Abstract
The present study explored in a sample of Flemish pain patients the role of prayer as a possible individual factor in pain management. The focus on prayer as a personal religious factor fits with the current religious landscape in Western-Europe where personal religious factors are more important than organizational dimensions of religion. Our study is framed in the transactional theory of stress and coping by testing first, whether prayer was related with pain severity and pain tolerance and second, whether cognitive positive re-appraisal was a mediating mechanism in the association between prayer and pain. We expected that prayer would be related to pain tolerance in reducing the impact of the pain on patient’s daily life, but not necessarily to pain severity. A cross-sectional questionnaire design was adopted in order to measure demographics, prayer, pain outcomes (i.e., pain severity and pain tolerance), and cognitive positive re-appraisal. Two hundred and two chronic pain (CP) patients, all members of a Flemish national patients association, completed the questionnaires. Correlational analyses showed that prayer was significantly related with pain tolerance, but not with pain severity. However, ancillary analyses revealed a moderational effect of religious affiliation in the relationship between prayer and pain severity as well as pain tolerance. Furthermore, mediation analysis revealed that cognitive positive re-appraisal was indeed an underlying mechanism in the relationship between prayer and pain tolerance. This study affirms the importance to distinguish between pain severity and pain tolerance, and indicates that prayer can play a role in pain management, especially for religious pain patients. Further, the findings can be framed within the transactional theory of stress and coping as the results indicate that positive re-appraisal might be an important underlying mechanism in the association between prayer and pain.
Keywords: Personal religious factors, Prayer, Pain, Pain management
Introduction
Chronic pain (CP) is a stressful condition that can severely impacts patients’ intrapersonal functioning (e.g., depression, suicidal ideation, despair) as well as interpersonal functioning (e.g., job loss, marital problems, social isolation) (Breivik et al., 2006). Chronic pain can negatively influence a patient’s quality of life as well as his or her environment (Roy, 2001). Moreover, traditional pain management strategies do not always alleviate pain or improve quality of life (Breivik et al., 2006; Shi et al., 2007). Therefore, recent research programs have focused on the efficacy and effectiveness of complementary pain relief strategies (Rosenberg et al., 2008).
As part of these complementary pain strategies, the use of spiritual and religious resources has gained increased attention among both patients and practitioners. Chronic pain appears to alter the role of religion and spirituality in patients’ lives as 40% of individuals report they are more religious/spiritual after the onset of a chronic pain condition, compared to 4% who report they are less religious/spiritual (Glover-Graf et al., 2007). Patients frequently use religious factors to cope with chronic pain. In fact, prayer use increases in response to pain (Turner & Clancy, 1986). Glover-Graf et al. (2007) found that pain clinic patients report prayer (61%) as the most frequent response to pain, after taking medication (89%). Dunn and Horgas (2004) identified that religious coping is often used in older adults experiencing chronic pain. Taking into account the sub-optimal effect of traditional pain management and the interest of patients in including religious factors into their pain management treatment, research studying the usefulness of religious factors in pain management seems warranted.
Religious factors in pain management
The role of religious factors in the pain management of chronic pain patients can be framed within the transactional theory of stress and coping (Lazarus & Folkman, 1984). This model states that the impact of stressful events must be understood in terms of how the individual perceives or evaluates these events. This involves two types of appraisal, primary and secondary. In the primary appraisal, the individual makes an evaluation of the situation (‘is this a threat, a challenge, or a harmful event?’). In the secondary appraisal, the individual takes stock of the resources he/she has for meeting the demands of this event. Within this model, the function of religion in the appraisal of events can be twofold. Religion may modify one’s primary appraisal of the pain by offering a framework to appraise the situation. The patient can positively re-asses the meaning of the pain and see it, for example, as an ‘opportunity’ for spiritual growth or as part of the divine plan instead of a threat. Religious re-appraisals can also be negative in nature (e.g., patients can experience their illness as a punishment of God), although most theorizing has focused on the benevolent appraisal possibilities (Koenig et al., 2001). Second, religion can offer additional resources affirming the patient that he or she is able to stand up to the pain (for example, support from a diving being, God taking part in the suffering). It is likely that this re-appraisal of the pain situation can affect the pain experience (Koenig et al., 2001).
Not all aspects of religion are equally valuable cross-culturally in the process of coping with pain. In secularized West-European countries, a focus on personal religious factors may be more useful to patients as organizational dimensions of religion have decreased in importance over time. For example, in Belgium, church attendance and denominational affiliation are very low (Dobbelaere & Voyé, 2000). The majority of the population are not active members of any religious tradition. Despite these low rates of church affiliation and active involvement, most individuals still believe in a transcendent reality and the presence of a divine being, and they affirm to posses a transcendent meaning system (Dezutter et al., 2010). Although these individuals do not feel affiliated with a specific religion or denomination (i.e., in Belgium this is predominantly the Roman Catholic religion), personal religious activities remain important. One personal religious activity that seems very valuable is prayer, and especially prayer is often mentioned as an important aspect in coping (Ai et al., 2007; Cronan et al., 1989). Moreover, several authors theorize that prayer is more likely to be used as a coping resource when problems are more severe, chronic, or unresponsive to other treatments or interventions (McCullough & Larson, 1999). Masters and Spielmans (2007) mention that people tend to pray more when they have exhausted other coping resources or when the situation seems desperate. As chronic pain is indeed a chronic and severe condition, often unresponsive to medical treatment, we can wonder whether prayer can provide a valuable psycho-social coping mechanism for those experiencing chronic pain. Referring to the transactional theory of stress and coping, prayer can be seen as a cognitive act in order to reframe the pain situation in a more positive way. Moments of prayer can offer the patient a demarcated ‘place’ both in time and in space where one can actively re-appraise his situation based on the frame-work of his meaning system. This cognitive processing can stimulate a healthy adaptation to the pain situation.
Prayer, pain severity and pain tolerance
Research on the role of prayer in pain management is scarce among West-European populations. Available European studies (Büssing et al., 2007, 2009) seem to focus on the broader concept of spirituality/religiosity as a relevant resource for patients with chronic pain conditions. To our knowledge, one study did focus on the role of prayer for chronic pain patients in Sweden revealing a positive association between prayer and distress (Andersson, 2008). However, the design of this study was very specific with participants taking part on an internet delivered cognitive behavioral therapy completing the ‘Praying and Hoping’ scale of the Coping Strategies Questionnaire (CSQ) as measurement of prayer. In addition, Sweden is categorized as a low-religiosity area with low levels of prayer in general (Hank & Schaan, 2008).
North-American research on this topic is more prevalent, but these studies seem to focus merely on the role of prayer on pain severity, and not on the impact of prayer on the pain experience. Rosenstiel and Keefe (1983), for example, found a positive relationship between level of pain severity and the Praying factor in the CSQ. This result was replicated in two other cross-sectional studies namely a sample of low back pain patients (Keefe et al., 1990) and in a sample of general pain patients (Tuttle et al., 1991). These suggest that the more intense pain becomes, the more likely people are to use prayer as a coping mechanism; but there is no evidence that this alters the patients’ experience of the intensity of the pain. In a review of the field, Hollywell and Walker (2008) found that private prayer was usually associated with lower levels of depression and anxiety in hospitalised patients. In line with this, Wachholtz and Pearce (2009) reported that the relationship between religious/spiritual coping and pain may be dependent on the way in which the outcome of pain is defined. Specifically, pain severity should be differentiated from pain tolerance. Although both concepts are based on the patient’s pain perception, when they are disentangled, a patient may report that he/she experiences the same intensity of pain but displays better coping with pain. Daily prayer, for example, may serve as a distraction or a shift away from the pain experience towards other aspects of life or to more transcendent beliefs, allowing patients to tolerate the pain for longer periods (Wachholtz et al., 2007). Linked to the stress and coping model of Lazarus and Folkman (1984), we can hypothesize that prayer, as a re-appraisal technique, will create a positive re-appraisal of pain and thus will be more strongly associated with pain tolerance than with pain severity. More concretely, we would expect that the patient feels the same level of pain, but is more able to cope with the pain and the pain would have less interference with his/her daily life.
Purpose of the study
Taking into account previous remarks as well as the recent call for theoretically driven models in prayer-health research (Masters & Spielmans, 2007), our study has two main aims. The first aim is to disentangle pain severity and pain tolerance as separate pain outcomes important for the pain patient. In line with earlier theoretical models, we predict that prayer will be positively related to pain tolerance and thus, reduce the impact that pain has on the CP patient’s daily life whereas we assume that prayer will not have an impact on pain severity. In addition, we want to study the role of religiosity (religious affiliation) in the relationship between prayer and both pain severity and pain tolerance. The second aim is to heed the recent call for theoretically driven research and therefore, we frame our study in the transactional theory of stress and coping. More specifically, we want to test the mediating role of positive religious re-appraisal in the relationship between prayer and pain outcomes. We hypothesize that prayer is closely related to a cognitive activity of positively re-framing the pain situation which, in turn, is associated with more pain tolerance but not necessary with less pain severity.
Method
Participants
The sample consisted of 202 chronic pain patients, members of a national patient organization (Flemish Pain League). This larger umbrella organization includes smaller support and information dissemination groups that organize informative as well as leisure activities for chronic pain patients. The patients association distributed the questionnaires by mail to their members (response rate 45%) and announced the study at their monthly meeting as well as in their journal. Selection criterion of at least six months pain duration was reached by all participants. Anonymity was guaranteed and all participants provided informed consent. The Board of the Flemish Pain League reviewed and approved the study.
A breakdown by gender yielded 71% women and mean age was 52 years (SD = 11.19, range 22–83). Average duration of pain was 15 years (SD = 10.55, range 2–60). There was a wide range of education levels including: primary school (9%), secondary school (52%), higher education (35%), and university (4%), which is representative for the Belgian population (Federal State Department of Economy Belgium, 2010). Eighteen percent of the sample were single, 62% married, 8% cohabited, 3% widowed, and 8% divorced. Religious affiliation reflected a wide range of belief systems: 32% of the sample self-identified as Catholic, 26% as adherents of the Christian tradition, 20% described themselves as believers in a transcendent reality but without any specific church or religious tradition, 13% atheists, 4% agnostics, and 5% others (Muslim, Buddhist). For 25% of the sample, religiosity was not important, for 31% of minor importance, for 28% important, and for 16% very important.
Measurements
Religiosity
Denomination (‘‘what kind of denomination do you have’’), and Importance of Religion (‘‘how important is religion for you’’; 1 = not important, 4 = very important) were measured with each a single item. Denomination and Belief Salience were only assessed for the purpose of sample description.
Prayer
Prayer was measured with a single item (‘‘How often do you pray?’’; 1 = never, 2 = seldom, 3 = sometimes, 4 = often).
Pain
Besides pain duration (measured with a single item for the purpose of sample description), pain severity was measured with three questions (‘‘what is the level of pain at this moment’’, ‘‘what was the highest pain level last week’’, and ‘‘what was the lowest pain level last week’’ (Bush et al., 1999). Questions were scored on a 10-point scale (1 = no pain at all, 10 = very high levels of pain). Principal component analysis was performed and the scree test (Cattell, 1966) pointed to a one-factor solution. This solution explained 73% of the total variance and one component had an eigenvalue over Kaiser’s criterion of 1. The factor loadings on this component were respectively .90, .79, and .86 for the three items, meeting the criterion level of .40. Cronbach’s alpha was .81. In line with Bush et al. a composite pain index was obtained through the mean of these items.
In order to measure the pain tolerance, 8 items are created for use in this study. We based our items on the Disability Scale of the Chronic Pain Grade Questionnaire (Von Korff et al., 1992) but reformulated and extended them in order to measure a broader range of more specific life domains where pain can impact. The final 8 items gauged to an evaluation of the tolerance of pain in different aspects of the patient’s life such as vocational (‘‘Despite my pain condition, I was able to carry out my job/run the house.’’), social (‘‘Despite my pain condition, I was able to meet friends’’), and family aspects (Despite my pain condition, I visited my family). By broadening the domains of the original Disability Scale we try to cover more aspects which are or can be important for a patient. Response possibilities ranged from 1 (totally disagree) to 5 (totally agree). Cronbach’s alpha was .84. Principal component analysis was performed and the scree test (Cattell, 1966) pointed to a one-factor solution. This one-factor solution explained 50% of the total variance and all the factor loadings on this factor were above the criterion level of .40.
Cognitive positive re-appraisal
Cognitive re-appraisal was measured with the Positive Reinterpretation and Growth Scale of the Coping Orientation to Problems Experienced Inventory (COPE, Carver et al., 1989). The scale exists of 4 items (e.g., ‘‘I learn something from the experience’’) measuring positive re-appraisal with response possibilities ranging from 1 = (never) to 5 = (very often). Cronbach’s alpha was .85.
Results
Preliminary analyses
Descriptive analyses of the study variables showed that the mean level for pain tolerance was 3.11 (range 1–5, SD = 0.78), for pain severity 5.94 (range 1–9; SD = 1.66), and for re-appraisal 3.37 (range 1–5, SD = .84). Mean-level analyses showed no significant differences between men and women concerning pain tolerance, pain severity, prayer, and re-appraisal (Hotelling’s trace = .03, F (4, 186) = 1.22, ns). To include the level of education in the analyses a dummy variable was created (0 = primary and secondary level, 1 = higher education). No differences were found between lower or higher educated patients on pain tolerance, pain severity, prayer, and re-appraisal (Hotelling’s trace = .04, F (4, 185) = 1.62, ns). Correlations between study variables and background variables can be found in Table 1. Age was not significantly correlated with pain tolerance, pain severity or re-appraisal, whereas age was significantly related with prayer (r = .24, P < .001). Educational level and duration of pain were not significantly correlated with pain tolerance, pain severity, re-appraisal, or prayer.
Table 1.
Correlations among the study variables and background variables
| Pain severity | Pain tolerance | Prayer | Re-appraisal | Pain duration | Age | Education | |
|---|---|---|---|---|---|---|---|
| Pain severity | – | ||||||
| Pain tolerance | −.41** | – | |||||
| Prayer | −.01 | .18* | – | ||||
| Re-appraisal | −.12 | .45** | .33** | – | |||
| Pain duration | −.05 | .12 | .08 | .04 | – | ||
| Age | −.02 | .05 | .24** | .06 | .40** | – | |
| Education | −.15 | .15 | .05 | .02 | .06 | −.13 | – |
P < .05
P < .01
As hypothesized, prayer was significantly correlated with pain tolerance (r = .18, P < .05) and with re-appraisal (r = .33, P < .001). Prayer was not correlated with pain severity (r = −.01, ns). Furthermore, re-appraisal was significantly related with pain tolerance (r = .45, P < .001), whereas it not related with pain severity (r = −.12, ns).
Primary analyses
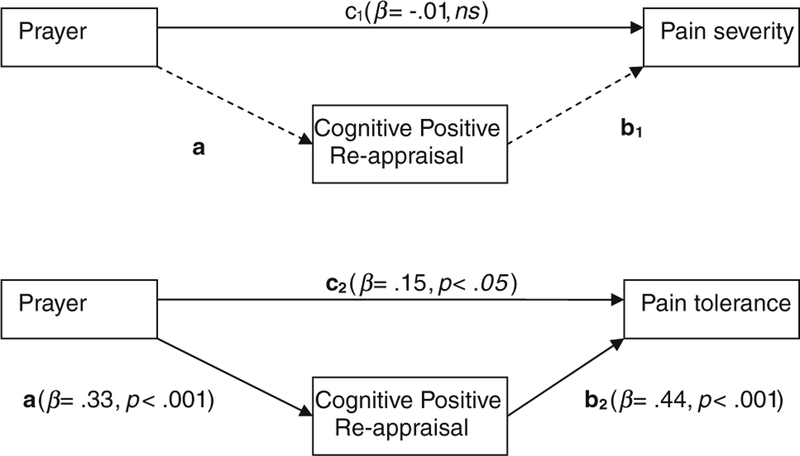
Mediation analysis was performed based on the causal steps strategy of Baron and Kenny (1986). Referencing the paths depicted in Fig. 1, linear regression was used to determine whether prayer was related significantly to pain severity and to pain tolerance (direct effects, path c1 and c2); whether prayer was significantly related to the mediator (re-appraisal, path a), and whether the mediator was related significantly to pain severity and pain tolerance (path b1 and b2). Because the background variables (age, educational level, and pain duration) were not significantly related with the dependent variables (pain tolerance and pain severity) or with the mediator, these variables were not inserted in the regression equation. The effect of prayer on pain severity was not significant (path c1; β = −.01, ns), whereas the effect of prayer on pain tolerance was significant (path c2; β = .15, P < .05). Because prayer had no significant effect on pain severity, the remaining steps of the mediation analysis are only performed for pain tolerance as dependent variable. Prayer had a significant effect on re-appraisal (path a, β = .33, P < .001) and re-appraisal on pain tolerance (path b2, β = .44, P < .001). The effect of prayer on pain tolerance was reduced markedly and became statistically non-significant when controlled for the effect of re-appraisal (path c’2; β = .01, ns) indicative of a full mediation effect.
Fig. 1.
Causal steps mediation test
Next, simple mediation was tested using Preacher and Hayes (2004) bootstrapping methodology for indirect effects. This bootstrapping procedure assumes that the distribution of the measured variables approximates that of the population while it avoids making the often-tenuous assumption that the indirect effect is distributed normally. Interpretation of the bootstrap data is accomplished by determining whether zero is contained within the 95% CI (thus indicating lack of significance). The indirect effect was found to be significant (point estimate = .11, 95% BC CI: .06–.16 with 3,000 resamples) indicating that the indirect effect significantly differed from zero and, thus, that the relationship between prayer and pain tolerance may be mediated by re-appraisal. Sobel test affirmed the mediational effect of cognitive re-appraisal in the association between prayer and pain tolerance (Sobel z = 3.79, P < .001).
Ancillary analyses
In a next set of analyses, we explored further the role of religiosity (religious affiliation) in the relationship between prayer and pain. Therefore, moderation analyses with a dummy coded variable (0 = religious non-affiliated patients, n = 35; 1 = religious affiliated patients, n = 166) were performed to examine the impact of religiosity on the relationship between prayer and pain severity on the one hand and between prayer and pain tolerance on the other hand.
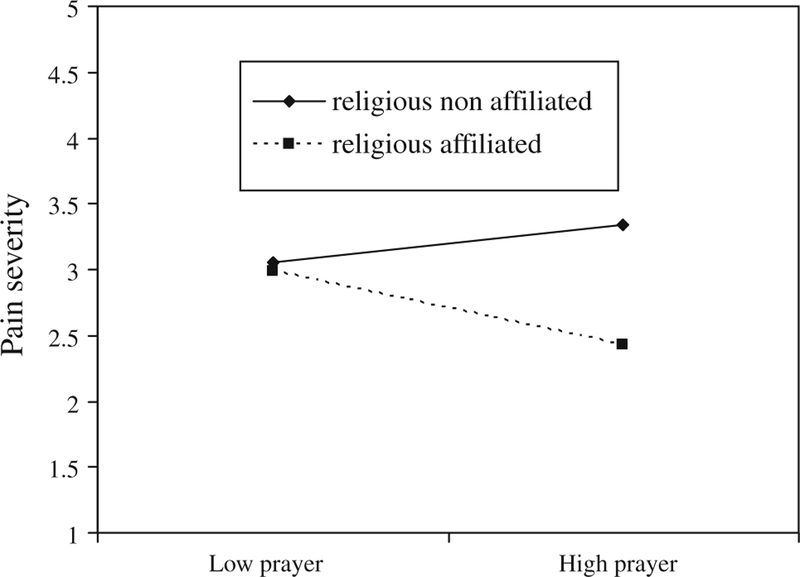
In the first moderational analysis, prayer and the dummy coded variable of religiosity were entered as simultaneous predictors of pain severity in Step 1 of the hierarchical regression analyses. The interaction term, created by multiplying the centered means of the predictors (Aiken & West, 1991), was entered in Step 2. Results indicated that the interaction significantly added to the prediction (Δ R2 = .03, F (1,195) = 6.97, P < .01) and revealed a significant regression coefficient (β = .27, P < .01). Graphical representation of this interaction effect (Fig. 2) showed that prayer is especially important for religious affiliated persons for whom high levels of prayer results in lower pain severity.
Fig. 2.
Simple slopes of prayer predicting pain severity at varying levels of religiosity
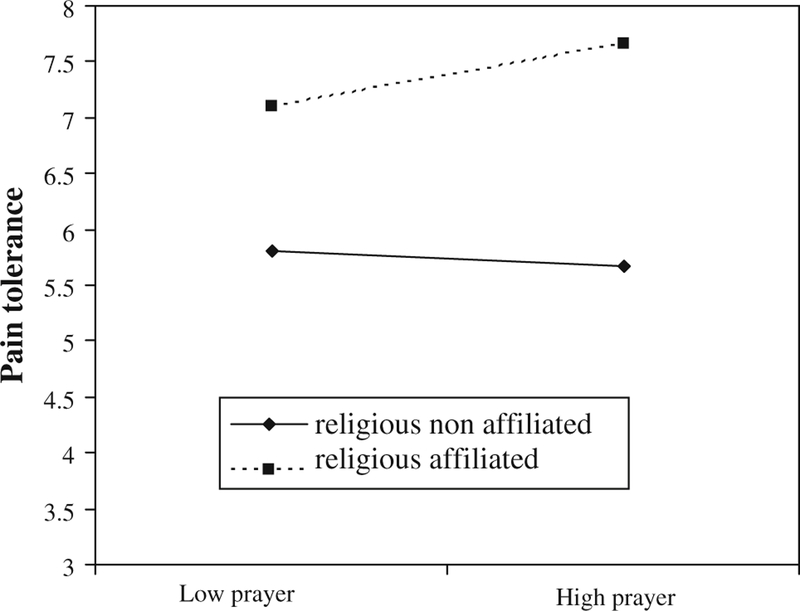
In the second moderational analysis, prayer and the dummy coded variable of religiosity were entered as simoultaneous predictors of pain tolerance in Step 1 and the interaction term was entered in Step 2. Results indicated that the interaction was significant (Δ R2 = .03, F (1,191) = 5.88, P < .05) and revealed a significant regression coefficient (β = −.25, P < .05). Graphical representation of this interaction effect (Fig. 3) showed that high levels of prayer are related with more pain tolerance in the group of religious affiliated persons.
Fig. 3.
Simple slopes of prayer predicting pain tolerance at varying levels of religiosity
Finally, in a last set of moderational analysis, the role of religiosity was investigated in the association between the mediator (i.e., cognitive re-appraisal) and pain tolerance. Results revealed that the interaction between cognitive re-appraisal and religiosity is not significant in the prediction of pain tolerance (Δ R2 = .00, F (1,189) = .17, P = .68) indicating that the relation between cognitive re-appraisal and pain tolerance is not influenced by religious affiliation.
Discussion
The aim of this study was to focus on the under-investigated aspect of personal religious factors, especially prayer, in the pain management of West-European CP patients. We framed our study in the transactional theory of stress and coping (Lazarus & Folkman, 1984) and we tested the mediational role of re-appraisal in the association between prayer and pain. Furthermore, based on previous studies (Keefe et al., 1990) as well as on theorizing that there are multiple forms of pain outcomes (Wachholtz & Pearce, 2009), we distinguished between pain severity and pain tolerance, with the latter indicating how pain impacts on the CP patient’s ability to maintain their general activities of daily living.
In line with earlier theoretical models, we hypothesized that prayer will be associated with pain tolerance, but not necessary with pain severity. Furthermore, we expected cognitive re-appraisal to be a mediating factor in the relation between prayer and pain tolerance. Our findings seem to support our hypotheses. First, correlational analyses showed that prayer is indeed positively related to pain but only to pain tolerance, and not to pain severity. This affirms the need to distinguish between the two forms of pain outcomes. However, ancillary moderation analyses showed that the relationship between prayer and pain severity as well as between prayer and pain tolerance is depending on the religiosity of the pain patient. Taking into account the religious affiliation of the pain patient, a more detailed picture appeared. Results indicated that for religious affiliated patients high levels of prayer were related with lower levels of pain severity whereas this is not the case for religious non affiliated patients. Furthermore, for this group of religious affiliated patients high levels of prayer were also related with more pain tolerance. These findings might indicate that prayer can be a useful factor in pain management but only for pain patients who are religious. It seems that prayer has to be incorporated in the religious meaning system of the patient before it can function as a tool in pain management. This is in line with earlier research (Dezutter et al., 2010) showing that a central religious meaning system can function as a buffer for the negative impact of pain on the life satisfaction of pain patients. In this study, the life satisfaction ratings of patients who reported a very central religious meaning system were not negatively influenced by higher levels of pain. Conversely, when the religious meaning system was reported as trivial, pain severity compromised life satisfaction ratings. We might assume that for a religious pain patient his or her religious meaning system can be a readily available source in coping with the pain. Prayer, then, can be a useful tool offered by this meaning system.
Second, mediation analyses showed that the cognitive activity of positive re-appraisal mediated the relationship between prayer and pain tolerance. The full mediational effect indicates that prayer is not related to pain tolerance directly, but that the psychological/cognitive process alters the impact of pain on daily life activities. Moreover, prayer seems to function as a positive re-appraisal technique for the CP patient. We assume that the CP patient, by praying, reframes his pain condition in more positive and meaningful terms. This process is also described by Park (2005, 2006) who stated that religiousness is associated with appraised meaning of stressors and with subsequent adjustment. The prayer activity offers the CP patient the opportunity to re-interpret his/her pain condition within his/her religious meaning framework, re-establishing a sense of meaningfulness and purpose in his/her life despite the pain. Although Park (2006) focuses on other personal aspects of religion (e.g., intrinsic religiousness), it is likely that the same underlying mechanism is present in the relation between prayer and pain tolerance.
Limitations and conclusion
There are several shortcomings to the study. First, it is possible that the participants, by virtue of their membership in a patients’ association, are more active than most individuals in the CP population. This attitude may have indicated a tendency to use more proactive coping strategies and thus, use prayer as a positive coping technique. Future studies should consider a more diverse group of CP patients, including those who are undergoing pain treatment or those who are hospitalized. Second, our study focused especially on frequency of prayer whereas some recent research indicates that other aspects of prayer are important as well. Poloma and Pendleton (1991), for example, pointed to the different types of prayer and state that these differences determine the experiential consequences of prayer such as general well-being. Moreover, Krause (2004) showed that attitudes towards prayer may be important variables relating to psychological outcomes. In one of his studies, for example, higher levels of self-esteem were found for adults who believed that only God knows when and how prayers should be answered than for adults who expected prayers to be answered immediately. Therefore, future studies should consider addressing different styles and content of prayer and the relationship of different prayer types with pain outcomes, including any moderating/mediating effects of these distinct aspects. Moreover, attention should be paid to negative re-appraisal aspects of prayer as well. Further, the instruments used to measure pain severity and pain tolerance were assessments with no comparison psychometrics. Future research need to validate these instruments. Next, as in most chronic pain research, we assumed that the pain condition is a stressful situation but we did not measure this explicitly which can be seen as a drawback in the study. Future research should advantage to implement a stress measure in order to gauge the level of stress. Finally, the cross-sectional design limits our study, and these limits are especially noteworthy in prayer research. The underlying question in most prayer studies is ‘does prayer influence health’. Cross-sectional studies, however, can only inform whether prayer is related to health, but is not able to identify causality in this relationship. Of course, the prayer–health dynamic can be a reciprocal process whereby higher levels of pain lead to higher use of prayer which, in turn, decreases the detrimental effect of pain on daily life. However, these kinds of mechanisms are only identifiable in longitudinal studies.
Despite these limitations, this study offers new perspectives in the field of prayer and pain. It first affirms the importance to distinguish between pain outcomes because pain severity and pain tolerance likely have separate bio-psycho-social pathways. The results, furthermore, might indicate that prayer has a positive relationship with pain tolerance for CP patients. Finally, this study shed light on a possible underlying mechanism in the association between prayer and pain tolerance. Framed in the transactional theory of stress and coping, re-appraisal of the pain situation seems to be an important factor for understanding the relationship between prayer and pain tolerance. We hope that these findings can stimulate further research on prayer in the field of CP clarifying the possible role of personal religious activities in the pain management of patients.
Contributor Information
Jessie Dezutter, Department of Psychology, Catholic University of Leuven, Tiensestraat 102 bus 3715, 3000 Leuven, Belgium.
Amy Wachholtz, University of Massachusetts Medical School, Worcester, MA, USA.
Jozef Corveleyn, Department of Psychology, Catholic University of Leuven, Tiensestraat 102 bus 3715, 3000 Leuven, Belgium; Free University of Amsterdam, Amsterdam, The Netherlands.
References
- Ai A, Park C, Huang B, Rodgers W, & Tice T (2007). Psychosocial mediation of religious coping styles: A study of short-term psychological distress following cardiac surgery. Personality and Social Psychology Bulletin, 33, 866–882. [DOI] [PubMed] [Google Scholar]
- Aiken LS, & West SG (1991). Multiple regression: Testing and interpreting interactions Newbury Park, CA: Sage. [Google Scholar]
- Andersson G (2008). Chronic pain and praying to a higher power: Useful or useless. Journal of Religion and Health, 47, 176–187. [DOI] [PubMed] [Google Scholar]
- Baron RM, & Kenny DA (1986). The moderator-mediator variable distinction in Social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology, 51, 1173–1182. [DOI] [PubMed] [Google Scholar]
- Breivik H, Collett B, Ventafridda V, Cohen R, & Gallacher D (2006). Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. European Journal of Pain, 10, 287–333. [DOI] [PubMed] [Google Scholar]
- Bush E, Rye M, Brant C, Emery E, Pargament K, & Riessinger C (1999). Religious coping with chronic pain. Applied Psychophysiology and Biofeedback, 24, 249–260. [DOI] [PubMed] [Google Scholar]
- Büssing A, Michalsen A, Balzat HJ, Grünther RA, Ostermann T, Neugebauer EAM, & Matthieseen PF (2009). Are spirituality and religiosity resources for patients with chronic pain conditions? Pain Medicine, 10, 327–339. [DOI] [PubMed] [Google Scholar]
- Büssing A, Ostermann T, & Koenig H (2007). Relevance of religion and spirituality in german patients with chronic diseases. International Journal of Psychiatry in Medicine, 37, 39–57. [DOI] [PubMed] [Google Scholar]
- Carver C, Scheier M, & Weintraub J (1989). Assessing coping strategies: A theoretically based approach. Jornal of Personality and Social Psychology, 56, 267–283. [DOI] [PubMed] [Google Scholar]
- Cattell R (1966). The scree test for the number of factors. Multivariate Behavioral Research, 1, 245–276. [DOI] [PubMed] [Google Scholar]
- Cronan T, Kaplan R, Posner L, Blumberg E, & Kozin F (1989). Prevalence of the use of unconventional remedies for arthritis in a metropolitan community. Arthritis and Rheumatism, 32, 1604–1607. [DOI] [PubMed] [Google Scholar]
- Dezutter J, Robertson L, Luyckx K, & Hutsebaut D (2010). Life satisfaction in chronic pain patients: The stress-buffering role of centrality of religion. Journal for the Scientific Study of Religion, 49, 507–516. [DOI] [PubMed] [Google Scholar]
- Dobbelaere K, & Voyé L (2000). Religie en kerkbetrokkenheid: Ambivalentie en vervreemding [Religion and church involvement: Ambivalence and alienation]. In Dobbelaere K, Elchardus M, Kerkhofs J, Voyé L, & Bawin-Legros B (Eds.), Verloren zekerheid: De Belgen en hun waarden, overtuigingen en houdingen (pp. 117–152). Tielt: Lannoo. [Google Scholar]
- Dunn K, & Horgas A (2004). Religious and nonreligious coping in older adults experiencing chronic pain. Pain Management Nursing, 5, 19–28. [DOI] [PubMed] [Google Scholar]
- Federal State Department of Economy Belgium. (2010). Training and education [Data file] Retrieved from http://statbel.fgov.be/nl/statistieken/cijfers/arbeid_leven/opleiding/index.jsp
- Glover-Graf N, Marini I, Baker J, & Buck T (2007). Religious and spiritual beliefs and practices of persons with chronic pain. Rehabilitation Counseling Bulletin, 51, 21–33. [Google Scholar]
- Hank K, & Schaan B (2008). Cross-national variations in the correlation between frequency of prayer and health among older Europeans. Research on Aging, 30, 35–54. [Google Scholar]
- Hollywell C, & Walker J (2008). Private prayer as a suitable intervention for hospitalised patients: A critical review of the literature. Journal of Clinical Nursing, 18, 637–651. [DOI] [PubMed] [Google Scholar]
- Keefe F, Crisson J, Urban B, & Williams D (1990). Analyzing chronic low back pain: The relative contribution of pain coping strategies. Pain, 40, 293–301. [DOI] [PubMed] [Google Scholar]
- Koenig H, Mc Cullough M, & Larson D (2001). Handbook of religion and health Oxford: University Press. [Google Scholar]
- Krause N (2004). Assessing the relationships among prayer expectancies, race, and self-esteem in late life. Journal for the Scientific Study of Religion, 43, 395–408. [Google Scholar]
- Lazarus R, & Folkman S (1984). Stress, appraisal, and coping New York: Springer. [Google Scholar]
- Masters K, & Spielmans G (2007). Prayer and health: Review, meta-analysis, and research agenda. Journal of Behavioral Medicine, 30, 329–338. [DOI] [PubMed] [Google Scholar]
- McCullough M, & Larson D (1999). Prayer. In Miller WR (Ed.), Integrating spirituality into treatment (pp. 85–110). Washington: American Psychological Association. [Google Scholar]
- Park C (2005). Religion as a meaning making framework in coping with life stress. Journal of Social Issues, 61, 707–729. [Google Scholar]
- Park C (2006). Exploring relations among religiousness, meaning, and adjustment to lifetime and current stressful encounters in later life. Anxiety, stress, and coping, 19, 33–45. [Google Scholar]
- Poloma M, & Pendleton B (1991). The effects of prayer and prayer experiences on measures of general well-being. Journal of Psychology and Theology, 19, 71–83. [Google Scholar]
- Preacher K, & Hayes A (2004). SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior Research Methods, Instruments, & Computers, 36, 717–731. [DOI] [PubMed] [Google Scholar]
- Rosenberg E, Inginia G, Chen I, Mechaber A, Wood J, Faselis C, et al. (2008). Complementary and alternative medicine use by primary care patients with chronic pain. Pain Medicine, 9, 1065–1072. [DOI] [PubMed] [Google Scholar]
- Rosenstiel A, & Keefe F (1983). The use of coping strategies in chronic low back pain patients: Relationship to patient characteristics and current adjustment. Pain, 17, 33–44. [DOI] [PubMed] [Google Scholar]
- Roy R (2001). Social relations and chronic pain New York: Plenum Publishers. [Google Scholar]
- Shi Q, Langer G, Cohen J, & Cleeland C (2007). People in pain: How do they seek relief? The Journal of Pain, 8, 624–636. [DOI] [PubMed] [Google Scholar]
- Turner J, & Clancy S (1986). Strategies for coping with chronic low back pain: Relationships to pain and disability. Pain, 24, 355–364. [DOI] [PubMed] [Google Scholar]
- Tuttle D, Shutty M, & DeGood D (1991). Empirical dimensions of coping in chronic pain patients: A factorial analysis. Rehabilitation Psychology, 36, 179–187. [Google Scholar]
- Von Korff M, Ormel J, Keefe F, & Dworkin S (1992). Grading the severity of chronic pain. Pain, 50, 133–149. [DOI] [PubMed] [Google Scholar]
- Wachholtz A, & Pearce M (2009). Does spirituality as a coping mechanism help or hinder coping with chronic pain? Current Pain and Headache Reports, 13, 127–132. [DOI] [PubMed] [Google Scholar]
- Wachholtz A, Pearce M, & Koenig H (2007). Exploring the relationship between spirituality, coping, and pain. Journal of Behavioral Medicine, 30, 311–318. [DOI] [PubMed] [Google Scholar]