Abstract
Objectives:
Unhealthy alcohol use is associated with negative health outcomes in clients attending methadone maintenance therapy (MMT) programs. However, debates exist regarding the methadone dose of drinkers, and little is known about the health outcomes of drinkers with other types of alcohol use. This study examined the drinking pattern and its association with methadone dose, and depressive and anxiety symptoms in Chinese clients undergoing MMT.
Methods:
A secondary data analysis was conducted with data from a large-scale cross-sectional survey of 549 clients of 3 MMT clinics in Wuhan, China. Depression, anxiety, and alcohol dependence were measured with Zung Self-rating Depression Scale, Zung Self-rating Anxiety Scale, and Alcohol Dependence Scale, respectively. Drinking pattern was assessed using 3 indicators: weekly amount of alcohol consumed, weekly frequency of alcohol consumed, and severity of alcohol dependence.
Results:
The prevalence of current drinking, hazardous drinking, regular drinking, and alcohol abuse/dependence was 29.0%, 10.4%, 14.2%, and 8.7%, respectively. In adjustment analyses, relative to nondrinkers, drinkers had significantly lower weight-based methadone dose (β = −0.136, P = 0.008); hazardous drinkers, irregular drinkers, and drinkers without alcohol abuse/dependence had less severe depression (β = −3.67, P = 0.004; β = −2.37, P = 0.034; β = −3.20, P = 0.001) and anxiety (β = −4.90, P < 0.001; β = −3.24, P = 0.006; β = −4.52, P < 0.001), but drinkers with alcohol abuse/dependence had more severe depression (β = 5.55, P < 0.001) and anxiety (β = 4.31, P = 0.005).
Conclusion:
In Chinese MMT clinics, drinkers may use alcohol to compensate for inadequate MMT and self-medicate negative emotions. Compared with nondrinkers, the severities of depression and anxiety were lower among drinkers without alcohol abuse/dependence, but higher among those with alcohol abuse/dependence.
Keywords: alcohol use, anxiety, depression, methadone maintenance treatment, self-medication
Alcohol consumption is a common clinical phenomenon in clients of methadone maintenance therapy (MMT) clinics across countries (Ottomanelli, 1999; Soyka, 2015; Nolan et al., 2016). Empirical studies have shown that approximately one-third of the methadone-maintained clients have some forms of alcohol use disorders according to study-defined criteria, including excessive drinking, hazardous drinking, heavy alcohol use, risky alcohol use, and alcohol abuse/dependence (el-Bassel et al., 1993; Rittmannsberger et al., 2000; Nyamathi et al., 2009; Rengade et al., 2009; Ryder et al., 2009; Chen et al., 2011). Unhealthy alcohol use has been reported to be a significant risk factor for nonadherence to MMT, increased risk of death due to overdose, difficulties in integrating into normal social life, criminal activities, relapse to illicit drugs, and physical and mental morbidity (el-Bassel et al., 1993; Ottomanelli, 1999; Rengade et al., 2009; Kreek et al., 2010; Soyka, 2015; Nolan et al., 2016). Despite extensive international studies in this area, however, the underlying causes of alcohol drinking in patients undergoing MMT remain under debate. For example, it remains unclear that whether drinking is a result of MMT and whether alcohol-drinking clients request higher doses of methadone (Ottomanelli, 1999; Srivastava et al., 2008; Soyka, 2015).
China has the world's largest single MMT program, which has been available in nearly all provinces of China until now and is currently providing services to over 160 thousand persons with opioid (mainly heroin) use disorders (Sullivan et al., 2015; Zhong et al., 2018). Although China's MMT program has substantially reduced heroin use, criminal behaviors, and heroin-related morbidity and mortality, it still has many challenges with poor adherence to MMT being a major one (Zhou and Zhuang, 2014; Sun et al., 2015). Due to the lack of training in addiction treatment and inappropriate concern for possible fatal overdose, Chinese service providers in MMT clinics (most of them are general practitioners and nurses) often prescribe a lower dosage of methadone compared with that in western countries (Lin and Detels, 2011). For example, survey data from several major Chinese cities indicate that the average doses of methadone in MMT clinics of Guangdong province and Ningbo municipality are as low as 46.1 and 37.0 mg/d, and high-dose methadone (≥60 mg/d) patients only account for 41.5% and 34.9% of the clients in MMT clinics of Chengdu and Guiyang municipalities, respectively (Chen et al., 2010; Xie et al., 2011; Fan et al., 2015; Leng et al., 2017). Because of the low rates of high-dose methadone across MMT clinics, the low dosage of methadone has been recognized as a strong risk factor for increased mortality and the early dropout from MMT in China (Bao et al., 2009; Liao et al., 2013; Zhou and Zhuang, 2014; Shen et al., 2016; Zhou et al., 2017). Further, there is also evidence that HIV-infected and HIV/hepatitis C virus-coinfected patients under opiate replacement treatment require higher methadone dose and HIV-positive MMT patients receiving lower doses of methadone are less likely to adhere to antiretroviral therapy (Lappalainen et al., 2015; Roncero et al., 2017).
In the general population, alcohol can serve a variety of functions, including ameliorating physical discomfort and negative emotions, and enhancing positive mood or well being (Kuntsche et al., 2005; Sayette, 2017). In the case of MMT clients, because these patients are still suffering from many health problems such as physical pain, depression, and anxiety (Yin et al., 2015; Yang et al., 2017), we speculate that MMT clients would be more likely to drink alcohol to self-medicate their negative emotions. This hypothesis is particularly suitable for Chinese clients receiving a low-dose MMT, due to the higher risk of uncontrolled negative emotions resulted from inadequate MMT.
Most previous studies found no significant difference in methadone doses between patients with and without unhealthy alcohol use (Rengade et al., 2009; Ryder et al., 2009; Chen et al., 2011). Nevertheless, there have been some preliminary findings showing a borderline trend towards higher methadone doses or greater increase in methadone doses in clients without than with alcohol use (P = 0.085 and P = 0.05) (Bickel and Amass, 1993; el-Bassel et al., 1993). A recently published study with a large sample of 2121 MMT participants in southwest China has reported that a low methadone dose (31–60 mg/d) was a significant predictor of heavier drinking (Duan et al., 2017). Because the majority of earlier studies employed relatively small samples of MMT clients (<200), they may have limited statistical power to detect the significant methadone dosage difference between drinkers and nondrinkers. Importantly, there is evidence that body weight is an important determinant of methadone dose (Mouly et al., 2015), but none of the existing studies control for weight when comparing methadone dosage between alcohol-using and nonalcohol-using patients (Bickel and Amass, 1993; el-Bassel et al., 1993; Rengade et al., 2009; Ryder et al., 2009; Chen et al., 2011), possibly resulting in false-negative results.
Alcohol use can be defined as a spectrum, including nondrinking, light drinking, moderate drinking, heavy drinking, abuse, and dependence (Reid et al., 1999; Rittmannsberger et al., 2000). Although significantly more depressive and anxiety symptoms in patients with than without unhealthy alcohol use and more depressive symptoms in heavy than moderate drinkers in MMT settings have been reported by 2 prior studies (el-Bassel et al., 1993; Nyamathi et al., 2012), little is known about the relationship between depression and anxiety, and other drinking types such as moderate drinking (relative to nondrinking). Findings from general population-based studies have shown that the association between depression and other psychological symptoms and drinking varied by the type of alcohol use (Graham et al., 2007; Coulson et al., 2014; Martinez et al., 2015; Salonsalmi et al., 2017). For example, Coulson et al. reported a U-shaped relationship between alcohol consumption and depression: significantly higher risk of depression in both nondrinkers and those consuming ≥3 standard drinks/d as compared with those consuming ≤2 standard drinks/d (Coulson et al., 2014). We therefore presume that the severity of depressive and anxiety symptoms of MMT clients would also vary depending on the drinking pattern.
The phenomena of drinking in MMT clients received little research attention in China. As far as we know, only one study by Duan et al. examined the characteristics of alcohol drinking of Chinese MMT clients (Duan et al., 2017). This study demonstrated a 16.6% prevalence of hazardous drinking, and several sociodemographic and clinical correlates of hazardous drinking, but did not provide data on the relationship between drinking pattern and mental health outcomes. To deepen our understanding on the alcohol use of MMT patients, the present study was set out to determine the drinking pattern and its association with methadone dose, and depressive and anxiety symptoms in Chinese clients undergoing MMT.
METHODS
Data Source and Sample
Between June, 2009 and July, 2010, we conducted a large-scale cross-sectional survey in 3 MMT clinics in Wuhan—a large metropolis with over 10 million people in central-southern China (Xu et al., 2017; Yang et al., 2017; Zhong et al., 2018). This study was a secondary data analysis based on data from it. By using cluster sampling, the study finally obtained a sample of 603 patients who were 20 years old or older, were undergoing MMT at the 3 clinics, and met Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition criteria for a life-time heroin dependence. The study collected a variety of variables and health outcomes, including sociodemographics, clinical characteristics, self-destructive behaviors, sexual life satisfaction, and poor mental health indicators. Data were collected by self-report questionnaires, supplemented by a medical record review and face-to-face interview (when necessary). The current analysis focused on a subsample of 549 patients who had undergone MMT for at least 6 months, because the methadone dose has generally been stabilized after this treatment duration. Details of this study can be found elsewhere (Xu et al., 2017; Yang et al., 2017; Zhong et al., 2018).
Before the survey, the study protocol was approved by the Ethical Review Board of Wuhan Mental Health Center. All subjects voluntarily participated in the study and provided written informed consent.
Measures
Depression and Anxiety
We used the validated Chinese Zung Self-rating Depression Scale (SDS) and Zung Self-rating Anxiety Scale (SAS) to evaluate depressive and anxiety symptoms, respectively (Wang et al., 1999). Both scales have 20 items, and all items are rated on a 4-point scale (1 = a little of the time to 4 = most of the time). Total scores of the 2 scales vary between 20 and 80, with higher total scores denoting more severe depressive and anxiety symptoms.
Weight-based Methadone Dose
Daily methadone dose and body weight at the time of the survey were obtained from medical records. Weight-based methadone dose (WMD) was calculated by dividing the prescribed methadone dose by the body weight (mg/kg/d).
Alcohol Use
Patients were asked: “Did you drink at least once per month over the past six months?” Those who drunk monthly in the past 6 months (current drinkers) were further asked to report types of alcoholic beverage (beer, wine, and white spirit), weekly frequency of drinking (<1, 1–2, 3–4, and ≥5 days), and quantity of alcohol drunk (expressed as the number of cans [250–350 mL] or bottles [330–600 mL] of beers, and the number of Chinese “Liang” [50 mL] for wines and white spirit) on a typical day of the last month.
Weekly amount of alcohol consumption in grams of pure alcohol was calculated based on types of alcoholic beverage, quantity of alcohol drunk, and weekly frequency of drinking, with the standard ethanol content being 4% for beer, 12% for wine, 38% for weak white spirits, and 53% for strong white spirits (Millwood et al., 2013). Hazardous drinking referred to a weekly amount of alcohol consumed that exceeded 196 g for men and 98 g for women, according to the threshold values recommended by the US National Institute on Alcohol Abuse and Alcoholism (Reid et al., 1999). Alcohol consumption at levels lower than threshold values for hazardous drinking was defined as moderate drinking.
Frequency of drinking was divided into 2 categories: irregular (≤4 days per week) and regular (≥5 days per week) (Lim et al., 2007).
Severity of alcohol dependence was assessed with the validated Chinese Alcohol Dependence Scale (ADS) (Skinner and Allen, 1982; Zhang, 2005). ADS is a 25-item self-rating scale, with 6 items being scored on a 2-point scale (0 and 1), 16 on a 3-point scale (0, 1, and 2), and 3 on a 4-point scale (0, 1, 2, and 3). The total ADS score ranges between 0 and 47, with a higher score representing the greater severity of dependence. A score of 9 or higher was used to indicate a current diagnosis of alcohol abuse/dependence (Zhang, 2005).
It should be noted that quite a few MMT entrants were referred patients from compulsory detoxification centers, and they were not allowed to drink alcohol in the compulsory detoxification settings before MMT. Therefore, the commonly used timeframe for defining alcohol use, “12-month” (Xu et al., 2014), was not feasible for some patients who received MMT for less than 1 year. After the pilot study, we decided to use the 6-month timeframe to define alcohol use. Due to the same reason, the 12-month timeframe of ADS was replaced with 6 months in our study.
Covariates
Sociodemographic variables collected in this study included sex, age, education, marital status, employment status, and self-rated financial status (poor, fair, and good).
Clinical factors were main route of past heroin use, length of heroin use, duration of MMT, and antisocial personality disorders (APDs). To ascertain the presence of a lifetime diagnosis of APD, patients were administered the APD module of the Chinese Mini-International Neuropsychiatric Interview (MINI) (Si et al., 2009) by our trained investigators.
Statistical Analysis
Sociodemographic and clinical characteristics of patients with and without current drinking were described and compared by t test or chi-square test, as appropriate. Multivariable linear regression analysis that entered SDS/SAS total score as the outcome variable, sociodemographic and clinical factors as control variables, and drinking pattern as the only predictor (current drinking status, amount of alcohol consumed, frequency of drinking, and severity of alcohol dependence; nondrinking as the reference category for all comparisons), was used to analyze the independent association of drinking with depressive/anxiety symptoms. The independent relationship between current drinking and WMD was examined in the same manner. All analyses were performed with SPSS, version16.0. The statistical significance level was set at P < 0.05 (2-sided).
RESULTS
The mean age of the 549 clients was 38.2 years (standard deviation [SD] 6.9, range 22–59), and 372 (67.8%) were males. The average durations of past heroin use and MMT were 10.0 years (SD: 4.0) and 25.2 months (SD: 10.4), respectively. The average methadone dose and WMD were 70.4 mg/d (SD 29.2) and 1.2 mg/kg/d (SD 0.5), respectively. In all, 210 (38.3%) patients were diagnosed with APD.
In all, 159 patients (29.0%) reported current drinking. Numbers of moderate, hazardous, irregular, and regular drinkers were 102 (18.6%), 57 (10.4%), 81 (14.8%), and 78 (14.2%), respectively. A total of 48 current drinkers (8.7%) were screened as having alcohol abuse/dependence according to ADS. The median amount of alcohol consumption per week was 94.7 g, ranging from 5 to 1184.
Table 1 shows characteristics of nondrinkers and drinkers. Compared with nondrinkers, drinkers were more likely to be men, older, married, and employed, and rate their financial status as “good,” have a longer duration of past heroin use, and suffer from APD (P ≤ 0.016). There was a marginally significant trend for the lower methadone dose in drinkers than nondrinkers (P = 0.054); interestingly, when weight was considered, a significantly lower WMD in drinkers than nondrinkers was detected (P < 0.001). In this univariate analysis, drinkers and nondrinkers differed significantly in terms of anxiety (P = 0.001), but not depression (P = 0.364).
TABLE 1.
Sociodemographic and Clinical Characteristics of Methadone-maintained Clients With and Without Current Drinking
| Nondrinkers (n = 390) | Drinkers (n = 159) | Statistics | ||
| Characteristics | n (%) | n (%) | χ2 | P |
| Male sex | 234 (60.0) | 138 (86.8) | 37.114 | <0.001 |
| Marital status of “married” | 171 (43.8) | 99 (63.2) | 15.421 | <0.001 |
| Employed | 192 (49.2) | 97 (61.0) | 5.841 | 0.016 |
| Self-rated financial status: good | 83 (21.3) | 52 (32.7) | 14.52 | 0.001 |
| A history of heroin injection | 329 (84.6) | 132 (83.0) | 0.154 | 0.695 |
| Antisocial personality disorder | 129 (33.1) | 81 (50.9) | 15.265 | <0.001 |
| Mean ± SD | Mean ± SD | t | P | |
| Age (yrs) | 37.7 ± 6.5 | 39.4 ± 7.8 | 2.602 | 0.010 |
| Education years | 9.5 ± 2.7 | 9.3 ± 2.3 | 1.058 | 0.291 |
| Duration of past heroin use (yrs) | 9.6 ± 4.0 | 10.8 ± 3.8 | 3.005 | 0.003 |
| Duration of MMT (mos) | 24.7 ± 10.3 | 26.5 ± 10.4 | 1.842 | 0.066 |
| Methadone dose (mg/d) | 71.9 ± 29.6 | 66.6 ± 28.1 | 1.931 | 0.054 |
| Weight-based methadone dose (mg/kg/d) | 1.2 ± 0.5 | 1.0 ± 0.5 | 4.251 | <0.001 |
| Zung Self-rating Depression Scale | 38.7 ± 8.2 | 38.3 ± 9.1 | 0.908 | 0.364 |
| Zung Self-rating Anxiety Scale | 45.8 ± 9.8 | 43.3 ± 9.2 | 3.211 | 0.001 |
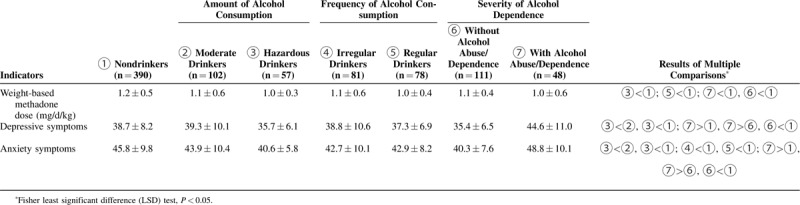
Table 2 displays the results of comparisons between subgroups according to the drinking pattern. Compared with nondrinkers, hazardous drinkers, regular drinkers, and drinkers without and with alcohol abuse/dependence, all had significantly lower WMDs; hazardous drinkers and drinkers without alcohol abuse/dependence had significantly less severe depressive symptoms, but drinkers with alcohol abuse/dependence had significantly more severe depressive symptoms; hazardous drinkers, irregular drinkers, regular drinkers, and drinkers without alcohol abuse/dependence all had significantly less severe anxiety symptoms, but drinkers with alcohol abuse/dependence had significantly more severe anxiety symptoms (P < 0.05).
TABLE 2.
Comparisons Between Drinkers With Different Types of Alcohol Use and Nondrinkers in Chinese Methadone Maintenance Treatment Clinics
After adjusting for sociodemographic and clinical covariates, relative to nondrinking, current drinking was still significantly associated with less severe anxiety symptoms (unstandardized coefficient [β] = −2.104, P = 0.012) and lower WMD (β = −0.126, P = 0.008); hazardous drinking, irregular drinking, and drinking without alcohol abuse/dependence were all significantly associated with less severe depressive (β = −3.665, P = 0.004; β = −2.365, P = 0.034; β = −3.197, P = 0.001) and anxiety (β = −4.897, P < 0.001; β = −3.243, P = 0.006; β = −4.517, P < 0.001) symptoms, but drinking with alcohol abuse/dependence was significantly associated with more severe depressive (β = 5.546, P < 0.001) and anxiety (β = 4.305, P = 0.005) symptoms (Table 3).
TABLE 3.
Independent Association Between Drinking Pattern and Weight-based Methadone Dose, and Depressive and Anxiety Symptoms, Controlling for Sociodemographic and Clinical Variables
| Weight-based Methadone Dose (mg/kg/d) | Depressive Symptoms | Anxiety Symptoms | ||||
| Drinking Pattern | Unstandardized Coefficients | P | Unstandardized Coefficients | P | Unstandardized Coefficients | P |
| Nondrinking (reference group) | 1 | 1 | 1 | |||
| Drinking | −0.128 | 0.008 | −0.739 | 0.396 | −2.104 | 0.022 |
| Moderate drinking | −0.096 | 0.093 | 0.746 | 0.448 | −0.685 | 0.502 |
| Hazardous drinking | −0.185 | 0.015 | −3.665 | 0.004 | −4.897 | <0.001 |
| Irregular drinking | −0.151 | 0.025 | −2.365 | 0.034 | −3.243 | 0.006 |
| Regular drinking | −0.106 | 0.09 | 0.809 | 0.46 | −1.023, | 0.376 |
| Drinking without alcohol abuse/dependence | −0.110 | 0.049 | −3.197 | 0.001 | −4.517 | <0.001 |
| Drinking with alcohol abuse/dependence | −0.167 | 0.041 | 5.546 | <0.001 | 4.305 | 0.005 |
DISCUSSION
To the best of our knowledge, this is the first large-scale study examining the drinking pattern and its association with methadone dose, and depressive and anxiety symptoms in Chinese MMT clients. The main findings of this study were as follows:
-
1.
Nearly one-third of the Chinese MMT patients drank alcohol, and the rates of hazardous drinking, regular drinking, and alcohol abuse/dependence were 10.4%, 14.2%, and 8.7%, respectively
-
2.
By using WMD, we were able to find the significantly lower methadone doses in drinkers than nondrinkers. Results of multiple analyses according to drinking pattern further showed that, compared with nondrinkers, the significantly lower WMDs was seen in hazardous drinkers, irregular drinkers, and drinkers without and with alcohol abuse/dependence, and marginally significantly lower WMDs were also observed in moderate and regular drinkers (P = 0.093 and P = 0.090).
-
3.
Very interestingly, corresponding to the significantly lower WMDs in hazardous drinkers, irregular drinkers, and drinkers without and with alcohol abuse/dependence, we found the significant negative associations of depressive and anxiety symptoms with hazardous drinking, irregular drinking, and drinking without alcohol abuse/dependence, despite an unexpected positive association between depressive and anxiety symptoms and alcohol abuse/dependence.
Existing research focused on pathological drinking but seldom studied the spectrum of alcohol use in MMT patients (Ottomanelli, 1999; Soyka, 2015; Nolan et al., 2016). These studies defined unhealthy alcohol use with a variety of ways, and their rate estimates varied widely: those with a cut-off value on the Alcohol Use Disorder Test or Michigan Alcohol Screening Test reported a prevalence of 20.9% to 35% (el-Bassel et al., 1993; Rengade et al., 2009; Ryder et al., 2009; Chen et al., 2011) and those with a threshold value on the amount or frequency of alcohol consumption reported a prevalence of 49.5% to 52% (Rittmannsberger et al., 2000; Nyamathi et al., 2009). Compared with these prevalence estimates, our study reported a lower prevalence of unhealthy alcohol use, in terms of all types of pathological drinking: hazardous drinking, regular drinking, and alcohol abuse/dependence. A similarly lower prevalence of hazardous drinking (16.6%) was also reported in the aforementioned Chinese study with a sample of MMT patients from southwest China (Duan et al., 2017). Hence, it seems that the Chinese MMT clients have lower prevalence of unhealthy alcohol use than western clients. This difference may be related to China's unique drug treatment policy (Yang et al., 2014), as we mentioned above, before MMT, many patients were treated in compulsory detoxification centers where they had little chance to drink; it is possible that many of them would no longer drink after entering MMT program. However, due to heterogeneity in the definition of alcohol use, timeframe for the assessment of drinking pattern, threshold values for excessive drinking, and instrument for the screening of alcohol abuse/dependence across studies, it is potentially problematic to directly compare our rates with those of previous studies.
There is convincing evidence that a low-to-moderate dose of methadone can suppress but not eliminate psychiatric symptoms, therefore a high-dose methadone is recommended for MMT clients; otherwise patients would seek other drugs such as alcohol to compensate for the inadequate MMT (Donny et al., 2002, Faggiano et al., 2003). Accordingly, the lower methadone dose in drinkers than nondrinkers was found in our study. Further, it seems that drinking alcohol works in reducing the negative emotions of MMT patients who were receiving a low dose of methadone, as partly evident by the overall negative association between current drinking and anxiety symptoms.
Psychopharmacological studies have found that both inhibitory and excitatory neurotransmitters can be affected by alcohol use. For example, it can cause the release of γ-aminobutyric acid (GABA), which acts primarily at the GABAA receptors and generates sedative effects, resulting in the relief of anxiety (Olsen and Liang, 2017). Alcohol consumption also can stimulate the release of dopamine and β-endorphins, and increase serotonin activity, which generates euphoric and antidepressive effects, leading to the mitigation of depression (Faingold et al., 1998). Both mechanisms can explain the negative associations of depressive and anxiety symptoms with hazardous drinking, irregular drinking, and drinking without alcohol abuse/dependence.
The positive association of depressive and anxiety symptoms with drinking with alcohol abuse/dependence suggests that alcohol drinking may exacerbate the negative emotions of MMT patients who had been alcohol abused/dependent. Hence, drinking seems like a failed attempt to self-medicate in MMT patients with alcohol abuse/dependence; this phenomenon is consistent with the elevated risk of comorbid depression and anxiety in patients with alcohol dependence (Gallagher et al., 2018). We consider that these patients also have the motivation to use alcohol to temporarily relieve or mask their negative feelings, but, because of the impaired emotion regulation associated with alcohol dependence (Petit et al., 2015), these patients exhibited higher level of depression and anxiety.
Much evidence has shown that the health consequence of alcohol drinking is influenced by its quantity and frequency, but the alcohol exposure–outcome relationship is not as simple as a linear relationship (Zakhari and Li, 2007; Coulson et al., 2014; Koloverou et al., 2015). In this study, we found that the beneficial effects of drinking on depressive and anxiety symptoms of MMT patients were limited to certain types of alcohol consumption. Unlike the commonly reported better mental health in moderate drinkers than nondrinkers or excessive drinkers (El-Guebaly, 2007), significantly less severe depressive and anxiety symptoms were found in hazardous drinkers in this study. Due to cross-tolerance induced by polydrug use, patients’ tolerance to alcohol would be higher than the general population. In this case, threshold values for defining excessive drinking of MMT patients would be higher than those of the general population; in other words, hazardous drinkers according to the threshold value of the general population in our study were not real hazardous drinkers (may be moderate drinkers of MMT patients). In addition, the effect of alcohol on methadone metabolism might depend on the frequency of alcohol intake, because experimental research has found the peak blood methadone concentration increases after short-term alcohol intake, but decreases after long-term alcohol intake (Nolan et al., 2016). Considering that irregular drinkers are more likely to drink alcohol intermittently, a way similar to short-term drinking, significantly less depressive and anxiety symptoms were presented in irregular drinkers.
Finally, although significant associations between some types of drinking and lower risk of depression and anxiety were found in this study, we do not intend to convey the impression or information that drinking is good for the mental health of MMT clients in certain situations. A prospective study has found that drinking to alleviate mood symptoms is a significant risk factor for the later development of alcohol dependence (Crum et al., 2013). Because the interaction between alcohol and methadone would complicate MMT, even result in fatal overdose, treating physicians in MMT clinics should advise their patients not to drink alcohol or stop drinking. Based on our clinical experiences in MMT, Chinese healthcare providers in MMT clinics seldom assess patients’ alcohol drinking habit. So a potential clinical implication of findings from the present study is that Chinese healthcare providers should be aware of the potential influence of drinking on the efficacy of MMT and take alcohol drinking pattern into consideration when determining or adjusting the methadone dose of a patient.
This study has several limitations. First, data of this study were collected cross-sectionally, not prospectively, so it may be questionable to regard drinking as a result of inadequate MMT and as a treatment for negative emotions. For example, patients may be prescribed lower doses of methadone due to their less severe depressive and anxiety symptoms. However, the elevated levels of depressive and anxiety symptoms and decreased WMDs in drinkers with alcohol abuse/dependence do not support this possibility. Therefore, the possibility of drinking as a self-medication for inadequate MMT is high. Second, our assessments on drinking pattern do not include never drinking and former drinking. It remains unclear whether the lower risk of depression and anxiety in certain types of drinkers versus non-drinkers would still exist after excluding abstainers from non-drinkers. Third, polydrug use is common among MMT patients, but we did not collect data on concomitant use of benzodiazepines and other addictive drugs. Therefore, the possible confounding effects of co-use of addictive drugs on associations between drinking and methadone dose and negative emotions could not be excluded. Cautions are needed when interpreting our results. Fourth, due to limited research funding, we did not collect data on blood methadone concentration and blood alcohol concentration, which are exact measures of current methadone dose and amount of alcohol consumed, respectively. Finally, because this was a self-report questionnaire survey and patients are generally not allowed to drink when they are receiving MMT, MMT patients may have the tendency to respond drinking pattern questions in a way that is socially acceptable: the so-called “social desirability bias”. As a result of this, frequency and amount of alcohol consumed by MMT patients may be underreported in our study.
CONCLUSIONS
In summary, nearly 1 out of every 3 Chinese MMT patients drink alcohol, and approximately 1 out of every 10 suffer from unhealthy alcohol use, indicating that alcohol use is a common issue in Chinese MMT clinics and therefore deserves clinical attention. The significantly lower WMDs in drinkers than nondrinkers and the significant association of depressive and anxiety symptoms with drinking pattern suggest that, in Chinese MMT clinics, drinkers may use alcohol to compensate for inadequate MMT and self-medicate negative emotions. However, the associations between negative emotions and alcohol use vary by drinking patterns; in particular, compared with nondrinking, drinking without alcohol abuse/dependence is significantly associated with less severe depressive and anxiety symptoms, whereas drinking with alcohol abuse/dependence is significantly associated with more severe depressive and anxiety symptoms. Further large-scale prospective studies are warranted to confirm the effects of alcohol drinking on depression and anxiety of MMT patients.
Acknowledgments
The authors thank all the patients involved in this study for their cooperation and support.
Footnotes
Funding: This study was funded by Wuhan Health and Family Planning Commission (WX17Q30, YM Xu, PI; WG16A02, BL Zhong, PI), Health and Family Planning Commission of Yunnan Province (2016NS027, JL, PI), and the Subject Leadership Training Programme for Medicine Discipline of Health and Family Planning Commission of Yunnan Province (D-2017048, JL, PI).
The authors declare no conflict of interest.
REFERENCES
- Bao YP, Liu ZM, Epstein DH, et al. A meta-analysis of retention in methadone maintenance by dose and dosing strategy. Am J Drug Alcohol Abuse 2009; 35:28–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bickel WK, Amass L. The relationship of mean daily blood alcohol levels to admission MAST, clinic absenteeism and depression in alcoholic methadone patients. Drug Alcohol Depend 1993; 32:113–118. [DOI] [PubMed] [Google Scholar]
- Chen J, Chen L, Lin L, et al. Dosage using in community methadone maintenance treatment at clinics in Guangdong and its evaluation. Modern Prev Med 2010; 37:1687–1689. [Google Scholar]
- Chen IC, Chie WC, Hwu HG, et al. Alcohol use problem among patients in methadone maintenance treatment in Taiwan. J Subst Abuse Treat 2011; 40:142–149. [DOI] [PubMed] [Google Scholar]
- Coulson CE, Williams LJ, Berk M, et al. Association between alcohol consumption and self-reported depression among elderly Australian men. Geriatric Mental Health Care 2014; 2:3–8. [Google Scholar]
- Crum RM, Mojtabai R, Lazareck S, et al. A prospective assessment of reports of drinking to self-medicate mood symptoms with the incidence and persistence of alcohol dependence. JAMA Psychiatry 2013; 70:718–726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donny EC, Walsh SL, Bigelow GE, et al. High-dose methadone produces superior opioid blockade and comparable withdrawal suppression to lower doses in opioid-dependent humans. Psychopharmacology (Berl) 2002; 161:202–212. [DOI] [PubMed] [Google Scholar]
- Duan S, Jin Z, Liu X, et al. Tobacco and alcohol use among drug users receiving methadone maintenance treatment: a cross-sectional study in a rural prefecture of Yunnan Province, Southwest China. BMJ Open 2017; 7:e014643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- el-Bassel N, Schilling RF, Turnbull JE, et al. Correlates of alcohol use among methadone patients. Alcohol Clin Exp Res 1993; 17:681–686. [DOI] [PubMed] [Google Scholar]
- El-Guebaly N. Investigating the association between moderate drinking and mental health. Ann Epidemiol 2007; 17:S55–S62. [Google Scholar]
- Faggiano F, Vigna-Taglianti F, Versino E, et al. Methadone maintenance at different dosages for opioid dependence. Cochrane Database Syst Rev 2003. CD002208. [DOI] [PubMed] [Google Scholar]
- Faingold CL, N’Gouemo P, Riaz A. Ethanol and neurotransmitter interactions: from molecular to integrative effects. Prog Neurobiol 1998; 55:509–535. [DOI] [PubMed] [Google Scholar]
- Fan J, Huang B, Ma Q, et al. Analysis of factors associated with dropout of methadone maintenance treatment in Guiyang. Chin J Dis Contr Prev 2015; 19:1215–1219. [Google Scholar]
- Gallagher C, Radmall Z, O’Gara C, et al. Anxiety and depression among patients with alcohol dependence: co-morbid or substance-related problems? Ir J Psychol Med 2018; 35:121–126. [DOI] [PubMed] [Google Scholar]
- Graham K, Massak A, Demers A, et al. Does the association between alcohol consumption and depression depend on how they are measured? Alcohol Clin Exp Res 2007; 31:78–88. [DOI] [PubMed] [Google Scholar]
- Koloverou E, Panagiotakos DB, Pitsavos C, et al. Effects of alcohol consumption and the metabolic syndrome on 10-year incidence of diabetes: the ATTICA study. Diabetes Metab 2015; 41:152–159. [DOI] [PubMed] [Google Scholar]
- Kreek MJ, Borg L, Ducat E, et al. Pharmacotherapy in the treatment of addiction: methadone. J Addict Dis 2010; 29:200–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuntsche E, Knibbe R, Gmel G, et al. Why do young people drink? A review of drinking motives. Clin Psychol Rev 2005; 25:841–861. [DOI] [PubMed] [Google Scholar]
- Lappalainen L, Nolan S, Dobrer S, et al. Dose-response relationship between methadone dose and adherence to antiretroviral therapy among HIV-positive people who use illicit opioids. Addiction 2015; 110:1330–1339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leng B, Yuan X, Wang D, et al. Evaluating the effect of methadone maintenance therapy on drug users in Chenghua district of Chengdu from 2007 to 2014. Chin Health Serv Manag 2017; 34:68–71. [Google Scholar]
- Liao DL, Chen PC, Chen CH, et al. Higher methadone doses are associated with lower mortality in patients of opioid dependence in Taiwan. J Psychiatr Res 2013; 47:1530–1534. [DOI] [PubMed] [Google Scholar]
- Lim WY, Fong CW, Chan JM, et al. Trends in alcohol consumption in Singapore 1992 2004. Alcohol Alcohol 2007; 42:354–361. [DOI] [PubMed] [Google Scholar]
- Lin C, Detels R. A qualitative study exploring the reason for low dosage of methadone prescribed in the MMT clinics in China. Drug Alcohol Depend 2011; 117:45–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez P, Neupane SP, Perlestenbakken B, et al. The association between alcohol use and depressive symptoms across socioeconomic status among 40- and 45-year-old Norwegian adults. BMC Public Health 2015; 15:1146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Millwood IY, Li L, Smith M, et al. Alcohol consumption in 0.5 million people from 10 diverse regions of China: prevalence, patterns and socio-demographic and health-related correlates. Int J Epidemiol 2013; 42:816–827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mouly S, Bloch V, Peoc’h K, et al. Methadone dose in heroin-dependent patients: role of clinical factors, comedications, genetic polymorphisms and enzyme activity. Br J Clin Pharmacol 2015; 79:967–977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nolan S, Klimas J, Wood E. Alcohol use in opioid agonist treatment. Addict Sci Clin Pract 2016; 11:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nyamathi A, Cohen A, Marfisee M, et al. Correlates of alcohol use among methadone-maintained adults. Drug Alcohol Depend 2009; 101:124–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nyamathi A, Albarran CR, Branson C, et al. Correlates of depressive symptoms among alcohol-using methadone maintained adults. Am J Addict 2012; 21 Suppl 1:S49–S55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olsen RW, Liang J. Role of GABAA receptors in alcohol use disorders suggested by chronic intermittent ethanol (CIE) rodent model. Mol Brain 2017; 10:45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ottomanelli G. Methadone patients and alcohol abuse. J Subst Abuse Treat 1999; 16:113–121. [DOI] [PubMed] [Google Scholar]
- Petit G, Luminet O, Maurage F, et al. Emotion regulation in alcohol dependence. Alcohol Clin Exp Res 2015; 39:2471–2479. [DOI] [PubMed] [Google Scholar]
- Reid MC, Fiellin DA, O’Connor PG. Hazardous and harmful alcohol consumption in primary care. Arch Intern Med 1999; 159:1681–1689. [DOI] [PubMed] [Google Scholar]
- Rengade CE, Kahn JP, Schwan R. Misuse of alcohol among methadone patients. Am J Addict 2009; 18:162–166. [DOI] [PubMed] [Google Scholar]
- Rittmannsberger H, Silberbauer C, Lehner R, et al. Alcohol consumption during methadone maintenance treatment. Eur Addict Res 2000; 6:2–7. [DOI] [PubMed] [Google Scholar]
- Roncero C, Fuster D, Palma-Alvarez RF, et al. HIV And HCV infection among opiate-dependent patients and methadone doses: the PROTEUS study. AIDS Care 2017; 29:1551–1556. [DOI] [PubMed] [Google Scholar]
- Ryder N, Cullen W, Barry J, et al. Prevalence of problem alcohol use among patients attending primary care for methadone treatment. BMC Fam Pract 2009; 10:42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salonsalmi A, Rahkonen O, Lahelma E, et al. The association between alcohol drinking and self-reported mental and physical functioning: a prospective cohort study among City of Helsinki employees. BMJ Open 2017; 7:e014368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sayette MA. The effects of alcohol on emotion in social drinkers. Behav Res Ther 2017; 88:76–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shen J, Wang M, Wang X, et al. Predictors of poor adherence to methadone maintenance treatment in Yunnan Province, China. J Addict Med 2016; 10:40–45. [DOI] [PubMed] [Google Scholar]
- Si T, Shu L, Dang W, et al. Evaluation of the reliability and validity of the Chinese version of the Mini-International Neuropsychiatric Interview in patients with mental disorders. Chin Mental Heal J 2009; 23:493–497. 503. [Google Scholar]
- Skinner HA, Allen BA. Alcohol dependence syndrome: measurement and validation. J Abnorm Psychol 1982; 91:199–209. [DOI] [PubMed] [Google Scholar]
- Soyka M. Alcohol use disorders in opioid maintenance therapy: prevalence, clinical correlates and treatment. Eur Addict Res 2015; 21:78–87. [DOI] [PubMed] [Google Scholar]
- Srivastava A, Kahan M, Ross S. The effect of methadone maintenance treatment on alcohol consumption: a systematic review. J Subst Abuse Treat 2008; 34:215–223. [DOI] [PubMed] [Google Scholar]
- Sullivan SG, Wu Z, Rou K, et al. Who uses methadone services in China? Monitoring the world's largest methadone programme. Addiction 2015; 110 Suppl 1:29–39. [DOI] [PubMed] [Google Scholar]
- Sun HM, Li XY, Chow EP, et al. Methadone maintenance treatment programme reduces criminal activity and improves social well-being of drug users in China: a systematic review and meta-analysis. BMJ Open 2015; 5:e005997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang X, CJ, Ma H. Handbook of Mental Health Rating Scales. Beijing: Chinese Mental Health Journal Press; 1999. [Google Scholar]
- Xie X, Zhuang D, Zhang Y, et al. The investigation of the methadone maintenance treatment dose in heroin addicts. Chin J Drug Abuse Prev Treat 2011; 17:314–316. [Google Scholar]
- Xu YM, Chen HH, Li F, et al. Prevalence and correlates of cigarette smoking among Chinese schizophrenia inpatients receiving antipsychotic mono-therapy. PLoS One 2014; 9:e88478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu YM, Zhong BL, Chen WC, et al. Suicidal ideation among Chinese methadone-maintained patients: prevalence and correlates. Oncotarget 2017; 8:86181–86187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang M, Zhou L, Hao W, et al. Drug policy in China: progress and challenges. Lancet 2014; 383:509. [DOI] [PubMed] [Google Scholar]
- Yang YJ, Xu YM, Chen WC, et al. Prevalence of pain and its socio-demographic and clinical correlates among heroin-dependent patients receiving methadone maintenance treatment. Sci Rep 2017; 7:8840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yin W, Pang L, Cao X, et al. Factors associated with depression and anxiety among patients attending community-based methadone maintenance treatment in China. Addiction 2015; 110 Suppl 1:51–60. [DOI] [PubMed] [Google Scholar]
- Zakhari S, Li TK. Determinants of alcohol use and abuse: Impact of quantity and frequency patterns on liver disease. Hepatology 2007; 46:2032–2039. [DOI] [PubMed] [Google Scholar]
- Zhang ZJ. Behavioral Medicine Inventory Handbook. Beijing: China Medical Electronic Audio and Video Publishing House; 2005. [Google Scholar]
- Zhong BL, Xu YM, Zhu JH, et al. Non-suicidal self-injury in Chinese heroin-dependent patients receiving methadone maintenance treatment: Prevalence and associated factors. Drug Alcohol Depend 2018; 189:161–165. [DOI] [PubMed] [Google Scholar]
- Zhou K, Zhuang G. Retention in methadone maintenance treatment in mainland China, 2004-2012: a literature review. Addict Behav 2014; 39:22–29. [DOI] [PubMed] [Google Scholar]
- Zhou K, Li H, Wei X, et al. Medication adherence in patients undergoing methadone maintenance treatment in Xi’an, China. J Addict Med 2017; 11:28–33. [DOI] [PubMed] [Google Scholar]


