Abstract
Objectives. To determine whether the 2014 Affordable Care Act Medicaid expansion affected well-being in the low-income and general adult US populations.
Methods. We obtained data from adults aged 18 to 64 years in the nationally representative Gallup-Sharecare Well-Being Index from 2010 to 2016 (n = 1 674 953). We used a difference-in-differences analysis to compare access to and difficulty affording health care and subjective well-being outcomes (happiness, sadness, worry, stress, and life satisfaction) before and after Medicaid expansion in states that did and did not expand Medicaid.
Results. Access to health care increased, and difficulty affording health care declined following the Medicaid expansion. Medicaid expansion was not associated with changes to emotional states or life satisfaction over the study period in either the low-income population who newly gained health insurance or in the general adult population as a spillover effect of the policy change.
Conclusions. Although the public health benefits of the Medicaid expansion are increasingly apparent, improved population well-being does not appear to be among them.
Public Health Implications. Subjective well-being indicators may not be informative enough to evaluate the public health impact of expanded health insurance.
A key component of the US Affordable Care Act (ACA) was the expansion of Medicaid eligibility to nonelderly adults with incomes up to 138% of the federal poverty level.1 This policy resulted in 9.6 million people becoming newly eligible for Medicaid beginning in 2014.2 The rapidly growing literature documents a range of beneficial outcomes for the newly eligible population, including higher rates of insurance coverage, increased access to health care providers, improved quality of care, increased use of preventive health services, reduced likelihood of emergency department visits, and reduced financial difficulties.3–7 Public health spillover effects with relevance to the general population also have been documented, including lower rates of crime, higher prescribing of opioid treatments, and reduced socioeconomic disparities in access to health care.8–11 Evidence of direct effects on health outcomes is relatively scarce,5 whereas a growing body of evidence shows mixed results for its effect on self-rated health.7,11–14 The effects of the ACA Medicaid expansion on population well-being in the United States are unknown.
Human well-being is gaining attention from researchers and policymakers as a metric of social welfare that goes beyond standard indicators for health policy evaluation.15–18 Broadly defined, subjective well-being is a multidimensional concept that refers to people’s evaluative judgments about their quality of life, referred to as “life satisfaction,” and emotional or affective states such as happiness, anger, or sadness.17 Life satisfaction and emotional states are sensitive to external events, such as the 2008 financial crisis and local employment shocks19–21 and are strongly predictive of health outcomes, including risks of cardiovascular disease and all-cause mortality.22–26 As direct and immediate indicators of welfare, these well-being measures have been proposed as metrics to assess the human welfare implications of policy interventions.17,27 However, the effects of health policies on the well-being of the US general population have rarely been investigated.
We hypothesized that the ACA Medicaid expansion would be associated with improved well-being in the policy-eligible low-income population through increasing access to health care, which in turn may reduce exposure to health and financial risks. With respect to effects on population well-being beyond the policy-eligible population, it is important to note that the ACA was politically unpopular when the Medicaid expansion component went into effect in January 2014. At this time, 50% of persons in the United States had an unfavorable view of the ACA, compared with just 34% who reported a favorable opinion of the ACA.28 Hence, whereas the societal welfare benefits introduced by the ACA Medicaid expansion could improve well-being in population members outside the policy-eligible population, the unpopularity of the ACA could also have resulted in the Medicaid expansion having negative effects on well-being in the general population. We thus hypothesized that the net population spillover effect could be in either direction or possibly null if changes to this health policy did not affect well-being or had mixed effects on well-being among the unaffected segment of the general adult population.
Using individual-level data from more than 1.6 million US adults aged 18 to 64 years in the population-representative Gallup-Sharecare Well-Being Index from 2010 to 2016, we used a difference-in-differences analysis to compare pre- to post-ACA Medicaid expansion changes in subjective well-being indicators in (1) the policy-eligible low-income population who newly gained access to health insurance, and (2) the general adult population as a spillover effect of this policy change.
METHODS
We conducted a secondary analysis of data from the nationally representative US Gallup-Sharecare Well-Being Index, a daily telephone survey of at least 500 interviews each day with adults 18 years and older conducted by the Gallup Organization.29 As with the US Gallup Daily Poll, the survey uses a dual-frame stratified sampling design targeting landlines and cell phones and represents more than 90% of the adult US population.29 We restricted our sample to include individual-level data from adults aged 18 to 64 years and the years 2010 through 2016 (n = 1 674 953).
Ethical Approval
The Gallup-Sharecare Well-Being Index is conducted according to the Gallup Citizenship Guide and Code of Conduct. All procedures were conducted in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000.
Identification of Policy-Eligible Population
The Medicaid expansion-eligible population with household incomes up to 138% of the federal poverty level was identified according to reported household income bracket (< $720, $720–$5999, $6000–$11 999, $12 000–$23 999, $24 000–$35 999, $36 000–$47 999, $48 000–$59 999, ≥ $60 000), adjusted for household size as determined by reported marital status and number of children younger than 18 years in the household. Because household income was reported in brackets, we assigned individuals the midpoint of their household income bracket that was reported in the study interview. Using this method, we estimated approximately 13% of the sample to be below 138% of the federal poverty rate, which is in line with national estimates.30 The analysis sample excludes observations between March and December of 2015 from the analysis because of missing information on income for this period.
Analytical Design
To identify effects of the ACA Medicaid expansion on well-being outcomes, we used a difference-in-differences analytical design to exploit plausibly exogeneous state-level variation in new eligibility for health insurance coverage resulting from the Medicaid expansion.31 This policy expanded Medicaid eligibility to cover individuals from households with incomes up to 138% of the federal poverty level and was optional for states to participate in. Between January 1, 2014, and December 31, 2016, 32 states and the District of Columbia participated in the ACA Medicaid expansion, whereas 18 states opted out. We categorized the 32 states that expanded Medicaid as implementing “full,” “substantial,” or “mild” expansion, following the definition from Simon et al. (see the box on page 1238).12
Classification of US States by Affordable Care Act Medicaid Expansion: 2010–2016.
| Full expansion |
| AK, AZ, AR, CO, IL, IA, IN, KY, LA, MD, MI, MT, NH, NV, NJ, NM, ND, OH, OR, PA, RI, WA, WV |
| Substantial expansion |
| CA, CT, HI, MN, WI |
| Mild expansion |
| DE, DC, MA, NY, VT |
| Nonexpansion |
| AL, FL, GA, ID, KS, ME, MS, MO, NE, NC, OK, SC, SD, TN, TX, UT, VA, WY |
Note. All expansion states in the box expanded Medicaid eligibility in January 2014 except MI in April 2014, NH in August 2014, PA in January 2015, IN in February 2015, AK in September 2015, MT in January 2016, and LA in July 2016. We retrieved dates of expansion from Kaiser Family Foundation28 and classification of changes in Medicaid from Simon et al.12 WI did not expand Medicaid, but childless adults up to 100% of the federal poverty level (as defined according to 2016 thresholds determined by the US Census Bureau) were eligible. ID, UT, ME, NE, and VA approved Medicaid expansion but did not implement it during the study period.28
We excluded the 4 states defined as having mild expansion (Delaware, Massachusetts, New York, Vermont) and the District of Columbia after confirming that access to health insurance did not significantly change in these states compared with those that did not expand Medicaid. These mild expansion states had already implemented strong Medicaid expansions separate from the ACA policy before 2014. The substantial expansion states had, for the most part, implemented some degree of Medicaid expansion before 2014, but all participated in and substantially expanded their Medicaid programs as part of the ACA beginning in January 2014. The full expansion states fully expanded Medicaid coverage according to the ACA-mandated expansion beginning in January 2014.12
Outcomes
We measured life satisfaction using Cantril’s Self-Anchoring Striving Scale, in which the respondent is asked to rate his or her life on a ladder scale in which 1 represents “the worst possible life for you” and 10 represents “the best possible life for you.”32 Two versions of the scale were administered in the study interview: 1 for current life satisfaction and 1 for the expectation of life satisfaction in 5 years.32 We rescaled the life satisfaction outcomes to be from 10 to 100 to aid with interpretability of the results. Emotional states were measured by asking respondents whether they had experienced happiness, sadness, worry, and stress on the day before the interview (yes vs no). We rescaled these dichotomous outcomes to be from 0 to 100, in which the rescaled outcomes indicate the average percentage of the sample, out of 100%, who responded “yes” to experiencing the emotional state.
Covariates
We adjusted all models for age, race/ethnicity, education, gender, marital status, and the presence of children in the household to account for any residual confounding by these factors. We additionally adjusted for time-invariant indicators for state of residence (state fixed effects) as well as calendar day of the interview (time fixed effects). The state fixed effects account for any unmeasured differences between states, such as average differences in the outcomes. The time fixed effects account for any unmeasured common secular trends or events across states that could potentially confound the associations between Medicaid expansion and the outcomes under study, such as holidays, political events, or stock market volatility.
Statistical Analysis
Our difference-in-differences analysis of the ACA Medicaid expansion consisted of 3 steps. First, we assessed whether adults living in states that expanded Medicaid reported changes in their rates of health insurance coverage, access to a personal doctor, and difficulty affording health care following the expansion relative to those in nonexpansion states. Second, we assessed whether adults living in states that expanded Medicaid had changes in their subjective well-being following the expansion relative to those in nonexpansion states. Third, we visually compared differential pre- and post-Medicaid expansion time trends in the outcomes between expansion and nonexpansion states to confirm that the outcomes followed parallel trends over time before Medicaid expansion in both groups. We conducted these 3 steps first among the policy-eligible low-income population and then among the general adult population.
For the first 2 steps, we used ordinary least squares regressions to model the associations between living in a state that expanded Medicaid and each of the access to health care and subjective well-being outcomes under study, adjusted for age, gender, race/ethnicity, education, marital status, the presence of children in the household, and the state and time fixed effects. We clustered the SEs at the state level in all models to account for spatial correlations in outcomes across individuals living in the same states. We did not include the Gallup sampling weights in our models, as we had no reason to believe that the probability of survey response was related to both subjective well-being and living in a state that had expanded Medicaid at a specific point in time over our study period. Our results were relatively unaffected by using the sampling weights in a sensitivity analysis.
The difference-in-differences research design relies on the assumption of parallel trends, meaning that, after accounting for covariates, all outcomes followed the same trends in expansion and nonexpansion states before the Medicaid expansion index date. This assumption allows interpretation of the post-Medicaid expansion outcome trends in the nonexpansion states to represent the counterfactual outcomes in the states that expanded Medicaid, had they not expanded it. We tested this assumption directly in the third step of our analysis by using a dynamic difference-in-differences analysis, which captures the differences in outcome trends between expansion and nonexpansion states over the full study period on a monthly basis. Specifically, we visually inspected monthly differences in covariate-adjusted outcomes between expansion and nonexpansion states. If the parallel trends assumption holds, these differences should be statistically indistinguishable from zero before Medicaid expansion.
For a more technical explanation of our analytical approach, please refer to the supplementary statistical analysis in Appendix A (available as a supplement to the online version of this article at http://www.ajph.org). We conducted the statistical analyses using Stata/SE version 15.1 (College Station, TX) and R version 3.6 (R Core Team, Vienna, Austria).
Heterogeneity of Policy Effects
We examined heterogeneity in the effects of the ACA Medicaid expansion on well-being outcomes by applying our main model to the following subgroups in the policy-eligible population: gender, race/ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic), education (less than college, college graduate), marital status (married, not married), and having any children younger than 18 years in the household (yes, no).
Sensitivity Analyses
We estimated the results separately for states that fully and substantially expanded Medicaid to assess whether the results differed between these 2 groups.
RESULTS
The characteristics of the sample were consistent with the US general adult population (Table 1). We observed increases in the rates of health insurance coverage, increases in the likelihood of having a doctor, and decreases in the likelihood of reporting difficulty affording medical care in states that fully or substantially expanded Medicaid (Table 2). In the policy-eligible population, mean insurance coverage over the period before the expansion was 64.1%, and following the expansion it increased by 7.5 percentage points (95% confidence interval [CI] = 5.3, 9.8; Table 2). Of the policy-eligible population, 66% had access to a personal doctor during the period before Medicaid expansion; following the expansion the proportion reporting having access to a personal doctor increased by 3.5 percentage points (95% CI = 1.5, 5.5; Table 2). Of the policy-eligible population, 38% had difficulty affording medical care during the period before the expansion; following the expansion the proportion reporting difficulty affording medical care decreased by 3.7 percentage points (95% CI = –6.2, –1.2; Table 2). In the general adult population, we saw average effects in the same direction but of smaller magnitude (Table 2).
TABLE 1—
Characteristics of the Study Population: Gallup-Sharecare Well-Being Index, United States, 2010–2016
| Policy-Eligible Adult Population |
General Adult Population |
|||
| Characteristic | Mean (SD) or % | No. | Mean (SD) or % | No. |
| Age, y | 41.1 (13.7) | 165 144 | 44.9 (13.5) | 1 186 733 |
| Non-Hispanic White | 55.7 | 161 221 | 74.8 | 1 148 122 |
| Non-Hispanic Black | 15.6 | 161 221 | 9.6 | 1 148 122 |
| Hispanic | 23.9 | 161 221 | 10.9 | 1 148 122 |
| Married | 48.4 | 164 805 | 60.6 | 1 176 407 |
| College | 16.6 | 163 491 | 44.2 | 1 173 981 |
| Any children | 54.6 | 164 927 | 38.7 | 1 184 418 |
Note. The general adult population includes the policy-eligible adult population.
TABLE 2—
Effects of the Affordable Care Act (ACA) Medicaid Expansion on Access to Health Care and Well-Being: Gallup-Sharecare Well-Being Index, United States, 2010–2016
| Policy-Eligible Adult Population |
General Adult Population |
|||
| Outcome | Effect (95% CI) | Preexpansion Mean | Effect (95% CI) | Preexpansion Mean |
| Access to health care | ||||
| Health insurance | 7.51 (5.24, 9.77) | 64.08 | 2.25 (0.88, 3.63) | 85.15 |
| Access to personal doctor | 3.48 (1.48, 5.48) | 65.91 | 1.18 (0.42, 1.95) | 80.82 |
| Difficulty affording health care | –3.71 (–6.20, –1.22) | 37.87 | –1.03 (–2.01, –0.06) | 17.16 |
| Well-being (on 0–100 scale) | ||||
| Current life satisfaction | 0.21 (–0.59, 1.01) | 61.41 | 0.18 (–0.13, 0.48) | 69.03 |
| Expected life satisfaction in 5 y | 0.08 (–0.82, 0.98) | 75.15 | –0.25 (–0.47, –0.03) | 78.30 |
| Worry | –0.06 (–1.70, 1.58) | 46.60 | 0.05 (–0.39, 0.49) | 33.44 |
| Sadness | –0.09 (–1.92, 1.74) | 30.29 | 0.10 (–0.25, 0.46) | 17.28 |
| Stress | –0.11 (–1.57, 1.36) | 52.94 | 0.17 (–0.30, 0.64) | 43.73 |
| Happiness | –0.76 (–1.91, 0.39) | 80.85 | 0.00 (–0.33, 0.34) | 88.11 |
Note. CI = confidence interval. This table shows the difference-in-differences estimates of the effect of the ACA Medicaid expansion on access to health care and subjective well-being. The sample excludes mild expansion states, as shown in the box on page 1238. All regressions control for age, race/ethnicity, education, gender, marital status, having any children in the household, and state and interview day fixed effects. The policy-eligible population is defined as reporting a family income below 138% of the federal poverty level (as defined according to 2016 thresholds determined by the US Census Bureau). The general adult population includes the policy-eligible adult population. All outcome means are rescaled to be out of 100 and calculated only for expansion states for the period 2010–2013, before the ACA Medicaid expansion took place. The minimum regression sample sizes for the policy-eligible and full general adult populations are 144 939 and 1 056 794, respectively. Estimated with ordinary least squares and SEs are clustered at the state level.
In both the policy-eligible and the general adult populations, we observed no meaningful changes in mean reported life satisfaction in the expansion states versus nonexpansion states following Medicaid expansion (Table 2). However, we observed a precisely estimated effect of an extremely small magnitude on expected life satisfaction in 5 years in the general population (–0.25 points of 100; 95% CI = –0.47, –0.03). However, this effect was not observed in the policy-eligible population. We observed no meaningful changes in mean reported measures of happiness, sadness, stress, or worry in the Medicaid expansion states versus nonexpansion states in either the policy-eligible population or the general population (Table 2).
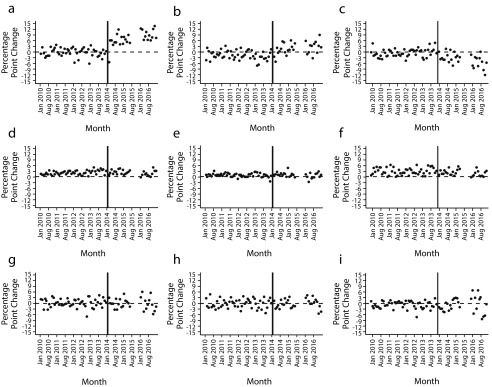
The results of the dynamic difference-in-differences analysis are shown in Figure 1. We observed no differential pre-Medicaid expansion trends in access to health care, life satisfaction, or emotional states in expansion versus nonexpansion states, consistent with the parallel trends assumption of the difference-in-differences analytic design. After Medicaid expansion, we observed statistically significant differential increases in reported access to a doctor and having health insurance and decreases in difficulty affording health care sustained over time in expansion states versus nonexpansion states (Figure 1). We did not observe any differential changes in the well-being outcomes after expansion. For ease of presentation, Figure 1 reports the results of the dynamic difference-in-differences models only for the policy-eligible population; the results for the general adult population were similar and are shown in Appendix A, Figure A.
FIGURE 1—
Month-to-Month Differences (Percentage Points) in Access to Health Care and Well-Being Between Medicaid Expansion States and Nonexpansion States in the Policy-Eligible Low-Income Population, by (a) Health Insurance, (b) Access to a Personal Doctor, (c) Financial Difficulty Affording Health Care, (d) Current Life Satisfaction, (e) Expected Life Satisfaction in 5 Years, (f) Happiness, (g) Worry, (h) Sadness, and (i) Stress: United States, 2010–2016
Heterogeneity of Policy Effects
In the policy-eligible population, we observed no heterogeneity in the association between Medicaid expansion and subjective well-being across population subgroups defined by gender, level of educational attainment, marital status, or number of children in the household (Appendix A, Tables A–F). We observed reduced life satisfaction and increased stress and worry in non-Hispanic Whites and, conversely, improved life satisfaction and reduced worry in non-Hispanic Blacks associated with the ACA Medicaid expansion, but these effects were of very small magnitude (Appendix A, Tables A–F). However, because of the number of simultaneous hypotheses we tested in this heterogeneity analysis, we interpret these statistically significant associations with caution.
Sensitivity Analyses
When the analyses were restricted to full and substantial Medicaid expansion states separately, the results were similar to the main analysis (Appendix A, Tables G and H).
DISCUSSION
Using the ACA Medicaid expansion in 2014 as a natural experiment in a difference-in-differences analysis of nationally representative data from 2010 to 2016, we observed that living in a state that expanded Medicaid was not associated with changes to subjective well-being either in the policy-eligible population or in the general adult population. We observed a very small decline in expected life satisfaction in 5 years’ time in the general adult population, which may have been a chance finding. The findings were consistent across a range of population subgroups and according to the degree of state-level Medicaid expansion.
Our results are consistent with previous studies that have documented health insurance coverage and health care access benefits of the ACA Medicaid expansion, which are outcomes that are seemingly relevant to well-being.3–7 We were also interested in whether the Medicaid expansion had a net spillover effect on general population well-being, as the ACA is a well-publicized expansion of the US social safety net that elicits strong responses across the political spectrum. However, in this nationally representative study of more than 1.6 million US adults from 2010 to 2016, we found no evidence of changes to well-being in either the policy-eligible low-income population or the general adult population following the ACA Medicaid expansion.
To the extent that people care about equity and the health care access of others in their state, we expected that subjective well-being, as captured by life satisfaction and emotional state, would improve in the general population. Positive community-level public health effects associated with the ACA Medicaid expansion—including reductions in crime, increased prescribing of opioid treatments, and reduced socioeconomic inequalities in access to health care—suggest the potential for positive effects of the policy beyond its direct effects on individual health insurance coverage.8–10
Although no other studies that we are aware of have investigated the effects of the ACA Medicaid expansion on dimensions of subjective well-being, evaluation of the 2008 Oregon Health Insurance Experiment found that reported happiness increased among those newly eligible for Medicaid after the first year,33 although the effect dissipated after 2 years.34 This finding contrasts with ours, which showed no changes in happiness in the US population following the ACA Medicaid expansion. However, our results are mostly consistent with those from other studies evaluating self-rated health following the expansion. Self-rated health captures aspects of subjective well-being in addition to being a robust indicator of physical health. Using data from the National Health Interview Surveys, the Gallup Well-Being Index, and the Behavioral Risk Factors Surveillance System, other studies also using a difference-in-differences design have found no effect7,11,13 or a very small positive effect12 of the expansion on self-rated health. The exception was 1 study that used survey data from Kentucky (full expansion), Arkansas (expansion of private insurance through the federal marketplace), and Texas (no expansion) and found a 5–percentage point increase in excellent self-rated health associated with expanded health insurance coverage in the former 2 states.14
These null results suggest that gaining access to health insurance has at most a negligible effect on life satisfaction and no impact on emotional states. The indicators of life satisfaction and emotional states that we used in this study are recommended by the Organisation for Economic Co-operation and Development for measuring subjective well-being in survey research.35 These indicators have shown sensitivity to external financial shocks, namely the 2008 financial crisis, whereby Deaton used data from the Gallup Well-Being Index to show that emotional states and life satisfaction worsened in the US population following the financial crisis.19
Newly gaining health insurance is presumably a less extreme and less instantaneous financial shock, to which life satisfaction and emotional states simply may not respond. We were unable to capture other dimensions of subjective well-being, including purpose in life, sense of belonging, locus of control, and other emotional states that are not assessed by Gallup. Additional research using robust, causal designs should investigate the effects of the ACA Medicaid expansion as well as other health policies on a diverse range of human well-being indicators. Future research should also replicate our results as more time passes since the ACA Medicaid expansion, assuming that it stays in place, as it may take time for individuals to become accustomed to the new range of health services available to them and to understand the broader societal implications of an expanded social safety net.
A limitation of this study is that we were not able to directly identify the individuals who were eligible to gain health insurance coverage through Medicaid expansion because Gallup collected household income information in categorical brackets. We identified household income by assigning respondents the midpoint of their reported household income bracket; this approach likely resulted in a degree of nondifferential misclassification of the policy-eligible population, which could bias our results, most likely toward the null. A main strength of this study is its extremely large and population-representative sample of US adults, with unique repeated cross-sectional data over a long follow-up that included comprehensive subjective well-being and other measures that are not available in any other nationally representative survey of the US population. We took advantage of exogeneous state-level Medicaid expansion as a natural experiment to assess the effects of Medicaid expansion on health care access and well-being in the adult US population.
As seemingly direct indicators of well-being, emotional state and life satisfaction measures appear useful for empirically assessing the human welfare implications of health policy interventions.19–21,27 However, this study puts into question whether these subjective well-being measures can be useful in drawing evaluative conclusions about health policies in the United States, as the ACA Medicaid expansion has generated many outcomes that policy analysts and researchers would consider to be beneficial to public health. These include higher rates of health insurance coverage, greater use of preventive health services, reduced use of emergency medical services, reduced financial difficulties, lower crime rates, and a narrowing of the socioeconomic gap in access to health care.3–10,14
This study contributes to this growing body of literature, demonstrating that although the ACA Medicaid expansion had meaningful effects on health insurance coverage and care access, its effects were not reflected in the emotional states or life satisfaction of the US adult population over the follow-up period that we examined. These results contribute to current discourse on the utility of subjective well-being measures for the evaluation of health policy and should be corroborated in the future as more time passes since the implementation of Medicaid expansion.
ACKNOWLEDGMENTS
This research was conducted while L. C. K. and O. A. were David E. Bell fellows and Y. T. was an Alfred P. Sloan Fellow on Aging and Work at the Harvard Center for Population and Development Studies.
We thank Gallup, for making their data available to us.
CONFLICTS OF INTEREST
L. F. B. has received financial support as a consulting senior scientist with Gallup.
HUMAN PARTICIPANT PROTECTION
As this was a secondary analysis of de-identified data, institutional review board approval was not required.
Footnotes
See also Galea and Vaughan, p. 1169.
REFERENCES
- 1.National Conference of State Legislatures. Affordable Care Act Medicaid expansion. 2018. Available at: http://www.ncsl.org/research/health/affordable-care-act-expansion.aspx. Accessed January 2, 2019.
- 2.O’Neill TH. How many are newly insured as a result of the ACA? 2017. Available at: https://www.americanactionforum.org/insight/20-million. Accessed January 2, 2019.
- 3.Sommers BD, Blendon RJ, Orav EJ, Epstein AM. Changes in utilization and health among low-income adults after Medicaid expansion or expanded private insurance. JAMA Intern Med. 2016;176(10):1501–1509. doi: 10.1001/jamainternmed.2016.4419. [DOI] [PubMed] [Google Scholar]
- 4.Sommers BD, Gawande AA, Baicker K. Health insurance coverage and health—what the recent evidence tells us. N Engl J Med. 2017;377(6):586–593. doi: 10.1056/NEJMsb1706645. [DOI] [PubMed] [Google Scholar]
- 5.Antonisse L, Garfield R, Rudowitz R, Artiga S. The effects of Medicaid expansion under the ACA: updated findings from a literature review. 2018. Available at: https://www.kff.org/medicaid/issue-brief/the-effects-of-medicaid-expansion-under-the-aca-updated-findings-from-a-literature-review-march-2018. Accessed January 2, 2019.
- 6.Hu L, Kaestner R, Mazumder B, Miller S, Wong A. The effect of the Patient Protection and Affordable Care Act Medicaid expansions on financial wellbeing. J Public Econ. 2018;163:99–112. doi: 10.1016/j.jpubeco.2018.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sommers BD, Gunja MZ, Finegold K, Musco T. Changes in self-reported insurance coverage, access to care, and health under the Affordable Care Act. JAMA. 2015;314(4):366–374. doi: 10.1001/jama.2015.8421. [DOI] [PubMed] [Google Scholar]
- 8.Vogler J. Access to health care and criminal behavior: short-run evidence from the ACA Medicaid expansions. 2018. Available at: https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3042267. Accessed January 2, 2019.
- 9.Griffith K, Evans L, Bor J. The Affordable Care Act reduced socioeconomic disparities in health care access. Health Aff (Millwood) 2017;36(8):1503–1510. doi: 10.1377/hlthaff.2017.0083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sharp A, Jones A, Sherwood J, Kutsa O, Honermann B, Milett G. Impact of Medicaid expansion on access to opioid analgesic medications and medication-assisted treatment. Am J Public Health. 2018;108(5):642–648. doi: 10.2105/AJPH.2018.304338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Courtemanche C, Marton J, Ukert B, Yelowitz A, Zapata D. Early Effects of the Affordable Care Act on Health Care Access, Risky Health Behaviors, and Self-Assessed Health. Cambridge, MA: National Bureau of Economic Research; 2017. NBER Working Paper Series, no. 23269. [Google Scholar]
- 12.Simon K, Soni A, Cawley J. The impact of health insurance on preventive care and health behaviors: evidence from the 2014 ACA Medicaid expansions. J Policy Anal Manage. 2017;36(2):390–417. doi: 10.1002/pam.21972. [DOI] [PubMed] [Google Scholar]
- 13.Miller S, Wherry LR. Health and access to care during the first 2 years of the ACA Medicaid expansions. N Engl J Med. 2017;376(10):947–956. doi: 10.1056/NEJMsa1612890. [DOI] [PubMed] [Google Scholar]
- 14.Sommers BD, Maylone B, Blendon RJ, John Orav E, Epstein AM. Three-year impacts of the affordable care act: improved medical care and health among low-income adults. Health Aff (Millwood) 2017;36(6):1119–1128. doi: 10.1377/hlthaff.2017.0293. [DOI] [PubMed] [Google Scholar]
- 15.Diener E. Guidelines for national indicators of subjective well-being and ill-being. J Happiness Stud. 2006;7(4):397–404. [Google Scholar]
- 16.Diener E, Tay L. Subjective well-being and human welfare around the world as reflected in the Gallup World Poll. Int J Psychol. 2015;50(2):135–149. doi: 10.1002/ijop.12136. [DOI] [PubMed] [Google Scholar]
- 17.Dolan P, White MP. How can measures of subjective well-being be used to inform public policy? Perspect Psychol Sci. 2007;2(1):71–85. doi: 10.1111/j.1745-6916.2007.00030.x. [DOI] [PubMed] [Google Scholar]
- 18.Stiglitz JE, Sen A, Fitoussi J-P. Report by the Commission on the Measurement of Economic and Social Progress. Paris: France; 2009. Commission on the Measurement of Economic and Social Progress. [Google Scholar]
- 19.Deaton AS. The Financial Crisis and the Well-Being of Americans. Cambridge, MA: National Bureau of Economic Research; 2011. NBER Working Paper Series, no. 17128. [Google Scholar]
- 20.Aghion P, Akcigit U, Deaton A, Roulet A. Creative destruction and subjective well-being. Am Econ Rev. 2016;106(12):3869–3897. doi: 10.1257/aer.20150338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lachowska M. The effect of income on subjective well-being: evidence from the 2008 economic stimulus tax rebates. J Hum Resour. 2017;52(2):374–417. [Google Scholar]
- 22.Idler EL, Benyamini Y. Self-rated health and mortality: a review of twenty-seven community studies. J Health Soc Behav. 1997;38(1):21–37. [PubMed] [Google Scholar]
- 23.Ortega FB, Lee D, Sui X et al. Psychological well-being, cardiorespiratory fitness, and long-term survival. Am J Prev Med. 2010;39(5):440–448. doi: 10.1016/j.amepre.2010.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Steptoe A, Shankar A, Demakakos P, Wardle J. Social isolation, loneliness, and all-cause mortality in older men and women. Proc Natl Acad Sci USA. 2013;110(15):5797–5801. doi: 10.1073/pnas.1219686110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chida Y, Steptoe A. Positive psychological well-being and mortality: a quantitative review of prospective observational studies. Psychosom Med. 2008;70(7):741–756. doi: 10.1097/PSY.0b013e31818105ba. [DOI] [PubMed] [Google Scholar]
- 26.Boehm JK, Chen Y, Williams DR, Ryff CD, Kubzansky LD. Subjective well-being and cardiometabolic health: an 8–11 year study of midlife adults. J Psychosom Res. 2016;85:1–8. doi: 10.1016/j.jpsychores.2016.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gruber JH, Mullainathan S. Do cigarette taxes make smokers happier. In: Ng Y, Ho L, editors. Happiness and Public Policy: Theory, Case Studies, and Implications. London, England: Palgrave Macmillan; 2006. pp. 109–146. [Google Scholar]
- 28.Kaiser Family Foundation. Kaiser Health Tracking Poll: the public’s views on the ACA. 2019. Available at: https://www.kff.org/interactive/kaiser-health-tracking-poll-the-publics-views-on-the-aca. Accessed January 2, 2019. [Google Scholar]
- 29.Gallup. How does the Gallup Sharecare Well-Being Index work? 2017. Available at: http://www.gallup.com/175196/gallup-healthways-index-methodology.aspx. Accessed January 2, 2019.
- 30.Bishaw A, Benson C Poverty: 2016 and 2017. 2018. American Community Survey Briefs. Available at: https://www.census.gov/content/dam/Census/library/publications/2018/acs/acsbr17-02.pdf. Accessed January 2, 2019. [Google Scholar]
- 31.Dimick JB, Ryan AM. Methods for evaluating changes in health care policy: the difference-in-differences approach. JAMA. 2014;312(22):2401–2402. doi: 10.1001/jama.2014.16153. [DOI] [PubMed] [Google Scholar]
- 32.Gallup. Understanding how Gallup uses the Cantril Scale. Available at: http://news.gallup.com/poll/122453/understanding-gallup-uses-cantril-scale.aspx. Accessed January 2, 2019.
- 33.Finkelstein AN, Taubman SL, Wright BJ et al. The Oregon health insurance experiment: evidence from the first year. Q J Econ. 2012;127(3):1057–1106. doi: 10.1093/qje/qjs020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Baicker K, Taubman SL, Allen HL et al. The Oregon experiment—effects of Medicaid on clinical outcomes. N Engl J Med. 2013;368(18):1713–1722. doi: 10.1056/NEJMsa1212321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Organisation for Economic Co-operation and Development. OECD Guidelines on Measuring Subjective Well-Being. Paris: OECD Publishing; 2013. Available at: https://www.oecd.org/statistics/oecd-guidelines-on-measuring-subjective-well-being-9789264191655-en.htm. Accessed June 25, 2019. [PubMed] [Google Scholar]