Abstract
Objectives
Examination of current temporal trends and clinical management patterns of eating disorders (ED) in primary care is lacking. We aimed to calculate annual incidence rates of EDs in primary care by age, sex and deprivation. We also explored the care received through referrals, psychotropic prescriptions and associated secondary care service use.
Participants and settings
A retrospective electronic cohort study was conducted using the Clinical Practice Research Datalink in those aged 11–24 years between 2004 and 2014 in England (n=1 135 038).
Results
A total of 4775 individuals with a first ever recorded ED diagnosis were identified. The crude incidence rate was 100.1 per 100 000 person years at risk (95% CI 97.2 to 102.9). Incidence rates were highest in females (189.3 per 100 000 person years, 95% CI 183.7 to 195.0, n=4336), 16–20 years of age (141.0 per 100 000 person years, 95% CI 135.4 to 146.9, n=2348) and individuals from the least deprived areas (115.8 per 100 000 person years (95% CI 109.3 to 122.5, n=1203). Incidence rates decreased across the study period (incidence rate ratio (IRR) 0.6, 95% CI 0.5 to 0.8), particularly for individuals with bulimia nervosa (IRR 0.5, 95% CI 0.3 to 0.7) and from the most deprived areas (IRR 0.5, 95% CI 0.4 to 0.7). A total of 17.4% (95% CI 16.3 to 18.5, n=831) of first ever recorded ED cases were referred from primary to secondary care. 27.1% (95% CI 25.9 to 28.4, n=1294) of individuals had an inpatient admission 6 months before or 12 months after an incident ED diagnosis and 53.4% (95% CI 52.0 to 54.9, n=2550) had an outpatient attendance. Antidepressants were the most commonly prescribed psychotropic medication.
Conclusions
New ED presentations in primary care are reducing. Understanding the cause of this decrease (coding behaviours, changes in help-seeking or a genuine reduction in new cases) is important to plan services, allocate resources and deliver effective care.
Keywords: children and young people, CPRD, incidence rates, eating disorders, prescribing
Strengths and limitations of this study.
Our study included over 1 million young people from Clinical Practice Research Datalink, a large primary care database representative of the general population
By analysing primary care data, we are able to identify all cases of eating disorders (ED) including less severe ones, not just those presenting to secondary care.
The estimated incidence of ED may be affected by coding behaviour or access to health services and are likely to be underestimates since not all people will present to services.
Analyses are limited to English data only due to the availability of neighbourhood deprivation data.
Prescriptions, inpatient admissions and outpatient attendance data are not directly attributable to a particular diagnosis in the primary care dataset.
Introduction
Eating disorders (ED) are a group of conditions in which negative beliefs about eating, body shape and weight accompany behaviours including restricting eating, binge eating, excessive exercise, vomiting and laxative use.1 They are often long term conditions, with severe short and ongoing physical implications2 and a high risk of suicide.3 4 The Mental Health of Children and Young People in England Survey 2017, estimated that 0.4% of children and young people aged 5–19 years had an ED5 with some sources quoting an overall population figure at 1.25 million people affected.6 Females and adolescents are most at risk of ED. While Bould et al found that females with higher educated parents had a higher risk of EDs,7 few whole population level studies have explored how deprivation impacts presentation. There is a current debate about whether the incidence of EDs has changed over time.8 Population studies demonstrate rates of anorexia nervosa (AN) remain relatively stable over time,9 and there are conflicting findings in rates of bulimia nervosa (BN).8 10 Trends for ED, not otherwise specified (EDNOS) have been investigated far less, despite EDNOS being the most common ED. One study found incident cases were increasing within primary care.10 Most research on individuals diagnosed with EDs is based on psychiatric case registers, surveys or in secondary care data sets.11 Few studies have explored the care received by patients with ED in primary care, despite it often being the first point of contact and the gateway to secondary and/or specialist services.12 It is important that patients are triaged, referred, signposted and managed appropriately in primary care. Temporal trends and relative risks inform both the need for and configuration of services and allocation of resources within primary care and at the interface with secondary care.12 The aims of this study are to explore the current recorded incidence of ED diagnoses in primary care (by ED subtype, age, sex, deprivation) and associated psychotropic prescriptions, referrals to secondary care, outpatient attendances and inpatient admissions in children and young people.
Methods
Study design
A retrospective electronic cohort study was conducted using the Clinical Practice Research Datalink (CPRD).
Data source
CPRD is a large population-based, longitudinal primary care database covering a representative sample of the UK population in terms of age, sex and ethnicity.13 It contains over 4.4 million active patient records from 674 registered general practices. The data set includes approximately 6.9% of the UK population with 82% of patients registered in England.13 Currently, only English data are linked to deprivation. Data include anonymised patient demographic information, medical diagnoses, prescriptions and referrals to secondary care. Clinical data are coded using modified 5-byte Read version 2. A total of 75% of English practices in CPRD are linked to hospital episode statistics (HES) data13 which includes both inpatient and outpatient records.
Study population and setting
The study population were children and young people aged 11–24 years who were registered with a contributing CPRD practice in England over an 11-year period (1 January 2004 to 31 December 2014). The onset of EDs is most common in adolescence10 and thus the basis of the age profile of the study population.
The basis for the analysis was CPRD’s (anonymised) list of patients with data of an acceptable standard for research purposes aged 11–24 years at any point during the study period. Acceptable standard means that CPRD’s checks for data completeness and validity were satisfied, this includes poor data recording and non-continuous follow up.13 An ‘open’ cohort was utilised so study start and end dates varied between individuals quantified as their ‘person years at risk’. Each individual was included in the study for a period dependent on the patients’ date of birth, death (if relevant), registration with a general practitioner (GP; minimum 6 months), the dates of the last collection of data from the GP and when the GP’s data met CPRD’s quality standard. Individuals had to contribute at least 6 months data to the study (and were therefore registered with a CPRD GP for a minimum of 1 year). An individual’s total time ‘at risk’ within the study was categorised by age band, year, sex and deprivation quintile.
Measures
Case definition
We queried the primary-care database using STATA V.1314 identifying CPRD codes converted from Read Codes version 2. Read codes, a hierarchical nomenclature, are used in primary care to record clinical summary information. Previously validated code lists10 that used weight, height and body mass index to validate 10% of records, were updated to identify EDs. EDs were divided into subtypes: AN, BN and EDNOS. EDNOS generally is recorded for an ED which causes distress and impairment but does not meet the full criteria for the other subtypes.1 We included atypical AN and atypical BN in the category EDNOS, in addition to other non-specified EDs, such as binge-eating disorder (BED).10 Atypical AN and atypical BN have commonalities with AN and BN, but they do not meet the threshold for diagnosis. BED is now a formally recognised ED under the Diagnostic and Statistical Manual of Mental Disorders 5 (DSM-5) released in 2013 and therefore after the remit of this analysis. Further, EDNOS is now referred to as Other Specified Feeding or Eating Disorder in DSM-5. We also explored recorded ED symptom codes. We used International Classification of Disease-10 diagnoses to query the HES Database for ED diagnosis (see online supplementary material 1 for list of all diagnosis and symptom codes used).
bmjopen-2018-026691supp001.pdf (699.6KB, pdf)
Other and admin codes
CPRD categorises some events as ‘other’ and ‘admin’. In previous work,15 we have excluded these codes in order to capture only individuals who had direct contact with a primary care practitioner (eg, through face-to-face or telephone consultation), to capture the burden on primary care services. In order to focus on the burden to individual patients, these codes were included in these analyses as in other similar studies.10 12 Diagnoses may have been made in other services (eg, secondary care or emergency departments), yet are recorded in primary care through communication between services for example, letters sent to the GP.
Frequency
First ever incidence rates and annual prevalence rates were calculated for diagnoses and symptoms. First ever cases used for incidence rates were defined as having had no previous record of the condition in their primary care records (dating back to 1979). Prevalence was defined as an individual with any record with an ED Read code in a target year regardless of any previous diagnosis.16 Proportions of individuals with a symptom code and whether they also had an ED diagnosis in either their primary care or inpatient records during the study period were calculated.
Age and sex
Age was recorded at the time of diagnosis in primary care. Age was categorised by age groups 11–15 years, 16–20 years and 21–24 years or under 18 (11–17) vs over 18 (18–24) years for selected analyses. This was to reflect differences in ED service provision around the age of transition from child and adolescent services to adult services. Indeterminate sex was excluded due to small numbers.
Deprivation
Deprivation quintiles were derived from the English Index of Multiple Deprivation 2010 (IMD). IMD is area-level data at Lower layer Super Output Area (LSOA) level. The index is based on seven key indicators of deprivation: income, employment, health and disability, education skills and training, barriers to housing and services, living environment and crime. These are combined and weighted appropriately to produce an overall IMD score.17 This score is divided into five equal groups to create the IMD quintiles 1 (least deprived) to 5 (most deprived).
Psychotropic prescriptions
British National Formulary codes converted into CPRD specific product codes were used to explore prescribing in the CPRD dataset (available on request) for antidepressants, anxiolytics/hypnotics and antipsychotics based on previously published Read code lists.18 19 Routine data do not explicitly link prescription data with diagnoses. Therefore an associated prescription was defined as 6 months before or 12 months after an ED diagnosis. This method is similar to previous studies.18
Referrals to secondary care
CPRD contains referral details to secondary care (including specialty and referral type) recorded on GP systems. We investigated the proportion of people aged under and over 18 years referred from primary care to secondary care child and adolescent or adult psychiatry services for EDs between 2004 and 2014.
Outpatient attendance and inpatient admission
We explored the proportion of individuals with a recorded first ever ED diagnosis in primary care who also had an ‘associated’ outpatient attendance and/or inpatient admission (6 months before and 12 months after): any outpatient attendance; outpatient attendances with a psychiatric specialty code; any inpatient admission; an inpatient admission where an ED is coded. Diagnoses in outpatient records are too poorly recorded to identify ED diagnoses robustly. We examined the proportion of associated outpatient attendance/inpatient admissions (6 months before 12 months after ED diagnosis) to adult or paediatric specialties for people aged under and over 18 years.
Statistical analyses
Annual incidence and prevalence rates were calculated using person years at risk as the denominator. This is a more appropriate denominator than the number of registered cases because each individual’s duration of follow-up was not fixed.19 Poisson regression was undertaken to model the counts of recorded ED diagnoses as a function of year of diagnosis, sex, age group and deprivation. Robust standard errors for the estimated incidence rate ratios (IRRs) were used to account for clustering within practices. Analysis was conducted using STATA V.13.14
Patient and public involvement
This study was conceived during the HQIP Adolescent Mental Health project (NCA134A) which examined outcomes for young people and young adults with a mental health diagnoses and included discussion with service users and clinicians.
Results
Study population
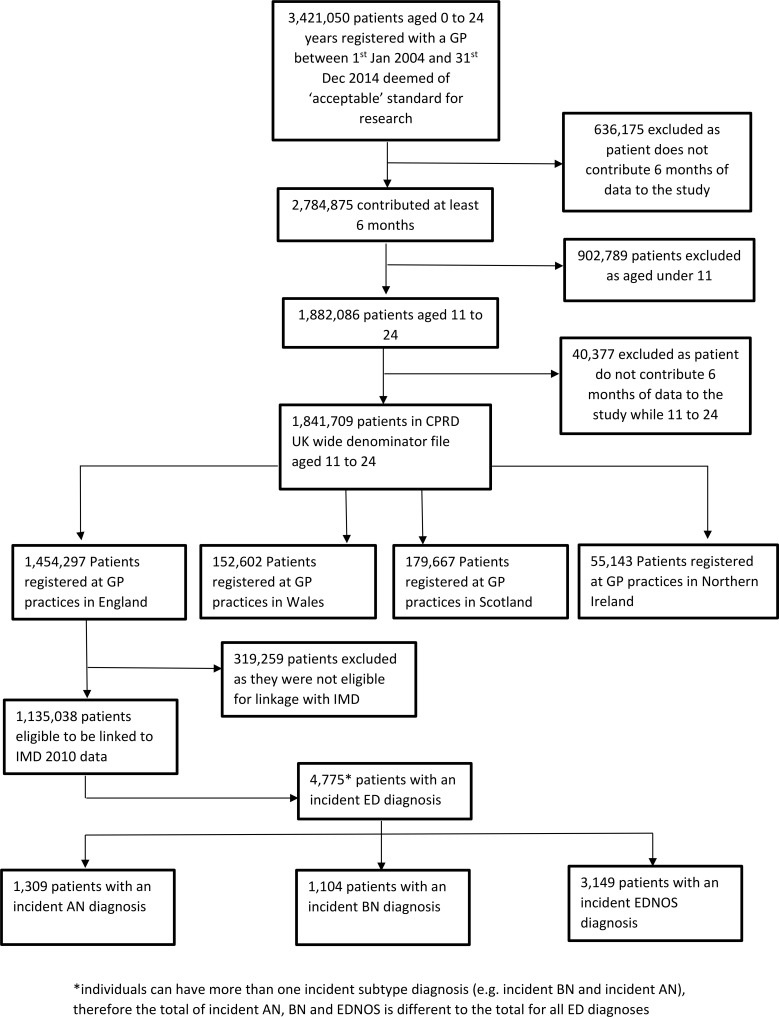
A total of 1 135 038 individuals aged 11–24 years between 1 January 2004 and 31 December 2014 contributed 4772 160.6 person-years of data. The mean follow-up time was 4.2 years. We identified 4775 individuals with a first ever ED diagnosis in primary care between 2004 and 2014. See figure 1 for study flow diagram.
Figure 1.
Study flow diagram. AN, anorexia nervosa; BN, bulimia nervosa; CPRD, Clinical Practice Research Datalink; ED, eating disorders; EDNOS, ED, not otherwise specified GP, general practitioner; IMD, English Index of Multiple Deprivation 2010.
Trends in the incidence rates over time
The crude incidence rate was 100.1 per 100 000 person years (95% CI 97.2 to 102.9). ‘Administration’ and ‘other codes’ made up 31.4% (n=1501) of first ever ED diagnoses. The crude incidence rate decreased significantly between 2004 and 2014 (see table 1). Adjusted rate ratios for year, sex, age group and deprivation are shown in table 1. Annual prevalence rates showed similar trends (see online supplementary material 2, figure S1 and table S1).
Table 1.
Crude incidence rates and adjusted rate ratios for first ever eating disorder diagnosis derived from Poisson regression analysis
| First ever incidence | |||
| Individuals (n, %) | Crude incidence rate* (95% CI) |
Incidence rate ratio† (95% CI) |
|
| Sex | |||
| Male | 439 (9.2) | 17.7 (16.1 to 19.4) | - |
| Female | 4336 (90.8) | 189.2 (183.7 to 195) | 10.8 (9.7 to 12.0) |
| Age | |||
| 11 to 15 | 1425 (29.8) | 80.2 (76.1 to 84.5) | 0.6 (0.5 to 0.6) |
| 16 to 20 | 2348 (49.2) | 141.0 (135.4 to 146.9) | - |
| 21 to 24 | 1002 (21.0) | 75.3 (70.7 to 80.1) | 0.5 (0.5 to 0.6) |
| Deprivation | |||
| 1 (least) | 1203 (25.2) | 115.8 (109.3 to 122.5) | 1.5 (1.4 to 1.7) |
| 2 | 1044 (21.9) | 105.2 (98.9 to 111.8) | 1.4 (1.2 to 1.5) |
| 3 | 884 (18.5) | 97.5 (91.2 to 104.2) | 1.2 (1.1 to 1.4) |
| 4 | 953 (20.0) | 97.8 (91.7 to 104.2) | 1.2 (1.1 to 1.4) |
| 5 (most) | 691 (14.5) | 80.3 (74.4 to 86.5) | - |
| Year | |||
| 2004 | 475 (9.9) | 117.5 (107.1 to 128.5) | - |
| 2005 | 462 (9.7) | 107.6 (98 to 117.9) | 0.9 (0.8 to 1.0) |
| 2006 | 491 (10.3) | 110.7 (101.1 to 120.9) | 0.9 (0.8 to 1.1) |
| 2007 | 526 (11.0) | 114.4 (104.9 to 124.6) | 1.0 (0.9 to 1.1) |
| 2008 | 499 (10.5) | 106.8 (97.7 to 116.6) | 0.9 (0.8 to 1.0) |
| 2009 | 478 (10.0) | 101.3 (92.4 to 110.8) | 0.8 (0.8 to 1.0) |
| 2010 | 408 (8.5) | 87.3 (79.1 to 96.3) | 0.7 (0.6 to 0.8) |
| 2011 | 419 (8.8) | 92.6 (83.9 to 101.9) | 0.7 (0.6 to 0.9) |
| 2012 | 394 (8.3) | 89.6 (81 to 98.9) | 0.7 (0.7 to 0.8) |
| 2013 | 357 (7.5) | 88.9 (79.9 to 98.6) | 0.7 (0.6 to 0.9) |
| 2014 | 266 (5.6) | 79.3 (70 to 89.4) | 0.6 (0.5 to 0.8) |
Total study Population=1 135 038 individuals.
*Per 100 000 person years.
†Adjusted for calendar year, sex, age group and deprivation 1(least).
There was similarly a significant decrease in recording of ED symptom codes between 2004 and 2014 (see online supplementary material 2, table S2). Of individuals who had an ED symptom code recorded in primary care, 1.1% (95% CI 0.7 to 1.8, n=19) also had an ED diagnosis in primary care and 11.4% (95% CI 10.0 to 13.1, n=192) also had an inpatient admission for an ED.
Age and sex patterns
Females were nearly 11 times more likely to have an incident diagnosis for an ED than males (see table 1). Crude annual incidence rates decreased significantly over the study period for females from 232.7 per 100 000 person years (95% CI 211.5 to 255.4, n=443) to 145.5 per 100 000 person years (95% CI 127.6 to 165.2, n=238). There was no significant change for males.
Crude incidence rates were significantly higher for people aged 16–20 years across the study period than for those aged 11–15 years and 21–24 years (see table 1 for rates and (adjusted) IRR). Incidence rates decreased significantly for those aged 16–20 years (IRR 0.6, 95% CI 0.5 to 0.7) and 21–24 years (IRR 0.5, 95% CI 0.4 to 0.7) over the study period (figure 2). There was no significant change over time in incidence rates for those aged 11–15 years (see online supplementary table S3, figure S2 for IRR by year).
Figure 2.
The crude annual incidence rate of individuals per 100 000 person years with eating disorders for children and young people aged 11–24 years by age group.
Deprivation
Crude incidence rates were significantly higher for individuals from the least deprived areas across the study period. Crude incidence rates and adjusted rate ratios are shown in table 1. Annual incidence rates significantly decreased across the study period for individuals from the most deprived areas (IMD quintiles 3–5), by half for the most deprived group (IRR 0.5, 95% CI 0.4 to 0.7). There was no significant decline in incidence rates for those from the least deprived areas. See online supplementary, table 4S and figure S3 for adjusted rate ratios.
By ED subtype
Crude annual incidence rates were significantly higher for those with recorded EDNOS (66.0 per 100 000 person years, 95% CI 63.7 to 68.3, n=3149), than AN (27.4 per 100 000 person years, 95% CI 26.0 to 29.0, n=1309) and BN (23.1 per 100 000 person years, 95% CI 21.8 to 24.5, n=1104).
The overall significant decrease in the incidence of recorded EDs over the study period varied by subtype. The most significant decrease was for BN. Rates for EDNOS fluctuated but overall there was a significant decrease. There was no significant change for AN. See table 2 for adjusted rate ratios.
Table 2.
Adjusted rate ratios for first ever ED diagnosis by ED subtype derived from Poisson regression analysis
| AN | BN | EDNOS | ||||
| Individuals (n) | Incidence rate ratio* (95% CI) | Individuals (n) | Incidence rate ratio* (95% CI) | Individuals (n) | Incidence rate ratio* (95% CI) | |
| Sex | ||||||
| Male | 71 | - | 72 | - | 335 | - |
| Female | 1238 | 19.1 (14.9 to 24.4) | 1032 | 15.7 (12.4 to 19.8) | 2814 | 9.1 (8.1 to 10.4) |
| Age | ||||||
| 11 to 15 | 449 | 0.6 (0.6 to 0.7) | 129 | 0.2 (0.2 to 0.2) | 998 | 0.6 (0.6 to 0.7) |
| 16 to 20 | 652 | - | 625 | - | 1480 | - |
| 21 to 24 | 208 | 0.4 (0.3 to 0.5) | 350 | 0.7 (0.6 to 0.8) | 671 | 0.6 (0.5 to 0.6) |
| Deprivation | ||||||
| 1 (least) | 395 | 2.7 (2.3 to 3.2) | 272 | 1.6 (1.3 to 1.9) | 769 | 1.4 (1.2 to 1.6) |
| 2 | 309 | 2.2 (1.8 to 2.7) | 249 | 1.4 (1.2 to 1.8) | 683 | 1.3 (1.1 to 1.4) |
| 3 | 254 | 2.0 (1.6 to 2.4) | 203 | 1.2 (1.0 to 1.5) | 569 | 1.1 (1 to 1.3) |
| 4 | 227 | 1.6 (1.3 to 2.0) | 219 | 1.2 (1.0 to 1.5) | 646 | 1.2 (1.1 to 1.4) |
| 5 (most) | 124 | - | 161 | - | 482 | - |
| Year | ||||||
| 2004 | 131 | - | 104 | - | 294 | - |
| 2005 | 111 | 0.8 (0.6 to 1.0) | 145 | 1.3 (1.0 to 1.7) | 276 | 0.9 (0.8 to 1.0) |
| 2006 | 121 | 0.8 (0.6 to 1.1) | 131 | 1.1 (0.9 to 1.5) | 318 | 1.0 (0.9 to 1.1) |
| 2007 | 141 | 0.9 (0.7 to 1.2) | 125 | 1.0 (0.8 to 1.4) | 352 | 1.0 (0.9 to 1.2) |
| 2008 | 132 | 0.9 (0.7 to 1.1) | 128 | 1.0 (0.8 to 1.4) | 321 | 0.9 (0.8 to 1.1) |
| 2009 | 127 | 0.8 (0.6 to 1.1) | 103 | 0.8 (0.6 to 1.1) | 329 | 0.9 (0.8 to 1.1) |
| 2010 | 105 | 0.7 (0.5 to 0.9) | 98 | 0.8 (0.6 to 1.1) | 267 | 0.8 (0.7 to 0.9) |
| 2011 | 107 | 0.7 (0.5 to 0.9) | 99 | 0.8 (0.6 to 1.1) | 282 | 0.8 (0.7 to 1.0) |
| 2012 | 111 | 0.8 (0.6 to 1.0) | 68 | 0.6 (0.4 to 0.8) | 278 | 0.8 (0.7 to 1.0) |
| 2013 | 132 | 1.0 (0.8 to 1.2) | 61 | 0.6 (0.4 to 0.8) | 245 | 0.8 (0.7 to 1.0) |
| 2014 | 91 | 0.8 (0.6 to 1.0) | 42 | 0.5 (0.3 to 0.7) | 187 | 0.7 (0.6 to 0.9) |
Total study Population=1 135 038 individuals.
*Adjusted for calendar year, sex, deprivation and stratified by age group.
AN, anorexia nervosa; BN bulimia nervosa; ED, eating disorder; EDNOS, ED, not otherwise specified.
Associated psychotropic prescriptions
A total of 1317 (27.6%, 95% CI 26.3 to 28.9) individuals with an incident ED diagnosis in primary care had an associated psychotropic prescription. Of these 26.3% (95% CI 25.0 to 27.5, n=1254) were for antidepressants, 3.3% (95% CI 2.8 to 3.8, n=156) for anxiolytics/hypnotics and 1.8% (95% CI 1.4 to 2.2, n=84) for antipsychotics. Females and older age groups were more likely to be prescribed antidepressants. Older age groups were more likely to be prescribed anxiolytic/hypnotics, but there was no significant difference between sexes. Numbers were small for antipsychotics but no differences in age and sex were detected. There were no significant differences by deprivation for all prescriptions. The number and proportion of individuals receiving psychotropic prescriptions has increased between 2004 and 2013 from 22.7% (95% CI 19.2 to 26.7, n=108) to 36.4% (95% CI 31.6 to 41.5, n=130). By medication type, there was an increase in antidepressant prescriptions and antipsychotic prescriptions. However, there was no significant change across the study period for anxiolytics/hypnotic prescriptions. See table 3 for a breakdown of numbers and proportions.
Table 3.
The number and proportion of associated* prescriptions for individuals with an incident ED diagnosis
| Antidepressants | Anxiolytic/hypnotics | Antipsychotics | ||||
| Individuals (n) | Proportion† (%, 95% CI) |
Individuals (n) | Proportion† (%, 95% CI) |
Individuals (n) | Proportion† (%, 95% CI) |
|
| Sex | ||||||
| Male | 78 | 17.8 (14.5 to 21.6) | 17 | 3.9 (2.4 to 6.1) | 14 | 3.2 (1.9 to 5.3) |
| Female | 1176 | 27.1 (25.8 to 28.5) | 139 | 3.2 (2.7 to 3.8) | 70 | 1.6 (1.3 to 2.0) |
| Age | ||||||
| 11 to 15 | 128 | 9.0 (7.6 to 10.6) | 21 | 1.5 (1.0 to 2.2) | 22 | 1.5 (1.0 to 2.3) |
| 16 to 20 | 687 | 29.3 (27.5 to 31.1) | 85 | 3.6 (2.9 to 4.5) | 42 | 1.8 (1.3 to 2.4) |
| 21 to 24 | 439 | 43.8 (40.8 to 46.9) | 50 | 5.0 (3.8 to 6.5) | 20 | 2.0 (1.3 to 3.1) |
| Deprivation | ||||||
| 1 (least) | 311 | 25.9 (23.5 to 28.4) | 37 | 3.1 (2.2 to 4.2) | 19 | 1.6 (1.0 to 2.5) |
| 2 | 295 | 28.3 (25.6 to 31.1) | 30 | 2.9 (2.0 to 4.1) | 24 | 2.3 (1.5 to 3.4) |
| 3 | 220 | 24.9 (22.1 to 27.8) | 28 | 3.2 (2.2 to 4.5) | 13 | 1.5 (0.9 to 2.5) |
| 4 | 229 | 24.0 (21.4 to 26.8) | 27 | 2.8 (2.0 to 4.1) | 11 | 1.2 (0.6 to 2.1) |
| 5 (most) | 197 | 28.5 (25.3 to 32.0) | 33 | 4.8 (3.4 to 6.6) | 17 | 2.5 (1.5 to 3.9) |
| Year | ||||||
| 2004 | 105 | 22.1 (18.6 to 26.1) | 8 | 1.7 (0.9 to 3.3) | 3 | 0.6 (0.2 to 1.8) |
| 2005 | 112 | 24.2 (20.6 to 28.4) | 10 | 2.2 (1.2 to 3.9) | 5 | 1.1 (0.5 to 2.5) |
| 2006 | 112 | 22.8 (19.3 to 26.7) | 16 | 3.3 (2.0 to 5.2) | 10 | 2.0 (1.1 to 3.7) |
| 2007 | 133 | 25.3 (21.8 to 29.2) | 19 | 3.6 (2.3 to 5.6) | 4 | 0.8 (0.3 to 1.9) |
| 2008 | 115 | 23.0 (19.6 to 26.9) | 15 | 3.0 (1.8 to 4.9) | 8 | 1.6 (0.8 to 3.1) |
| 2009 | 125 | 26.2 (22.4 to 30.3) | 12 | 2.5 (1.4 to 4.3) | 5 | 1.0 (0.4 to 2.4) |
| 2010 | 105 | 25.7 (21.7 to 30.2) | 21 | 5.1 (3.4 to 7.7) | 12 | 2.9 (1.7 to 5.1) |
| 2011 | 127 | 30.3 (26.1 to 34.9) | 17 | 4.1 (2.5 to 6.4) | 9 | 2.1 (1.1 to 4.0) |
| 2012 | 115 | 29.2 (24.9 to 33.9) | 14 | 3.6 (2.1 to 5.9) | 8 | 2.0 (1.0 to 4.0) |
| 2013 | 123 | 34.5 (29.7 to 39.5) | 18 | 5.0 (3.2 to 7.8) | 12 | 3.4 (1.9 to 5.8) |
| 2014 | 82 | 30.8 (25.6 to 36.6) | 6 | 2.3 (1.0 to 4.8) | 8 | 3.0 (1.5 to 5.8) |
| ED subtype | ||||||
| AN | 290 | 22.2 (20.0 to 24.5) | 30 | 2.3 (1.6 to 3.3) | 26 | 2.0 (1.4 to 2.9) |
| BN | 315 | 28.5 (25.9 to 31.3) | 35 | 3.2 (2.3 to 4.4) | 14 | 1.3 (0.8 to 2.1) |
| EDNOS | 649 | 20.6 (19.2 to 22.1) | 91 | 2.9 (2.4 to 3.5) | 44 | 1.4 (1.0 to 1.9) |
Total study Population=1 135 038 individuals.
*Associated prescription was defined as 6 months before or 12 months after an ED diagnosis.
† Proportion of individuals with an incident ED diagnosis (n=4775).
AN, anorexia nervosa; BN, bulimia nervosa; ED, eating disorder; EDNOS, ED, not otherwise specified.
Individuals diagnosed with BN were the most likely to have an associated antidepressant prescription. There was no difference by ED sub-type for associated anxiolytics/hypnotic prescriptions, nor antipsychotic prescriptions (see table 3).
Referrals to secondary care
A total of 17.4% (95% CI 16.3 to 18.5, n=831) of individuals with a first ever ED diagnosis (n=4775) were referred to secondary care with a crude referral rate of 17.4 per 100 000 person years (95% CI 16.3 to 18.6). There was no significant change in ED referral rate over time or by demographics. Of those not referred (n=3941, three individuals missing since not eligible for HES linkage) 28.4% (95% CI 27.0 to 29.8, n=1118) had an associated inpatient admission for any reason and 9.5% (95% CI 8.7 to 10.5), n=376) had an associated inpatient admission with an ED diagnosis code.
Age-appropriate referrals
There were 380 referrals for individuals aged under 18 years (11–17) and 451 for those aged over 18 years (18–24) with first ever recorded EDs from primary to secondary care. For individuals under 18: 26.6% (95% CI 22.4 to 31.2, n=101) were referred to child and adolescent psychiatry; 7.1% (95% CI 4.9 to 10.1, n=27) to paediatrics; 8.4% (95% CI 6.0 to 11.6, n=32) to adult psychiatry; none were referred to general medicine. For individuals under 18 referred to adult psychiatry, a minority were under the age of 16 (n<5). For those aged over 18 years 28.8% (95% CI 24.8 to 33.2, n=130) were referred to adult psychiatry; less than n=5 were referred to general medicine. A large proportion of referrals for those with recorded EDs did not have a specialty code recorded: 39.2% (95% CI 34.4 to 44.2, n=149) for under 18 s; 40.6% (95% CI 36.1 to 45.2, n=183) for over 18 s.
Associated secondary healthcare use (HES linked)
Outpatient attendance
A total of 2550 (53.4% of 4775, 95% CI 52.0 to 54.9) individuals with an incident ED diagnosis in primary care had an associated outpatient attendance, 23.8% (1135/4775, 95% CI 22.6 to 25.0) in a mental health specialty. The percentage of individuals with an incident ED diagnosis in primary care who had an outpatient attendance to a mental health specialty decreased with age (11 to 15: 27.7%, 95% CI 25.4 to 30.0, n=394, 16 to 20: 22.9%, 95% CI 21.2 to 24.6, n=537 and 21 to 24: 20.4%, 95% CI 18.0 to 23.0, n=204). There were no significant differences in proportions with an associated mental health specialty outpatient attendance by sex or deprivation or over time.
A similar pattern was observed for all outpatient appointments regardless of specialty, except: females were proportionately more likely to have an attendance than males (53.1%, 95% CI 51.6 to 54.6, n=2302 vs 56.5%, 95% CI 51.8 to 61.1, n=248); and the proportion of individuals with an associated outpatient attendance under any specialty has increased over the study period from 47.4% (95% CI 42.9 to 51.9, n=225) in 2004 to 62.5% (95% CI 57.3 to 67.3, n=223) in 2013.
Age-appropriate outpatient attendance
There were 1399 individuals who had an associated outpatient attendance under the age of 18 years and 1272 individuals over 18 years (some individuals were seen in outpatients in both age categories). Of those with an outpatient attendance under the age of 18: 40.1% (95% CI 37.6 to 42.7, n=561) were seen in child and adolescent psychiatry and 32.3% (95% CI 29.9 to 34.8, n=452) in paediatrics. Of those aged under 18 years, 8.2% (95% CI 6.9 to 9.8, n=115) were seen in adult psychiatry and 3.2% (95% CI 2.4 to 4.3, n=45) in general medicine, however these individuals were mainly 16 or 17 years old (83.9%, n=135). Of those over the age of 18 years: 34.8% (95% CI 32.3 to 37.5, n=443) were seen in adult psychiatry and 5.0% (95% CI 3.9 to 6.3, n=63) general medicine.
Inpatient
There were 1294 (27.1%, 95% CI 25.9 to 28.4) individuals with an incident ED diagnosis in primary care with an associated inpatient admission. Of these individuals, 445 (34.4%, 95% CI 31.9 to 37.0) had an inpatient admission with an ED code, making up 9.3% (95% CI 8.5 to 10.2; 445/4775) of incident cases in primary care. For inpatient admissions with an ED diagnosis there were no differences proportionally between sexes or by deprivation. However the younger age groups were more likely to be admitted (11 to 15: 14.7%, 95% CI 13.0 to 16.7, n=210 vs 16 to 20: 8.3%, 95% CI 7.3 to 9.5, n=195 vs 21 to 24: 4.0%, 95% CI 3.0 to 5.4, n=40). The number and proportion of individuals with an associated inpatient admission for an ED has increased over the study period from 5.9% (95% CI 4.1 to 8.4, n=28) in 2004 to 15.0% (95% CI 11.2 to 19.8, n=40) in 2014.
Age-appropriate inpatient admissions
There were 315 individuals who had an associated inpatient admission which included an ED code under the age of 18 years old and 132 individuals who had an associated admission over 18 years old (some individuals were admitted in both age categories). Of those with an inpatient admission with an ED code under the age of 18: 57.5% (95% CI 51.9 to 62.8, n=181) were admitted under paediatrics; 27.3% (95% CI 22.7 to 32.5, n=86) child and adolescent psychiatry; 6.0% (95% CI 3.9 to 9.2, n=19) general medicine; 3.5% (95% CI 2.0 to 6.1, n=11) under adult psychiatry. Only those aged 16 or 17 years were admitted to general medicine or adult psychiatry. Of those admitted with a diagnosis in primary care over the age of 18: 32.6% (95% CI 25.2 to 41, n=43) were under general medicine; 25.8% (95% CI 19.1 to 33.8, n=34) under adult psychiatry.
Psychotropic prescriptions, outpatient attendances and inpatient admissions
Of the 1314 individuals with an associated psychotropic prescription and eligible for HES linkage (three individuals missing), 40.5% (95% CI 37.9 to 43.2, n=532) did not have an associated outpatient attendance. Individuals aged 21–24 years were significantly more likely than those aged 11–15 years to have a prescription without an associated outpatient attendance (11–15 years: 31.3%, 95% CI 24.3 to 39.2, n=45 vs 21–24 years: 44.6%, 95% CI 40.1 to 49.2, n=203). Individuals prescribed antidepressants were the least likely to have an associated outpatient attendance (40.6%, 95% CI 37.8 to 43.3, n=508), followed by anxiolytics/hypnotics (30.1%, 95% CI 23.5 to 37.7, n=47) and antipsychotics (21.4%, 95% CI 14.0 to 31.4, n=18). For those who had an associated prescription but did not have an outpatient attendance, 16.7% (95% CI 13.8 to 20.1, n=89) had an associated inpatient admission for any reason.
Discussion
Summary of main findings
EDs recorded in primary care are nearly 11 times more common in females than males, twice as common in people aged 16–20 years as in those aged 11–15 or 21–24 years and one and a half times as common in individuals from the least deprived areas compared with the most. EDNOS was the most commonly recorded ED with crude incidence rates more than double those for BN or AN. Females were nine times more likely to be diagnosed with EDNOS than males compared with almost 20 times in AN.
The incidence of ED diagnoses in primary care decreased significantly between 2004 and 2014. This was not uniform across ED subtype nor demographics. Incidence rates decreased most significantly for BN, less so for EDNOS and remained stable for AN. Decreases were demonstrated in females and those aged 16–24 years. The numbers of males diagnosed with an ED were too small, particularly for BN which witnessed the greatest decrease for females, to demonstrate any significant change in rates over time. Significant decreases were also found in individuals from the most deprived areas, but not the least, where rates are higher, therefore widening the disparity in recorded diagnosis further.
For associated secondary healthcare use, approximately half of those diagnosed in primary care had an associated outpatient attendance (almost one quarter under a mental health specialty) and just over one quarter had an inpatient admission (less than 10% with an ED diagnosis recorded during admission). Younger age groups were more likely to have an inpatient admission for an ED or an outpatient attendance and females were more likely to have an outpatient attendance under any specialty. The proportion of those with associated secondary healthcare use has increased significantly except for outpatient attendances treated under mental health specialties.
Over one quarter of individuals diagnosed in primary care had an associated psychotropic prescription in primary care. Older age groups were more likely to be prescribed antidepressants or anxiolytics/hypnotics. Females and those with a recorded BN diagnosis were more likely to be prescribed antidepressants. In older patients with BN Selective Serotonin Reuptake Inhibitors (SSRIs) including fluoxetine are recommended as a symptomatic treatment to reduce patients drive to respond to bulimic impulses.
The proportion of those receiving psychotropic prescriptions has increased significantly over the study period except for anxiolytics/hypnotics prescriptions. For individuals prescribed medication, 40% did not have an associated outpatient attendance. The National Institute for Health and Care Excellence (NICE) guidelines state that medication should not be the sole treatment for EDs.20 21 However, it is possible that these prescriptions were for other co-morbid psychiatric conditions often associated with EDs such as anxiety or depression.22 Older age groups and individuals prescribed antidepressants were the most likely to have a prescription without an associated outpatient attendance. Approximately 17% of individuals without an outpatient attendance had an inpatient admission instead. This was more common for those aged 11–15 years.
In general, people aged 11–24 years were being treated in age-appropriate settings. The majority of people aged under 18 years who were being treated under adult specialties were aged either 16 or 17 years.
Comparisons with existing literature
The last UK study calculating the incidence of EDs in primary care uses general practice records dating back to 2009.10 We found higher crude incidence rates probably reflecting the younger age of our study population (aged 10–49 vs 11–24 years) since EDs are less prevalent in older age groups and the different denominators used (Office of National Statistics mid-year population estimates vs person years). Similar to previous studies, we found that rates of recorded AN have remained stable over time8 10 and EDNOS was the most commonly recorded ED.10 We found that recorded rates of BN had decreased since 2009 in keeping with a Dutch study.8 Micali et al 10 found that rates remained stable between 2000 and 2009. Smink et al 8 suggest that BN is a Western world phenomena based on a pressure to be thin whereas AN is less culture bound existing across time, cultures and even species. Based on this theory, they suggest that the decrease in BN could be attributed to the normalisation of being overweight, thereby reducing the pressure to be thin and leading to a decrease in BN. However, this concept is contested with the rise in social media use suggested as increasing concerns about weight and body image leading to eating concerns and disordered eating.23 24 The fluctuation of EDNOS rates found in this study could reflect the combination of the change in rates for BN and the stability of AN, since diagnoses in this category border both BN and AN.
Previous studies18 19 have attributed a decrease in diagnoses for common mental health disorders in primary care to a change in the coding behaviour of GPs to code for symptoms (in order to avoid labelling or strategically in relation to the Quality Outcomes Framework). ED symptom codes are less specific than symptom codes for conditions such as depression or anxiety and when explored further, the coding behaviour of GPs seen in studies for depression19 and anxiety18 was not observed for EDs. EDs can be problematic conditions for doctors to identify, refer and manage for several reasons. Currin et al 25 found that GPs diagnosed less than 70% of cases with clear ED presentation. House et al 26 found that GPs were less likely to diagnose if there were no specialist services in the area. Availability of child and adolescent mental health services and lower thresholds for acceptance of referrals than in adult services for EDs, could explain why ED diagnosis rates for people aged 11–15 years have remained stable over the study period, yet decreased for those aged 16–24 years. NICE 2004 guidelines recommend that care is shared between primary and specialist care with a clear (preferably written) agreement of roles.20 It is argued that GPs are sometimes reluctant to diagnose EDs due to this associated burden of care and poor access to specialist services.27 This type of impact on recording of diagnoses and labelling may impact those from the most deprived areas disproportionately since historically they experience inequity of access to healthcare services.28 They may be less persistent in obtaining a diagnosis in order to access the services they need: a phenomena named ‘the inverse care law’.29 By diagnosing individuals later in the course of development of an ED, patients are put at greater risk of serious medical complications and increasing the likelihood of treatment resistance.30
From one perspective it is reassuring that we found the proportion of those receiving care from specialists services is increasing as this could suggest better care, particularly through outpatient services. However the increase in those receiving inpatient care could suggest that first presentations to primary care (or at least first recorded) are later and becoming more severe, therefore requiring inpatient admission. This is supported by Waller et al 27 who report that GPs use a ‘wait and see’ approach, but then rapidly escalate care and request inpatient management when the patient deteriorates. NICE guidelines recommend inpatient admission for medical stabilisation or to initiate refeeding if the individual’s physical health is severely compromised if these cannot be done in an outpatient setting21 but possibly do not provide sufficient advice on early management of potentially emerging EDs in primary care.
Strengths and limitations
The study’s key strength is the size of the sample population used. CPRD is one of the largest primary care databases in the world and is representative of the English population.13 There is no reason to believe the results would differ for the entire population of UK. Using primary care data allowed us to identify milder cases not captured in studies using secondary care databases or psychiatric case registers.
However the study may still underestimate the incidence of EDs. The analysis essentiality is one of coding behaviour,19 and differences in rates could be due to a wider availability of other services, rather than true differences in occurrence.31 Another limitation was restricting the analysis to English data only. Deprivation data based on the patients LSOA was not available in Wales, Scotland or Northern Ireland and so was excluded in order to account for deprivation in Poisson regression models. These data accounted for 22% of the total study population. This approach was different to Carr et al 12 who used IMD data according to the postcode of the general practice which had the benefit of availability across all nations. However we felt the accuracy of linking to the LSOA of the individual’s home address was greater than using the general practice’s address. Furthermore, since IMD is measured differently across nations, it is not considered comparable.32 Another limitation was the poor recording of some data, particularly the specialty code for referrals where 40% of the data was not entered; this impedes the accuracy of the results reflecting the age appropriateness of GP referrals for EDs. Second, 97.3% of outpatient records had the diagnosis code ‘Unknown and unspecified causes of morbidity’; this meant we could not infer whether outpatient attendances were for EDs. Finally with regard to associated prescriptions, inpatient admissions or outpatient attendances, since these indications are not explicitly recorded in routinely collected primary-care data, the indications can only be inferred and not conclusively determined.
Implications for clinical practice and research
This study explicitly linked deprivation to individuals with ED diagnoses. This evidence can be used to target services more effectively towards individuals from the least deprived areas, but also should be used to ensure that there are no barriers preventing individuals from the most deprived areas from attending their GP if they have a problem. Future research should explore why ED rates are declining for individuals from the most deprived areas, as well as individuals diagnosed with BN. We also need to establish if first presentations are becoming more severe or if GPs are waiting for ED symptoms to worsen until they diagnose, record and refer.
In the NICE guidelines there is little advice for GPs about how to manage patients with EDs, particularly for BN. Wilson and Shafran33 claim NICE guidelines for EDs are not evidence-based, but argue this is due to a lack of good quality research for the treatment of EDs. Currin et al 25 found that only 4% of GPs reported using published guidelines when managing individuals with an ED and none of the GPs questioned used the national guidelines. They also found there was little association between recommended and practised treatment behaviour. This highlights a huge gap in the research field which needs to be addressed to inform appropriate management and referral guidelines, as well as best methods to disseminate and encourage GPs to follow them. Guidelines and training for the recording of conditions need to be developed and put into practice. As far as we are aware there is no treatment trial in young people to establish the efficacy of either psychological or pharmacological interventions, let alone comparing the two approaches alone or in combination.
If there is harmonisation of the identification and recording of EDs in primary care this would not only support clinical improvement, we will be able to assess more accurately if rates in primary care are reducing or not. We found 40% of those prescribed psychotropic medication did not have an associated outpatient attendance. This may not be in keeping with NICE21 guidelines and should be explored further. This could be part of any evaluation of the NHS England implementation of Access and Waiting Time Standards for Eating Disorders, 2015.34
Supplementary Material
Acknowledgments
This study is based on data from the Clinical Practice Research Datalink (CPRD) obtained under licence from the UK Medicines and Healthcare products Regulatory Agency. The data is provided by patients and collected by the National Health Service (NHS) as part of their care and support. The Office of National Statistics is the provider on the ONS data contained within the CPRD Data. Copyright © (2018), re-used with the permission of The Health & Social Care Information Centre. All rights reserved The OPCS Classification of Interventions and Procedures, codes, terms and text is Crown copyright (2016) published by Health and Social Care Information Centre, also known as NHS Digital and licensed under the Open Government License available at www.nationalarchives.gov.uk/doc/open-government-licence/open-governmentlicence.htm
Footnotes
Contributors: AJ, KW, MA conceived the study; all authors designed the study; AJ supervised the study; SW, AM, HJ, JB analysed the data; AJ, SW wrote the initial draft and all authors commented on the manuscript.
Funding: This study was funded by MQ through the Adolescent Data Platform. AJ and HJ are supported by The Farr Institute CIPHER, funded by Arthritis Research UK, the British Heart Foundation, Cancer Research UK, the Economic and Social Research Council, the Engineering and Physical Sciences Research Council, the Medical Research Council, the National Institute of Health Research, the National Institute for Social Care and Health Research (Welsh Assembly Government), the Chief Scientist Office (Scottish Government Health Directorates), and the Wellcome Trust, (MRC Grant No: MR/K006525/1).
Disclaimer: The interpretation and conclusions contained in this study are those of the author/s alone.
Competing interests: None declared.
Ethics approval: Ethical approval was obtained under licence from the Independant Scientific Advisory Committee of the UK Medicines and Healthcare products Regulatory Agency.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Data analysed for this study were obtained under institutional licence from the Clinical Practice Research Datalink (https://www.cprd.com/intro.asp). Data are not available for sharing but can be applied for through the CPRD. Relevant data are also available in the paper and its Supporting Information files.
Press Release: Once we have a publication date we plan to write a press release and an article for the Conversation
Patient consent for publication: Permissions granted to CPRD of anonymised routine data
References
- 1. Bould H, Newbegin C, Stewart A, et al. Eating disorders in children and young people. BMJ 2017;359:j5245 10.1136/bmj.j5245 [DOI] [PubMed] [Google Scholar]
- 2. Katzman DK. Medical complications in adolescents with anorexia nervosa: a review of the literature. Int J Eat Disord 2005;37(Suppl):S52–9. 10.1002/eat.20118 [DOI] [PubMed] [Google Scholar]
- 3. Pompili M, Girardi P, Tatarelli G, et al. Suicide and attempted suicide in eating disorders, obesity and weight-image concern. Eat Behav 2006;7:384–94. 10.1016/j.eatbeh.2005.12.004 [DOI] [PubMed] [Google Scholar]
- 4. Arcelus J, Mitchell AJ, Wales J, et al. Mortality rates in patients with anorexia nervosa and other eating disorders. A meta-analysis of 36 studies. Arch Gen Psychiatry 2011;68:724–31. 10.1001/archgenpsychiatry.2011.74 [DOI] [PubMed] [Google Scholar]
- 5. Sadler K, Vizard T, Ford T, et al. Mental Health of Children and Young People in England, 2017. NHS Digital, 2018. [Google Scholar]
- 6. BEAT eating disorders. Statistics for Journalists. Available at https://www.beateatingdisorders.org.uk/media-centre/eating-disorder-statistics.
- 7. Bould H, De Stavola B, Magnusson C, et al. The influence of school on whether girls develop eating disorders. Int J Epidemiol 2016;45:480–8. 10.1093/ije/dyw037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Smink FR, van Hoeken D, Donker GA, et al. Three decades of EDs in Dutch primary care: decreasing incidence of BN but not of AN. Psychol Med 2016;46:1189–96. [DOI] [PubMed] [Google Scholar]
- 9. Hoek HW. Review of the worldwide epidemiology of eating disorders. Curr Opin Psychiatry 2016;29:336–9. 10.1097/YCO.0000000000000282 [DOI] [PubMed] [Google Scholar]
- 10. Micali N, Hagberg KW, Petersen I, et al. The incidence of eating disorders in the UK in 2000–2009: findings from the General Practice Research Database. BMJ Open 2013;3:e002646 10.1136/bmjopen-2013-002646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Smink FR, van Hoeken D, Hoek HW. Epidemiology of eating disorders: incidence, prevalence and mortality rates. Curr Psychiatry Rep 2012;14:406–14. 10.1007/s11920-012-0282-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Carr MJ, Ashcroft DM, Kontopantelis E, et al. The epidemiology of self-harm in a UK-wide primary care patient cohort, 2001-2013. BMC Psychiatry 2016;16:53 10.1186/s12888-016-0753-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Herrett E, Gallagher AM, Bhaskaran K, et al. Data Resource Profile: Clinical Practice Research Datalink (CPRD). Int J Epidemiol 2015;44:827–36. 10.1093/ije/dyv098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. StataCorp. Stata Statistical Software: Release 13. College Station: StataCorp LP, 2013. [Google Scholar]
- 15. NCEPOD. The mental healthcare of young people and young adults. The National Confidential Enquiry into Patient Outcome and Death. In Press. [Google Scholar]
- 16. Frisher M, Collins J, Millson D, et al. Prevalence of comorbid psychiatric illness and substance misuse in primary care in England and Wales. J Epidemiol Community Health 2004;58:1036–41. 10.1136/jech.2003.017384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. DCLG. English Indices of Deprivation 2010 Guidance document. London: Department for Communities and Local Government, 2011. [Google Scholar]
- 18. John A, Marchant AL, McGregor JI, et al. Recent trends in the incidence of anxiety and prescription of anxiolytics and hypnotics in children and young people: An e-cohort study. J Affect Disord 2015;183:134–41. 10.1016/j.jad.2015.05.002 [DOI] [PubMed] [Google Scholar]
- 19. John A, Marchant AL, Fone DL, et al. Recent trends in primary-care antidepressant prescribing to children and young people: an e-cohort study. Psychol Med 2016;46:3315–27. 10.1017/S0033291716002099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. NICE. Core Interventions in the Treatment and Management of Anorexia Nervosa, Bulimia Nervosa and Related Eating Disorders (CG9). The British Psychological Society and Gaskell 2004. [PubMed] [Google Scholar]
- 21. NICE. EDs: recognition and treatment (NG69): National Institute for Healthcare and Excellence, 2017. [Google Scholar]
- 22. Hudson JI, Hiripi E, Pope HG, et al. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biol Psychiatry 2007;61:348–58. 10.1016/j.biopsych.2006.03.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Mabe AG, Forney KJ, Keel PK. Do you "like" my photo? Facebook use maintains eating disorder risk. Int J Eat Disord 2014;47:516–23. 10.1002/eat.22254 [DOI] [PubMed] [Google Scholar]
- 24. Sidani JE, Shensa A, Hoffman B, et al. The Association between Social Media Use and Eating Concerns among US Young Adults. J Acad Nutr Diet 2016;116:1465–72. 10.1016/j.jand.2016.03.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Currin L, Waller G, Treasure J, et al. The use of guidelines for dissemination of "best practice" in primary care of patients with eating disorders. Int J Eat Disord 2007;40:476–9. 10.1002/eat.20385 [DOI] [PubMed] [Google Scholar]
- 26. House J, Schmidt U, Craig M, et al. Comparison of specialist and nonspecialist care pathways for adolescents with anorexia nervosa and related eating disorders. Int J Eat Disord 2012;45:949–56. 10.1002/eat.22065 [DOI] [PubMed] [Google Scholar]
- 27. Waller G, Micali N, James A. General Practitioners are poor at identifying the eating disorders. Adv Eat Disord 2014;2:146–57. 10.1080/21662630.2013.859437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Cookson R, Propper C, Asaria M, et al. Socio‐Economic Inequalities in Health Care in England. Fiscal Studies 2016;37:0143–5671. [Google Scholar]
- 29. Tudor Hart J. The Inverse Care Law. The Lancet 1971;297:405–12. 10.1016/S0140-6736(71)92410-X [DOI] [PubMed] [Google Scholar]
- 30. Gurney VW, Halmi KA. An eating disorder curriculum for primary care providers. Int J Eat Disord 2001;30:209–12. 10.1002/eat.1074 [DOI] [PubMed] [Google Scholar]
- 31. van Son GE, van Hoeken D, Bartelds AI, et al. Time trends in the incidence of eating disorders: a primary care study in the Netherlands. Int J Eat Disord 2006;39:565–9. 10.1002/eat.20316 [DOI] [PubMed] [Google Scholar]
- 32. Abel GA, Barclay ME, Payne RA. Adjusted indices of multiple deprivation to enable comparisons within and between constituent countries of the UK including an illustration using mortality rates. BMJ Open 2016;6:e012750 10.1136/bmjopen-2016-012750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Wilson GT, Shafran R. EDs guidelines from NICE. Lancet 2005;365:79–81. [DOI] [PubMed] [Google Scholar]
- 34. National Collaborating Centre for Mental Health, Access and Waiting Time Standard for Children and Young People with an Eating Disorder Commissioning Guide. Available at https://www.england.nhs.uk/wp-content/uploads/2015/07/cyp-eating-disorders-access-waiting-time-standard-comm-guid.pdf.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2018-026691supp001.pdf (699.6KB, pdf)