Abstract
Background & Aims:
Estimates of disease burden can inform national health priorities for research, clinical care, and policy. We aimed to estimate health care use and spending among gastrointestinal (GI) (including luminal, liver, and pancreatic) diseases in the United States.
Methods:
We estimated health care use and spending based on the most currently available administrative claims from commercial and Medicare Supplemental plans, data from the GI Quality Improvement Consortium Registry, and national databases.
Results:
In 2015, annual health care expenditures for gastrointestinal diseases totaled $135.9 billion. Hepatitis ($23.3 billion), esophageal disorders ($18.1 billion), biliary tract disease ($10.3 billion), abdominal pain ($10.2 billion), and inflammatory bowel disease ($7.2 billion) were the most expensive. Yearly, there were more than 54.4 million ambulatory visits with a primary diagnosis for a GI disease, 3.0 million hospital admissions, and 540,500 all-cause 30-day readmissions. There were 266,600 new cases of GI cancers diagnosed and 144,300 cancer deaths. Each year, there were 97,700 deaths from non-malignant GI diseases. An estimated 11.0 million colonoscopies, 6.1 million upper endoscopies, 313,000 flexible sigmoidoscopies, 178,400 upper endoscopic ultrasound examinations, and 169,500 endoscopic retrograde cholangiopancreatography procedures were performed annually. Among average-risk persons ages 50–75 years who underwent colonoscopy, 34.6% had 1 or more adenomatous polyps, 4.7% had 1 or more advanced adenomatous polyps, and 5.7% had 1 or more serrated polyps removed.
Conclusions:
GI diseases contribute substantially to health care use in the United States. Total expenditures for GI diseases are $135.9 billion dollars annually—greater than for other common diseases. Expenditures are likely to continue increasing.
Keywords: health care costs, endoscopy, digestive system diseases, neoplasms
Introduction
Gastrointestinal (GI) diseases account for considerable health care utilization and spending. We provide an updated and expanded report1 detailing select estimates of disease incidence and prevalence, health care utilization and spending across GI diseases (including luminal, liver, and pancreatic) in the United States.
To achieve this objective, we used multiple data sources to generate summary statistics on office-based and emergency department (ED) visits, hospitalizations including readmissions, cancer, and mortality. We have included estimates of the prevalence of chronic hepatitis C virus (HCV) to highlight recent and clinically important trends. Because GI endoscopic procedures are responsible for considerable costs and effort, we report an estimate of the annual number of endoscopies by procedure as well as selected pathology (adenomatous polyps, advanced adenomatous polyps, serrated polyps, and adenocarcinoma). We have estimated health care expenditures for GI diseases and summarized funding for GI diseases research from the National Institutes of Health.
Methods
Symptoms and Diagnoses across Ambulatory Settings
We used the 2014 National Ambulatory Medical Care Survey (NAMCS) to tabulate the leading GI symptoms and diagnoses in the United States for office-based outpatient visits. We used the National Hospital Ambulatory Medical Care Survey (NHAMCS) for ED visits for 2014. NHAMCS collects data on the utilization of ambulatory care services in hospital EDs, regardless of outcome (discharge from the ED, hospital admission, transfer or death). NAMCS and NHAMCS are annual national surveys sponsored by the US Centers for Disease Control and Prevention (CDC) (http://www.cdc.gov/nchs/ahcd.htm). The NAMCS surveys non-federal employed office-based physicians or non-physician clinicians who are primarily engaged in direct patient care. The NHAMCS collects data on visits to ED and hospital-based outpatient visits exclusive of Federal, military, and Veterans Administration hospitals. We downloaded public use data files from the CDC website to perform our analyses.
Patient-reported symptoms are available in both NAMCS and NHAMCS. We used the patient’s self-reported most important complaint for our analyses. We combined related symptoms (supplemental tables), and we totaled data from office and ED visits to present the top 10 most common GI symptoms. We categorized physician and non-physician clinician diagnoses into relevant disease categories based on clinical expertise using International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) (supplemental tables). We used the primary diagnosis code only. After combining the related diagnoses, we created a rank order list. NAMCS and NHAMCS are based on probability samples. Therefore, sampling weights were applied to all analyses in order to generate national estimates. When there are fewer than 30 observations for a specific condition, estimates are unreliable and should be interpreted with caution. Unreliable estimates are clearly labeled in the tables with footnotes. Both analyses include children and adults. These analyses were conducted using SAS version 9.4 (Cary, NC).
Emergency Department Visits
The most common ED GI diagnoses were compiled from the Nationwide Emergency Department Sample (NEDS), one of the databases in the Healthcare Cost and Utilization Project (HCUP) (https://hcupnet.ahrq.gov). The NEDS was constructed using the HCUP State Emergency Department Databases (SEDD) and the State Inpatient Databases (SID). The SEDD captures discharge information on ED visits that do not result in an admission, and SID has information on patients initially seen in the ED and then admitted to the same hospital. NEDS is the largest all-payer ED database that is publicly available in the United States. The 2014 NEDS contains information from 31 million ED visits at 945 hospitals participating in HCUP across 33 states and the District of Columbia, approximating a 20-percent stratified sample of U.S. The weighted national estimates pertain to 138 million ED visits in 2014. The NEDS sampling frame includes discharge information on patients admitted to the hospital from EDs, patients treated and released from EDs, and patients transferred to another hospital from an ED.
We queried the database for the rank order of the principal visit diagnosis (i.e., ICD-9-CM) from the ED for all patients in all hospitals. From the top 100 diagnoses, we identified the GI diagnoses, which were subsequently rank-ordered after combining related diagnosis codes. Weighted national estimates for visits in 2014 were generated. Diagnosis categories and associated codes (supplemental tables) were determined using previously published GI coding categories1–5, and modified for accuracy and relevance with the input of multiple gastroenterology subspecialists. We calculated the percent change in the number of visits between the year 2006 (first year of NEDS) and 2014. We then performed a separate query for each individual ICD-9-CM code (or group of codes) to generate estimates of the total number of visits, rate of visits per 100,000 people, patients admitted to the same hospital from the ED with that diagnosis, and percent deaths either in the hospital or the ED.
Hospitalizations
The most common inpatient GI discharge diagnoses were compiled from the National Inpatient Sample (NIS), a publically available dataset part of HCUP (http://hcup.ahrq.gov/hcupnet.jsp). The 2014 NIS contains a 20 percent sample of discharges from 4,411 community hospitals participating in HCUP across 44 states. The sampling frame for the 2014 NIS comprises over 96 percent of the U.S. population and includes more than 94 percent of discharges from U.S. community hospitals. The NIS is the only national hospital database containing charge information on all patients, regardless of payer, including persons covered by Medicare, Medicaid, private insurance, and the uninsured.
We queried the database for the rank order of the principal discharge diagnosis (i.e., ICD-9-CM) for all patients in all hospitals. From the top 100 diagnoses, we identified the GI diagnoses, which were subsequently rank-ordered after combining related diagnosis codes. Weighted national estimates for visits in 2014 were generated. We then performed a separate query for each individual ICD-9-CM code (or group of codes) to obtain estimates of the mean and median length of stay (LOS), median charges and costs, aggregate charges (i.e. “the national bill”) and aggregate costs, and number of inpatient deaths associated with each diagnosis or diagnosis group. We calculated the percent change in the number of admissions between the year 2005 and 2014 and performed temporal analyses for the principal diagnoses with the greatest change in number of admissions. The 2014 version of NIS (the last full calendar year of ICD-9-CM coding) was used for this analysis to facilitate measurement of trends.
Diagnosis categories and associated codes (supplemental tables) were determined using previously published GI coding categories1–5, as described above. The total LOS was estimated by the product of the mean LOS and the number of discharges for each diagnosis. Total charges were converted to costs by HCUP using cost-to-charge ratios based on hospital accounting reports from the Centers for Medicare and Medicaid Services (CMS). Cost data are presented preferentially, as costs tend to reflect the actual costs of production, while charges represent what the hospital billed for the case.
Readmissions
Common and select GI readmissions were compiled from the 2015 Nationwide Readmissions Database (NRD), a resource of HCUP State Inpatient Databases. The NRD is a publicly available all-payer inpatient database from the United States that includes data from 14,208,678 admissions across 27 states. Using individual linkage identifiers within a state, the NRD is designed to be nationally-representative of readmission rates for all payers and the uninsured.
We identified all patients with an ICD-9-CM or ICD, 10th Revision (ICD-10-CM) code for the most common inpatient GI discharge diagnoses in the NRD. From January 1, 2015 through September 31, 2015, ICD-9-CM codes were utilized by HCUP in the NRD. Beginning on October 1, 2015, ICD-10-CM coding was used to categorize diagnoses. Any patient with an ICD-9-CM or ICD-10-CM diagnosis code as a primary diagnosis on the index admission was eligible for inclusion in this study. Diagnosis categories and associated codes (supplemental tables) were determined using previously published GI coding categories.1−5
We included patients age 18 years and older with a full 30 days between the date of discharge from their index admission and December 31, 2015. We excluded patients with an index hospitalization that ended in death or transfer to another acute care faculty. The primary outcome of interest was the first all-cause readmission within 30 days of the index hospitalization. Weighted national estimates for visits in 2015 were generated. We calculated the total charges associated with both the index admission and the first readmission. There is no cost-to-charge ratio available from HCUP for the 2015 NRD data, therefore only total charges are reported. These analyses were conducted using survey procedures in SAS version 9.4 (Cary, NC) to account for the complex survey design.
Hepatitis C Virus Infection
We estimated the prevalence of chronic HCV in the United States between 2009–2016 using cross-sectional data from The National Health and Nutrition Examination Survey (NHANES) (https://www.cdc.gov/nchs/nhanes/index.htm). The NHANES is a nationally representative household survey designed to assess the health and nutritional status of adults and children in the United States. NHANES is a major program of the National Center for Health Statistics (NCHS). Data from NHANES has been used previously to estimate the prevalence of HCV in the United States.6–8 The survey examines a nationally representative sample of approximately 5,000 noninstitutionalized persons each year and includes demographic, socioeconomic, and health-related questions. The examination component consists of medical, dental, and physiological measurements, as well as laboratory tests. Serum samples were tested for HCV antibody. Serum samples positive or indeterminate for anti-HCV were tested for HCV RNA. Prevalence was calculated as confirmed HCV cases (RNA positive) divided by the total population at risk (sum of HCV antibody testing including positive, negative, and indeterminate cases) as in prior prevalence studies with NHANES. These analyses were conducted using SAS version 9.4 (Cary, NC).
Cancer Incidence and Mortality
We estimated age-adjusted (2000 U.S. standard population) incidence of and mortality from GI cancers among adults (age ≥20 years) using data from the United States Cancer Statistics (USCS) in 2014 (www.cdc.gov/uscs). USCS collects data on incidence from state cancer registries, in collaboration with the National Program of Cancer Registries and the Surveillance, Epidemiology, and End Results program. Information on cancer deaths comes from death certificates collected by the National Vital Statistics System at the National Center of Health Statistics. To further illustrate time trends, we plotted incidence and mortality rates (per 100,000 persons) of colorectal cancer by 10-year age group over the period 2000 – 2014.
Non-Cancer Mortality
We generated a list of the most common non-malignant GI causes of death using data from the Centers for Disease Control Wide-ranging Online Data for Epidemiologic Research (CDC WONDER) (http://wonder.cdc.gov). CDC WONDER is a publically available database provided by the Centers for Disease Controls. The CDC reports national mortality of children and adults collected and reported by state registries. The causes of death are derived from death certificates and are classified using the ICD-10 system. The underlying cause of death is defined as the disease that initiated the sequence of morbid events leading directly to death. Contributing cause of death statistics include all deaths with the disease of interest as either the underlying cause or any of 20 additional diseases leading to death.
To perform our analyses, we downloaded the 2016 public use data files for underlying cause of death and multiple cause of death from the CDC website. Using ICD-10 codes (supplemental tables), the 15 most common non-malignant GI causes of death were ranked. Diagnoses were combined to create clinically meaningful categories. The crude rate per 100,000 deaths was calculated by dividing the number of deaths listed as an underlying cause by the total U.S. population in the United States in 2016 (323,127,513 from the U.S. Census Bureau) then multiplying by 100,000. Results include children and adults.
Endoscopy Use and Trends
Using MarketScan Commercial Claims and Encounters data (Truven Health Analytics, Ann Arbor, MI) and a 5% random sample of all Medicare beneficiaries with at least one month of Part A (hospital) and B (outpatient) coverage (excluding HMO plans), we examined patterns of endoscopy use in adults between 2002 and 2013. We looked at temporal trends in upper endoscopy, colonoscopy, flexible sigmoidoscopy, endoscopic retrograde cholangiopancreatography (ERCP) and upper and lower endoscopic ultrasound (EUS). MarketScan is a large, employer-based claims database that includes 77 contributing employers and 12 contributing health plans, with 126 unique carriers and 8 Medicaid states representing approximately 165 million covered lives. Medicare provides public insurance to over 98% of older US adults and approximately 75% have coverage with Parts A and B. We summed the total number of months individuals aged 18–64 years (MarketScan) and > 65 years (Medicare) were enrolled in their insurance plan in each calendar year as standardized denominators of “enrollee-time.” We then depicted time trends by calculating a rate of the procedure per 1,000 enrollee-years in each calendar year, assuming constant rates within each calendar year. We examined rates by age group (18–29, 30–39, 40–49, 50–64, 65–74 and ≥75 years). We estimated the number of procedures performed in the United States in 2013 by standardizing the number of procedures in each database to 2013 United States Census Bureau data (within age categories). These analyses were conducted using SAS version 9.4 (Cary, NC).
Endoscopy Safety, Quality and Findings
Using 2014–2016 data from the GI Quality Improvement Consortium (GIQuIC) Registry, we report select findings and quality measures for upper endoscopy and colonoscopy. The GIQuIC Registry is a gastrointestinal endoscopy quality improvement registry that is a joint collaboration of the American College of Gastroenterology and the American Society for Gastrointestinal Endoscopy. GIQuIC was established in 2010 and is a voluntary nationwide registry. Participating sites submit patient and procedural data using standardized data elements. During the study period, 538 sites contributed colonoscopy data and 232 sites contributed upper endoscopy data (supplemental tables).
The GIQuIC Registry captures patient demographics, procedure details (indication for procedure, immediate adverse events), and post-procedure details (documentation of discharge instructions, pathology results, recommended follow-up interval) for both colonoscopy and upper endoscopy procedures. For colonoscopy reports, procedure type (screening, surveillance, or diagnostic), colorectal neoplasm risk assessment (average or high-risk), photo documentation of the cecum, bowel preparation adequacy, and cecal insertion/withdrawal times are also collected.
Data for all colonoscopy procedures performed at the site are required to be submitted to the registry. Contribution of upper endoscopy records is optional, but for those practices who do opt in for such reporting, they must submit data from all upper endoscopy procedures. For research purposes, data from GIQuIC is de-identified and stored in a research database that is maintained on a separate server from the overall registry.
We estimated the rates of immediate adverse events for upper endoscopy and colonoscopy. We report the percentage of colonoscopies with an adequate bowel preparation, documented cecal landmarks and average withdrawal time. We have estimated the prevalence of adenomatous polyps, advanced adenomatous polyps, serrated polyps, and adenocarcinoma among average risk persons having a screening colonoscopy by age, sex and race. We also report overall colonoscopy polyp pathology in the total population and screening population. These analyses were conducted using SAS version 9.4 (Cary, NC).
Expenditures
We estimated total expenditures and distribution of expenditures for GI diseases and symptoms using data from the 2015 Medical Expenditure Panel Survey (MEPS) (https://meps.ahrq.gov/). The MEPS is a set of large-scale surveys of families and individuals, their medical providers (doctors, hospitals, pharmacies, etc.), and employers across the United States. MEPS collects data on the use of specific health services, how frequently they are used, the cost of these services, and how they are paid for. These surveys are designed to collect data from a nationally representative sample of households in the United States and reports detailing health care expenses in the United States are routinely published.9, 10 In the 2015 MEPS Household Component, 33,983 persons from 13,800 families were surveyed. This survey represents the civilian noninstitutionalized population. All GI diseases and symptoms available in MEPS were pulled for this analysis (supplemental tables). The condition categories are defined using the Clinical Classification Software (CCS), which is a tool, developed by Agency for Healthcare Research and Quality for clustering diagnoses into a manageable number of clinically meaningful policy-relevant categories. All estimates were weighted by the MEPS person-level weight (PERWT08F) to produce national estimates of expenditures. These analyses were conducted using SAS version 9.4 (Cary, NC).
We estimated total expenditures by prescribed acid suppressing drug using data from the 2001–2015 MEPS household component summary tables (https://meps.ahrq.gov/mepstrends/home/index.html).11 The estimates are for prescribed drugs obtained by household members and do not include drugs administered in hospitals or provider offices. These estimates represent persons in the United States civilian non-institutionalized population.
National Institutes of Health Categorical Spending
We collected estimates of grants, contracts, and other funding mechanisms used across the National Institutes of Health (NIH) for select research, condition, and disease categories for 2013–2018 (https://report.nih.gov/categorical_spending.aspx). Actual expenditures are reported when available, otherwise the values were estimated. Categories specific to GI diseases were selected from 282 total research/disease areas. The research categories are not mutually exclusive. Individual research projects could be included in multiple categories.
Results
Symptoms and Diagnoses across Ambulatory Settings
Using weighted national data, in 2014 there were more than 40.7 million ambulatory visits in the United States for GI symptoms (Table 1) and 54.4 million ambulatory visits with a primary diagnosis code for a GI disease (Table 2). The symptom of abdominal pain was responsible for more than 21.8 million total visits, followed by vomiting (4.7 million visits) and diarrhea (3.4 million visits) (Table 1). Abdominal pain was also the most frequent diagnosis (Table 2) with 16.5 million annual visits. There were more than 5.6 million visits for gastroesophageal reflux disease and reflux esophagitis. Constipation and hemorrhoids each accounted for 2.5 million visits.
Table 1.
Leading Gastrointestinal Symptoms Prompting an Ambulatory Visit in the United States, 2014
| Estimated number of annual visits | ||||
|---|---|---|---|---|
| Rank | Symptoms | Office visits | Emergency Department | Total |
| 1 | Abdominal pain | 10,705,448 | 11,135,099 | 21,840,547 |
| 2 | Vomiting | 1,725,616 | 2,936,210 | 4,661,826 |
| 3 | Diarrhea | 2,423,825 | 994,454 | 3,418,279 |
| 4 | Nausea | 1,063,883 | 2,004,732 | 3,068,615 |
| 5 | Bleeding | 2,147,949 | 606,970 | 2,754,919 |
| 6 | Constipation | 1,086,452 | 511,317 | 1,597,769 |
| 7 | Anorectal symptomsa | 928,119 | 220,585 | 1,148,704 |
| 8 | Heartburn and indigestiona | 878,808 | 63,485 | 942,293 |
| 9 | Decreased appetitea,b | 564,112 | 94,685 | 658,797 |
| 10 | Dysphagiaa | 537,975 | 88,731 | 626,706 |
| Total | 40,718,455 | |||
Source: The 2014 National Ambulatory Medical Care Survey (NAMCS) and the National Hospital Ambulatory Medical Care Survey (NHAMCS), Emergency Department only (https://www.cdc.gov/nchs/ahcd/index.htm)
Denotes category reported from the NHAMCS (Emergency Department only) with <30 observations that should be interpreted with caution
Denotes category reported from the NAMCS with <30 observations that should be interpreted with caution
Table 2.
Leading Physician Diagnoses in the Ambulatory Setting for Gastrointestinal, Liver and Pancreatic Disorders in the United States, 2014
| Estimated number of annual visits | |||
|---|---|---|---|
| Diagnosis | Office Visits | Emergency Department | Total |
| Abdominal pain | 8,565,933 | 7,906,926 | 16,472,859 |
| Gastroesophageal reflux disease/reflux esophagitis | 5,235,107 | 325,666 | 5,560,773 |
| Nausea and vomiting | 1,935,544 | 2,943,220 | 4,878,764 |
| Diarrhea | 2,173,179 | 800,794 | 2,973,973 |
| Gastritis and dyspepsia | 2,398,740 | 462,065 | 2,860,805 |
| Abdominal wall and inguinal hernia | 2,548,881 | 236,684 | 2,785,565 |
| Constipation | 1,746,404 | 771,058 | 2,517,462 |
| Hemorrhoids | 2,237,642 | 246,623 | 2,484,265 |
| Diverticular disease of the colon | 1,748,508 | 172,462 | 1,920,970 |
| Malignant neoplasm of the colon or rectuma | 1,621,053 | 28,852 | 1,649,905 |
| Cholelithiasis | 1,126,944 | 466,832 | 1,593,776 |
| Lower gastrointestinal hemorrhage | 1,269,312 | 191,724 | 1,461,036 |
| Chronic liver disease and cirrhosisa | 1,003,102 | 41,934 | 1,045,036 |
| Ulcerative colitisa | 935,150 | 21,953 | 957,103 |
| Dysphagiaa | 861,769 | 43,172 | 904,941 |
| Pancreatitis - acute and chronicb | 562,048 | 195,113 | 757,161 |
| Appendicitisb | 523,524 | 212,046 | 735,570 |
| Hepatitis C infectiona | 709,338 | 3,643 | 712,981 |
| Crohn’s diseasea | 642,547 | 42,399 | 684,946 |
| Irritable bowel syndromea | 585,061 | 18,638 | 603,699 |
| Benign neoplasm of colon and rectuma, b | 332,191 | - | 332,191 |
| Barrett’s esophagusa | 274,482 | - | 274,482 |
| Celiac diseasea, b | 190,381 | - | 190,381 |
| Hepatitis, unspecifieda, b | 24,088 | 9,775 | 33,863 |
| Total | 54,392,507 | ||
Source: The 2014 National Ambulatory Medical Care Survey (NAMCS) and the National Hospital Ambulatory Medical Care Survey (NHAMCS), Emergency Department only (https://www.cdc.gov/nchs/ahcd/index.htm)
Denotes category reported from the NHAMCS (Emergency Department only) with <30 observations that should be interpreted with caution
Denotes category reported from the NAMCS with <30 observations that should be interpreted with caution
Emergency Department Visits
In 2014, there were more than 15.7 million emergency department visits in the United States with a principal diagnosis code for a GI disease (Table 3). Abdominal pain (6.0 million), nausea/vomiting (2.1 million) and noninfectious gastroenteritis/colitis (1.2 million) were the most common diagnoses in the emergency department. Of the 18 listed diagnoses, the numbers of visits for 16 of the diagnoses have increased in the last 10 years. HCV, constipation, and inflammatory bowel disease had the largest increase in number of visits compared to 2006. Among the most common principal GI diagnoses, liver diseases had the highest mortality at 3.1% overall.
Table 3.
Most Common Gastrointestinal, Liver and Pancreatic Principal Diagnoses From Emergency Department Visits, 2014a
| Rank | Principal diagnosisb | Annual # visits | % change from 2006 | Rate of visits per 100,000 persons | Admitted to hospital with principal diagnosis N (%) | ED or hospital deaths N (%)c |
|---|---|---|---|---|---|---|
| 1 | Abdominal pain | 5,981,182 | +32% | 1,876 | 104,842 (1.8) | 230 (0.004) |
| 2 | Nausea and vomiting | 2,062,444 | +44% | 647 | 30,236 (1.5) | 195 (0.01) |
| 3 | Noninfectious gastroenteritis/colitis | 1,234,264 | −22% | 387 | 111,441 (9.0) | 332 (0.03) |
| 4 | Constipation | 882,235 | +78% | 276.7 | 47,757 (5.4) | 408 (0.05) |
| 5 | Gastrointestinal hemorrhage | 844,451 | +17% | 264.8 | 456,935 (54.1) | 10,007 (1.2) |
| Lowerd | 367,881 | +25% | 115.4 | 144,401 (39.3) | 1,923 (0.5) | |
| Upperd | 231,567 | −4% | 72.6 | 181,603 (78.4) | 3,739 (1.6) | |
| 6 | Cholelithiasis and cholecystitis | 664,977 | +34% | 208.6 | 293,408 (44.1) | 1,137 (0.2) |
| 7 | Gastritis/duodenitis | 623,768 | +21% | 195.6 | 58,123 (9.3) | 81 (0.01) |
| 8 | Diarrhea | 599,122 | +43% | 187.9 | 19,668 (3.3) | 173 (0.03) |
| 9 | Gastrointestinal infectione | 474,341 | +9% | 148.8 | 188,570 (39.8) | 1,876 (0.4) |
| 10 | Pancreatitis | 390,940 | +18% | 122.6 | 255,966 (65.5) | 1,584 (0.4) |
| Acute | 351,526 | +18% | 110.2 | 246,023 (70.0) | 1,571 (0.5) | |
| Chronic | 39,413 | +12% | 12.4 | 9,944 (25.3) | 13 (0.03) | |
| 11 | Diverticulitis | 371,742 | +45% | 116.6 | 159,966 (43.0) | 674 (0.2) |
| 12 | Appendicitis | 344,744 | +4% | 108.1 | 181,877 (52.8) | 181 (0.05) |
| 14 | Liver disease/viral hepatitis | 325,643 | +40% | 102.1 | 204,511 (62.8) | 10,110 (3.1) |
| Alcoholic liver disease | 70,009 | +7% | 22.0 | 55,692 (79.6) | 2,544 (3.6) | |
| Ascites or SBP | 58,950 | +128%g | 18.5 | 12,651 (21.5) | 470 (0.8) | |
| Hepatic encephalopathyf | 57,578 | +35% | 18.1 | 49,079 (85.2) | 2,258 (3.9) | |
| Hepatitis C | 34,922 | +190% | 11.0 | 28,073 (80.4) | 1153 (3.3) | |
| Acute liver failure | 11,054 | +32% | 3.5 | 7,731 (69.9) | 994 (9.0) | |
| Hepatitis B | 4,662 | +34% | 1.5 | 3,807 (81.7) | 174 (3.7) | |
| 15 | Gastroesophageal reflux | 316,695 | +2% | 99.3 | 30,147 (9.5) | 52 (0.02) |
| 16 | GI disorders during pregnancy | 287,644 | +35% | 90.2 | 12,229 (4.3) | NE |
| 17 | Foreign body in GI tract | 182,353 | +17% | 57.2 | 11,972 (6.6) | 69 (0.04) |
| 18 | Inflammatory bowel disease | 137,946 | +52% | 43.3 | 73,637 (53.4) | 217 (0.2) |
| Crohn’s disease | 93,277 | +48% | 29.3 | 45,888 (49.2) | 72 (0.08) | |
| Ulcerative colitis | 44,669 | +60% | 14.0 | 27,749 (62.1) | 146 (0.3) | |
| Total | 15,724,491 | |||||
Source: Healthcare Cost and Utilization Project Nationwide Emergency Department Sample (NEDS) (https://hcupnet.ahrq.gov)
Weighted national estimates from HCUP Nationwide Emergency Department Sample (NEDS) 2014 and 2006, Agency for Healthcare Research and Quality (AHRQ)
See supplementary table for specific groupings of ICD-9 CM codes for each category
Includes deaths in ED and in hospital deaths for patients admitted from ED with corresponding diagnoses
The code “Gastrointestinal hemorrhage NOS” (578.9) was included in the overall GI bleeding category but was not included in subcategories of upper and lower GI bleeding, because it is nonspecific.
Includes Salmonella, Shigella, E.coli, and other viral, bacterial, and parasitic GI infections. Also includes Clostridium difficile infections
Category may not include encephalopathy associated with viral hepatitis
Part of measured increase since 2006 may be due to coding change in 2007 for ascites
ICD-9-CM: International Classification of Diseases, 9th edition, Clinical Modification; SBP: spontaneous bacterial peritonitis; NE: no estimate due to few data
Hospitalizations
In 2014, there were more than 3.0 million hospital admissions in the United States with a principal diagnosis code for a GI disease at a cost of $30.6 billion dollars (Table 4). GI hemorrhage, gallbladder disease, and pancreatitis were the most common GI discharge diagnoses overall. The combined cost of these 3 diagnostic categories was nearly $12 billion dollars. GI hemorrhage alone was responsible for over 500 thousand hospitalizations, 2.2 million days of hospitalization, $5 billion dollars in direct costs, and nearly 11 thousand deaths. Chronic liver disease had the highest inpatient mortality (5.6%) with over 14 thousand annual hospital deaths. Colorectal cancer was ranked ninth overall in hospitalizations, and was associated with the highest median costs ($16,904 per hospitalization) and the second highest inpatient mortality (3%) among included conditions.
Table 4.
Most Common Gastrointestinal, Liver and Pancreatic Principal Diagnoses in US Hospitals, 2014a
| Rank | Principal diagnosesb | Annual # admissions | % ∆ from 2005 | Median LOS (days) | Total hospital days)c | Median costs (USD) | Aggregate charges (USD) “National bill” | Aggregate cost (USD) | In hospital deaths n (%) |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Gastrointestinal hemorrhage | 512,925 | ‒0.1% | 3.0 | 2,205,578 | 6,901 | 19,202,312,421 | 4,992,811,950 | 10,930 (2.1) |
| Upperd | 203,460 | ‒18% | 3.0 | 895,224 | 7,413 | 2,143,858,020 | 4,100 (2.0) | 4,100 (2.0) | |
| Lowerd | 161,540 | +2% | 3.0 | 678,468 | 6,376 | 1,488,914,180 | 2,280 (1.4) | 2,280 (1.4) | |
| 2 | Cholelithiasis and cholecystitis | 347,985 | ‒13% | 3.0 | 1,322,343 | 9,609 | 16,334,942,913 | 4,083,951,960 | 1,445 (0.4) |
| 3 | Pancreatitis | 291,915 | +10% | 3.0 | 1,342,809 | 6,240 | 10,486,824,627 | 2,772,024,840 | 1,855 (0.6) |
| Acute | 279,145 | +15% | 3.0 | 1,284,067 | 6,240 | 2,640,588,806 | 1,840 (0.7) | 1,840 (0.7) | |
| Chronic | 12,770 | ‒42% | 3.0 | 62,573 | 6,202 | 133,586,970 | NE | NE | |
| 4 | Intestinal obstruction | 266,465 | +33% | 3.0 | 1,465,558 | 5,273 | 11,066,475,706 | 2,943,372,390 | 4,225 (1.6) |
| 5 | Liver disease/viral hepatitis | 251,790 | +25% | 4.0 | 1,435,203 | 6,354 | 13,629,085,670 | 3,545,958,570 | 14,130 (5.6) |
| Alcoholic liver disease | 64,565 | ‒2% | 4.0 | 380,934 | 8,552 | 924,829,060 | 3,420 (5.3) | 3,420 (5.3) | |
| Hepatic encephalopathye | 55,485 | +33% | 4.0 | 305,168 | 6,354 | 619,490,025 | 3,010 (5.4) | 3,010 (5.4) | |
| Hepatitis C | 33,940 | +250% | 4.0 | 186,670 | 7,388 | 500,920,460 | 1,715 (5.1) | 1,715 (5.1) | |
| Ascites or SBP | 16,155 | +134%h | 3.0 | 82,391 | 6,073 | 177,801,930 | 595 (3.7) | 595 (3.7) | |
| Acute liver failure | 10,245 | +57% | 4.0 | 69,666 | 9,005 | 205,811,805 | 1405 (13.7) | 1405 (13.7) | |
| Hepatitis B | 4,720 | +51% | 3.0 | 24,072 | 5,134 | 53,841,040 | 210 (4.5) | 210 (4.5) | |
| 6 | Diverticulitis | 208,015 | +7% | 4.0 | 977,671 | 6,406 | 8,052,870,324 | 2,132,777,795 | 785 (0.4) |
| 7 | Appendicitis | 195,330 | ‒35% | 1.0 | 585,990 | 7,724 | 7,892,884,821 | 2,036,901,240 | 215 (0.1) |
| 8 | Obesity | 151,400 | +32% | 2.0 | 302,800 | 11,049 | 7,404,847,404 | 1,866,913,400 | 75 (0.05) |
| 9 | Colorectal cancer | 128,385 | ‒14% | 6.0 | 975,726 | 16,904 | 9,858,093,695 | 2,590,809,300 | 3,910 (3.0) |
| 10 | Noninfectious gastroenteritis/colitis | 118,825 | ‒20% | 3.0 | 380,240 | 5,007 | 2,915,143,399 | 744,082,150 | 300 (0.3) |
| 11 | Abdominal pain | 116,680 | ‒40% | 2.0 | 338,372 | 4,794 | 2,845,489,883 | 723,416,000 | 410 (0.4) |
| 12 | Clostridium difficile infection | 107,760 | +46% | 4.0 | 625,008 | 6,675 | 3,873,484,119 | 1,003,784,400 | 1,800 (1.7) |
| 13 | Functional/motility disordersf | 106,695 | +2% | 2.0 | 405,441 | 4,433 | 3,121,346,077 | 22,618,450 | 455 (0.4) |
| 14 | Gastrointestinal infectiong | 106,490 | ‒7% | 2.0 | 330,119 | 4,305 | 2,415,213,189 | 52,357,740 | 235 (0.2) |
| 15 | Inflammatory bowel diseases | 99,370 | +13% | 3.0 | 526,661 | 5,782 | 4,063,858,790 | 1,082,238,670 | 275 (0.3) |
| Crohn’s disease | 61,805 | +13% | 3.0 | 302,845 | 5,782 | 631,647,100 | 130 (0.2) | 130 (0.2) | |
| Ulcerative colitis | 37,565 | +14% | 4.0 | 217,877 | 7,443 | 450,817,565 | 145 (0.4) | 145 (0.4) | |
| Total | 3,010,030 | 17,709,474 | 133,134,979,999 | $30,594,018,855 | |||||
Source: Healthcare Cost and Utilization Project National Inpatient Sample (http://hcup.ahrq.gov/hcupnet.jsp)
Weighted national estimates from HCUP National Inpatient Sample (NIS), 2014 Agency for Healthcare Research and Quality (AHRQ).
Total number of weighted discharges in the U.S. based on HCUP NIS = 35,358,818
See supplementary table for specific groupings of ICD-9 CM codes for each category. In diagnosis categories represented by multiple ICD-9-CM codes, median LOS and median costs are presented for most common ICD-9-CM code in these categories. Rate of visits, admissions and deaths represent the sum from all codes
Total hospital days per year for all persons with each diagnosis, estimated by the product of number of discharges and mean LOS
The code “Gastrointestinal hemorrhage NOS” (578.9) was included in the overall GI bleeding category but was not included in subcategories of upper and lower GI bleeding, because it is nonspecific.
Category may not include hepatic encephalopathy associated with viral hepatitis
Includes esophageal (e.g. achalasia), gastric (e.g. dyspepsia), and intestinal (e.g. irritable bowel syndrome) functional/motility syndromes, as well as constipation and diarrhea
Includes Salmonella, Shigella, E.coli, and other viral, bacterial, and parasitic GI infections. Does not include Clostridium difficile infections (reported separately).
Part of measured increase since 2006 may be due to coding change in 2007 for ascites
Abbreviations: ICD-9-CM: International Classification of Diseases, 9th edition, Clinical Modification; %∆: percent change; LOS length of stay; USD: US dollars ($); SBP: spontaneous bacterial peritonitis; NE: no estimate due to few data
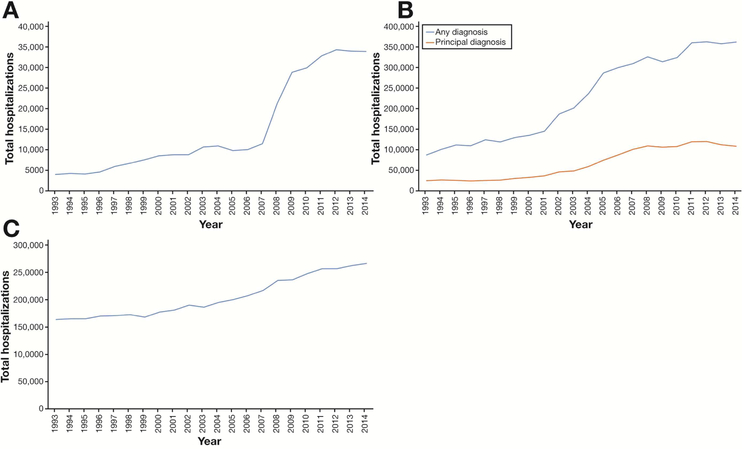
Hospitalizations for chronic liver disease increased 25% over the past 10 years, with the largest increase in hepatitis C hospitalizations (Figure 1a). Hospitalizations for clostridium difficile infections increased until 2011 and have since plateaued (Figure 1b). There has been a gradual rise in hospitalizations for intestinal obstruction since the 1990s (Figure 1c). The number of hospital admissions for appendicitis and appendectomies has decreased substantially since 2009–2010, while emergency department visits have remained static, and discharges from the emergency department have increased (Figure 2).
Figure 1A.
Temporal trend in hospitalizations with a principal diagnosis of chronic hepatitis C virus infection, National Inpatient Sample, 1993–2014. (B) Temporal trends in hospitalizations with any diagnosis or principal diagnosis of clostridium difficile infection, National Inpatient Sample, 1993–2014. (C) Temporal trend in hospitalizations with principal diagnosis of intestinal obstruction, National Inpatient Sample, 1993–2014.
Figure 2.
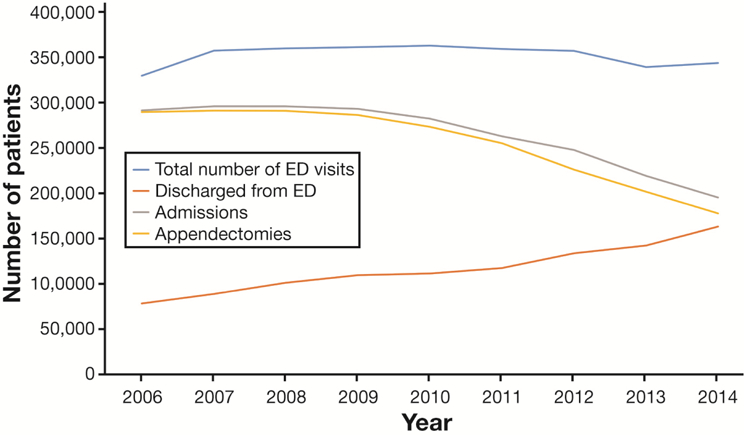
Temporal trends in emergency department visits, hospitalizations and surgeries for appendicitis, Nationwide Emergency Department Sample and National Inpatient Sample, 2006–2014
Readmissions
There are more than 540 thousand readmissions in the United States annually within 30 days of an index admission for a GI disease (Table 5). GI hemorrhage, gallbladder disease and intestinal obstruction had the highest number of all-cause readmissions within 30 days (Table 5). Liver disease, GI hemorrhage and gallbladder disease had the highest rates of all-cause readmissions. The median charge for a readmission was higher than the median charge for an index admission for each disease category.
Table 5.
All-cause 30-day Readmissions Ranked by Most Frequently Readmitted Gastrointestinal, Liver or Pancreatic Conditions in US Hospitals, 2015a
| Rank | Principal diagnosisb for index hospital stay | Number of index stays | Number of 30-day all cause readmissions | % Readmitted | Median Charge per Index stay (USD) | Median Charge per Readmission (USD) |
|---|---|---|---|---|---|---|
| 1 | Gastrointestinal hemorrhage | 669,488 | 96,945 | 14.5 | 28,819 | 30,800 |
| Upperc | 312,081 | 43,734 | 14.0 | 26,019 | 27,717 | |
| Lowerc | 241,349 | 37,361 | 15.5 | 36,385 | 36,231 | |
| 2 | Cholelithiasis and cholecystitis | 585,770 | 85,257 | 14.6 | 31,622 | 33,990 |
| 3 | Intestinal obstruction | 433,873 | 54,409 | 12.5 | 23,472 | 27,837 |
| 4 | Pancreatitis | 393,913 | 56,148 | 14.3 | 28,477 | 30,201 |
| Acute | 371,503 | 53,261 | 14.3 | 28,633 | 30,507 | |
| Chronic | 22,614 | 2,919 | 12.9 | 25,140 | 25,503 | |
| 5 | Appendicitis | 294,012 | 42,197 | 14.4 | 29,657 | 31,231 |
| 6 | Obesity | 230,476 | 31,884 | 13.8 | 33,607 | 34,871 |
| 7 | Inflammatory bowel disease | 175,917 | 23,881 | 13.6 | 26,345 | 27,735 |
| Ulcerative colitis | 120,017 | 16,401 | 13.7 | 28,766 | 27,158 | |
| Crohn’s disease | 55,900 | 7,480 | 13.4 | 25,222 | 29,586 | |
| 8 | Diverticulitis | 143,050 | 19,733 | 13.8 | 25,912 | 29,562 |
| 9 | Liver disease and viral hepatitis | 139,971 | 20,936 | 15.0 | 29,692 | 30,607 |
| Alcoholic liver disease | 23,202 | 3,439 | 15.3 | 28,519 | 29,678 | |
| Hepatitis C | 12,422 | 1,865 | 15.5 | 29,371 | 31,838 | |
| Hepatitis B | 1,704 | 261 | 16.3 | 30,637 | 37,120 | |
| Ascites or SBP | 6,142 | 895 | 14.4 | 28,058 | 29,857 | |
| Hepatic Encephalopathy | 19,563 | 2,847 | 14.8 | 27,816 | 30,250 | |
| 10 | Clostridium difficile infection | 130,895 | 18,382 | 14.0 | 22,550 | 25,939 |
| 11 | Gastritis | 114,861 | 16,118 | 14.0 | 28,349 | 31,111 |
| 12 | Gastroesophageal reflux disease | 86,188 | 11,413 | 13.4 | 34,513 | 38,956 |
| 13 | Gastrointestinal infectiond | 86,183 | 12,302 | 14.3 | 26,338 | 26,690 |
| 14 | Non-infectious gastroenteritis/colitis | 82,128 | 11,834 | 14.4 | 26,396 | 29,428 |
| 15 | Functional/motility disorderse | 70,963 | 10,058 | 14.2 | 25,583 | 28,071 |
| 16 | Abdominal pain | 62,758 | 8,969 | 14.3 | 28,562 | 30,752 |
| Total | 540,466 | |||||
Source: Healthcare Cost and Utilization Project Nationwide Readmissions Database (https://hcupnet.ahrq.gov)
Weighted national estimates from HCUP Nationwide Readmissions Database (NEDS) 2015, Agency for Healthcare Research and Quality (AHRQ).
See supplementary table for specific groupings of ICD-9 CM codes for each category
The code “Gastrointestinal hemorrhage NOS” (578.9) was included in the overall GI bleeding category but was not included in subcategories of upper and lower GI bleeding, because it is nonspecific.
Includes Salmonella, Shigella, E.coli, and other viral, bacterial, and parasitic GI infections. Does not include Clostridium difficile infections
Includes esophageal (e.g. achalasia), gastric (e.g. dyspepsia), and intestinal (e.g. irritable bowel syndrome) functional/motility syndromes, as well as constipation and diarrhea
Abbreviations: USD: US dollars ($); SBP: spontaneous bacterial peritonitis
Hepatitis C Virus Infection
Based on 248 participants who tested positive for HCV RNA, the estimated prevalence of chronic HCV in the United States between 2009–2016 was 0.80% (95% CI 0.66–0.96) (Table 6). Chronic HCV was most common individuals aged 51–69 years (68% of cases), however more than a quarter of cases (26%) occurred among individuals between the ages of 18 and 50. As compared to those who tested negative on screening (i.e. HCV antibody negative), HCV cases occurred more predominantly in males (68% vs. 49%) and non-Hispanic blacks (41% vs. 21%).
Table 6.
Estimated Chronic Hepatitis C Virus Infection in the United States, 2009–2016
| Characteristic | HCV Status | |||
|---|---|---|---|---|
| Never exposed (Anti-HCV Ab Negative) N= 29,170 | Chronic Hepatitis C (HCV RNA Positive) N=248 | |||
| n | % | n | % | |
| Age at interview | ||||
| <18 | 7,544 | 27 | 0 | 0 |
| 18–34 | 6,093 | 22 | 9 | 4 |
| 35–50 | 5,342 | 19 | 54 | 23 |
| 51–69 | 5,930 | 21 | 162 | 68 |
| >=70 | 3,323 | 12 | 15 | 6 |
| Sex | ||||
| Male | 14,317 | 49 | 169 | 68 |
| Female | 14,853 | 51 | 79 | 32 |
| Race/Ethnicity | ||||
| Non-Hispanic White | 10,744 | 37 | 84 | 34 |
| Non-Hispanic Black | 6,249 | 21 | 101 | 41 |
| Hispanic | 8,408 | 29 | 51 | 21 |
| Other/Multi-racial | 3,769 | 13 | 12 | 5 |
| Highest Level Education (age>20 years) | ||||
| <9th grade | 2,163 | 11 | 24 | 10 |
| 9–11 grade | 2,792 | 14 | 69 | 28 |
| High school grad/GED | 4,512 | 22 | 69 | 28 |
| Some college | 6,108 | 30 | 70 | 28 |
| College grad or above | 4,957 | 24 | 14 | 6 |
| Refused/Don’t Know | 18 | 0 | 2 | 1 |
| Annual Household Income | ||||
| <$14,999 | 3,692 | 14 | 64 | 29 |
| $15,000–34,999 | 7,539 | 29 | 95 | 42 |
| $35,000–54,999 | 4,951 | 19 | 31 | 14 |
| $55,000–74,999 | 2,926 | 11 | 16 | 7 |
| $75,000–99,999 | 2,553 | 10 | 7 | 3 |
| >100,000 | 4,707 | 18 | 11 | 5 |
Source: National Health and Nutrition Examination Survey (NHANES)
Abbreviations: Anti-HCV Ab = antibody to Hepatitis C Virus; HCV = Hepatitis C Virus;
Cancer Incidence and Mortality
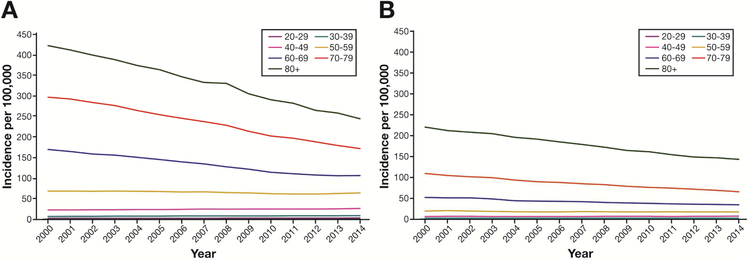
There were 266,564 incident cases of GI cancers diagnosed in 2014 (Table 7). The incidence of colorectal cancer was highest (53.7 per 100,000), followed by pancreatic (17.6 per 100,000) and liver (11.3 per 100,000) cancers. The incidence and mortality of colorectal (Figures 3A and 3B) cancer decreased markedly among older adults (age ≥60 years) from 2000 – 2014. We observed slight increases in the incidence of colon and rectal cancers in younger populations, although mortality remained stable during the same time period (supplemental tables).
Table 7.
Age-adjusted (2000 U.S. Standard Population) Incidence and Mortality of Gastrointestinal, Pancreatic and Liver Cancers in the United States, 2014
| Cancer Site | Number of new cases | Rate per 100,000 | Number of deaths | Rate per 100,000 |
|---|---|---|---|---|
| Colon and Rectum | 139,773 | 53.7 | 51,646 | 19.8 |
| Pancreas | 46,477 | 17.6 | 40,413 | 15.3 |
| Liver and Intrahepatic Bile Ducts | 31,181 | 11.3 | 24,659 | 9.1 |
| Stomach | 23,696 | 9.1 | 11,306 | 4.4 |
| Esophagus | 16,910 | 6.3 | 14,933 | 5.6 |
| Small Intestine | 8,527 | 3.3 | 1,349 | 0.5 |
| Total | 266,564 | 144,306 |
Source: United States Cancer Statistics: 1999 – 2014 Incidence and Mortality Web-based Report. Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute; 2017. Available at: www.cdc.gov/uscs.
Figure 3A.
Age-adjusted incidence (2000 U.S. standard population) of colorectal cancer by 10-year age group, United States Cancer Statistics, 2000 – 2014. (B) Age-adjusted mortality (2000 U.S. standard population) of colorectal cancer by 10-year age group, United States Cancer Statistics, 2000 – 2014.
Non-Cancer Mortality
There were 97,698 deaths from non-malignant GI diseases in 2016 (Table 8). The most common causes of non-malignant mortality were alcoholic liver disease, all-cause cirrhosis, gastrointestinal hemorrhage, vascular disorders of the intestine and clostridium difficile colitis. More than half (54%) of deaths from all non-malignant GI diseases were attributable to liver disease.
Table 8.
Causes of Death from Non-Malignant Gastrointestinal, Pancreatic and Liver Diseases in the United States, 2016
| Women | Men | Total | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Rank | Diseasea | Deaths underlying | Deaths contributing | Crude mortality rate (per 100,000)a | Deaths underlying | Deaths contributing | Crude mortality rate (per 100,000)a | Deaths underlying | Deaths contributing | Crude mortality rate (per 100,000)a |
| 1 | Alcoholic liver disease | 6,665 | 8,264 | 4.1 | 15,150 | 20,331 | 9.5 | 21,815 | 28,595 | 6.8 |
| 2 | Hepatic fibrosis/cirrhosis (all-cause) | 8,047 | 16,191 | 4.9 | 10,629 | 24,247 | 6.7 | 18,676 | 40,438 | 5.8 |
| 3 | Gastrointestinal hemorrhage, unspecified | 4,415 | 15,046 | 2.7 | 4,411 | 17,925 | 2.8 | 8,826 | 32,971 | 2.7 |
| 4 | Vascular disorders of the Intestine | 4,785 | 8,852 | 2.9 | 2,945 | 6,114 | 1.9 | 7,730 | 14,966 | 2.4 |
| 5 | Clostridium difficile colitis | 4,045 | 6,733 | 2.5 | 2,723 | 4,846 | 1.7 | 6,768 | 11,579 | 2.1 |
| 6 | Paralytic ileus and intestinal obstruction | 3,890 | 9,800 | 2.4 | 2,659 | 7,425 | 1.7 | 6,549 | 17,225 | 2.0 |
| 7 | Chronic hepatitis C | 1,992 | 5,270 | 1.2 | 3,734 | 12,800 | 2.3 | 5,726 | 18,070 | 1.8 |
| 8 | Hepatic failure (acute and chronic) | 1,867 | 11,417 | 1.1 | 2,316 | 14,972 | 1.5 | 4,183 | 26,389 | 1.3 |
| 9 | Ulcers (gastric/duodenal/peptic) | 1,561 | 3,056 | 1.0 | 1,647 | 3,354 | 1.0 | 3,208 | 6,410 | 1.0 |
| 10 | Acute pancreatitis | 1,159 | 2,310 | 0.7 | 1,743 | 3,257 | 1.1 | 2,902 | 5,567 | 0.9 |
| 11 | Diverticular disease | 1,951 | 2,950 | 1.2 | 984 | 1,652 | 0.6 | 2,935 | 4,602 | 0.9 |
| 12 | Perforation of intestine (non-traumatic) | 1,537 | 3,874 | 0.9 | 949 | 2,784 | 0.6 | 2,486 | 6,658 | 0.8 |
| 13 | Cholecystitis | 1,265 | 1,893 | 0.8 | 1,244 | 1,948 | 0.8 | 2,509 | 3,841 | 0.8 |
| 14 | Fatty change of liver-not elsewhere specified | 1,486 | 2,616 | 0.9 | 888 | 2,058 | 0.6 | 2,374 | 4,674 | 0.7 |
| 15 | Cholangitis | 504 | 959 | 0.3 | 507 | 1,101 | 0.3 | 1,011 | 2,060 | 0.3 |
| Total | 97,698 | 224,045 | ||||||||
Source: Centers for Disease Control Wide-ranging Online Data for Epidemiologic Research (http://wonder.cdc.gov). See supplementary table for specific groupings of ICD-10 CM codes for each category
Crude rate per 100,000 deaths was calculated by dividing the number of deaths listed as an underlying cause by the total U.S. population in the United States in 2016 then multiplying by 100,000
Endoscopy Use and Trends
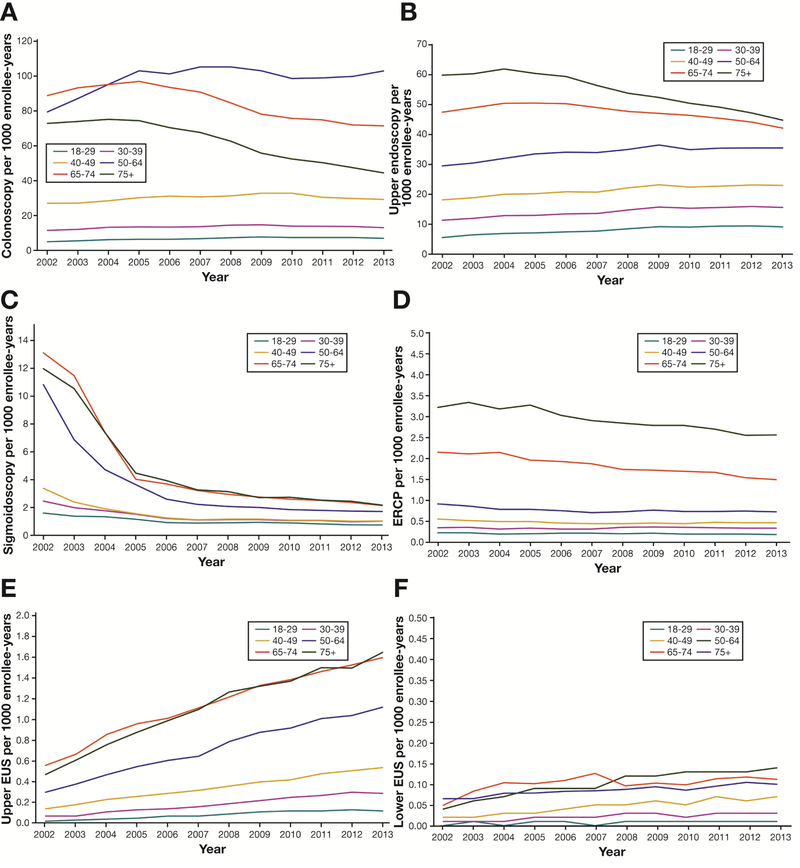
There were an estimated 10,964,034 colonoscopies, 6,069,647 upper endoscopies, 313,045 flexible sigmoidoscopies, 178,417 upper EUSs, 169,510 ERCPs and 17,727 lower EUSs performed in adults in the United States in 2013 (Table 9). Colonoscopy use in adults aged 18–64 increased between 2002 and 2008 and then began to decrease (Figure 4A). Colonoscopy use has been decreasing in adults over the age of 65 years since 2005 (Figure 4A). Between 2002 and 2013, the rates of upper endoscopies increased slightly in adults aged 18–64 but decreased in adults over the age of 65 years (Figure 4B). The rates of flexible sigmoidoscopies have decreased each year across all age groups since 2002 (Figure 4C). The rates of ERCPs decreased each year across all age groups (Figure 4D), while use of upper EUSs increased each year (Figure 4E). The rates of lower EUSs have increased each year (Figure 4F).
Table 9.
Estimated Annual Number of Endoscopic Procedures in the United States, 2013
| Procedure | Number |
|---|---|
| Colonoscopy | 10,964,034 |
| Upper endoscopy | 6,069,647 |
| Flexible sigmoidoscopy | 313,045 |
| Upper endoscopic ultrasound | 178,417 |
| Endoscopic retrograde cholangiopancreatography | 169,510 |
| Lower endoscopic ultrasound | 17,727 |
| Total | 17,712,380 |
Source: MarketScan Commercial Claims and Encounters and Medicare
Figure 4A.
Colonoscopies performed per 1,000 enrollee-years, by age group, MarketScan Commercial Claims and Encounters and Medicare, 2002–2013. (B) Upper endoscopies performed per 1,000 enrollee-years, by age group, MarketScan Commercial Claims and Encounters and Medicare, 2002–2013. (C) Flexible sigmoidoscopies performed per 1,000 enrollee-years, by age group, MarketScan Commercial Claims and Encounters and Medicare, 2002–2013. (D) Endoscopic retrograde cholangiopancreatographies performed per 1,000 enrollee-years, by age group, MarketScan Commercial Claims and Encounters and Medicare, 2002–2013. (E) Upper endoscopic ultrasound performed per 1,000 enrollee-years, by age group, MarketScan Commercial Claims and Encounters and Medicare, 2002–2013. (F) Lower endoscopic ultrasound performed per 1,000 enrollee-years, by age group, MarketScan Commercial Claims and Encounters and Medicare, 2002–2013
Endoscopy Adverse Events, Quality Measures and Findings
Between 2014–2016, quality improvement data were collected on 3,916,419 colonoscopies and 564,691 upper endoscopies performed across the United States (supplemental tables). Rates of immediate adverse events for upper endoscopy and colonoscopy are reported in Table 10. Among all screening and surveillance colonoscopies, 95% had an adequate bowel preparation, 94% had documented cecal landmarks and the average withdrawal time was 10.7 minutes (standard deviation 5.8 minutes). The average withdrawal time when no tissue was collected was 8.1 minutes (standard deviation 3.4 minutes).
Table 10.
Immediate Risk of Adverse Events During Colonoscopy and Upper Endoscopy, 2014–2016
| Screening & Surveillance Colonoscopy | Screening, Surveillance and Diagnostic Colonoscopy | Upper Endoscopy | ||||
|---|---|---|---|---|---|---|
| N= 2,809,509 | N= 3,916,419 | N= 564,691 | ||||
| Events (n) | Event Rate per 10,000 | Events (n) | Event Rate per 10,000 | Event (n) | Event Rate per 10,000 | |
| Bowel perforation | 134 | 0.48 | 237 | 0.61 | 15 | 0.27 |
| Bleeding (unplanned intervention or | 281 | 1.00 | 433 | 1.11 | 67 | 1.19 |
| Emergency department visit | 69 | 0.25 | 128 | 0.33 | 15 | 0.27 |
| Hospital admission | 63 | 0.22 | 110 | 0.28 | 17 | 0.30 |
| Sedation related (unplanned intervention) | 276 | 0.98 | 360 | 0.92 | 56 | 0.99 |
| Death | 8 | 0.03 | 9 | 0.02 | 6 | 0.11 |
Source: GI Quality Improvement Consortium Endoscopy
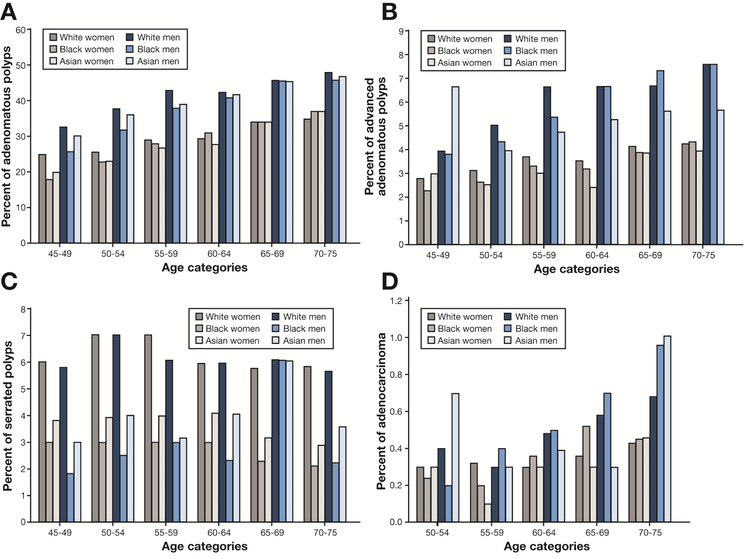
Among average-risk persons ages 50–75 years having a colonoscopy for a screening indication, 34.6% had 1 or more adenomatous polyps removed (Table 11). The prevalence of any adenomatous polyp increased with age and was higher in men compared with women (Figure 5a). Among average-risk persons ages 50–75 years having a colonoscopy for a screening indication, 4.7% had 1 or more advanced adenomatous (≥ 10 mm, high grade dysplasia, villous component) polyps removed (Table 11). The prevalence of advanced adenomatous polyps increased with age and was higher in men compared with women (Figure 5b). Among average-risk persons ages 50–75 years having a colonoscopy for a screening indication, 5.7% had 1 or more serrated polyps removed (Table 11). The prevalence of serrated polyps did not increase with age, was similar in men and women, and was higher among whites compared with other races (Figure 5c). Among average-risk persons ages 50–75 years having a colonoscopy for a screening indication, 0.4% had an adenocarcinoma found. The prevalence of adenocarcinoma increased with age, was higher in men compared with women and was higher in blacks compared with other races (Figure 5d). Colonoscopy findings in the total population and screening population are reported in Table 11.
Table 11.
Colonoscopy Findings in the Total Population and Screening Population in GI Quality Improvement Consortium Endoscopy, 2014–2016
| Total population (n = 3,901,576) |
Screening only, ages 50–75 y, average risk (n = 1,476,145) |
|||
|---|---|---|---|---|
| Pathology | n | % | n | % |
| Adenocarcinoma | 22,118 | 0.6 | 5409 | 0.4 |
| Adenomatous polyps | 1,328,060 | 34.0 | 510,539 | 34.6 |
| 1 or 2 tubular adenomas <10 mm | 945,263 | 24.2 | 371,706 | 25.2 |
| 3 or more tubular adenomas <10 mm | 245,223 | 6.3 | 84,707 | 5.7 |
| ≥10 mm, high-grade dysplasia, villous component | 178,217 | 4.6 | 69,304 | 4.7 |
| Serrated polyps | 211,915 | 5.4 | 83,410 | 5.7 |
| <10 mm with no dysplasia | 150,866 | 3.9 | 59,771 | 4.1 |
| >10 mm or with dysplasia or traditional serrated adenoma | 56,801 | 1.5 | 21,997 | 1.5 |
| Hyperplastic polyps | 695,155 | 17.8 | 275,809 | 18.7 |
| Other pathology | 540,268 | 13.9 | 120,157 | 8.1 |
Source: GI Quality Improvement Consortium Endoscopy.
Figure 5A.
Adenomatous polyps on colonoscopy in screening only, ages 45–75, average risk persons by age, sex and race. (B) Advanced adenomatous polyps (≥ 10 mm, high grade dysplasia, villous component) on colonoscopy in screening only, ages 45–75, average risk persons by age, sex and race (C) Serrated polyps on colonoscopy in screening only, ages 45–75, average risk persons by age, sex and race (D) Adenocarcinoma on colonoscopy in screening only, ages 50–75, average risk persons by age, sex and race
Expenditures
In 2015, health care expenditures for GI conditions totaled $135.9 billion (Table 12). Among the 22 condition categories available, the five most expensive categories were hepatitis ($23.3 billion), esophageal disorders ($18.1 billion), biliary tract disease ($10.3 billion), abdominal pain ($10.2 billion) and inflammatory bowel disease ($7.2 billion). Prescription medications accounted for 96% of total expenditures for hepatitis and 54% of total expenditures for esophageal disorders. Hospital inpatients stays accounted for the majority of cost among all other conditions. Expenditures by prescribed acid suppressing drug in the United States from 2001 to 2015 are detailed in Table 13. In the last five years, expenditures for acid suppressing drugs totaled $60 billion.
Table 12.
Total Expenses Gastrointestinal, Pancreatic and Liver Diseases in the United States, 2015
| Percent Distribution by Type of Service | |||||||
|---|---|---|---|---|---|---|---|
| Condition Category | Total Expenses ($) (in millions) | Office-Based Visits | Outpatient Department Visits | Hospital Inpatient Stays | EEmergency Room Visits | Prescribed Medicines | Home Health |
| Hepatitis | 23,301 | 1.4% | 0.3% | 1.7% | 0.2% | 96.4% | NE |
| Intestinal infection | 6,448 | 10.2% | 0.4% | 70.1% | 8.0% | 11.3% | 0.1% |
| Colon cancer | 4,059 | 18.7% | 3.9% | 68.1% | 0.6% | 0.1% | 8.5% |
| Cancer of other GI organs | 6,106 | 14.6% | 22.6% | 56.5% | 0.4% | 2.7% | 3.2% |
| Esophageal disorders | 18,113 | 13.6% | 9.7% | 12.7% | 1.8% | 54.4% | 7.8% |
| Gastritis and duodenitis | 1,187 | 23.5% | 15.4% | 15.0% | 10.2% | 22.5% | 13.4% |
| Gastroduodenal ulcer | 777 | 19.2% | 11.4% | 43.5% | 0.4% | 24.4% | 1.2% |
| Other disorders of stomach and duodenum | 7,010. | 24.6% | 10.5% | 21.1% | 15.8% | 23.1% | 4.8% |
| Appendicitis | 4,528. | 2.8% | 2.3% | 74.7% | 19.8% | 0.4% | NE |
| Abdominal hernia | 6,762. | 19.7% | 31.0% | 38.2% | 6.5% | 2.5% | 2.0% |
| Crohn’s disease and ulcerative colitis | 7,248 | 19.3% | 10.4% | 14.3% | 3.3% | 52.4% | 0.1% |
| Noninfectious gastroenteritis | 1,765 | 15.3% | 3.4% | 13.4% | 17.8% | 17.1% | 32.9% |
| Intestinal obstruction without hernia | 3,970.3 | 2.2% | 0.3% | 77.9% | 14.6% | 3.4% | 1.6% |
| Diverticulosis and diverticulitis | 5,461 | 6.0% | 9.3% | 65.4% | 11.1% | 7.0% | 1.2% |
| Anal and rectal conditions | 4,355 | 6.9% | 1.4% | 69.5% | 1.0% | 2.3% | 18.9% |
| Hemorrhoids | 877 | 64.1% | 19.2% | NE | 3.9% | 12.8% | NE |
| Other liver disease | 5,174 | 14.1% | 9.9% | 55.4% | 4.2% | 12.2% | 4.1% |
| Biliary tract disease | 10,296 | 8.2% | 14.0% | 64.3% | 11.8% | 1.2% | 0.5% |
| Pancreatic disorders | 2,386 | 5.2% | 8.9% | 71.2% | 7.8% | 5.5% | 1.4% |
| Gastrointestinal hemorrhage | 2,794 | 20.7% | 5.4% | 59.4% | 9.3% | 1.7% | 3.7% |
| Nausea and vomiting | 3,053 | 10.7% | 13.4% | 41.0% | 18.1% | 14.6% | 2.1% |
| Abdominal pain | 10,246 | 6.2% | 6.5% | 77.9% | 7.6% | 0.8% | 1.0% |
| Total | $135,926 | ||||||
Source: Medical Expenditure Panel Survey data, Household Component 2015 survey (https://meps.ahrq.gov/)
All estimates were weighted by the MEPS person-level weight to produce national estimates of expenditures.
The condition categories were defined using the Clinical Classification Software (CCS), which is a tool, developed by Agency for Healthcare Research and Quality for clustering diagnoses into a manageable number of clinically meaningful policy-relevant categories
Abbreviations: NE: No survey participants reported services from which expenditures can be extrapolated
Table 13.
Total Expenditures in Millions By Prescribed Acid Suppressing Drug in the United States, 2001–2015
| Prescribed drug | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Dexlansoprazolea | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | 646 | 709 | 681 | -- | 1,131 |
| Famotidine | 562 | 295 | 225 | 202 | 316 | 184 | 332 | 349 | 128 | 214 | 144 | 141 | 267 | 236 | 140 |
| Lansoprazole | 2,250 | 2,633 | 2,983 | 3,031 | 3,517 | 3,122 | 3,654 | 3,478 | 3,601 | 1,559 | 1,079 | 894 | 857 | 688 | 509 |
| Omeprazole | 3,161 | 2,103 | 1,797 | 1,604 | 1,328 | 2,267 | 2,225 | 2,567 | 2,318 | 3,638 | 3,034 | 2,944 | 3,099 | 3,185 | 3,298 |
| Pantoprazole | 539 | 840 | 1,348 | 1,640 | 2,129 | 1,973 | 2,512 | 2,056 | 1,906 | 1,908 | 689 | 644 | 974 | 1,102 | 1,528 |
| Rabeprazolea | 383 | 720 | 1,316 | 1,098 | 1,105 | 973 | 1,039 | 1,340 | 1,168 | 672 | -- | -- | -- | -- | -- |
| Esomeprazole | 181 | 1,083 | 2,049 | 3,264 | 4,412 | 3,006 | 6,050 | 7,586 | 6,257 | 6,731 | 6,250 | 5,338 | 6,016 | 6,448 | 5,326 |
| Ranitidine | 866 | 838 | 893 | 711 | 1,250 | 1,150 | 990 | 561 | 320 | 225 | 221 | 326 | 280 | 517 | 505 |
| Total | 7,942 | 8,512 | 10,611 | 11,550 | 14,057 | 12,675 | 16,802 | 17,937 | 15,698 | 14,947 | 12,063 | 10,996 | 12,174 | 12,176 | 12,437 |
Source: Center for Financing, Access and Cost Trends, Agency for Healthcare Research and Quality, Medical Expenditure Panel Survey
-- Estimates suppressed due to inadequate precision
National Institutes of Health Categorical Spending
In 2017, the National Institutes of Health supported $1,832 million dollars in digestive diseases and $661 million dollars in liver disease research. Spending for all available GI categories are detailed in Table 14.
Table 14.
National Institutes of Health Estimates of Funding for Select Research, Condition, and Disease Categories, 2013–2018
| Research/Disease Areasa (US Dollars in millions and rounded) |
2013 Actual |
2014 Actual |
2015 Actual |
2016 Actual |
2017 Estimated (Enacted) |
2018 Estimated |
|---|---|---|---|---|---|---|
| Digestive Diseases | 1,575 | 1,607 | 1,684 | 1,745 | 1,832 | 1,416 |
| Inflammatory Bowel Disease | 114 | 125 | 128 | 126 | 130 | 100 |
| Colorectal Cancer | 281 | 271 | 309 | 274 | 296 | 232 |
| Pancreatic Cancer | 125 | 123 | 174 | 168 | 183 | 143 |
| Liver Cancer | 71 | 74 | 85 | 83 | 89 | 69 |
| Liver Disease | 594 | 605 | 616 | 635 | 661 | 509 |
| Hepatitis | 195 | 251 | 262 | 267 | 277 | 212 |
| Hepatitis - A | 2 | 3 | 4 | 3 | 3 | 2 |
| Hepatitis - B | 48 | 48 | 42 | 47 | 49 | 37 |
| Hepatitis - C | 101 | 111 | 96 | 107 | 111 | 86 |
| Organ | 140 | 142 | 148 | 153 | 159 | 122 |
| Obesity | 812 | 857 | 900 | 965 | 997 | 780 |
| Alcohol | 437 | 475 | 473 | 486 | 503 | 375 |
Source: National Institutes of Health Research Portfolio Online Reporting Tools. NIH Categorical Spending. Table Published. July 3, 2017. Available at: https://Report.nih.gov
Categories are not mutually exclusive.
Discussion
The impact of GI diseases on patients and the health care system in the United States is substantial. Annual health care expenditures for these diseases total $135.9 billion dollars. This is more than expenditures for heart disease ($113.4 billion), trauma-related disorders ($102.7 billion) and mental disorders ($98.8 billion).12 There are more than 40.7 million ambulatory visits for GI symptoms and 54.4million visits with a primary diagnosis for a GI disease each year. There are more than 3.0 million hospital admissions at a cost of 31 billion dollars. Among those patients admitted to the hospital, roughly one in seven will be readmitted to the hospital within 30 days. There are 267,000 new cases of GI cancers diagnosed each year and 242,004 deaths from benign and malignant GI diseases. An estimated 17.7 million endoscopic procedures are performed annually in the United States.
In the last twenty years, there has been a dramatic increase in emergency department visits and hospital admission for HCV in the United States. This is a likely consequence of the increasing prevalence of HCV-related cirrhosis and hepatocellular carcinoma in the United States.13, 14 Mortality attributable to non-malignant liver diseases, including HCV, is also increasing.15 Among the 22 GI categories available in MEPS, hepatitis was the most expensive category at $23.3 billion per year, with prescription medications accounting for 96% of these expenditures. This estimate is congruent with the IMS Institute report that 249,000 patients received treatment for HCV in 2015, resulting in $18.8 billion dollars in non-discounted spending (for direct-acting antiviral therapy).16 Because only 12.8% of the baby boomer population has been screened for HCV17 and because the opioid epidemic is likely contributing to an increased incidence of HCV18–21, health care spending for HCV treatment will likely continue to be substantial. Despite the substantial costs of HCV treatment, there is good evidence that treatment is cost-effective at currently available discounts.22
Using data from NHANES, the prevalence of chronic HCV appears to be stable and possibly decreasing in the United States. The prevalence of chronic HCV was 1.8% between 1988–1994, 1.6% between 1999–2002 and 1% between 2003–2010 in NHANES.6–8 We are hesitant to overstate the significance of this decline because there are important limitations of using NHANES to estimate the prevalence of chronic HCV. This survey does not include inmates, the homeless, hospital inpatients, nursing home residents, active duty military, and people living on Indian reservations.23 Moreover, the NHANES survey may underrepresent individuals who inject drugs, a high-risk population. Therefore, the survey likely substantially underestimates the actual prevalence of chronic HCV in the United States. Despite a decreasing prevalence of HCV in NHANES, there is growing evidence to believe that the burden of chronic HCV may be increasing. The rising opioid epidemic and rates of people who inject drugs is suspected to be contributing to increased incidence of HCV for the first time in over two decades.18–20, 24 Direct-acting antiviral (DAA) therapy offers a cure for HCV, but with the current practice of only screening baby boomers, many individuals will remain unaware of their HCV status. The limitations of NHANES data demonstrate the critical need for a better strategy to investigate the prevalence of chronic HCV in the U.S.
The incidence of and mortality from colorectal cancer continues to decline among older adults in the United States, which is partly attributable to colorectal cancer screening.25 Figure 3 highlights the marked decrease in colorectal cancer but also demonstrates the increasing risk of young-onset colorectal cancer. While the incidence of colorectal cancer has increased in young adults, it is important to note that the absolute risk is very low and mortality has remained stable. The reason for the increase in colorectal cancer in not known, but appears to be a birth cohort effect.26
Understanding utilization of endoscopy is important not only for gastroenterology workforce allocation but for understanding and potentially controlling health care costs. We continue to observe, a decline in ERCP procedures and an increase in EUS.27–29 This suggests that diagnostic ERCPs are being replaced by less invasive and less risky imaging procedures such as MRCP and EUS. With regard to colonoscopy use, surveys estimated that 14.2 million colonoscopies were performed in the United States in 200230 and 15 million total colonoscopies in 2012.31 In our report from 2012, we used 2009 MarketScan data (which included commercial, Medicare, and Medicaid enrollees) and found slightly higher estimated numbers of procedures compared to the current estimates we report here.32 There is evidence that insured Americans aged 50 to 64 years significantly reduced their use of screening colonoscopy during the 2007–2009 recession33 and these lower rates may have persisted following the economic upturn. With stricter reimbursement and quality measures, colonoscopy use in the United States may be decreasing. Finally, the numbers of colonoscopies in populations 65 and older are also decreasing. These changes may indicate that we are performing colonoscopies in more appropriate populations or perhaps decreasing unnecessary or too frequent colonoscopies.
With the large volume of endoscopic procedures performed nationally, ensuring high quality exams is paramount, particularly for colonoscopy.34, 35 Using the GIQuIC Registry, we were able to show high rates of procedural completion as documented by cecal landmarks, adequate bowel preparation, and appropriate withdrawal times, all accepted quality metrics for which there is substantial variation between endoscopists.36 We have also shown that the risk of immediate adverse events is very low. Notably, our complication rates are lower than prior estimates37–39 perhaps because these events were documented at the time of the procedure and not within the standard 30-days.
Using data from the GIQuIC Registry, we estimated a “national” adenoma detection rate of 34.6% among 1.5 million screening only, ages 50–75, average risk colonoscopies. The adenoma detection rate is a quality measure inversely associated with the risk of interval colorectal cancer and mortality.40, 41 Endoscopists with an annual adenoma detection rate > 24.6% achieve a significantly reduced risk.41 Among the 1.5 million screening only, age 50–75, average risk colonoscopies, we also found that 4.7% had 1 or more advanced adenomatous polyps and 5.7% had 1 or more serrated polyps.
We were also able to stratify the proportion of polyps by histology using age, race, and sex. In contrast with prior studies42–45, we found that the prevalence of any adenomatous polyps was higher in white women compared with black women before the age of 60. Before the age of 65, the prevalence of any adenomatous polyps was higher in white men compared with black men. Advanced adenomatous (≥ 10 mm, high grade dysplasia, villous component) polyps were more common in white women compared with black women before the age of 65 and white men compared with black men before the age of 60. Despite the lower prevalence of adenomatous polyps on screening colonoscopy, black women and men were more likely to be diagnosed with adenocarcinoma on screening colonoscopy at almost every age category compared with white women and men. While we replicated the known finding that the prevalence of adenomas is higher with increasing age and in men42, we also demonstrated that the prevalence of serrated polyps did not increase with age, was similar in men and women, and was higher among whites compared with other races. The prevalence of serrated polyps is likely underestimated in this database, due to their minimal role in GIQuIC quality measures, but this would not change the differences we found in prevalence based on age, sex and race/ethnicity. These findings may have implications for screening and detection practices.
This report has limitations, which are inherent to each of the datasets used. We relied on NAMCS and NHAMCS data collected by the CDC to generate an estimate of office visits in the United States for GI symptoms and diagnoses. There were sometimes significant differences between the estimates that we report here using 2014 data compared to estimates that we previously reported using 2010 data.1 Some of these differences can be accounted for by sparse data. Additionally, the CDC excluded information from community healthcare centers in 2014, which would also lead to smaller numbers. Despite the use of the standard sampling weights from HCUP, differences in the total estimated admissions are demonstrated within the multiple databases presented. This could be due to the use of different years of HCUP data, or a different sampling structure, particularly in the NIS and NRD data sources. We estimated the number of procedures performed in the United States in 2013 by standardizing the number of procedures in MarketScan Commercial Claims and Encounters data and a 5% random sample of all Medicare beneficiaries to United States Census Bureau data. Because we do not have data from the uninsured and those covered by Medicaid, we may have overestimated the number of procedures each year. However, compared with other estimates, ours appears to be conservative.30, 31 We used GIQuIC to report on quality measures and this registry relies on voluntary reporting of findings linked to endoscopic reporting software. GIQuIC is not population-based, and despite the large number of procedures captured in this database, may not be generalizable to all endoscopic procedures or providers.
This report is a comprehensive and current estimate of the burden of GI diseases in the United States. Health care spending for these diseases is considerable at $135.9 billion dollars annually and is likely to continue increasing for the foreseeable future. It is our hope that this paper will enable clinicians to better understand the challenges our patients face and best target both clinical and research resources to help them.
Supplementary Material
Acknowledgments
Grant Support: This research was supported in part by grants from the National Institutes of Health, K23DK113225, KL2TR001109, KL2TR001103 and T32 DK07634.
Footnotes
No conflicts of interest exist for any author.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Peery AF, Crockett SD, Barritt AS, et al. Burden of Gastrointestinal, Liver, and Pancreatic Diseases in the United States. Gastroenterology 2015;149:1731–1741 e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Myer PA, Mannalithara A, Singh G, et al. Clinical and economic burden of emergency department visits due to gastrointestinal diseases in the United States. Am J Gastroenterol 2013;108:1496–507. [DOI] [PubMed] [Google Scholar]
- 3.Everhart JE, Ruhl CE. Burden of digestive diseases in the United States Part III: Liver, biliary tract, and pancreas. Gastroenterology 2009;136:1134–44. [DOI] [PubMed] [Google Scholar]
- 4.Everhart JE, Ruhl CE. Burden of digestive diseases in the United States part II: lower gastrointestinal diseases. Gastroenterology 2009;136:741–54. [DOI] [PubMed] [Google Scholar]
- 5.Everhart JE, Ruhl CE. Burden of digestive diseases in the United States part I: overall and upper gastrointestinal diseases. Gastroenterology 2009;136:376–86. [DOI] [PubMed] [Google Scholar]
- 6.Armstrong GL, Wasley A, Simard EP, et al. The prevalence of hepatitis C virus infection in the United States, 1999 through 2002. Ann Intern Med 2006;144:705–14. [DOI] [PubMed] [Google Scholar]
- 7.Alter MJ, Kruszon-Moran D, Nainan OV, et al. The prevalence of hepatitis C virus infection in the United States, 1988 through 1994. N Engl J Med 1999;341:556–62. [DOI] [PubMed] [Google Scholar]
- 8.Denniston MM, Jiles RB, Drobeniuc J, et al. Chronic hepatitis C virus infection in the United States, National Health and Nutrition Examination Survey 2003 to 2010. Ann Intern Med 2014;160:293–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gonzalez JM. National Health Care Expenses in the U.S. Civilian Noninstitutionalized Population, 2011. Statistical Brief (Medical Expenditure Panel Survey (US)) Rockville (MD), 2001. [PubMed] [Google Scholar]
- 10.Carroll W, Miller GE. Heart Disease among Elderly Americans: Estimates for the U.S. Civilian Noninstitutionalized Population, 2010. Statistical Brief (Medical Expenditure Panel Survey (US)) Rockville (MD), 2001. [PubMed] [Google Scholar]
- 11.Agency for Healthcare Research and Quality. Total expenditures in millions by prescribed drug, United States, 1996–2015. Medical Expenditure Panel Survey Generated interactively: Thursday June 07, 2018. [Google Scholar]
- 12.Agency for Healthcare Research and Quality. Total expenditures in millions by condition, United States, 2015. Medical Expenditure Panel Survey Generated interactively: Thursday July 26, 2018. [Google Scholar]
- 13.Beste LA, Leipertz SL, Green PK, et al. Trends in burden of cirrhosis and hepatocellular carcinoma by underlying liver disease in US veterans, 2001–2013. Gastroenterology 2015;149:1471–1482 e5; quiz e17–8. [DOI] [PubMed] [Google Scholar]
- 14.Davis GL, Alter MJ, El-Serag H, et al. Aging of hepatitis C virus (HCV)-infected persons in the United States: a multiple cohort model of HCV prevalence and disease progression. Gastroenterology 2010;138:513–21, 521 e1–6. [DOI] [PubMed] [Google Scholar]
- 15.Ly KN, Hughes EM, Jiles RB, et al. Rising Mortality Associated With Hepatitis C Virus in the United States, 2003–2013. Clin Infect Dis 2016;62:1287–1288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.IMS Health. Medicines use and spending shifts. IMS Institute for Healthcare Informatics, Parsippany, NJ: (2015). [Google Scholar]
- 17.Kasting ML, Giuliano AR, Reich RR, et al. Hepatitis C Virus Screening Trends: Serial Cross-Sectional Analysis of the National Health Interview Survey Population, 2013–2015. Cancer Epidemiol Biomarkers Prev 2018;27:503–513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Liang TJ, Ward JW. Hepatitis C in Injection-Drug Users - A Hidden Danger of the Opioid Epidemic. N Engl J Med 2018;378:1169–1171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zibbell JE, Asher AK, Patel RC, et al. Increases in Acute Hepatitis C Virus Infection Related to a Growing Opioid Epidemic and Associated Injection Drug Use, United States, 2004 to 2014. Am J Public Health 2018;108:175–181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ly KN, Jiles RB, Teshale EH, et al. Hepatitis C Virus Infection Among Reproductive-Aged Women and Children in the United States, 2006 to 2014. Ann Intern Med 2017;166:775–782. [DOI] [PubMed] [Google Scholar]
- 21.Morse A, Barritt ASt, Jhaveri R. Individual State Hepatitis C Data Supports Expanding Screening Beyond Baby Boomers to All Adults. Gastroenterology 2018;154:1850–1851 e2. [DOI] [PubMed] [Google Scholar]
- 22.Chhatwal J, He T, Hur C, et al. Direct-Acting Antiviral Agents for Patients With Hepatitis C Virus Genotype 1 Infection Are Cost-Saving. Clin Gastroenterol Hepatol 2017;15:827–837 e8. [DOI] [PubMed] [Google Scholar]
- 23.Edlin BR, Eckhardt BJ, Shu MA, et al. Toward a more accurate estimate of the prevalence of hepatitis C in the United States. Hepatology 2015;62:1353–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Barritt ASt, Lee B, Runge T, et al. Increasing Prevalence of Hepatitis C among Hospitalized Children Is Associated with an Increase in Substance Abuse. J Pediatr 2018;192:159–164. [DOI] [PubMed] [Google Scholar]
- 25.Murphy CC, Sandler RS, Sanoff HK, et al. Decrease in Incidence of Colorectal Cancer Among Individuals 50 Years or Older After Recommendations for Population-based Screening. Clin Gastroenterol Hepatol 2017;15:903–909 e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Murphy CC, Singal AG, Baron JA. Decrease in incidence of young-onset colorectal cancer before recent increase Gastroenterology 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Committee AT, Maple JT, Pannala R, et al. Interventional EUS (with videos). Gastrointest Endosc 2017;85:465–481. [DOI] [PubMed] [Google Scholar]
- 28.Yachimski PS, Ross A. The Future of Endoscopic Retrograde Cholangiopancreatography. Gastroenterology 2017;153:338–344. [DOI] [PubMed] [Google Scholar]
- 29.Huang RJ, Thosani NC, Barakat MT, et al. Evolution in the utilization of biliary interventions in the United States: results of a nationwide longitudinal study from 1998 to 2013. Gastrointest Endosc 2017;86:319–326 e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Seeff LC, Richards TB, Shapiro JA, et al. How many endoscopies are performed for colorectal cancer screening? Results from CDC’s survey of endoscopic capacity. Gastroenterology 2004;127:1670–7. [DOI] [PubMed] [Google Scholar]
- 31.Joseph DA, Meester RG, Zauber AG, et al. Colorectal cancer screening: Estimated future colonoscopy need and current volume and capacity. Cancer 2016;122:2479–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Peery AF, Dellon ES, Lund J, et al. Burden of gastrointestinal disease in the United States: 2012 update. Gastroenterology 2012;143:1179–87 e1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dorn SD, Wei D, Farley JF, et al. Impact of the 2008–2009 economic recession on screening colonoscopy utilization among the insured. Clin Gastroenterol Hepatol 2012;10:278–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ketwaroo GA, Sawhney MS. Quality measures and quality improvements in colonoscopy. Curr Opin Gastroenterol 2015;31:56–61. [DOI] [PubMed] [Google Scholar]
- 35.Rex DK. Polyp detection at colonoscopy: Endoscopist and technical factors. Best Pract Res Clin Gastroenterol 2017;31:425–433. [DOI] [PubMed] [Google Scholar]
- 36.Mehrotra A, Dellon ES, Schoen RE, et al. Applying a natural language processing tool to electronic health records to assess performance on colonoscopy quality measures. Gastrointest Endosc 2012;75:1233–9 e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wang L, Mannalithara A, Singh G, et al. Low Rates of Gastrointestinal and Non-Gastrointestinal Complications for Screening or Surveillance Colonoscopies in a Population-Based Study. Gastroenterology 2018;154:540–555 e8. [DOI] [PubMed] [Google Scholar]
- 38.Lin J, Piper M, Perdue L, et al. Screening for colorectal cancer: an updated systematic review for the USPSTF. AHRQ, 14 (2015), pp. 1–240. [Google Scholar]
- 39.Reumkens A, Rondagh EJ, Bakker CM, et al. Post-Colonoscopy Complications: A Systematic Review, Time Trends, and Meta-Analysis of Population-Based Studies. Am J Gastroenterol 2016;111:1092–101. [DOI] [PubMed] [Google Scholar]
- 40.Corley DA, Jensen CD, Marks AR, et al. Adenoma detection rate and risk of colorectal cancer and death. N Engl J Med 2014;370:1298–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kaminski MF, Wieszczy P, Rupinski M, et al. Increased Rate of Adenoma Detection Associates With Reduced Risk of Colorectal Cancer and Death. Gastroenterology 2017;153:98–105. [DOI] [PubMed] [Google Scholar]
- 42.Lieberman DA, Williams JL, Holub JL, et al. Race, ethnicity, and sex affect risk for polyps >9 mm in average-risk individuals. Gastroenterology 2014;147:351–8; quiz e14–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mendelsohn RB, Winawer SJ, Jammula A, et al. Adenoma Prevalence in Blacks and Whites Having Equal Adherence To Screening Colonoscopy: The National Colonoscopy Study. Clin Gastroenterol Hepatol 2017;15:1469–1470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Schroy PC 3rd, Coe A, Chen CA, et al. Prevalence of advanced colorectal neoplasia in white and black patients undergoing screening colonoscopy in a safety-net hospital. Ann Intern Med 2013;159:13–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Corley DA, Jensen CD, Marks AR, et al. Variation of adenoma prevalence by age, sex, race, and colon location in a large population: implications for screening and quality programs. Clin Gastroenterol Hepatol 2013;11:172–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.