Abstract
This paper describes a mental health capacity-building partnership between the University of Nairobi (UON) and the University of Washington (UW) that was built upon a foundational 30-year HIV/AIDS research training collaboration between the two institutions. With funding from the US National Institute of Mental Health Medical Education Program Initiative (MEPI), UW and UON faculty collaborated to develop and offer a series of workshops in research methods, grant writing, and manuscript publication for UON faculty and post-graduate students committed to mental health research. UON and UW scientists provided ongoing mentorship to UON trainees through Skype and email. Three active thematic research groups emerged that focused on maternal and child mental health, gender-based violence, and HIV-related substance abuse. Challenges to conducting mental health research in Kenya included limited resources to support research activities, heavy teaching responsibilities, clinical duties, and administrative demands on senior faculty, and stigmatization of mental health conditions, treatment, and research within Kenyan society. The partnership yielded a number of accomplishments: a body of published papers and presentations at national and international meetings on Kenyan mental health topics, the institution of systematic mental health data collection in rural clinics, funded research proposals, and a mental health research resource centre. We highlight lessons learned for future mental health research capacity-building initiatives.
Keywords: Mental, Health, Medical, Education, Research, Collaboration
Background
The majority of Sub-Saharan countries suffer from a shortage of health workers in general (Machayo & Keraro, 2013). This shortage becomes even more acute in specialties like mental health, with untreated mental disorders accounting for a large proportion of the disease burden that afflicts the continent (Fryers, Melzer, & Jenkins, 2003; Global Burden of Disease Study 2013 Collaborators, 2015). Strong evidence demonstrates that addressing common mental disorders can help improve outcomes for people living with communicable and non-communicable diseases in a cost effective manner (Katon et al., 2012). Many countries, however, do not have mental health budgets to implement public mental health programs. Of those countries with mental health budgets, the proportion of total health expenditures designated for mental health is under 1% (Shekhar Saxena, Thornicroft, Knapp, & Whiteford, 2007).
Strengthening mental health research capacity in low resource contexts will contribute towards reducing disease burden globally (Whiteford et al., 2013). The World Health Organization-Mental Health Global Action Programme asserts that well-grounded local research is critical for identifying mental health needs, prioritizing relevant mental health problems, and developing and evaluating appropriate interventions that can be integrated into community and clinical settings (World Health Organization, 2016). Low resource settings, including Kenya, have very few health workers with specialized training in mental health care (Vasquez, Hirsch, Giang, & Parker, 2013), and among those who have received such training, only a small proportion conducts research due to the high demand for clinical services and poor access to research mentorship, funding, and materials (Pratap, Itzhak, Sylvie, Francisco, & Shekhar, 2007; S. Saxena, Paraje, Sharan, Karam, & Sadana, 2006). While low resource settings shoulder 75% of the burden of mental illness (Patel, 2007), fewer than 10% of research trials on mental health interventions occur in these settings. Between 1992 and 2001 researchers in low resource settings authored fewer than 4% of mental health-related publications (Saxena et al. 2006). The situation in Kenya is no different. A 2007 survey showed that Kenya was among 12 African countries that together contributed only 2% of the indexed mental health research articles from low and moderate resource contexts that were published from 1999–2003 (Pratap et al., 2007).
To enhance the likelihood that research will have the desired public health impact, Collins and colleagues (2013) argue that researchers need a skill set that enables them to effectively “engage community stakeholders, journalists, decision-makers, and policymaking organizations before, during, and following the completion of research activities” (Collins, 2013). Thus, an important consideration in building research capacity is to equip a workforce with methodological training that is suited to the setting and that prioritizes local health demands. While international collaboration can be a helpful resource for faculty and students to overcome impediments to the production of useful research findings, over-reliance on quantitative measures, diagnostic categories, and treatment paradigms based in western psychiatry have created cultural inappropriateness and neocolonialist frameworks that can yield uninterpretable research findings and irrelevant interventions (Horton, 2013). Research training grants require writing skills and multidisciplinary teamwork to produce and execute, which can foster overreliance upon institutions in high resource settings.
Several initiatives have been undertaken worldwide to build research capacity in low resource settings (Council on Health Research and Development 2012). These initiatives typically provide funds to individual researchers or academic institutions and offer research training and opportunities for research collaboration (Lansang & Dennis, 2004; Vasquez et al., 2013). This paper describes one such South-North collaborative mental health research capacity-building collaboration between Kenya and the U.S. We used a complementary approach that included: 1) training of individual researchers from masters to doctoral level with a small research seed grant; 2) learning by doing approach-requiring all trainees, academic or on the job mental health workers, to carry out a research project or write a grant proposal and thirdly built on a creation of a south-north partnership (Lansang & Dennis, 2004). Our collaboration was initiated in 2011 and has built a foundation upon the National Institutes of Health (NIH) Medical Education Partnership Initiative (MEPI) funding mechanism (R25 MH099132) which required that low resource setting institutions submit proposals and become the recipients of the grants, thereby developing capacity for grant and subcontract administration.
Within the partnership model, the NIH provides a multiple Principal Investigator option that “encourages collaboration among equals when that is the most appropriate way to address a scientific problem.” The Multiple PI designation provided a project framework for promoting equity across institutions and disciplines. During project implementation, decision-making at the PI, grant administration, and co-investigator levels reflected this collaborative model (NIH, 2011).
The Kenyan Context
University of Nairobi (UON) and University of Washington (UW) Research Collaboration
For over thirty years, the University of Nairobi and University of Washington have been working together to build health research capacity and conduct research in the area of HIV/AIDS. The UON/UW collaboration (Child et al., 2014) has built a significant research infrastructure within Kenya with the aid of United States government funding. Bilateral research teams have been working on infectious disease prevention and control, reproductive health, and psychosocial issues related to engagement in care in three regions: Nairobi, Kisumu, and Kilifi. During the past 25 years about 153 health workers have received training from the University of Washington through the AIDS International Training and Research Program (AITRP), funded by the Fogarty International Center at the National Institutes of Health (NIH). These are the researchers who have become the driving force in health research at the University of Nairobi (Child et al., 2014). The collaboration hosts regular training programs and workshops that cover topics such as the responsible conduct of research, implementation science, grant writing, and manuscript preparation. In addition, the UW has worked to strengthen UON administrative capacity to take on foreign research grants. The “Partnership for Medical Education in Kenya” (PRIME-K) was a MEPI collaborative research program between the two institutions that approached medical education from a multidisciplinary and community-based perspective. The main objective was to expand clinical training opportunities at the UON and other Kenyan universities through innovative training methods and community integration as potential training sites (Osanjo et al., 2015). The MEPI program also provided its participants training in rigorous research methodologies, as well as mentorship.
After the initial MEPI program was funded, the NIH announced opportunities for capacity-building in mental health research. Applications were limited to schools with a previous MEPI grant. In response to the call, the Departments of Psychiatry at UON and UW, as well as the UW Department of Global Health took advantage of the links that had been previously forged through PRIME-K.
Status of Mental Health Research in Kenya
Since 1971 the Department of Psychiatry at the University of Nairobi has been training psychiatrists, clinical psychologists, and other mental health workers. To complete their Master’s degrees in psychiatry or clinical psychology, trainees must complete a thesis based on original research. Between 1980 and 2013, 106 postgraduate theses and dissertations were completed, but only eight (7.5%) were published. In a 9 years period between 2002 and 2011 there were 49 peer reviewed publications authored by faculty within the Department of Psychiatry, compared with over 100 publications produced by the Department of Obstetrics and Gynecology at UON within a 5 year time period. Of the 49 publications from Psychiatry, one researcher served as first author for 37% of papers.
The department of Psychiatry has from the onset worked with some renowned researchers among the faculty, including being involved in international projects, few faculty however have had formal training in research methods and grant writing and those who had training were hampered in their research productivity by the real demands of their academic roles in two institutions which serve as teaching hospitals for the UON College of Health Sciences. Faculty take on heavy responsibilities for clinical teaching and supervision, clinical service, and academic program administration. Without time and resources the Department had made little progress towards developing or adapting culturally appropriate tools, intervention approaches and models for delivering mental health care in general health care facilities, schools, work and other community settings. Faculty needed grant writing skills to enable them to fund their research.
Other Barriers to Mental Health Research Capacity Building
Stigma associated with mental illness presents another significant barrier to mental health research in Kenya. This stigma discourages health care providers from entering mental health professions, people with mental illnesses from seeking treatment and disclosing their status to researchers, and researchers from focusing on mental health questions (Rüsch et al., 2014). The stigma impedes interdisciplinary dialogue between mental health specialists, (e.g., psychiatrists, psychologists, social workers, and psychiatric nurses), and researchers from other disciplines, (e.g., public health, anthropology, nursing, general, pediatric, and gynecologic medicine, and pharmacy) (Rao et al., 2012). Without interdisciplinary collaboration, the critical interplay between “physical” and “mental” health is not recognized, and mental health research and practice remain “siloed’. To expand expertise in relevant research methodologies, UON faculty needed training in both qualitative and quantitative methodologies to elucidate local mental health problems and to adapt and test culturally appropriate mental health assessment tools, interventions, and service delivery models.
Proposal Development and Project Initiation
In 2011 the UON and UW wrote a response to the NIH call for mental health research capacity-building proposals. The proposal was developed with joint input across institutions to ensure that it had local relevance for the Kenyan setting, while integrating the research and writing expertise of the multidisciplinary UW team that included co-investigators from Psychiatry, Psychology, Epidemiology, and Global Health. Two Principal Investigators from UON and UW were designated. UON was the primary grant recipient, and UW the subcontractor, with budget management onsite at UON. The objectives of the project were to train interdisciplinary groups of postgraduate trainees and faculty in mental health research methods and engage in collaborative efforts to disseminate knowledge about mental health in Kenya and conduct funded mental health research. The ultimate goal was to improve the health of Kenyans.
The project had three aims. AIM 1: Improve mental health research capacity at UON by training UON and KNH faculty in research methods, grant writing, and manuscript writing; AIM 2. Train postgraduates in mental health research through coursework and mentored research projects; and AIM 3. Establish a mental health research resource centre. A secondary aim was to train non-academic health workers in other decentralized sites in research methods and support them through a project.
Methods
Project Implementation
NIH funded the three-year MEPI-mental health research capacity-building project (R25 MH099132) with project kick-off held in August of 2012 in which the chairs of the UON and UW Departments of Psychiatry, the UW Department of Global Health participated. The project followed the process initiated by PRIME-K of an integrated approach involving multidisciplinary partners and key stakeholders from the beginning (Child et al., 2014). The Director in charge of mental health at the Ministry of Health, Kenya, representatives from the Mathari Teaching and Referral Hospital for Psychiatry, heads of departments from the different schools and representatives from two other Universities were involved in the inaugural capacity-building activities in January 2013. Mental health research capacity-building was promoted through five activities: conducting annual research training workshops for faculty and trainees at the University of Nairobi; forming thematic groups to focus research efforts on four priority areas; engaging mental health professionals from decentralized sites in research training and collaborative projects; establishing a mental health research resource centre that was accessible to UON and KNH researchers and other health workers; and providing ongoing mentorship for post-graduate trainees at UON.
UW faculty members have been onsite at the UON for two, four, and five weeks across the three successive years of the project. Over the course of the project UON faculty made two week-long visits to UW. An official visit to UW by the UON principal investigator in May 2013 helped strengthen ties and develop mutual understanding of the academic environments and work responsibilities across institutions. In 2015, two UON faculty members traveled to the UW to participate in an intensive training workshop in Interpersonal Therapy (IPT) and to consult with experts who had implemented IPT research studies to address depression in Ugandan adults and adolescents (Bass et al., 2006; Bolton et al., 2007; Verdeli et al., 2008). The face-to-face time that collaborators had at the two institutions was instrumental in fostering an understanding of differences and similarities in mental health resources and service delivery models and infrastructures for supporting research activities.
Research Methods and Writing Workshops
In each of the project years, UW and UON faculty led research methods workshops in Kenya for postgraduate trainees and faculty members with representation from six health disciplines: psychiatry, clinical psychology, public health, pharmacy, nursing, and obstetrics/gynecology. The first training workshop, held for two weeks in January 2013, was modeled after an AFYA BORA Consortium grant writing course and a UW graduate course in psychiatric epidemiology, (i.e., public mental health research methods). An extensive review of the literature yielded scientific articles about mental health conducted in Kenya and neighboring countries in East Africa. Workshops were augmented with e-learning modules available for download on the internet or cd-rom. The initial curriculum was based on a research needs assessment tool (Table 1), that was given to eight faculty involved in the study, this was then revised jointly over email and Skype discussions, and further revision occurred in-person on a day-to-day basis as the workshops progressed. A post workshop evaluation with all participants was done at the end of each workshop and this was used to modify the next workshop.
Table 1:
Research needs assessment tool
| Research Needs Assessment | Tick | |
|---|---|---|
| 1 | Basic research methods | |
| a. Quantitative methods | ||
| b. Qualitative methods | ||
| c. Mixed methods | ||
| 2 | Levels within these methodologies | |
| a. Introductory and Intermediate quantitative methods | ||
| b. Advanced quantitative methods | ||
| c. Introductory and Intermediate qualitative methods | ||
| d. Advanced qualitative methods | ||
| e. Advanced mixed methods | ||
| 3 | Ethical, human rights based and legal considerations of research | |
| 4 | Mental Health needs | |
| 5 | Critically reviewing research material | |
| a. what should the focus be on in reading MH papers? | ||
| b. parameters to evaluate research process and results? | ||
| 6 | Interdisciplinary/ multidisciplinary research in clinical health psychology | |
| a. how to make it possible | ||
| b. what elements need deliberation | ||
| c. ways of formulating and assessing various factors under study | ||
| d. research assessment | ||
| 7 | How to publish research | |
| 8 | How to write grant proposals | |
| a. identifying the appropriate grant | ||
| b. collective action | ||
| c. log framework development | ||
| d. thinking and presenting own expertise | ||
| 9 | New approaches | |
| a. Randomized controlled trials | ||
| b. Advanced introduction to RCTs | ||
| 10 | Digital Technologies and MH | |
| a. how to use literature search and digital software | ||
| b. use of videos, audios in research and teaching | ||
| c. special training for statistical software like MATLAB, SPSS, NVIVO | ||
| 11 | Basic introduction to applications and methods | |
| a. Health and Mental health challenges within nursing |
||
| b. Health and Mental Health challenges within Community social work | ||
| c. H and MH challenges in Public Health | ||
| d. Psychiatry and its interface with familial and social institutions -key issues | ||
| 12 | Thematic research areas needing focus on | |
| a. HIV : Stigma, prevention, and intervention research | ||
| b. Disaster mental health: Natural disasters and social violence | ||
| c. Maternal health | ||
| d. Domestic and sexual violence | ||
| e. Substance abuse: prevention and interventions | ||
| f. Psychotherapy process and outcome research | ||
| 13 | Research Supervision | |
| a. supervision of students | ||
| b. peer supervision | ||
| c. ethics, principles and basic guidelines | ||
In the month prior to each annual workshop, interested trainees applied to participate by submitting a research concept; 15 were selected annually by UON faculty. An important criterion for selection was that the research topics were mental health-related and focused on prioritized thematic areas of mental health issues of persons with HIV/AIDs, alcohol and substance use disorders, gender-based violence and PTSD, and maternal and child mental health.
In the workshops, instructors used problem-based and interactive pedagogical approaches with locally relevant examples from mental health studies conducted in Kenya and other sub-Saharan African countries. The workshops began with overview of why it is important to conduct research and the need for mental health research in Kenya. Subsequent sessions introduced basic quantitative and qualitative research topics of study design, sampling, mental health measurement, research ethics, sample size determination, data management and statistical analysis (See Table 2).
Table 2:
Outline of Year 1 and Year 2 Mental Health Research Methods Workshop Curriculum
| Year 1 Curriculum | Year 2 Curriculum | |
|---|---|---|
|
Mental Health Research Methods and Grant Writing Workshop |
Mental Health Research Methods Workshop |
|
| Day 1 | Overview of Global Mental Health and Mental Health in Kenya; Introductions; Why do Research? Time Management |
Overview; Introductions; Why do Research? Time Management; Ethics and Institutional Review Board Applications |
| Day 2 | Working with Collaborators and Mentors; Literature Reviews and Literature Searching Tools |
Research Questions; Study Design; |
| Thematic Group Presentations | ||
| Day 3 | Components of a Research Grant; Budgets; | Qualitative Methods |
| Day 4 | Grant Review Process; Proposal Formats | Measurement; Sampling |
| Day 5 | Individual Presentations of Aims Pages and Abstracts |
Biostatistics; Power Analysis |
| Day 6 | Research Study Designs with Student Examples |
|
| Day 7 | Journal Club, Data Collection and Recruitment; Database Management |
Scientific Writing |
| GrantWriting: Background/Introduction; Literature Searches and Reviews; Global Communication (Skype, Dropbox) | ||
| Day 8 | Culturally Appropriate Measurement | Grant Writing: Methods Sections; Aims Pages |
| Thematic Group Work | ||
| Day 9 | Sample Size Calculation; Data Analysis | Model Building; Confounders/Mediators |
| Thematic Group Work | ||
| Day 10 | Presentation of Proposals; Consultation on Sample Size; Scientific Writing |
Discussion Sections, Abstracts |
| Break Out Sections on Statistics; Evaluations |
Over the course of the three project years, responsibility for teaching topics in the workshops shifted from UW to UON faculty. In the initial year, UON faculty taught single sessions on the following topics: research ethics, sample size calculation, qualitative research methods, and literature review, while UW faculty taught multiple sessions on quantitative research methods and grant writing. In year 2, a UON faculty member was assigned to co-facilitate each of the quantitative research methods sessions with UW faculty. In year 3, UON faculty prepared for teaching by participating in coaching sessions with UW faculty and delivered all of the didactic portions of the workshop on their own. To help trainees solidify concepts, UON and UW faculty co-led discussions following didactic sessions. Table 2 also illustrates how the workshop curriculum was modified from Year 1 to Year 2 in response to UON faculty and trainee needs.
In the final project year UW faculty led two additional types of workshops: three grant-writing workshops for each of the thematic groups and a “thesis-to-publication” workshop for eight Year 1 trainees who had successfully completed their theses. The grant writing workshops included didactic content to familiarize UON thematic group members with typical grant formats and requirements. Group members selected a funding mechanism and a research topic and produced a draft of a grant proposal.
On successive days of the thesis-to-publication writing workshop, participants were introduced to techniques of writing each part of a scientific article: Introduction, Methods, Results and Discussion, and Abstract. Didactic sessions were followed by writing sessions where participants adapted parts of their theses to journal article format with consultation from UON and UW mentors. In both types of writing workshops, in the early evening, each group (grant-writing) or participant (manuscript-writing) made a brief presentation of their progress. In Years 2 and 3 trainees were encouraged to attend other manuscript writing workshops organized by PRIME-K in the UON College of Health Sciences.
Thematic Groups
The project investigators established priority areas and thematic work groups, taking into account areas of research interest and specialization at both the UON and UW. Pairs of local and UW mentors helped trainees to design and conduct their research and provided mentorship on the write-up of their results. At the end of the three-year award, all thematic groups had met separately at least once in retreats in Kenya with their respective UON/UW faculty to craft a proposal for submission for external funding of future work.
One thematic group focused on substance use disorders and HIV/AIDS. The chair of the UON Department of Psychiatry, a UW-based specialist in substance use disorders, and a local substance use disorder intervention specialist met with interested trainees individually and in groups to help them design their studies.
The second thematic group met with a UON psychiatrist and a UW-based trauma psychologist and supported trainees as they crafted projects centered around gender-based violence (GBV) research. The trainees and mentors then designed and implemented studies to identify socio-cultural reasons for delayed reporting of gender-based violence and examine the psychosocial and medical outcomes of survivors seen in a GBV clinic based in the Kenyan teaching hospital. Results of these studies are being used to improve services in the Kenyatta National Hospital’s GBV programme. In the second project year, a UW co-investigator provided a one-day training on Cognitive Processing Therapy (CPT), with case examples from CPT implementation in the Democratic Republic of Congo.
The thematic group focusing on maternal and child mental health (MCMH) convened with two clinical psychologists who were UON faculty and a UW child psychiatric epidemiologist. Members of the MCMH group were interested in the effects of pre- and post-partum depression on mothers and their infants. This important topic had received little research attention in Kenya. Trainees attached to this thematic group addressed a number of related topics, including depression screening in antenatal clinics, maternal depression and its impact on infant feeding and growth, depression in pregnant women with HIV, and parent-child attachment in Kenyan school children. The UON Department of Psychiatry has begun to collaborate with the UON Department of Obstetrics/Gynecology to broaden the scope and potential impact of antenatal depression research.
Ongoing Mentorship
Over the three-year funding period and up to the present, UON trainees have worked closely with UON faculty and UW to write collaborative manuscripts for publication based on their completed thesis research projects. Weekly consultation occurred amongst trainees at UON while field work was in process, and UW faculty members were consulted more frequently to mentor on data analysis and writing.
Engaging Mental Health Professionals from Decentralized Sites
In year 3 UON faculty recruited non-academic health workers from sites outside of Nairobi and from the Gender-Based Violence Recovery Centre at Kenyatta National Hospital to participate in mental health research capacity-building activities. Six ‘decentralized’ sites representing diversity in geographical regions were selected, and selected representatives to participate in the research methods workshop.
Establishing a Mental Health Resource Centre
To meet our third aim, the Kenyan national teaching hospital, Kenyatta National Hospital, refurbished a space to create a Mental Health Resource Centre. The Centre is stocked with relevant resource books on research methodology, training videos, computers with statistical and referencing software, and internet/e-learning materials provided by UW. The Centre is staffed by two researchers who help trainees through the process of submitting proposals for UON Ethics Committee review, managing field research stipends, reviewing literature, implementing research protocols, and conducting data entry and analysis. The resource centre has become a hub for student and faculty consultations. A second resource centre has been established at Mathari Hospital, the national psychiatric referral and teaching hospital in Nairobi.
Results
Progress towards building mental health research capacity is reflected in the generation of research products, including theses completed, manuscripts developed for publication, research grant proposals submitted and funded, and research career pathways taken. This progress is summarized in a diagram below (see Figure 1).
Figure 1.
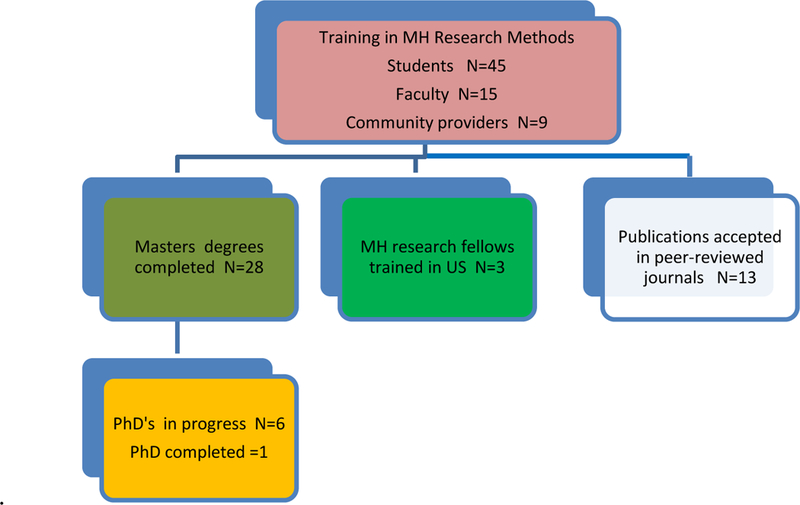
Accomplishments of MEPI mental health trainees
Workshop Participation and Thesis Completion
Over the three-year project period, a total of 45 trainees, 15 faculty, and nine non-academic health workers from remote clinical sites participated in research capacity-building activities implemented through the MEPI mental health project. Benefits to the trainees of participation included learning research methods and skills through workshop attendance, mentorship from UON and UW faculty to design and carry out thesis research projects, seed funding for conducting field research, and membership in an ongoing collaborative multidisciplinary thematic research group of UON and UW faculty and UON trainees.
Responses on daily workshop evaluations conveyed that trainees gained an appreciation of the value of conducting research and enjoyed working with mentors and a team of scientists. They also gained useful skills for searching the research literature which provided them with a strong foundation from which to generate their research questions and write their proposals (See Table 3).
Table 3:
Student Feedback after First Mental Health Research Methods Workshop
| Day | Topic/Activity | Participant Comments |
|---|---|---|
| Day 1 | Overview of Global Mental Health and Mental Health in Kenya; |
“Set a good basis for the workshop” “Set the research initiatives within a global context” “We all have a long way to go in mental health.” |
| Why Do Research? | “There are more reasons to research than I thought!” “They made research seem like an exciting activity/ demystified the complex nature of research work.” |
|
| Time Management | “Prioritizing and strategies to employ in creating time made research doable.” |
|
| Day 2 | Working with Collaborators and Mentors |
“Appreciating the concept of mentorship” |
| Literature Reviews and Literature Searching Tools Endnote Web overview |
“I learned how to look for the necessary material from PubMed” “Demystified the literature search” “Felt more competent and empowered” “How much I can actually save time” “Ahh!! The relief!! I didn’t know that referencing can be easy!” |
|
| Day 3 | Components of a Research Grant; Overview of Background, Innovation and Past Studies |
“Learned that the research has to be innovative” and “The relevance and importance of doing background research (lit review)” |
| Grant Mechanisms Available to Kenyan Investigators |
“Discovering that there are many opportunities to get grants” “I didn’t know that any qualified person can apply for a grant.” |
|
| Day 4 | Grant Review Process; Proposal Formats |
“It was a total eye-opener on how to do an eye- catching attractive grant” |
| Thematic group work session | “There were new ideas I had not considered.” “Teamwork and collaboration results in ideas exchange.” |
Research Theses, Presentations and Papers
Twenty-eight trainees who participated in the mental health research capacity-building workshops have completed their master’s theses and one has completed a PhD thesis. Strong efforts have been made towards disseminating emerging research findings locally where they have their most relevance. To date, UON workshop participants have made presentations at three local, three regional, and two international conferences where they engaged in extensive networking with other African and global mental health researchers. In 2015 the MEPI-Mental Health research capacity-building project co-sponsored the Kenya Psychiatric Association (KPA) annual conference in Eldoret, Western Kenya and contributed to eleven presentations at the conference. In 2016, in keeping with the conference theme of “Depression, a Global Crisis,” our trainees made four presentations at the annual KPA conference in Nyeri, Central Kenya. In 2017 KPA hosted the 4th annual conference of the African Association of Psychiatrists and Allied Professionals (AAPAP), where our trainees and faculty made two presentations (see Table 4).
Table 4.
Presentations at the 2015, 2016 and 2017 annual conferences of the Kenya Psychiatric Association
| Presentations at the 2015 conference of the Kenya Psychiatric Association: Eldoret Kenya | |
| Project overview | Overview and outcomes of Kenya mental health research capacity- building project, UON/UW (A. Mbwayo) |
|
Thematic Group Presentations |
Research Topic (primary author) |
| Alcohol and Substance Use Disorders |
Overview of research in alcohol and substance use disorders in Kenya (M. Kuria) |
| Substance use literacy, addiction severity and adherence to HIV medication in Naivasha district hospital (Kenya) (R, Maina) | |
| Prevalence of depression among HIV positive female injecting drug users (J. Anundo) | |
| Maternal Depression and Child Mental Health |
Attachment styles among children aged from 8 to 14 years in Nairobi, Kenya (B. Madeghe) |
| Antepartum risk factors of postpartum depression (L. Ongeri) | |
| HIV related stigma and prevalence of postpartum depression (O. Yator) | |
| Maternal depression, stunting and later cognitive deficits in children- Kitui, Kenya (E. Mbelega) | |
| Interpersonal Therapy (IPT) in the management of depression (M. Mathai) | |
| Gender-Based Violence and Trauma |
Childhood exposure to inter-parental violence as a risk factor for intimate partner violence (E. Khamba) |
| Female survivors of sexual violence and cultural and socio-economic factors that influence first visits to the Sexual Gender Violence Clinic- Nairobi (Janet-Rose Kamau) | |
| Presentations at 2016 conference of the Kenya Psychiatric Association,: Nyeri, Kenya | |
| Gender-Based Violence and Trauma |
Depression in children who have been sexually abused (T. Mutavi); |
| Maternal Depression and Child Mental Health |
Depression during pregnancy and preterm delivery (K. Mochache) |
| Depression among teenage pregnant girls in low resource urban setting (J. Osok) | |
| Alcohol and Substance Use Disorders |
Depression and adherence to HIV medication among substance users (Maina, |
| Presentations at 2017 annual conference of the African Association of Psychiatrists and Allied Professionals: Mombasa Kenya | |
| Maternal Depression and Child Mental Health |
HIV-related stigma burden and post-partum depression in women attending Prevention of Mother–to-Child Transmission (PMCT) Clinic at Kenyatta National Hospital, Nairobi (O. Yator) |
| Project Overview | Outcomes of NIMH mental health research capacity-building project (M. Mathai). |
In 2015, a trainee in the first workshop won a scholarship to present her dissertation findings at the biannual meeting of International Society for Research in Child and Adolescent Psychopathology held in the U.S. The UON Principal Investigator was invited to present accomplishments in Kenya research capacity-building at National Institute of Mental Health-sponsored Global Mental Health workshops held in Toronto (2016) and Washington, DC (2017). Significantly, over the past three years sixteen trainees have made a contribution to the mental health research literature by submitting eighteen manuscripts for publication in peer-reviewed journals. To date, thirteen have been accepted for publication (Ambale CA, Sinei KA, Amugune BK, & Oluka MN, 2017; Jomo, Amugune, Sinei, & Oluka, 2016; Madeghe, Kimani, Vander Stoep, Nicodimos, & Kumar, 2016; Maina et al., 2015; Manasi, Linnet, Ongeri, Mathai, & Mbwayo, 2015; Mbwayo & Mathai, 2016; Musyoka, Obwenyi, Mathai, & Ndetei, 2016; Mutavi, Mathai, & Obondo, 2017; Mutavi, Obondo, Nganga, Kumar, & Mathai, 2016; Mutavi, Obondo, Nganga, Kumar & Mathai, 2016; Polkovnikova-Wamoto, Mathai, Vander Stoep, & Kumar, 2016; Waititu, Mwangangi, Amugune, Bosire, & Makanyengo, 2016; Yator, Mathai, Vander Stoep, Rao, & Kumar, 2016). Several other manuscripts are currently under review.
Development of Research Proposals
The substance abuse thematic group submitted one R21 proposal to the US National Institute of Alcohol and Drug Abuse. The aim of the proposed project was to conduct a pilot study to test the effectiveness of a community-based intervention program developed in Kenya that combines motivational interviewing, 12-step support, and cognitive behavioral coping skills. Based on pilot findings from a study conducted by a postgraduate trainee, the GBV thematic working group applied for foundation funding to test the feasibility of an intervention to address intergenerational effects of gender-based violence towards Kenyan women. The maternal and child mental health group has submitted three proposals for funding to generate information from community surveys and focus groups that will lay the groundwork for a future randomized clinical trial to test the effectiveness of group-based brief Interpersonal Therapy (IPT) for improving engagement in antenatal services of pregnant Kenyan adolescents and overall outcomes for these adolescents and their babies.
To date, none of the thematic groups have been awarded funding for their proposed research; however, signs of a growing capacity to conduct mental health research are in evidence. One of the UON faculty who received research training has a prominent role on an NIH-funded U-19 project entitled, “African Regional Research Partnerships for Scaling Up Child Mental Health Evidence-Based Practices” (M. McKay and K. Hoagwood, PIs, U19 MH110001–01-6883). And in autumn of 2017 UON and UW faculty submitted a collaborative R-21 grant proposal in response to the NIMH funding announcement, “Mobile Health: Technology and Outcomes in Low and Middle Income Countries” (M. Mathai and A. Vander Stoep, PIs).
UON and UW faculty also collaborated to write a multi-disciplinary proposal, entitled, “Partnerships of Health Research Training in Kenya (P-HERT)” (D. Wamalwa and C. Farquhar, PIs, D43 DW010141) to provide additional research training opportunities for UON junior faculty. The five-year project was funded by the US National Institute of Health/Fogarty International in 2015. The P-HERT project is supporting junior faculty in the areas of mental health, HIV/AIDS, and maternal newborn and child health. Faculty from three Kenyan universities take epidemiology and biostatistics courses in the UW School of Public Health and link with a UW mentor to design and carry out a small PHERT grant-funded research project in Kenya that can lay the groundwork for future intervention development and research. To date three junior faculty members from UON and Kenyatta Universities who are in the mental health field have been selected as P-HERT fellows.
Research Initiated at Decentralized Sites.
In the third project year, we recruited six health workers from non-academic health facilities designated as “decentralized sites” for medical education in the PRIME-K project and three health workers from the Gender-based Violence Recovery Centre (GBVRC) at Kenyatta National hospital, for training in mental health research alongside postgraduate trainees. The health workers deliberated on priority mental health topics in their respective geographic settings and in the end pooled these together to come up with a multisite study design. They opted to conduct a multi-site prevalence study of depression and suicidality, alcohol use disorders and PTSD in patients seen at outpatient clinics in County Hospitals. The GBVRC group decided to evaluate barriers to successful treatment completion among child sexual abuse survivors (CSA). With support from UON faculty, four sites and the GBVRC team have gone on to write proposals that have passed ethical review. Data have been collected and are currently undergoing analysis.
Lessons Learned
Our collaborative activities yielded a number of lessons that we hope will be of value to institutions who engage in mental health research capacity-building efforts in the future. The first lesson was that the NIH Multiple PI model provided a strong platform for distributing responsibilities equitably among faculty from the two participating institutions. The Multiple PI model was extended to the shared leadership by UON and UW subject-matter experts of thematic groups and shared guidance of mentees. This model enabled trainees to draw optimally on combined strengths of local and US mentors.
While we envisioned that UON thematic groups members would meet altogether regularly with UW mentors via Skype, this turned out to be impossible. Ten hour differences in time zones, different work schedules, problems with equipment, and power outages were technical problems that made multiple member Skype calls impossible. In addition, having multiple trainees participate on a single one-hour call was ineffective, when each needed a stronger dose of individual mentorship. We developed a more constructive pattern that took a layered form of supervision, whereby the UON trainee consulted with the local thematic group leader, and who then had a 1:1 consultation with the UW leader to address questions raised in trainee consultations. A second lesson learned was that designating thematic groups was a very helpful mechanism to create a narrow, tangible perimeter for the selection of research ideas by trainees and provision of leadership by mentors.
Another lesson learned was about the pace and content of the workshop curriculum. In the first workshop, what the UW team had planned was found to be too ambitious, with didactic teaching taking up both morning and afternoon sessions. UON collaborators suggested a slower pace, more active learning and including sessions on qualitative research methods. In year 2, the curriculum was considerably leaner in content, with only morning sessions devoted to didactics. Each afternoon UON/UW thematic group leaders met with their constituent trainees and applied the research methodology skills they had learned to design their master’s thesis research projects. In the smaller groups, we could devote attention to each of 5–6 proposals, starting with determining the research question, reviewing the literature, designing the study, selecting the sample source and size, determining the measurement strategy, considering the ethical considerations, and formulating a detailed study protocol. At the end of the workshop, trainees had in hand a strong outline for their UON Ethics Committee application.
We learned other lessons about the value of being able to augment data analyses by deploying skilled UW graduate students. It is typical for the UON trainees, after executing the field work of their thesis research, to hand off their data to a statistician whom they hire and who has no familiarity with the topic they are studying. The statistical output they produced is often adequate for meeting requirements of the thesis, but inadequate for publication in peer reviewed journals. Graduate students in the UW Department of Epidemiology volunteered to give statistical support to move manuscripts from thesis to publication. The UON trainee would send their de-identified datasets with variable and value labels to the UW in excel or SPSS data files. UW mentors then supervised the graduate students through the process of re-analysis of the Kenyan data. UW graduate students were grateful to be added as co-authors.
Another generative process was when UW mentors set aside a block of time to collaborate on editing and polishing UON trainees’ manuscripts together with the UON faculty mentors, working together with the motto, “Many hands make light labor.”
Other Challenges
Heavy demands on a limited number of UON faculty made it difficult for them to set aside their teaching, clinical, and administrative responsibilities to participate in intensive research training workshops. Difficulties were overcome by ensuring that the workshops were organized during times when faculty were not responsible for monitoring student exams. The first workshop was organized on the UON College of Health Sciences campus, and there were frequent interruptions when workshop participants were called to attend to administrative, clinical, and family duties. Afternoons were characterized by anxiety from anticipating rush hour traffic jams in Nairobi. We learned that we could hold briefer, more intensive workshops outside of college settings, allowing UON faculty to get away from multiple demands on their time, carry out team-building activities in the early evening, participate in group work in the evenings, and socialize.
Building and maintaining collaborative relationships and supporting trainees to design, implement, and disseminate research findings requires major commitments of time. UW and UON faculty have both been challenged by low salary support relative to high mentorship demands from the MEPI activities. Faculty members from both academic institutions have capitalized on opportunities to meet in person at global mental health conferences to carry forward collaborative projects.
The most crucial ingredients to our successful South-North collaboration include the Multiple PI model that has promoted equitable South/North collaboration. Implementing this model generated a two-way transfer of skills and knowledge, as well as mutual trust, respect and even friendship. Other key ingredients include strong institutional support, multidisciplinary collaboration, a good relationship with the UON Ethics Review Committee, appropriate funding mechanisms, and good communication with and support from the funding organization.
Looking to the Future
UON faculty members have made considerable progress in moving beyond single-discipline research silos to acquire and utilize mental health research skills, to foster research team development, and to promote international and interdisciplinary research collaboration. Currently, the UON Department of Psychiatry faculty members are integrating the project research methods workshop curriculum into research training for the master’s program in Psychiatry. They are also in the process of building up this curriculum to form the core of course work for a PhD program. The research centre is still used as the hub for mental health researchers at the university, KNH and Mathari Hospital. In summary, the “Mental Health Research Training for Improved Health Outcomes in Kenya” project succeeded in setting the stage for an enduring and mutually beneficial partnership that we hope will yield future funded programs and sustain efforts to improve mental health and well-being for Kenyans.
Acknowledgments
Funding for this work came from the National Institute of Health/ National Institute of Mental Health (NIMH) through award number R25MH099132 and D43DW010141. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the National Institute of Mental Health. All research conducted in this project receives approval from the KNH-UON Ethics and Research Committee (http://erc.uonbi.ac.ke)
Footnotes
Conflict of Interest statement
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Contributor Information
Muthoni Mathai, Senior lecturer Department of Psychiatry, University of Nairobi. Kenyatta National Hospital, P O Box 19676 - 00202, NAIROBI, KENYA.
Ann Vander Stoep, Associate professor, department of Psychiatry and Behavioural sciences, Epidemiology University of Washington. Seattle. Box 354920, Child Health Institute, 6200 NE 74th Street, Suite 210, Seattle, WA 98115 -1538 Tel: 206-543-1538.
Manasi Kumar, Senior lecturer Department of Psychiatry, University of Nairobi, Kenyatta National Hospital, P O Box 19676 - 00202, NAIROBI, KENYA.
Mary Kuria, Associate Professor and head of Department of Psychiatry, University of Nairobi, Kenyatta National Hospital, P O Box 19676 - 00202, NAIROBI, KENYA.
Anne Obondo, Associate Professor Department of Psychiatry, University of Nairobi, Kenyatta National Hospital, P O Box 19676 - 00202, NAIROBI, KENYA.
Violet Kimani, Professor School of Public Health, University of Nairobi, Kenyatta National Hospital, P O Box 19676 - 00202, NAIROBI, KENYA.
Beatrice Amugune, Senior lecturer, School of Pharmacy, University of Nairobi. Kenyatta National Hospital, P O Box 19676 - 00202, NAIROBI, KENYA.
Margaret Makanyengo, Clinician Kenyatta National Hospital, Honorary Lecturer University of Nairobi, Kenyatta National Hospital, P O Box 19676 - 00202, NAIROBI, KENYA.
Anne Mbwayo, Lecturer Department of Psychiatry, University of Nairobi. Kenyatta National Hospital, P O Box 19676 - 00202, NAIROBI, KENYA Mara Child,.
Jürgen Unützer, Professor and Chair department of Psychiatry and Behavioural Sciences, adjunct professor School of Public Health and Department of Global Health, University of Washington. Seattle. 1959 NE Pacific Street, Seattle, WA 98195, United States.
James Kiarie, Associate Professor Department of Obstetrics and Gynaecology, University of Nairobi; World Health Organisation: Coordinator, Human Reproduction Team. Kenyatta National Hospital, P O Box 19676 - 00202, NAIROBI, KENYA.
Deepa Rao, Associate Professor Department of Global Mental health, Psychiatry and Behavioural Sciences. University of Washington, Seattle. Department of Global Health; Harborview Medical Center, Box 359931, 325 9th Ave, Seattle, WA 98104 USA.
References
- Ambale CA, Sinei KA, Amugune BK, & Oluka MN. (2017). Accessibility of medicines used in the management of substance use disorders in selected hospitals in Nairobi. African Journal of Pharmacology and Therapeutics, 6(2), 102–108. [Google Scholar]
- Bass J, Neugebauer R, Clougherty KF, Verdeli H, Wickramaratne P, Ndogoni L, … Bolton P. (2006). Group interpersonal psychotherapy for depression in rural Uganda: 6-month outcomes: randomised controlled trial. The British Journal of Psychiatry : The Journal of Mental Science, 188(6), 567–73. 10.1192/bjp.188.6.567 [DOI] [PubMed] [Google Scholar]
- Bolton P, Bass J, Betancourt T, Speelman L, Onyango G, Clougherty KF, … Verdeli H (2007). Interventions for depression symptoms among adolescent survivors of war and displacement in northern Uganda: a randomized controlled trial. JAMA, 298(5), 519–27. 10.1001/jama.298.5.519 [DOI] [PubMed] [Google Scholar]
- Child MJ, Kiarie JN, Allen SM, Nduati R, Wasserheit JN, Kibore MW, … Farquhar C (2014). Expanding clinical medical training opportunities at the University of Nairobi: adapting a regional medical education model from the WWAMI program at the University of Washington. Academic Medicine : Journal of the Association of American Medical Colleges, 89(8 Suppl), S35–9. 10.1097/ACM.0000000000000350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins P (2013). Research priorities, capacity, and networks in global mental health. In Patel Vikram, Minas Harry, Cohen Alex, & Prince Martin J. (Eds.), Global Mental Health Principles and Practice (1st ed., pp. 425–449). New York: Oxford University Press. [Google Scholar]
- Fryers T, Melzer D, & Jenkins R (2003). Social inequalities and the common mental disorders. Social Psychiatry and Psychiatric Epidemiology, 38(5), 229–237. 10.1007/s00127-003-0627-2 [DOI] [PubMed] [Google Scholar]
- Global Burden of Disease Study 2013 Collaborators. (2015). Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet (London, England), 386(9995), 743–800. 10.1016/S0140-6736(15)60692-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horton R (2013). Offline: Is global health neocolonialist? The Lancet, 382(9906), 1690 10.1016/S0140-6736(13)62379-X [DOI] [Google Scholar]
- Jomo S, Amugune B, Sinei K, & Oluka M (2016). Assessing the prevalence and severity of potential drug-drug interactions among mentally ill inpatients. Indian Research Journal of Pharmacy and Science, 8(8), 331–343. [Google Scholar]
- Katon W, Russo J, Lin EHB, Schmittdiel J, Ciechanowski P, Ludman E, … Korff M. Von. (2012). Cost-effectiveness of a Multicondition Collaborative Care Intervention. Archives of General Psychiatry, 69(5), 506 10.1001/archgenpsychiatry.2011.1548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lansang MA, & Dennis R (2004). Building capacity in health research in the developing world. Bulletin of the World Health Organization, 82(10), 764–70. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/15643798 [PMC free article] [PubMed] [Google Scholar]
- Machayo J, & Keraro V (2013). Brain drain among health professionals in Kenya: A case of poor working conditions? - A critical review of the causes and effects. Prime Journal of Business Administration and Management, 3(6), 1047–1063. [Google Scholar]
- Madeghe BA, Kimani VN, Vander Stoep A, Nicodimos S, & Kumar M (2016). Postpartum depression and infant feeding practices in a low income urban settlement in Nairobi-Kenya. BMC Research Notes, 9(1), 506 10.1186/s13104-016-2307-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maina R, Obondo AA, Kuria MW, & Donovan DM (2015). Substance use literacy: Implications for HIV medication adherence and addiction severity among substance users. African Journal of Drug and Alcohol Studies, 14(2), 137–151. Retrieved from https://www.ajol.info/index.php/ajdas/article/view/133134 [Google Scholar]
- Manasi K, Linnet O, Ongeri L, Mathai M, & Mbwayo A (2015). Translation of EPDS Questionnaire into Kiswahili: Understanding the Cross-Cultural and Translation Issues in Mental Health Research. Journal of Pregnancy and Child Health, 2(1). 10.4172/2376-127X.1000134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mbwayo AW, & Mathai M (2016). Association between Hopelessness and Conduct Problem among School Going Adolescents in a Rural and Urban Setting in Kenya. Journal of Child and Adolescent Behaviour, 4(291). 10.4172/2375-4494.1000291 [DOI] [Google Scholar]
- Musyoka CM, Obwenyi AM, Mathai M, & Ndetei DM (2016). Models and approaches to alcohol and drug addiction rehabilitation in Kenya. International Journal of Health and Psychology Research, 44(44), 1–12. Retrieved from http://www.eajournals.org/wp-content/uploads/Models-and-Approaches-to-Alcohol-and-Drug-Addiction-Rehabilitation-in-Kenya.pdf [Google Scholar]
- Mutavi T, Mathai M, & Obondo A (2017). Post-Traumatic Stress Disorder (PTSD) in Sexually Abused Children and Educational Status in Kenya: A Longitudinal Study. Journal of Child and Adolescent Behavior 2017 5:5, 5(357), 1–8. 10.4172/2375-4494.1000357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mutavi T, Obondo A, Nganga P, Kumar M, & Mathai M (2016). Psychosocial Outcomes Among Children Following Defilement And The Caregivers Responses To The Children’s Trauma: A Qualitative Study From Nairobi Suburbs, Kenya. African Journal of Traumatic Stress, 5(1), 29–32. [PMC free article] [PubMed] [Google Scholar]
- NIH. (2011). Multiple Principal Investigators - General Information Retrieved from https://grants.nih.gov/grants/multi_pi/overview.htm
- Osanjo GO, Oyugi JO, Kibwage IO, Mwanda WO, Ngugi EN, Otieno FC, … Kiarie JN (2015). Building capacity in implementation science research training at the University of Nairobi. Implementation Science, 11(1), 30 10.1186/s13012-016-0395-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel V (2007). Mental health in low- and middle-income countries. British Medical Bulletin, 81– 82(1), 81–96. 10.1093/bmb/ldm010 [DOI] [PubMed] [Google Scholar]
- Polkovnikova-Wamoto A, Mathai M, Vander Stoep A, & Kumar M (2016). “Haven of safety” and “secure base”: a qualitative inquiry into factors affecting child attachment security in Nairobi, Kenya. Vulnerable Children and Youth Studies, 11(4), 286–296. 10.1080/17450128.2016.1201237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pratap S, Itzhak L, Sylvie O, Francisco A. de, & Shekhar S (Eds.). (2007). Research capacity for mental health in low-and middle-income countries: Results of a mapping project. Global Forum for Health Research and World Health Organization Geneva: Geneva, World Health Organization & Global Forum for Health Research; Retrieved from http://www.who.int/mental_health/MHRC_FullText.pdf [Google Scholar]
- Rao D, Feldman BJ, Fredericksen RJ, Crane PK, Simoni JM, Kitahata MM, & Crane HM (2012). A Structural Equation Model of HIV-Related Stigma, Depressive Symptoms, and Medication Adherence. AIDS and Behavior, 16(3), 711–716. 10.1007/s10461-011-9915-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rüsch N, Müller M, Ajdacic-Gross V, Rodgers S, Corrigan PW, & Rössler W (2014). Shame, perceived knowledge and satisfaction associated with mental health as predictors of attitude patterns towards help-seeking. Epidemiology and Psychiatric Sciences, 23(2), 177–187. 10.1017/S204579601300036X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saxena S, Paraje G, Sharan P, Karam G, & Sadana R (2006). The 10/90 divide in mental health research: trends over a 10-year period. The British Journal of Psychiatry, 188(1), 81–82. 10.1192/bjp.bp.105.011221 [DOI] [PubMed] [Google Scholar]
- Saxena S, Thornicroft G, Knapp M, & Whiteford H (2007). Resources for mental health: scarcity, inequity, and inefficiency. The Lancet, 370(9590), 878–889. 10.1016/S0140-6736(07)61239-2 [DOI] [PubMed] [Google Scholar]
- Vasquez EE, Hirsch JS, Giang LM, & Parker RG (2013). Rethinking health research capacity strengthening. Global Public Health, 8 Suppl 1(sup1), S104–24. 10.1080/17441692.2013.786117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verdeli H, Clougherty K, Onyango G, Lewandowski E, Speelman L, Betancourt TS, … Bolton P (2008). Group Interpersonal Psychotherapy for depressed youth in IDP camps in Northern Uganda: adaptation and training. Child and Adolescent Psychiatric Clinics of North America, 17(3), 605–24, ix. 10.1016/j.chc.2008.03.002 [DOI] [PubMed] [Google Scholar]
- Waititu AI, Mwangangi EM, Amugune B, Bosire KO, & Makanyengo M (2016). Impact of depression on adherence to antiretroviral therapy among HIV/AIDS patients at a Kenyan referral hospital Retrieved from http://erepository.uonbi.ac.ke:8080/xmlui/handle/11295/95964
- Whiteford HA, Degenhardt L, Rehm J, Baxter AJ, Ferrari AJ, Erskine HE, … Vos T (2013). Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. The Lancet, 382(9904), 1575–1586. 10.1016/S0140-6736(13)61611-6 [DOI] [PubMed] [Google Scholar]
- World Health Organization (2012): Report of the Consultative Expert Working Group on Research and Development: Financing and Coordination http://www.who.int/phi/CEWG_Report_5_April_2012.pdf
- World Health Organization. (2016). mhGAP Intervention Guide - Version 2.0 for mental, neurological and substance use disorders in non-specialized health settings Geneva. [PubMed] [Google Scholar]
- Yator O, Mathai M, Vander Stoep A, Rao D, & Kumar M (2016). Risk factors for postpartum depression in women living with HIV attending prevention of mother-to-child transmission clinic at Kenyatta National Hospital, Nairobi. AIDS Care, 28(7), 884–889. 10.1080/09540121.2016.1160026 [DOI] [PMC free article] [PubMed] [Google Scholar]


