Abstract
Omsk hemorrhagic fever virus (OHFV) is a tick-borne flavivirus classified as a biosafety level-4 (BSL4) pathogen. Studies of OHFV are restricted to be conducted within BSL4 laboratories. Currently, no commercial vaccines or antiviral drugs are available against OHFV infection. In this study, we recovered a replication-deficient OHFV with an NS1 deletion (OHFV-ΔNS1) and reporter virus replacing NS1 with the Gaussia luciferase (Gluc) (OHFV-ΔNS1-Gluc). Both the defective OHFV-ΔNS1 and OHFV-ΔNS1-Gluc virus could only replicate efficiently in the BHK21 cell line expressing NS1 (BHK21NS1) but not in naïve BHK21 cells. The Gluc reporter gene of OHFV-ΔNS1-Gluc virus was maintained stably after serial passaging of BHK21NS1 cells and was used to surrogate the replication of OHFV. Using NITD008, OHFV-ΔNS1-Gluc virus was validated for antiviral screening, and high-throughput screening parameters were optimized in a 96-well plate format with a calculated Z′ value above 0.5. The OHFV-ΔNS1-Gluc reporter virus is a powerful tool for antiviral screening as well as viral replication and pathogenesis studies in BSL2 laboratories.
Keywords: Omsk hemorrhagic fever virus (OHFV), Trans complementation, NS1, Gaussia luciferase (Gluc), Antiviral screening
Introduction
Omsk hemorrhagic fever (OHF) is caused by Omsk hemorrhagic fever virus (OHFV), which belongs to the tick-borne encephalitis (TBE) serocomplex, genus Flavivirus, family Flaviviridae. The Flavivirus genus includes many other important pathogens such as dengue virus (DENV), zika virus (ZIKV), West Nile virus (WNV), Japanese encephalitis virus (JEV), yellow fever virus (YFV), and tick-borne encephalitis virus (TBEV). The clinical symptoms of OHF include fever, headache, cough, myalgia, hemorrhage, and sometimes meningeal signs with neurological system damage, and the mortality rate ranges from 0.5% to 3% (Charrel et al.2004; Ruzek et al.2010). Since its first isolation in 1947 from a human presenting with hemorrhagic fever in Omsk area (Dobler 2010; Lani et al.2014), OHFV had become prevalent in Omsk, Novosibirsk, Tyumen, and Kurgan in some regions of western Siberia in Russia (Charrel et al.2004; Ruzek et al.2010).
OHFV is transmitted by the bites of the meadow tick Dermacentor reticulatus (Charrel et al.2004; Ruzek et al.2010) and contact with infected vole (Microtus gregalis) and muskrats (Ondatra zibethicus). It had been reported that the introduction of muskrats, which are sensitive to OHFV, caused the virus to spread widely (Ruzek et al.2010). OHF is an example of a human disease that has emerged because of human-mediated disturbances to an ecological niche. The widespread presence of ticks enabled the global spread of the virus. Additionally, OHFV can be transmitted by aerosol and contaminated water which played important roles in the spread of the virus to humans and wider propagation of this virus (Dobler 2010; Lani et al.2014). Although the morbidity and mortality of infection are low, many cases of human infection may be undiagnosed because of the lack of effective diagnostic methods. Because of its numerous transmission routes, OHFV may spread worldwide and become prevalent, as observed for TBEV. Although a recombinant TBEV vaccine may cross-protect against OHFV (Orlinger et al.2011), no licensed vaccine or compound is available against OHFV. Therefore, additional antiviral screening, vaccine development, and pathogenesis studies of OHFV are needed.
OHFV is classified as a biosafety level-4 (BSL4) pathogen, limiting further progress in OHFV research because of insufficient BSL4 containment facilities. To overcome this limitation, researchers have developed numerous alternatives for studying BSL3 or BSL4 viruses in BSL2 laboratories. A noncytopathic replicon system and virus-like particle (VLP) system with reporter genes have been constructed for several BSL3 viruses such as chikungunya virus (Pohjala et al.2011), TBEV (Hayasaka et al.2004; Yoshii et al.2009), and WNV (Shi et al.2002; Scholle et al.2004; Pierson et al.2006), as well as for BSL4 viruses such as Ebola virus (Wang et al.2016) for screening inhibitors, neutralization test and vaccine development. Viral replicons do not contain structural proteins and only perform transcription and replication functions. VLPs generated by the packaging of replicon RNA with structural proteins in trans are efficient tools for substituting wild-type virus to monitor the entire viral life cycle.
Additionally, replication-defective viruses are typically produced by exogenously supplied proteins or other factors to complement the deficient genome with gene deletions or mutations. Defective viruses reproduce only in complementary cells and function similarly to the wild-type virus. This replication-defective virus system has been generated for the Ebola virus with VP30 gene deletion (Ebola∆VP30-neo virus) for propagation in the Vero cell line stably expressing VP30 protein (Halfmann et al.2008). The viruses resemble wild-type virus in their life cycle, but can be handled in a non-BSL4 laboratory. Moreover, a similar strategy based on the replication-defective system was used for influenza A viruses (BSL3) (Si et al.2016). Because of the replication defects of the genome itself, these defective viruses cannot replicate in conventional cells but only propagate in complementary cells; thus, replication-defective viruses are safe for use in BSL2 laboratories for studying high biosecurity level viruses.
OHFV genome is a single-stranded, positive-sense RNA approximately 11 kb in length and consists of a large open reading frame flanked by 5′ and 3′ untranslated regions. The genome is translated into a polyprotein that is processed into three structural proteins (C, prM, and E) and seven nonstructural proteins (NS1, NS2A, NS2B, NS3, NS4A, NS4B, and NS5). The structural proteins play an important role in virion entry, fusion, and assembly. The nonstructural proteins function in replication complex formation and viral genome replication. Among them, NS1 is a multifunctional glycoprotein secreted into the extracellular space and modulates early viral RNA replication and immune evasive functions (Lindenbach and Rice 1997; Youn et al.2012; Zhang et al.2017b). Deletion of NS1 from the viral genome abrogates replication. However, it had been reported that NS1-deleted YFV and WNV can be complemented in trans by exogenous expression of NS1 and packaged into a replication-defective virus (Lindenbach and Rice 1997; Khromykh et al.2000; Zhang et al.2017a).
Few antiviral screening and pathogenicity studies have evaluated alternatives for replacing OHF live virus without the requirement for BSL4 facilities. Only OHFV VLPs packaging replicons with structural proteins have been established for neutralization testing of the strain Guriev (Yoshii and Holbrook 2009), while inhibitor screening is still performed using authentic viruses (Lo et al.2016). Thus, it is necessary to develop a novel, safe, and stable system for antiviral screening against OHFV in BSL2 laboratories.
In this study, replication-deficient OHFV-ΔNS1 and OHFV-ΔNS1-Gluc viruses were produced by complementation with a deficient genome using the BHK21NS1 cell line expressing NS1 in trans. Both defective viruses replicated only efficiently in the BHK21NS1 cell line without reversion to the wild-type virus after serial passaging, and could not replicate in naïve BHK21 cells, demonstrating its safety. Luciferase activity can be used to quantify the viral replication of OHFV-ΔNS1-Gluc. Using a known inhibitor of flaviviruses, NITD008, we found that the luciferase activities derived from OHFV-ΔNS1-Gluc-infected BHK21NS1 cells were inhibited in a concentration-dependent manner, demonstrating that OHFV-ΔNS1-Gluc can be used for antiviral screening. A high-throughput screening (HTS) assay using the OHFV-ΔNS1-Gluc on BHK21NS1 cell line was optimized, showing a Z′ value above 0.5. In general, a stable and safe replication-deficient OHFV system was developed for use in antiviral studies in a BSL2 laboratory.
Materials and Methods
Cells, Antibodies, and Reagents
BHK21 and 293T cells were cultured in Dulbecco’s modified Eagle’s medium supplemented with 10% fetal bovine serum, 100 U/mL of penicillin, and 100 μg/mL of streptomycin at 37 °C with 5% CO2. The BHK21NS1 cell line stably expressing OHFV-NS1 was grown in complete medium containing 0.8 μg/mL puromycin (Sigma, St. Louis, MO, USA). The antibody anti-HA tag was purchased from Cell Signaling Technology (Danvers, MA, USA) and used for Western blotting and immunofluorescent assays (IFA) to detect the expression of OHFV-NS1. The antibody against OHFV-NS3 was obtained by immunizing mice with NS3 protein and used for IFA. The secondary antibodies, horseradish peroxidase-conjugated goat anti-mouse antibody and fluorescein isothiocyanate-conjugated goat anti-mouse IgG (purchased from ProteinTech Group, Rocky Hill, NJ, USA) were used for Western blotting and IFA, respectively. NITD008 was synthesized as reported previously (Yin et al.2009).
Plasmid Construction
OHFV full-length infectious clone (OHF-IC) was kindly provided by Professor Yoshii et al. (2011). According to a previous strategy, the truncated NS1 fragment with a deletion of amino acids (aa) 4–298 was generated by fusion PCR using OHF-IC as a template (Khromykh et al.2000; Zhang et al.2017a). The engineered fragment was then inserted into OHF-IC between the restriction sites BsrG I and Hpa I to generate the OHFV-ΔNS1 clone. To generate OHFV-ΔNS1-Gluc, the Gluc2A sequence was introduced by overlap PCR to replace the deleted NS1 sequence. Initially, the Gluc2A sequence was amplified using the plasmid pACYC-WNV-Gluc-∆NS1 as a template (Zhang et al.2017a). The fragment encompassing the C-terminal 54 aa of the NS1 gene and NS2A was amplified using OHF-IC as a template. The two fragments were fused by overlapping PCR and inserted into OHFV-ΔNS1 between the restriction sites Cla I and Hpa I.
pBABEpuro-OHFV-NS1 was constructed by standard PCR using OHF-IC as a template with the BamH I and EcoR I restriction sites. The NS1 cassette contains full-length NS1 with an N-terminal signal peptide sequence (the last 24 aa of the envelope protein) and C-terminal HA-tag. All clones were sequenced prior to subsequent experiments.
Western Blotting Assay
Total proteins from FuGENE® HD (Promega, Madison, WI, USA) transfected BHK21 cells at 36 h post-transfection were lysed by RIPA buffer (Beyotime Biotechnology, Shanghai, China) and separated by sodium dodecyl sulfate–polyacrylamide gel electrophoresis (12%). Proteins were then transferred onto 0.2-μm polyvinylidene fluoride membranes (Bio-Rad, Hercules, CA, USA), followed by blocking with 5% skim milk (Bio-Rad) in 1 × TBST and sequential incubation with anti-HA (1:1000) and secondary anti-mouse IgG conjugated to horseradish peroxidase (1:2000, Beyotime Biotechnology). After three washes with 1 × TBST, the signals were detected with a chemiluminescence system (ChemiDoc, Bio-Rad).
In Vitro RNA Transcription and Transfection
The OHFV-ΔNS1 and OHFV-ΔNS1-Gluc cDNA plasmids were linearized by Xba I and purified by phenol/chloroform extraction. The linearized cDNA was then subjected to in vitro transcription with the mMESSAGE mMACHINE® T7 Kit (Ambion, Foster City, CA, USA) according to the manufacturer’s protocols. The resulting RNA was dissolved in nuclease-free water and quantified by NanoDrop spectrophotometry (Thermo Fisher Scientific, Waltham, MA, USA). Next, 1 μg RNA was transfected into BHK21 or BHK21NS1 cells with reagent DMRIE-C (Invitrogen, Carlsbad, CA, USA). At different time points after transfection, the supernatants were collected. All experiments involving deficient virus rescue and passaging were performed under BSL3 conditions.
Establishment of a Stable BHK21NS1 Cell Line Expressing OHFV-NS1
The retroviral vector system was used to generate a stable BHK21 cell line expressing NS1. Briefly, the constructs pBABEpuro-OHFV-NS1, m57, and VSV-G were co-transfected into 293T cells by using calcium phosphate-DNA precipitates. At 6 h post-transfection (hpt), half of the culture medium was replaced with an equal volume of fresh medium. The combined retroviral supernatants were harvested at 48 and 72 hpt followed by filtration through a 0.45-μm filter, and then used to infect naïve BHK21 cells in the presence of 8 μg/mL polybrene. At 2 h post-infection, the medium was removed and replaced with fresh culture medium. On the second day, the cells were selected with medium containing 0.8 μg/mL of puromycin. After several rounds of puromycin selection, monoclonal cells were picked and amplified.
IFA
BHK21 and BHK21NS1 cells cultured on cover slips were fixed in cold (− 20 °C) 5% acetone in methanol at 25 °C for 10 min. After washing three times with PBS (pH 7.4), the fixed cells were sequentially incubated with anti-HA tag or OHFV-NS3 antibody (1:200 dilution in PBS) and goat-anti-mouse IgG conjugated with fluorescein isothiocyanate (1:125 dilution in PBS) for 1 h. The slides were mounted with 95% glycerol and examined under a fluorescence microscope at 100 × or 400 × magnification.
Reverse Transcription Polymerase Chain Reaction (RT-PCR)
Total RNA was extracted using Trizol reagent (Takara, Shiga, Japan) from BHK21 and BHK21NS1 cells infected with OHFV-ΔNS1 or OHFV-ΔNS1-Gluc virus. The obtained RNA was identified by RT-PCR using the PrimeScript One Step RT-PCR Kit (Takara) with primers OHFV-1964-F (5′-CATTCTCTGGGACAAAGCCGT-3′) and OHFV-3822-R (5′-TGTTAGACTTCTGCGCAGCAC-3′), which spanned the E and NS2A regions.
Growth Kinetics and Titers Determination of Complemented Virus
The growth kinetics of complemented virus were evaluated in the BHK21NS1 cell line (12-well plate, 1 × 105 cells/well) and infected at a multiplicity of infection (MOI) of 0.05 IU/cell (infectious unit per cell). At the indicated time points post-infection, the culture supernatants were collected and used for viral titer detection. To determine the virus titer, 1 × 105 BHK21NS1 cells were seeded into a 24-well plate with coverslips. The cells were infected with the virus of different dilutions for 1 h at 37 °C and covered with 2% methyl cellulose for culturing for 1 day. Infected cells were washed three times with PBS, fixed with 5% acetone, and then subjected to IFA to count the number of NS3-positive foci.
Luciferase Assay
BHK21NS1 cells infected by OHFV-ΔNS1-Gluc were lysed with 1 × lysis buffer (Thermo Fisher Scientific). The luciferase activity of the cell extracts was assayed by mixing 20 μL lysate with 50 μL substrate, followed by incubation for 10 min for signal stabilization and detection of the light output using a Multimode Microplate Reader (Varioskan Flash, Thermo Fisher Scientific).
Antiviral Treatment for Complemented Virus with Gluc Reporter Gene
BHK21NS1 cells were seeded into 12-well plates at a density of 1 × 105 cells/well. Next, the cells were infected with OHFV-ΔNS1-Gluc virus at an MOI of 0.1 IU/cell and cultured in medium containing different concentrations of NITD008. After 48 h of treatment, the cell lysates were obtained, and luciferase activity was measured as described above. The 50% effective concentration (EC50) was calculated with GraphPad Prism software 5.0 (GraphPad, Inc., La Jolla, CA, USA).
HTS Assays
For HTS assays, 5000, 7500, or 10,000 BHK21NS1 cells were plated into 96-well plates at the indicated densities per well and incubated for 24 h. Next, the cells were infected with OHFV-ΔNS1-Gluc virus at an MOI of 0.1 IU/cell and cultured in the presence of dimethyl sulfoxide or 3 μmol/L of NITD008. At 24 h post-infection (hpi), the infected cells were lysed, and luciferase activity was measured. All luciferase assays were performed with 6 replicates.
Results
Complementation of Replication-defective OHFV-ΔNS1 with Entire NS1 in Trans
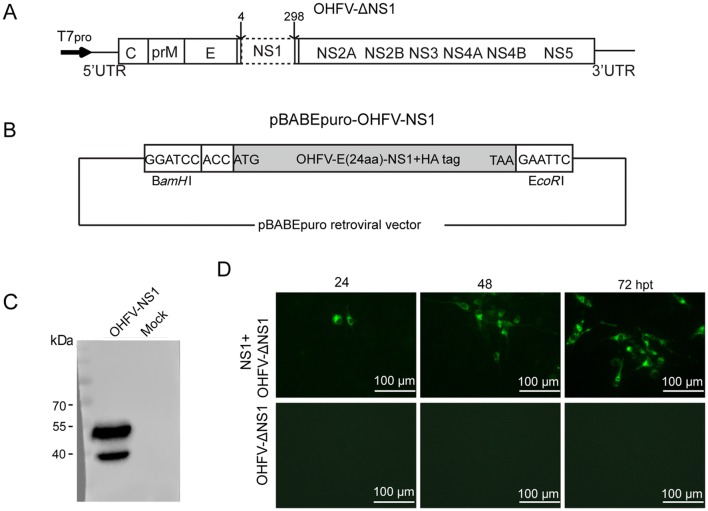
Based on the results of efficient trans complementation of NS1 protein on YFV and WNV RNA with a large in-frame deletion in the NS1 gene generating replication defective viruses (Lindenbach and Rice 1997; Khromykh et al.2000; Zhang et al.2017a), we applied a similar strategy for establishing a replication-defective virus system of OHFV. A cDNA clone of OHFV-ΔNS1 with deletion of the 4–298 aa in the NS1 gene (Fig. 1A) was first prepared in a background of the full-length cDNA clone of the OHFV strain Guriev (OHF-IC), which was constructed by inserting the T7 promoter as well as T7 terminator and HDVr sequence at the 5′ and 3′ ends of the genome, respectively (Yoshii et al.2011). To efficiently express OHFV NS1 protein, we used a retroviral vector system to construct the pBABEpuro-OHFV-NS1 expression plasmid containing the last 24 aa of E at the N-terminal to ensure the proper localization of NS1 and the presence of an HA-tag at the C-terminal for convenient detection of expression (Fig. 1B).
Fig. 1.
Trans complementation of OHFV-ΔNS1 RNA with exogenous expression of NS1. A Schematic of the construction of OHFV-ΔNS1 clone. By fusion PCR, aa 4–298 in the NS1 gene were deleted using the full-length infectious clone as a template. Deletion sites are represented by a dotted box. B Schematic of the expression plasmid of OHFV-NS1. pBABEpuro retroviral vector and BamH I/EcoR I sites were used for clone construction. The cassette includes full-length NS1 with N-terminal 24 aa of E sequence and C-terminal HA-tag. C Detection of expression of OHFV-NS1 by Western blotting assay using anti-HA antibody. DTrans complementation of OHFV-ΔNS1 with exogenous expression of NS1. BHK21 cells were sequentially transfected with 2 μg pBABEpuro-OHFV-NS1 plasmid and 1 μg OHFV-ΔNS1 RNA, and NS3 expression was analyzed by IFA at different times post-transfection. As a negative control, 1 μg OHFV-ΔNS1 RNA was transfected into BHK21 cells.
To determine the expression of NS1, BHK21 cells transfected with pBABEpuro-OHFV-NS1 plasmid were analyzed by Western blotting at 36 hpt. Because of the N-linked glycosylation of NS1, two forms of NS1 (approximately 39 kDa and 47 kDa) were observed (Blitvich et al.1999) (Fig. 1C). To assess trans-complementation, NS1 expression plasmids and in vitro-transcribed recombinant OHFV-ΔNS1 RNA were sequentially transfected into BHK21 cells and an equal amount of OHFV-ΔNS1 RNA was transfected into BHK21 cells. IFA for complementation of NS1 for OHFV-ΔNS1 using an anti-OHFV-NS3 antibody revealed no IFA-positive cells in cells transfected with OHFV-ΔNS1 RNA alone (Fig. 1D), demonstrating that deletion of the NS1 gene abrogated RNA replication. In contrast, IFA-positive cells were observed for cells which co-transfected with the OHFV-NS1 expression plasmid and OHFV-ΔNS1 RNA, demonstrating that the replication defects of OHFV-ΔNS1 can be trans-complemented efficiently by exogenous expression of NS1. Additionally, the number of positive cells increased from 24 to 72 hpt, indicating that OHFV-ΔNS1 RNA can be packaged into a defective virus and propagated in the cells expressing homologous NS1 protein.
Generation and Characterization of a Stable BHK21 Cell Line Expressing OHFV-NS1
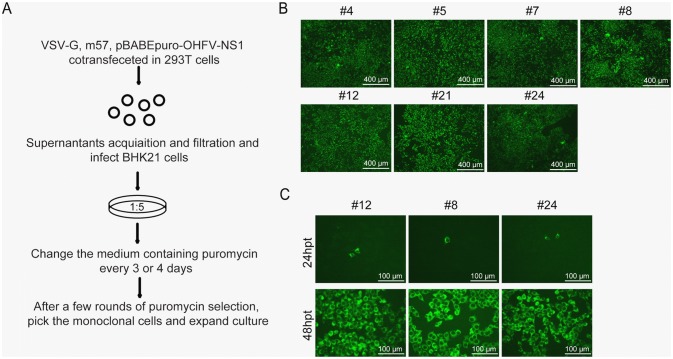
To improve the trans-complementation efficiency and constantly obtain defective virus of high yield, we attempted to establish a stable BHK21 cell line that could continuously and stably express NS1 using the retrovirus gene transfer system (Morgenstern and Land 1990; Zhang et al.2017a) (Fig. 2A). Twenty-five resistant monoclonal cell clusters were selected and expanded. Seven cell lines (labeled as #4, #5, #7, #8, #12, #21, and #24) from total 25 selected cell lines showed 100% IFA-positive cells using the anti-HA antibody (Fig. 2B). To test the efficiency of trans complementation, OHFV-ΔNS1 RNA was transfected into these seven cell lines and viral protein expression was visualized by IFA. Three cell lines (#8, #12, and #24) showed high complementary efficiency, as increasing numbers of IFA-positive cells were observed from 24 to 48 hpt (Fig. 2C). Cell line #8 was selected arbitrarily for subsequent analysis and designated as BHK21NS1.
Fig. 2.
Generation and characterization of BHK21 cell line stably expressing OHFV-NS1. A Flowchart for cell line selection. VSV-G, m57, and pBABEpuro-OHFV-NS1 plasmids were co-transfected into 293T cells, and obtained retroviral supernatants were filtered with a 0.45-μm filter. BHK21 cells were infected with recombinant retroviral virus containing polybrene. After 24 h, cells were cultured in a medium containing 8 μg/mL puromycin. After several rounds of selection, visible monoclonal cells were picked and propagated. B Selected cell clones were subjected to IFA to determine the expression levels of NS1 using anti-HA antibody. The figure shows 7 cell lines that were 100% IFA positive. C Generation of OHFV-ΔNS1 virus in BHK21NS1 cells. Obtained cell lines were transfected with 1 μg recombinant OHFV-ΔNS1 RNA. Transfected cells were subjected to IFA at 24 and 48 hpt using anti-NS3 antibody.
Characterization of Trans-complemented Replication-defective OHFV-ΔNS1 Virus
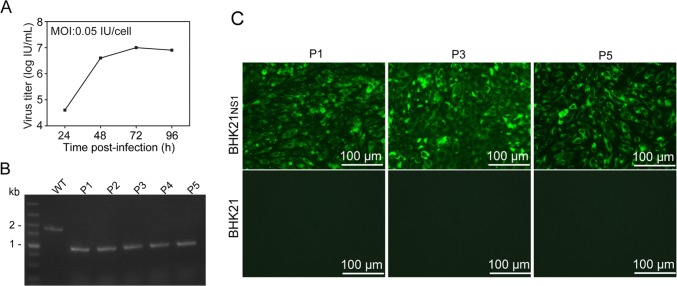
To confirm that defective OHFV-ΔNS1 virus was propagated only within the BHK21NS1 cell line, supernatants from OHFV-ΔNS1 RNA-transfected BHK21NS1 cells were used to infect naïve BHK21 cells and BHK21NS1 cells. As expected, IFA-positive cells were only detected in BHK21NS1 but not in BHK21 cells, suggesting that complemented virus was produced constantly by complementation with NS1 in BHK21NS1 cells and replication of OHFV-ΔNS1 virus was confined to BHK21NS1 cells. BHK21NS1 cells were infected and the growth properties of OHFV-ΔNS1 virus were analyzed over time. The virus titer of OHFV-ΔNS1 reached 107 IU/mL at 72 hpi (Fig. 3A), indicating that the complemented OHFV-ΔNS1 defective virus replicated efficiently in BHK21NS1 cells.
Fig. 3.
Characterization of complemented-defective OHFV-ΔNS1 virus. A Growth kinetics of OHFV-ΔNS1 virus in BHK21NS1 cells. B Genetic stability of OHFV-ΔNS1 virus. Total RNA was extracted from BHK21NS1 cells infected with P1–P5 viruses. RT-PCR was performed with primer pairs spanning E and NS2A. As a control, WT represents the products obtained by PCR using OHF-IC as a template. C Stability and biosafety of defective OHFV-ΔNS1 virus. BHK21NS1 and BHK21 cells were infected with equal volumes of P1, P3, and P5 OHFV-ΔNS1 virus, followed by IFA analysis.
To test the stability and biosafety of this complemented virus, the supernatants collected from OHFV-ΔNS1 RNA transfected BHK21NS1 were designated as P0 and subjected to continuous passaging in BHK21NS1 cells. Viral RNA from P1–P5 was subjected to RT-PCR with primers spanning the E and NS2A region. An approximately 1-kb product from P1 to P5 was observed, which was smaller than that obtained using wild-type cDNA as a template (Fig. 3B). The product of P5 virus was sequenced without reversion, suggesting that deletion of NS1 was stably maintained and no reversion occurred. Additionally, supernatants from P1, P3 and P5 were used to infect fresh BHK21NS1 and BHK21 cells. Comparable IFA-positive cells were only observed in BHK21NS1, but not in BHK21 cells (Fig. 3C), conforming that the complemented replication-defective OHFV-ΔNS1 virus did not revert to the virulent wild-type virus for at least 5 passages. These results demonstrate the stability and safety of defective OHFV-ΔNS1 virus.
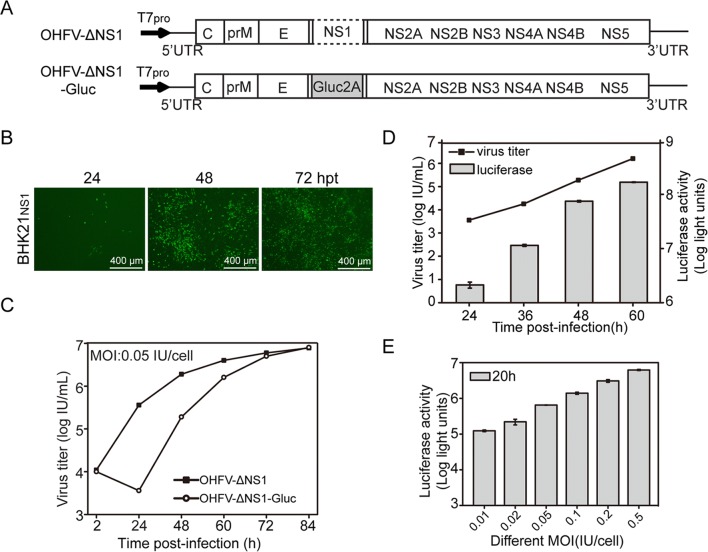
Generation and Characterization of Complemented Replication-defective OHFV-ΔNS1-Gluc Reporter Virus
To establish an OHFV high-throughput screening platform, we constructed OHFV-ΔNS1-Gluc by inserting the Gaussia luciferase (Gluc) reporter gene to replace NS1 (Fig. 4A). IFA-positive BHK21NS1 cells transfected with OHFV-ΔNS1-Gluc RNA increased from 24 to 72 hpt, indicating that OHFV-ΔNS1-Gluc RNA was trans complemented by NS1 and the defective OHFV-ΔNS1-Gluc virus was produced efficiently (Fig. 4B). To compare the growth kinetics between complemented OHFV-ΔNS1 and OHFV-ΔNS1-Gluc virus, BHK21NS1 cells were infected with the two viruses. As shown in Fig. 4C, the titer of OHFV-ΔNS1-Gluc was tenfold lower than that of OHFV-ΔNS1 before 60 hpi, with no significant replication difference after 72 hpi, demonstrating that the Gluc insertion had a subtle effect on the complementation efficiency of the defective virus. We then determined whether the Gluc signal was correlated with viral replication within the OHFV-ΔNS1-Gluc virus-infected BHKNS1 cell line. As shown in Fig. 4D, the luciferase signal was increased in proportion with the virus titer in culture. Additionally, the Gluc signal from BHK21NS1 cells infected with different MOIs of viruses was elevated with an increasing viral load (Fig. 4E). Thus, the defective OHFV-ΔNS1-Gluc reporter virus was replication-competent and propagated efficiently within BHK21NS1 cells, and replication of the OHFV-ΔNS1-Gluc reporter virus was surrogated by Gluc signals.
Fig. 4.
Generation and characterization of complemented-defective OHFV-ΔNS1-Gluc virus. A Schematic of construction of OHFV-ΔNS1-Gluc clone. The Gluc2A sequences were inserted to replace the NS1 gene. B Generation of complemented OHFV-ΔNS1-Gluc virus. OHFV-ΔNS1-Gluc RNA was transfected into BHK21NS1 cells and NS3 expression was analyzed by IFA at different times post-transfection. C Comparison of growth kinetics between complemented OHFV-ΔNS1 and OHFV-ΔNS1-Gluc virus in BHK21NS1 cells. BHK21NS1 cells were infected at MOI of 0.05 IU/cell. Supernatants at indicated times were harvested and titers were determined as described in “Materials and Methods” section. D Correlation between viral titer and Gluc signals of defective OHFV-ΔNS1-Gluc virus in BHK21NS1 cells. BHK21NS1 cells were infected with OHFV-ΔNS1-Gluc virus at MOI of 0.05 IU/cell in a 12-well format. Supernatants and cell lysates were collected at indicated times. The titer of supernatants and Gluc signals of cell lysates were determined as described in “Materials and Methods” section. The data shown are the mean values of triplicate measurements with error bars showing standard deviation. E Correlation between Gluc activity and viral load of OHFV-ΔNS1-Gluc virus in BHK21NS1 cells. BHK21NS1 cells were infected with OHFV-ΔNS1-Gluc virus at MOI of 0.01, 0.02, 0.05, 0.1, 0.2, and 0.5 IU/cell in a 12-well format. At 20 hpi, cell lysates were collected and analyzed for Gluc activity. The data shown are the mean values of triplicate measurements with error bars showing standard deviation.
We also tested the stability of the OHFV-ΔNS1-Gluc reporter virus. P0 supernatants were blind-passaged in BHK21NS1 cells. Continuous strong luciferase activities were observed in BHK21NS1 cells infected with different passaging viruses, indicating that the reporter gene was stably maintained (Fig. 5A). To further confirm the stability of Gluc, total RNA was extracted for RT-PCR. The expected 1.5-kb products of OHFV-ΔNS1-Gluc viruses were observed, which were smaller than those of the wild-type (1.8-kb) and larger than those of OHFV-ΔNS1 (1-kb) (Fig. 5B). Sequencing of P5 without NS1 reversion and Gluc deletion suggested that the OHFV-ΔNS1-Gluc reporter virus is stable for at least 5 passages.
Fig. 5.
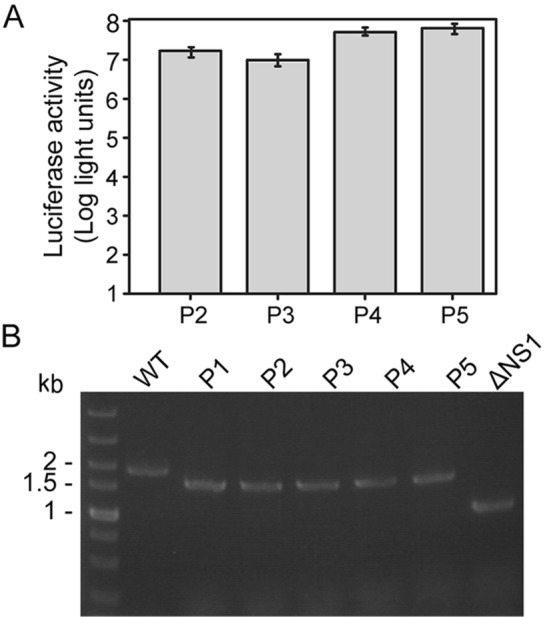
Characterization of stability and safety of complemented-defective OHFV-ΔNS1-Gluc virus. A Gluc signals of OHFV-ΔNS1-Gluc viruses during passaging. The OHFV-ΔNS1-Gluc virus was passaged for five rounds in BHK21NS1 cells and cell lysates were obtained at 72 hpi. Data shown are the mean values of triplicate measurements with error bars showing standard deviation. B Genetic stability of Gluc reporter gene of passaged reporter virus. Total RNA was extracted from BHK21NS1 cells infected with passaging OHFV-ΔNS1-Gluc virus and RT-PCR was performed. As a control, WT represents the products obtained by PCR using OHF-IC cDNA as a template and ΔNS1 represents the products of RT-PCR with OHFV-ΔNS1 RNA. The products size of WT, P1–P5, and ΔNS1 were 1.8, 1.5, and 1 kb, respectively.
Antiviral Assay of Defective OHFV-ΔNS1-Gluc Reporter Virus
Reporter viruses are powerful tools for rapid antiviral compound screening (Shang et al.2013; Xu et al.2015; Li et al.2017; Zhang et al.2017a). To validate whether this defective OHFV-ΔNS1-Gluc reporter virus can be used for antiviral assays, we used NITD008 to assess the performance of OHFV-ΔNS1-Gluc reporter virus in antiviral screening. NITD008, a mosquito-borne flavivirus antiviral (Yin et al.2009), suppressed the replication of tick-borne flavivirus such as OHFV in vitro (Lo et al.2016). With antiviral assay, Gluc activities were decreased in an NITD008 concentration-dependent manner (Fig. 6A). The EC50 was 0.15 μmol/L, which was similar to the value of the cell-based flavivirus immunodetection EC50 (Lo et al.2016).
Fig. 6.
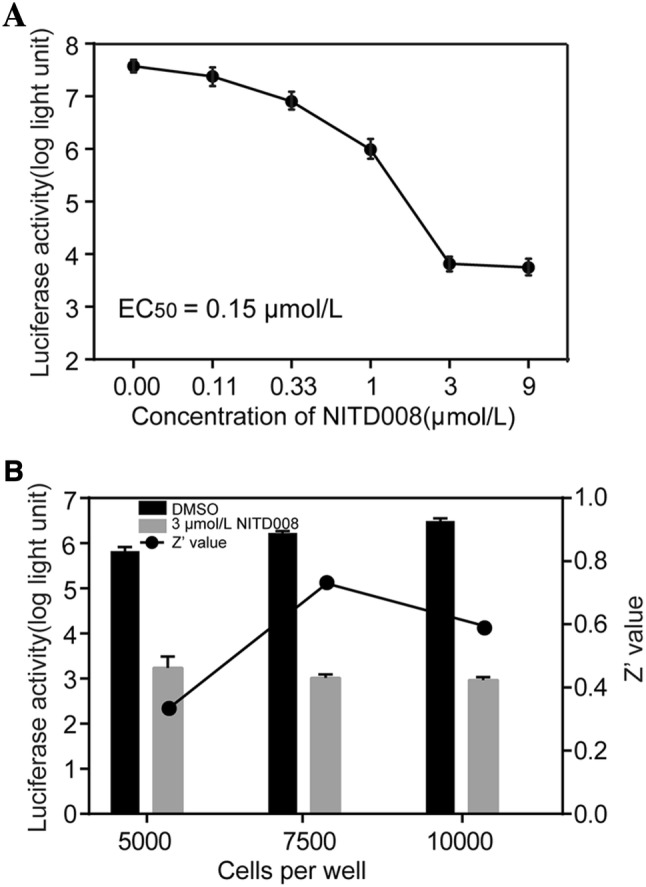
Antiviral activity of NITD008 on OHFV-ΔNS1-Gluc virus in BHK21NS1 cells. A Antiviral activity of NITD008 on OHFV-ΔNS1-Gluc virus replication. BHK21NS1 cells were infected with OHFV-ΔNS1-Gluc virus and incubated with different concentrations of NITD008. After 48 h, cells were lysed and Gluc activity was examined. Three independent experiments were performed in duplicate, with error bars indicating standard deviation. B Optimization of HTS assay using OHFV-ΔNS1-Gluc viruses. Different densities of BHK21NS1 cells were seeded into a 96-well plate. Cells were infected with OHFV-ΔNS1-Gluc virus and incubated with a medium containing 3 μmol/L NITD008. At 24 hpi, the cells were lysed and assayed for luciferase activity. The Z′ value was calculated to evaluate the effectiveness of the HTS assay.
The defective virus-based HTS assay was conducted in a 96-well plate format using NITD008 as a positive control drug using different numbers of BHK21NS1 cells in each well. After 24 h, the cells were incubated in medium containing virus and NITD008 or DMSO. As shown in Fig. 6B, the Z′ values were > 0.5 in wells of seeded with 7500 and 10,000 cells, suggesting that the HTS assay was reliable under these two conditions for detecting the inhibitory effect of NITD008. For 10,000 cells/well and 24 h incubation, we confirmed that the replication-defective OHFV-ΔNS1-Gluc reporter virus can be used for HTS assays in a 96-well plate format to screen for inhibitors of OHFV.
Discussion
OHFV is classified as a BSL4 virus; the requirement for BSL4 containment facilities has prevented progress in OHFV research. Thus, an alternative to the authentic virus is needed. In this study, we generated safe and stable replication-defective OHFV-ΔNS1 and OHFV-ΔNS1-Gluc viruses for studying virus replication and antiviral screening in BSL2 laboratories.
Replicons, the VLP system, and defective viruses are powerful tools for studying viral replication, antiviral screening, and vaccine candidate development for many flaviviruses (Lo et al.2003; Hayasaka et al.2004; Qing et al.2010; Zhang et al.2017a, c; Li et al.2018; Salat et al.2018). Because they lack capsid genes, YFV- and WNV-defective viruses have been generated as vaccine candidates in trans-complementing cell lines expressing high levels of the capsid or all three viral structural proteins (Mason et al.2006). Moreover, replication-defective virus genomic WNV RNA with a range of large deletions in NS1 was successfully trans-complemented using a replicon cell line or by foreign expression of NS1 (Khromykh et al.2000; Zhang et al.2017a). The defective viruses generated by these complementation strategies exhibit genetic stability and biosafety, making them useful for HTS of antiviral compounds in BSL2 laboratories.
Previous studies showed that for WNV virus, approximately 84%–97% large-frame deletions in the NS1 gene can be efficiently complemented by exogenous NS1 expression (Khromykh et al.2000; Zhang et al.2017a). Here, we constructed the cDNA clone of OHFV with deletion of the NS1 gene (4–295 aa). The first three amino acids of NS1 were retained to ensure proper cleavage by cellular signal peptidase, and the presence of the C-terminus of NS1 was essential for efficient trans complementation (Khromykh et al.2000). Through sequential transfection, recombinant OHFV-ΔNS1 RNA was trans-complemented efficiently by exogenous expression of NS1 protein (Fig. 1D). By generating a BHK21NS1 cell line continuously expressing NS1, the yield of OHFV-ΔNS1 virus was improved (Fig. 2). Additionally, this defective virus stably and efficiently replicated in BHK21NS1 cells with no recombination within five rounds of passaging, indicating its potential as a vaccine candidate (Fig. 3). This complemented OHFV-ΔNS1 defective virus will be a powerful tool for studying the replication mechanism and pathogenesis of OHFV in BSL2 laboratories.
To achieve HTS for OHFV inhibitors, complemented OHFV-ΔNS1-Gluc virus with a Gluc reporter gene was obtained. Because of the plasticity of the NS1 gene which can highly tolerate the insertion of foreign genes (Eyre et al.2017), we inserted Gluc2A sequences to replace NS1 (Fig. 4A), which differed from previous strategies of inserting a reporter gene between the 5′ untranslated region and structural gene (Shang et al.2013; Xu et al.2015; Zhang et al.2017a). The OHFV-ΔNS1-Gluc virus showed comparable replication characteristics to OHFV-ΔNS1 virus (Fig. 4C). By monitoring the Gluc activity of cells containing different virus loads, we found that replication of this defective virus was effectively reflected by Gluc signals (Fig. 4D, 4E). Additionally, this defective OHFV-ΔNS1-Gluc virus produced steady and robust luciferase activity for 5 rounds of passaging in BHK21NS1 cells (Fig. 5), displaying relatively good genetic stability.
The inhibition effect of NITD008 on OHFV-ΔNS1-Gluc replication was concentration-dependent (Fig. 6A). In a 96-well format, we optimized the parameters of the HTS assay and found that the Z′ value was between 0.5 and 1, revealing that this complemented reporter virus can be used for HTS screening of OHFV inhibitors (Fig. 6B).
In conclusion, we constructed stable, safe defective OHFV-ΔNS1 and OHFV-ΔNS1-Gluc viruses that can be handled under BSL2 conditions for at least 5 passages. This novel complemented replication-defective system is a powerful tool for researching virus replication, pathogenesis, and HTS of antiviral compounds for OHFV.
Acknowledgements
This work was supported by National Science and Technology Major Project on Important Infectious Diseases Prevention and Control (2018ZX10734404-010) and National Key Research and Development Program of China (2018YFA0507201). We thank the Center for Instrumental Analysis and Metrology, Wuhan Institute of Virology, Wuhan National Biosafety Level 4 Lab of CAS and Wuhan Key Laboratory of Special Pathogens and Biosafety for helpful assistance during the course of the work.
Author Contributions
BZ designed the experiments. QZ, NL, CD, and ZZ carried out the experiments. HY, and BZ analyzed the data. QZ, XL, CD, and BZ wrote the paper. All authors read and approved the final manuscript.
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflict of interest.
Animal and Human Rights Statement
This article does not contain any studies with human or animal subjects performed by any of the authors.
References
- Blitvich BJ, Scanlon D, Shiell BJ, Mackenzie JS, Hall RA. Identification and analysis of truncated and elongated species of the flavivirus NS1 protein. Virus Res. 1999;60:67–79. doi: 10.1016/S0168-1702(99)00003-9. [DOI] [PubMed] [Google Scholar]
- Charrel RN, Attoui H, Butenko AM, Clegg JC, Deubel V, Frolova TV, Gould EA, Gritsun TS, Heinz FX, Labuda M, Lashkevich VA, Loktev V, Lundkvist A, Lvov DV, Mandl CW, Niedrig M, Papa A, Petrov VS, Plyusnin A, Randolph S, Suss J, Zlobin VI, de Lamballerie X. Tick-borne virus diseases of human interest in Europe. Clin Microbiol Infect. 2004;10:1040–1055. doi: 10.1111/j.1469-0691.2004.01022.x. [DOI] [PubMed] [Google Scholar]
- Dobler G. Zoonotic tick-borne flaviviruses. Vet Microbiol. 2010;140:221–228. doi: 10.1016/j.vetmic.2009.08.024. [DOI] [PubMed] [Google Scholar]
- Eyre NS, Johnson SM, Eltahla AA, Aloi M, Aloia AL, McDevitt CA, Bull RA, Beard MR. Genome-wide mutagenesis of dengue virus reveals plasticity of the NS1 protein and enables generation of infectious tagged reporter viruses. J Virol. 2017;91:e01455-17. doi: 10.1128/JVI.01455-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halfmann P, Kim JH, Ebihara H, Noda T, Neumann G, Feldmann H, Kawaoka Y. Generation of biologically contained Ebola viruses. Proc Natl Acad Sci USA. 2008;105:1129–1133. doi: 10.1073/pnas.0708057105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayasaka D, Yoshii K, Ueki T, Iwasaki T, Takashima I. Sub-genomic replicons of Tick-borne encephalitis virus. Arch Virol. 2004;149:1245–1256. doi: 10.1007/s00705-003-0262-y. [DOI] [PubMed] [Google Scholar]
- Khromykh AA, Sedlak PL, Westaway EG. cis- and trans-acting elements in flavivirus RNA replication. J Virol. 2000;74:3253–3263. doi: 10.1128/JVI.74.7.3253-3263.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lani R, Moghaddam E, Haghani A, Chang LY, AbuBakar S, Zandi K. Tick-borne viruses: a review from the perspective of therapeutic approaches. Ticks Tick Borne Dis. 2014;5:457–465. doi: 10.1016/j.ttbdis.2014.04.001. [DOI] [PubMed] [Google Scholar]
- Li XF, Li XD, Deng CL, Dong HL, Zhang QY, Ye Q, Ye HQ, Huang XY, Deng YQ, Zhang B, Qin CF. Visualization of a neurotropic flavivirus infection in mouse reveals unique viscerotropism controlled by host type I interferon signaling. Theranostics. 2017;7:912–925. doi: 10.7150/thno.16615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li JQ, Deng CL, Gu D, Li X, Shi L, He J, Zhang QY, Zhang B, Ye HQ. Development of a replicon cell line-based high throughput antiviral assay for screening inhibitors of Zika virus. Antivir Res. 2018;150:148–154. doi: 10.1016/j.antiviral.2017.12.017. [DOI] [PubMed] [Google Scholar]
- Lindenbach BD, Rice CM. trans-Complementation of yellow fever virus NS1 reveals a role in early RNA replication. J Virol. 1997;71:9608–9617. doi: 10.1128/jvi.71.12.9608-9617.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lo MK, Tilgner M, Bernard KA, Shi PY. Functional analysis of mosquito-borne flavivirus conserved sequence elements within 3′ untranslated region of West Nile virus by use of a reporting replicon that differentiates between viral translation and RNA replication. J Virol. 2003;77:10004–10014. doi: 10.1128/JVI.77.18.10004-10014.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lo MK, Shi PY, Chen YL, Flint M, Spiropoulou CF. In vitro antiviral activity of adenosine analog NITD008 against tick-borne flaviviruses. Antivir Res. 2016;130:46–49. doi: 10.1016/j.antiviral.2016.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mason PW, Shustov AV, Frolov I. Production and characterization of vaccines based on flaviviruses defective in replication. Virology. 2006;351:432–443. doi: 10.1016/j.virol.2006.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgenstern JP, Land H. Advanced mammalian gene transfer: high titre retroviral vectors with multiple drug selection markers and a complementary helper-free packaging cell line. Nucleic Acids Res. 1990;18:3587–3596. doi: 10.1093/nar/18.12.3587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orlinger KK, Hofmeister Y, Fritz R, Holzer GW, Falkner FG, Unger B, Loew-Baselli A, Poellabauer EM, Ehrlich HJ, Barrett PN, Kreil TR. A tick-borne encephalitis virus vaccine based on the European prototype strain induces broadly reactive cross-neutralizing antibodies in humans. J Infect Dis. 2011;203:1556–1564. doi: 10.1093/infdis/jir122. [DOI] [PubMed] [Google Scholar]
- Pierson TC, Sanchez MD, Puffer BA, Ahmed AA, Geiss BJ, Valentine LE, Altamura LA, Diamond MS, Doms RW. A rapid and quantitative assay for measuring antibody-mediated neutralization of West Nile virus infection. Virology. 2006;346:53–65. doi: 10.1016/j.virol.2005.10.030. [DOI] [PubMed] [Google Scholar]
- Pohjala L, Utt A, Varjak M, Lulla A, Merits A, Ahola T, Tammela P. Inhibitors of alphavirus entry and replication identified with a stable Chikungunya replicon cell line and virus-based assays. PLoS ONE. 2011;6:e28923. doi: 10.1371/journal.pone.0028923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qing M, Liu W, Yuan Z, Gu F, Shi PY. A high-throughput assay using dengue-1 virus-like particles for drug discovery. Antivir Res. 2010;86:163–171. doi: 10.1016/j.antiviral.2010.02.313. [DOI] [PubMed] [Google Scholar]
- Ruzek D, Yakimenko VV, Karan LS, Tkachev SE. Omsk haemorrhagic fever. Lancet. 2010;376:2104–2113. doi: 10.1016/S0140-6736(10)61120-8. [DOI] [PubMed] [Google Scholar]
- Salat J, Formanova P, Hunady M, Eyer L, Palus M, Ruzek D. Development and testing of a new tick-borne encephalitis virus vaccine candidate for veterinary use. Vaccine. 2018;36:7257–7261. doi: 10.1016/j.vaccine.2018.10.034. [DOI] [PubMed] [Google Scholar]
- Scholle F, Girard YA, Zhao Q, Higgs S, Mason PW. trans-Packaged West Nile virus-like particles: infectious properties in vitro and in infected mosquito vectors. J Virol. 2004;78:11605–11614. doi: 10.1128/JVI.78.21.11605-11614.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shang B, Deng C, Ye H, Xu W, Yuan Z, Shi PY, Zhang B. Development and characterization of a stable eGFP enterovirus 71 for antiviral screening. Antivir Res. 2013;97:198–205. doi: 10.1016/j.antiviral.2012.12.010. [DOI] [PubMed] [Google Scholar]
- Shi PY, Tilgner M, Lo MK. Construction and characterization of subgenomic replicons of New York strain of West Nile virus. Virology. 2002;296:219–233. doi: 10.1006/viro.2002.1453. [DOI] [PubMed] [Google Scholar]
- Si L, Xu H, Zhou X, Zhang Z, Tian Z, Wang Y, Wu Y, Zhang B, Niu Z, Zhang C, Fu G, Xiao S, Xia Q, Zhang L, Zhou D. Generation of influenza A viruses as live but replication-incompetent virus vaccines. Science. 2016;354:1170–1173. doi: 10.1126/science.aah5869. [DOI] [PubMed] [Google Scholar]
- Wang SR, Zhang QY, Wang JQ, Ge XY, Song YY, Wang YF, Li XD, Fu BS, Xu GH, Shu B, Gong P, Zhang B, Tian T, Zhou X. Chemical targeting of a G-quadruplex RNA in the Ebola virus L gene. Cell Chem Biol. 2016;23:1113–1122. doi: 10.1016/j.chembiol.2016.07.019. [DOI] [PubMed] [Google Scholar]
- Xu LL, Shan C, Deng CL, Li XD, Shang BD, Ye HQ, Liu SQ, Yuan ZM, Wang QY, Shi PY, Zhang B. Development of a stable Gaussia luciferase enterovirus 71 reporter virus. J Virol Methods. 2015;219:62–66. doi: 10.1016/j.jviromet.2015.03.020. [DOI] [PubMed] [Google Scholar]
- Yin Z, Chen YL, Schul W, Wang QY, Gu F, Duraiswamy J, Kondreddi RR, Niyomrattanakit P, Lakshminarayana SB, Goh A, Xu HY, Liu W, Liu B, Lim JY, Ng CY, Qing M, Lim CC, Yip A, Wang G, Chan WL, Tan HP, Lin K, Zhang B, Zou G, Bernard KA, Garrett C, Beltz K, Dong M, Weaver M, He H, Pichota A, Dartois V, Keller TH, Shi PY. An adenosine nucleoside inhibitor of dengue virus. Proc Natl Acad Sci USA. 2009;106:20435–20439. doi: 10.1073/pnas.0907010106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoshii K, Holbrook MR. Sub-genomic replicon and virus-like particles of Omsk hemorrhagic fever virus. Arch Virol. 2009;154:573–580. doi: 10.1007/s00705-009-0345-5. [DOI] [PubMed] [Google Scholar]
- Yoshii K, Ikawa A, Chiba Y, Omori Y, Maeda J, Murata R, Kariwa H, Takashima I. Establishment of a neutralization test involving reporter gene-expressing virus-like particles of tick-borne encephalitis virus. J Virol Methods. 2009;161:173–176. doi: 10.1016/j.jviromet.2009.05.016. [DOI] [PubMed] [Google Scholar]
- Yoshii K, Igarashi M, Ito K, Kariwa H, Holbrook MR, Takashima I. Construction of an infectious cDNA clone for Omsk hemorrhagic fever virus, and characterization of mutations in NS2A and NS5. Virus Res. 2011;155:61–68. doi: 10.1016/j.virusres.2010.08.023. [DOI] [PubMed] [Google Scholar]
- Youn S, Li T, McCune BT, Edeling MA, Fremont DH, Cristea IM, Diamond MS. Evidence for a genetic and physical interaction between nonstructural proteins NS1 and NS4B that modulates replication of West Nile virus. J Virol. 2012;86:7360–7371. doi: 10.1128/JVI.00157-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang HL, Ye HQ, Deng CL, Liu SQ, Shi PY, Qin CF, Yuan ZM, Zhang B. Generation and characterization of West Nile pseudo-infectious reporter virus for antiviral screening. Antivir Res. 2017;141:38–47. doi: 10.1016/j.antiviral.2017.02.006. [DOI] [PubMed] [Google Scholar]
- Zhang HL, Ye HQ, Liu SQ, Deng CL, Li XD, Shi PY, Zhang B. West Nile virus NS1 antagonizes interferon beta production by targeting RIG-I and MDA5. J Virol. 2017;91:e02396-16. doi: 10.1128/JVI.02396-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang QY, Li XD, Liu SQ, Deng CL, Zhang B, Ye HQ. Development of a stable Japanese encephalitis virus replicon cell line for antiviral screening. Arch Virol. 2017;162:3417–3423. doi: 10.1007/s00705-017-3508-9. [DOI] [PubMed] [Google Scholar]