for suburban areas. This is especially important because suburban areas face increasing levels of poverty, which itself may serve as a barrier to obtaining efficient transit and access to care.32
This study describes a single barrier to PrEP care. To obtain care, patients must overcome this geographic barrier, but also many other obstacles. PrEP care has been conceptualized as a continuum, featuring 5 steps required for engagement in care: awareness, access (geographic, financial), likelihood of receiving a prescription (sexual risk disclosure to clinician, screening eligibility), adherence, and maintenance.2 Factors contributing to retention through this cascade include health insurance,7 region,7,29 and cost for medical services.6,9,10 The present analysis found that residing in a PrEP desert was significantly and positively associated with some of these predictors, including proportion of residents without health insurance and living in the South. Given the presence of multiple barriers to care facing those living in PrEP deserts, programs should seek to simultaneously address both geographic and other access barriers to achieve maximum effect.
Describing spatial access to HIV prevention can support tailored prevention strategies, as well as inform the allocation of resources to address existing gaps. Geographic information systems (GIS) approaches, including using population-weighted centroids to measure proximity and access, can help detect underserved areas, identifying geographic and region-specific gaps in proximity to health care services due to increased travel burden. A recent analysis using similar methods described block group–level access to abortion providers in the United States and identified geographic and urban–rural disparities in service provision similar to those observed in this analysis, with 20% of women having to travel at least 42 miles to access the nearest clinic.33 The patterns in access observed for PrEP clinics may therefore reflect similar patterns for less socially accepted services, which are disproportionately located in population-dense urban areas.
Limitations
There are limitations to this analysis. It was restricted to MSM because small-area population size estimates for other at-risk groups were not available. Future efforts to provide such estimates are needed to allow for analyses that can inform policy not only for PrEP but for other health issues that disproportionately affect groups at elevated risk for HIV transmission. By using a single point in each census tract to describe access, more nuanced findings regarding geographic access to PrEP may have been missed. Individuals often do not visit their closest provider, instead selecting more distant providers based on other considerations. The closest-provider metric used might therefore underestimate transit time to care. However, individuals may attend health care visits closer to other points of interest (e.g., shopping or work), resulting in overestimation of transit time. Another limitation of the analysis is that it only accounts for car transit, which could have led to substantial underestimation of the number of individuals facing time transit barriers to PrEP care. Future analyses should seek to incorporate public transit time estimates.12 Geographic proximity is a single component of health care access, situated within many other barriers to care. Although we observed and explored spatial disparities, the data set did not allow a full consideration of other, known barriers to accessing PrEP care.
Although we attempted to address small-area population distribution using population-weighted center points, other methods, including dasymetric methods, can address this concern further. Smaller levels of data analysis can leverage individual data to gain information regarding work and other frequented locations. We used previously developed estimates of MSM population that were adjusted for potential rural–urban differences in population concentration at the county level.21 Census tract–level data were not available, so we assumed equal MSM population distributions within counties. This could overestimate PrEP desert population size if MSM populations within counties are systematically more densely located in areas closer to the nearest PrEP-prescribing clinics.
We found that geographic access to PrEP care is limited for many MSM in the United States. Expanding geographic access is therefore likely to be a key component in bringing this highly effective intervention to scale, a finding that echoes previous recommendations.7,16,29 The dearth of PrEP providers offering services in rural and Southern areas is likely best addressed by systems-level interventions to address this unmet need, such as programs to train more providers or to offer telemedicine. To maximize the implementation effectiveness of PrEP, geography should not dictate access.34
Public Health Implications
These findings highlight the magnitude of geographic disparities in access to PrEP for HIV. Applying these geographic methods to other important public health issues can highlight deserts with limited access to care or prevention services, as well as inform where resources are geographically targeted to address these gaps. For suburban and more densely populated rural areas, programs can be targeted to provide PrEP through alternative venues (e.g., pharmacies are currently running hundreds of sites that offer PrEP, and this could be expanded) or to train willing clinicians. For more remote rural areas, telemedicine options may be optimal. A National Institutes of Health (NIH) Adolescent Medicine Trials Network–funded multisite clinical trial (NIH ATN159) is assessing the impact of providing app-based telemedicine PrEP care and remote laboratory testing on the uptake of and maintenance in PrEP care.35 The use of technology-based interventions may be key to overcoming geographic barriers to accessing care.
ACKNOWLEDGMENTS
This work was supported by the National Institute of Mental Health (R01MH114692) and the Adolescent Medicine Trials Network for HIV/AIDS Interventions (Protocol 159) from the National Institutes of Health (U19HD089881). The work was facilitated by the Emory Center for AIDS Research (P30AI050409).
Note. The contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health.
CONFLICTS OF INTEREST
A. J. Siegler is a coinvestigator on a grant funded by the Gilead Foundation. All other authors have no conflicts of interest to report.
HUMAN PARTICIPANT PROTECTION
This study did not involve human participants and therefore was not subject to review by an institutional review board.
Footnotes
REFERENCES
- 1.Patel P, Borkowf CB, Brooks JT, Lasry A, Lansky A, Mermin J. Estimating per-act HIV transmission risk. AIDS. 2014;28(10):1509–1519. doi: 10.1097/QAD.0000000000000298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kelley CF, Kahle E, Siegler A et al. Applying a PrEP continuum of care for men who have sex with men in Atlanta, Georgia. Clin Infect Dis. 2015;61(10):1590–1597. doi: 10.1093/cid/civ664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Marcus JL, Hurley LB, Hare CB et al. Preexposure prophylaxis for HIV prevention in a large integrated health care system. J Acquir Immune Defic Syndr. 2016;73(5):540–546. doi: 10.1097/QAI.0000000000001129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Grant RM, Lama JR, Anderson PL et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med. 2010;363(27):2587–2599. doi: 10.1056/NEJMoa1011205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McCormack S, Dunn DT, Desai M et al. Pre-exposure prophylaxis to prevent the acquisition of HIV-1 infection (PROUD): effectiveness results from the pilot phase of a pragmatic open-label randomised trial. Lancet. 2016;387(10013):53–60. doi: 10.1016/S0140-6736(15)00056-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rolle C-P, Rosenberg ES, Siegler AJ et al. Challenges in translating PrEP interest into uptake in an observational study of young black MSM. J Acquir Immune Defic Syndr. 2017;76(3):250–258. doi: 10.1097/QAI.0000000000001497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Doblecki-Lewis S, Liu A, Feaster D et al. Healthcare access and PrEP continuation in San Francisco and Miami after the US PrEP Demo Project. J Acquir Immune Defic Syndr. 2017;74(5):531–538. doi: 10.1097/QAI.0000000000001236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.US Public Health Service. Preexposure prophylaxis for the prevention of HIV infection in the United States—2017 update: a clinical practice guideline. Available at: https://www.cdc.gov/hiv/pdf/risk/prep/cdc-hiv-prep-guidelines-2017.pdf. Accessed August 9, 2018.
- 9.Chan PA, Mena L, Patel R et al. Retention in care outcomes for HIV pre-exposure prophylaxis implementation programmes among men who have sex with men in three US cities. J Int AIDS Soc. 2016;19(1):20903. doi: 10.7448/IAS.19.1.20903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Serota DP, Rosenberg ES, Lockard AM et al. Beyond the biomedical: preexposure prophylaxis failures in a cohort of young black men who have sex with men in Atlanta, GA. Clin Infect Dis. 2018;67(6):965–970. doi: 10.1093/cid/ciy297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hankins C, Macklin R, Warren M. Translating PrEP effectiveness into public health impact: key considerations for decision-makers on cost-effectiveness, price, regulatory issues, distributive justice and advocacy for access. J Int AIDS Soc. 2015;18(4 suppl 3):19973. doi: 10.7448/IAS.18.4.19973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Syed ST, Gerber BS, Sharp LK. Traveling towards disease: transportation barriers to health care access. J Community Health. 2013;38(5):976–993. doi: 10.1007/s10900-013-9681-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kelly C, Hulme C, Farragher T, Clarke G. Are differences in travel time or distance to healthcare for adults in global north countries associated with an impact on health outcomes? A systematic review. BMJ Open. 2016;6(11):e013059. doi: 10.1136/bmjopen-2016-013059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ambroggi M, Biasini C, Del Giovane C, Fornari F, Cavanna L. Distance as a barrier to cancer diagnosis and treatment: review of the literature. Oncologist. 2015;20(12):1378–1385. doi: 10.1634/theoncologist.2015-0110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bilinski A, Birru E, Peckarsky M et al. Distance to care, enrollment and loss to follow-up of HIV patients during decentralization of antiretroviral therapy in Neno District, Malawi: a retrospective cohort study. PLoS One. 2017;12(10):e0185699. doi: 10.1371/journal.pone.0185699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Siegler AJ, Bratcher A, Weiss KM et al. Location location location: an exploration of disparities in access to publicly listed PrEP clinics in the United States. Ann Epidemiol. 2018;28(12):858–864. doi: 10.1016/j.annepidem.2018.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Siegler AJ, Wirtz S, Weber S, Sullivan PS. Developing a Web-based geolocated directory of HIV pre-exposure prophylaxis-providing clinics: The PrEP Locator Protocol and Operating Procedures. JMIR Public Health Surveill. 2017;3(3):e58. doi: 10.2196/publichealth.7902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bratcher A, Schlueter Wirtz S, Siegler AJ. Users of a national directory of PrEP service providers: beliefs, self-efficacy, and progress toward prescription. J Acquir Immune Defic Syndr. 2018;78(4):e28–e30. doi: 10.1097/QAI.0000000000001706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Smith DK, Van Handel M, Wolitski RJ et al. Vital signs: estimated percentages and numbers of adults with indications for preexposure prophylaxis to prevent HIV acquisition—United States, 2015. MMWR Morb Mortal Wkly Rep. 2015;64(46):1291–1295. doi: 10.15585/mmwr.mm6446a4. [DOI] [PubMed] [Google Scholar]
- 20.US Census Bureau. Centers of population. Available at: https://www.census.gov/geographies/reference-files/2010/geo/2010-centers-population.html. Accessed June 21, 2019.
- 21.Grey JA, Bernstein KT, Sullivan PS et al. Estimating the population sizes of men who have sex with men in US states and counties using data from the American Community Survey. JMIR Public Health Surveill. 2016;2(1):e14. doi: 10.2196/publichealth.5365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.National Center for Health Statistics. Urban–rural classification scheme for counties. Available at: https://www.cdc.gov/nchs/data_access/urban_rural.htm. Accessed October 23, 2017.
- 23.Dasgupta S, Kramer MR, Rosenberg ES, Sanchez TH, Sullivan PS. Spatial accessibility to HIV providers in Atlanta, Georgia. AIDS Res Hum Retroviruses. 2015;31(5):473–474. doi: 10.1089/aid.2014.0365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bosanac EM, Parkinson RC, Hall DS. Geographic access to hospital care: a 30-minute travel time standard. Med Care. 1976;14(7):616–624. doi: 10.1097/00005650-197607000-00006. [DOI] [PubMed] [Google Scholar]
- 25.Yen W Washington State Health Services Research Project. How long and how far do adults travel and will adults travel for primary care? 2013. Available at: https://www.ofm.wa.gov/sites/default/files/public/legacy/researchbriefs/2013/brief070.pdf. Accessed April 1, 2019.
- 26.Oklahoma State Dept of Health. Data and reports—Oklahoma health workforce databook. Available at: https://www.ok.gov/health/Organization/Center_for_Health_Innovation_and_Effectiveness/Data_and_Reports_/index.html. Accessed April 1, 2019.
- 27.Defense Health Agency. TRICARE prime distance and drive time standards. Available at: https://tricare.mil/primeaccess. Accessed April 1, 2019.
- 28.Ellis RP, Manning WG. Optimal health insurance for prevention and treatment. J Health Econ. 2007;26(6):1128–1150. doi: 10.1016/j.jhealeco.2007.09.002. [DOI] [PubMed] [Google Scholar]
- 29.Siegler AJ, Mouhanna F, Giler RM et al. The prevalence of pre-exposure prophylaxis use and the pre-exposure prophylaxis-to-need ratio in the fourth quarter of 2017, United States. Ann Epidemiol. 2018;28(12):841–849. doi: 10.1016/j.annepidem.2018.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Siegler AJ, Mayer KH, Liu AY et al. Developing and assessing the feasibility of a home-based PrEP monitoring and support program. Clin Infect Dis. 2019;68(3):501–504. doi: 10.1093/cid/ciy529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tung E, Thomas A, Eichner A, Shalit P. Feasibility of a pharmacist-run HIV PrEP clinic in a community pharmacy setting. Paper presented at: Conference on Retroviruses and Opportunistic Infections (CROI); March 4–7, 2018; Boston, MA.
- 32.Boeri MW, Tyndall BD, Woodall DR. Suburban poverty: barriers to services and injury prevention among marginalized women who use methamphetamine. West J Emerg Med. 2011;12(3):284–292. [PMC free article] [PubMed] [Google Scholar]
- 33.Bearak JM, Burke KL, Jones RK. Disparities and change over time in distance women would need to travel to have an abortion in the USA: a spatial analysis. Lancet Public Health. 2017;2(11):e493–e500. doi: 10.1016/S2468-2667(17)30158-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mayer KH, Krakower DS. Editorial commentary: scaling up antiretroviral preexposure prophylaxis: moving from trials to implementation. Clin Infect Dis. 2015;61(10):1598–1600. doi: 10.1093/cid/civ665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Siegler AJ, Brock JB, Hurt CB et al. An electronic pre-exposure prophylaxis initiation and maintenance home care system for nonurban young men who have sex with men: protocol for a randomized controlled trial. JMIR Res Protoc. 2019;8(6):e13982. doi: 10.2196/13982. [DOI] [PMC free article] [PubMed] [Google Scholar]