Abstract
Objectives. To estimate the population-level frequencies and standardized rates of sexual assault cases in the province of Ontario, Canada.
Methods. We conducted a 15-year retrospective analysis (2002–2016) of sexual assault cases by linking 5 provincial administrative health databases. We defined sexual assault by an algorithm of 23 International Classification of Diseases, 10th Revision, and physician billing codes. We calculated age- and sex-stratified standardized rates per 100 000 census population, and we used age- and sex-stratified Poisson regressions to determine annual rate ratios.
Results. Between 2002 and 2016, there were 52 780 incident cases of sexual assault in Ontario at a rate of 27.38 per 100 000 population. The highest rates were found among females aged 15 to 19 years (187 per 100 000) and 20 to 24 years (127 per 100 000). Among males, the highest rates were observed among children aged 0 to 4 years (41 per 100 000) and 5 to 9 years (29 per 10 000). Among males and females, the annual rate ratio increased among those aged 15 years and older and decreased among those aged 14 years and younger.
Conclusions. Sexual assault was documented across all age groups and sexes, from children to elders, with high standardized rates among adolescents and children.
Sexual assault and gender-based violence is a pervasive phenomenon affecting people of all ages and sexes or genders. Globally, it has been estimated that approximately 33% of women have experienced sexual abuse from an intimate partner1 and 7% have been abused by nonpartners including strangers, friends, teachers, neighbors, or family members.2 Having reliable and consistent measures of sexual violence is a priority for monitoring trends over time and making comparisons across settings and populations. However, documenting the magnitude of sexual violence is methodologically challenging. The Global Status Report on Violence Prevention by the World Health Organization (WHO) reported that out of 133 countries with national action plans to address sexual violence, only 52% have regular data collection systems to monitor prevalence and inform action.1 Accurate documentation of the burden of sexual violence is a prerequisite for better allocation of health resources and services for survivors and is required to address the existing knowledge gap surrounding sexual violence within our population and across age and sex.3
Data from the National Intimate Partner and Sexual Violence Survey found that, within the United States, 19.3% of women and 1.7% of men have been raped or sexually assaulted during their lifetime, and an estimated 43.9% of women and 23.4% of men have experienced other forms of sexual violence (e.g., unwanted sexual contact or being forced to penetrate another person).4 Global estimates from a large meta-analysis of 65 studies from 22 countries found that 7.9% of males and 19.7% of females faced sexual abuse before the age of 18 years.5 There is also a growing recognition of the prevalence of elder abuse6,7; however, there is less information on sexual abuse within elderly populations. Information from the Canadian General Social Survey estimated that the sexual victimization rate in Canada was 24 per 1000 inhabitants, with 70% of the sexual assaults perpetrated against women.8 Women and girls are consistently documented as having the highest estimates of sexual and gender-based violence; however, sexual violence against men remains a neglected issue and the inclusion of men and boys in the investigation of gendered violence is needed.
Measuring the volume of sexual assault cases presenting to the health care system is an important but relatively unexplored source of routine information.9 Sexual violence often does not fit discretely into standardized health coding systems such as the International Classification of Diseases, Tenth Revision (ICD-10; Geneva, Switzerland: World Health Organization; 1992), particularly if there are not visible injuries, as sexual assault can often occur in the absence of injury.10 Because of the well-documented underascertainment of violence, many studies that use health care administrative data create a composite outcome to capture the broad categories of intimate partner violence or domestic violence, which can capture physical, sexual, emotional, and financial abuse, as well as maltreatment or neglect.10–14 These studies have the advantage of capturing a broad range of abuse, but are perpetrator-specific, often female survivor–focused and restricted to those experiencing violence from a spouse or current or former intimate partner.10,11,13–15 The majority of child abuse research reports on both male and female children; however, many studies either use a composite outcome or focus specifically on physical abuse and neglect with less information on sexual abuse.16–20 The majority of sexual assault studies that use health care data are cross-sectional, and few studies have used a longitudinal design to investigate changes over time.17
Given the relatively limited information on sexual assault from the health care perspective, and even less measuring changes over time, we designed this study to use multiple routinely collected administrative health care databases to explore population-level patterns of sexual assault across all ages and sexes. The overarching goal was to create a comprehensive case definition using all accessible health care databases that can be shared and used to maximize comparability of estimates across settings. The specific objectives of this study were to (1) estimate the frequency of sexual assault cases by using routinely collected administrative health care databases, (2) document sociodemographic characteristics of sexual assault cases, (3) calculate age- and sex-stratified standardized rates, and (4) investigate time trends between 2002 and 2016.
METHODS
We performed a retrospective population-level study investigating patterns of sexual assault in the province of Ontario between 2002 and 2016. Ontario is the largest province in Canada with a resident population of 13.45 million, accounting for more than 38% of the Canadian population.21 The province is larger than 900 000 square kilometers with 75% of the population living in urban centers (≥ 100 000 population).
We sourced data from routinely collected administrative health care databases held at ICES (Toronto, Ontario), a provincial repository of health-related data collected across Ontario. ICES is an independent, nonprofit research institute funded by the Ontario Ministry of Health and Long-Term Care. ICES is authorized to collect and use health care data for the purposes of health system analyses, evaluation, and decision support. Secure access to the data is governed by policies and procedures that are approved by the Information and Privacy Commissioner of Ontario.
Data Sources
We used 5 linked databases in this analysis: the National Ambulatory Care Reporting Systems (NACRS), the Canadian Institute of Health and Information—Discharge Abstracts Database (DAD), the Registered Persons Database, the Ontario Health Insurance Plan (OHIP), and the Canadian Census data (2011). We removed all direct personal identifiers during analyses. These data sets were linked by using unique encoded identifiers and analyzed at ICES.
NACRS is an annually updated national database containing information on emergency and ambulatory care visits. In all, 180 hospitals across the province are required to submit data. DAD contains acute patient-level hospitalization in Ontario. Both NACRS and DAD use the ICD-10 coding system, the ICD-10 Canadian coding standards, and the Canadian Classification of Health Interventions. The Registered Persons Database contains information regarding patient demographics including postal code, sex, birth date, and death date. Ontario has a single-payer universal health insurance plan (OHIP) through which most hospital and physician services are insured. OHIP billing codes contain information regarding physician visits, diagnoses, and procedures. We used the Canadian Census postal code conversion file to link patient postal codes to population-level demographic characteristics and population denominators. We used the 2011 Census data because the most recent census (2016) was not available at the time of analyses.
Outcome Measures
The unit of analysis was each unique case of sexual assault. Individuals experiencing multiple sexual assaults contributed an additional data point for each subsequent sexual assault. We excluded all cases occurring within 30 days of the index sexual assault to ensure that follow-up care or duplicate coding within multiple databases was not misclassified as a new event.
We identified sexual assault cases by any ICD-10 or OHIP codes displayed in Table 1. We included diagnosis code T74.2 (sexual abuse) and external cause code of injury Y05 (sexual assault by bodily force). We used 5 examination codes (Z codes) to identify examination and observation following alleged rape and seduction (Z04.4, Z04.5, Z04.51) and problems related to alleged sexual abuse of children (Z61.4, Z61.5). To improve case ascertainment for childhood sexual abuse, we included a previously validated algorithm of 16 ICD-10 codes for suspected child sexual abuse.22 The algorithm included diagnoses of sexually transmitted infections and genital injuries in children younger than 10 years, including genital herpes, gonococcal infection, pelvic inflammatory disease, or contusion of genital organs. The full list is included in Appendix A (available as a supplement to the online version of this article at http://www.ajph.org). Within the OHIP database, we included 2 physician billing codes used for sexual assault examination for females (K018) and males (K021).
TABLE 1—
Data Sources and Codes Identifying Sexual Assault Cases: Ontario, Canada, 2002–2016 (n = 52 780)
| Data Sources and Codes | Total No. (%) | Females, No. (%) | Males, No. (%) |
| Discharge Abstract Database (DAD; n = 2362; 4.4% of cases) | |||
| T74.2: sexual abuse | 274 (0.5) | 254 (0.6) | 20 (0.3) |
| Y05: sexual assault by bodily force | 400 (0.8) | 368 (0.8) | 32 (0.5) |
| Z04.4: examination and observation following alleged rape and seduction | 119 (0.2) | . . . | . . . |
| Z04.5: examination and observation following alleged adult sexual and physical abuse | 102 (0.2) | 90 (0.2) | 12 (0.2) |
| Z04.51: examination and observation following alleged child sexual and physical abuse | 379 (0.7) | 190 (0.4) | 189 (2.7) |
| Z61.4: problems related to alleged sexual abuse of child by person within primary support group | 700 (1.3) | 615 (1.3) | 85 (1.2) |
| Z61.5: problems related to alleged sexual abuse of child by person outside primary support group | 550 (1.0) | 465 (1.0) | 85 (1.2) |
| Suspected ICD-10 codes for childhood sexual assaulta | 83 (0.2) | 36 (0.1) | 47 (0.7) |
| National Ambulatory Care Reporting System (NACRS; n = 49 727; 94.2% of cases) | |||
| T74.2: sexual abuse | 7 178 (13.6) | 6 850 (15.0) | 328 (4.6) |
| Y05: sexual assault by bodily force | 12 276 (23.3) | 11 362 (24.9) | 914 (12.9) |
| Z04.4: examination and observation following alleged rape and seduction | 17 510 (33.2) | 16 731 (36.6) | 779 (11.0) |
| Z04.5 examination and observation following alleged adult sexual and physical abuse | 9 664 (18.3) | 9 006 (19.7) | 658 (9.3) |
| Z04.51: examination and observation following alleged child sexual and physical abuse | 8 693 (16.5) | 6 343 (13.9) | 2 350 (33.1) |
| Z61.4: problems related to alleged sexual abuse of child by person within primary support group | 1 427 (2.7) | 1 093 (2.4) | 334 (4.7) |
| Z61.5: Problems related to alleged sexual abuse of child by person outside primary support group | 785 (1.5) | 569 (1.2) | 216 (3.0) |
| Suspected ICD-10 codes for childhood sexual assaulta | 2 454 (4.6) | 1 101 (2.4) | 1 353 (19.1) |
| Ontario Health Insurance Plan (OHIP; n = 4542; 8.6% of cases) | |||
| K018: sexual assault examination—female | 4 129 (7.8) | . . . | . . . |
| K021: sexual assault examination—male | 413 (0.8) | . . . | . . . |
| Data source overlap | |||
| DAD only | 1 853 (3.5) | 1 495 (3.3) | 358 (5.0) |
| DAD and NACRS | 450 (0.9) | 348 (0.8) | 102 (1.4) |
| DAD and NACRS and OHIP | 45 (0.1) | . . . | . . . |
| DAD and OHIP | 14 (0.0) | . . . | . . . |
| NACRS only | 45 935 (87.0) | 39 718 (86.9) | 6 217 (87.6) |
| NACRS and OHIP | 3 297 (6.2) | 3 133 (6.9) | 164 (2.3) |
| OHIP only | 1 186 (2.2) | 934 (2.0) | 252 (3.6) |
Note. ICD-10 = International Classification of Diseases, Tenth Revision (Geneva, Switzerland: World Health Organization; 1992). Row percentages do not total 100% as individuals can have multiple codes and be in multiple databases. Ellipses denote cells suppressed due to small cell sizes < 5.
List of suspected codes presented in Appendix A (available as a supplement to the online version of this article at http://www.ajph.org).
Covariables
Patient-level information included sex (female vs male) and age, measured both continuously and by 5-year increments. We used 3 variables to investigate patterns on the timing of the assault, including the year, month, day of the week, and whether the assault took place during a public holiday (i.e., New Year’s Day, Family Day, Good Friday, Easter [Sunday], Victoria Day, Canada Day, Canada Day Observed, August Long Weekend, Labor Day, Thanksgiving, Christmas, Boxing Day).
Health care–based variables included facility presentation comparing outpatient clinic to hospitals. We defined revictimization as having 2 or more unique sexual assaults within the same fiscal year that were separated by more than 30 days to avoid duplication and coding assigned during follow-up visits.
We extracted 3 sociodemographic variables from the Canadian Census by using the Postal CodeOM Conversion File (release date June 2017), an SAS program (SAS Institute, Cary, NC) that converts 6-digit postal codes into census tracts (approximately 4000 dwellings).23 Community size quintile measured population density, ranging from more than 1.5 million to less than 10 000 per census tract. Neighborhood income quintile measured socioeconomic status. The Local Health Integrated Network is an Ontario-based variable that identifies the geographic location and responsible health authority and is included in Appendix B and C (available as supplements to the online version of this article at http://www.ajph.org).
Statistical Analyses
We conducted all analyses with SAS version 9.4 (SAS Institute, Cary, NC). We calculated and sex-stratified both the 15-year amalgamated total and the annual number of sexual assault cases between 2002 and 2016. In accordance with privacy guidelines, we suppressed any cell sizes less than 5 to ensure nonidentification. Descriptive statistics included frequencies and percentages for categorical variables. We measured continuous variables with medians and interquartile ranges (IQRs).
We calculated the annual rate by taking the 15-year median stratified by age and sex. We standardized the counts to the Ontario 2011 Canadian Census Standard Population with a 100 000 multiplier. We calculated and plotted the overall rate (age- and sex-standardized) and the age-standardized rates for females and males for each study year. For the purposes of the plot, we calculated the age-standardized rates based on 10-year age groups and truncated at 60 or older to prevent sparse strata.
We developed Poisson regression models to calculate the rate ratio (RR) and 95% confidence interval (CI) for each age group and sex across the 15-year study period. We counted anyone living in Ontario with a valid health card that was alive on July 1 of each respective fiscal year to be eligible in the denominator. We fit stratified Poisson regression models for every age group and sex combination with the number of sexual assault cases as the outcome, the natural log of the number of eligible Ontarians yearly as the offset term, and the fiscal year as the exposure. We included year of sexual assault as a continuous variable. We calculated the annual percent change with the formula RR–1.
RESULTS
Between 2002 and 2016, there were 52 780 unique cases of sexual assault. Table 1 displays the distribution of code frequencies per database. The highest volume of cases, 49 727 (94.2%), was captured through emergency department visits in the NACRS Ambulatory Care database, 4542 (8.6%) through OHIP physician billing codes, and 2362 (4.4%) through hospital admissions (DAD). Only 3806 (7.2%) cases were captured in more than 1 database. The most commonly assigned ICD-10 code was Z04.4 (examination and observation following alleged rape and seduction), which identified 17 510 (33.2%) cases in NACRS and 119 (0.2%) in DAD. The external cause code, Y05 (sexual assault by bodily force), identified 12 276 (23.3%) cases in NACRS and 400 (0.8%) in DAD. The suspected child sexual abuse codes identified an additional 2454 (4.6%) cases in NACRS and 83 (0.2%) in DAD.
The demographic characteristics of sexual assault cases are displayed in Table 2. Out of all the sexual assault cases, the majority of cases were among female patients (86.6%); however, 7094 (13.4%) cases of sexual assault among males were identified. The overall median age was 19 years (IQR = 14–29). The highest frequency of sexual assault among females occurred to those aged 15 to 19 years (25.9%), 20 to 24 years (17.7%), and 25 to 29 years (10.2%). Among males, the highest frequency of sexual assault occurred to those aged 0 to 4 years (31.8%) and 5 to 9 years (22.7%). Of note, there were 896 cases of elder sexual assault among patients aged 60 years and older.
TABLE 2—
Demographic and Descriptive Characteristics of Sexual Assault Cases: Ontario, Canada, 2002–2016
| Variables | Total (n = 52 780), Median (IQR) or No. (%) | Female (n = 45 686), Median (IQR) or No. (%) | Male (n = 7094), Median (IQR) or No. (%) |
| Age at time of sexual assault, y | 19 (14–29) | 20 (15–29) | 8 (3–24) |
| 0–4 | 6 122 (11.6) | 3 863 (8.5) | 2 259 (31.8) |
| 5–9 | 4 127 (7.8) | 2 518 (5.5) | 1 609 (22.7) |
| 10–14 | 3 889 (7.4) | 3 422 (7.5) | 467 (6.6) |
| 15–19 | 12 379 (23.5) | 11 829 (25.9) | 550 (7.8) |
| 20–24 | 8 570 (16.2) | 8 069 (17.7) | 501 (7.1) |
| 25–29 | 5 036 (9.5) | 4 641 (10.2) | 395 (5.6) |
| 30–34 | 3 501 (6.6) | 3 233 (7.1) | 268 (3.8) |
| 35–39 | 2 686 (5.1) | 2 448 (5.4) | 238 (3.4) |
| 40–44 | 2 332 (4.4) | 2 098 (4.6) | 234 (3.3) |
| 45–49 | 1 727 (3.3) | 1 530 (3.3) | 197 (2.8) |
| 50–54 | 990 (1.9) | 885 (1.9) | 105 (1.5) |
| 55–59 | 525 (1.0) | 454 (1.0) | 71 (1.0) |
| 60–64 | 272 (0.5) | 217 (0.5) | 55 (0.8) |
| 65–69 | 158 (0.3) | 128 (0.3) | 30 (0.4) |
| ≥ 70 | 466 (0.9) | 351 (0.8) | 115 (1.6) |
| Year | 3 449 (3 329–3 734) | 3 017 (2 872–3 257) | 478 (417–512) |
| 2002 | 3 347 (6.3) | 2 787 (6.1) | 560 (7.9) |
| 2003 | 3 311 (6.3) | 2 787 (6.1) | 524 (7.4) |
| 2004 | 3 355 (6.4) | 2 872 (6.3) | 483 (6.8) |
| 2005 | 3 529 (6.7) | 3 041 (6.7) | 488 (6.9) |
| 2006 | 3 229 (6.1) | 2 850 (6.2) | 379 (5.3) |
| 2007 | 3 329 (6.3) | 2 936 (6.4) | 393 (5.5) |
| 2008 | 3 449 (6.5) | 2 997 (6.6) | 452 (6.4) |
| 2009 | 3 294 (6.2) | 2 877 (6.3) | 417 (5.9) |
| 2010 | 3 420 (6.5) | 3 017 (6.6) | 403 (5.7) |
| 2011 | 3 804 (7.2) | 3 317 (7.3) | 487 (6.9) |
| 2012 | 3 842 (7.3) | 3 272 (7.2) | 570 (8.0) |
| 2013 | 3 615 (6.8) | 3 103 (6.8) | 512 (7.2) |
| 2014 | 3 564 (6.8) | 3 093 (6.8) | 471 (6.6) |
| 2015 | 3 734 (7.1) | 3 257 (7.1) | 477 (6.7) |
| 2016 | 3 958 (7.5) | 3 480 (7.6) | 478 (6.7) |
| Month | |||
| April | 4 111 (7.8) | 3 552 (7.8) | 559 (7.9) |
| May | 4 612 (8.7) | 3 924 (8.6) | 688 (9.7) |
| June | 4 741 (9.0) | 4 111 (9.0) | 630 (8.9) |
| July | 5 058 (9.6) | 4 376 (9.6) | 682 (9.6) |
| August | 5 074 (9.6) | 4 423 (9.7) | 651 (9.2) |
| September | 4 643 (8.8) | 4 069 (8.9) | 574 (8.1) |
| October | 4 474 (8.5) | 3 883 (8.5) | 591 (8.3) |
| November | 4 247 (8.0) | 3 679 (8.1) | 568 (8.0) |
| December | 3 760 (7.1) | 3 217 (7.0) | 543 (7.7) |
| January | 4 048 (7.7) | 3 483 (7.6) | 565 (8.0) |
| February | 3 712 (7.0) | 3 198 (7.0) | 514 (7.2) |
| March | 4 300 (8.1) | 3 771 (8.3) | 529 (7.5) |
| Weekday | |||
| Saturday | 8 946 (16.9) | 7 966 (17.4) | 980 (13.8) |
| Sunday | 8 029 (15.2) | 6 963 (15.2) | 1 066 (15.0) |
| Monday | 7 194 (13.6) | 6 202 (13.6) | 992 (14.0) |
| Tuesday | 6 669 (12.6) | 5 670 (12.4) | 999 (14.1) |
| Wednesday | 6 730 (12.8) | 5 717 (12.5) | 1 013 (14.3) |
| Thursday | 7 229 (13.7) | 6 141 (13.4) | 1 088 (15.3) |
| Friday | 7 983 (15.1) | 7 027 (15.4) | 956 (13.5) |
| Holiday | |||
| No | 51 195 (97.0) | 44 273 (96.9) | 6 922 (97.6) |
| Yes | 1 585 (3.0) | 1 413 (3.1) | 172 (2.4) |
| Facility presentation | |||
| Outpatient clinic | 4 542 (8.6) | 4 125 (9.0) | 417 (5.9) |
| Hospital | 48 238 (91.4) | 41 561 (91.0) | 6 677 (94.1) |
| Revictimization within 1 y | |||
| Single sexual assault | 51 322 (97.2) | 44 328 (97.0) | 6 994 (98.6) |
| Multiple sexual assaults | 1 458 (2.8) | 1 385 (3.0) | 100 (1.4) |
| Community size (population) | |||
| ≥ 1 500 000 | 14 198 (26.9) | 12 286 (26.9) | 1 912 (27.0) |
| 500 000–1 499 999 | 7 538 (14.3) | 6 525 (14.3) | 1 013 (14.3) |
| 100 000–499 999 | 16 178 (30.7) | 14 317 (31.3) | 1 861 (26.2) |
| 10 000–99 999 | 6 394 (12.1) | 5 374 (11.8) | 1 020 (14.4) |
| < 10 000 | 8 256 (15.6) | 7 017 (15.4) | 1 239 (17.5) |
| Missing | 216 (0.4) | 167 (0.4) | 49 (0.7) |
| Neighborhood income quintile | |||
| Lowest | 17 607 (33.4) | 15 354 (33.6) | 2 253 (31.8) |
| Medium–low | 11 035 (20.9) | 9 474 (20.7) | 1 561 (22.0) |
| Middle | 8 736 (16.6) | 7 553 (16.5) | 1 183 (16.7) |
| Medium–high | 7 703 (14.6) | 6 684 (14.6) | 1 019 (14.4) |
| Highest | 6 912 (13.1) | 5 953 (13.0) | 959 (13.5) |
| Missing | 787 (1.5) | 668 (1.5) | 119 (1.7) |
Note. IQR = interquartile range. Sample size was n = 52 780.
The majority of identified cases, 48 238 (91.94%), presented to hospital emergency departments while 4542 (8.6%) sought care from outpatient clinics. There were 1458 revictimization cases, with some being revictimized more than 6 times in a fiscal year. We observed a gradient effect by income quintile, with the highest frequency of sexual assault cases seen in the lowest-income quintile (33.4%) and the fewest in the highest-income quintile (13.1%).
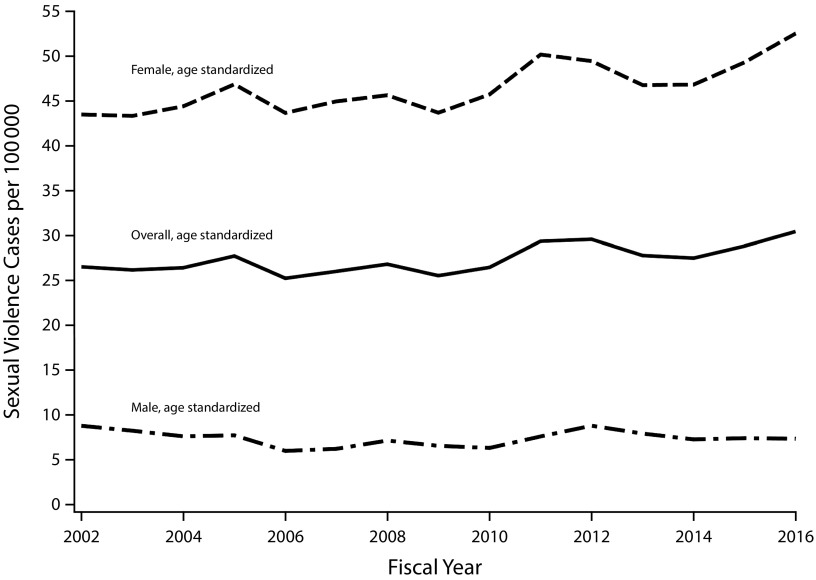
Table 3 displays the age- and sex-stratified standardized rates per 100 000 population. The total annual rate was 27.38 per 100 000, with 46.23 among females and 7.55 among males. Among females, the highest rates were in those aged 15 to 19 years (187.78 per 100 000) and 20 to 24 years (127.96 per 100 000). Among males, the highest rates were among children aged 0 to 4 years (41.76 per 100 000) and 5 to 9 years (29.37 per 100 000). Figure 1 displays the standardized rates per fiscal year including the total rate (age- and sex-standardized) and the sex-disaggregated rates (age-standardized) for males and females.
TABLE 3—
Age- and Sex-Stratified Standardized Rates of Sexual Assault and Poisson Regression Models: Ontario, Canada, 2002–2016
| Standardized Rates per 100 000a |
Females |
Males |
|||||
| Age, Years | Females | Males | Total | RRb (95% CI) | Annual % Change (95% CI) | RRb (95% CI) | Annual % Change (95% CI) |
| 0–4 | 74.94 | 41.76 | 57.95 | 0.98 (0.97, 0.98) | −2.40 (−3.11, −1.68) | 0.98 (0.97, 0.99) | −1.79 (−2.73, −0.85) |
| 5–9 | 48.31 | 29.37 | 38.60 | 0.99 (0.98, 1.00) | −1.28 (−2.16, −0.39) | 0.95 (0.94, 0.97) | −4.52 (−5.60, −3.43) |
| 10–14 | 61.31 | 7.95 | 33.95 | 0.97 (0.97, 0.98) | −2.57 (−3.33, −1.80) | 0.98 (0.96, 1.00) | −2.12 (−4.17, −0.03) |
| 15–19 | 187.78 | 8.26 | 95.56 | 1.01 (1.00, 1.01) | 0.79 (0.37, 1.22) | 1.01 (0.99, 1.02) | 1.01 (−0.95, 3.01) |
| 20–24 | 127.96 | 7.72 | 66.99 | 1.02 (1.01, 1.03) | 1.99 (1.47, 2.51) | 1.05 (1.03, 1.07) | 5.09 (2.93, 7.30) |
| 25–29 | 74.54 | 6.58 | 41.19 | 1.02 (1.01, 1.03) | 1.83 (1.15, 2.51) | 1.04 (1.02, 1.06) | 3.92 (1.54, 6.34) |
| 30–34 | 51.68 | 4.66 | 29.16 | 1.03 (1.03, 1.04) | 3.39 (2.56, 4.21) | 1.02 (0.99, 1.05) | 1.81 (−0.94, 4.64) |
| 35–39 | 37.22 | 3.91 | 21.21 | 1.02 (1.01, 1.03) | 1.86 (0.94, 2.80) | 1.04 (1.01, 1.07) | 3.59 (0.60, 6.66) |
| 40–44 | 29.37 | 3.48 | 16.82 | 1.02 (1.01, 1.03) | 1.92 (0.91, 2.94) | 1.05 (1.02, 1.08) | 4.93 (1.83, 8.12) |
| 45–49 | 18.95 | 2.54 | 10.90 | 1.03 (1.01, 1.04) | 2.66 (1.45, 3.89) | 1.09 (1.05, 1.13) | 8.86 (5.18, 12.67) |
| 50–54 | 11.49 | 1.42 | 6.56 | 1.06 (1.04, 1.08) | 5.97 (4.30, 7.67) | 1.06 (1.01, 1.11) | 5.65 (0.89, 10.64) |
| 55–59 | 6.79 | 1.13 | 4.05 | 1.04 (1.02, 1.07) | 4.35 (2.08, 6.66) | 1.04 (0.98, 1.10) | 3.99 (−1.60, 9.89) |
| 60–64 | 3.66 | 0.99 | 2.37 | 1.04 (1.00, 1.07) | 3.73 (0.45, 7.12) | 1.02 (0.95, 1.09) | 2.03 (−4.62, 9.14) |
| 65–69 | 2.92 | 0.74 | 1.87 | 1.01 (0.97, 1.05) | 0.83 (−3.14, 4.95) | 0.97 (0.87, 1.09) | −3.02 (−13.34, 8.53) |
| ≥ 70 | 3.11 | 1.36 | 2.36 | 1.02 (1.00, 1.05) | 2.48 (0.01, 5.01) | 1.06 (1.02, 1.11) | 6.29 (1.71, 11.08) |
| Total | 46.23 | 7.55 | 27.38 | 1.00 (1.00, 1.01) | 0.31 (0.10, 0.52) | 0.99 (0.99, 1.00) | −0.97 (−1.50, −0.43) |
Note. CI = confidence interval; RR = rate ratio.
With 2011 Census population data.
Interpretation: rate change for each additional year.
FIGURE 1—
Standardized Rates of Sexual Assault Longitudinally: Ontario, Canada, 2002–2016
From the Poisson regression models in Table 3, the annual RR for sexual assault among females overall was 1.00 (95% CI = 1.00, 1.01) with a 0.31% (95% CI = 0.10, 0.52) increase per year. Within the age strata, the annual rate increased among females aged 15 years and older and decreased among females aged 14 years and younger. The annual RR for sexual assault among males overall was 0.99 (95% CI = 0.99, 1.00) with −0.97% (95% CI = –1.50, –0.43) decrease per year. Within age strata, the annual rate increased slightly among males aged 15 years and older and decreased slightly among males aged 14 years and younger.
DISCUSSION
Using a combination of ICD-10 codes and physician billing codes, we identified more than 52 000 sexual assault cases seen by the Ontario health care system between 2002 and 2016, with an annual average of 3519 cases per year. The overall rate of sexual assault was 27 per 100 000, with the highest rates seen among females aged 15 to 19 years (187 per 100 000). Although the majority of cases were among females, we identified more than 7000 (13.4%) cases of male sexual assault with the highest standardized rates found in the pediatric population younger than 10 years (29–41 per 100 000). Sexual assault was documented across all age groups and sexes, from children to elders, reinforcing the disturbing pattern of sexual violence across the life span.
One of the priorities of this analysis was to broaden the definition of sexual assault to improve case ascertainment. In the majority of studies, the most commonly used code to identify sexual assault is ICD-10 code Y05 (sexual assault by bodily force).13,15,24 This is an optional external cause code that requires a health care provider and health coder to confirm that an assault happened. A recent study among clinical coders found that many have reluctance to assign the Y05 code in the absence of evidence of physical force.24 Within our study population, the Y05 code captured less than 25% of cases. This code identified approximately 12 000 cases of sexual assault, while the combination of the examination codes (i.e., Z04.4, Z.04.5, Z04.51: examination and observation following alleged rape and seduction) identified more than 35 000 cases. Physicians and coders may be more inclined to document that an examination was performed rather than confirm that a sexual assault happened, potentially because of legal implications (e.g., legal testimony, reporting requirements). Our results show that even the most commonly assigned code (Z04.4) will only capture approximately a third of cases and the comprehensive case definition for sexual assault considerably improved ascertainment.
The majority (91.4%) of sexual assault cases were captured through emergency department visits. Sexual assault cases that present at hospitals only represent a fraction of cases, as they either are so severely injured that they require medical attention or are willing to overcome barriers and seek hospital care. Only 8.6% of cases were seen in outpatient clinics and captured through the physician billing database (OHIP).25 Although the OHIP codes are specific to Ontario, it provides information from a primary care perspective and, to our knowledge, has not yet been used for research purposes. With growing awareness surrounding the common experience of sexual assault, these additional codes offer physicians an opportunity to record sexual assault cases outside of hospital-based care and potentially capture less-severe cases.
In this population, the highest rates of sexual assault occurred among children and youths. Our analyses included 3 ICD-10 codes specific to child sexual abuse (Z04.51, Z61.4, Z61.5) and a combination of 16 codes for suspected sexual abuse,22,26 collectively identifying more than 13 000 cases. Among the male population, we observed the highest rates among children aged 0 to 4 years (41 per 100 000) and 5 to 9 years (29 per 100 000). The literature surrounding child maltreatment has been one of the most inclusive sources of sex-disaggregated information for sexual abuse.18,19,27–30
A similar study of children younger than 18 years in Hong Kong found that the annual incidence of child sexual abuse was 15 per 100 000 (26 among females, 4 among males), substantially lower than the rates identified in this study. The higher rates of reported child sexual abuse in this study could be attributed to the broader case definition or the strict child protection protocols and relatively low room for interpretation when a child presents for sexual assault. When dealing with cases of child abuse, studies have found that physicians were more likely to report child sexual abuse than to report physical abuse or neglect.31 Despite this, a recent meta-analysis of 45 studies reported that more than a third of children who have been sexually assaulted do not disclose their experience during interviews, and underreporting still remains an issue.32
Figure 1 shows the standardized rates for each year from 2002 to 2016, indicating some increases over time particularly in the female population. When we investigated each sex and age combination, we found relatively stable sexual assault RRs over the 15-year time period, ranging from 0.95 to 1.09 (Table 3). Of interest, in the pediatric population (aged 0–14 years), we observed small annual decreasing rates in both male and female strata while, in almost all other age groups, the annual rates were increasing. Rate changes are a combination of the number of sexual assault cases occurring in the general population and the number presenting for health care. Although these differences are small, it is an interesting pattern that should continue to be monitored.
Of importance, this study took place between 2002 and 2016, stopping just shy of the global #MeToo social movement that went viral in October 2017. New empirical research has identified an increase in police reporting, Internet searches, and new workplace regulations on sexual assault and harassment after #MeToo.33–35 It is possible that this pattern may also be present in health care administrative data and important for future research.
Limitations
Many studies that use administrative data are prone to measurement bias. A limitation of this study is the absence of a validation study to assess the accuracy and reliability of the broad case definition against a reference standard of confirmed sexual assault cases. The case definition was built to overcome the general pattern of underreporting of sexual assault; however, we do not have information on the degree or direction of misclassification. In our study, we used census population rates (per 100 000) for standardization, which limits comparison with many sexual assault studies that use hospitalizations (per 1000) as the denominator.20,28 Census population standardized rates have broad population and public health application; however, hospitalization standardized rates are useful to hospital administrators and emergency department staff.
The main source of selection bias in this study was the use of data primarily from ambulatory care settings, representing the most severe hospital-based cases of sexual assault. These estimates should be considered hospital-based rates and not representative of the volume of sexual violence in the general population. In addition, not all hospitals and emergency departments have specialized clinics for sexual assault cases, which may result in a higher volume of cases from hospitals with specialized services. Although there are ICD codes available to collect information on the perpetrator (e.g., intimate partner, spouse, family member), at this time, we chose to create a case definition restricted to diagnostic and procedural codes. We additionally do not have information on race, ethnicity, or gender diversity, including information on trans and nonbinary individuals, all factors known to influence risk.
Public Health Implications
Sexual assault is often a stigmatizing experience that has historically been underreported and underestimated. Accurate documentation of the burden of sexual assault is a prerequisite for better allocation of health resources and services for survivors. Results from this study highlight a high annual frequency of sexual assault, across all age categories and sexes, with rates increasing from adolescence onward. The results from this study suggest that health care administrative databases are a useful source of routinely collected information to investigate the epidemiology of sexual assault in the population over time. Broadening the case definition of sexual assault by including several ICD-10 codes, including procedural and examination codes, is a useful strategy to identify cases in which there may be ambiguity or hesitation to apply the singular diagnostic code (e.g., Y05: sexual assault by bodily force).24 Ultimately, if there is a source of routinely collected information on the temporal patterns of sexual assault, it will provide the infrastructure to evaluate sexual assault treatment, prevention, and care programming. With more people than ever coming forward and disclosing experiences of sexual violence, it is a public health imperative to have a strong system in place to document and monitor the prevalence and patterns of sexual assault in the population.
ACKNOWLEDGMENTS
This study was funded by an Applied Health Research Question grant provided by the Ministry of Health and Long-Term Care (MOHLTC): 2019-0901-168-000. This study was supported by ICES, which is funded by an annual grant from the Ontario MOHLTC.
Information previously presented at the Society for Epidemiologic Research; June 18-21, 2019; Minneapolis, MN.
The authors thank and acknowledge all survivors of sexual assault who presented for care.
Note. The opinions, results, and conclusions reported in this article are those of the authors and are independent from the funding sources. No endorsement by ICES or the Ontario MOHLTC is intended or should be inferred.
CONFLICTS OF INTEREST
All authors declare no conflict of interest.
HUMAN PARTICIPANT PROTECTION
The use of data in this project was authorized under section 45 of Ontario’s Personal Health Information Protection Act, which does not require review by a research ethics board.
Footnotes
See also Galea and Vaughan, p. 1169.
REFERENCES
- 1. Global status report on violence prevention. Geneva, Switzerland: World Health Organization; 2014.
- 2.Abrahams N, Devries K, Watts C et al. Worldwide prevalence of non-partner sexual violence: a systematic review. Lancet. 2014;383(9929):1648–1654. doi: 10.1016/S0140-6736(13)62243-6. [DOI] [PubMed] [Google Scholar]
- 3.Basile KC, Smith SG, Breiding MJ, Black MC, Mahendra RR. Sexual violence surveillance: uniform definitions and recommended data elements. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention; 2014.
- 4.Breiding MJ, Smith SG, Basile KC, Walters ML, Chen J, Merrick MT. Prevalence and characteristics of sexual violence, stalking, and intimate partner violence victimization—National Intimate Partner and Sexual Violence Survey, United States, 2011. MMWR Surveill Summ. 2014;63(8):1–18. [PMC free article] [PubMed] [Google Scholar]
- 5.Pereda N, Guilera G, Forns M, Gómez-Benito J. The prevalence of child sexual abuse in community and student samples: a meta-analysis. Clin Psychol Rev. 2009;29(4):328–338. doi: 10.1016/j.cpr.2009.02.007. [DOI] [PubMed] [Google Scholar]
- 6.Lachs MS, Pillemer K. Elder abuse. N Engl J Med. 2015;373(20):1947–1956. doi: 10.1056/NEJMra1404688. [DOI] [PubMed] [Google Scholar]
- 7.Acierno R, Hernandez MA, Amstadter AB et al. Prevalence and correlates of emotional, physical, sexual, and financial abuse and potential neglect in the United States: the National Elder Mistreatment Study. Am J Public Health. 2010;100(2):292–297. doi: 10.2105/AJPH.2009.163089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Perreault S. Criminal victimization in Canada, 2014. Juristat, Canadian Centre for Justice Statistics. 2015: 85-002-X. Available at: https://www150.statcan.gc.ca/n1/en/pub/85-002-x/2015001/article/14241-eng.pdf?st=YWTNC3_W. Accessed June 28, 2019.
- 9.Chou D, Cottler S, Khosla R, Reed GM, Say L. Sexual health in the International Classification of Diseases (ICD): implications for measurement and beyond. Reprod Health Matters. 2015;23(46):185–192. doi: 10.1016/j.rhm.2015.11.008. [DOI] [PubMed] [Google Scholar]
- 10.Yau RK, Stayton CD, Davidson LL. Indicators of intimate partner violence: identification in emergency departments. J Emerg Med. 2013;45(3):441–449. doi: 10.1016/j.jemermed.2013.05.005. [DOI] [PubMed] [Google Scholar]
- 11.Biroscak BJ, Smith PK, Roznowski H, Tucker J, Carlson G. Intimate partner violence against women: findings from one state’s ED surveillance system. J Emerg Nurs. 2006;32(1):12–16. doi: 10.1016/j.jen.2005.11.002. [DOI] [PubMed] [Google Scholar]
- 12.Btoush R, Campbell JC, Gebbie KM. Care provided in visits coded for intimate partner violence in a national survey of emergency departments. Womens Health Issues. 2009;19(4):253–262. doi: 10.1016/j.whi.2009.03.004. [DOI] [PubMed] [Google Scholar]
- 13.Btoush R, Campbell JC, Gebbie KM. Visits coded as intimate partner violence in emergency departments: characteristics of the individuals and the system as reported in a national survey of emergency departments. J Emerg Nurs. 2008;34(5):419–427. doi: 10.1016/j.jen.2007.10.015. [DOI] [PubMed] [Google Scholar]
- 14.Schafer SD, Drach LL, Hedberg K, Kohn MA. Using diagnostic codes to screen for intimate partner violence in Oregon emergency departments and hospitals. Public Health Rep. 2008;123(5):628–635. doi: 10.1177/003335490812300513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Davidov DM, Larrabee H, Davis SM. United States emergency department visits coded for intimate partner violence. J Emerg Med. 2015;48(1):94–100. doi: 10.1016/j.jemermed.2014.07.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gonzalez-Izquierdo A, Ward A, O’Donnell M, Li L, Roposch A, Stanley F. Cross-country comparison of victimisation-related injury admission in children and adolescents in England and Western Australia. BMC Health Serv Res. 2013;13(1):260. doi: 10.1186/1472-6963-13-260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lo CK, Ho FK, Chan KL et al. Linking healthcare and social service databases to study the epidemiology of child maltreatment and associated health problems: Hong Kong’s experience. J Pediatr. 2018;202:291–299.e1. doi: 10.1016/j.jpeds.2018.06.033. [DOI] [PubMed] [Google Scholar]
- 18.McKenzie K, Scott D, Fraser JA, Dunne MP. Assessing the concordance of health and child protection data for “maltreated” and “unintentionally injured” children. Inj Prev. 2012;18(1):50–57. doi: 10.1136/ip.2011.031849. [DOI] [PubMed] [Google Scholar]
- 19.O’Donnell M, Nassar N, Jacoby P, Stanley F. Western Australian emergency department presentations related to child maltreatment and intentional injury: population level study utilising linked health and child protection data. J Paediatr Child Health. 2012;48(1):57–65. doi: 10.1111/j.1440-1754.2011.02189.x. [DOI] [PubMed] [Google Scholar]
- 20.Schnitzer PG, Slusher P, Van Tuinen M. Child maltreatment in Missouri: combining data for public health surveillance. Am J Prev Med. 2004;27(5):379–384. doi: 10.1016/j.amepre.2004.08.007. [DOI] [PubMed] [Google Scholar]
- 21.Statistics Canada. Census Profile, 2016 Census. 2016. Available at: https://www12.statcan.gc.ca/census-recensement/2016/dp-pd/prof/details/Page.cfm. Accessed April 18, 2019.
- 22.Schnitzer PG, Slusher PL, Kruse RL, Tarleton MM. Identification of ICD codes suggestive of child maltreatment. Child Abuse Negl. 2011;35(1):3–17. doi: 10.1016/j.chiabu.2010.06.008. [DOI] [PubMed] [Google Scholar]
- 23.Statistics Canada. Postal Code Conversion File (92-154-X) 2017. Available at: http://www5.statcan.gc.ca/olc-cel/olc.action?ObjId=92-154-X&ObjType=2&lang=en&limit=0. Accessed April 17, 2017.
- 24.Olive P. Intimate partner violence and clinical coding: issues with the use of the International Classification of Disease (ICD-10) in England. J Health Serv Res Policy. 2018;23(4):212–221. doi: 10.1177/1355819618781413. [DOI] [PubMed] [Google Scholar]
- 25. Government of Ontario Ministry of Health and Long-Term Care. OHIP - Bulletins - Health Care Professionals - MOHLTC. Available at: http://www.health.gov.on.ca/en/pro/programs/ohip/sob. Accessed January 14, 2019.
- 26.Seña AC, Hsu KK, Kellogg N et al. Sexual assault and sexually transmitted infections in adults, adolescents, and children. Clin Infect Dis. 2015;61(suppl 8):S856–S864. doi: 10.1093/cid/civ786. [DOI] [PubMed] [Google Scholar]
- 27.McKenzie K, Scott DA. Quantity of documentation of maltreatment risk factors in injury-related paediatric hospitalisations. BMC Public Health. 2012;12(1):563. doi: 10.1186/1471-2458-12-563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McKenzie K, Scott DA. Using routinely collected hospital data for child maltreatment surveillance: issues, methods and patterns. BMC Public Health. 2011;11:7. doi: 10.1186/1471-2458-11-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.McKenzie K, Scott DA, Waller GS, Campbell M. Reliability of routinely collected hospital data for child maltreatment surveillance. BMC Public Health. 2011;11:8. doi: 10.1186/1471-2458-11-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Puls HT, Bettenhausen JL, Markham JL et al. Urban–rural residence and child physical abuse hospitalizations: a national incidence study. J Pediatr. 2019;205:230–235.e2. doi: 10.1016/j.jpeds.2018.09.071. [DOI] [PubMed] [Google Scholar]
- 31.Flaherty EG, Sege R. Barriers to physician identification and reporting of child abuse. Pediatr Ann. 2005;34(5):349–356. doi: 10.3928/0090-4481-20050501-08. [DOI] [PubMed] [Google Scholar]
- 32.Azzopardi C, Eirich R, Rash CL, Macdonald S, Madigan S. A meta-analysis of the prevalence of child sexual abuse disclosure in forensic settings. Child Abuse Negl. 2019;93:291–304. doi: 10.1016/j.chiabu.2018.11.020. [DOI] [PubMed] [Google Scholar]
- 33.Rotenberg C, Cotter A. Police-reported sexual assaults in Canada before and after #MeToo, 2016 and 2017. Statistics Canada. 2018. Available at: https://www150.statcan.gc.ca/n1/pub/85-002-x/2018001/article/54979-eng.pdf. Accessed June 28, 2019.
- 34.Choo EK, Byington CL, Johnson N-L, Jagsi R. From #MeToo to #TimesUp in health care: can a culture of accountability end inequity and harassment? Lancet. 2019;393(10171):499–502. doi: 10.1016/S0140-6736(19)30251-X. [DOI] [PubMed] [Google Scholar]
- 35.Caputi TL, Nobels AL, Ayers JW. Internet searches for sexual harassment and assault, reporting and training since the #MeToo movement. JAMA. 2019;179(2):258–259. doi: 10.1001/jamainternmed.2018.5094. [DOI] [PMC free article] [PubMed] [Google Scholar]