Abstract
Objective: To compare complication rates following amniocentesis in twin gestations, according to sampling technique and number of needle insertions.
Study design: A retrospective cohort study of all women with twin gestations who underwent amniocentesis and delivered in a single university affiliated medical center during 2002−2016. Amniocentesis was performed either through one uterine entry with passage through the inter-twin membrane or through two different entries to the two amniotic sacs. Pregnancy outcome of women that underwent single needle insertion amniocentesis, was compared to this of double needle insertion. Primary outcome was neonatal complications within 4 weeks after amniocentesis (late abortion, chorioamnionitis, preterm premature rupture of membranes, or hospitalization due to related symptoms). Secondary outcomes were gestational week at delivery and labor characteristics.
Results: The study group comprised 212 women. Of them, 73 (34.4%) underwent a single uterine insertion and 139 (65.6%) two separate needle insertions. Baseline characteristics did not differ between the groups. The amniocentesis complication rate was 13.7% in the single insertion group and 16.5% in the double insertion group (p = 0.587). Multivariate analysis found that a single insertion method had no statistically significant influence on complication rate, after making adjustments for potential confounders (OR = 1.085, 95% CI 0.4–2.9; p = 0.871). Other labor characteristics were similar between the groups.
Conclusion: Needle insertion technique in twin gestation amniocentesis was not associated with procedure related complications.
Keywords: Twin pregnancy, Amniocentesis, Abortion, Needle insertion
Introduction
During recent decades, there has been a significant increase in the incidence of twin pregnancies. [1] This trend is accounted for both by the increase in maternal age in developed countries, and the rise in pregnancies achieved by assisted reproductive technologies. According to the American Society for Assisted Reproductive Technology (SART), approximately 8 percent of pregnancies conceived through assisted reproductive technology in 2016 were twin pregnancies [2]. Patients with multiple gestations possess higher risk for fetal genetic and chromosomal anomalies compared to singleton pregnancies, and dizygotic twin pregnancies have approximately twice the singleton risk of an affected fetus [3]. As a result, the genetic workup, which in most cases includes amniocentesis to obtain fetal cells for analysis, has an important role in the prenatal evaluation of these pregnancies. [4] While the risk of pregnancy loss after amniocentesis in singleton pregnancies is well established [5,6], a paucity of data exists regarding the risk in twin pregnancies [7]. Studies have demonstrated different rates of pregnancy loss following amniocentesis in twin pregnancies, ranging from 0 to 9 percent [4,7–9].
One of the factors that might influence amniocentesis complications rate is the sampling technique – a single uterine entry technique with sampling of both gestational sacs following one puncture, versus a double uterine-entry technique and separate punctures of each sac. [7]
There is an insufficient body of data addressing the relationship between sampling technique and pregnancy outcome [10]. Thus, we aimed to investigate the potential impact of amniocentesis technique on related complications in a large cohort of twin pregnancies.
Materials and methods
Study cohort
A retrospective cohort study of all women carrying twin gestation who underwent amniocentesis during pregnancy and delivered in a single university-affiliated tertiary hospital, between October 2002 and February 2016. The cohort was divided into two groups according to amniocentesis technique with regard to the number of trans-abdominal needle applications. Procedures in which a single trans-abdominal needle insertion was performed were compared to procedures using the double insertion technique. Amniocentesis related complication rates were investigated in both groups. Our local institutional review board (0165-16-RMC) approved the study. Informed consent was waived due to the retrospective design of the study and in accordance with good clinical practice.
Our hospital is a referral center for high-risk pregnancies. Thus, we were able to access a large cohort of women with twin pregnancies who were carefully followed during pregnancy and then delivered in the same institution. Some of these pregnancies underwent amniocentesis. The indications for amniocentesis during twin gestation are variable. Our study included only indications that are recommended and funded by the Ministry of Health, in accordance with Israeli guidelines: (1) amniocentesis for fetal karyotype when maternal age exceeds 35 years; (2) suspected anatomical anomalies demonstrated by ultrasound during primary or secondary anatomical survey; (3) Cytomegalovirus (CMV) seroconversion when diagnosed during pregnancy. Amniocentesis to trace virus presence in the amniotic fluid is recommended after 21 weeks of gestation and at least 6 weeks after suspected maternal exposure to virus; and(4) when recommended during genetic counseling generally because of abnormal results in the first or second trimester screening, or when there was hereditary disease in the family.
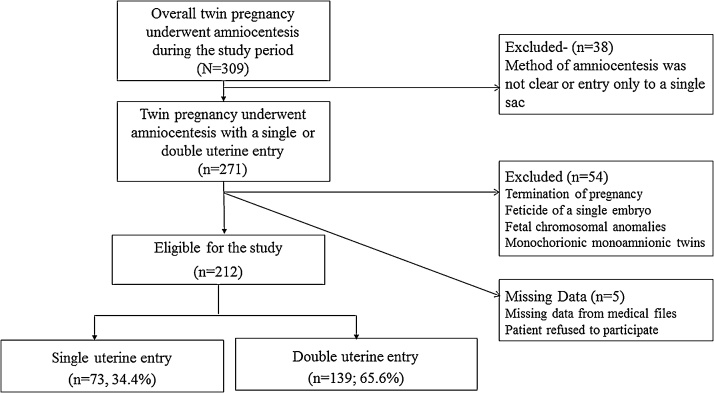
The following cases were excluded: 1) method of amniocentesis was not clear or puncture was made only in a single sac; 2) termination of pregnancy; 3) feticide of a single embryo; 4) fetal chromosomal anomalies; 5) monochorionic monoamniotic twins; and 6) missing data we were not able to attain.
The timing for amniocentesis depended on the indication for the procedure. Elective procedures indicated due to maternal age or pathological screening tests were held at 17 + 0–22 + 6 weeks of gestation. Subsequent procedures were initiated as a result of findings diagnosed later in pregnancy.
Procedure
All procedures were performed by well trained, experienced senior Ob-Gyn physicians specialized in ultrasound. For the investigated cohort, amniocentesis was performed by seven elected physicians and 84% of cases were performed by three of them. After elaborating on the risks associated with amniocentesis, informed consent was obtained from the patient. The procedure was performed under continuous ultrasound vision. Initially, the first selected amniotic sac was punctured and amniotic fluid aspirated. In most cases, after aspirating the required amount of fluid for genetic analysis, color was injected into the same sac, to mark the first-entered amniotic sac. The entrance to the second amniotic sac involved injecting a needle into the inter-twin membrane (single insertion) or directly into the uterus (double insertion). The procedure was completed when amniotic fluid from the second sac was obtained.
Data collection
Data regarding the procedure, pregnancy, and birth were retrieved from our departmental comprehensive computerized perinatal database, and cross-tabulated using an individualized identification number per patient. Data from the ultrasound unit and the neonatal intensive care unit (NICU) were integrated into the delivery ward database.
The following baseline characteristics were recorded: maternal age, gravidity, parity, previous preterm labor, pregnancy achieved by assisted reproductive technology, twin amnionicity and chorionicity, fetal gender, gestational age at amniocentesis and placental location. Missing data was obtained through a careful manual chart review performed by the study personnel or by calling the patient's personal physician after receiving informed consent.
Primary outcome was defined as the composite complications outcome, including any one of the following amniocentesis related complications occurring within 4 weeks post procedure: late abortion, chorioamnionitis, premature rupture of membranes, or hospitalization for observation in gynecologic ward due to procedure associated symptoms (i.e. fever above 38 ºC, premature contractions, abdominal pain and tenderness). Secondary outcomes were labor characteristics.
Outcomes were stratified for study groups according to amniocentesis technique: single vs. double insertion.
Statistical analysis
Pregnancy loss rates related to twin amniocentesis range from 0% and up to 9% in different studies [[4], [5], [6], [7], [8], [9]], Using the Epi-info™, program for this pregnancy loss frequencies assuring 80% power with a limit of 0.05 for type I error; a sample size of 116 cases for each subgroup is needed. Since we performed a retrospective design for our study, and used all cases eligible according to the inclusion criteria, we defined a primary outcome composed of any procedure associated complications. Post-hoc power analysis calculated with the above-mentioned definitions, for a complication’s frequency of 14%, a sample size of 64 cases is needed for each subgroup.
Data analysis was performed using the SPSS v21.0 package (Chicago, IL). Continuous variables were compared using the Student's t-test and Mann-Whitney U test. The chi-square and Fisher's exact tests were used for categorical variables. Differences were considered significant when the p-value was less than 0.05. Following the bivariate analysis, logistic regression analysis was utilized to adjust outcomes for potential confounders. Variables with clinical impacts or that differed significantly between the groups (p < 0.05) in the bivariate analysis entered the regression model: maternal age, gravidity, parity, previous preterm labor, gestational age at amniocentesis and composite complications outcome.
Results
During the study period, 309 mothers with twin pregnancies underwent amniocentesis and delivery in our institution; 212 (68.6%) met the inclusion criteria. In 73 (34.4%) cases amniocentesis was performed by a single uterine entry, and in 139 (65.6%) cases amniocentesis was performed by double uterine entry. A total of 97 cases were excluded as presented in Fig. 1.
Fig. 1.
Study cohort selection.
Baseline characteristics of women in both groups are presented in Table 1. No significant difference was found between the groups regarding demographic characteristics, prior preterm labor, and indication for procedure, or placental location. The majority of the women carried a bichorionic twin pregnancy and only 20 women carried a monochorionic diamniotic pregnancy. Of them, four underwent a single uterine entry and 16 underwent a double uterine entry. Thus, chorionicity did not differ between study groups (p = 0.149). The use of color as elaborated in the Methods section was performed in 190 (89.6%) of all cases; while a higher rate of its use was documented in the single insertion technique (95.6% vs. 86.3% in the double insertion technique, p = 0.03).
Table 1.
Baseline characteristics for the study groups.
| Variable | Single insertion (N = 73) | Double insertion (N = 139) | p value |
|---|---|---|---|
| Maternal age (years) | 34.7 ± 4.8 | 34.9 ± 4.8 | 0.828 |
| Gravidity | 2.3 ± 1.4 | 2.8 ± 1.7 | 0.071 |
| Parity | 0.9 ± 0.9 | 1.2 ± 1.1 | 0.147 |
| Previous preterm labor | |||
| <37 weeks | 5/63 (7.9) | 11/112 (8.9) | 0.915 |
| <34 weeks | 1/63 (1.6) | 2/123 (1.6) | 0.984 |
| Assisted reproductive technology | 41/63 (65.1) | 71/119 (59.7) | 0.555 |
| Chorionicity | 0.149 | ||
| Bichorionic diamniotic | 58(93.5) | 102(86.4) | |
| Monichorionic diamniotic | 4(6.5) | 16 | |
| Indication for amniocentesis | 0.914 | ||
| Maternal age >35 years | 36/71 (50.7) | 62/135 (45.9) | – |
| Maternal request | 9/71 (12.7) | 20/135 (14.8) | – |
| Anatomic anomalies | 16/71 (22.5) | 36/135 (26.7) | – |
| CMV seroconversion | 2/71 (2.8) | 4/135 (3) | – |
| Genetic counseling | 8/71 (11.3) | 12/135 (8.9) | – |
| Male neonates | |||
| Fetus #1 | 38/65 (58.5) | 67/118 (56.8) | 0.379 |
| Fetus #2 | 35/65 (58.3) | 48/116 (41.4) | 0.094 |
| Gestational age at amniocentesis (weeks) | 19.6 ± 4.1 | 20.3 ± 4.68 | 0.296 |
| Anterior placenta | |||
| Fetus #1 | 43/71 (60.6) | 63/135 (46.6) | 0.363 |
| Fetus #2 | 29/68 (42.7) | 66/134 (49.3) | 0.477 |
| Use of color in amniocentesis | 70/73 (95.9) | 120/139 (86.3) | 0.030 |
For all variables, categorical data are presented as n/N (%) and continuous variables are presented as average±2 SD.
CMV, cytomegalovirus.
Bivariate analysis of individual and composite complications outcomes is presented in Table 2. Regarding primary outcome as defined in the Methods section, no significant difference was demonstrated between the groups. A composite complications outcome rate of 13.7% was found in the single insertion technique vs. 16.5% in the double insertion technique (p = 0.587). A specific analysis of the monochorionic twin subgroup demonstrated an overall frequency of the composite complications outcome of up to 40%. Moreover, the only one case of abortion ascribed to amniocentesis (0.5%) that was identified in the cohort and was found in the double entry group was a monochorionic twin gestation. The patient presented at 19 weeks of gestation, two weeks following the procedure, with no cardiac activity to both twins.
Table 2.
Amniocentesis related complication rates.
| Variable | Single insertion (N = 73) | Double insertion (N = 139) | p value |
|---|---|---|---|
| Complications within 4 weeks after Amniocentesis | |||
| Late abortion | 0/65 (0) | 1/125 (0.8) | 0.470 |
| Chorioamnionitis | 0/62 (0) | 1/118 (0.8) | 0.655 |
| PPROM | 3/62 (4.8) | 6/122 (4.9) | 0.981 |
| Hospitalization | 6/62 (9.7) | 16/118 (13.6) | 0.655 |
| Composite complications outcome* | 9/73 (13.7) | 24/139 (16.5) | 0.587 |
For all variables, categorical data are presented as n/N (%).
PPROM, preterm premature rupture of membranes.
Composite includes any of the following within 4 weeks of amniocentesis: Late abortion, chorioamnionitis, pre-term premature rupture of membranes, or hospitalization.
Following adjustment for potential confounders as elaborated in the Methods section, amniocentesis technique was not associated with composite complication outcome (OR = 1.085, 95% CI 0.4–2.9, p = 0.871).
Labor characteristics for the study groups are presented in Table 3. No differences regarding pregnancy complications, induction of labor or mode of delivery were found between the groups. The mean gestational age at delivery was 35.1 weeks and birth weights were statistically similar in both study groups.
Table 3.
Pregnancy and labor characteristics for the study groups.
| Variable | Single Insertion (N = 73) | Double Insertion (N = 139) | p value | p value |
|---|---|---|---|---|
| Pregnancy complications | ||||
| Pre-eclampsia | 5/59 (8.5) | 12/118 (10.2) | 0.718 | 0.718 |
| Gestational DM | 7/61 (11.5) | 15/118 (12.7) | 0.593 | 0.593 |
| Suspected intrauterine growth restriction | 7/61 (11.5) | 17/116 (14.7) | 0.557 | 0.557 |
| Twin to twin transfusion syndrome | 0/61 (0) | 1/118 (0.8) | 0.471 | 0.471 |
| Labor characteristics | ||||
| Labor induction | 29/61 (47.5) | 63/118 (53.4) | 0.298 | 0.298 |
| Cesarean delivery | 51/67 (76.1) | 101/126 (80.2) | 0.307 | 0.307 |
| Gestational age at delivery (weeks) | 35.1 ± 3.0 | 35.1 ± 2.9 | 0.973 | 0.973 |
| Birth weight (grams) | ||||
| Fetus #1 | 2169.2 ± 506.2 | 2324.3 ± 550.3 | 0.071 | 0.071 |
| Fetus #2 | 2145.5 ± 553.5 | 2198.7 ± 502.6 | 0.529 | 0.529 |
For all variables, categorical data are presented as n/N (%); continuous variables are presented as average± 2SD.
DM, diabetes mellitus.
Discussion
This study sought to evaluate the association between amniocentesis technique and pregnancy complications in twin pregnancies, comparing single uterine entry to conventional double uterine entry, and found the two methods comparable. Pregnancies complications directly relate to amniocentesis are known to occur within 4 weeks following the procedure [[11], [12], [13]]. Thus, we presented a primary outcome composite comprised of complications occurring up to 4 weeks following the procedure. The results showed that both techniques were similar in terms of pregnancy and complications outcomes.
A single uterine entry technique, as was described in several studies, requires good visualization of the amniotic membranes in order to advance the same needle into both gestational sacs [10,14,15]. This procedure was described as both swift and easy, and reduces discomfort to the patient [14].
It is commonly accepted that the risk for adverse outcome rises with increase in number of uterine entries during the procedure [7]. We hypothesized that single uterine entry technique might present a lower complications rate compared to the double uterine entry technique, and might resemble published complications rates in singleton pregnancies. However, single uterine entry technique is more complex than the singleton amniocentesis since it requires the passage through the inter-twin membrane, which exposes one of the gestational sacs to two different amniotic punctures (one at the entry and the second through the inter-twin membrane). Moreover, the single-entry technique raises the theoretical risk of inter-twin membrane rupture, evidence for this hypothesis is lacking.
To date, only one study has addressed the effect of number of uterine entries during amniocentesis of twin pregnancies on pregnancy outcomes [10]. In that study, the authors reviewed 100 cases of amniocentesis in twin pregnancies described total fetal loss before 24 weeks or PPROM < 34 weeks at a rate of 1 (2.7%) (n = 37) for single entry vs. 3 (4.76%) (n = 63) for double entry, with no statistic significant differences (RR = 0.57). Our study of a larger cohort of 212 pregnancies, showed similar results. This sample size is correlated with the power calculations and presents a much larger cohort compared to previous studies. The lack of statistically significant differences between the two groups, despite our larger sample size and adequate power as elaborated in the statistical analysis section, may be attributed to the very low rate of fetal loss in our study (0.5%) which is consistent with some earlier studies [[14], [15], [16], [17]].
In general, our results compare favorably with the literature in terms of gestational age at delivery, complication rate and birth weight [7,8]. However, to the best of our knowledge, our study includes one of the largest cohorts of twin pregnancies who underwent amniocentesis reported in the literature.
Another potential problem with single uterine entry technique, is that it may cause sampling errors or cross contaminations [4,10]. In our series, there were no such complications. This might be attributed to our well experienced procedure operators, to the widely used color injection and to the thorough ultrasound evaluation conducted both prior to and during the procedure.
The strengths of our study are the relatively large sample size and the detailed prenatal information we were able to collect. Operator dependent complications bias was diminished by an elected group of well experienced operators. Limitations include the retrospective design, the lack of randomization for procedure technique and the small numbers of monochorionic twin gestation that constrained our ability to imply significant results over this subgroup.
In conclusion, we found similar pregnancy outcomes for twin pregnancies following amniocentesis by a single or double uterine entry technique. Both techniques are optional and medically acceptable. Choice should be left to the operator considering their skills and real-time ultrasound findings.
Disclosure
The authors report no conflict of interest.
Funding
None.
References
- 1.Russell R.B., Petrini J.R., Damus K., Mattison D.R., Schwarz R.H. The changing epidemiology of multiple births in the United States. Obstet Gynaecol. 2003;101:129–135. doi: 10.1016/s0029-7844(02)02316-5. [DOI] [PubMed] [Google Scholar]
- 2.American Society for Assisted Reproductive Technology (SART) Clinic Summary Report. At: https://www.sartcorsonline.com/rptCSR_PublicMultYear.aspx?ClinicPKID=0. Updated April 2018. Accessed: June 2018.
- 3.Jenkins T.M., Wapner R.J. The challenge of prenatal diagnosis in twin pregnancies. Curr Opin Obstet Gynecol. 2000;12:87–92. doi: 10.1097/00001703-200004000-00006. [DOI] [PubMed] [Google Scholar]
- 4.Weisz B., Rodeck C.H. Invasive diagnostic procedures in twin pregnancies. Prenat Diagn. 2005;25:751–758. doi: 10.1002/pd.1263. [DOI] [PubMed] [Google Scholar]
- 5.Alfirevic Z., Sundberg K., Brigham S. Amniocentesis and chorionic villus sampling for prenatal diagnosis. Cochrane Database Syst Rev. 2003;(3) doi: 10.1002/14651858.CD003252. CD003252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mujezinovic F., Alfirevic Z. Procedure-related complications of amniocentesis and chorionic villous sampling: a systematic review. Obstet Gynecol. 2007;110:687–694. doi: 10.1097/01.AOG.0000278820.54029.e3. [DOI] [PubMed] [Google Scholar]
- 7.Agarwal K., Alfirevic Z. Pregnancy loss after chorionic villus sampling and genetic amniocentesis in twin pregnancies: a systematic review. Ultrasound Obstet Gynecol. 2012;40:128–134. doi: 10.1002/uog.10152. [DOI] [PubMed] [Google Scholar]
- 8.Vink J., Fuchs K., D’Alton M.E. Amniocentesis in twin pregnancies: a systematic review of the literature. Prenat Diagn. 2012;32:409–416. doi: 10.1002/pd.2897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Millaire M., Bujold E., Morency A.M., Gauthier R.J. Mid-trimester genetic amniocentesis in twin pregnancy and the risk of fetal loss. Obstet Gynaecol. 2006;28:512–518. doi: 10.1016/s1701-2163(16)32171-5. [DOI] [PubMed] [Google Scholar]
- 10.Simonazzi G., Curti A., Farina A., Pilu G., Bovicelli L., Rizzo N. Amniocentesis and chorionic villus sampling in twin gestations: which is the best sampling technique? Am J Obstet Gynecol. 2010;202(365):e1–e5. doi: 10.1016/j.ajog.2009.11.016. [DOI] [PubMed] [Google Scholar]
- 11.Tabor A., Philip J., Madsen M., Bang J., Obel E.B. Randomised controlled trial of genetic amniocentesis in 4606 low-risk women. Lancet. 1986;1 doi: 10.1016/s0140-6736(86)91218-3. 1287-1283. [DOI] [PubMed] [Google Scholar]
- 12.Eddleman K.A., Malone F.D., Sullivan L. Pregnancy loss rates after midtrimester amniocentesis. Obstet Gynecol. 2006;108:1067–1072. doi: 10.1097/01.AOG.0000240135.13594.07. [DOI] [PubMed] [Google Scholar]
- 13.Mazza V., Pati M., Bertucci E. Age-specific risk of fetal loss post second trimester amniocentesis: analysis of 5043 cases. Prenat Diagn. 2007;27:180–183. doi: 10.1002/pd.1647. [DOI] [PubMed] [Google Scholar]
- 14.Van Vugt J.M., Nieuwint A., Van Geijn H.P. Single-needle insertion: an alternative technique for early second-trimester genetic twin amniocentesis. Fetal Diagn Ther. 1995;10:178–181. doi: 10.1159/000264229. [DOI] [PubMed] [Google Scholar]
- 15.Buscaglia M., Ghisoni L., Bellotti M. Genetic amniocentesis in biamniotic twin pregnancies by a single transabdominal insertion of the needle. Prenat Diagn. 1995;15:17–19. doi: 10.1002/pd.1970150105. [DOI] [PubMed] [Google Scholar]
- 16.Reid K.P., Gurrin L.C., Dickinson J.E., Newnham J.P., Phillips J.M. Pregnancy loss rates following second trimester genetic amniocentesis. Aust N Z J Obstet Gynaecol. 1999;39:281–285. doi: 10.1111/j.1479-828x.1999.tb03397.x. [DOI] [PubMed] [Google Scholar]
- 17.Ko T.M., Tseng L.H., Hwa H.L. Second trimester genetic amniocentesis in twin pregnancy. Int J Gynecol Obstet. 1998;61:285–287. doi: 10.1016/s0020-7292(98)00045-9. [DOI] [PubMed] [Google Scholar]