Abstract
Purpose of review
To summarize the status of HIV and substance use in Central Asia and discuss potential ways to move forward to effective epidemic control among people who inject drugs (PWID) in the region and beyond.
Recent findings
PWID and their partners remain the population most affected by HIV in Central Asia. Lack of effective substance use prevention and treatment options and limited involvement of PWID-led community-based organizations in HIV programs, combined with the requirement for official registration, stigma and discrimination of PWID, and criminalization of drug use remain key barriers to effective HIV prevention and treatment.
Summary
Sustainable HIV epidemic control among PWID will not be feasible without decriminalization of drug use, addressing stigma and discrimination and policy changes to enhance uptake of HIV-related prevention, treatment and support services by PWID. It is also critical to ensure adoption of innovations, particularly those that combine evidence-based biomedical, behavioral and structural interventions tailored to the needs of the PWID.
Keywords: Central Asia, HIV, people who inject drugs
INTRODUCTION
According to the 2018 World Drug Report, an estimated 275 million people worldwide used drugs for nonmedical purposes at least once during 2016. More than 30 million people who use drugs suffer from drug use disorders, and approximately 10.6 million people inject drugs, with opioids causing the most harm and accounting for 76% of drug use-related deaths [1]. In 2017, the risk of acquiring HIV by people who inject drugs (PWID) was 22 times higher than for people who do not inject drugs [2]. Thus, it is estimated that as many as 1.3 million PWID globally are living with HIV [1]. Noninjecting drug use, particularly methamphetamine and cocaine, and alcohol use are also associated with increased risks of HV acquisition [3,4▪,5▪,6,7▪,8,9]. Along with this increased risk, substance use negatively affects the health of persons living with HIV (PLHIV) and has a negative impact on HIV care and treatment outcomes [10▪,11▪,12▪▪,13,14]. A study conducted by Lancaster et al.[11▪] among HIV-infected female sex workers in Malawi found that harmful drinking or alcohol dependence was associated with sub-optimal engagement in HIV treatment. Another recent study conducted among a cohort of 1799 HIV-positive women in the United States found that substance use was associated with suboptimal adherence to antiretroviral therapy (ART) among study participants on multiple-tablet ART regimens, as well as single-tablet ART regimens [10▪].
On a regional level, countries of Eastern Europe and Central Asia are severely affected by substance use and its interrelation with HIV. According to the Joint United Nations Programme on HIV/AIDS (UNAIDS), unlike other regions in the world, countries of this region demonstrate neither reduction in HIV-related mortality nor in HIV incidence with a doubling in the annual number of new HIV infections noted in less than 20 years [15]. In addition, this region has one of the largest numbers of PWID, as well as the highest number of PWID who are living with HIV [1,2].
Central Asia includes five countries: Kazakhstan, the Kyrgyz Republic, Tajikistan, Turkmenistan and Uzbekistan with a total population of more than 60 million ethnically, culturally and religiously diverse people. The region is located on what has been called the ‘Northern drug traffic route’ and in this article, we primarily focus on three countries – Kazakhstan, the Kyrgyz Republic and Tajikistan. The most recent population size estimates show that there are 120 500 PWID in Kazakhstan (UNAIDS, 2016), 25 000 in the Kyrgyz Republic (UNAIDS, 2016) and 23 100 in Tajikistan (UNAIDS, 2015). PWID and their sex partners remain the population most affected by HIV in the region. By the end of 2018, national HIV program data showed that approximately 40% of all PLHIV in Kazakhstan and the Kyrgyz Republic, and 30% in Tajikistan reported a history of injecting drug use in the past and/or were currently injecting drugs. Considering the potential underreporting of injection drug use because of stigmatization of this behavior, especially among women, the accurate proportion of HIV infections related to injection drug use might be even higher [16▪].
Data from the last rounds of the national integrated bio-behavioral surveys (IBBS) show that HIV prevalence among PWID ranged from 0 to 25% across sentinel sites (geographical areas) in Kazakhstan (IBBS 2018), 9.5–24.0% across sites in the Kyrgyz Republic (IBBS 2016), and from 4 to 18.5% across sites in Tajikistan (IBBS 2018). In addition, a large proportion of PWID also have hepatitis virus C (HCV) infection, with HCV antibody prevalence among PWID ranging from 36 to 99% across sentinel sites in Kazakhstan (IBBS, 2018) and 47–79% in the Kyrgyz Republic (IBBS, 2016). In Central Asia as in other parts of the world, PWID, especially those with an incarceration history, are at high risk of tuberculosis (TB) and TB-related mortality [17,18]. Thus, for this region, the dual stigma of injection drug use and HIV as well as the high prevalence of comorbid conditions, such as hepatitis C virus (HCV) and tuberculosis, impacts the health and well being of this population [19].
Box 1.
no caption available
CHALLENGES TO THE HIV CONTINUUM FOR PEOPLE WHO INJECT DRUGS
Key populations, including PWID face considerable challenges from the perspective of both the HIV prevention as well as the HIV care continua [20▪▪,21].
Firstly, stigma and discrimination associated with the use of illicit drugs create significant barriers for people in their attempts to access HIV prevention, care and treatment services in many countries [2,22▪–24▪]. In countries of Central Asia, stigma and discrimination at the level of service providers and the general population, combined with the requirement for official registration of PWID, and criminalization of drug use lead to high rates of incarceration and reluctance to engage with the health establishment [25▪,26▪,27▪▪,28▪]. Local sociocultural contexts, in particular, cultural customs, religious beliefs and gender norms, particularly in more conservative rural areas further facilitate stigmatizing beliefs [29▪], especially towards women who inject drugs [30▪,31]. Secondly, limited involvement of community-based organizations in HIV programming for PWID and limited availability of HIV services for PWID at the community level also negatively affect access to and uptake of HIV services by PWID [32,33]. Thirdly, another challenge is that very few PWID in the region have access to high-quality pharmacological and abstinence-oriented drug treatment interventions. Options for rehabilitation, recovery and social reintegration are limited [34▪▪]. Although coverage of PWID with opioid agonist therapy (OAT) using methadone has increased by approximately 50% over the past 5 years in the Kyrgyz Republic and Tajikistan, it remains alarmingly low. For example, in Kazakhstan, access in 2018 was extremely limited, with only 250 patients (0.2% of the estimated number of PWID) enrolled in OAT programs at any point in time. In the absence of appropriate substance use treatment services, the impaired judgment and mental health effects of substance use create difficulties for PWID in engaging with HIV prevention or treatment interventions [25▪,35,36,37▪].
The increasing number of people, especially young people, injecting synthetic cathinones (‘bath salts’) in Kazakhstan poses another challenge to HIV prevention because of very risky drug preparation and use practices and lack of appropriate supportive services for such individuals [38▪].
With regards to HIV treatment specifically, data from the region show that substance use including injecting drugs and harmful use of alcohol have been noted to be associated with treatment discontinuation among PWID living with HIV who were initiated on ART in Kazakhstan [39▪]. As a result, PLHIV who inject drugs tend to be enrolled in HIV care less often and are less likely to be initiated and effectively retained on treatment compared with those who do not inject drugs as noted in Fig. 1. As a result, only 30% of PWID diagnosed with HIV had viral load suppression, compared with 37% among non-PWIDs living with HIV [40▪▪].
FIGURE 1.
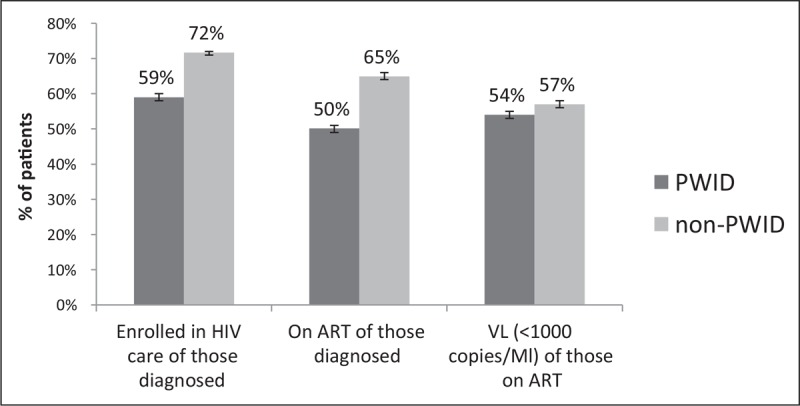
Proportion of people living with HIV (people who inject drugs [N1 = 13 727] and non-PWID [N2 = 20177]) enrolled in HIV care, on antiretroviral therapy and with viral load suppression (<1000 copies/ml) as of 31 December 2018 in Kazakhstan, the Kyrgyz Republic and Tajikistan (Ministry of Health data). PWID, people who inject drugs.
IMPROVING ACCESS TO HIV TESTING
HIV self-testing and community-based peer HIV testing are approaches that hold promise for reaching people who are not accessing existing HIV testing services, including PWID. A cross-sectional study of 1230 individuals, including 287 PWID, conducted in Vietnam showed that HIV testing conducted by peers enabled identifying HIV-positive individuals with high rates of ART initiation, and, thus, may be an effective approach to reach PWID who are unaware of their HIV status [41▪]. In another study from Vietnam [42▪], HIV self-testing was noted to be acceptable among PWID. Further work is needed to determine how best to utilize the self-test, particularly as privacy and confidentiality of HIV self-testing were the key reasons that PWID cited for choosing HIV self-testing. Implementation of social network methods, such as respondent-driven sampling and peer-based active case-finding have also been shown to be effective in identifying and engaging PWID with prior unknown HIV status in studies conducted in Tajikistan, India and Ukraine [43▪–45▪].
IMPROVING ANTIRETROVIRAL THERAPY INITIATION AND ADHERENCE
Opioid antagonist therapy is associated with substantial reductions in the risk for all-cause mortality in people dependent on opioids [46▪▪]. There is strong evidence of the positive effects of OAT on ART initiation, ART adherence, retention on ART and viral load suppression [47,48▪,49▪▪]. Integration of OAT and ART services increases ART and OAT use and reduces mortality among PWID [50▪]. Enrollment in OAT also has positive effects on HCV and TB among PWID, facilitating the engagement in treatment, as well as improving treatment outcomes [51,52,53▪]. On the basis of these findings, since 2014, we have supported the piloting of integrated delivery of HIV and OAT using methadone and TB services at six sites across Kazakhstan and Tajikistan. A cross-sectional analysis of patient records from 179 HIV-positive patients enrolled in OAT at integrated delivery and standard-of-care sites showed a significantly positive effect of the former on viral load suppression. Overall, 87% (95% CI: 80–93%) of PLHIV receiving services at the integrated service delivery sites had viral load suppression, whereas only 63% (95% CI 49–76%) of PLHIV enrolled at standard-of-care sites were virally suppressed [54▪].
Two recent randomized clinical trials showed positive effects of extended-release naltrexone (XR-NTX), an opiate antagonist that is available in long-acting formulation, on viral load suppression among incarcerated PLHIV with opioid dependence or alcohol use disorders 6 months after transitioning to the community [55▪▪,56▪▪]. PLHIV who had history of injection drug use released from prison were given a monthly injection of XR-NTX for 6 months, beginning with a week before their release. Participants on the XR-NTX arm of the study were more likely than the placebo group to improve viral suppression (30.3 vs. 18.5%); maintain viral suppression (30.3 vs. 27.3%), and less likely to lose viral suppression (7.6 vs. 33.3%) by 6 months. Findings from another study among 1613 PWID in Ukraine, a setting similar to Central Asia context in terms of HIV epidemic drivers and treatment coverage for opioid use disorders, showed that 28% of PWID were willing to initiate XR-NTX. Thus, XR-NTX offers an option for addiction treatment and ART adherence support especially for PWID who have shorter history of injection and who harbor negative attitudes regarding methadone maintenance therapy (MMT) [57▪]. However, XR-NTX's high cost and lack of pharmacopeia registration makes it inaccessible in several countries in Central Asia.
INTERVENTIONS FOR PREVENTION OF HIV ACQUISITION
It is widely acknowledged that needle and syringe programs (NSPs) and OAT decrease HIV incidence among persons who inject opioids by reducing injecting drug use and sharing of injecting equipment [58]. Thus, the expansion of access to NSP and OAT is as critically important to prevention of HIV acquisition as it is for enhancing outcomes among PWID living with HIV.
In terms of interventions for primary prevention, the evidence of the efficacy of preexposure prophylaxis (PrEP) for prevention of HIV acquisition among individuals at substantial risk for HIV has generated interest in its potential value among PWID. The Bangkok PrEP Trial, conducted among a large cohort of PWID, demonstrated 70% reduction of HIV acquisition among participants with detectable tenofovir levels [59]. However, implementation of PrEP among PWID is still limited and PWID are often unaware of PrEP as an HIV prevention intervention. Others from this population do not always support use of PrEP -- fearing that this might shift attention from harm reduction initiatives, such as needle and syringe programs, OAT and naloxone [60]. However, a recently published qualitative study conducted in the Northeastern USA among 33 HIV-uninfected PWID and 12 clinical and social service providers [61▪▪] showed that there was substantial interest in PrEP; however, both PWID and providers described several barriers to PrEP use, including fears that the high costs of PreP could reduce funding for harm reduction programs, such as NSP, and uncertainty about the effectiveness of PrEP among PWID. Further work is needed to explore the potential use of PrEP among PWID in Central Asia. Given the high proportion of HIV-positive PWID with unsuppressed virus and low rates of consistent condom use with regular partners, implementation of PrEP should also be explored among sex partners of PWID.
Lastly, combining use of index testing of injecting and sex partners of PWID with assays that identify recent HIV infection could be fruitful in identifying those at risk for HIV acquisition for prevention efforts while ensuring prompt initiation of HIV treatment for those found to be HIV positive to prevent further transmission of HIV [62].
CONCLUSION
Control of the HIV epidemic among PWID will not be feasible without addressing fundamental factors that drive transmission of HIV and that impede engagement of HIV-positive PWID in effective care and treatment in the countries of Central Asia. Prevention of new HIV infections among PWID will require expanding access of PWID to key evidence-based primary prevention interventions, such as harm reduction programs, and OAT.
Efforts to ensure critical social enablers are essential to control of the HIV epidemic among PWID (Fig. 2). This will require prioritization of human rights over political agendas and over rigid moralistic attitudes. Decriminalization of drug use and other policy changes are needed including abandoning the existing requirement for mandatory collection of personal data as part of the registration of persons with substance use disorders, which may enhance access to and uptake of health services by this population and may facilitate reduction in stigma and discrimination related to drug use.
FIGURE 2.

Requirements to achieving HIV epidemic control among people who inject drugs.
In addition, there is the urgent need for adoption of innovations, such as expansion of HIV testing at the community level, including self-testing options for PWID and their partners, as well as pursuit of PrEP as an additional HIV prevention intervention. Assessment of the feasibility and effectiveness of combinations of evidence-based biomedical, behavioral and structural interventions is needed. Such interventions need to be developed and implemented with active community engagement to inform their design and implementation and to take into account the needs of sub-populations of PWID, for example, substance-using youth and women. Ultimately, adoption of differentiated service delivery models is needed in order to tailor services to the needs of this population [63▪].
With the decrease in external HIV funding for Central Asian countries, it becomes crucially important to garner strong political will and sufficient national funding are available to enable PWID to access the package of recommended interventions that have been shown to be effective in reducing HIV transmission among this population [64]: OAT must be acknowledged as a fundamental component of the management of opioid dependence and must be integrated with other relevant health services, such as HIV services and/or primary healthcare services.
In summary, successful control of the global HIV epidemic requires attention to addressing the contribution of substance use to continued transmission of HIV. It will also require overcoming deep societal prejudices regarding substance users and concerted efforts to shape the HIV response to their unique needs.
Acknowledgements
We acknowledge support of Katherine Harripersaud, MPH in the development of this manuscript.
Financial support and sponsorship
None.
Conflicts of interest
There are no conflicts of interest.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
REFERENCES
- 1.UNODC. World Drug Report 2018. United Nations Publication; 2019. [Google Scholar]
- 2.UNAIDS. Miles to go: closing gaps, breaking barriers, fighting injustices. Global AIDS Report, 2018. Geneva; 2018. [Google Scholar]
- 3.Sandfort TGM, Knox JR, Alcala C, et al. Substance use and HIV risk among men who have sex with men in Africa: a systematic review. J Acquir Immune Defic Syndr 2017; 76:e34–e46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4▪.Williams EC, Hahn JA, Saitz R, et al. Alcohol use and human immunodeficiency virus (HIV) infection: current knowledge, implications, and future directions. Alcoholism Clin Exp Res 2016; 40:2056–2072. [DOI] [PMC free article] [PubMed] [Google Scholar]; This narrative review described literature regarding alcohol's impact on transmission, care, coinfections and comorbidities that are common among people living with HIV (PLWH), as well as literature regarding interventions to address alcohol use and its influences among PLWH. Alcohol use appears to have additive and potentially synergistic effects on common HIV-related comorbidities.
- 5▪.Des Jarlais DC, Arasteh K, McKnight C, et al. What happened to the HIV epidemic among noninjecting drug users in New York City? Addiction (Abingdon, England) 2017; 112:290–298. [DOI] [PMC free article] [PubMed] [Google Scholar]; The study included serial cross sectional surveys of people entering drug treatment programs. HIV prevalence has declined and a high percentage of HIV-positive noninjecting drug users (NIDUs) are receiving antiretroviral treatment, suggesting an end to the HIV epidemic among NIDUs in New York City.
- 6.Des Jarlais DC, McKnight C, Arasteh K, et al. A perfect storm: crack cocaine, HSV-2, and HIV among noninjecting drug users in New York City. Subst Use Misuse 2014; 49:783–792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7▪.França D, Del-Rios NHA, Carneiro M, et al. HIV-1 infection among crack cocaine users in a region far from the epicenter of the HIV epidemic in Brazil: prevalence and molecular characteristics. PloS One 2018; 13:e0199606. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study showed high prevalence of and risk factors for HIV infection among crack cocaine users admitted to a referral hospital in Central-West Brazil for psychiatric disorders.
- 8.Degenhardt L, Mathers B, Guarinieri M, et al. Reference Group to the United Nations on HIV and injecting drug use. Meth/amphetamine use and associated HIV: implications for global policy and public health. Int J Drug Policy 2010; 21:347–358. [DOI] [PubMed] [Google Scholar]
- 9.Vu NT, Maher L, Zablotska I. Amphetamine-type stimulants and HIV infection among men who have sex with men: implications on HIV research and prevention from a systematic review and meta-analysis. J Int AIDS Soc 2015; 18:19273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10▪.Zhang Y, Wilson TE, Adedimeji A, et al. The impact of substance use on adherence to antiretroviral therapy among HIV-infected women in the United States. AIDS Behav 2018; 22:896–908. [DOI] [PMC free article] [PubMed] [Google Scholar]; In this study, substance use was associated with suboptimal adherence to ART among single tablet regimens (STR) and/or multiple tablet regimens (MTR) users.
- 11▪.Lancaster KE, Lungu T, Mmodzi P, et al. The association between substance use and sub-optimal HIV treatment engagement among HIV-infected female sex workers in Lilongwe, Malawi. AIDS Care 2017; 29:197–203. [DOI] [PMC free article] [PubMed] [Google Scholar]; The study found that harmful drinking or alcohol dependence is associated with sub-optimal engagement in HIV treatment among HIV-infected FSW.
- 12▪▪.Lancaster KE, Hetrick A, Jaquet A, et al. Substance use and universal access to HIV testing and treatment in sub-Saharan Africa: implications and research priorities. J Virus Erad 2018; 4 Suppl 2:26–32. [DOI] [PMC free article] [PubMed] [Google Scholar]; In this article, authors identified several implementation and operations research priorities and metrics for monitoring the impact of substance use and Treat All (a universal testing and treatment for HIV). As the rollout of ART expands in SSA, substance use will remain an ongoing challenge for achieving universal testing and treatment. Negative impact of substance use on HIV care and treatment outcomes is emphasized in evidence from other settings.
- 13.Altice FL, Kamarulzaman A, Soriano VV, et al. Treatment of medical, psychiatric, and substance-use comorbidities in people infected with HIV who use drugs. Lancet 2010; 376:367–387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kamarulzaman A, Altice FL. Challenges in managing HIV in people who use drugs. Curr Opin Infect Dis 2015; 28:10–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.UNAIDS. UNAIDS data 2018. UNAIDS/JC2929E. Available at: http://www unaids org/sites/default/files/media_asset/unaidsdata-2018_en pdf# page= 4&zoom= auto,-62,843. (Accessed 8 February 2019). 2018; 12 (08). [Google Scholar]
- 16▪.Deryabina AP, Patnaik P, El-Sadr WM. Underreported injection drug use and its potential contribution to reported increase in sexual transmission of HIV in Kazakhstan and Kyrgyzstan. Harm Reduct J 2019; 16:1. [DOI] [PMC free article] [PubMed] [Google Scholar]; In this study, high prevalence of HIV and HCV was reported among noninjecting sex-partners of PWID suggesting possible underreporting of previous or current injection drug use among partners, especially women.
- 17.Getahun H, Baddeley A, Raviglione M. Managing tuberculosis in people who use and inject illicit drugs. Bull World Health Organ 2013; 91:154–156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hermosilla S, El-Bassel N, Aifah A, et al. Tuberculosis report among injection drug users and their partners in Kazakhstan. Public health 2015; 129:569–575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kazatchkine M. Drug use, HIV, HCV and TB: major interlinked challenges in Eastern Europe and Central Asia. J Int AIDS Soc 2014; 17 4 Suppl 3:19501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20▪▪.Brown AE, Attawell K, Hales D, et al. Monitoring the HIV continuum of care in key populations across Europe and Central Asia. HIV Med 2018. [DOI] [PubMed] [Google Scholar]; Data from 48 European and Central Asian countries reported through 2016 ECDC survey was used to measure and compare the continuum of HIV care estimates in 3 key subpopulations (Men who have sex with men (MSM), Migrants, People who inject drugs (PWID)). While the estimates are only slightly below the national picture in Western European countries, PWID in Eastern Europe and Central Asia countries have consistently worse estimates compared with the national picture in all analytical frameworks.
- 21.El-Bassel N, Strathdee SA, El Sadr WM. HIV and people who use drugs in central Asia: confronting the perfect storm. Drug Alcohol Depend 2013; 132 Suppl 1:S2–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22▪.Turan B, Rogers AJ, Rice WS, et al. Association between perceived discrimination in healthcare settings and HIV medication adherence: mediating psychosocial mechanisms. AIDS Behav 2017; 21:3431–3439. [DOI] [PMC free article] [PubMed] [Google Scholar]; Findings from this study confirm the serial mediation hypothesis on which the study was based on suggesting that perceived discrimination in healthcare settings contributes to internalization of HIV-related stigma by women living with HIV, which in turn leads to depressive symptoms, with adverse effects on ART adherence.
- 23▪.Johannson A, Vorobjov S, Heimer R, et al. The role of internalized stigma in the disclosure of injecting drug use among people who inject drugs and self-report as HIV-positive in Kohtla-Järve, Estonia. AIDS Behav 2017; 21:1034–1043. [DOI] [PubMed] [Google Scholar]; The study showed that when PWID self-report as HIV-positive, they experience relatively high levels of internalized HIV and drug stigmas and also the disclosure of injecting drug use varies significantly by the disclosure target.
- 24▪.Mburu G, Ayon S, Tsai AC, et al. Who has ever loved a drug addict? It'sa lie. They think a ‘teja’is as bad person’: multiple stigmas faced by women who inject drugs in coastal Kenya. Harm Reduct J 2018; 15:29. [DOI] [PMC free article] [PubMed] [Google Scholar]; Women who inject drugs in the Kenyan coast often self-stigmatize, face stigma of injecting drug use in social contexts as well as in healthcare facilities (from providers), which results in poor access and utilization of health services, specifically harm reduction, HIV and reproductive health. These stigmas are even more aggravated among women who live with HIV.
- 25▪.Davis A, McCrimmon T, Dasgupta A, et al. Individual, social, and structural factors affecting antiretroviral therapy adherence among HIV-positive people who inject drugs in Kazakhstan. Int J Drug Policy 2018; 62:43–50. [DOI] [PMC free article] [PubMed] [Google Scholar]; Findings from this study suggest the need for interventions at individual and/or couple level, healthcare provider, healthcare system and at larger structural levels to address adherence barriers faced by PWID, which will eventually help increase viral suppression among this population, thus reducing or eliminating HIV transmission, and prevent the development of drug-resistant virus.
- 26▪.Deryabina A, El-Sadr WM. Uptake of needle and syringe program services in the Kyrgyz Republic: key barriers and facilitators. Drug Alcohol Depend 2017; 179:180–186. [DOI] [PubMed] [Google Scholar]; Social, institutional and interpersonal barriers as well as stigma and discrimination of PWID, combined with the criminalization of drug use and the requirement for official registration of drug users leads to poor uptake of NSP services in Kyrgyzstan.
- 27▪▪.Altice FL, Azbel L, Stone J, et al. The perfect storm: incarceration and the high-risk environment perpetuating transmission of HIV, hepatitis C virus, and tuberculosis in Eastern Europe and Central Asia. Lancet 2016; 388:1228–1248. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study applies the risk environment framework to describe how incarceration, HIV, hepatitis C virus, tuberculosis, and substance use disorders converge to produce drug-related harm and clarify how individual HIV risk behaviors are embedded within social processes, specifically incarceration within Eastern Europe and Central Asia (EECA).
- 28▪.Azbel L, Polonsky M, Wegman M, et al. Intersecting epidemics of HIV, HCV, and syphilis among soon-to-be released prisoners in Kyrgyzstan: implications for prevention and treatment. Int J Drug Policy 2016; 37:9–20. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study found that compared with the community, HIV was concentrated 34-fold higher in prisoners. Also a gap exists in HIV care continuum because of the high proportion of undiagnosed syphilis and HIV infections.
- 29▪.Ibragimov U, Cooper HL, Haardorfer R, et al. Stigmatization of people who inject drugs (PWID) by pharmacists in Tajikistan: sociocultural context and implications for a pharmacy-based prevention approach. Harm Reduct J 2017; 14:64. [DOI] [PMC free article] [PubMed] [Google Scholar]; The study suggests that stigma plays an important role in pharmacists’ decision-making via different pathways and usually results in refusal to provide syringes to PWID in Tajikistan. Findings also suggest that the local sociocultural context, in particular religious beliefs, collectivistic mentality and, in a broader sense, social conservatism, may facilitate stigmatizing beliefs and attitudes.
- 30▪.King EJ, Maksymenko KM, Almodovar-Diaz Y, Johnson S. ’If she is a good woman ’ and ’to be a real man ’: gender, risk and access to HIV services among key populations in Tajikistan. Culture, Health Sexuality 2016; 18:422–434. [DOI] [PubMed] [Google Scholar]; The results of this study show that there are well defined gender norms in Tajikistan, and these gender norms influence key populations’ access to HIV services.
- 31.Des Jarlais DC, Boltaev A, Feelemyer J, et al. Gender disparities in HIV infection among persons who inject drugs in Central Asia: a systematic review and meta-analysis. Drug Alcohol Depend 2013; 132 Suppl 1:S7–S12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Terlikbayeva A, Zhussupov B, Primbetova S, et al. Access to HIV counseling and testing among people who inject drugs in Central Asia: strategies for improving access and linkages to treatment and care. Drug Alcohol Depend 2013; 132 Suppl 1 0 1:S61–S64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Deryabina A. Mapping of key HIV services assessment of their quality and analysis of gaps and needs of most-at-risk populations in Chui oblast and Bishkek city Kyrgyzstan. 2011. [Google Scholar]
- 34▪▪.Michels I KB, Trautmann F, et al. Improvement of treatment of drug use disorders in Central Asia the contribution of the EU Central Asia Drug Action Programme (CADAP). J Addict Med Ther 2017; 5:1025. [Google Scholar]; The article discusses drug-related problems, health risks and the impact of externally donor-driven programs on HIV and drug use situation in Central Asian countries.
- 35.Cohn SE, Jiang H, McCutchan JA, et al. Association of ongoing drug and alcohol use with nonadherence to antiretroviral therapy and higher risk of AIDS and death: results from ACTG 362. AIDS Care 2011; 23:775–785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tucker JS, Orlando M, Burnam MA, et al. Psychosocial mediators of antiretroviral nonadherence in HIV-positive adults with substance use and mental health problems. Health Psychology 2004; 23:363–370. [DOI] [PubMed] [Google Scholar]
- 37▪.Zhang Y, Wilson TE, Adedimeji A, et al. The impact of substance use on adherence to antiretroviral therapy among HIV-infected women in the United States. AIDS Behav 2018; 22:896–908. [DOI] [PMC free article] [PubMed] [Google Scholar]; In this study conducted among HIV-infected women, substance use overall remained detrimental to ART adherence; specifically, both marijuana and other drug use predicted suboptimal adherence.
- 38▪.Corazza O, Roman-Urrestarazu A. Novel psychoactive substances: policy. Economics and drug regulation. 2017; Switzerland: Springer International Publishing [Google Scholar]; The increasing number of people, especially young people, injecting synthetic cathinones (‘bath salts’) in Kazakhstan practice risky drug preparation and use practices.
- 39▪.Deryabina A ET, Baiserkin B, Ivakin V, Killam W. Lack of effective opioid dependence and alcohol abuse treatment leads to high rates of treatment discontinuation among patients initiated on antiretroviral therapy in Kazakhstan. The 22nd International AIDS Conference (AIDS 2018) Amsterdam. 2018. [Google Scholar]; Substance abuse including injecting drugs and harmful use of alcohol were associated with treatment discontinuation among patients initiated on ART in Kazakhstan.
- 40▪▪. UNAID.S. 90–90–90 - an ambitious treatment target to help end the AIDS epidemic2014 February 2 2019. [Google Scholar]; Behind the 90-90-90 target is the idea that by 2020, 90% of all people living with HIV will know their HIV status. By 2020, 90% of all people with diagnosed HIV infection will receive sustained antiretroviral therapy. By 2020, 90% of all people receiving antiretroviral therapy will have viral suppression. Modeling suggests that achieving these targets by 2020 will enable the world to end the AIDS epidemic by 2030, which in turn will generate profound health and economic benefits.
- 41▪.Vu BN, Green KE, Thi Thu Phan H, et al. Lay provider HIV testing: a promising strategy to reach the undiagnosed key populations in Vietnam. PLoS One 2018; 13:e0210063. [DOI] [PMC free article] [PubMed] [Google Scholar]; Study finding suggest that lay provider HIV testing is effective to reach key populations and sexual partners of people living with HIV.
- 42▪.Green K. NB, Thi Thu P, Vo Hai S, M. Hung T, Vu Song H, Tran H HG, editors. Is HIV self-testing acceptable to key populations in Vietnam? Results from a cross-sectional study of men who have sex with men, female sex workers and people who inject drugs. 21st International AIDS Conference; 2016; Durban, South Africa. [Google Scholar]; The majority of key populations in the study reported intention to use HIV self-testing as well as willingness to pay for it.
- 43▪.Smyrnov P, Williams LD, Korobchuk A, et al. Risk network approaches to locating undiagnosed HIV cases in Odessa, Ukraine. J Int AIDS Soc 2018; 21:e25040.http://onlinelibrary.wiley.com/doi/10.1002/jia2.25040/full [DOI] [PMC free article] [PubMed] [Google Scholar]; Study suggests that racing risk networks can be more effective in recruiting higher proportions of undiagnosed positives than outreach-based testing or respondent-driven sampling.
- 44▪.Kan M, Garfinkel DB, Samoylova O, et al. Social network methods for HIV case-finding among people who inject drugs in Tajikistan. J Int AIDS Soc 2018; 21 Suppl 5:e25139–e25140. [DOI] [PMC free article] [PubMed] [Google Scholar]; In this study, RDS-based HIV-testing interventions resulted in higher yields and overall case-finding, especially when recruitment was restricted. However, active case finding approach identified a higher proportion of first-time testers.
- 45▪.Solomon SS, McFall AM, Lucas GM, et al. Respondent-driven sampling for identification of HIV- and HCV-infected people who inject drugs and men who have sex with men in India: a cross-sectional, community-based analysis. PLoS Med 2017; 14:e1002460. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study proved the ability of RDS to rapidly identify substantial number of individuals in key populations at nominal costs. Authors suggest combining RDS with strategies focused on linkage to care to achieve 90-90-90 targets in key populations in resource-limited settings.
- 46▪▪.Sordo L, Barrio G, Bravo MJ, et al. Mortality risk during and after opioid substitution treatment: systematic review and meta-analysis of cohort studies. BMJ 2017; 357:j1550–j1560. [DOI] [PMC free article] [PubMed] [Google Scholar]; In pooled trend analysis, all cause mortality dropped sharply over the first 4 weeks of methadone treatment and decreased gradually 2 weeks after leaving treatment. All cause and overdose mortality remained stable during induction and remaining time on buprenorphine treatment.
- 47.Lappalainen L, Nolan S, Dobrer S, et al. Dose-response relationship between methadone dose and adherence to antiretroviral therapy among HIV-positive people who use illicit opioids. Addiction 2015; 110:1330–1339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48▪.Mlunde LB, Sunguya BF, Mbwambo JK, et al. Association of opioid agonist therapy with the initiation of antiretroviral therapy - a systematic review. Int J Infect Dis 2016; 46:27–33. [DOI] [PubMed] [Google Scholar]; Mlunde et al. conducted a systematic review to examine the association of opioid agonist therapy with ART initiation among HIV-positive people who inject drugs (PWID). Overall effect size through meta-analysis shows that agonist therapy is positively associated with ART initiation among HIV-positive PWID.
- 49▪▪.Low AJ, Mburu G, Welton NJ, et al. Impact of opioid substitution therapy on antiretroviral therapy outcomes: a systematic review and meta-analysis. Clin Infect Dis 2016; 63:1094–1104. [DOI] [PMC free article] [PubMed] [Google Scholar]; In this meta-analysis, OST was associated with a 45% increase in odds of viral suppression, but there was limited evidence from six studies for OST decreasing mortality for PWID on ART.
- 50▪.Miller WC, Hoffman IF, Hanscom BS, et al. A scalable, integrated intervention to engage people who inject drugs in HIV care and medication-assisted treatment (HPTN 074): a randomised, controlled phase 3 feasibility and efficacy study. Lancet 2018; 392:747–759. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study provides evidence that a flexible, scalable intervention increases ART and MAT use and reduces mortality among PWID.
- 51.Harris KA, Arnsten JH, Litwin AH. Successful integration of hepatitis C evaluation and treatment services with methadone maintenance. J Addict Med 2010; 4:20–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Morozova O, Dvoryak S, Altice FL. Methadone treatment improves tuberculosis treatment among hospitalized opioid dependent patients in Ukraine. Int J Drug Policy 2013; 24:e91–e98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53▪.Norton BL, Beitin A, Glenn M, et al. Retention in buprenorphine treatment is associated with improved HCV care outcomes. J Subst Abuse Treat 2017; 75:38–42. [DOI] [PMC free article] [PubMed] [Google Scholar]; In this study, patients retained (vs. not retained) in buprenorphine treatment were more likely to be referred for HCV specialty care, achieve an HCV-specific evaluation, be offered HCV treatment, and initiate HCV treatment.
- 54▪.ICAP. Integrated MAT, TB and HIV service delivery program for people who inject drugs in Kazakhstan and Tajikistan. Almaty: ICAP at Columbia University; 2019. [Google Scholar]; This program evaluation assessed the effectiveness of the integrated HIV, TB and MAT service delivery model in improving access of MAT patients to HIV services. Results of this evaluation show that integrated delivery of HIV and TB services at MAT sites was feasible and highly acceptable for both the service providers and the patients in both countries. Evaluation shows significant positive effects on ART effectiveness as well as on viral load suppression.
- 55▪▪.Springer SA, Di Paola A, Barbour R, et al. Extended-release naltrexone improves viral suppression among incarcerated Persons living with HIV and alcohol use disorders transitioning to the community: results from a double-blind, placebo-controlled trial. J Acquir Immune Defic Syndr 2018; 79:92–100. [DOI] [PMC free article] [PubMed] [Google Scholar]; The study showed that XR-NTX improves or maintains viral supression after release to the community for incarcerated people living with HIV with opioid use disorders.
- 56▪▪.Springer SA, Di Paola A, Azar MM, et al. Extended-release naltrexone improves viral suppression among incarcerated persons living with HIV with opioid use disorders transitioning to the community: results of a double-blind, placebo-controlled randomized trial. J Acquir Immune Defic Syndr 2018; 78:43–53. [DOI] [PMC free article] [PubMed] [Google Scholar]; The study extends the benefits of XR-NTX as a treatment for alcohol use disorders and supports the additional benefit it has on improving HIV treatment outcomes in combination with ART in incarcerated individuals with HIV and alcohol use disorders transitioning to the community.
- 57▪.Marcus R, Makarenko I, Mazhnaya A, et al. Patient preferences and extended-release naltrexone: a new opportunity to treat opioid use disorders in Ukraine. Drug Alcohol Depend 2017; 179:213–219. [DOI] [PMC free article] [PubMed] [Google Scholar]; Researcher concluded that In the context of Eastern Europe and Central Asia where HIV is concentrated in PWID and where HIV prevention with opioid agonist therapies (OAT) is under-scaled, new options for treating opioid use disorders are urgently needed, therefore XR-NTX can become an option for addiction treatment and HIV prevention especially for PWID who have shorter duration of injection and who have negative attitudes to OAT.
- 58.MacArthur GJ, Minozzi S, Martin N, et al. Opiate substitution treatment and HIV transmission in people who inject drugs: systematic review and meta-analysis. BMJ 2012; 345:e5945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Choopanya K, Martin M, Suntharasamai P, et al. Bangkok Tenofovir Study Group. Antiretroviral prophylaxis for HIV infection in injecting drug users in Bangkok, Thailand (the Bangkok Tenofovir Study): a randomised, double-blind, placebo-controlled phase 3 trial. Lancet 2013; 381:2083–2090. [DOI] [PubMed] [Google Scholar]
- 60.Escudero DJ, Lurie MN, Kerr T, et al. HIV preexposure prophylaxis for people who inject drugs: a review of current results and an agenda for future research. J Int AIDS Soc 2014; 17:18899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61▪▪.Biello KB, Bazzi AR, Mimiaga MJ, et al. Perspectives on HIV preexposure prophylaxis (PrEP) utilization and related intervention needs among people who inject drugs. Harm Reduct J 2018; 15:55. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study described barriers to PrEP utilization. Individual-level barriers included low PrEP knowledge and limited HIV risk perception, concerns about PrEP side effects, and competing health priorities and needs because of drug use and dependence. Interpersonal-level barriers included negative experiences with healthcare providers and HIV-related stigma within social networks. Clinical barriers included poor infrastructure and capacity for PrEP delivery to PWID, and structural barriers related to homelessness, criminal justice system involvement, and lack of money or identification to get prescriptions.
- 62.Friedman SR, Smyrnov P, Bondarenko K. A new approach to prevent HIV transmission: project protect intervention for recently infected individuals AU - Vasylyeva, T.I. AIDS Care 2015; 27:223–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63▪.El-Sadr WM, Harripersaud K, Rabkin M. Reaching global HIV/AIDS goals: what got us here, won’t get us there. PLoS Med 2017; 14:e1002421. [DOI] [PMC free article] [PubMed] [Google Scholar]; In a perspective, Wafaa El-Sadr et al. discuss tailored approaches to treatment and prevention of HIV infection.
- 64.WHO. WHO, UNODC, UNAIDS technical guide for countries to set targets for universal access to HIV prevention, treatment and care for injecting drug users–2012 revision. 2012. [Google Scholar]


