Reproductive coercion and female relationship abuse are prevalent and associated with poor sexual health; health care providers should assess for harmful partner behaviors among all patients who are adolescents or young women.
Abstract
OBJECTIVE:
To investigate demographic differences and evaluate how reproductive coercion and relationship abuse influences young females' care-seeking and sexual health behaviors.
METHODS:
We conducted a secondary analysis of cross-sectional baseline survey data from sexually active female students (aged 14–19 years) who sought care from school health centers. Outcomes included recent (previous 3 months) reproductive coercion, physical or sexual adolescent relationship abuse, and nonpartner sexual violence victimization. Cluster-adjusted χ2 tests compared demographics and generalized linear mixed models estimated associations among reproductive coercion, adolescent relationship abuse (physical and sexual abuse in romantic relationships), and care-seeking and sexual health behaviors.
RESULTS:
Of 550 sexually active high school females, 12% reported recent reproductive coercion and 17% reported physical or sexual adolescent relationship abuse, with no significant demographic differences. Prevalence of recent nonpartner sexual violence was 17%. There were no observed significant differences in care-seeking behaviors among those with recent reproductive coercion compared with those without. Physical or sexual adolescent relationship abuse was associated with increased odds of seeking testing or treatment for sexually transmitted infections (adjusted odds ratio [aOR] 2.08, 95% CI 1.05–4.13). Females exposed to both adolescent relationship abuse and reproductive coercion had higher odds of having a partner who was 5 or more years older (aOR 4.66, 95% CI 1.51–14.4), having two or more recent sexual partners (aOR 3.86, 95% CI 1.57–9.48), and using hormonal contraception only (aOR 3.77, 95% CI 1.09–13.1 vs hormonal methods with condoms).
CONCLUSION:
Almost one in eight females experienced recent reproductive coercion. We did not observe significant demographic differences in reproductive coercion. Partner age and number of sexual partners may elevate risk for abusive relationships. Relationship abuse is prevalent among high school students seeking care, with no clear pattern for case identification. By failing to identify factors associated with harmful partner behaviors, our results support universal assessment for reproductive coercion and relationship abuse among high school–aged adolescents, involving education, resources, and harm-reduction counseling to all patients.
CLINICAL TRIAL REGISTRATION:
One in five female high school students in the United States experienced physical or sexual violence from a romantic partner in the past year.1 Adolescent relationship abuse (physical, sexual, and emotional abuse among adolescents in romantic relationships) increases risk of sexually transmitted infections (STIs), depression, substance use, and subsequent intimate partner violence in adulthood.2–6 Likely related to these health consequences, relationship abuse is generally more prevalent in clinic settings compared with the general population.7,8
Reproductive coercion is a form of relationship abuse that increases risk for unintended pregnancy.7,9 Examples include contraception sabotage, condom manipulation, and pregnancy coercion.8,10 Reproductive coercion has been found to overlap with other forms of adolescent relationship abuse (eg, cyber dating abuse) and confers poor sexual and reproductive health outcomes.11,12 One clinic-based study among adult women found associations between reproductive coercion and race,13 and another study found that sexual minority adolescent females exposed to reproductive coercion were more likely to report STI testing or treatment.14 Despite these studies, gaps remain in identifying demographic characteristics, care-seeking patterns, and sexual health behaviors among female samples of younger ages that may inform the provision of interventions for these females experiencing reproductive coercion and other forms of relationship abuse. The American College of Obstetricians and Gynecologists has underscored the importance of assessing for healthy adolescent relationships and offering harm-reduction strategies during clinic visits.15,16 Thus, we aim to investigate demographic differences among females' (aged 14–19 years) reproductive coercion experiences and to elucidate how harmful partner behaviors may influence care-seeking and sexual health behaviors.
METHODS
We conducted a secondary analysis using data from a cross-sectional baseline survey used in a cluster-randomized trial of a brief universal education intervention for healthy relationships (NCT01678378). The study involved eight student health centers across multiple cities in northern California during the 2012–2013 school year. Descriptions of both the randomized controlled trial and the baseline survey are detailed elsewhere.11,14,17 In short, the original randomized controlled trial included high school students (aged 14–19 years) of all genders who sought services from participating health centers. Of the 1,062 students recruited, a total of 1,011 agreed to participate (95% participation rate). The original study waived parental permission because students were seeking confidential clinical services. All participants provided informed consent. Data were collected before the clinical encounter using a computer-assisted survey. All participating students received a $10 gift card for their time. The University of Pittsburgh and the Public Health Institute Institutional Review Boards, as well as administrators at participating schools, approved all study protocols.
In this analysis, our focus was female high school students who reported ever having sex (N=550) with a male partner to better characterize females' experiences with reproductive coercion. The outcomes included: 1) recent (previous 3 months) reproductive coercion and 2) recent (previous 3 months) physical or sexual adolescent relationship abuse. For the remainder of the article, we will use “adolescent relationship abuse” and “relationship abuse” interchangeably. Reproductive coercion was operationalized as a positive response to at least one item on a 10-item validated measure.10 Similarly, physical or sexual adolescent relationship abuse victimization was defined by a positive response to at least one of three items, derived from the Conflict Tactics Scale 218 and the Sexual Experiences Survey (Box 1).19
Box 1.
Questionnaires
Reproductive Coercion Questionnaire
In the past 3 months, has someone you were dating, going out with, or hooking up with:
Tried to force or pressure you to become pregnant?
Told you not to use any birth control (like the pill, shot, ring, etc.)?
Said he would leave you if you didn't get pregnant?
Told you he would have a baby with someone else if you didn't get pregnant?
Taken off the condom while you were having sex so you would get pregnant?
Put holes in the condom so you would get pregnant?
Broken the condom on purpose while you were having sex so you would get pregnant?
Taken your birth control (like pills) away from you or kept you from going to the clinic to get birth control?
Made you have sex without a condom so you would get pregnant?
Hurt you physically because you did not agree to get pregnant?
Adolescent Relationship Abuse Questionnaire
In the past 3 months, has someone you were going out with or hooking up with hit, pushed, slapped, choked, or otherwise physically hurt you?
In the past 3 months, has someone you were going out with or hooking up with used force or threats to make you have sex [vaginal, oral, or anal sex] when you didn't want to?
In the past 3 months, have you had sex with someone you were going out with or hooking up with when you didn't want to, because you felt like you didn't have a choice, even though they did not use physical force or threats?
Separately for both outcomes, we used Wald log-linear χ2 tests (α=0.05), accounting for school-level clustering, to compare demographic variables between those who were and were not abused, and conducted subgroup analyses for those who had sex in the previous 3 months (as opposed to ever had sex). We used generalized linear mixed models with binary distributions and random effects for school-level clustering to examine the relationship between reproductive coercion and physical or sexual adolescent relationship abuse with care-seeking behaviors and sexual health behaviors; we decided a priori to include race and ethnicity and grade level as covariates in the adjusted models.13,20,21 All analyses were conducted using SAS 9.3. De-identified participant data are publicly available through the National Institute of Justice under the award number 2011-MU-MU-0023.
RESULTS
A total of 771 female students participated in the original study. Of those participants, 71.3% reported ever having had sex with male partner(s) (oral, vaginal, or anal sexual intercourse), resulting in 550 high school students (grades 9–12) who were included in these analyses. Females who had ever had sex with a male partner were in higher grades compared with those who were never sexually active with a male partner (P<.001). The largest racial or ethnic group was Hispanic (36.9%), followed by black (29.3%), multi-racial (15.6%), Asian (13.3%), and white (4.9%). A total of 86.4% disclosed recent (previous 3 months) vaginal sex, 54.9% had recent oral sex, and 11.3% had recent anal sex, with the majority of females reporting male partners only (89.8%) (Table 1).
Table 1.
Demographics of Females Reporting Any Heterosexual Sex, Total and by Reproductive Coercion and Physical or Sexual Adolescent Relationship Abuse
Overall, 12% reported reproductive coercion in the previous 3 months (Fig. 1). Although not significantly differing by race (P=.103), 14.9% of black, 14.8% of Hispanic, and 3.7% of white females reported recent reproductive coercion. Physical or sexual adolescent relationship abuse experiences also did not vary by race or ethnicity (P=.879) but ranged from 12.3% of Asian females to 22.2% of white adolescent females endorsing such experiences. By year of schooling, 6.7% of those in grade 9 to 13.6% of those in grade 12 reported reproductive coercion (P=.873); 11.0% of those in grade 10 to 21.7% of those in grade 9 reported relationship abuse (P=.557) (Table 1).
Fig. 1. Participant experiences with reproductive coercion, adolescent relationship abuse, and nonpartner sexual violence. A total of 5.6%, 8.9%, and 8.9% of the total sample experienced either recent (previous 3 months) reproductive coercion only, adolescent relationship abuse only, or nonpartner sexual violence only, respectively. A total of 2.4% experienced both reproductive coercion and adolescent relationship abuse, 2.0% experienced both reproductive coercion and nonpartner sexual violence, and 4.0% experienced both adolescent relationship abuse and nonpartner sexual violence. Finally, a total of 2.0% experienced all three harmful partner behaviors.
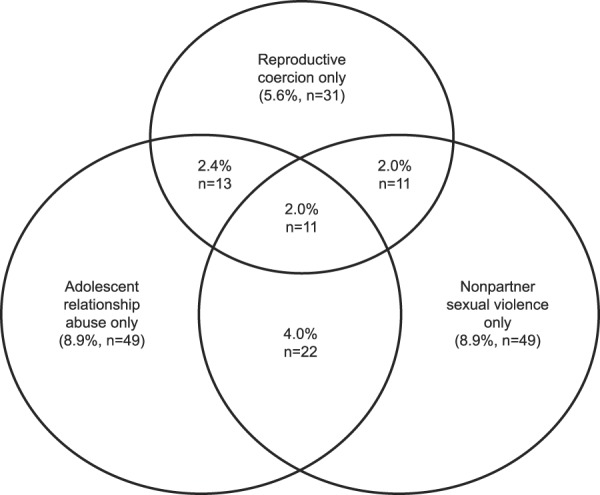
Hill. Reproductive Coercion Among High-School Females. Obstet Gynecol 2019.
We examined several care-seeking behaviors, including pregnancy testing, STI testing or treatment, and any reproductive health visits. There were significant differences in care-seeking behaviors based on the participants' reporting of relationship abuse, but no significant differences based on reporting of reproductive coercion (Tables 2 and 3). In adjusted logistic regression, females who reported relationship abuse had higher odds of seeking STI testing or treatment than those not reporting relationship abuse (adjusted odds ratio [aOR] 2.08, 95% CI 1.05–4.13) (Table 3). We also recorded frequencies of visits and compared them among groups. Before the study (before the beginning of the school year), the majority of the participants in both the relationship abuse and reproductive coercion sample had had at least one visit. Since the start of the study, the majority visited the clinic more than three times in one academic year, indicating high health care utilization. However, we failed to find statistically significant associations between number of visits and reproductive coercion or relationship abuse victimization (Table 2).
Table 2.
Reproductive Coercion and Physical or Sexual Adolescent Relationship Abuse by Pregnancy Risk Behaviors and Care-Seeking Behaviors
Table 3.
Odds of Sexual Health and Care-Seeking Behaviors by Recent Reproductive Coercion and Adolescent Relationship Abuse
Among those who had sex in the previous 3 months, participants with recent reproductive coercion were more likely than those without to report hormonal contraceptive method use only (28.8% vs 18.6%, P=.045). Females without reproductive coercion exposure were more likely than those with exposure to report simultaneous hormonal methods and condom use (33.3% vs 24.2%, P=.045) (Table 2). Recent condom use did not differ significantly between those who reported reproductive coercion and those who did not (59.1% vs 69.4%, P=.126), neither did use of emergency contraception (12.1% vs 15.2%, P=.542) (Table 2). Individuals who had experienced both relationship abuse and reproductive coercion had significantly higher odds of reporting hormonal methods only (aOR 3.77, 95% CI 1.09–13.1) (Table 3). Furthermore, they also had higher odds of having two or more sexual partners recently (aOR 3.86, 95% CI 1.57–9.48) and a partner who was 5 or more years older (aOR 4.66, 95% CI 1.51–14.4) (Table 3).
Of the total sample, 5.6% of participants reported reproductive coercion only, 2.4% reported reproductive coercion and adolescent relationship abuse only, 2.0% reported reproductive coercion and nonpartner sexual violence only, and 2.0% reported all three. Of the total sample, 8.9% of participants reported relationship abuse only and 4.0% reported relationship abuse and nonpartner sexual violence only. Finally, 8.9% of participants reported nonpartner sexual violence only (Fig. 1). Compared with those who had not experienced reproductive coercion, participants who had reproductive coercion had higher rates of recent physical relationship abuse (22.7% vs 7.0%, P=.009), recent sexual relationship abuse (27.3% vs 9.1%, P=.019), and recent nonpartner sexual violence (33.3% vs 14.7%, P=.035) (Table 2). Among the participants who disclosed recent physical or sexual relationship abuse, we observed higher rates of nonpartner sexual violence (34.7% vs 13.2%, P=.009) compared with those who had not experienced relationship abuse. Similarly, among females who had sex in the previous 3 months, those who reported recent physical or sexual relationship abuse had higher rates of recent reproductive coercion compared with those who did not (27.0% vs 10.9%, P=.002) (Table 2). These results remained significant in adjusted models investigating the relationship between recent relationship abuse and reproductive coercion (Table 3). Females who had recent reproductive coercion had more than four times the odds of experiencing recent physical relationship abuse (aOR 4.32, 95% CI 2.12–8.79) and recent sexual relationship abuse (aOR 4.24, 95% CI 2.21–8.11), adjusting for race or ethnicity and grade level. Females who had recent relationship abuse had more than three times the odds of experiencing reproductive coercion (aOR 3.21, 95% CI 1.81–5.71). Both groups (those who had reported reproductive coercion and those who had reported relationship abuse) had higher odds of recent nonpartner sexual violence (reproductive coercion aOR 2.88, 95% CI 1.33–6.21, relationship abuse aOR 3.55, 95% CI 1.95–6.48) (Table 3).
DISCUSSION
These data indicate that reproductive coercion is common among adolescents and young women who are high school students and is associated with adolescent relationship abuse, yet there were no observed significant demographic differences or care-seeking patterns among participants with this exposure. The majority of females with recent reproductive coercion identified as black or Hispanic, similar to research with older women.7,13,22–25 Given persistent disparities in reproductive and sexual health among women and girls of color,26–28 further study is needed on the potential contribution of reproductive coercion to these disparities among adolescents and young women, specifically.
There were no observed differences in visit frequency between those with and without reproductive coercion or relationship abuse. Individuals reporting relationship abuse had higher odds of seeking STI testing or treatment, but not pregnancy testing, which may reflect ease of obtaining over-the-counter pregnancy tests. These data confirm previous studies while challenging others. Miller et al29 found that adolescents who experienced relationship abuse were more likely to have foregone health care (ie, not seeking care despite needing to do so),20 whereas another study noted that recent reproductive coercion and partner violence were positively associated with seeking pregnancy and STI testing.30 In school health centers where barriers to confidential care are minimized (eg, no cost, transportation, or reliance on a parent or guardian for transport), reproductive coercion may not be associated with differential care-seeking patterns.
Females who experienced both reproductive coercion and relationship abuse had higher odds of having a partner who was 5 or more years older. Providers should be aware of mandated reporting laws relevant to child sexual abuse (including partner age in sexual abuse definitions) and discuss these with patients before asking about relationships. Additionally, participants who experienced both exposures had higher odds of having two or more recent sexual partners. A patient's disclosure of unprotected intercourse or sexual activity with multiple partners could indicate previous or current reproductive coercion or relationship abuse.31–34
With contraceptive use, those exposed to reproductive coercion and relationship abuse had higher odds of using hormonal methods only, as opposed to hormonal methods and condoms. Condom manipulation (eg, damaging condoms, removing condoms during sex) is a critical dimension of reproductive coercion that is challenging to include in harm-reduction counseling as behaviors are driven by the perpetrator.10 In fact, research has documented that those experiencing partner violence may be less likely to negotiate condom use or fear the consequences of negotiating condom use with their sexual partners.32–34 Providers should consider discussions on how to safely negotiate condom use and make emergency contraception accessible for patients, as part of harm-reduction counseling to address reproductive coercion and relationship abuse.
Study limitations include the cross-sectional design, limiting causal inference. Our sample only included participants at school health centers in northern California and is not necessarily generalizable to stand-alone adolescent clinics or health settings in other areas. To be consistent with prior studies with older adolescent and young adult women, we focused on reproductive coercion and physical and sexual relationship abuse only. Effects of emotional and cyber abuse are detailed elsewhere.11 Finally, given that the study was not initially powered to detect group differences, our results do not provide definitive evidence of lack of demographic differences and associations with care-seeking behaviors.
Our study explicitly seeks to investigate demographic differences in reproductive coercion and the effects of harmful partner behaviors on care-seeking behaviors among adolescents and young women. Examining adolescent and young women–only populations is important, given how abusive behaviors can manifest differently in adolescence compared with adulthood.35 These findings underscore the need for universal education and assessment of harmful partner behaviors among female patients. Furthermore, although clinical guidelines exist to address reproductive coercion, adherence to these guidelines is not yet ubiquitous.15,16,36,37 By highlighting the relevance of reproductive coercion in adolescence, this study substantiates the urgent need for developmentally appropriate interventions.
There are several clinical practice implications of these findings: 1) reproductive coercion and relationship abuse are prevalent among high school–aged females and should be addressed during clinic visits; 2) multiple sexual partners and older partner age may elevate risk for reproductive coercion or relationship abuse, but there are few care-seeking characteristics to guide case identification; thus, providing education to all patients on healthy and unhealthy relationships and reproductive coercion is appropriate; and 3) harm-reduction counseling should go beyond hidden (or “invisible”) contraception7 and include discussions of condom manipulation as a form of abusive behavior. All patients who are adolescents and young women should receive information and resources about reproductive coercion and relationship abuse, and routine inquiry for these exposures can be integrated into every clinical encounter.
Footnotes
The National Institute of Justice, Office of Justice Programs, U.S. Department of Justice (2011-MU-MU-0023) and the National Center for Advancing Translational Sciences of the National Institutes of Health (TL1R001858) supported this research. The content is solely the responsibility of the authors and do not necessarily represent the official view of the U.S. Department of Justice or National Institutes of Health.
Financial Disclosure The authors did not report any potential conflicts of interest.
The authors thank the staff of the school health centers for their invaluable support with the original study design and data collection.
Each author has confirmed compliance with the journal's requirements for authorship.
Peer reviews and author correspondence are available at http://links.lww.com/AOG/B449.
REFERENCES
- 1.Rasberry C, Tiu G, Kann L, McManus T, Michael SL, Merlo CL, et al. Health-related behaviors and academic achievement among high school students—United States, 2015. MMWR Morb Moral Wkly Rep 2017;66:921–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Exner-Cortens D, Eckenrode J, Rothman E. Longitudinal associations between teen dating violence victimization and adverse health outcomes. Pediatrics 2013;131:71–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Decker MR, Miller E, McCauley HL, Tancredi DJ, Anderson H, Levenson RR, et al. Recent partner violence and sexual and drug-related STI/HIV risk among adolescent and young adult women attending family planning clinics. Sex Transm Infect 2013;90:145– 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hess KL, Javanbakht M, Brown JM, Weiss RE, Hsu P, Gorbach PM. Intimate partner violence and sexually transmitted infections among young adult women. Sex Transm Dis 2012;39:366– 71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Foshee VA, Reyes HL, Gottfredson NC, Chang LY, Ennett ST. A longitudinal examination of psychological, behavioral, academic, and relationship consequences of dating abuse victimization among a primarily rural sample of adolescents. J Adolesc Health 2013;53:723–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ackard DM, Eisenberg ME, Neumark-Sztainer D. Long-term impact of adolescent dating violence on the behavioral and psychological health of male and female youth. J Pediatr 2007;151:476–81. [DOI] [PubMed] [Google Scholar]
- 7.Miller E, Decker MR, McCauley HL, Tancredi DJ, Levenson RR, Waldman J, et al. Pregnancy coercion, intimate partner violence and unintended pregnancy. Contraception 2010;81:316– 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Grace KT, Anderson JC. Reproductive coercion: a systematic review. Trauma Violence Abuse 2018;19:371–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Miller E, Levenson RR, Herrera L, Kurek L, Stofflet M, Marin L. Exposure to partner, family, and community violence: gang-affiliated Latina women and risk of unintended pregnancy. J Urban Health 2012;89:74– 86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McCauley HL, Silverman JG, Jones KA, Tancredi DJ, Decker MR, McCormick MC, et al. Psychometric properties and refinement of the reproductive coercion scale. Contraception 2017;95:292–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dick RN, McCauley HL, Jones KA, Tancredi DJ, Goldstein S, Blackburn S, et al. Cyber dating abuse among teens using school-based health centers. Pediatrics 2014;134:e1560–7. [DOI] [PubMed] [Google Scholar]
- 12.Northridge JL, Silver EJ, Talib HJ, Coupey SM. Reproductive coercion in high school-aged girls: associations with reproductive health risk and intimate partner violence. J Pediatr Adolesc Gynecol 2017;30:603–8. [DOI] [PubMed] [Google Scholar]
- 13.Holliday CN, McCauley HL, Silverman JG, Ricci E, Decker MR, Tancredi DJ, et al. Racial/ethnic differences in women's experiences of reproductive coercion, intimate partner violence, and unintended pregnancy. J Womens Health (Larchmt) 2017;26:828–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McCauley HL, Dick RN, Tancredi DJ, Goldstein S, Blackburn S, Silverman J, et al. Differences by sexual minority status in relationship abuse and sexual and reproductive health among adolescent females. J Adolesc Health 2014;55:652–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Reproductive and sexual coercion. Committee Opinion No. 554. American College of Obstetricians and Gynecologists. Obstet Gynecol 2013;121:411–5. [DOI] [PubMed] [Google Scholar]
- 16.Promoting healthy relationships in adolescents. ACOG Committee Opinion No. 758. American College of Obstetricians and Gynecologists. Obstet Gynecol 2018;132:e213–20. [DOI] [PubMed] [Google Scholar]
- 17.Miller E, Goldstein S, McCauley HL, Jones KA, Dick RN, Jetton J, et al. A school health center intervention for abusive adolescent relationships: a cluster RCT. Pediatrics 2015;135:76–85. [DOI] [PubMed] [Google Scholar]
- 18.Straus MA, Hamby SL, Boney-McCoy S, Sugarman DB. The revised conflict Tactics scales (CTS2): development and preliminary psychometric data. J Fam Issues 1996;17:283–316. [Google Scholar]
- 19.Koss MP, Abbey A, Campbell R, Cook S, Norris J, Testa M, et al. Revising the SES: a collaborative process to improve assessment of sexual aggression and victimization. Psychol Women Q 2007;31:357–70. [Google Scholar]
- 20.Ford CA, Bearman PS, Moody J. Foregone healthcare among adolescents. JAMA 1999;282:2227–34. [DOI] [PubMed] [Google Scholar]
- 21.Dubow EF, Lovko KR, Kausch DF. Demographic difference in adolescents' health Concerns and perceptions of helping agents. J Clin Psychol 1990;19:44–54. [Google Scholar]
- 22.Clark LE, Allen RH, Goyal V, Raker C, Gottlieb AS. Reproductive coercion and co-occurring intimate partner violence in obstetrics and gynecology patients. Am J Obstet Gynecol 2014;210:42.e1–8. [DOI] [PubMed] [Google Scholar]
- 23.Sutherland MA, Fantasia HC, Fontenot H. Reproductive coercion and partner violence among College women. J Obstet Gynecol Neonatal Nurs 2015;44:218–27. [DOI] [PubMed] [Google Scholar]
- 24.Nikolajski C, Miller E, McCauley H, Akers A, Schwarz EB, Freedman L, et al. Race and reproductive coercion: a qualitative assessment. Womens Health Issues 2015;25:216–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Holliday CN, Miller E, Decker MR, Burke JG, Documet PI, Borrero SB, et al. Racial differences in pregnancy intention, reproductive coercion, and partner violence among family planning clients: a qualitative exploration. Womens Health Issues 2018;28:205–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dehlendorf C, Rodriguez MI, Levy K, Borrero S, Steinauer J. Disparities in family planning. Am J Obstet Gyencol 2010;202:214–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Horowitz ME, Pace LE, Ross-Degnan D. Trends and disparities in sexual and reproductive health behaviors and service use among young adult women (aged 18–25) in the United States, 2002–2015. Am J Public Health 2018;108:S336–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kim TY, Dagher RK, Chen J. Racial/ethnic differences in unintended pregnancy: evidence from a national sample of U.S. women. Am J Prev Med 2016;50:427–35. [DOI] [PubMed] [Google Scholar]
- 29.Miller E, Decker MR, Raj A, Reed E, Marable D, Silverman JG. Intimate partner violence and health care-seeking patterns among female users of urban adolescent clinics. Matern Child Health J 2010;14:910–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kazmerski T, McCauley HL, Jones K, Borrero S, Silverman JG, Decker MR, et al. Use of reproductive and sexual health services among female family planning clinic clients exposed to partner violence and reproductive coercion. Matern Child Health J 2015;19:1490–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lang DL, Salazar L, Wingood GM, DiClemente RJ, Mikhail I. Association between recent gender-based violence and pregnancy, sexually transmitted infections, condom use practices, and negotiation of sexual practices among HIV-positive women. J Acquir Immune Defic Syndr 2007;46:216–21. [DOI] [PubMed] [Google Scholar]
- 32.Wingood GM, DiClemente RJ. The effects of an abuse primary partner on the condom use and sexual negotiation practices of African-American women. Am J Public Health 1997;87:1016–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Coker AL. Does physical intimate partner violence affect sexual health? A Systematic Review. Trauma Violence Abuse 2007;8:149–77. [DOI] [PubMed] [Google Scholar]
- 34.Swan H, O'Connell DJ. The impact of intimate partner violence on women's condom negotiation efficacy. J Interpers Violence 2012;27:775–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Miller E. Prevention of and interventions for dating and sexual violence in adolescence. Pediatr Clin N Am 2017;64:423–34. [DOI] [PubMed] [Google Scholar]
- 36.Chamberlain L, Levenson R. Reproductive health and partner violence guidelines: an integrated response to intimate partner violence and reproductive coercion. Available at: https://www.futureswithoutviolence.org/userfiles/file/HealthCare/Repro_Guide.pdf. Retrieved November 26, 2018. [Google Scholar]
- 37.Futures Without Violence. Protocol for adolescent relationship abuse prevention and intervention. Available at: https://www.futureswithoutviolence.org/protocol-for-adolescent-relationship-abuse-prevention-and-intervention/. Retrieved November 26, 2018. [Google Scholar]





