Abstract
Purpose
Comparing radiation treatment plans by using the same safety margins and dose objectives for all techniques, to ascertain the optimal radiation technique for the stereotactic body radiotherapy (SBRT) of low-risk prostate cancer.
Material and methods
Treatment plans for 27 randomly selected patients were compared using intensity-modulated (IMRT) techniques as Sliding Window (SW), volumetric modulated arc therapy (VMAT), and helical tomotherapy (HT), as well as Cyber Knife (CK) system. The target dose was calculated to 36.25 Gy delivered in five fractions over 1 week. Dosimetric indices for target volume and organs at risk (OAR) as well as normal tissue complication probability (NTCP) of late rectal and urinary bladder toxicities were analyzed.
Results
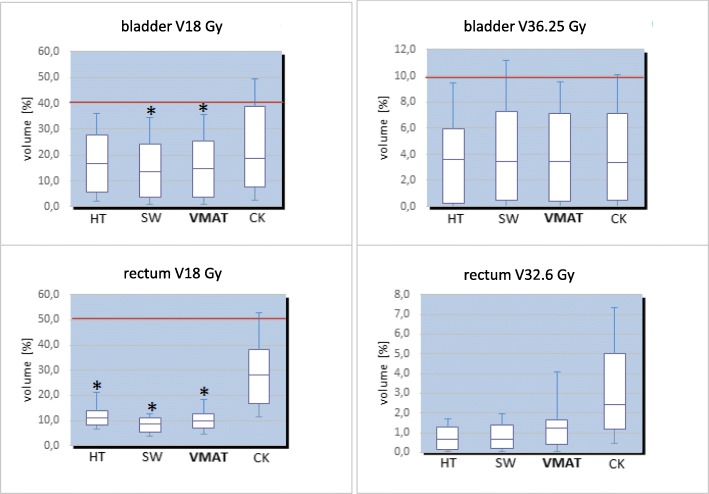
The CK provided lower homogeneity in the target volume, but higher values for most of the conformity indices compared to the IMRT approaches. The SW demonstrated superior rectum sparing at medium-to-high dose range (V18 Gy - V32.6 Gy) compared to other techniques (p < 0.05). The whole urinary bladder experienced the best shielding by SW and VMAT at the medium dose (V18 Gy, p < 0.05 versus CK), however we obtained no relevant differences between techniques at the high dose. Generally, the CK demonstrated significantly superior rectum and bladder exposure at V18 Gy as compared to HT, SW, and VMAT. For the rectum, mean NTCP values were significantly superior for HT (NTCP = 2.3%, p < 0.05), and for urinary bladder, the NTCP showed no significant advantages for any technique.
Conclusion
No absolute dosimetric advantage was revealed to choose between CK or IMRT techniques for the SBRT of low-grade prostate cancer. Using the same safety margins and dose objectives, IMRT techniques demonstrated superior sparing of the rectum and bladder at a medium dose compared to CK. Comparing different IMRT approaches SW displayed superior rectum sparing at a medium-to-high dose range, whereas both SW and RA revealed superior bladder sparing compared to HT. HT demonstrated a significantly lower NTCP outcome compared to CK or IMRT techniques regarding the rectum. Radiation plans can be optimized further by an individual modification of dose objectives independent of the treatment plan strategy.
Electronic supplementary material
The online version of this article (10.1186/s13014-019-1353-6) contains supplementary material, which is available to authorized users.
Keywords: Prostate carcinoma, Stereotactic radiotherapy, Intensity-modulated radiotherapy, Cyber knife, Dosimetric indices, Normal tissue complication probability
Introduction
Different radiotherapy techniques, as well as fractionation regimens, are currently used for localized prostate cancer. A conventionally-fractionated intensity modulated radiotherapy (IMRT) is the most frequently applied treatment modality in the case of prostate cancer. One retrospective analysis evaluated the standard fractionation versus hypofractionation regimens. This analysis suggests that the α/β value for prostate cancer is 1.4 Gy (0.9–2.2) regardless of risk status [1]. Furthermore, hypofractionated radiotherapy (RT) may be radiobiologically favorable in the treatment of prostate cancer due to potentially greater sensitivity of high fraction dose [2–4]. Previous studies of moderate hypofractionated RT (fraction dose between 2.5 Gy and 3.5 Gy) showed better disease local control, as well as similar toxicity rate compared to conventionally-fractionated RT [5–7]. Different radiation techniques, additionally, may be applied for stereotactic body RT (SBRT) in order to deliver a large fraction dose to the prostate. RT modality as provided by the robot-assisted technique Cyber Knife® (CK), which can deliver such radiation within a high fraction dose, is currently witnessing increased usage in the treatment of prostate cancer with low-to-intermediate risk [2, 8–12]. All IMRT techniques, especially rotational approaches as helical tomotherapy (HT) and volumetric modulated arc therapy (VMAT), can potentially deliver a high daily fraction, thus, achieving the treatment plans with high conformity and reducing the dose delivered to the surrounding healthy tissue. In the series of studies a good dosimetric quality for several SBRT techniques for the treatment of localized prostate cancer was demonstrated [13–17]. In this study, we performed a comparative statistical analysis of dosimetric parameters between Sliding Window (SW), HT, VMAT, and CK for the SBRT in patients with low-risk prostate cancer. It is the first planning study that, specifically, uses the Lyman-Kutcher-Burman (LKB) model in the analysis of late rectal and urinary toxicities following prostate SBRT based on estimation of NTCP parameters.
Material and methods
Patients
The treatment plans were generated for 27 randomly selected patients with low-risk prostate cancer who underwent definitive HT. The patient and tumor characteristics are presented in Additional file 1: Table S1 The mean age of study patients was 68 years (range 58 to 77 years). Patient selection criteria was based on the pathology of proven low-risk prostate cancer; PSA less than 10 ng/mL, Gleason Score 6 - 7a, and T1c - T2a per national comprehensive cancer network (NCCN) criteria [18].
Plan generation and analysis of dosimetric parameters
The databases of a thin-cut 3 mm CT scans were fused with 1.5 T MRI. The prescription dose was 5 fractions of 7.25 Gy to the 80% isodose. The corresponding dose was 36.25 Gy, with at least 98% coverage of the PTV. The potential maximum coverage of 100% of the prescribed dose covered 2% of PTV. This corresponds to a biological equivalent dose (BED) of approximately 90 Gy by the α/β value of 1.5 for prostate, 3 for rectum and 6 for urinary bladder [3, 4, 19–21]. Similar dose objectives adapted to the criteria of ICRU 83 were used by the planning for VMAT, SW, HT, as well as for CK.
The clinical target volume (CTV) and planning target volume (PTV) were defined according to Boehmer et al. [22]. The CTV included the prostate directly without seminal vesicles. A 3 mm margin in the dorsal direction and 5 mm margin in ventral and lateral directions was further added for PTV delineation. The prescription dose was limited to ≥80% in order to restrict maximum dose to the prostatic urethra with 110% of the prescription dose. To assess the PTV coverage, we have used the following parameters: PTVV80% – percentage volume of PTV receiving 36.25 Gy; PTVD2% (max, Gy) and PTVD98% (min, Gy) - maximum and mean dose to the PTV. The dose-volume objectives for the OAR are presented in Table 1. The dose constraints for OAR, furthermore, had met qualifying criteria per the Quantitative Analyses of Normal Tissue Effects in the Clinic (QUANTEC) reports (Table 1) [8, 9, 13, 14, 19, 20]. The patient-averaged dose-volume histograms (DVH) were statistically analyzed for PTV and OAR.
Table 1.
Organ at risk dose constraints
| Organ | ||
|---|---|---|
| Rectum | V18 Gy | < 50% |
| V29 Gy | < 20% | |
| V32.6 Gy | < 10% | |
| V36.25 Gy | < 5% | |
| Urinary bladder | V18 Gy | < 40% |
| V36.25 Gy | < 10% | |
| Femoral heads | V14.5 Gy | < 5% |
Abbreviations: Vx Percent of OAR volume exposed to certain radiation dose
Based on the recommendations of the ICRU 83 reports and several clinical studies, specific conformal indices were used to describe the dose distribution. These indices refer to the PTV volume, partial PTV volume covered by prescribed isodose (PTVpi), and volume treated by prescribed isodose (TVpi) [23]. The homogeneity index characterizes dose homogeneity inside of the PTV and is calculated using the near maximum (D2%), near minimum (D98%), and the mean dose (Dmean): D2% – D98%/Dmean (optimal at 0) [21]. The CN provides complementary information about irradiation of PTV and healthy tissues, and is calculated as PTVpi/PTV x PTVpi/TVpi, demonstrating the optimal results at a value of 1 [24]. The CIICRU was described in the ICRU 62 report and is defined as a quotient of TVpi/PTV (optimal at 1) [25]. The CΔ quantified the radiation exposure of the surrounding healthy tissue and is defined as TVpi - PTVpi/PTV (optimal at 0) [26]. The CΔCOV describes the coverage of the target volume by the prescribed isodose and is calculated as PTVpi/PTV, reflecting ideal PTV coverage for the value of 1 [27].
For this study the plans were generated by more than 3 independent planners. All plans were created for a possible use in the institute. The planning was not affected by previously generated plans because different plans were created by different planners for a patient case.
Radiation techniques
Seven-field IMRT plans using the SW technique were created on the Eclipse™ 10 treatment planning system [Varian Medical Systems, Palo Alto USA]. All plans were generated for the Varian True Beam linear accelerator (LINAC) using beam energies of 15 MV photons and beam angles of 0°, 51°, 102°, 153°, 204°, 255° and 306°. The VMAT plans were created using the same treatment planning system as for SW. Two incomplete arcs from 200° to 160° for the protection of the posterior rectum wall were used. The plans were created using 15 MV photons with a 0.5 cm leaf width. A maximum dose rate of 600 MU/min as well as MLC motion of 2.5 cm/s was applied. The MLC-leakage was at 1.8%. The HT plans were assessed using Tomo planning system version 5 (Accuray® Inc., Sunnyvale, USA). The plans were created for the High Art HDII HT system that uses a helical slice 6 MV photon beam modulated by 64 binary multileaf collimators. The Multiplan® planning system version 5.2 was used to generate the CK plans (Accuray®, Sunnyvale, USA). The CK robotic arm moves in six different axes with a specific positioning accuracy of 0,2 mm. It delivers a 6 MV photon beam with a dose rate of 850 MU/min. The collimator system consists of 12 fixed cones with a size of 5 mm to 60 mm (at 800 mm SAD).
NTCP estimation
Lyman’s model of rectal and bladder toxicities was used for estimating NTCPs, which is integrated in the biological evaluation module [28]. Parameters used in the Lyman’s model are presented in Table 2. The dose was recalculated to the conventionally fractionated treatment schedule of 2 Gy per fraction using the α/β value of 3 for rectum, and α/β value of 6 for bladder [29–31]. Lyman’s model is based on a probit function: , where and , where D50 = dose giving a 50% response probability, m = slope of the response curve, n = volume dependence, M = total number of voxels, = relative volume of voxel compared to reference volume, and EQD2 = the equivalent dose in voxel when given in 2 Gy fractions.
Table 2.
Parameters used in the Lyman-Kutcher-Burman model
| Parameter | Rectum | Urinary bladder |
|---|---|---|
| D50% | 80 | 62 |
| α/β | 3 | 6 |
| n | 0.06 | 0.13 |
| m | 0.15 | 0.11 |
Abbreviations: D50% Tolerance dose leading to 50% complications, n Volume effect, m Steepness of the dose-response curve
Statistical analysis
The statistical analysis was carried out through SPSS software (SPSS for Windows, Version 24.0). A p-value < 0.05 was considered statistically significant. The comparison of dose distribution in the target volume and in the OAR through use of different radiation techniques was examined with the Wilcoxon Test for paired-samples. In a similar way, we tested the homogeneity and conformity of the radiation field in the target volume for different field arrangements. The effect of the variables (techniques) on the NTCP outcome of urinary and rectal toxicities was statistically analyzed by use of Wilcoxon Test.
Results
The volumes of the prostate and urinary bladder did not exhibit any relevant data concerning dose distribution volumetric differences in analyzed patients. The average of these volumes was 31 cm3 (range, 27 cm3 to 58 cm3) and 300 mL (range, 220 mL to 410 mL), correspondingly. Similarly, the rectal diameter did not significantly vary between patients (median 5 cm, range 3.4 cm to 7.4 cm) (Additional file 1: Table S1.
Conformal indices are summarized in Table 3. HI around 0.2 was received for all techniques. The HT provided a higher homogeneity of dose distribution than in any other technique employing the target volume. This demonstrates a significant advantage compared to CK (p = 0.03). Similarly, the coverage index COV appeared inferior for the CK. Other conformity indices (CN, CIICRU, CΔ) revealed superior values for the CK.
Table 3.
Summary of dosimetric indices averaged from the treatments plans of 27 patients
| Index | HT Mean ± SD |
SW Mean ± SD |
VMAT Mean ± SD |
CK Mean ± SD |
|---|---|---|---|---|
| Homogeneity index, HI | 0.18 ± 0.01* | 0.21 ± 0.01 | 0.19 ± 0.01 | 0.21 ± 0.04* |
| Conformation number, CN | 0.85 ± 0.05 | 0.81 ± 0.05 | 0.87 ± 0.03 | 0.87 ± 0.06 |
| ICRU Conformity index, CIICRU | 1.16 ± 0.08 | 1.22 ± 0.07 | 1.13 ± 0.04 | 1.08 ± 0.07 |
| Coverage index, CΔ | 0.16 ± 0.08 | 0.23 ± 0.07 | 0.14 ± 0.04 | 0.11 ± 0.06 |
| Coverage index, COV | 0.99 ± 0.01 | 0.99 ± 0.01 | 0.99 ± 0.01 | 0.97 ± 0.02 |
Abbreviations: VMAT Volumetric Modulated Arc Therapy, SW Sliding Window, HT Helical tomotherapy, CK Cyber Knife, SD Standard deviation, HI Homogeneity index, CN Conformation number, CIICRU ICRU conformity index, C∆ Coverage index, COV Coverage index COV; *-values with statistically significant difference (p < 0.05)
The time for the planning averaged 2.5 h for CK, 2 h for HT, and 1 h for VMAT and SW. The mean treatment delivery time was significantly higher for CK with 42 min compared to IMRT techniques. Among IMRT approaches, the median treatment time of the HT was significantly higher with 22 min (range: 16–26 min; p < 0.05) compared to SW (6 min, range: 4.5–8.2 min) or VMAT (5 min, range: 4–6 min).
We assessed the dosimetric values for PTV and OAR from the patient-averaged DVH (these values are presented in further detail in Table 4). The mean prescription volumes did not show any relevant volumetric differences between the radiation techniques and varied between 90 cm3 and 160 cm3. The PTVV80 was found significantly lower for CK compared to other IMRT techniques (p = 0.04), whereas D2% and D98% values did not significantly vary between the techniques (Table 4). The patient-averaged DVH revealed statistically superior rectum sparing by IMRT techniques at the doses range of V18 Gy -– 32.6 Gy compared to CK technique (p < 0.05) (Figs. 1 and 2, Table 4). The highest rectum shielding was received by SW at medium-to-high dose range (Figs. 1 and 2, Table 4). The whole urinary bladder experienced the significant shielding by SW and VMAT at 18 Gy (V18 Gy, p < 0.05 versus CK) (Figs. 1 and 2; Table 4). No relevant dosimetric difference in the dose distribution to rectum and urinary bladder was found between techniques at V36.25 Gy. A significantly superior sparing of femoral heads was received by HT (V14.5 Gy). The CK affected mostly the left femoral head, for that spared highly the right femoral head (Figs. 1 and 2; Table 4).
Table 4.
Averaged dosimetric values for PTV and organ at risk
| HT Mean ± SD |
SW Mean ± SD |
VMAT Mean ± SD |
CK Mean ± SD |
|
|---|---|---|---|---|
| PTV | ||||
| V80 (%) | 99.03 ± 0.63* | 99.15 ± 0.59* | 99.35 ± 0.44* | 96.84 ± 2.48* |
| D2% (Gy) | 44.10 ± 0.72 | 45.41 ± 0.69 | 45.17 ± 0.26 | 44.08 ± 0.39 |
| D98% (Gy) | 36.90 ± 0.41 | 36.86 ± 0.46 | 37.10 ± 0.27 | 35.82 ± 0.92 |
| Urinary Bladder | ||||
| V18 Gy (%) | 17.30 ± 12.88 | 15.46 ± 12.33* | 15.52 ± 12.48* | 22.51 ± 17.64* |
| V36.25 Gy (%) | 3.70 ± 3.49 | 4.24 ± 4.11 | 3.98 ± 3.75 | 4.04 ± 3.82 |
| Rectum | ||||
| V18 Gy (%) | 11.51 ± 3.87* | 8.34 ± 3.13* | 10.40 ± 4.45* | 29.62 ± 13.79* |
| V29 Gy (%) | 2.72 ± 1.46* | 2.18 ± 1.30* | 2.99 ± 1.91* | 8.11 ± 5.03* |
| V32.6 Gy (%) | 0.72 ± 0.59 | 0.82 ± 0.69 | 1.29 ± 1.11 | 3.10 ± 2.24 |
| V36.25 Gy (%) | 0.01 ± 0.03 | 0.08 ± 0.11 | 1.22 ± 3.70 | 0.19 ± 0.25 |
| Femoral head right | ||||
| V14.5 Gy (%) | 0.05 ± 0.13* | 11.21 ± 13.78 | 11.59 ± 18.60 | 2.04 ± 3.67 |
| Femoral head left | ||||
| V14.5 Gy (%) | 0.07 ± 0.18* | 9.07 ± 11.04 | 10.16 ± 13.35 | 21.16 ± 13.75* |
Abbreviations: HT Helical tomotherapy, SW Sliding Window, VMAT Volumetric Modulated Arc Therapy, CK Cyber Knife, PTV Planning target volume, SD standard deviation, Dx (Gy) Dose (Gy) absorbed by the certain percent (%) or absolute volume (cc) of the countered structure, Vx Percent of OAR volume exposed to certain radiation dose; *- Values with statistically significant difference (p < 0.05)
Fig. 1.
Boxplot demonstrating a difference in the sparing of urinary bladder and rectum by using of different radiation techniques. Red lines represent dose objective levels (level rectum V32.6 Gy < 10% out of scale). * - Significantly (p < 0.05) superior sparing for urinary bladder was found for VMAT and SW at V18 Gy vs. CK, and of rectum for Tomo, SW and VMAT at V18 Gy vs. CK. Abbreviations: VMAT – Volumetric Modulated Arc Therapy; SW – Sliding Window; HT– helical tomotherapy; CK – Cyber Knife; Vx – percent of OAR volume exposed to certain radiation dose
Fig. 2.
Pair-wise statistical dosimetric comparison between radiation techniques. The differences in sparing of OAR are shown at V18 Gy - V36.25 Gy for rectum and urinary bladder, and V14.5 Gy for femoral heads. Urinary bladder is indicated in yellow, rectum in brown, femoral heads in green. *- significant difference in dose distribution to OAR between radiation techniques
The calculated mean NTCP values and the model parameters for the rectum and urinary bladder are.
listed in Table 5. The HT revealed significantly superior mean NTCP values for rectum (NTCP = 2.3%, p < 0.05) than was demonstrated by VMAT (NTCP = 4.5%), SW (NTCP = 3.8%) and CK (NTCP = 5.8%). For urinary bladder the mean NTCP values were not significantly lower for SW (NTCP = 1.8%) compared to VMAT (NTCP = 2.5%) HT (NTCP = 2.8%) and CK (NTCP = 2.2%). Consequently, the HT demonstrated a lower NTCP outcome compared to CK or IMRT techniques for rectum and the NTCP for the urinary bladder showed no significant advantages for any technique.
Table 5.
Calculated mean NTCP values (%) of all patients
| Technique/Organ | Rectum | Urinary bladder |
|---|---|---|
| HT | 2.3* | 2.8 |
| SW | 3.8 | 1.8 |
| VMAT | 4.5 | 2.8 |
| CK | 5.8 | 2.2 |
Abbreviations: HT Helical tomotherapy, SW Sliding Window, VMAT Volumetric Modulated Arc Therapy, CK Cyber Knife; * - value with statistically significant difference (p < 0.05)
Discussion
Our study evaluated a dosimetric comparison between IMRT-based techniques and robotic-assisted CK system by applying the SBRT for low risk prostate carcinoma. To our knowledge, this is the first time, when the NTCP parameters, which demonstrate probability of late rectal and urinary bladder radiation-related complications, were comparatively analyzed for SBRT techniques. Previous reports showed a high rate of biochemical, disease-free survival, along with an acceptable toxicity profile, with a larger fraction dose by applying SBRT techniques [9, 32–35]. Most single-center studies have used the CK technology demonstrating the feasibility of CK-based prostate SBRT [9–13, 33, 35–38]. McBride et al. demonstrated in their first multi-institutional Phase I study, an effective and safe use of hypofractionation with a CK System, by applying a 7.25–7.5 Gy fraction dose delivered in 5 fractions for the treatment of low-risk prostate adenocarcinoma [12]. The Prospective Randomized Phase III study, “PACE,” was developed to evaluate a clinical outcome following the SBRT monotherapy with CK, and further examined this therapy in comparison to surgery and conventionally fractionated IMRT in localized prostate carcinoma (http://www.clinicaltrials.gov/ct2/show/NCT01584258?term=PACE&rank=12). Unlike standard IMRT a technique, the CK technology performs an intrafractional matching of the beam targeting the prostate when motion is detected achieving the targeting errors of less than 1 mm [39, 40]. However, the longer treatment time with CK may result in intrafraction dose uncertainty because of bladder and bowel motion with anatomical deformation during the radiation treatment. Thus, Reggiori et al. showed that dose uncertainties for the targets and rectum amplified with the increase of time in patients treated with VMAT [41]. The mean treatment time that we observed for IMRT techniques, especially for VMAT and SW, was significantly less than for CK, (6 and 5 min compared to 42 min, respectively). The short treatment time helps to avoid dosimetric uncertainties in the target volume caused by bladder and bowel intrafraction form variation. Most treatment planning systems used for CK do not have advanced algorithms for the reducing of the planning time. Rossi et al. have proposed an automated treatment plan generation by using of “Erasmus-iCycle” optimizer for the creation of a beam angle class solution for noncoplanar prostate SBRT with CK to replace time-consuming beam angle optimization for each individual patient [16]. Using the in-house developed optimizer, the authors established 15-, 20-, and 25-beam class solutions without significant loss in plan quality compared to individualized beam angle selection, reducing the computation time for the plans generation by a factor of 14 to 25. Thus, using beam angle class solution instead of individualized beam angel selection, 25-beam plans could be generated in 31 min compared with 13 h.
We have demonstrated that both CK and IMRT-based techniques achieve similar dosimeteric outcomes, concerning PTV coverage, as well as providing highly conformal dose distribution. However, PTV homogeneity was significantly lowered in the CK treatment plans compared to rotational IMRT approaches. In addition, the IMRT techniques provided lower rectum and urinary bladder exposure at medium-to-high dose ranges than CK. Our findings are in agreement with the results obtained by MacDougall et al. [13]. Their results were provided from a dosimetric analysis gathered by comparing dose distribution between the CK and a VMAT with delivery of 35 Gy to the prostate in 5 fractions. The dose constraints for OAR were achieved by both techniques, however, PTV homogeneity as well as the mean planning and delivery time were in favor of VMAT. Furthermore, the use of VMAT was found to be superior when sparing OAR at lower radiation doses. Similarly, Lin et al. showed that applying 37.5 Gy in 5 fractions revealed superior PTV coverage and better rectum sparing at low doses with VMAT plans than with CK plans, although 6 MV photon beams were used for the VMAT treatment plans as opposed to 15 MV in our analysis [14]. Moreover, the VMAT plans demonstrated an excellent dose conformity resulting in faster dose falloff compared to CK plans. Finally, the author observed with VMAT plans fewer low-dose area, lower Monitor Units (MU), and faster delivery time than with CK plans. The authors speculated that the overall risk of secondary malignancy might be higher for CK through greater involvement of normal tissue receiving low RT dose, as well as higher MUs and treatment delivery time. Dong et al. comparatively analyzed the dose distribution for prostate SBRT (40 Gy in 5 fractions) by using of optimized robotic non-coplanar RT, termed 4π therapy, which is established on C-arm LINAC platform, and 2-arc VMAT [15]. Both planning methods demonstrated adequate PTV coverage. However, the 4π plans achieved significantly superior sparing of anterior rectum wall and penile bulb, reducing the maximum doses ad V50%, V80%, V90% and D1 cm3. The bladder dose was only slightly reduced by using of 4π therapy. Thus, by optimizing beam angles and fluences in the non-coplanar solution space, the authors have achieved superior quality for prostate SBRT compared to advanced VMAT plans. Rossi et al. developed systems for automatic generation of clinically deliver-able plans for robotic SBRT (autoROBOT). The quality of these plans was compared with VMAT plans that were also automatically generated, by applying of 9.5 Gy in 4 fractions [17]. Interestingly, in the autoROBOT and autoVMAT comparison with 3 mm PTV margins for all techniques, rectum doses (D1 cm3 and Dmean) was significantly lower in autoROBOT plans, with comparable PTV coverage and other OAR sparing. Compared to manual sparing, autoROBOT significantly improved rectum and urinary bladder sparing (D1 cm3 and Dmean), with equal PTV coverage. Thus, in contrast to results observed in our study by the comparison of manually generated VMAT and CK plans, authors demonstrated a superiority of non-coplanar robotic SBRT compared to coplanar VMAT when using the autoplanning for both techniques.
Assuming the same dose objectives for treatment planning, we can explain differences in dose distribution within PTV and OAR by the impact of radiation technique and by different dose calculation algorithms. The Multiplan planning system used for CK is less sensitive to dose constraints than the planning systems used for rotational approaches. Lowered sensitivity can result in the difference of PTV homogeneity in CK plans while using the same dose objectives in the planning system for IMRT techniques. However, a crucial factor that determinates the feasibility of radiation treatment plans is the optimization of dose constraints in each individual case.
Varying selection criteria, as well as differences in the target volume definition and dose constraints for OAR that do exist, actually describe the prostate SBRT. The difference in a cumulative radiation dose (between 33 Gy and 38 Gy), as well as in RT regimens (4 to 5 fractions) lead to substantial variations in an applied BED. Similarly, there is a wide spectrum of dose constraints for PTV and OAR in the available literature date [2, 7–9, 42–44]. For this reason, we used a combination of constraints from the PACE study and those recommended by Accuray and Varian Centers which deliver SBRT with CK/tomotherapy and RA/Sliding Window, consecutively. We assessed the BED by using the α/β value of 3 for rectum and 6 for urinary bladder to convert all constraint dose to 2 Gy per fraction. This allowed for an appreciation of the used dose objectives, according to criteria proposed by QUANTEC reports, which establishes the conventionally fractionated RT [19, 20]. Concerning the urethral sparing, is suggested that more heterogeneous dose distribution may provide a requisite prostatic urethra sparing within PTV. We restricted the maximum dose to 110% of the prescription dose in the treatment plans for all techniques to reduce the irradiation dose for the prostatic urethra. In the aspect of urethral toxicity, a multicentric Phase II study, which evaluates the SBRT in prostate cancer delivered by VMAT, including urethral sparing, is ongoing (http://www.clinicaltrials.gov/ct2/show/NCT01764646?term=NCT01764646&rank=1). Generally, the dose objectives for the prostate SBRT should be based on the datasets of the advanced radiotherapy technologies and large prospective randomized trials.
Another concern is the safety margins in the PTV delineation, which should be used to deliver SBRT for low-risk prostate carcinoma, to achieve a validated dosimetric comparison we used the same safety margins in both the CK and IMRT techniques, with a 3 mm margin in the dorsal direction and 5 mm margin in ventral and lateral directions. The use of image-guided RT with prostate verification immediately before treatment may not be enough for the precise delivery of radiation dose due to intrafraction prostate motion. According to established literature, the standard deviation of systematic and random errors due to intrafraction prostate motion varies from 0.2 to 1.7 mm and 0.4 to 1.3 mm, respectively [41, 45–49]. Considering that CK performs the real-time tracking of intrafractional prostate motion with a 1 mm precision in radiation dose delivery, MacDougall et al. have suggested the use of a safety margin of 3 mm for all directions in CK and 5 mm in VMAT [13]. Some authors observed a good clinical response as well as very low risk of intestinal grade 4 and 3 adverse effects applying the CK-based SBRT for low-risk prostate carcinoma by using of 2 or 2.5 mm safety margins into the rectal directions [50, 51]. Similarly, in the newly initiated prospective observational bi-center trial “HYPOSTAT”, the PTV was delineated with posterior margins of 2 mm for the CK-based SBRT [52]. On the other side, in the large series of reports describing the stereotactic RT with CK for localized prostate carcinoma, was observed a low rate of transient grade 3 and 2 urinary and rectal toxicities by using of 3 mm dorsal PTV margin and 5 mm safety margins in all other directions [41, 45–49]. Considering the highest exposure of rectum and urinary bladder for CK compared to IMRT that was revealed in this study, we would recommend reducing the PTV margins up to 2 mm in all directions for the CK-based SBRT, to minimize the risk of urinary and rectal toxicities as well as to provide a dosimetric advantage compared to advanced IMRT techniques.
One lingering question in regards to SBRT for prostate cancer is the RT regimen. King et al. reported on the fourfold reduction in Grade 1 urinary toxicity and a sevenfold reduction in Grade 1 rectal toxicity in favor of the every-other-day SBRT compared to daily SBRT consisted of 36.25 Gy in 5 fractions [9]. The authors, ultimately, recommended treating the prostate with an every-other-day dose schedule in order to allow the SBRT to minimize late effects in normal tissue. However, only a randomized trial would be able to properly study differences between different RT regimens.
We focused on analyzing the probability of late rectal and urinary toxicities by using SBRT on low-risk prostate carcinoma. Despite the significant dosimetric advantage in rectum protection for SW (Table 4), the NTCP values of late rectal toxicities reveal that HT is superior in this regard (Table 5). Use of fixed-fields IMRT, but not rotational techniques, was shown to improve the NTCP parameters for urinary bladder. The SW or HT, but not VMAT, generally are preferred in order to reduce the probability of late rectal in the treatment of low-risk prostate carcinoma. The NTCP for the urinary bladder showed no significant advantages for any technique.
This study is based on the treatment planning systems Eclipse™10, Tomo planning system version 5 and the Multiplan® planning system version 5.2. In the development process of this work the treatment planning systems were routinely used in our institute. The newer algorithms for the optimization lead into a different way of planning. For example the new Photon Optimizer in the Eclipse™15 has an improved OAR and target overlap modeling. With similar dose objectives in the planning process the resulting dose distribution and DVH differs slightly between Eclipse™10 and Eclipse™15. Therefore, the individual optimization of dose objectives may improve the target coverage and OAR sparing by using of Eclipse™10 treatment planning system. The NTCP values are based on DVH results so a newer algorithm could show a different result. There are some studies about the influence or impact of dose calculation algorithms on NTCP values, especially for lung cancer [53–55]. Because of a steady progress of algorithms to increase the accuracy of dose distribution and to minimize uncertainties, an additional work could investigate the impact of an update of the Eclipse™10 to Eclipse™15 regarding the NTCP of prostate SBRT.
Our study is limited by its retrospective nature and small number of study population which precludes big conclusions and planning’s parameters used should not be extrapolated for all cases. For example, the PTV margins for prostate SBRT should be defined based on radiation technique used, carcinoma stage and prostate volume. Another possible limitation is selection bias due to large difference in the prostate and rectal volume in analyzed patients (Additional file 1: Table S1. For this reason, the estimated treatment plans demonstrated large variations in the values of PTV coverage and OAR sparring between patients. In addition, the dose constraints for rectum and urinary bladder recommended by QUANTEC are based on 3-D conventional RT datasets. The advanced IMRT and CK techniques provide highly conformal dose distribution, performing superior OAR sparing compared to 3-D CRT, thus the dose constraints for OAR must be adopted for advanced IMRT and CK techniques used for prostate SBRT. Regarding NTCP analysis, we used the Lyman’s model of rectal and bladder toxicities for estimating of NTCP values. However, Viswanathan et al. aver that no convenient quantitative model exists, which can satisfactorily analyze late bladder toxicity after external beam radiotherapy [20]. This is due to lack of a clear dose response and functional variability of the bladder. Finally, the radiation plans can be optimized by individual modification of dose objectives for each treatment case. This argument can diminish the relevance of the obtained results, despite the use of similar dose objectives in the estimation of the radiation plans. Thus, selection criteria for dosimetric comparison between different radiation approaches should be further optimized.
Conclusion
This analysis is focused on the evaluation of the dosimetric feasibility of different SBRT techniques in the therapy of low-risk prostate cancer. For all techniques we applied the same safety margins for the delineation of the target volume as well as the same dose objectives were used for the plan optimizations. Major findings to emerge from this study are as follows: (i) All techniques showed a high conformal dose distribution in achieving OAR constraints; (ii) The CK revealed lower homogeneity within the target volume; (iii) The CK revealed the highest exposure of rectum and urinary bladder compared to IMRT, especially at medium-to-high dose ranges; (iv) comparing IMRT techniques, the SW displayed superior rectum sparing at medium-to-high dose range, whereas both SW and VMAT revealed superior bladder sparing; (v) techniques such as SW or HT — but not VMAT — demonstrate a reduced probability of late rectal complications; (vi) The mean treatment delivery time was significantly less for IMRT techniques than for CK, with shorter mean values for SW (6 min) and VMAT (5 min) compared to 42 min for CK. Generally, this dosimetric analysis revealed a higher protection of the rectum and bladder by using IMRT techniques compared to CK for the SBRT of prostate cancer. However, considering the possible optimization of radiation plans by the individual modification of dose objectives for each case, the radiation technique for prostate SBRT should be selected individually dependent on the treatment strategy.
Additional file
Table S1. Variables for patients’ population. (DOCX 12 kb)
Acknowledgements
Not applicable in this section.
Abbreviations
- BED
Biological equivalent dose
- CBCT
Cone beam computed tomography
- CK
Cyber Knife
- CTV
Clinical target volume
- DVH
Dose-volume histograms
- HT
Helical tomotherapy
- IMRT
Intensity-modulated radiotherapy
- LINAC
linear-accelerator
- LKB
Lyman-Kutcher-Burman model
- MRI
Magnetic resonance imaging
- NCCN
National Comprehensive Cancer Network
- NTCP
Normal tissue complication probability
- OAR
Organ at risk
- PFS
Progression free survival
- PTV
Planning target volume
- QUANTEC
Quantitative Analyses of Normal Tissue Effects in the Clinic
- SBRT
Stereotactic body radiotherapy
- SW
Sliding Window
- TCP
Tumor control probability
- VMAT
Volumetric Modulated Arc Therapy
Authors’ contributions
All authors participated in patient treatment and were involved in the preparation of the manuscript. All authors reviewed and approved the final manuscript.
Funding
Not applicable in this section.
Availability of data and materials
The datasets supporting the conclusions of this article are available in the repository of the Department of Radiotherapy and Radiooncology, University Hospital of Muenster.
Ethics approval and consent to participate
Not applicable in this section.
Consent for publication
Not applicable in this section.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Sergiu Scobioala and Christopher Kittel contributed equally to this work.
Contributor Information
Sergiu Scobioala, Phone: +49 251-83-47384, Email: sscobioala@yahoo.com.
Christopher Kittel, Email: Christopher.Kittel@ukmuenster.de.
Khaled Elsayad, Email: khaled.elsayad@ukmuenster.de.
Kai Kroeger, Email: Kai.Kroeger@ukmuenster.de.
Michael Oertel, Email: Michael.Oertel@ukmuenster.de.
Laith Samhouri, Email: Laith.Samhouri@ukmuenster.de.
Uwe Haverkamp, Email: uwe.haverkamp@ukmuenster.de.
Hans Theodor Eich, Email: hans.eich@ukmuenster.de.
References
- 1.Miralbell R, Roberts SA, Zubizarreta E, Hendry JH. Dose-fractionation sensitivity of prostate cancer deduced from radiotherapy outcomes of 5,969 patients in seven international institutional datasets: α/β = 1.4 (0.9–2.2) Gy. Int J Radiat Oncol Biol Phys. 2012;82:17–24. doi: 10.1016/j.ijrobp.2010.10.075. [DOI] [PubMed] [Google Scholar]
- 2.Ju AW, Wang H, Oermann EK, Sherer BA, Uhm S, Chen VJ, Pendharkar AV, Hanscom HN, Kim JS, Lei S, Suy S, Lynch JH, Dritschilo A, Collins SP. Hypofractionated stereotactic body radiation therapy as monotherapy for intermediate-risk prostate cancer. Radiat Oncol. 2013;31:8–30. doi: 10.1186/1748-717X-8-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fowler J, Chappell R, Ritter M. Is alpha/beta for prostate tumors really low? Int J Radiat Oncol Biol Phys. 2001;50:1021–1031. doi: 10.1016/S0360-3016(01)01607-8. [DOI] [PubMed] [Google Scholar]
- 4.Wang JZ, Guerrero M, Li XA. How low is the alpha/beta ratio for prostate cancer? Int J Radiat Oncol Biol Phys. 2003;55:194–203. doi: 10.1016/S0360-3016(02)03828-2. [DOI] [PubMed] [Google Scholar]
- 5.Yeoh EE, Botten RJ, Butters J, Di Matteo AC, Holloway RH, Fowler J. Hypofractionated versus conventionally fractionated radiotherapy for prostate carcinoma: final results of phase III randomized trial. Int J Radiat Oncol Biol Phys. 2010;81:1271–1278. doi: 10.1016/j.ijrobp.2010.07.1984. [DOI] [PubMed] [Google Scholar]
- 6.Lukka H, Hayter C, Julian JA, Warde P, Morris WJ, Gospodarowicz M, Levine M, Sathya J, Choo R, Prichard H, Brundage M, Kwan W. Randomized trial comparing two fractionation schedules for patients with localized prostate cancer. J Clin Oncol. 2005;23:6132–6138. doi: 10.1200/JCO.2005.06.153. [DOI] [PubMed] [Google Scholar]
- 7.Arcangeli G, Saracino B, Gomellini S, Petrongari MG, Arcangeli S, Sentinelli S, Marzi S, Landoni V, Fowler J, Strigari L. A prospective phase III randomized trial of hypofractionation versus conventional fractionation in patients with high-risk prostate cancer. Int J Radiat Oncol Biol Phys. 2010;78:11–18. doi: 10.1016/j.ijrobp.2009.07.1691. [DOI] [PubMed] [Google Scholar]
- 8.Chen LN, Suy S, Uhm S, Oermann EK, Ju AW, Chen V, Hanscom HN, Laing S, Kim JS, Lei S, Batipps GP, Kowalczyk K, Bandi G, Pahira J, McGeagh KG, Collins BT, Krishnan P, Dawson NA, Taylor KL, Dritschilo A, Lynch JH, Collins SP. Stereotactic Body Radiation Therapy (SBRT) for clinically localized prostate cancer: the Georgetown University experience. Radiat Oncol. 2013;8:58. doi: 10.1186/1748-717X-8-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.King CR, Brooks JD, Gill H, Presti JC., Jr Long-term outcomes from a prospective trial of stereotactic body radiotherapy for low-risk prostate cancer. Int J Radiat Oncol Biol Phys. 2012;82:877–882. doi: 10.1016/j.ijrobp.2010.11.054. [DOI] [PubMed] [Google Scholar]
- 10.Bolzicco G, Favretto MS, Scremin E, Tambone C, Tasca A, Guglielmi R. Image-guided stereotactic body radiation therapy for clinically localized prostate cancer: preliminary clinical results. Technol Cancer Res Treat. 2010;9:473–477. doi: 10.1177/153303461000900505. [DOI] [PubMed] [Google Scholar]
- 11.Jabbari S, Weinberg VK, Kaprealian T, Hsu IC, Ma L, Chuang C, Descovich M, Shiao S, Shinohara K, Roach M, 3rd, Gottschalk A. RStereotactic body radiotherapy as monotherapy or post-external beam radiotherapy boost for prostate cancer: technique, early toxicity, and PSA response. Int J Radiat Oncol Biol Phys. 2012;82:228–234. doi: 10.1016/j.ijrobp.2010.10.026. [DOI] [PubMed] [Google Scholar]
- 12.McBride SM, Wong DS, Dombrowski JJ, Harkins B, Tapella P, Hanscom HN, Collins SP, Kaplan ID. Hypofractionated stereotactic body radiotherapy in low-risk prostate adenocarcinoma: preliminary results of a multi-institutional phase 1 feasibility trial. Cancer. 2012;118:3681–3690. doi: 10.1002/cncr.26699. [DOI] [PubMed] [Google Scholar]
- 13.Macdougall ND, Dean C, Muirhead R. Stereotactic body radiotherapy in prostate cancer: is Rapidarc a better solution than Cyberknife? Clin Oncol (R Coll Radiol) 2013;26:4–9. doi: 10.1016/j.clon.2013.08.008. [DOI] [PubMed] [Google Scholar]
- 14.Lin YW, Lin KH, Ho HW, Lin HM, Lin LC, Lee SP, Chui CS. Treatment plan comparison between stereotactic body radiation therapy techniques for prostate cancer: non-isocentric CyberKnife versus isocentric RapidArc. Phys Med. 2014;30:654–661. doi: 10.1016/j.ejmp.2014.03.008. [DOI] [PubMed] [Google Scholar]
- 15.Dong P, Nguyen BS, Ruan D, King C, Long T, Romeijn E, Low DA, Kupelian P, Steinberg M, Yang Y, Sheng K. Feasibility of prostate robotic radiation therapy on conventional C-arm linacs. Pract Radiat Oncol. 2014;4:254–260. doi: 10.1016/j.prro.2013.10.009. [DOI] [PubMed] [Google Scholar]
- 16.Rossi L, Breedveld S, Aluwini S, Heijmen B. Noncoplanar beam angle class solutions to replace time-consuming patient-specific beam angle optimization in robotic prostate stereotactic body radiation therapy. Int J Radiat Oncol Biol Phys. 2014;92:762–770. doi: 10.1016/j.ijrobp.2015.03.013. [DOI] [PubMed] [Google Scholar]
- 17.Rossi L, Sharfo AW, Aluwini S, Dirkx M, Breedveld S, Heijmen B. First fully automated planning solution for robotic radiosurgery – comparison with automatically planned volumetric arc therapy for prostate cancer. Acta Oncol. 2018;57:1490–1498. doi: 10.1080/0284186X.2018.1479068. [DOI] [PubMed] [Google Scholar]
- 18.Network NCCN . Clinical practise guidelines for oncology, prostate cancer, version 01.2016. 2017. [Google Scholar]
- 19.Michalski JM, Gay H, Jackson A, Tucker SL, Deasy JO. Radiation dose-volume effects in radiation-induced rectal injury. Int J Radiat Oncol Biol Phys. 2010;76:123–129. doi: 10.1016/j.ijrobp.2009.03.078. [DOI] [PubMed] [Google Scholar]
- 20.Viswanathan AN, Yorke ED, Marks LB, Eifel PJ, Shipley WU. Radiation dose-volume effects of the urinary bladder. Int J Radiat Oncol Biol Phys. 2010;76:116–122. doi: 10.1016/j.ijrobp.2009.02.090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.ICRU, Report 83 . Prescribing, recording, and reporting intensity-modulated photon-beam. Bethesda: International Commission on Radiation Units and Measurements; 2010. [Google Scholar]
- 22.Boehmer D, Maingon P, Poortmans P, Baron MH, Miralbell R, Remouchamps V, Scrase C, Bossi A. Bolla M; EORTC radiation oncology group. Guidelines for primary radiotherapy of patients with prostate cancer. Radiother Oncol. 2006;79:259–269. doi: 10.1016/j.radonc.2006.05.012. [DOI] [PubMed] [Google Scholar]
- 23.Haverkamp U, Norkus D, Kriz J, Müller MM, Prott FJ, Eich HT. Optimization by visualization of indices. Strahlenther Onkol. 2014;190:1053–1059. doi: 10.1007/s00066-014-0688-z. [DOI] [PubMed] [Google Scholar]
- 24.Van't Riet A, Mak AC, Moerland MA, Elders LH, van der Zee W. A conformation number to quantify the degree of conformality in brachytherapy and external beam irradiation: application to the prostate. Int J Radiat Oncol Biol Phys. 1997;37:731–736. doi: 10.1016/S0360-3016(96)00601-3. [DOI] [PubMed] [Google Scholar]
- 25.ICRU, Report 62 . Prescribing, recording and reporting photon beam therapy (supplement to ICRU report 50) Bethesda: International Commission on Radiation Units and Measurements; 1999. [Google Scholar]
- 26.Van Gellekom MP, Moerland MA, Battermann JJ, Lagendijk JJ. MRI-guided prostate brachytherapy with single needle method--a planning study. Radiother Oncol. 2004;71:327–332. doi: 10.1016/j.radonc.2004.03.002. [DOI] [PubMed] [Google Scholar]
- 27.Das IJ, Cheng CW, Healey GA. Optimum field size and choice of isodose lines in electron beam treatment. Int J Radiat Oncol Biol Phys. 1995;31:157–163. doi: 10.1016/0360-3016(94)E0299-Y. [DOI] [PubMed] [Google Scholar]
- 28.Burman C, Kutcher GJ, Emami B, Goitein M. Fitting of normal tissue tolerance data to an analytic function. Int J Radiat Oncol Biol Phys. 1991;21:123–135. doi: 10.1016/0360-3016(91)90172-Z. [DOI] [PubMed] [Google Scholar]
- 29.Buyyounouski MK, Price RA, Jr, Harris EE, Miller R, Tomé W, Schefter T, Parsai EI, Konski AA, Wallner PE. Stereotactic body radiotherapy for primary management of early-stage, low- to intermediate-risk prostate cancer: report of the American Society for Therapeutic Radiology and Oncology Emerging Technology Committee. Int J Radiat Oncol Biol Phys. 2010;76:1297–1304. doi: 10.1016/j.ijrobp.2009.09.078. [DOI] [PubMed] [Google Scholar]
- 30.Dale E, Hellebust TP, Skjonsberg A, Hogberg T, Olsen DR. Modeling normal tissue complication probability from repetitive computed tomography scans during fractionated high-dose-rate brachytherapy and external beam radiotherapy of the uterine cervix. Int J Radiat Oncol Biol Phys. 2000;47:963–971. doi: 10.1016/S0360-3016(00)00510-1. [DOI] [PubMed] [Google Scholar]
- 31.Stavrev P, Hristov D. Prostate IMRT fractionation strategies: two-phase treatment versus simultaneous integrated boost. Radiol Oncol. 2003;37:115–126. [Google Scholar]
- 32.Boike TP, Lotan Y, Cho LC, Brindle J, DeRose P, Xie XJ, Yan J, Foster R, Pistenmaa D, Perkins A, Cooley S, Timmerman R. Phase I dose-escalation study of stereotactic body radiation therapy for low- and intermediate-risk prostate cancer. J Clin Oncol. 2011;29:2020–2026. doi: 10.1200/JCO.2010.31.4377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Madsen BL, His RA, Pham HT, Fowler JF, Esagui L, Corman J. Stereotactic hypofractionated accurate radiotherapy of the prostate (SHARP), 33.5 Gy in five fractions for localized disease: first clinical trial results. Int J Radiat Oncol Biol Phys. 2007;67:1099–1105. doi: 10.1016/j.ijrobp.2006.10.050. [DOI] [PubMed] [Google Scholar]
- 34.Aluwini S, van Rooij P, Hoogeman M, Bangma C, Kirkels WJ, Incrocci L, Kolkman-Deurloo IK. CyberKnife stereotactic radiotherapy as monotherapy for low- to intermediate-stage prostate cancer: early experience, feasibility, and tolerance. J Endourol. 2010;24:865–869. doi: 10.1089/end.2009.0438. [DOI] [PubMed] [Google Scholar]
- 35.Freeman DE, King CR. Stereotactic body radiotherapy for low-risk prostate cancer: five-year outcomes. Radiat Oncol. 2011;6:13. doi: 10.1186/1748-717X-6-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tang CI, Loblaw DA, Cheung P, Holden L, Morton G, Basran PS, Tirona R, Cardoso M, Pang G, Gardner S, Cesta A. Phase I/II study of a five-fraction hypofractionated accelerated radiotherapy treatment for low-risk localised prostate cancer: early results of pHART3. Clin Oncol. 2008;20:729–737. doi: 10.1016/j.clon.2008.08.006. [DOI] [PubMed] [Google Scholar]
- 37.Friedland JL, Freeman DE, Masterson-McGary ME, Spellberg DM. Stereotactic body radiotherapy: an emerging treatment approach for localized prostate cancer. Technol Cancer Res Treat. 2009;8:387–392. doi: 10.1177/153303460900800509. [DOI] [PubMed] [Google Scholar]
- 38.Katz AJ, Santoro M, Ashley R, Diblasio F, Witten M. Stereotactic body radiotherapy for organ-confined prostate cancer. BMC Urol. 2010;110:11. doi: 10.1186/1471-2490-10-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.van der Wielen GJ, Mutanga TF, Incrocci L, Kirkels WJ, Vasquez Osorio EM, Hoogeman MS, Heijmen BJ, de Boer HC. Deformation of prostate and seminal vesicles relative to intraprostatic fiducial markers. Int J Radiat Oncol Biol Phys. 2008;72:1604–1611. doi: 10.1016/j.ijrobp.2008.07.023. [DOI] [PubMed] [Google Scholar]
- 40.Nichol AM, Brock KK, Lockwood GA, Moseley DJ, Rosewall T, Warde PR, Catton CN, Jaffray DA. A magnetic resonance imaging study of prostate deformation relative to implanted gold fiducial markers. Int J Radiat Oncol Biol Phys. 2007;67:48–56. doi: 10.1016/j.ijrobp.2006.08.021. [DOI] [PubMed] [Google Scholar]
- 41.Reggiori G, Mancosu P, Tozzi A, Cantone MC, Castiglioni S, Lattuada P, Lobefalo F, Cozzi L, Fogliata A, Navarria P, Scorsetti M. Cone beam CT pre- and post-daily treatment for assessing geometrical and dosimetric intrafraction variability during radiotherapy of prostate cancer. J App Clin Med Phys. 2011;12:141–152. doi: 10.1120/jacmp.v12i1.3371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Soete G, Arcangeli S, De Meerleer G, Landoni V, Fonteyne V, Arcangeli G, De Neve W, Storme G. Phase II study of a four-week hypofractionated external beam radiotherapy regimen for prostate cancer: report on acute toxicity. Radiother Oncol. 2006;80:78–81. doi: 10.1016/j.radonc.2006.06.005. [DOI] [PubMed] [Google Scholar]
- 43.Martin JM, Rosewall T, Bayley A, Bristow R, Chung P, Crook J, Gospodarowicz M, McLean M, Ménard C, Milosevic M, Warde P, Catton C. Phase II trial of hypofractionated image-guided intensity-modulated radiotherapy for localized prostate adenocarcinoma. Int J Radiat Oncol Biol Phys. 2007;69:1084–1089. doi: 10.1016/j.ijrobp.2007.04.049. [DOI] [PubMed] [Google Scholar]
- 44.Kupelian P, Willoughby T, Mahadevan A, Djemil T, Weinstein G, Jani S, Enke C, Solberg T, Flores N, Liu D, Beyer D, Levine L. Multi-institutional clinical experience with the Calypso system in localization and continuous, real-time monitoring of the prostate gland during external radiotherapy. Int J Radiat Oncol Biol Phys. 2007;67:1088–1098. doi: 10.1016/j.ijrobp.2006.10.026. [DOI] [PubMed] [Google Scholar]
- 45.Wilder RB, Chittenden L, Mesa AV, Bunyapanasarn J, Agustin J, Lizarde J, Ravera J, Tokita KM. A prospective study of intrafraction prostate motion in the prone vs. supine position. Int J Radiat Oncol Biol Phys. 2010;77:165–170. doi: 10.1016/j.ijrobp.2009.04.041. [DOI] [PubMed] [Google Scholar]
- 46.Mutanga TF, de Boer HC, Rajan V, Dirkx ML, Incrocci L, Heijmen BJ. Day-to-day reproducibility of prostate intrafraction motion assessed by multiple kV and MV imaging of implanted markers during treatment. Int J Radiat Oncol Biol Phys. 2012;83:400–407. doi: 10.1016/j.ijrobp.2011.05.049. [DOI] [PubMed] [Google Scholar]
- 47.Rosewall T, Chung P, Bayley A, Lockwood G, Alasti H, Bristow R, Kong V, Milosevic M, Catton C. A randomized comparison of interfraction and intrafraction prostate motion with and without abdominal compression. Radiother Oncol. 2008;88:88–94. doi: 10.1016/j.radonc.2008.01.019. [DOI] [PubMed] [Google Scholar]
- 48.Kotte AN, Hofman P, Lagendijk JJ, van Vulpen M, van der Heide U. Intrafraction motion of the prostate during external-beam radiation therapy: analysis of 427 patients with implanted fiducial markers. Int J Radiat Oncol Biol Phys. 2007;69:419–425. doi: 10.1016/j.ijrobp.2007.03.029. [DOI] [PubMed] [Google Scholar]
- 49.Aubry JF, Beaulieu L, Girouard LM, Aubin S, Tremblay D, Laverdière J, Vigneault E. Measurements of intrafraction motion and interfraction and intrafraction rotation of prostate by three-dimensional analysis of daily portal imaging with radiopaque markers. Int J Radiat Oncol Biol Phys. 2004;60:30–39. doi: 10.1016/j.ijrobp.2004.02.045. [DOI] [PubMed] [Google Scholar]
- 50.Pontoriero A, Iatì G, Mondello S, Midili F, Siragusa C, Brogna A, Ielo I, Anastasi G, Magno C, Pergolizzi S, De Renzis C. High-Dose Robotic Stereotactic Body Radiotherapy in the Treatment of Patients With Prostate Cancer: Preliminary Results in 26 Patients. Technol Cancer Res Treat. 2016;15:179–185. doi: 10.1177/1533034614566994. [DOI] [PubMed] [Google Scholar]
- 51.Lee SW, Jang HS, Lee JH, Kim SH, Yoon SC. Stereotactic body radiation therapy for prostate cancer patients with old age or medical comorbidity: a 5-year follow-up of an investigational study. Medicine (Baltimore) 2014;93:e290. doi: 10.1097/MD.0000000000000290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Jiang P, Krockenberger K, Vonthein R, Tereszczuk J, Schreiber A, Liebau S, Huttenlocher S, Imhoff D, Balermpas P, Keller C, Dellas K, Baumann R, Rödel C, Hildebrandt G, Jünemann KP, Merseburger AS, Katz A, Ziegler A, Blanck O, Dunst J. Hypo-fractionated SBRT for localized prostate cancer: a German bi-center single treatment group feasibility trial. Radiat Oncol. 2017;12:138. doi: 10.1186/s13014-017-0872-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Nielsen TB, Wieslander E, Fogliata A, Nielsen M, Hansen O, Brink C. Influence of dose calculation algorithms on the predicted dose distributions and NTCP values for NSCLC patients. Med Phys. 2011;38:2412–2418. doi: 10.1118/1.3575418. [DOI] [PubMed] [Google Scholar]
- 54.Hedin E, Bäck A. Influence of different dose calculation algorithms on the estimate of NTCP for lung complications. J Appl Clin Med Phys. 2013;14:127–139. doi: 10.1120/jacmp.v14i5.4316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Liang X, Penagaricano J, Zheng D, Morrill S, Zhang X, Corry P, Griffin RJ, Han EY, Hardee M, Ratanatharathom V. Radiobiological impact of dose calculation algorithms on biologically optimized IMRT lung stereotactic body radiation therapy plans. Radiat Oncol. 2016;11:10. doi: 10.1186/s13014-015-0578-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Variables for patients’ population. (DOCX 12 kb)
Data Availability Statement
The datasets supporting the conclusions of this article are available in the repository of the Department of Radiotherapy and Radiooncology, University Hospital of Muenster.