Abstract
Susceptibility to many human autoimmune diseases is under strong genetic control by class II human leukocyte antigen (HLA) allele combinations. These genes remain by far the greatest risk factors in the development of type 1 diabetes and celiac disease. Despite this, little is known about HLA influences on the composition of the human gut microbiome, a potential source of environmental influence on disease. Here, using a general population cohort from the All Babies in Southeast Sweden study, we report that genetic risk for developing type 1 diabetes autoimmunity is associated with distinct changes in the gut microbiome. Both the core microbiome and beta diversity differ with HLA risk group and genotype. In addition, protective HLA haplotypes are associated with bacterial genera Intestinibacter and Romboutsia. Thus, general population cohorts are valuable in identifying potential environmental triggers or protective factors for autoimmune diseases that may otherwise be masked by strong genetic control.
Subject terms: Microbiome, Risk factors
HLA alleles and microbiome alterations have been separately associated with human autoimmunity. Here the authors identify differences in stool microbiome between healthy carriers of HLA alleles conferring low- and high-risk for type 1 diabetes, suggesting that HLA shaping of microbiome may contribute to HLA impact on autoimmunity risks.
Introduction
Type 1 diabetes mellitus (T1D) is an autoimmune disorder characterized by the destruction of insulin-producing ß-cells in the pancreas, resulting in a life-long dependence on exogenous insulin. T1D development is thought to be driven by both genetic and environmental influences, as genetic susceptibility alone is not enough to cause disease1. Environmental factors are considered to be important in triggering the onset of disease development in genetically susceptible individuals; however, identifying universal triggers remains a challenge1,2.
Genetic risk factors for T1D have been identified in over 50 diverse genetic loci but the greatest genetic determinant of T1D remains the human leukocyte antigen (HLA) region3. HLA genes are highly polymorphic, resulting in sequence variations that have been shown to be both detrimental (e.g., HLA-DR3, DQB1*0201 and HLA-DR4, DQB1*0302) and protective (e.g., HLA-DR2, DQB1*0602) with regard to T1D susceptibility4. These polymorphisms result in distinct changes to the class II major histocompatibility complex (MHC) at the amino acid level, thereby altering the structure and peptide-binding capabilities of the molecule and thus, the presentation of antigens5. HLA polymorphisms could therefore be a driving force in controlling immune responses to microbes in the gut, a proposed environmental risk factor of T1D development6.
The effect that MHC class II variation has on gut microbiome composition has been explored previously in mice6–8. For example, Kubinak et al. were able to demonstrate that the inability to present class II antigens led to distinct changes in gut microbial composition and structure, namely a decrease in Lactobacillus species and an enrichment of segmented filamentous bacteria8. More pertinently, they showed that gut microbial communities of the congenic mice were distinct based on MHC II polymorphisms that control T follicular helper cell influence on antibody response to commensal bacteria and that the effect of these polymorphisms was most potent at the mucosal interface of the gut vs. the feces8. Furthermore, results obtained by Silverman et al. showed that protection against insulitis in NOD mice transgenic for the missing MHC II Eα gene promoter led to distinct changes in the gut microbial community, and the protective effect was reliant on both the genotype and the gut community but not exclusively one or the other6. It is therefore feasible that MHC II genotype is important in not only shaping the bacterial community in the gut, but also in how the genetic and environmental components interact within the host leading to progression of or protection from autoimmune disease.
The intestinal microbiome has attracted a great deal of interest as a potential environmental component of T1D, as it is known to interact with and influence the immune system of the host9–11. Many previous and ongoing studies have aimed to identify organisms within the gut that may play a role in either the development or prevention of T1D12–15. Importantly, those efforts focused only on subjects at high genetic risk for T1D. In the Finnish Type 1 Diabetes Prediction and Prevention (DIPP) study, a high abundance of Bacteroides dorei preceded T1D autoimmunity by several months12. In the German BABYDIET study, no associations were found between anti-islet autoimmunity and bacterial diversity or composition16, while analysis of bacterial co-occurrence networks revealed an association with butyrate production in controls17. In the multinational Environmental Determinants of Diabetes in the Young (TEDDY) study, only a few weak bacterial associations with T1D autoimmunity were identified18,19.
Given that mostly weak bacterial associations with T1D autoimmunity have been observed in high T1D genetic risk cohorts, the question arose whether genetic risk alone imparts a dysbiosis of the microbiome and thus, whether any effect HLA may have on the microbiome may be masked in a high genetic risk cohort. Here, a microbiome analysis of stool samples from the ABIS general population cohort shows the effect of HLA alleles on the human gut microbiome composition. Bacterial taxa negatively and positively associated with genetic risk for type 1 diabetes are identified.
Results
Description of cohort and study design
The ABIS cohort has enrolled 17,055 newborn babies from Southeast Sweden born between 1 October 1997 and 1 October 1999. All mothers of babies born during this time period were invited to participate. This cohort serves as a large biobank of biological specimens obtained longitudinally from the enrolled children at birth, 1 year, 2–3 years, and 5–6 years of age. Collected samples types include blood, urine, stool and hair. In addition, parents of enrolled children completed questionnaires including information on duration of breastfeeding, antibiotic use, diet, etc. Many of the children enrolled also had their HLA genotype determined. The aim of the ABIS cohort, in part, is to identify the importance of environmental factors in autoimmune diseases (e.g. type 1 diabetes) and how genetic and environmental factors may interact in such diseases.
In the present study, we used high-throughput 16S rRNA sequencing to assess the microbiome of stool collected at 1 year of age from ABIS children. This time point was chosen due to the proximity in timing for development of T1D autoimmunity. Because HLA genotype data was available for only some of the children at the time of analysis, 403 individual 1-year stool samples were used. Associations between the 16S data and HLA genotype information for these children were made using multiple common statistical methods. Additionally, culturing methods were used to asses stool bacterial viability.
HLA genetic risk explains microbiome variation
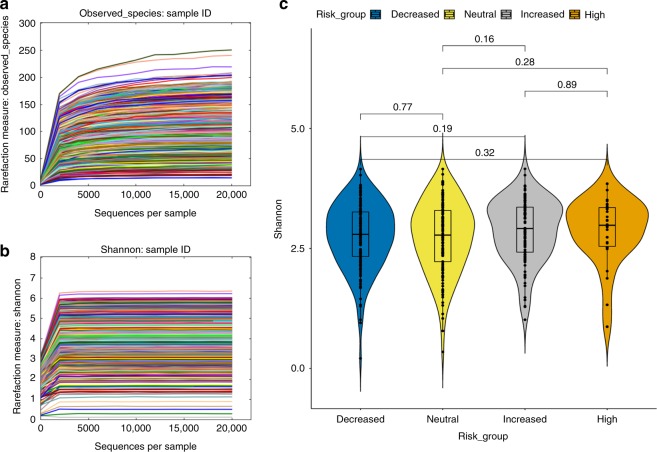
Rarefaction curves for the observed number of amplicon sequencing variants (ASVs) and the Shannon alpha diversity index show that the chosen depth of 10,000 reads per sample was sufficient to represent the diversity of unique sequences in each sample (Fig. 1a, b). Shannon diversity was not significantly different overall among the genetic risk groups (Kruskal–Wallis, p-value = 0.4906), nor through pairwise comparisons between groups (Fig. 1c). The lack of difference in diversity between risk groups suggests that HLA does not have an effect on gut bacterial diversity. Antibiotic use (yes/no) within the first year (PERMANOVA: R2 = 0.00522; F Model = 1.0526; p-value = 0.285), duration of exclusive breastfeeding (PERMANOVA: df = 10; R2 = 0.0241; F Model = 0.97047; p-value = 0.6), mode of delivery (PERMANOVA: R2 = 0.00504; F Model = 1.015, p-value = 0.395) and gender (PERMANOVA: R2 = 0.00242; F Model = 0.97412; p-value = 0.529) did not have significant effects on gut bacterial composition at 1 year of age. Also, antibiotic use within 1 month prior to sample collection (n = 30) did not significantly impact gut bacterial composition (PERMANOVA: R2 = 0.00282; F.Model = 1.1386; p-value = 0.168). Out of the total 403 subjects analyzed, 43 were still at least partially breastfed at the time of the 1-year sample collection. Gut microbiome composition was significantly impacted by breastfeeding status at the time of stool sample collection (PERMANOVA: R2 = 0.00966; F.Model = 3.92; p-value = 0.001). Because breastfeeding status at the time of sample collection could be a confounding variable, this was corrected or accounted for in all subsequent analyses.
Fig. 1.
No significant difference in microbial alpha diversity between genetic risk groups. a, b Rarefaction curves were generated based on both the number of unique amplicon sequencing variants (a) and the Shannon diversity index measure (b) for each sample. c Violin box plots and pairwise statistical comparison (Wilcoxon test) between alpha diversities among genetic risk groups. P-values for each comparison are depicted above the boxplots of the groups being compared. For statistical testing, n = 403 independent stool samples. Boxplot medians (center lines); interquartile ranges (box ranges); whisker ranges: Decreased = 2.795; 2.335–3.262; 0.210–4.155, Neutral = 2.798; 2.226–3.299; 0.345–4.156, Increased = 2.915; 2.425–3.362; 1.015–4.160, High = 2.983; 2.545–3.353; 0.871–3.851. Source data for Fig. 1c are provided in the source data file
HLA risk for T1D was able to explain significant differences in gut microbiome composition (PERMANOVA: R2 = 0.0097; F Model = 1.3088, p-value = 0.01, distance metric: binomial). Pair-wise comparisons between each group showed that all but the high vs. increased and decreased vs. neutral group comparisons were significantly different after correction for false discovery rate (FDR) (Table 1). Note that both high and increased risk groups are comprised of DR3 and/or DR4 haplotypes without protective haplotypes. Similarly, the decreased and neutral risk groups include at least one protective haplotype. Thus, similar groups in terms of haplotype makeup and risk do not significantly differ in gut bacterial composition. Additionally, the R2 values of these comparisons show a gradient trend in the amount of variation explained by risk groups at opposite ends of the risk spectrum. For example, the greatest amount of variation is explained between the high and decreased risk groups (R2 = 0.00923), followed by the high and neutral risk groups (R2 = 0.00824), then the high and increased risk groups (R2 = 0.00805). Because HLA risk explains little of the variation in the model, this suggests that the effect HLA has on the gut microbiome is modest and likely specific toward certain taxa. Also, comparisons between the highest risk subjects consistently explained the most amount of variation. This suggests that the risk-associated haplotypes together are more strongly driving compositional changes within the gut, whereas those without risk haplotypes or with at least one protective haplotype tend to be more similar in bacterial gut composition.
Table 1.
Risk groups that are significantly different by PERMANOVA
| Df | SumsOfSqs | MeanSqs | F Model | R 2 | P value | P adjusted | Significance | |
|---|---|---|---|---|---|---|---|---|
| Binomial | ||||||||
| Risk_group | 3 | 20755 | 6918.4 | 1.3088 | 0.0097 | 0.01 | – | * |
| High vs. Decreased | – | – | – | 1.5698 | 0.00923 | 0.005 | 0.017 | * |
| High vs. Increased | – | – | – | 1.0236 | 0.00805 | 0.383 | 0.402 | |
| High vs. Neutral | – | – | – | 1.354 | 0.00824 | 0.035 | 0.042 | * |
| Increased vs. Decreased | – | – | – | 1.3248 | 0.00554 | 0.035 | 0.038 | * |
| Increased vs. Neutral | – | – | – | 1.5178 | 0.00649 | 0.004 | 0.011 | * |
| Decreased vs. Neutral | – | – | – | 1.0601 | 0.00385 | 0.304 | 0.311 | |
| Bray–Curtis | ||||||||
| Risk_group | 3 | 1.169 | 0.38973 | 1.0445 | 0.00757 | 0.43 | – | |
| High vs. Decreased | – | – | – | 1.1425 | 0.00657 | 0.204 | 0.225 | |
| High vs. Increased | – | – | – | 0.6467 | 0.00499 | 0.964 | 0.973 | |
| High vs. Neutral | – | – | – | 0.9827 | 0.00583 | 0.46 | 0.467 | |
| Increased vs. Decreased | – | – | – | 1.3912 | 0.00569 | 0.066 | 0.077 | |
| Increased vs. Neutral | – | – | – | 0.9212 | 0.00385 | 0.56 | 0.587 | |
| Decreased vs. Neutral | – | – | – | 1.0117 | 0.00358 | 0.398 | 0.423 | |
| Jaccard (binary) | ||||||||
| Risk_group | 3 | 1.372 | 0.45718 | 1.2257 | 0.00893 | 0.007 | – | * |
| High vs. Decreased | – | – | – | 1.4114 | 0.00816 | 0.003 | 0.011 | * |
| High vs. Increased | – | – | – | 1.0449 | 0.00806 | 0.271 | 0.286 | |
| High vs. Neutral | – | – | – | 1.3679 | 0.00816 | 0.012 | 0.016 | * |
| Increased vs. Decreased | – | – | – | 1.2179 | 0.00501 | 0.041 | 0.047 | * |
| Increased vs. Neutral | – | – | – | 1.3952 | 0.00586 | 0.002 | 0.008 | * |
| Decreased vs. Neutral | – | – | – | 0.9719 | 0.00346 | 0.551 | 0.555 | |
PERMANOVA results after testing for significant differences in inter-subject distances using three metrics: Binomial, Bray–Curtis and Jaccard (n = 403 individual stool samples). Breastfeeding status at the time of sample collection was corrected for in the PERMANOVA model design. SumsOfSqs and MeanSqs refer to Sums of Squares and Mean Squares, respectively
The PERMANOVA test is dependent upon distances of dissimilarity between samples. Previous work has shown that the choice of distance metric can have a drastic effect on the test result20. This is because different metrics test different hypotheses. Here the binomial distance measure was used as an improved alternative to the Bray–Curtis index. Other commonly used metrics applied to 16S rRNA amplicon data include Bray–Curtis and Jaccard. Bray–Curtis is considered quantitative, because it is mainly sensitive to highly abundant species, whereas Jaccard is qualitative and considers the overlap of community members regardless of their relative abundances. The binomial distance metric is also quantitative but, unlike Bray–Curtis, includes joint absences, allowing pairs of samples missing the same ASV to appear more similar21. Differences in gut communities between risk groups were not significant using the Bray–Curtis distance (PERMANOVA: R2 = 0.00757; F Model = 1.0445; p-value = 0.43), but significant differences were observed with the Jaccard distance (PERMANOVA: R2 = 0.00893, F Model = 1.2257, p-value = 0.007). This suggests that the abundance of the bacterial ASVs observed may not be significantly influenced by HLA genetics. However, the presence or absence of certain bacteria are likely influenced by HLA as differences in community member overlap varies significantly by genetic risk.
An assumption of the PERMANOVA test is that all groups compared have similar variance (homogeneity of variance assumption), particularly in cases of uneven sampling between groups22. Beta dispersion was calculated based on genetic risk category adjusted for sampling bias, and an ANOVA was applied to test whether the average distance to the median variance was significantly different between groups. The result of the ANOVA showed that average distance to the median variance between groups was not significantly different (F value = 0.3928; p-value = 0.7583). Also, a Tukey HSD test showed that pair-wise tests of the variance assumption are not significant. Therefore, significance testing through PERMANOVA is not expected to be influenced by uneven dispersion among groups.
Amplicon sequence variants associate with HLA genetic risk
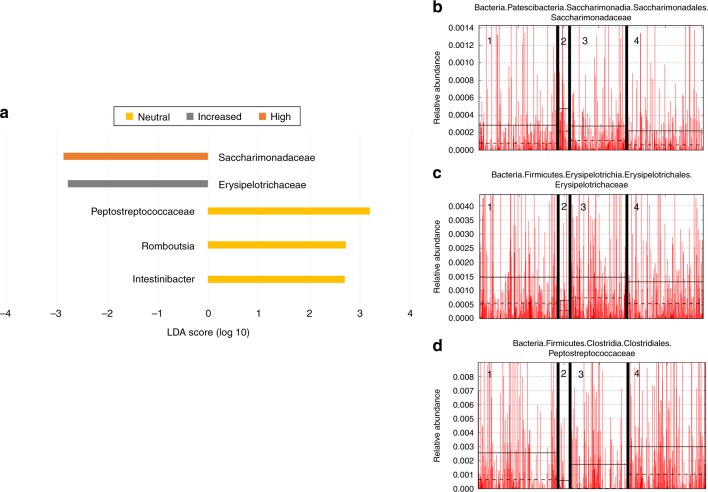
Because there are significant differences in microbiome composition between genetic risk groups, bacteria associated with genetic risk across the entire dataset were identified. Using Linear discriminant analysis Effect Size (LEfSe) after grouping ASVs at the genus level, significant associations between high risk subjects and members of the Saccharimonadaceae family were identified (Fig. 2a, b). Additionally, the family Erysipelotrichaceae was associated with subjects at increased genetic risk (Fig. 2a, c). Interestingly, two genera of the family Peptostreptococcaceae, specifically Intestinibacter and Romboutsia, were associated with neutral risk HLA (Fig. 2a, d). Differential feature plots show that the taxa described above have higher average relative abundance in their associated risk group than any other group (Fig. 2b–d). Overall, taxa found to be associated with a particular risk group through LEfSe had higher average relative abundance in their associated risk group. Because subjects at neutral risk often have either DR3 or DR4 plus at least one protective haplotype, the protective haplotypes may be important for this association, though no associations with the decreased risk group were observed in the entire dataset level with LEfSe.
Fig. 2.
Specific taxa are associated with genetic risk. a LEfSe biomarker discovery results for the entire dataset (n = 403 individual stool samples). Significant taxa are displayed according to their associated risk group and their differential log10 LDA score. b–d Differential features identified by LEfSe have higher average relative abundance with their associated risk group. b Saccharimonadaceae, c Erysipelotrichaceae, d Peptostreptococceae, (1) Decreased risk, (2) High risk, (3) Increased risk, (4) Neutral risk. Breastfeeding status at the time of sample collection was corrected for in the LEfSe model design. Source data are provided in the source data file
DESeq2 was used to find ASVs associated with genetic risk through pair-wise comparisons (Table 2). Again, Intestinibacter and Romboutsia were found to be associated with neutral risk compared with the high-risk group. Comparing the high (DR3/DR4 only) vs. decreased risk groups revealed that Intestinibacter and Romboutsia were also associated with decreased risk. This suggests that DR3 and DR4 together have a greater impact on the association of these ASVs than either haplotype alone (as in the increased risk group), and that the presence of protective haplotypes may also be important for their presence and/or abundance. Also, when comparing the increased vs. neutral groups, Bifidobacterium was associated with neutral risk with a relatively high base mean compared to other associated ASVs found by DESeq2, suggesting this ASV was more abundant across all samples compared to other identified significant ASVs. Even though Escherichia/Shigella members were shared within both the neutral and increased risk groups, they represent unique ASVs and therefore, have the potential to be unique strains. Klebisella and Veillonella ASVs were consistently associated with high risk (DR3/4) (Table 2).
Table 2.
DESeq2 supports LEfSe results at the ASV level
| Pair-wise | base mean | Log2 fold change | lfcSE | stat | p value | p adjusted | Genus |
|---|---|---|---|---|---|---|---|
| High | 33.90 | 11.12 | 2.85 | 3.90 | 9.74E-05 | 0.0093 | Klebsiella |
| 16.16 | 23.66 | 5.92 | 4.00 | 9.74E-05 | 0.0067 | Veillonella* | |
| 2.59 | 23.04 | 5.92 | 3.89 | 9.93E-05 | 0.009345 | Veillonella* | |
| Decreased | 68.40 | −2.89 | 0.84 | −3.45 | 0.0005576 | 0.03653 | Romboutsia |
| 40.17 | −4.74 | 1.24 | −3.83 | 0.000128 | 0.011178 | Enterococcus | |
| 36.80 | −3.37 | 0.75 | −4.49 | 7.13E-06 | 0.001006 | Intestinibacter | |
| High | 91.95 | 19.79 | 5.84 | 3.39 | 0.0007063 | 0.023203 | Veillonella* |
| 33.90 | 9.69 | 2.87 | 3.37 | 0.0007523 | 0.024312 | Klebsiella | |
| 16.16 | 35.34 | 5.97 | 5.92 | 3.14E-09 | 5.95E-07 | Veillonella* | |
| Neutral | 68.40 | −2.88 | 0.84 | −3.40 | 0.0006627 | 0.021951 | Romboutsia |
| 40.17 | –4.42 | 1.25 | −3.55 | 0.0003914 | 0.013917 | Enteroccocus | |
| 36.80 | −3.86 | 0.76 | −5.10 | 3.43E-07 | 4.40E-05 | Intestinibacter | |
| High | 91.95 | 23.27 | 5.98 | 3.89 | 9.97E-05 | 0.003386 | Veillonella |
| 33.90 | 11.17 | 2.94 | 3.79 | 0.0001484 | 0.00458 | Klebsiella | |
| 17.77 | 13.94 | 4.43 | 3.15 | 0.0016554 | 0.035626 | Phascolarctobacterium | |
| Increased | 40.17 | −4.61 | 1.27 | −3.62 | 0.0002916 | 0.007681 | Enterococcus |
| 20.27 | −2.43 | 0.64 | −3.81 | 0.0001388 | 0.004329 | Lachnoclostridium | |
| 17.55 | −2.33 | 0.63 | −3.72 | 0.0002009 | 0.005902 | Erysipelatoclostridium | |
| Increased | 9.15 | 30.00 | 3.85 | 7.78 | 7.03E-15 | 3.26E-12 | Escherichia/Shigella* |
| 6.86 | 16.40 | 3.86 | 4.25 | 2.10E-05 | 0.000638 | Escherichia/Shigella* | |
| 5.84 | 9.63 | 2.42 | 3.98 | 6.90E-05 | 0.002038 | Bacteroides | |
| Decreased | 19.75 | −19.63 | 3.86 | −5.09 | 3.53E-07 | 2.00E-05 | Veillonella |
| 13.36 | −29.79 | 3.86 | −7.72 | 1.12E-14 | 4.15E-12 | Megasphaera | |
| 6.97 | −6.55 | 1.70 | −3.85 | 0.0001173 | 0.003287 | Klebsiella | |
| Increased | 14.13 | 7.69 | 1.71 | 4.49 | 6.96E-06 | 0.000299 | Citrobacter |
| 5.84 | 10.89 | 2.44 | 4.47 | 8.00E-06 | 0.00034 | Bacteroides | |
| 3.06 | 27.04 | 3.89 | 6.95 | 3.61E-12 | 3.02E-10 | Escherichia/Shigella | |
| Neutral | 267.32 | −2.30 | 0.68 | −3.39 | 0.0007071 | 0.026723 | Bifidobacterium |
| 19.75 | −16.58 | 3.89 | −4.26 | 2.01E-05 | 0.000822 | Veillonella | |
| 6.97 | −7.24 | 1.71 | −4.23 | 2.38E-05 | 0.000964 | Klebsiella | |
| Neutral | 9.15 | 18.37 | 3.56 | 5.16 | 2.48E-07 | 3.18E-05 | Escherichia/Shigella* |
| 6.86 | 15.09 | 3.56 | 4.24 | 2.24E-05 | 0.001983 | Escherichia/Shigella* | |
| 5.81 | 14.73 | 3.56 | 4.14 | 3.50E-05 | 0.002961 | Anaeroglobus | |
| Decreased | 13.36 | −28.66 | 3.56 | −8.05 | 8.41E-16 | 8.83E-13 | Megasphaera |
| 6.20 | −12.57 | 3.56 | −3.53 | 0.0004112 | 0.02818 | Sarcina | |
| 2.59 | −27.94 | 3.56 | −7.84 | 4.33E-15 | 3.45E-12 | Veillonella |
The top three ASVs by base mean from each group in the pair-wise comparison are listed and described taxonomically at the genus level (n = 403 individual stool samples). Genera indicated with an asterisk (*) represent bacteria shared at the taxonomic level but are actually unique sequences. Breastfeeding status at the time of sample collection was corrected for in the DESeq2 model design. Source data are provided in the source data file
DESeq2 was also able to identify bacterial ASVs associated with particular HLA genotypes or haplotypes (e.g., heterozygous DR3/DR4, or genotypes positive for DR3 or DR4 without protective haplotypes). Intestinibacter and Romboutsia were associated with the DR3 positive increased risk genotype over the DR3/DR4 group. However, neither ASV was associated when comparing DR4 positive with DR3 positive increased risk genotypes, suggesting that the high-risk heterozygous genotype may be exerting a selective pressure against these bacteria. Interestingly, when comparing genotypes where DR3 or DR4 positive haplotype is associated with a protective haplotype, these two ASVs are associated with the absence of DR3 and at the same time, are also not associated with DR4. Because different haplotype combinations will lead to varying degrees of antigen-binding affinity, associations between HLA genotype and bacteria within the gut are likely to be genotype-specific. This is evident in that either having or lacking a protective haplotype in combination with DR3 associates with a different group of gut flora.
Prevalence analysis reveals trends by limiting noise
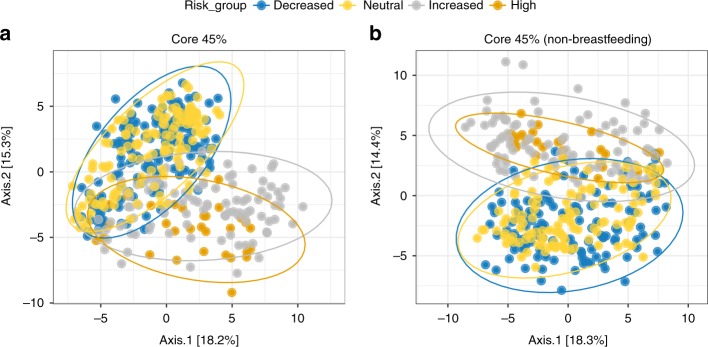
Amplicon 16S data is sparse and therefore populated with numerous low or zero counts for ASVs that are rarely seen. These rare taxa could be considered noise, as they may not be relevant to the biological question because they appear in very few subjects. To limit this noise, we filtered these data using a method that considers ASV prevalence. ASVs were filtered at 5% increments for the entire dataset (Table 3). A prevalence cutoff of 45% was chosen to assess those ASVs which were present in nearly half of all individuals analyzed. Higher prevalence cutoffs, up to 75%, could be obtained for the full dataset at the cost of additional ASVs. This filtering resulted in clear separation by PCoA between genetic risk groups that could not be observed from the raw dataset, where more distinct clusters form between ASVs prevalent in 45% of each risk group (Fig. 3), regardless of whether those samples from participants still breastfeeding at the time of sample collection were included (Fig. 3a) or not (Fig. 3b). In other words, those ASVs that are present more frequently (in at least 45% of subjects in this dataset) make up distinct patterns of composition depending on HLA-driven genetic risk for T1D.
Table 3.
Prevalence filtering focuses analysis on most shared ASVs
| Prevalence cutoff (%) | Out of bag error rate | ASV count | Number of sequences |
|---|---|---|---|
| 0 | 0.691 | 4450 | 7610000 |
| 5 | 0.45544554 | 532 | 3572138 |
| 10 | 0.18316832 | 262 | 3274985 |
| 15 | 0.19306931 | 183 | 3091195 |
| 20 | 0.13861386 | 138 | 2842684 |
| 25 | 0.10148515 | 107 | 2588149 |
| 30 | 0.10148515 | 85 | 2351261 |
| 35 | 0.09158416 | 70 | 2110874 |
| 40 | 0.07920792 | 49 | 1808389 |
| 45 | 0.0470297 | 40 | 1499585 |
| 50 | 0.13366337 | 28 | 1242599 |
| 55 | 0.25742574 | 23 | 1196297 |
| 60 | 0.16584158 | 16 | 1087380 |
| 65 | 0.13613861 | 13 | 1010804 |
| 70 | 0.34405941 | 8 | 930300 |
| 75 | 0.14108911 | 7 | 860687 |
Results of calculating prevalence levels for the entire dataset (n = 403 individual stool samples) in 5% increments. A prevalence cutoff of 45% was chosen to focus on the most commonly shared set of 40 ASV sequences
Fig. 3.
Prevalence uncovers unique clusters among the most shared ASVs by risk. a, b PCoA depicting inter-subject distances based on the binomial metric at 45% prevalence, both including participants breastfed at sample collection (a) and without participants breastfed at sample collection (b). Ellipses for each risk group are calculated based on a 95% confidence for each group
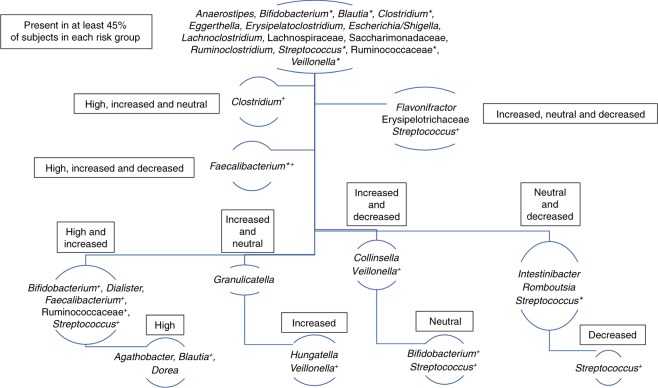
Considering only those ASVs that are present in at least 45% of subjects in each risk group, 40 unique ASVs remain from the total 4450 ASVs in the raw dataset. Of the 40 total ASVs, 14 are prevalent among all risk groups, yet the other 16 are shared among 2 or 3 groups, while others still are unique to only one group (Fig. 4). Though, at the genus level, some taxa are shared, these organisms are represented by unique sequences and should therefore be considered unique organisms. In support of the differential abundance results, ASVs that are members of Intestinibacter and Romboutsia are most prevalent in the neutral and decreased HLA-risk groups. This provides further evidence that protective HLA haplotypes may be important for shaping the composition of bacteria in the human gut. Interestingly, an ASV belonging to the Bifidobacterium genus was prevalent among all risk groups. However, another Bifidobacterium ASV was prevalent just among high and increased risk subjects, while yet another was unique to just those at neutral risk. This highlights the importance of pairing ASV-level sequence resolution with prevalence, since the distinction among these unique sequences would be overshadowed by rare sequences and overlooked at the taxonomic rather than the single nucleotide variant level.
Fig. 4.
Highly prevalent ASVs are either shared or unique to HLA groups. Hierarchy organization map displaying those taxa that are present in at least 45% of subjects in one or more risk groups. Taxa indicated with an asterisk (*) are represented by more than one ASV which are considered unique. Furthermore, those taxa indicated with a cross (+) represent bacteria shared at the taxonomic level but are actually unique to one or a combination of groups at the ASV level
Geographical clustering identifies bacterial hotspots
Geography explains a significant amount of variation between subjects’ gut microbiomes in ABIS (PERMANOVA: R2 = 0.03651; F Model = 1.3503; p-value = 0.001). Differences in geography can include underlying covariates such as diet and other lifestyle factors, and the effects of these factors can be exacerbated with increasing geographical distance23. Although the ABIS cohort benefits from geography confined to southeast Sweden, the significant impact that geographical factors have on subjects’ gut microbiomes is still evident through PERMANOVA. To limit this impact, towns were divided into three distinct clusters: the northeastern region (Linköping and Norrköping), the central region (Jönköping, Nässjö, Gislaved and Värnamo), and the southern region (Kalmar and Karlskrona). The towns within these regions were chosen for clustering based on their geographical proximity and because they provide the largest number of samples in the dataset, including many of those from high-risk subjects.
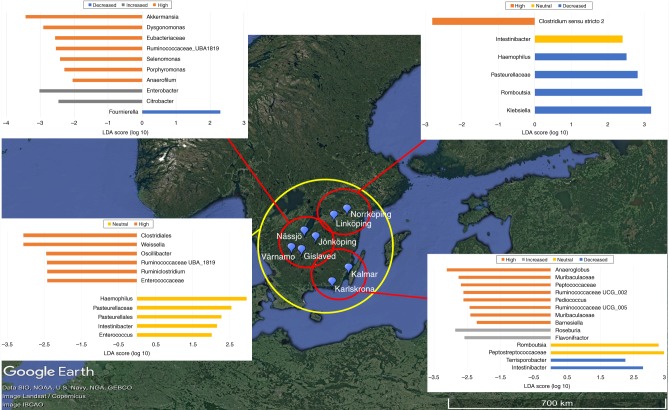
This geographical clustering, paired with differential abundance and prevalence analysis, allowed us to determine at which sites associations within the entire dataset were likely to have originated. LEfSe was again able to identify taxa associated with genetic risk at each cluster and overall among the clusters (Fig. 5). The LEfSe results show that among all clusters, Intestinibacter remains associated with neutral risk. Furthermore, this association was identified in the northeastern region while Romboutsia was associated with decreased risk in this region. In the southern region, Romboutsia was associated with neutral risk while Intestinibacter was associated with decreased risk. DESeq2 results also confirm that ASVs belonging to Intestinibacter and Romboutsia were associated with neutral and decreased HLA groups in the northeastern and southern regions.
Fig. 5.
LEfSe identifies sources of ASVs by geographical region. Linear discriminant analysis Effect Size (LEfSe) is able to identify taxa as biomarkers associated with genetic risk groups in the three geographical regions and among all three regions. Northeastern region n = 140 individual stool samples, Southern region n = 65 individual stool samples, Central region n = 160 individual stool samples. Map data © 2019 Google, SIO, NOAA, U.S. Navy, NGA, GEBCO. Image © 2019 Landsat/Copernicus. Source data are provided in the source data file
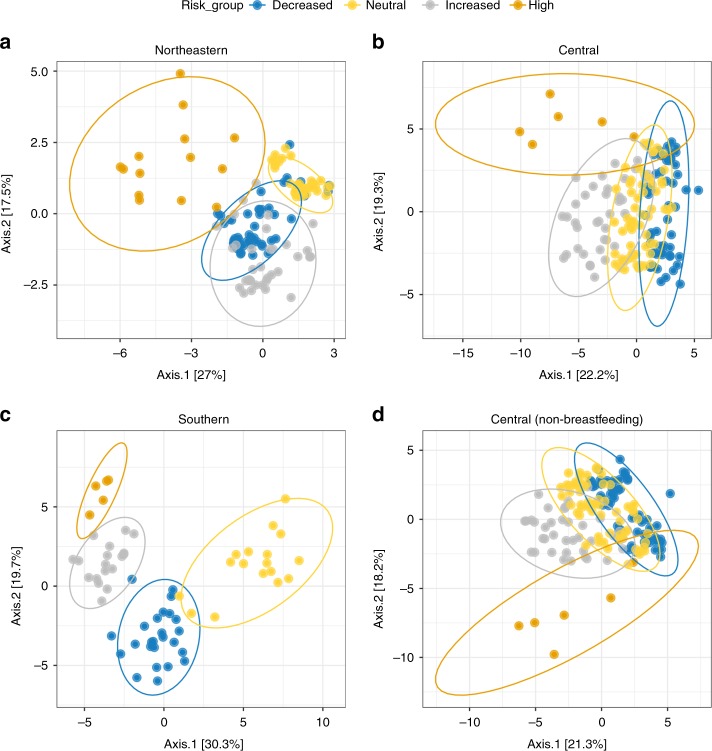
Prevalence filtering was also applied to each geographical region separately by the same prevalence level used for the entire dataset (45%). The prevalence filtered regions show distinct patterns of separation by HLA risk group through PCoA (Fig. 6). Variation among the most prevalent ASVs by risk group is most considerable in the Southern region, though overlap with these ASVs can be seen between the high/increased and decreased/neutral risk groups, respectively. In the Northeastern region, overlap between gut bacterial communities is more consistent across all risk groups. Meanwhile, in the Central region, a high degree of overlap exists between all risk groups aside from the highest risk, which are substantially separated, indicating that the variation in community overlap among the most prevalent bacteria in this risk group is strong, regardless of breastfeeding status (Fig. 6d). In other words, each genetic risk group comprises a distinct combination of ASVs that are present in most of the participants at each risk level. This would suggest that the ASVs forming these highly prevalent clusters are those most influenced by host HLA genotype, posing a potential mechanism of selection toward those bacteria in the gut.
Fig. 6.
Prevalent ASV clusters vary by HLA genotype across geography. a–d PCoA of inter-subject binomial distances for each of the three geographical clusters after applying 45% prevalence filter: a the Northeastern, b the Central, and c the Southern region. d Central region 45% prevalence after removal of samples from participants still breastfed at the time of sample collection. Ellipses are calculated based on a 95% confidence for each group
Bifidobacteria viable after storage at −80 °C for 19 years
Sample integrity is an important consideration when working with samples that have been stored for decades. Here, we assessed the viability of −80 °C frozen stool samples through isolation of non-spore forming, facultative anaerobic strains of Bifidobacterium. Members of the Bifidobacterium genus are considered relatively sensitive to long-term storage conditions, since they are non-spore forming and are sensitive to oxygen exposure. Nevertheless, strains of two Bifidobacterium species, B. breve and B. longum, were isolated from a stool sample stored at −80 °C for 19 years using media selective for the genus.
Discussion
HLA gene alleles appear to have a significant effect on the bacterial composition of the late infant gut based on our findings from children in the ABIS cohort. This effect is important because of the many implications with how genetic pre-disposition to autoimmune disorders might determine environmental factors, such as the microbiome, that ultimately may lead to disease progression. In the case of T1D, this is the first time to our knowledge that HLA genetic risk for developing autoimmunity has been associated with distinct changes in the gut microbiome in a general population human cohort. Beyond just genetic risk for T1D, our results implicate specific HLA genotypes with distinct changes in members of the gut community, which highlights an important understanding of the interaction and influence of host genetics on the human microbiome. How HLA genetics might lead to environmental triggers for autoimmune disease originating in the gut deserves further investigation on many fronts.
The greatest advantage to the ABIS cohort is its general population design. Because the general population is sampled and not just those at high genetic risk for T1D, HLA associations with the gut microbiome can be tested across a spectrum of genotypes. High genetic risk for autoimmunity likely obscures potential effects from the environment that can be identified by inclusion of all genetic types as we see with ABIS. Additionally, geography is known to be a potent source of variation between subjects13. Like the DIPP cohort in Finland, ABIS benefits from a relatively confined geographic sampling design restricted to southeast Sweden12. Unlike other studies which have historically relied on operational taxonomic unit (otu) clustering analysis, this work has benefited from higher sequence resolution through the use of ASVs24. At the ASV level, sequences may share the same taxonomy at the genus or species levels while being distinct at the sequence level. This implies that bacteria of the same name may actually be functionally distinct within or between subject groups and should be treated as such. In addition, taking into account the prevalence of each ASV within risk groups has allowed us to identify potentially important bacteria in the gut that would have been overlooked by examining an entire dataset with all its noise.
Recent findings from the TEDDY study show that development of insulin autoantibodies (IAA)-only is associated with DR3/4 and DR4/4 HLA genotypes around 1 year of age, while development of glutamic acid decarboxylase autoantibodies (GADA)-only is associated with DR3/325. In addition, previous work in Finland has shown that insulinoma associated antigen-2 autoantibodies (IA-2A)-only is associated with (DR4)-DQA1*03-DQB1*030226. This would suggest that the development of autoimmunity is directly impacted by host HLA genetics. However, the results presented here also implicate HLA with specific changes in gut bacterial composition relative to DR3/4 heterozygosity and genotypes positive for either DR3 or DR4. Therefore, the question persists whether the association between HLA and the route of autoimmunity is primarily genetic or is caused by secondary changes in the bacterial gut environment that are mediated by genetic risk. Nevertheless, these findings contribute to our understanding of the interaction between environmental exposures in the gut and host genetics in disease development.
Both differential abundance and prevalence analysis indicate that two members of the family Peptostreptococcaceae, Intestinibacter and Romboutsia, are consistently associated with lower genetic risk HLA genotypes compared to DR3/DR4. Not only does this hint at a potential for conserved functions, which may be beneficial in preventing T1D, but also the possibility of a conserved bacterial antigen recognized by higher risk genotypes that leads to the depletion of these taxa in the gut. This selection would be afforded by polymorphisms in the antigen-binding groove of the class II MHC molecule that will ultimately alter the binding affinity of the MHC molecule toward a subset of bacterial antigens. Effects of MHC polymorphism on the binding of bacterial superantigens or toxins, non-processed molecules binding to non-conventional binding sites of MHC and TCR molecules, has also been observed5. Many studies have implicated class II MHC genetics in the shaping of the gut microbiome6–8,27. However, this work was done using animal models including mainly transgenic mice. Thus, the results presented here show that HLA genotype is linked to unique changes in the human gut microbiome in a general population cohort.
Members of the order Clostridiales have recently undergone reclassification in the light of phenotypic and phylogenetic data28. Intestinibacter bartlettii, formerly Clostridium bartlettii, was reclassified at the same time the genus Romboutsia was described (with the isolation of Romboutsia ilealis)29,30. I. bartlettii is the only species currently in the Intestinibacter genus after its reclassification from Clostridium and is yet to be represented by a single complete genome sequence in a public database. Little has been described about Intestinibacter spp. other than a decreased abundance associated with administration of metformin (a type 2 diabetes (T2D) drug) and a negative correlation with insulin resistance in T2D31,32. The association of Intestinibacter with lower genetic risk for autoimmunity requires further work to understand what role these organisms play in the gut and how they may be selected against by high-risk HLA.
Probiotics have great potential as a means to modulate changes in the host microbiome to prevent or ameliorate a number of different diseases including T1D autoimmunity. Both mouse and rat models have implicated lactic acid bacteria (e.g. Lactobacillus spp.) as potential probiotics for the prevention of T1D33,34. Administration of a multi-species probiotic (including Lactobacilli) has been shown to be beneficial in treating acute pancreatitis in a rat model by reducing both bacterial translocation to the pancreas and bacterial overgrowth of potential pathogens in the duodenum35,36. Probiotic administration was associated with an increase in abundance of a new bacterial phylotype referred to as CRIB (commensal rat ileum bacterium) which was later described as Romboutsia ilealis30,37. The increased abundance of R. ilealis was also associated with lower plasma levels of pro-inflammatory cytokines37. As the authors speculate, it is possible that the administration of the probiotic mixture worked indirectly by stimulating the growth of R. ilealis in the ileum. A study conducted in mice demonstrated that colonization with certain Clostridia led to decreased mucosal erosion and increased IL-10 producing regulatory T cell accumulation in the colon. These functions within the host could be important in preventing the development of autoimmunity. The role Romboutsia plays in mediating these effects is unknown.
The effects HLA genetics have on shaping the host microbiome could be important for other autoimmune diseases besides T1D where HLA is the main genetic component. Like T1D, much of the genetic risk for developing celiac disease autoimmunity (CDA) is conferred by the class II HLA region38. Similarly, environmental influences are thought to be important as not all those who are genetically susceptible develop the disease upon exposure to dietary gluten, the main trigger of CDA. Unlike T1D, the greatest genetic risk for developing CDA is attributable to the (DR3)-DQA1*05-DQB1*02 haplotype39. Because the level of genetic risk for CDA and T1D differ by HLA genotype, in addition to differences in the localization of the pathology (small intestine in CDA vs. pancreas in T1D), the etiology of the two diseases likely vary. Still, shaping of the host intestinal microbiome through an HLA mechanism could play an important role in not just T1D but in CDA and other autoimmune disorders.
The association between HLA risk alleles for T1D and the gut microbiome is shown here using a general population cohort from southeastern Sweden. Three methods were used to consistently identify specific bacterial taxa and 16S rRNA sequences (ASVs) associated with genetic risk. These results have implications that go far beyond the gut microbiome. They suggest that HLA alleles can shape the subject’s ability to interact with the environment. Thus, HLA risk alleles can mask potentially co-occurring environmental influences so strongly that environmental effects can be difficult to observe in the those T1D cohorts designed to include only subjects at high genetic risk for T1D. Indeed, previous studies exploring the effects of other environmental factors such as vitamin D, breast feeding duration, probiotic use, gluten introduction and virus infection may also be masked by increased genetic risk. Only a large, general population study may be able to evaluate the full impact of these environmental influences and their interactions with genetic risk for T1D.
The All Babies in Southeast Sweden (ABIS) cohort is ideal for investigating the influence of HLA genetic risk on the microbiome since it was designed to survey the general population, making up a diverse range of HLA genotypes. The information gained from this type of cohort furthers our understanding of how HLA genetic risk drives changes in the gut microbiome and how genetics may be “setting the stage” for environmental triggers that ultimately lead to T1D autoimmunity. Furthermore, the results obtained in this study can likely be extended to investigate other autoimmune diseases where HLA serves as the primary genetic risk factor.
Methods
Sample collection
This study is based on the ABIS cohort (All Babies in Southeast Sweden), a prospective population-based cohort study including all children born in southeast Sweden during the period 1 October 1997–1 October 1999. The parents gave their informed consent after oral and written information and possibility of obtaining information via video film. Participating mothers completed questionnaires both at birth and at 1 year of age for the infant and diaries were kept during the first year of life40. Information collected in the questionnaires and diaries include, but are not limited to, antibiotic use, duration of breast feeding, and more.
Stool samples were collected from the diaper of the infant by use of a sterile spatula and tube provided by the WellBaby Clinic. The sample tubes were labeled with a unique subject identifier and frozen immediately after collection, either at the infant’s home or at the clinic. Samples collected at home were transported frozen, using freeze clamps, to the WellBaby Clinic. After arrival at the clinic, the samples were stored dry at −80 °C. All 403 stool samples used in this analysis were collected at 1 year of age, and each subject is represented by a single one-year sample.
Institutional Review Board approvals
The ABIS-study has ethical approvals from the Research Ethics Committees of the Faculty of Health Science at Linköping University, Sweden, Ref. 1997/96287 and 2003/03-092 and the Medical Faculty of Lund University, Sweden (Dnr 99227, Dnr 99321). All parents of the children in the ABIS-study gave their informed consent after careful oral and written information in addition to video film presentation. The microbiome analysis performed at the University of Florida was approved by the University of Florida’s Institutional Review Board as an exempt study assigned as IRB201800903.
HLA genotyping
HLA-DR/DQ genotypes associated with risk and protection were defined using typing for HLA-DQB1 and informative -DQA1 and DRB1 alleles for deducing presence of common European HLA-DR-DQ haplotypes variously associated with disease risk using sequence specific hybridization with lanthanide labelled oligonucleotide probes41,42. To enable the comparison of different levels of HLA risk for developing T1D autoimmunity, subjects with available HLA genotype data were placed into one of four categories of risk based on their HLA genotype. Subjects at the highest genetic risk for developing autoimmunity are represented by a single HLA genotype in this dataset, consisting of both increased risk-associated haplotypes: (DR3)-DQA1*05-DQB1*02 and (DR4)-DQA1*03-DQB1*0302 (DR3/4). In contrast, those at lowest risk are denoted by the absence of these haplotypes and the presence of one or two of protective haplotypes (DR15)-DQB1*0602, (DR13)-DQB1*0603, (DR5)-DQA1*05-DQB1*0301 and (DR7)-DQA1*0201-DQB1*0303. Subjects having either (DR3)-DQA1*05-DQB1*02 or (DR4)-DQA1*03-DQB1*0302 without presence of protective haplotypes were defined to be at increased risk. Those with (DR3)-DQA1*05-DQB1*02 or (DR4)-DQB1*0302 and one of the protective haplotypes and those without any risk or protective haplotypes are at neutral genetic risk. A subset of subject characteristics for the samples used in this work is described in Supplementary Table 1. HLA genotype information for the subjects included in this study is provided in the source data file.
DNA Extraction and 16S rRNA barcoded PCR
DNA from each sample was extracted from ~200 mg of stool12, using the E.Z.N.A Stool Extraction Kit following the manufacturer’s protocol (Omega Bio-tek, Doraville, CA). Samples were randomized to prevent the introduction of bias during extraction and blank negative controls were introduced alongside the samples to verify the absence of contamination in the extraction kit components. DNA used for subsequent PCR was quantified and assessed for purity using a Nanodrop spectrophotometer (Thermo Scientific, Wilmington, DE). Previously used custom barcoded primers 341F and 806R, targeting the V3-V4 variable regions of the 16S rRNA gene, were employed and PCR amplification was carried out with the following modifications. Briefly, 50 nanograms of extracted DNA was used as template in a final reaction volume of 50 μl containing 25 μl of 2X GoTaq Colorless Master Mix (Promega, Madison, WI), 10 μM of each primer, 0.1 μg/μl BSA, brought to final volume with nuclease free water. The following cycling conditions were used for amplification: initial denaturation at 95 °C for 2 min, followed by 30 cycles of 95 °C for 20 s, 61 °C for 30 s, 72 °C for 30 s, and a final elongation step of 72 °C for 5 min. All PCR reactions were run on 1% agarose gels to verify correct amplification and purified using the E.Z.N.A Cycle Pure kit per the manufacturer’s instructions (Omega Bio-tek, Doraville, CA). The purified PCR products were then quantified using the 1X dsDNA High Sensitivity kit with a Qubit 2.0 fluorometer (Invitrogen, Life Technologies Inc., Carlsbad, CA). An equal mass of amplicons from each sample were pooled and sequenced on the Illumina MiSeq platform (ICBR, Gainesville, FL).
V3-V4 16S sequencing using Illumina Miseq 2 × 300bp
Five Illumina MiSeq flow cells were used to generate 67 gigabases of nucleotide sequencing data for 965 samples. Sequencing read pre-processing, including merging and demultiplexing, was done using scripts available through Qiime v1.9.143. Forward and reverse sequencing reads were merged based on overlap to generate single reads using fastq-join https://github.com/ExpressionAnalysis/ea-utils. The joined reads were analyzed for quality using FastQC https://github.com/s-andrews/FastQC. The forward primer sequence used during PCR was trimmed using the fastx_trimmer tool available in the FASTX-Toolkit (http://hannonlab.cshl.edu/fastx_toolkit). The reads were then labelled according to 11-base barcodes located at the 3′ end of the read. Finally, the labelled reads were demultiplexed into separate FASTQ files by sample ID.
Sequencing read processing into amplicon sequencing variants
Demultiplexed sequences were further processed into amplicon sequencing variants (ASVs) using the DADA2 software package available in R44 (https://www.R-project.org). Briefly, the demultiplexed FASTQ files were visually assessed for quality via the “plotQualityProfile” function. Read quality dropped sharply beyond 400 nucleotides and the reads were truncated to this length. The truncated reads were also filtered to allow for no ambiguous nucleotides (N), a maximum expected error rate of 2, further truncation after encountering a base with Q-score 2 and the removal of PhiX reads. Chimeric sequences were filtered using the consensus method and taxonomy was assigned using the SILVA_v132 training set45–48. The resulting ASV table was used to analyze the composition of the stool microbiome using the phyloseq package49.
Further filtering removed samples with fewer than 1000 reads and samples with no subject genotype information. The remaining samples were rarefied to an even sequencing depth of 10,000 reads per sample, a sufficient sequencing depth verified through rarefaction curves. After filtering, 603 of the total 965 samples with HLA genotype data remained for analysis. Because not all genetic risk groups are represented in every town sampled, only those towns with at least one subject from each risk group were retained, resulting in 403 samples for analysis. The number of subjects in each risk group category are described in Supplementary Table 1.
Statistical analysis of stool microbiome
Differentially abundant ASVs between the genetic risk groups were determined using DESeq2 and LEfSe50,51. Alpha diversity (including plots) were calculated using the Microbiome R package (http://microbiome.github.com/microbiome). The Microbiome package was also used to calculate and filter by ASV prevalence. Differences in microbiome composition by genetic risk and other covariates were tested for using the permutational multivariate analysis of variance (PERMANOVA) test through the “adonis” function in the vegan R package (https://github.com/vegandevs/vegan). All PERMANOVA tests were performed with the default 999 permutations. PERMANOVA was used to test for significant differences in distance dissimilarity on a number of covariates including duration of breastfeeding, breastfeeding status at sample collection, antibiotic usage in the first year and within one month of sample collection (yes/no), mode of delivery and gender. The vegan package was also used for assessing multivariate homogeneity of variance (beta dispersion) between sampling groups using PERMDISP2. For calculating presence/absence metrics such as Jaccard, the “binary = TRUE” option was set. P-value results from statistical testing were corrected for false discovery rate (FDR) using the Benjamin–Hochberg (B–H) method52. Principal coordinate analysis (PCoA) plots, including the calculated 95% confidence ellipses, were generated using the ggplot2 R package53.
Culturing and identification of ASV isolates
Aliquots of stool were stored at −80 °C prior to DNA extraction to culture bacteria of interest, such as those associated with health and low genetic risk. Samples showing the highest relative abundance of significant Bifidobacterium ASVs were serially diluted in 1X phosphate buffered saline and plated on pre-reduced Modified Bifidobacterium Agar (Becton, Dickinson and Company) without the addition of lactulose. Individual colonies were isolated from the two lowest dilution plates and culture stocks were stored in a 15% glycerol solution at −80 °C. DNA from each isolate was extracted using the E.Z.N.A Bacterial DNA kit (Omega Bio-tek, Doraville, CA) and the full length 16 S rRNA gene sequence was amplified by PCR using universal primers 27F and 1492R54. The resulting PCR products were Sanger sequenced to determine the identity of the isolates (Eton Bioscience, Inc., San Diego, CA). Resulting sequences were compared to the GenBank nucleotide database for identification using BLAST55.
Supplementary information
Acknowledgements
We thank all children and their parents in the ABIS study, and the staff working with collection of questionnaires and biological samples in ABIS. ABIS was supported by Barndiabetesfonden (Swedish Child Diabetes Foundation); Swedish Council for Working Life and Social Research, Grant/Award Numbers: FAS2004-1775, FAS2004–1775; Swedish Research Council, Grant/Award Numbers: K2005-72 × -11242-11A and K2008-69 × -20826-01-4, K2008-69 × -20826-01-4; Östgöta Brandstodsbolag; Medical Research Council of Southeast Sweden (FORSS); JDRF Wallenberg Foundation, Grant/Award Number: K 98-99D-12813-01A; ALF-and LfoU grants from Region Östergötland and Linköping University, Sweden
Author contributions
J.T.R performed the data generation, processing, and analysis and prepared the paper and figures; L.F.W.R and M.O. contributed to data analysis and interpretation; J.I. performed the HLA genotyping; M.A.A, D.A.S. and E.W.T contributed to result interpretation; J.L. performed ABIS, designed the study and carried out sample collection, storage and transport; and all authors were involved in paper revisions and approval of the final version.
Data availability
The paired-end 16S raw sequencing data generated in this study is available through the NCBI Sequence Read Archive under BioProject PRJNA510423. The source data underlying Figs. 1c, 2, 5 and Table 2 are provided as a source data file. Also, the HLA genotypes and associated sample metadata used for statistical comparison are available in the source data file.
Competing interests
The authors declare no competing interests.
Footnotes
Peer review information: Nature Communications would like to thank the anonymous reviewers for their contributions to the peer review of this work. Peer review reports are available.
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Information accompanies this paper at 10.1038/s41467-019-11460-x.
References
- 1.Rewers M, Ludvigsson J. Environmental risk factors for type 1 diabetes. Lancet Lond. Engl. 2016;387:2340–2348. doi: 10.1016/S0140-6736(16)30507-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jakobsen Odin Andreas Johan, Szereday Laszlo. The “Three Amigos” lurking behind type 1 diabetes: Hygiene, gut microbiota and viruses. Acta Microbiologica et Immunologica Hungarica. 2018;65(4):421–438. doi: 10.1556/030.65.2018.017. [DOI] [PubMed] [Google Scholar]
- 3.Noble, J. A. & Erlich, H. A. Genetics of type 1 diabetes. Cold Spring Harb. Perspect. Med. 2, A007732 (2012). [DOI] [PMC free article] [PubMed]
- 4.Jerram, S. T. & Leslie, R. D. The genetic architecture of type 1 diabetes. Genes8, 209 (2017). [DOI] [PMC free article] [PubMed]
- 5.Llewelyn M, et al. HLA class II polymorphisms determine responses to bacterial superantigens. J. Immunol. 2004;172:1719–1726. doi: 10.4049/jimmunol.172.3.1719. [DOI] [PubMed] [Google Scholar]
- 6.Silverman M, et al. Protective major histocompatibility complex allele prevents type 1 diabetes by shaping the intestinal microbiota early in ontogeny. Proc. Natl Acad. Sci. USA. 2017;114:9671–9676. doi: 10.1073/pnas.1712280114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Toivanen P, Vaahtovuo J, Eerola E. Influence of major histocompatibility complex on bacterial composition of fecal flora. Infect. Immun. 2001;69:2372–2377. doi: 10.1128/IAI.69.4.2372-2377.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kubinak JL, et al. MHC variation sculpts individualized microbial communities that control susceptibility to enteric infection. Nat. Commun. 2015;6:8642. doi: 10.1038/ncomms9642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brestoff JR, Artis D. Commensal bacteria at the interface of host metabolism and the immune system. Nat. Immunol. 2013;14:676–684. doi: 10.1038/ni.2640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hooper, L. V., Littman, D. R. & Macpherson, A. J. Interactions between the microbiota and the immune system. Science. 336, 1268–1273 (2012). [DOI] [PMC free article] [PubMed]
- 11.Kinross JM, Darzi AW, Nicholson JK. Gut microbiome-host interactions in health and disease. Genome Med. 2011;3:14. doi: 10.1186/gm228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Davis-Richardson AG, et al. Bacteroides dorei dominates gut microbiome prior to autoimmunity in Finnish children at high risk for type 1 diabetes. Front. Microbiol. 2014;5:678. doi: 10.3389/fmicb.2014.00678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kemppainen KM, et al. Early childhood gut microbiomes show strong geographic differences among subjects at high risk for type 1 diabetes. Diabetes Care. 2015;38:329–332. doi: 10.2337/dc14-0850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vatanen T, et al. Variation in microbiome LPS immunogenicity contributes to autoimmunity in humans. Cell. 2016;165:842–853. doi: 10.1016/j.cell.2016.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Paun A, Yau C, Danska JS. The influence of the microbiome on type 1 diabetes. J. Immunol. 2017;198:590–595. doi: 10.4049/jimmunol.1601519. [DOI] [PubMed] [Google Scholar]
- 16.Endesfelder D, et al. Compromised gut microbiota networks in children with anti-islet cell autoimmunity. Diabetes. 2014;63:2006–2014. doi: 10.2337/db13-1676. [DOI] [PubMed] [Google Scholar]
- 17.Endesfelder D, et al. Towards a functional hypothesis relating anti-islet cell autoimmunity to the dietary impact on microbial communities and butyrate production. Microbiome. 2016;4:17. doi: 10.1186/s40168-016-0163-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vatanen T, et al. The human gut microbiome in early-onset type 1 diabetes from the TEDDY study. Nature. 2018;562:589. doi: 10.1038/s41586-018-0620-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stewart CJ, et al. Temporal development of the gut microbiome in early childhood from the TEDDY study. Nature. 2018;562:583. doi: 10.1038/s41586-018-0617-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Koren O, et al. A guide to enterotypes across the human body: meta-analysis of microbial community structures in human microbiome datasets. PLOS Comput. Biol. 2013;9:e1002863. doi: 10.1371/journal.pcbi.1002863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Anderson MJ, et al. Navigating the multiple meanings of β diversity: a roadmap for the practicing ecologist. Ecol. Lett. 2011;14:19–28. doi: 10.1111/j.1461-0248.2010.01552.x. [DOI] [PubMed] [Google Scholar]
- 22.Anderson MJ, Walsh DCI. PERMANOVA, ANOSIM, and the Mantel test in the face of heterogeneous dispersions: What null hypothesis are you testing? Ecol. Monogr. 2013;83:557–574. doi: 10.1890/12-2010.1. [DOI] [Google Scholar]
- 23.Yatsunenko T, et al. Human gut microbiome viewed across age and geography. Nature. 2012;486:222–227. doi: 10.1038/nature11053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Callahan BJ, McMurdie PJ, Holmes SP. Exact sequence variants should replace operational taxonomic units in marker-gene data analysis. ISME J. 2017;11:2639–2643. doi: 10.1038/ismej.2017.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Krischer JP, et al. Genetic and environmental interactions modify the risk of diabetes-related autoimmunity by 6 years of age: the TEDDY study. Diabetes Care. 2017;40:1194–1202. doi: 10.2337/dc17-0238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mäkinen A, Härkönen T, Ilonen J, Knip M. Characterization of the humoral immune response to islet antigen 2 in children with newly diagnosed type 1 diabetes. Eur. J. Endocrinol. 2008;159:19–26. doi: 10.1530/EJE-07-0853. [DOI] [PubMed] [Google Scholar]
- 27.Bolnick DI, et al. Major histocompatibility complex class IIb polymorphism influences gut microbiota composition and diversity. Mol. Ecol. 2014;23:4831–4845. doi: 10.1111/mec.12846. [DOI] [PubMed] [Google Scholar]
- 28.Galperin MY, Brover V, Tolstoy I, Yutin N. Phylogenomic analysis of the family Peptostreptococcaceae (Clostridium cluster XI) and proposal for reclassification of Clostridium litorale (Fendrich et al. 1991) and Eubacterium acidaminophilum (Zindel et al. 1989) as Peptoclostridium litorale gen. nov. comb. nov. and Peptoclostridium acidaminophilum comb. nov. Int. J. Syst. Evol. Microbiol. 2016;66:5506–5513. doi: 10.1099/ijsem.0.001548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Song YL, Liu CX, McTeague M, Summanen P, Finegold SM. Clostridium bartlettii sp. nov., isolated from human faeces. Anaerobe. 2004;10:179–184. doi: 10.1016/j.anaerobe.2004.04.004. [DOI] [PubMed] [Google Scholar]
- 30.Gerritsen J, et al. Characterization of Romboutsia ilealis gen. nov., sp. nov., isolated from the gastro-intestinal tract of a rat, and proposal for the reclassification of five closely related members of the genus Clostridium into the genera Romboutsia gen. nov., Intestinibacter gen. nov., Terrisporobacter gen. nov. and Asaccharospora gen. nov. Int. J. Syst. Evol. Microbiol. 2014;64:1600–1616. doi: 10.1099/ijs.0.059543-0. [DOI] [PubMed] [Google Scholar]
- 31.Mardinoglu A, Boren J, Smith U. Confounding effects of metformin on the human gut microbiome in type 2 diabetes. Cell Metab. 2016;23:10–12. doi: 10.1016/j.cmet.2015.12.012. [DOI] [PubMed] [Google Scholar]
- 32.Brahe LK, et al. Specific gut microbiota features and metabolic markers in postmenopausal women with obesity. Nutr. Diabetes. 2015;5:e159. doi: 10.1038/nutd.2015.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Calcinaro F, et al. Oral probiotic administration induces interleukin-10 production and prevents spontaneous autoimmune diabetes in the non-obese diabetic mouse. Diabetologia. 2005;48:1565–1575. doi: 10.1007/s00125-005-1831-2. [DOI] [PubMed] [Google Scholar]
- 34.Valladares R, et al. Lactobacillus johnsonii N6.2 mitigates the development of type 1 diabetes in BB-DP rats. PloS One. 2010;5:e10507. doi: 10.1371/journal.pone.0010507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Timmerman HM, et al. Design of a multispecies probiotic mixture to prevent infectious complications in critically ill patients. Clin. Nutr. 2007;26:450–459. doi: 10.1016/j.clnu.2007.04.008. [DOI] [PubMed] [Google Scholar]
- 36.van Minnen LP, et al. Modification of intestinal flora with multispecies probiotics reduces bacterial translocation and improves clinical course in a rat model of acute pancreatitis. Surgery. 2007;141:470–480. doi: 10.1016/j.surg.2006.10.007. [DOI] [PubMed] [Google Scholar]
- 37.Gerritsen J, et al. Correlation between protection against sepsis by probiotic therapy and stimulation of a novel bacterial phylotype▿. Appl. Environ. Microbiol. 2011;77:7749–7756. doi: 10.1128/AEM.05428-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sollid LM. The roles of MHC class II genes and post-translational modification in celiac disease. Immunogenetics. 2017;69:605–616. doi: 10.1007/s00251-017-0985-7. [DOI] [PubMed] [Google Scholar]
- 39.Liu E, et al. Risk of pediatric celiac disease according to HLA haplotype and country. N. Engl. J. Med. 2014;371:42–49. doi: 10.1056/NEJMoa1313977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ludvigsson J, Ludvigsson M, Sepa A. Screening for prediabetes in the general child population: maternal attitude to participation. Pediatr. Diabetes. 2001;2:170–174. doi: 10.1034/j.1399-5448.2001.20405.x. [DOI] [PubMed] [Google Scholar]
- 41.Ilonen J, et al. Genetic susceptibility to type 1 diabetes in childhood—estimation of HLA class II associated disease risk and class II effect in various phases of islet autoimmunity. Pediatr. Diabetes. 2016;17:8–16. doi: 10.1111/pedi.12327. [DOI] [PubMed] [Google Scholar]
- 42.Mikk ML, et al. The HLAB*39 allele increases type 1 diabetes risk conferred by HLA- DRB1*04:04-DQB1*03:02 and HLA-DRB1*08- DQB1*04 class II haplotypes. Hum. Immunol. 2014;75:65–70. doi: 10.1016/j.humimm.2013.09.008. [DOI] [PubMed] [Google Scholar]
- 43.Caporaso JG, et al. QIIME allows analysis of high-throughput community sequencing data. Nat. Methods. 2010;7:335–336. doi: 10.1038/nmeth.f.303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Callahan BJ, et al. DADA2: High resolution sample inference from Illumina amplicon data. Nat. Methods. 2016;13:581–583. doi: 10.1038/nmeth.3869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Pruesse E, et al. SILVA: a comprehensive online resource for quality checked and aligned ribosomal RNA sequence data compatible with ARB. Nucleic Acids Res. 2007;35:7188–7196. doi: 10.1093/nar/gkm864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Glöckner FO, et al. 25 years of serving the community with ribosomal RNA gene reference databases and tools. J. Biotechnol. 2017;261:169–176. doi: 10.1016/j.jbiotec.2017.06.1198. [DOI] [PubMed] [Google Scholar]
- 47.Yilmaz P, et al. The SILVA and “All-species Living Tree Project (LTP)” taxonomic frameworks. Nucleic Acids Res. 2014;42:D643–D648. doi: 10.1093/nar/gkt1209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Quast C, et al. The SILVA ribosomal RNA gene database project: improved data processing and web-based tools. Nucleic Acids Res. 2013;41:D590–D596. doi: 10.1093/nar/gks1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.McMurdie PJ, Holmes S. phyloseq: an R aackage for reproducible interactive analysis and graphics of microbiome census data. PLOS ONE. 2013;8:e61217. doi: 10.1371/journal.pone.0061217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Love, M. I., Huber, W. & Anders, S. Moderated estimation of fold change and dispersion for RNA-seq data with DESeq2. Genome Biol. 15, 550 (2014). [DOI] [PMC free article] [PubMed]
- 51.Segata N, et al. Metagenomic biomarker discovery and explanation. Genome Biol. 2011;12:R60. doi: 10.1186/gb-2011-12-6-r60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Benjamini Y, Hochberg Y. Controlling the false discovery rate: A practical and powerful approach to multiple testing. J. R. Stat. Soc. 1995;57:289–300. [Google Scholar]
- 53.Wickham, H. ggplot2: elegant graphics for data analysis. (Springer-Verlag, New York, 2009).
- 54.Lane, D. J. 16S/23S rRNA sequencing. (eds. Stackebrandt E. Goodfellow M) Nucleic Acid Tech. Bact. Syst. 115–175 (Wiley, New York, 1991).
- 55.Madden, T. The BLAST sequence analysis tool. (National Center for Biotechnology Information 2013).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The paired-end 16S raw sequencing data generated in this study is available through the NCBI Sequence Read Archive under BioProject PRJNA510423. The source data underlying Figs. 1c, 2, 5 and Table 2 are provided as a source data file. Also, the HLA genotypes and associated sample metadata used for statistical comparison are available in the source data file.